Abstract
A common challenge encountered with both traditional and digitally produced dentures involves the extraction of artificial teeth from the denture base. This narrative review seeks to present an updated perspective on the adherence of synthetic teeth for denture base materials, employing diverse methods. Dental technicians often employ chemical approaches and mechanical techniques (including abrasion, laser treatment, and abrasive blasting) to augment the retention of denture teeth. However, the efficacy of these treatments remains uncertain. In certain instances, specific combinations of Denture Base Resin (DBR) materials and artificial teeth exhibit improved performance in conventional heat-cured dentures following these treatments. The primary reasons for failure are attributed to material incompatibility and inadequate copolymerization. As new denture fabrication techniques and materials continue to emerge, further research is imperative to identify optimal tooth-DBR combinations. Notably, 3D-printed tooth–DBR combinations have demonstrated reduced bond strength and less favorable failure patterns, while utilizing milled and traditional combinations appears to be a more prudent choice until advancements in additive manufacturing enhance the reliability of 3D-printing methods.
Keywords:
3D-printing; artificial teeth; CAD/CAM; milling; denture base polymers; complete dentures; adhesion 1. Introduction
To meet the social and physiological needs of edentulous patients, complete dentures are frequently employed as an economical solution, replacing the complete set of teeth and associated structures in either the upper or lower jaw [1]. While traditional complete dentures remain the most common approach, modern manufacturing techniques have been implemented in clinical practice to accelerate denture production, simplify production, and lower overall expenses [2,3].
In addition to traditional techniques like heat curing and self-curing, advanced technologies now enable the production of dentures, including both additive and subtractive processes [4,5]. The additive method involves fabricating the denture by building layer upon layer with 3D-printing methods including stereolithography (SLA) or digital light processing (DLP), achieving precise resin layers (ranging from 20 to 150 μm) [6]. Furthermore, additive monolithic manufacturing utilizing material jetting technology has been introduced, enabling the simultaneous printing of different materials with various colors and properties into a single, unified unit. This technique operates by extruding a UV-curable photopolymer liquid in layered form, employing multiple nozzles to handle different materials and colors at once, which are then immediately cured with UV light [7].
Conversely, the subtractive approach employs computer-aided design and computer-aided manufacturing (CAD/CAM), guiding cutting tools via computer numerical control to mill the material. The introduction of additive monolithic manufacturing presents a significant advancement, as it eliminates the need for adhesives by allowing different materials to be printed together in a cohesive unit, thereby enhancing the durability and performance of the denture.
Understanding the types of bonds involved in bonding artificial teeth to denture bases is crucial for optimizing dental prosthetic fabrication techniques. Various bonding techniques are utilized in dentistry, each with distinct characteristics impacting bond strength and durability. In conventional dentures, common bonding techniques include heat curing, self-curing, and microwave curing. Heat polymerization, a form of heat curing, is often favored due to its ability to produce strong bonds [8]. This method involves placing the denture in a heated environment, causing the resin to polymerize and form strong covalent bonds between the denture base and artificial teeth. The heat facilitates optimal resin flow and adhesion, resulting in enhanced mechanical properties and longevity of the denture. In digital workflows, such as CAD/CAM (Computer-Aided Design/Computer-Aided Manufacturing), teeth can be separately fabricated through 3D printing or milling processes before being bonded to the printed denture base. This approach allows for precise customization and alignment of teeth, improving aesthetics and potentially reducing prosthesis failures [9]. The bonding of acrylic teeth to a printed denture base can involve various techniques, including adhesive bonding with resin-based materials or mechanical retention through surface roughening and conditioning. Chemically, these bonding processes rely on interactions such as covalent bonds formed between the resin matrix of the denture base and the bonding agent used to affix the teeth [6]. Covalent bonds involve the sharing of electron pairs between atoms, resulting in strong and stable connections. Surface preparation techniques, such as sandblasting or chemical etching, enhance bonding by increasing surface area and promoting mechanical interlocking or chemical adhesion. Physically, mechanical retention plays a role in bonding strength when teeth are mechanically interlocked with the denture base. This can occur through features like undercuts or grooves in the denture base that physically engage with corresponding features on the artificial teeth [3]. A notable challenge with complete removable dentures is the separation of teeth from the denture base, occurring in 22–30% of conventional removable dentures, particularly around the anterior teeth [10]. The effectiveness of bonding relies on the contact between the denture tooth and the polymerizing denture base material. Improving the adhesive area through surface treatments such as alumina abrasive blasting or macro-retentive elements, such as grooves and inverted cones, enhances the contact region, establishing mechanical interlocking between teeth and denture base [11,12].
With the increased use of dental implants, acrylic resin has become more important in implant restorations [13,14]. Findings indicate that fractures of acrylic teeth are a prevalent complication among patients with prosthetic restorations on implants [15]. With the increased prevalence of osseointegrated implants, the acrylic resin has seen extended use in implant restorations, and highlighting the criticality of the adhesion between dental resin and the PMMA base is essential in restorations such as overdenture implants and combined implant structures [7]. Given their exposure to higher chewing loads, these constructions require high strength to ensure reliability for clinicians.
A variety of commercially available Denture Base Resins (DBRs) and denture teeth are utilized in removable denture manufacturing [16]. However, the specific process used for creating denture teeth can influence their adherence to DBRs. The adhesive strength can be evaluated according to International Standard Organization (ISO) standards, which outline material specifications and testing procedures [17,18]. Despite the introduction of novel manufacturing techniques like CAD/CAM and 3D printing for denture production, there is a current lack of investigations to verify the bonding efficacy of additive and subtractive manufactured denture bases to artificial teeth. Regardless of the method employed, it is crucial to consider the strength of the bond [19,20].
This review aims to provide an up-to-date analysis of the adhesion of denture teeth to resin substrates in traditional and digitally fabricated complete dentures. It also discusses the factors that influence adhesive strength in traditional and modern manufacturing methods.
- Search Strategy and Study Selection
Following the PRISMA guidelines, a comprehensive search of PubMed, Scopus, EMBASE databases, and the grey literature was conducted without imposing any specific time constraints. The search strategy employed a variety of terms related to denture fabrication and adhesion, including ‘artificial teeth’ and ‘bond strength’, ‘complete removable dentures’ and ‘adhesion’, ‘3D printed teeth’ and ‘complete denture’, ‘CAD-CAM teeth’ and ‘complete denture’, ‘milled teeth’ and ‘complete denture’, ‘acrylic teeth’ and ‘complete denture’, and ‘denture teeth’ and ‘denture base’ and ‘adhesion’.
- Inclusion and Exclusion Criteria
The inclusion criteria were focused on retrieving in vitro studies published in English that examined the adhesion, bonding, or detachment of denture teeth and materials. Articles were excluded if they did not provide relevant data on these aspects, or if they focused on removable partial dentures or partial dental prostheses.
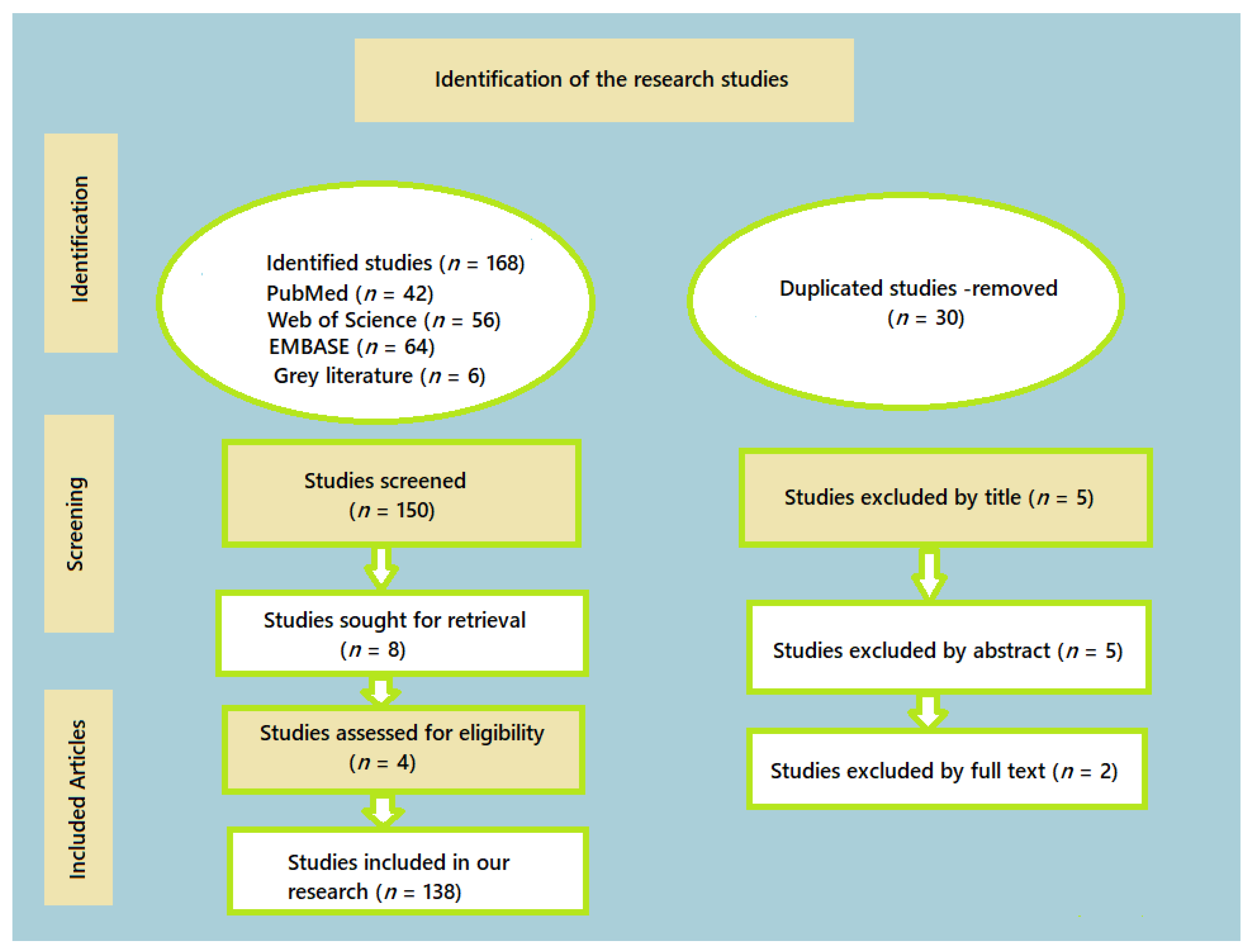
Out of the initial pool of 168 articles screened, 138 articles met the following inclusion criteria and were taken into account for the review:
- -
- Written in English;
- -
- Published between 1989 and 2024;
- -
- Focused on the adhesion resistance between artificial teeth and denture base for complete removable dentures, including clinical and in vitro studies;
- -
- Provided information on various manufacturing methods, properties, and clinical assessments involving traditional, 3D–printed, and milled complete removable dentures.
- Manual Search
To ensure the comprehensiveness of our review, we also conducted a manual search of all included articles and relevant reviews. This additional step aimed to identify any pertinent studies that may have been missed in the initial database searches (Figure 1).
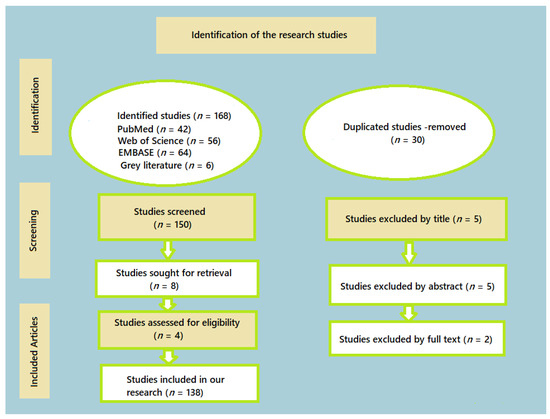
Figure 1.
The configuration of the study undertaken.
- Selection Process
Throughout the selection process, we meticulously documented the number of articles selected and refined at every stage. The period from 1 January 1993 to 31 April 2024, was chosen because of the heightened accessibility of clinical and in vitro studies during this time frame. This thorough methodology ensured that only the pertinent and superior literature was included in the review. Table 1 lists the articles that were selected, highlighting those that were most pertinent to the subject matter.

Table 1.
The most relevant articles incorporated in the study.
2. Mechanism of Adhesion of Artificial Prefabricated Teeth to Traditional PMMA Denture Base
From a standpoint in clinical practice, the dislodgment of teeth from removable complete or partial dentures, particularly in the anterior region, can lead to patient discomfort and often requires immediate dental attention. The causes of tooth detachment may arise from errors in the denture manufacturing steps, issues related to the types of materials used (both teeth and denture base resin), or excessive forces applied during chewing [21]. The long-term reliability of these prosthetic devices is crucial for achieving greater patient satisfaction [22].
Reports indicate that a substantial number of denture repairs, exceeding 60% of annually produced dentures, are linked to issues of tooth detachment [19]. Similar findings are reiterated in other studies, emphasizing that one of the most prevalent types of repairs involves the debonding of artificial teeth in removable dentures [23]. While excessive pressure on the occlusal surface during chewing may contribute to tooth detachment, the literature suggests the presence of other contributing factors.
A significant explanation for the breakdown of the adhesion between denture teeth and the base is associated with surface contamination on the teeth [24], impeding the establishment of a strong bond. Contaminants typically include traces of wax absorbed during polymerization or residual material left at the base of the artificial teeth during the denture’s investment. However, Spartley’s research contradicts this perspective, indicating that residual material on teeth does not significantly affect adhesion strength if wax elimination is performed at temperatures of at least 90 °C [8]. Debonding may also result from variations in surface properties where the tooth meets the base. This incompatibility is believed to arise from either surface contamination or structural disparities between the two components due to distinct fabrication methods [22,23,24,25]. Research indicates that tooth detachment contributes to 22–30% of denture repairs, especially in the front section, although there is no differentiation made between fracture and debonding [26].
The repair process may involve creating an inverted cone within the denture tooth, a technique commonly employed by many dental technicians before introducing heat-cured acrylic, to address these challenges more effectively [27,28]. Another contributing factor may involve the routine use of disinfectants or cleaning chemicals, which have the potential to alter the mechanical and physical characteristics of both DBR and the teeth [29,30,31]. This alteration can lead to a weakening of the bond between them, resulting in detachment [32].
Concerning material-related aspects impacting the connection between artificial denture teeth and Denture Base Resin (DBR) materials, these factors include differences in the composition and polymerization technique of the denture base, the type of acrylic teeth employed, and the preparation of their interfacial surfaces [33]. The primary process governing the adhesion involves the expansion of the polymer induced through the dispersion of a suitable solvent. The rate of diffusion is dependent on factors such as time, temperature, solvent, polymer structure, and the polymer’s glass transition temperature [34].
Since denture teeth are pre-polymerized, achieving chemical co-polymerization to establish interconnected polymer chains with any denture base material is challenging due to the very low concentration of free radicals [22]. Additionally, the adhesion of denture base resin to denture teeth is attributed to the involvement of unreacted methyl-methacrylate groups. However, this cannot be verified in cold-cured materials because residual double bonds remain unreacted at room temperature [35]. Although PMMA conventional acrylic achieves a high level of double-bond conversion and generates a significant number of reactive free radicals, the low concentration of free radicals in pre-polymerized resin teeth does not guarantee adhesion to PMMA denture bases [36]. To address this challenge, several approaches have been explored to enhance the bond strength at the interface. These approaches involve the creation of micro- or macro-mechanical interlocking or the initiation of some form of a chemical interaction occurring between various polymer types [37].
3. Mechanism of Adhesion of 3D-Printed and Milled Artificial Teeth to Denture Base
In the conventional production of removable dentures, the adhesion between denture bases and teeth is accomplished via PMMA polymerization, which happens upon contact with the artificial teeth, resulting in an intertwined polymer network. Nonetheless, the digital denture process usually entails digitally designing and separately manufacturing bases and artificial teeth, subsequently bonding them together using a bonding agent, surface conditioning, or the usage of auto-polymerizing PMMA resin [38].
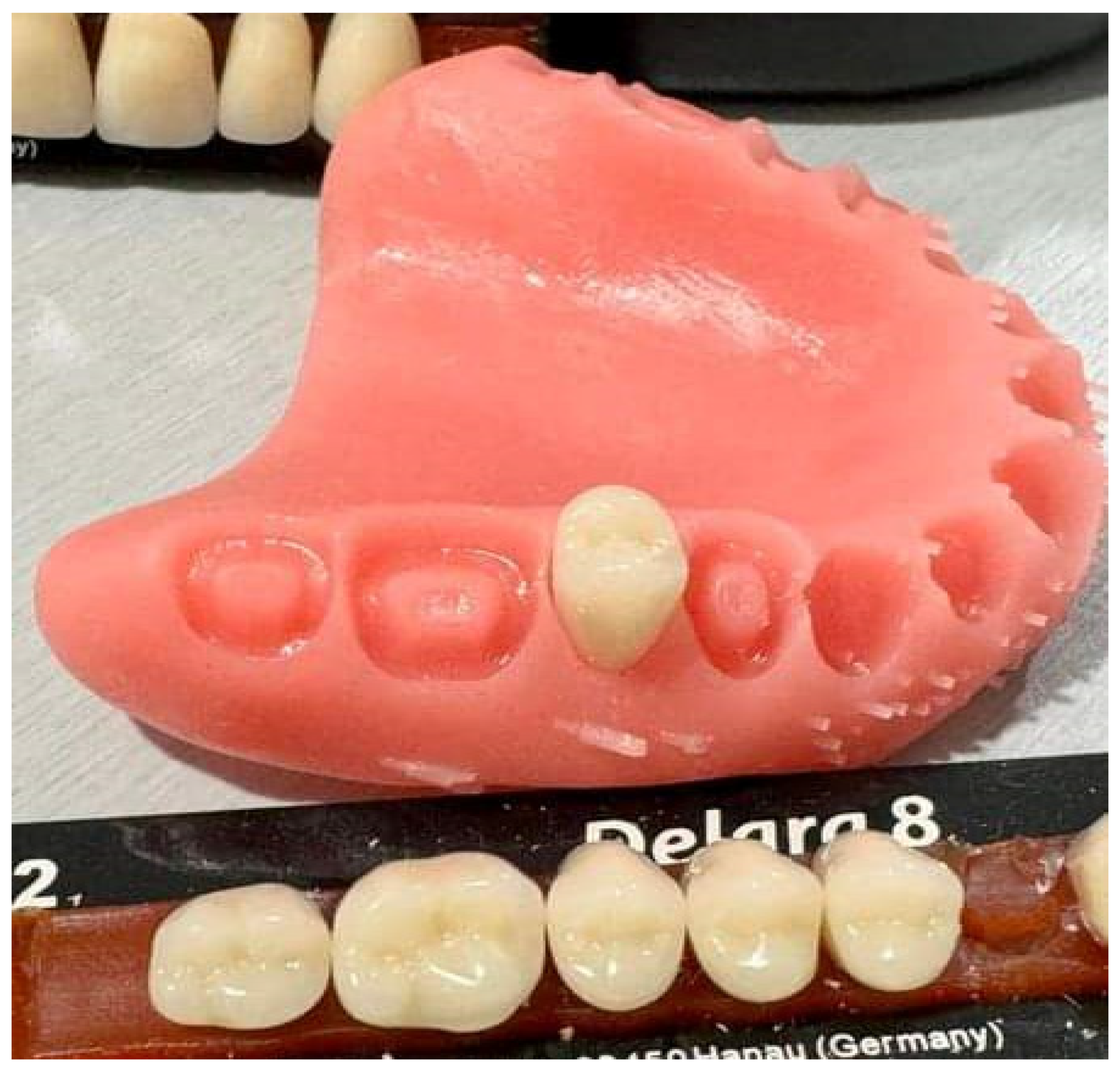
Pre-made or milled teeth are bonded to the denture base either through adhesive application or by bonding with resin cured through cold and heat methods. With 3D-printed dentures, the base is initially printed, followed by the separate printing of teeth in a subsequent stage [39]. The artificial teeth can be attached to the denture base utilizing a designated adhesive agent or resin that has not undergone polymerization, which is then solidified using light. The teeth can be bonded individually or fused and bonded as one unit (Figure 2). Alternatively, artificial denture teeth can be adhered to a printed denture base using specialized bonding agents and sealants [40].

Figure 2.
Artificial prefabricated tooth—second premolar (Delara, Heraeus Kulzer, Hanau, Germany) placed in the socket of the 3D-printed upper denture base (NextDent Denture 3D+, NextDent, 3D Systems, Soesterberg, The Netherlands). Source of the figure: clinical case from the author; no copyright concerns.
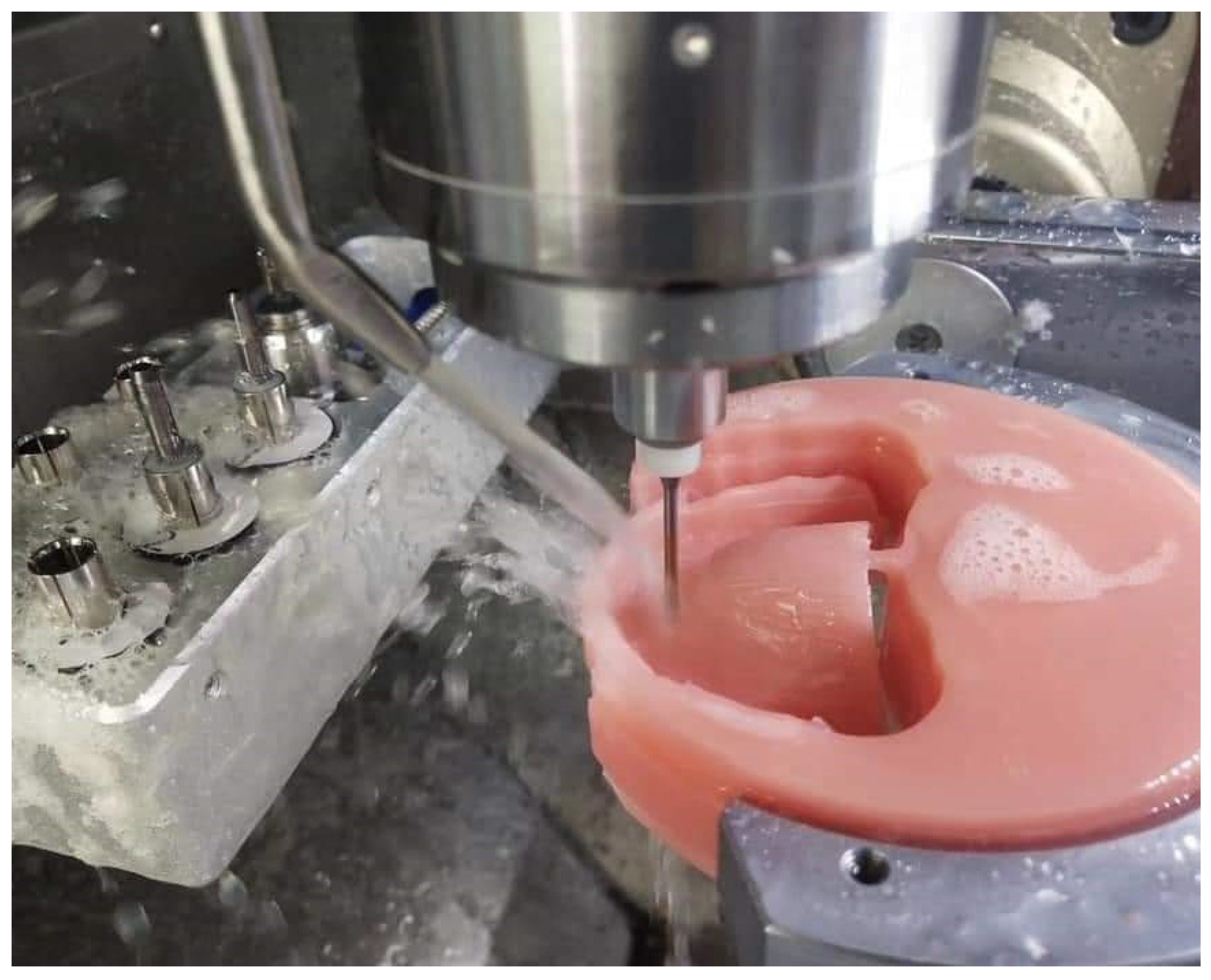
Lately, there have been developments in monolithic digital denture solutions. The additive technique revolutionizes manufacturing by facilitating the simultaneous printing of an array of materials, each possessing unique colors and properties, that are seamlessly fused into a single, unified entity [7]. Manufacturers now provide teeth and denture base materials, both made of high-quality PMMA, on two-toned discs (pink and white) (Figure 3). These materials are intended to undergo milling together in a unified milling operation [41]. Throughout the industrial manufacturing process, both materials are polymerized concurrently, creating a direct chemical adhesion and removing the necessity for additional bonding materials and processes [42,43].
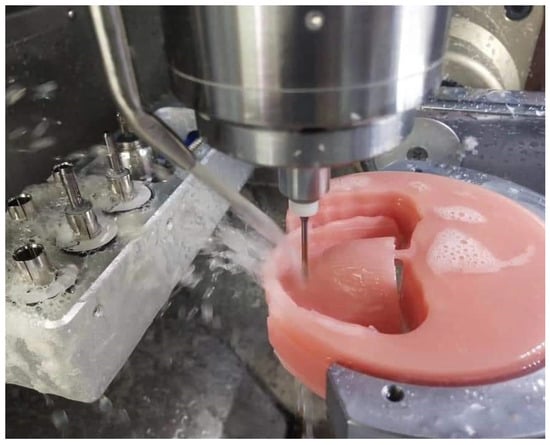
Figure 3.
Fabrication of a complete removable denture using a PMMA disc through a milling process (Ivotion Denture System, Ivoclar Vivadent, Schaan, Liechtenstein). Source of the figure: clinical case from the author; no copyright concerns.
The recent literature indicates that the connection between 3D-printed denture bases and separately printed teeth is less robust compared to traditional methods (Figure 4) [44,45,46]. One study demonstrated that the printed group exhibited both cohesive and adhesive breakdowns, while the traditionally processed group only showed cohesive failures, implying a stronger bond in the conventionally processed denture group [47]. Despite limited investigation in this domain, it seems that printed dentures generally display diminished bond strength. Further research is necessary to evaluate whether this has clinical relevance, and a comparison of different adhesive techniques should be undertaken, as several adhesive procedures have been suggested [35,48].
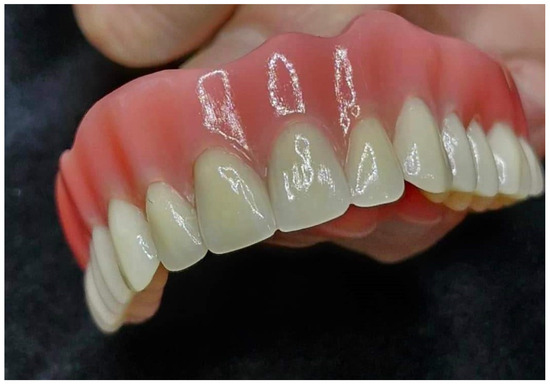
Figure 4.
A 3D-printed denture with a separately manufactured base and artificial teeth (NextDent Denture 3D+, NextDent, 3D Systems, Soesterberg, The Netherlands). Source of the figure: clinical case from the author; no copyright concerns.
Presently, there are limited in vitro investigations examining the adhesion strength of denture teeth across heat-processed and contemporary-processed denture bases. Choi et al. [49] conducted a study comparing four distinct varieties of commercial denture teeth (PMMA, cross-linked PMMA, PMMA incorporating nanofillers, and 3D printed) with three types of DBRs (heat-cured, milled, and 3D printed). Their results revealed that heat-polymerized denture base resins still offer the greatest bond strength and fracture toughness, notwithstanding the growing popularity of CAD-milled and 3D-printed materials [50].
Prpić et al. [51] conducted a study comparing the shear bond strengths between various denture base resins and different types of prefabricated teeth, including acrylic, nanohybrid composite, and cross-linked teeth, as well as CAD/CAM-produced denture teeth. Their findings revealed that cold-cured resin exhibited the lowest values among the different polymerization methods [52].
Remarkably, there was no significant difference in shear bond strength values between CAD/CAM (milled) denture base resins and heat-cured resins. The bond strengths were comparable when milled and heat-cured denture base resins were bonded to various types of prefabricated teeth [53]. This suggests that the primary factor influencing bond strength was the polymerization process of the denture base resin. Given the variability in bonding strength between removable denture bases and denture teeth based on material combinations, the authors recommended avoiding the use of cold-cured resin for attaching prefabricated teeth to a denture base [54,55].
4. Approaches to Enhance the Adhesion Resistance between Denture Base and Artificial Teeth
Researchers have explored various methods to enhance the attachment between denture base and teeth. Most of these approaches require preparation of the surface in the bonding region of the artificial tooth [56,57,58]. The strength of the connection is affected by both the type of artificial teeth and the composition of the denture bases [59]. In simple terms, the chemical makeup of pre-polymerized artificial denture teeth influences the surface treatment process. Additionally, the composition of the denture base material and the polymerization techniques utilized also affect the bonding capability of pre-made artificial teeth.
Typically, approaches to modifying the surface of a prefabricated artificial tooth are grounded in principles of micro-mechanical retention, chemical co-polymerization, and managing polymerization shrinkage in polymers [39,60].
Chemical treatments function by utilizing polymerizable monomers to soften the surface of the acrylic tooth, enabling them to permeate the acrylic material. Monomers from the polymerized resin of the base material then infiltrate the acrylic resin of the denture teeth, causing surface expansion [61]. The thickness of this layer, resulting from the interaction of monomers with polymer particles and the resin matrix, appears crucial for the strength of adhesion between the PMMA of the teeth and the base resin. Upon polymerization, these monomers form a network of polymer chains that interconnect the two polymers [62]. Various chemical modifications have been explored to improve the bond between teeth and denture base materials (Table 2).
Numerous researchers have explored different treatments for acrylic teeth, including the application of liquid methyl methacrylate (MMA) [62,63,64,65] or a mixture of MMA and methylene chloride [66,67,68]. Spratley et al. [8] found that the placement of monomer on the cervical region of the teeth did not seem to impact bond strength. Similarly, Barpal et al. [69] observed that treatment of the surface of acrylic teeth with MMA monomer either decreased bond strength or had no discernible effect on the adhesion resistance of the thermosetting PMMA resin to the denture base when applied for 30 s prior to applying the resin layers.

Table 2.
Investigations assessing the adhesion between artificial teeth and denture base substances.
Table 2.
Investigations assessing the adhesion between artificial teeth and denture base substances.
| Type of Artificial Teeth | Type of Denture Base Material | Type of Chemical Treatment | Type of Mechanical Treatment | References |
|---|---|---|---|---|
| PMMA teeth | Heat-polymerized resin Auto-polymerized resin | MMA, 180 s | Using 120-grit sandpaper for grinding, create two grooves and a retention hole with a diameter of 1.5 mm, F = 10 MPa | Vallittu et al., 1997 [22] |
| PMMA teeth Composite teeth Nanocomposite teeth | Heat-cured resin | MMA | N/A | Gharebagh et al., 2019 [56] |
| 3D-printed teeth, Prefabricated acrylic teeth | 3D-printed denture resin, Heat-cured resin | MMA, 3D-printed resin, Auto-polymerized acrylic resin | 400–1200-grit SiC paper, F = 10 MPa | Cleto et al., 2022 [63] |
| PMMA teeth, Composite teeth | Heat-cured resin, CAD/CAM-milled | DCM, PMMA-based bonding agent | Roughening with bur 250 m Al2O3, 15 s, 4.8 bars, 10 mm, F = 10 MPa | Helal et al., 2022 [30] |
| PMMA teeth, 3D-printed teeth | Heat-cured resin, Milled PMMA resin 3D-printed resin | Self-curing Bonding agent, Uncured 3D-printing resin | N/A | Choi et al., 2020 [49] |
| PMMA teeth | Heat-cured resin | MMA DCM | 250 m Al2O3, 4.8 bars, 5 s, 5 mm 5 mm, F = 10 MPa | Viegas et al., 2021 [53] |
| 3D-printed teeth, Prefabricated composite teeth, Milled teeth | Heat-cured resin Milled PMMA resin 3D-printed resin | 3D tooth conditioning agent, 4 min, 40 C + light-cured bonding agent | N/A | Mohamed et al., 2022 [43] |
| PMMA teeth Artificial teeth Milled teeth | Heat-cured resin Cold-cured resin PMMA resin produced by milling | PMMA-based bonding | N/A | Prpić et al., 2020 [51] |
| Acrylic teeth | Heat-polymerized resin | MMA | 50 mm Al2O3, 20 s Diatoric cavity 1.5 mm, F = 10 MPa | Barpal et al., 1998 [69] |
| Acrylic teeth | Auto-polymerized resin | Methyl methacrylate (MMA), 3 min Composite bonding agent 37% phosphoric acid etchant + Methyl methacrylate MMA + composite bonding agent | F = 10 MPa, Grinding at low speed (0.5 mm/s) | Yanikoglu et al., 2002 [25] |
Morrow et al. [70] indicated that applying a monomer–polymer mixture to the unmodified cervical region of denture teeth reduced the bond strength, which aligns with findings by Dimitrova et al. [71], who observed decreased bonding when monomer was applied to the tooth surface with self-curing acrylic resin. Palitsch et al. [72] found that using MMA in combination with light-cured denture base materials resulted in inadequate adhesion performance, consistent with the existing literature. They attributed these outcomes to factors such as the limited penetration of denture base resin (DBR) into MMA-treated tooth surfaces, the viscous nature of the denture base material hindering micromechanical interlocking, or the insufficient copolymerization between MMA and the bifunctional monomers in light-cured DBR materials [73,74]. These variations in the results can be attributed to differences in testing methods and the materials used for denture base and teeth.
Apart from MMA, various chemical substances have been investigated. Sorensen and Fjeldstad [75] reported an improved bond resistance when acrylic teeth were treated with suitable solutions like ethyl acetone or monomer. Takahashi et al. [76] discussed the beneficial effects of dichloromethane (CH2Cl2), an organic solvent capable of breaking down PMMA polymer structure, on enhancing the retention of both conventional and cross-linked acrylic teeth. In a related study, dichloromethane significantly increased the tooth bond strength, tripling the initial value observed in untreated teeth. This solvent expanded the external surface volume of acrylic resin in the teeth, facilitating the infiltration of polymerizable acrylic resin monomers from the base into artificial teeth and forming a comprehensive interlaced polymer network [77,78]. The increased mechanical retention resulting from the micro-roughness observed on tooth surfaces treated with dichloromethane may contribute to the higher bond strength [79]. Suzuki et al. [80] observed a significant improvement in bonding when administering 4-META adhesive agents on extensively cross-linked teeth before packing the resin dough. Fletcher-Stark et al. [81] studied a notable increase in bond strength in IPN denture teeth when an adhesive agent (Eclipse, Ottawa, ON, Canada; Dentsply, Charlotte, NC, USA) was used in conjunction with a light-polymerized UDMA resin, but this enhancement was not observed when paired with a heat-polymerized PMMA resin.
Another adhesive agent utilized for attaching the denture base materials to acrylic teeth is methylacetate, commercially known as Eclipse Bonding Agent (Eclipse; Dentsply) [82]. In research by Akin et al. [83], its application did not yield an optimal bond strength when paired with a conventional denture base. Nonetheless, in a subsequent investigation conducted by the same researchers [84], significant improvements in bond strength were observed when it was paired with light-cured denture base materials. The same bonding agent was tested alongside a dichloromethane-based bonding agent for its effectiveness in bonding to a light-cured DBR. It demonstrated effectiveness only when utilized alongside a surface that had been mechanically roughened [85].
Nishigawa et al. [86] used an adhesive bonding substance composed of 85% MMA and 15% low-molecular-weight polyethylmethacrylate (PEMA). They found that this adhesive significantly increased the shear bond strength between DBR and artificial denture teeth, even without sandblasting, and maintained the highest bond strength even after 100 days of water immersion. Specifically, interfaces that were sandblasted and treated with this additional adhesive agent retained their strength notably well after prolonged water exposure. Perea et al. [87] conducted experiments using four different monomer systems to evaluate the shear bond strength between PMMA denture base resin (DBR) and acrylic resin denture teeth. These systems included flowable composite resin, methyl methacrylate (MMA), stick resin, and composite primer. All materials, except MMA, contained a photopolymerizable initiator system. It was observed that a strong bond could be achieved when these monomer systems were given sufficient time to effectively dissolve the polymer network of acrylic teeth [88,89]. Furthermore, there have been suggestions to improve the overall contact surface area between the two polymer materials by adjusting macro-mechanical retention and roughness. Sandblasting, a conventional technique used before cementing base metal and zirconia restorations, is a common method to achieve this [90]. It appears that sandblasting improves the bonding strength of both denture teeth made of acrylic and ceramic. Other approaches involve altering the adhesive region through mechanical abrasion or by creating macro-retentive patterns. Research has shown that vertical grooves reduce stress concentration at the interface between the tooth and base material [91,92]. Additionally, the inclusion of two aligned grooves and one retention aperture has been found to enhance the tensile strength of denture teeth in the base material. An investigation conducted by Akin et al. [84] did not utilize grooves but ground the bonding surface with a tungsten carbide bur for generating regions with macro-retentive features. They also explored alternative mechanical treatments, such as Er: YAG laser and airborne-particle abrasion using 120 µm Al2O3 particles at a pressure of 2 bar for 10 s and found that all these mechanical pretreatment methods effectively improve the adhesion strength. Chung et al. [93] integrated sandblasting using 250 µm Al2O3 particles with grinding and observed that this combination notably enhances the bond strength due to the increased surface area and mechanical interlocking [94].
On the other hand, Cardash et al. [95] observed varying effects on bond effectiveness in artificial teeth with a mechanically altered cervical portion, with both increases and decreases noted. Cunningham et al. also mentioned that adding grooves and grinding the tooth surface can be effective even in the absence of a thorough dewaxing [96].
5. Impact of Various Denture Base Materials on Bond Efficiency
Denture base materials are typically classified based on their method of polymerization [97]. Several types of denture base materials have been developed, including heat-cured, visible-light-cured, microwave-cured, cold-cured, and pour-type denture base materials. Poly (methyl methacrylate) (PMMA) is the most commonly used material for Denture Base Resin (DBR) due to its widespread acceptance, despite its relatively low mechanical strength [85]. To improve the mechanical properties of PMMA denture base resin (DBR) and reduce the risk of fractures, various additives have been explored. These include rubber, glass, polyethylene, and polypropylene fibers, as well as alumina, titanium, zirconia, silver, silica-based, and hydroxyapatite fillers [98].
One drawback of PMMA is its potential to cause allergies in patients sensitive to the methyl methacrylate monomer [99]. As an alternative to PMMA, light-polymerized resins were introduced, which consist of dimethacrylates such as Bis-GMA, TEGDMA, and UDMA [100]. However, these light-polymerized resins have shown a lower bond strength with denture teeth, often requiring the use of bonding agents [101]. Composite materials offer advantages such as easier processing and a reduced risk of allergic reactions [102]. Depending on the specific material used, particular conditioning solutions are recommended for chemically preparing resin denture teeth. The primary function of a conditioning liquid is believed to be its ability to penetrate the bonding surface and solubilize and/or swell it, thereby facilitating a chemical bond with the denture base material [79,83].
Artificial teeth generally form stronger bonds with heat-cured acrylic resins compared to self-cured acrylic resins. This is attributed to the more thorough polymerization process in heat-cured acrylic resins, as noted by some researchers [89]. Others suggest that the higher polymerization temperature in heat-cured acrylic resins promotes monomer diffusion into the teeth, resulting in an enhanced adhesion performance [103].
The various types of artificial teeth and the different materials used in denture bases influence the strength of their bond. Recently introduced highly cross-linked artificial teeth offer significantly improved properties such as an enhanced fracture resistance, abrasion resistance, and color stability [104]. However, traditional acrylic teeth typically establish a stronger bond with the resin base of the denture compared to highly cross-linked acrylic teeth. To ensure the copolymerization process during the manufacture of acrylic teeth, manufacturers incorporate a less cross-linked polymer in the cervical part. According to a study [105], conventional acrylic teeth have more non-crosslinked polymer chains available for bonding to the denture base.
Clancy et al. [89] evaluated the adhesion strength of light-cured and heat-cured resins with both conventional acrylic teeth and abrasion-resistant teeth. They found that the most effective combination was heat-cured resin with conventional acrylic teeth, exhibiting a higher bond strength compared to abrasion-resistant teeth with IPN (interpenetrating polymer network) properties. In contrast, the bond strength with light-cured resin was consistently lower for both types of teeth [106]. In the study conducted by Saponaro et al. [107], a pour-type Denture Base Resin (DBR) was bonded to both traditional and cross-linked denture teeth and evaluated before and after undergoing thermal cycling. The researchers found no significant differences between the groups, either before or after thermal cycling. They highlighted the effectiveness of dichloromethane in improving adhesion strength even after thermal cycling. Dichloromethane works by causing swelling in the resin of denture teeth, which allows deeper penetration of monomers and strengthens their network. Additionally, it induces micro-roughening on the surface, thereby enhancing micromechanical bonding [108]. Evaluating the adhesion resistance of each possible combination is a substantial undertaking, given the extensive array of teeth and denture base materials available in the market. Instead, a more effective approach might involve assessing the bonding characteristics of both “matched” and “mismatched” combinations of teeth and denture base materials [109]. There is limited literature suggesting that a stronger bond may be attained when both the Denture Base Resin (DBR) and denture teeth are manufactured by the same company [110,111,112]. In a study conducted by Tanoue et al. [113], NHC teeth with various DBR materials were tested, which showed notably lower adhesion performance when paired with denture bases from different manufacturers, despite their chemical similarity.
6. Discussion
This narrative review has summarized the findings from in vitro studies investigating the bonding effectiveness between traditional and modern combinations of artificial teeth and denture base materials. While there is an abundant literature on studies involving traditional materials and methods, research on CAD/CAM and 3D-printed teeth remains scarce. However, challenges in synthesizing and extrapolating findings arise from variations in experimental design, specimen preparation, material combinations, sample sizes, and other factors.
In the conventional process of fabricating removable full dentures, denture base resins derived from methyl methacrylate monomers can be polymerized into PMMA using methods such as heat, chemical agents, visible light, and microwave energy [114]. Despite their relative speed, these methods often leave residual free monomers due to incomplete polymerization. Additionally, heat-polymerized dentures may exhibit porosities caused by factors like inadequate mixing, excessive heating, evaporation of unreacted monomer, or insufficient pressure during polymerization [115]. In contrast, milled dentures are crafted from pre-polymerized PMMA blocks known for their minimal shrinkage, high density, and low porosity. These materials lack residual monomers because of their more thorough transformation process and effective polymerization. It has been noted that free monomers present during manufacturing can affect the adhesive strength between denture teeth and Denture Base Resins (DBRs) [116]. Consequently, traditional processing methods may provide better adhesion compared to bonds formed with pre-polymerized modern materials [117]. Choi et al. [49] found that following the manufacturer’s instructions for conventional and CAD/CAM complete denture fabrication results in a 2.5-fold increase in free monomer concentration at the interface, initiating the bonding process in heat-polymerized dentures compared to pre-polymerized CAD/CAM materials. This higher concentration of free monomers could explain the weaker bond strength observed in CAD/CAM specimens in their study. Specific research indicates that the bond strength between artificial teeth and heat-cured resins is greater than that of self-cured acrylic resins [118,119,120,121]. In a study by Takahashi et al. [76], heat-cured and microwave-processed Denture Base Resins (DBRs) were compared with a poured PMMA DBR resin. The heat-cured DBR exhibited the best results, highlighting a significant difference. Both heat-cured and microwave-processed DBRs exhibited a superior bond strength compared to pour-type resin [122,123,124,125]. Similar findings were reported by Damade et al. [126] in their tensile tests, where they assessed the bonding of cross-linked acrylic teeth using heat and microwave polymerization methods. The materials utilized for artificial teeth in both removable complete and partial dentures primarily comprise heat-activated poly (methyl methacrylate) (PMMA) grains integrated within a cross-linked PMMA matrix [127]. Additionally, highly cross-linked polyacrylic resins incorporate uniformly dispersed inorganic microfillers that polymerize within the matrix, forming materials such as interpenetrating polymer networks (IPN) or nanohybrid composite resins. These include blends of UDMA matrix with inorganic SiO2 fillers and clusters of PMMA [128].
The manufacturing method that builds dentures by adding material layer by layer can introduce flaws and pores due to inadequate packing between the layers. These imperfections have the potential to impact the mechanical performance of the bonded interface [129,130]. It has been proposed that the orientation of applied loads, particularly concerning the printing configuration, could heighten the risk of artificial teeth detachment, frequently leading to adhesive-type fractures at the interface [131]. Cleto et al. [63] have proposed that using a methyl-methacrylate monomer may be more effective compared to other bonding agents like auto-polymerizing or 3D-printing resin. However, the monolithic additive manufacturing method successfully addresses these challenges linked with conventional layer-by-layer fabrication techniques, particularly the problem of bonding teeth to the denture base [132,133]. By employing a unified printing process, this technique eradicates the necessity for adhesives entirely. This seamless integration is accomplished by meticulously layering materials, resulting in the teeth and base melding into a unified structure with each successive layer [134,135,136]. Consequently, the prevalent risks of separation or detachment between teeth and base, typically encountered in traditional denture construction, are essentially eradicated [137,138].
Given the conflicting findings observed in the limited studies, there is a clear necessity for further research to determine if there is a consistent trend in the prevalence of modern techniques over traditional ones. Furthermore, the inconsistencies in methodologies used to assess the actual bond strength between denture teeth and denture bases, combined with irregular adherence to ISO guidelines, hinder the ability to systematically analyze the findings across the studies included.
7. Conclusions
In summary, ongoing debates persist regarding the most effective combination, as different studies yield conflicting results. Some studies indicate that composite teeth bond to PMMA base materials more effectively than acrylic teeth, while others propose the opposite. Future research should explore new materials and processes to address the problem of artificial teeth detachment from denture bases. Moreover, the increasing popularity of 3D-printing removable dentures, thanks to their ease of production, the capacity to create complex dentures, and cost-efficiency, underscores the necessity to optimize bonding protocols for modern 3D-printed teeth to ensure long-lasting bonds.
Author Contributions
Conceptualization, M.D. and A.V.; methodology, M.D.; software, R.K.; validation, A.V. and R.K.; formal analysis, M.D.; investigation, A.V.; resources, I.H. and R.K.; data curation, M.D.; writing—original draft preparation, M.D.; writing—review and editing, A.V.; visualization, A.V. and I.H.; supervision, I.H. and R.K.; project administration, R.K.; funding acquisition, I.H. and R.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Medical University of Plovdiv, Bulgaria.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| CAD/CAM | Computer-aided design and computer-aided manufacturing |
| CCD | Conventional complete dentures |
| DCM | Dichloromethane |
| DBR | Denture base resin |
| DCMA | Glacial acetic acid |
| DLP | Digital light processing |
| GA | Glacial acetic acid |
| IPN | Interconnected penetrating network |
| ISO | International Standard Organization |
| MA | Methacrylic acid |
| MMM | Monomethyl methacrylate monomer |
| MMRP | Microfillers polymerized into the matrix |
| MMA | Methyl-methacrylate |
| PEMA | Polyethylmethacrylate |
| PMMA | Polymethyl-methacrylate |
| SBS | Shear bond strength test |
| SLA | Stereolithography |
| TCM | Trichloromethane |
| UDMA | Urethane-dimethacrylate |
References
- Stierman, B.; Afful, J.; Carroll, M.D.; Chen, T.C.; Davy, O.; Fink, S.; Fryar, C.D.; Gu, Q.; Hales, C.M.; Hughes, J.P.; et al. National Health and Nutrition Examination Survey 2017–March 2020 Prepandemic Data Files-Development of Files and Prevalence Estimates for Selected Health Outcomes. National Health Statistics Reports. 2021. Available online: https://stacks.cdc.gov/view/cdc/106273 (accessed on 15 September 2023).
- Zitzmann, N.U.; Scherrer, S.S.; Weiger, R.; Lang, N.P.; Walter, C. Preferences of dental care providers in maintaining compromised teeth in relation to their professional status: Implants instead of periodontally involved maxillary molars? Clin. Oral Implants Res. 2011, 22, 143–150. [Google Scholar] [CrossRef]
- Wagner, B.; Kern, M. Clinical evaluation of removable partial dentures 10 years after insertion: Success rates, hygienic problems, and technical failures. Clin. Oral Investig. 2000, 4, 74–80. [Google Scholar] [CrossRef]
- Driscoll, C.F.; Freilich, M.A.; Guckes, A.D.; Knoernschild, K.L.; Mcgarry, T.J.; Goldstein, G.; Goodacre, C.; Guckes, A.; Mor, S.; Rosenstiel, S.; et al. The Glossary of Prosthodontic Terms. J. Prosthet. Dent. 2017, 117, e1–e105. [Google Scholar]
- Marra, J.; De Souza, R.F.; Barbosa, D.B.; Pero, A.C.; Compagnoni, M.A. Evaluation of the bond strength of denture base resins to acrylic resin teeth: Effect of thermocycling. J. Prosthodont. 2009, 18, 438–443. [Google Scholar] [CrossRef]
- Punj, A. Digital Dentistry for Complete Dentures a Review of Digital Dentistry versus Conventional Approaches to Complete Dentures. Decis. Dent. 2020, 26, 12–20. [Google Scholar]
- Mohamed, A.; Takaichi, A.; Kajima, Y.; Takahashi, H.; Wakabayashi, N. Physical Properties of Additively Manufactured Tooth-Colored Material Attached to Denture Base-Colored Material in a Printed Monolithic Unit. Polymers 2023, 15, 2134. [Google Scholar] [CrossRef]
- Spratley, M.H. An investigation of the adhesion of acrylic resin teeth to dentures. J. Prosthet. Dent. 1987, 58, 389–392. [Google Scholar] [CrossRef]
- Chung, Y.J.; Park, J.M.; Kim, T.H.; Ahn, J.S.; Cha, H.S.; Lee, J.H. 3D printing of resin material for denture artificial teeth: Chipping and indirect tensile fracture resistance. Materials 2018, 11, 1798. [Google Scholar] [CrossRef]
- Schneider, R.L.; Curtis, E.R.; Clancy, J.M.S. Tensile bond strength of acrylic resin denture teeth to a microwave- or heat-processed denture base. J. Prosthet. Dent. 2002, 88, 145–150. [Google Scholar] [CrossRef]
- Darbar, U.R.; Huggett, R.; Harrison, A. Denture fracture—A survey. Br. Dent. J. 1994, 176, 342–345. [Google Scholar] [CrossRef]
- van Dam, J.P.B.; Abrahami, S.T.; Yilmaz, A.; Gonzalez-Garcia, Y.; Terryn, H.; Mol, J.M.C. Effect of surface roughness and chemistry on the adhesion and durability of a steel-epoxy adhesive interface. Int. J. Adhes. 2020, 96, 102450. [Google Scholar] [CrossRef]
- Koksal, T.; Dikbas, I. Colour Stability of Different Denture Teeth Materials against Various Staining Agents. Dent. Mater. J. 2008, 27, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Bahrani, F.; Khaledi, A.A.R. Effect of surface treatments on shear bond strength of denture teeth to denture base resins. Dent. Res. J. 2014, 11, 114–118. [Google Scholar]
- Jemt, T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in edentulous jaws: A study of treatment from the time of prosthesis placement to the first annual checkup. Int. J. Oral Maxillofac. Implants 1991, 6, 270–276. [Google Scholar] [PubMed]
- Feine, J.S.; Carlsson, G.E.; Awad, M.A.; Chehade, A.; Duncan, W.J.; Gizani, S.; Head, T.; Heydecke, G.; Lund, J.P.; MacEntee, M.; et al. The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Gerodontology 2002, 19, 3–4. [Google Scholar]
- ISO 20795-1:2013(en); Dentistry—Base Polymers—Part 1: Denture Base Polymers. ISO-International Organization for Standardization: Geneva, Switzerland, 2013.
- ISO/TS 19736:2017; Dentistry—Bonding Test between Polymer Teeth and Denture Base Materials. ISO-International Organization for Standardization: Geneva, Switzerland, 2017.
- Cunningham, J.L.; Benington, I.C. Bond strength variation of synthetic resin teeth in dentures. Int. J. Prosthodont. 1995, 8, 69–72. [Google Scholar] [PubMed]
- Teodorescu, C.; Preoteasa, E.; Preoteasa, C.T.; Murariu-Magureanu, C.; Teodorescu, I.M. Perception and attitudes of dentists regarding the complications of conventional acrylic dentures and overdentures supported by teeth or implants. J. Med. Life 2022, 15, 1031–1037. [Google Scholar] [CrossRef]
- Matos, A.O.; Costa, J.O.; Beline, T.; Ogawa, E.S.; Assunção, W.G.; Mesquita, M.F.; Consani, R.X.; Barão, V.A. Effect of Disinfection on the Bond Strength between Denture Teeth and Microwave-Cured Acrylic Resin Denture Base. J. Prosthodont. 2018, 27, 169–176. [Google Scholar] [CrossRef]
- Vallittu, P.K.; Ruyter, I.E. The swelling phenomenon of acrylic resin polymer teeth at the interface with denture base polymers. J. Prosthet. Dent. 1997, 78, 194–199. [Google Scholar] [CrossRef]
- Kiteska, B.; Funduk, N.; Cevc, P.; Jesih, A.; Anžlovar, A.; Kopač, I. The influence of free-radical concentration on the shear bond strength of dental composites. Mater. Tehnol. 2018, 52, 177–182. [Google Scholar] [CrossRef]
- Burtscher, P. Stability of radicals in cured composite materials. Dent. Mater. 1993, 9, 218–221. [Google Scholar] [CrossRef] [PubMed]
- Yanikoglu, D.N.; Duymus, D.Z.; Bayindir, D.F. Comparative bond strengths of autopolymerising denture resin and light cured composite resin to denture teeth. Int. Dent. J. 2002, 52, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Adeyemi, A.A.; Lyons, M.F.; Cameron, D.A. The acrylic tooth-denture base bond: Effect of mechanical preparation and surface treatment. Eur. J. Prosthodont. Restor. Dent. 2007, 15, 108–114. [Google Scholar] [PubMed]
- Baghani, M.T.; Yahyazadehfar, N.; Zamanian, A.; Abbasi, K.; Shanei, F.; Shidfar, S.; Zohri, Z.; Baghani, M.T.; Yahyazadehfar, N.; Zamanian, A.; et al. Factors affecting bonding strength of artificial teeth: A literature review. J. Res. Med. Dent. Sci. 2018, 6, 184–191. [Google Scholar]
- Boonpitak, K.; Wongkamhaeng, K.; Sanpanyawai, P.; Somsat, N.; Aunaumporn, A.; Klaisiri, A. Experimental Article Comparative effect of Different Surface Treatments on the Shear Bond Strength between 3D-printed Artificial Acrylic Teeth and 3D-printed Denture Based Resins. J. Int. Dent. Med. Res. 2022, 15, 1416–1421. [Google Scholar]
- Al-Somaiday, H.M.; Rafeeq, A.K.; Al-Samaray, M.E. Effect of Different Surface Modifications of Acrylic Teeth and Thermocycling on Shear Bond Strength to Polycarbonate Denture Base Material. Int. J. Biomater. 2022, 2022, 9855836. [Google Scholar] [CrossRef]
- Helal, M.A.; Al-Gazzar, A.E.; Abas, M.; Akhtar, S.; Gad, M.M.; Al-Thobity, A.M. Comparative Effect of Different Surface Treatments on the Shear Bond Strength of Two Types of Artificial Teeth Bonded to Two Types of Denture Base Resins. J. Prosthodont. 2022, 31, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Schoonover, I.C.; Fischer, T.E.; Serio, A.F.; Sweeney, W.T. Bonding of plastic teeth to heat-cured denture base resins. J. Am. Dent. Assoc. 1952, 44, 285–287. [Google Scholar] [CrossRef] [PubMed]
- Catterlin, R.K.; Plummer, K.D.; Gulley, M.E. Effect of tinfoil substitute contamination on adhesion of resin denture tooth to its denture base. J. Prosthet. Dent. 1993, 69, 57–59. [Google Scholar] [CrossRef]
- Meloto, C.B.; Silva-Concílio, L.R.; Rodrigues-Garciai, R.C.M.; Canales, G.T.; Rizzatti-Barbosa, C.M. Effect of surface treatments on the bond strength of different resin teeth to complete denture base material. Acta Odontol. Latinoam. 2013, 26, 37–42. [Google Scholar]
- Kurt, M.; Saraç, Y.Š.; Ural, Ç.; Saraç, D. Effect of pre-processing methods on bond strength between acrylic resin teeth and acrylic denture base resin. Gerodontology 2012, 29, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Söderholm, K.J.M. Coatings in dentistry—A review of some basic principles. Coatings 2012, 2, 138–159. [Google Scholar] [CrossRef]
- Huggett, R.; John, G.; Jagger, R.G.; Bates, J.F. Strength of the acrylic denture base tooth bond. Br. Dent. J. 1982, 153, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Paravina, R.D.; Pérez, M.M.; Ghinea, R. Acceptability and perceptibility thresholds in dentistry: A comprehensive review of clinical and research applications. J. Esthet. Restor. Dent. 2018, 31, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.N. The strength of the joint between plain and copolymer acrylic teeth and denture base resins. Br. Dent. J. 1958, 104, 317–320. [Google Scholar]
- Rupp, N.W.; Bowen, R.L.; Paffenbarger, G.C. Bonding Cold-Curing Denture Base Acrylic Resin to Acrylic Resin Teeth. J. Am. Dent. Assoc. 1971, 83, 601–606. [Google Scholar] [CrossRef]
- Machado, A.L.; Breeding, L.C.; Vergani, C.E.; da Cruz Perez, L.E. Hardness and surface roughness of reline and denture base acrylic resins after repeated disinfection procedures. J. Prosthet. Dent. 2009, 102, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Goiato, M.C.; Dos Santos, D.M.; Moreno, A.; Iyda, M.G.; Rezende, M.C.R.A.; Haddad, M.F. Effect of disinfection and storage on the flexural strength of ocular prosthetic acrylic resins. Gerodontology 2012, 29, e838–e844. [Google Scholar] [CrossRef] [PubMed]
- Alhallak, K.; Hagi-Pavli, E.; Nankali, A. A review on clinical use of CAD/CAM and 3D printed dentures. Br. Dent. J. 2023, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, A.; Takaichi, A.; Kajima, Y.; Takahashi, H.; Wakabayashi, N. Bond strength of CAD/CAM denture teeth to a denture base resin in a milled monolithic unit. J. Prosthodont. Res. 2023, 67, 610–618. [Google Scholar] [CrossRef]
- Alharbi, N.; Alharbi, A.; Osman, R. Mode of Bond Failure Between 3D-Printed Denture Teeth and Printed Resin Base Material: Effect of Fabrication Technique and Dynamic Loading. An In Vitro Study. Int. J. Prosthodont. 2021, 34, 763–774. [Google Scholar] [CrossRef] [PubMed]
- Kane, B.; Shah, K.C. In Vitro Analysis of Shear Stress: CAD Milled vs Printed Denture Base Resins with Bonded Denture Tooth. J. Prosthodont. 2023, 32, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Ranjith, K.P.; Sivaprasad, K.K.; Karunakaran, D.A. Comparative evaluation of bond strength of denture base resin to acrylic resin teeth following different surface treatments: An In vitro study. Int. J. Appl. Dent. Sci. 2021, 7, 74–78. [Google Scholar]
- Tashiro, S.; Kawaguchi, T.; Hamanaka, I.; Takahashi, Y. Bond strength of artificial teeth to thermoplastic denture base resin for injection molding. Dent. Mater. J. 2021, 40, 657–663. [Google Scholar] [CrossRef]
- Han, S.Y.; Moon, Y.H.; Lee, J. Shear bond strength between CAD/CAM denture base resin and denture artificial teeth when bonded with resin cement. J. Adv. Prosthodont. 2020, 12, 251–258. [Google Scholar] [CrossRef]
- Choi, J.J.E.; Uy, C.E.; Plaksina, P.; Ramani, R.S.; Ganjigatti, R.; Waddell, J.N. Bond Strength of Denture Teeth to Heat-Cured, CAD/CAM and 3D Printed Denture Acrylics. J. Prosthodont. 2020, 29, 415–421. [Google Scholar] [CrossRef] [PubMed]
- ShanmugaSundaram, L.; Jeyaraj, B.J.; Krishnan, M.; Balasubramanian, M. Evaluation of Bond Strength on Surface Treated Denture Teeth to Injection Molded PMMA Denture Base. Ann. Dent. Spec. 2021, 9, 7–12. [Google Scholar] [CrossRef]
- Prpić, V.; Schauperl, Z.; Glavina, D.; Ćatić, A.; Čimić, S. Comparison of shear bond strengths of different types of denture teeth to different denture base resins. J. Adv. Prosthodont. 2020, 12, 376–382. [Google Scholar] [CrossRef]
- Sayed, M.E.; Lunkad, H.; Fageeh, I.; Jaafari, M.; Tawhari, A.; Muaidi, T.; Alshehri, M.I.; Jethlia, A.; Jain, S. Comparative evaluation of compressive bond strength between acrylic denture base and teeth with various combinations of mechanical and chemical treatments. Coatings 2021, 11, 1527. [Google Scholar] [CrossRef]
- Viegas, M.M.; Bhat, V.S.; Shetty, S.K. Effect of mechanical and chemical surface treatment on bond strength of acrylic denture teeth to heat cure acrylic resin—An invitro study. IP Ann. Prosthodont. Restor. Dent. 2021, 7, 161–168. [Google Scholar] [CrossRef]
- Klaiber, D.; Spintzyk, S.; Geis-Gerstorfer, J.; Klink, A.; Unkovskiy, A.; Huettig, F. Bonding behavior of conventional pmma towards industrial cad/cam pmma and artificial resin teeth for complete denture manufacturing in a digital workflow. Materials 2021, 14, 3822. [Google Scholar] [CrossRef] [PubMed]
- Phukela, S.S.; Chintalapudi, S.K.; Sachdeva, H.; Dhall, R.S.; Sharma, N.; Prabhu, A. Comparative evaluation of different mechanical modifications of denture teeth on bond strength between high-impact acrylic resin and denture teeth: An in vitro study. J. Int. Soc. Prev. Community Dent. 2016, 6, 161–166. [Google Scholar] [CrossRef]
- Gharebagh, T.G.; Hamedirad, F.; Miruzadeh, K. Comparison of bond strength of acrylic, composite, and nanocomposite artificial teeth to heat-cure acrylic denture base resin. Front. Dent. 2019, 16, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Sharma, E.; Kumar, M.; Sharma, R.; Bansal, A.; Katoch, S. Comparative Evaluation of Bond Strength between Ridge Lap Surface of Acrylic Teeth and Denture Base Resin: An In Vitro Study. Dent. J. Adv. Stud. 2019, 7, 12–18. [Google Scholar] [CrossRef][Green Version]
- Pathak, R.; Kumar, R.; Mahajan, S.; Singh, P.; Tiwari, D.; Deval, P. Evaluation and comparison of the effect of different chemical surface treatments (monomethyl methacrylate monomer, dichloromethane, and 1:1 v/v 30% trichloromethane and monomethyl methacrylate monomer solvent) on the shear bond strength of acrylic resin t. Int. J. Prev. Clin. Dent. Res. 2019, 6, 1. [Google Scholar] [CrossRef]
- Prasad, A.H.; Roopwani, K.; Mohammed, H.S.; Kundapur, V.; Anand, M.; Dutta, A. To Compare and Evaluate the Bond Strength of Acrylic Denture Teeth with Heat Cure Acrylic Resin and Thermoplastic Denture Base Material after Different Surface Treatments of Acrylic Teeth—An In Vitro Study. Int. J. Biomed. Sci. 2018, 14, 20–25. [Google Scholar] [CrossRef]
- Aguiar, E.F.; Tonani, R.; Paiola, F.d.G.; Chinelatti, M.A.; de Arruda, C.N.F.; da Matta, J.C.S.; Pires-de-Souza, F.d.C.P. Influence of aging on bond strength of artificial teeth to denture base acrylic resins. Braz. J. Oral Sci. 2018, 17, e18373. [Google Scholar] [CrossRef]
- Hatami, M.; Taghavipour, M.; Daneshkazemi, A.; Ahmadi, S.; Hatami, M.; Taghavipour, M.; Daneshkazemi, A.; Ahmadi, S. Effect of surface treatment on the bond strength of Multilithic denture teeth to heat-polymerized denture base resin. Int. J. Adv. Biotechnol. Res. 2017, 8, 1317–1323. [Google Scholar]
- Mohamed, R.; Noufal, P.K.; Shenoy, D.; Reddy, P.S.; Jain, A.R. A comparitive study on the tensile bond strength of conventional denture base resin to cross linked acrylic tooth using two different curing cycles: An invitro study. Biomed. Pharmacol. J. 2017, 10, 447–454. [Google Scholar] [CrossRef]
- Cleto, M.P.; Silva, M.D.D.; Nunes, T.S.B.S.; Viotto, H.E.C.; Coelho, S.R.G.; Pero, A.C. Evaluation of Shear Bond Strength between Denture Teeth and 3D-Printed Denture Base Resin. J. Prosthodont. 2022, 32, 3–10. [Google Scholar] [CrossRef]
- Corsalini, M.; Venere, D.D.; Pettini, F.; Stefanachi, G.; Catapano, S.; Boccaccio, A.; Lamberti, L.; Pappalettere, C.; Carossa, S. A Comparison of Shear Bond Strength of Ceramic and Resin Denture Teeth on Different Acrylic Resin Bases. Open Dent. J. 2015, 8, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Jain, G.; Palekar, U.; Awinashe, V.; Mishra, S.K.; Kawadkar, A.; Rahangdale, T. The effect of different chemical surface treatments of denture teeth on shear bond strength: A comparative study. J. Clin. Diagn. Res. 2014, 8, 15–18. [Google Scholar] [CrossRef] [PubMed]
- Chittaranjan, B.; Taruna, M.; Sudheer, N.; Patil, N.S. Evaluation of shear bond strength of three different types of artificial teeth to heat cure denture base resin: An in vitro study. Indian J. Dent. Res. 2013, 24, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Aljudy, H.J. Effect of Plasma Treatment of Acrylic Denture Teeth and Thermocycling on the Bonding Strength to Heat Cured Acrylic Denture Base Material. J. Baghdad Coll. Dent. 2013, 25, 6–11. [Google Scholar] [CrossRef]
- Krishna, V.P.; Premalatha, A.; Babu, P.J.; Raju, D.S.; Kumar, M.P.; Rao, D.B. Effect of various chemicals on the bond strength of acrylic tooth and denture base—An Invitro comparative study. J. Int. Oral Health JIOH 2014, 6, 100–105. [Google Scholar] [PubMed]
- Barpal, D.; Curtis, D.A.; Finzen, F.; Perry, J.; Gansky, S.A. Failure load of acrylic resin denture teeth bonded to high impact acrylic resins. J. Prosthet. Dent. 1998, 80, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Morrow, R.M.; Matvias, F.M.; Windeler, A.S.; Fuchs, R.J. Bonding of plastic teeth to two heat-curing denture base resins. J. Prosthet. Dent. 1978, 39, 565–568. [Google Scholar] [CrossRef] [PubMed]
- Dimitrova, M.; Vlahova, A.; Kalachev, Y.; Zlatev, S.; Kazakova, R.; Capodiferro, S. Recent Advances in 3D Printing of Polymers for Application in Prosthodontics. Polymers 2023, 15, 4525. [Google Scholar] [CrossRef] [PubMed]
- Palitsch, A.; Hannig, M.; Ferger, P.; Balkenhol, M. Bonding of acrylic denture teeth to MMA/PMMA and light-curing denture base materials: The role of conditioning liquids. J. Dent. 2012, 40, 210–221. [Google Scholar] [CrossRef] [PubMed]
- Saavedra, G.; Valandro, L.F.; Leite, F.P.P.; Amaral, R.; Ozcan, M.; Bottino, M.A.; Kimpara, E.T. Bond strength of acrylic teeth to denture base resin after various surface conditioning methods before and after thermocycling. Int. J. Prosthodont. 2007, 20, 199–201. [Google Scholar]
- Meng, G.K.; Chung, K.H.; Fletcher-Stark, M.L.; Zhang, H. Effect of surface treatments and cyclic loading on the bond strength of acrylic resin denture teeth with autopolymerized repair acrylic resin. J. Prosthet. Dent. 2010, 103, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, S.E.; Fjeldstad, E. Bonding of plastic teeth to acrylic resin denture base material. Odont. Tidskr. 1961, 40, 776. [Google Scholar]
- Takahashi, Y.; Chai, J.; Takahashi, T.; Habu, T. Bond strength of denture teeth to denture base resins. Int. J. Prosthodont. 2000, 13, 59–65. [Google Scholar] [PubMed]
- de Chaves, C.A.L.; Regis, R.R.; Machado, A.L.; de Souza, R.F. Effect of ridge lap surface treatment and thermocycling on microtensile bond strength of acrylic teeth to denture base resins. Braz. Dent. J. 2009, 20, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Bragaglia, L.E.; Prates, L.H.M.; Calvo, M.C.M. The role of surface treatments on the bond between acrylic denture base and teeth. Braz. Dent. J. 2009, 20, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Mosharraf, R.; Abed-Haghighi, M. A comparison of acrylic and multilithic teeth bond strengths to acrylic denture base material. J. Contemp. Dent. Pract. 2009, 10, 17–22. [Google Scholar] [CrossRef]
- Suzuki, S.; Sakoh, M.; Shiba, A. Adhesive bonding of denture base resins to plastic denture teeth. J. Biomed. Mater. Res. 1990, 24, 1091–1103. [Google Scholar] [CrossRef]
- Fletcher-Stark, M.L.; Chung, K.H.; Rubenstein, J.E.; Raigrodski, A.J.; Mancl, L.A. Shear Bond Strength of Denture Teeth to Heatand Light-Polymerized Denture Base Resin. J. Prosthodont. 2011, 20, 52–59. [Google Scholar] [CrossRef]
- Official Webpage. Available online: https://www.dentsplysirona.com/en-us (accessed on 9 October 2023).
- Akin, H.; Kirmali, O.; Tugut, F.; Coskun, M.E. Effects of different surface treatments on the bond strength of acrylic denture teeth to polymethylmethacrylate denture base material. Photomed. Laser Surg. 2014, 32, 512–516. [Google Scholar] [CrossRef]
- Akin, H.; Tugut, F.; Guney, U.; Akar, T. Shear bond strength of denture teeth to two chemically different denture base resins after various surface treatments. J. Prosthodont. 2014, 23, 152–156. [Google Scholar] [CrossRef]
- Marchack, B.W.; Yu, Z.; Zhao, X.Y.; White, S.N. Adhesion of denture tooth porcelain to heat-polymerized denture resin. J. Prosthet. Dent. 1995, 74, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Nishigawa, G.; Maruo, Y.; Okamoto, M.; Oki, K.; Kinuta, Y.; Minagi, S.; Irie, M.; Suzuki, K. Effect of adhesive primer developed exclusively for heat-curing resin on adhesive strength between plastic artificial tooth and acrylic denture base resin. Dent. Mater. J. 2006, 25, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Perea, L.; Matinlinna, J.P.; Tolvanen, M.; Lassila, L.V.; Vallittu, P.K. Monomer priming of denture teeth and its effects on the bond strength of composite resin. J. Prosthet. Dent. 2014, 112, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Kawara, M.; Carter, J.M.; Ogle, R.K.; Johnson, H.H. Bonding of plastic teeth to denture base resins. J. Prosthet. Dent. 1991, 66, 566–571. [Google Scholar] [CrossRef] [PubMed]
- Clancy, J.M.S.; Boyer, D.B. Comparative bond strengths of light-cured, heat-cured, and autopolymerizing denture resins to denture teeth. J. Prosthet. Dent. 1989, 61, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Wayne Caswell, C.; Norling, B.K. Comparative study of the bond strengths of three abrasion-resistant plastic denture teeth bonded to a cross-linked and a grafted, cross-linked denture base material. J. Prosthet. Dent. 1986, 55, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Lagouvardos, P.E.; Polyzois, G.L. Shear bond strength between composite resin and denture teeth: Effect of tooth type and surface treatments. Int. J. Prosthodont. 2003, 16, 499–504. [Google Scholar] [PubMed]
- Vergani, C.E.; Machado, A.L.; Giampaolo, E.T.; Pavarina, A.C. Effect of Surface Treatments on the Bond Strength between Composite Resin and Acrylic Resin Denture Teeth. Int. J. Prosthodont. 2000, 13, 383–386. [Google Scholar] [PubMed]
- Chung, K.H.; Chung, C.Y.; Chung, C.Y.; Chan, D.C.N. Effect of pre-processing surface treatments of acrylic teeth on bonding to the denture base. J. Oral Rehabil. 2008, 35, 268–275. [Google Scholar] [CrossRef]
- Jorge, J.H.; Giampaolo, E.T.; Machado, A.L.; Vergani, C.E. Cytotoxicity of denture base acrylic resins: A literature review. J. Prosthet. Dent. 2003, 90, 190–193. [Google Scholar] [CrossRef]
- Cardash, H.S.; Applebaum, B.; Baharav, H.; Liberman, R. Effect of retention grooves on tooth-denture base bond. J. Prosthet. Dent. 1990, 64, 492–496. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, J.L.; Benington, I.C. An investigation of the variables which may affect the bond between plastic teeth and denture base resin. J. Dent. 1999, 27, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, D.B.; Monteiro, D.R.; Barão, V.A.R.; Pero, A.C.; Compagnoni, M.A. Effect of monomer treatment and polymerisation methods on the bond strength of resin teeth to denture base material. Gerodontology 2009, 26, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Ariff, F.T.M.; Yunus, N.; Baig, M.R. The effect of mechanical roughening and chemical treatment on shear bond strength of urethane dimethacrylate denture base resin. Int. J. Adhes. Adhes. 2011, 31, 112–118. [Google Scholar] [CrossRef]
- Clancy, J.M.S.; Hawkins, L.F.; Keller, J.C.; Boyer, D.B. Bond strength and failure analysis of light-cured denture resins bonded to denture teeth. J. Prosthet. Dent. 1991, 65, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Tzanakakis, E.G.; Dimitriadi, M.; Tzoutzas, I.; Koidis, P.; Zinelis, S.; Eliades, G. Effect of water storage on hardness and interfacial strength of resin composite luting agents bonded to surface-treated monolithic zirconia. Dent. J. 2021, 9, 78. [Google Scholar] [CrossRef] [PubMed]
- Alzaher, Z.A.; Almaskin, D.F.; Qaw, M.S.; Abu Showmi, T.H.; Abualsaud, R.; Akhtar, S.; Gad, M.M. Chemo-Mechanical Approach to Improve Repair Bond Strength of Denture Teeth. Int. J. Dent. 2020, 8870361. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K.; Vojtkova, H.; Lassila, V.P. Impact strength of denture polymethyl methacrylate reinforced with continuous glass fibers or metal wire. Acta Odontol. Scand. 1995, 53, 392–396. [Google Scholar] [CrossRef]
- Cardash, H.S.; Liberman, R.; Helft, M. The effect of retention grooves in acrylic resin teeth on tooth denture-base bond. J. Prosthet. Dent. 1986, 55, 526–528. [Google Scholar] [CrossRef]
- Della Bona, A.; van Noort, R. Shear vs. Tensile Bond Strength of Resin Composite Bonded to Ceramic. J. Dent. Res. 1995, 74, 1591–1596. [Google Scholar] [CrossRef]
- Rasmussen, S.T. Analysis of dental shear bond strength tests, shear or tensile? Int. J. Adhes. Adhes. 1996, 16, 147–154. [Google Scholar] [CrossRef]
- Mahadevan, V.; Krishnan, M.; Krishnan, C.S.; Azhagarasan, N.S.; Sampathathkumar, J.; Ramasubramanian, H. Influence of surface modifications of acrylic resin teeth on shear bond strength with denture base resin—An invitro study. J. Clin. Diagn. Res. 2015, 9, ZC16–ZC21. [Google Scholar] [CrossRef]
- Saponaro, P.C.; Yilmaz, B.; Johnston, W.; Heshmati, R.H.; McGlumphy, E.A. Evaluation of patient experience and satisfaction with CAD-CAM-fabricated complete dentures: A retrospective survey study. J. Prosthet. Dent. 2016, 116, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Inokoshi, M.; Kanazawa, M.; Minakuchi, S. Evaluation of a complete denture trial method applying rapid prototyping. Dent. Mater. J. 2012, 31, 40–46. [Google Scholar] [CrossRef]
- Zuckerman, G.R. A reliable method for securing anterior denture teeth in denture bases. J. Prosthet. Dent. 2003, 89, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Nejatian, T.; Pezeshki, S.; Syed, A.U.Y. Acrylic Denture Base Materials; Elsevier Ltd.: Amsterdam, The Netherlands, 2019; ISBN 9780081024768. [Google Scholar]
- Gad, M.M.; Fouda, S.M.; Al-Harbi, F.A.; Näpänkangas, R.; Raustia, A. PMMA denture base material enhancement: A review of fiber, filler, and nanofiller addition. Int. J. Nanomed. 2017, 12, 3801–3812. [Google Scholar] [CrossRef]
- Chai, J.; Takahashi, Y.; Takahashi, T.; Habu, T. Bonding durability of conventional resinous denture teeth and highly crosslinked denture teeth to a pour-type denture base resin. Int. J. Prosthodont. 2000, 13, 112–116. [Google Scholar]
- Tanoue, N.; Nagano, K.; Matsumura, H. Use of a light-polymerized composite removable partial denture base for a patient hypersensitive to poly(methyl methacrylate), polysulfone, and polycarbonate: A clinical report. J. Prosthet. Dent. 2005, 93, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, J.L. Shear bond strength of resin teeth to heat-cured and light-cured denture base resin. J. Oral Rehabil. 2000, 27, 312–316. [Google Scholar] [CrossRef]
- Meng, T.R.; Latta, M.A. Physical properties of four acrylic denture base resisns. J. Contemp. Dent. Pract. 2005, 6, 93–100. [Google Scholar] [CrossRef]
- Robison, N.E.; Tantbirojn, D.; Versluis, A.; Cagna, D.R. Failure strengths of denture teeth fabricated on injection molded or compression molded denture base resins. J. Prosthet. Dent. 2016, 116, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Patil, R.; Juszczyk, A.S.; Radford, D.R.; Clark, R.K.F. Is the bond between acrylic resin denture teeth and denture base resin stronger if they are both made by the same manufacturer? Eur. J. Prosthodont. Restor. Dent. 2010, 18, 39–41. [Google Scholar]
- Colebeck, A.C.; Monaco, E.A.; Pusateri, C.R.; Davis, E.L. Microtensile bond strength of different acrylic teeth to high-impact denture base resins. J. Prosthodont. 2015, 24, 43–51. [Google Scholar] [CrossRef]
- Reis, K.R.; Bonfante, G.; Pegoraro, L.F.; Conti, P.C.R.; De Oliveira, P.C.G.; Kaizer, O.B. In vitro wear resistance of three types of polymethyl methacrylate denture teeth. J. Appl. Oral Sci. 2008, 16, 176–180. [Google Scholar] [CrossRef] [PubMed]
- Farbkommunikation, V. VITA-Perfect Match. VITA Denture Teeth Technical and Scientific Documentation. 2023. Available online: https://mam.vita-zahnfabrik.com/portal/ecms_mdb_download.php?id=78332&sprache=en&fallback=de&cls_session_id=&neuste_version=1 (accessed on 20 March 2023).
- Vallittu, P.K. Interpenetrating polymer networks (IPNs) in dental polymers and composites. J. Adhes. Sci. Technol. 2009, 23, 961–972. [Google Scholar] [CrossRef]
- Clements, J.L.; Tantbirojn, D.; Versluis, A.; Cagna, D.R. Do denture processing techniques affect the mechanical properties of denture teeth? J. Prosthet. Dent. 2018, 120, 246–251. [Google Scholar] [CrossRef]
- Munshi, N.; Rosenblum, M.; Jiang, S.; Flinton, R. In Vitro Wear Resistance of Nano-Hybrid Composite Denture Teeth. J. Prosthodont. 2017, 26, 224–229. [Google Scholar] [CrossRef]
- Ivoclar SR Phonares II. 2022. Available online: https://downloadcenter.ivoclar.com/#dc=global&search-text=20305&details=20305 (accessed on 26 July 2023).
- Saeed, F.; Muhammad, N.; Khan, A.S.; Sharif, F.; Rahim, A.; Ahmad, P.; Irfan, M. Prosthodontics dental materials: From conventional to unconventional. Mater. Sci. Eng. C 2020, 106, 110167. [Google Scholar] [CrossRef] [PubMed]
- Damade, S.; Parlani, S.; Beohar, G.; Agrawal, B.; Dwivedi, P.; Shrivastava, K. Comparative evaluation of shear and tensile bond strength of cross linked acrylic denture teeth to denture base resins cured by heat and microwave polymerisation techniques—An in vitro study. Univ. J. Dent. Sci. 2019, 5, 17–22. [Google Scholar]
- Dalal, A.; Juszczyk, A.S.; Radford, D.R.; Clark, R.K.F. Effect of curing cycle on the tensile strength of the bond between heat cured denture base acrylic resin and acrylic resin denture teeth. Eur. J. Prosthodont. Restor. Dent. 2009, 17, 146–149. [Google Scholar]
- Takaichi, A.; Fueki, K.; Murakami, N.; Ueno, T.; Inamochi, Y.; Wada, J.; Arai, Y.; Wakabayashi, N. A systematic review of digital removable partial dentures. Part II: CAD/CAM framework, artificial teeth, and denture base. J. Prosthodont. Res. 2022, 66, 53–67. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, N.; Sarfraz, Z.; Zafar, M.S.; Liaqat, S.; Rahim, A.; Ahmad, P.; Alsubaie, A.; Almalki, A.S.A.; Khandaker, M.U. Characterization of various acrylate based artificial teeth for denture fabrication. J. Mater. Sci. Mater. Med. 2022, 33, 17. [Google Scholar] [CrossRef] [PubMed]
- Ghahramani, L.; Shahabi, S.; Amirjan, A.; Fazel, A. Comparison of bond strength of composite and acrylic teeth to heat-cured andauto-polymerized acrylic denture base. J. Dent. Med. 2011, 23, 215–226. [Google Scholar]
- Papazoglou, E.; Vasilas, A.I. Shear bond strengths for composite and autopolymerized acrylic resins bonded to acrylic resin denture teeth. J. Prosthet. Dent. 1999, 82, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Infante, L.; Yilmaz, B.; McGlumphy, E.; Finger, I. Fabricating complete dentures with CAD/CAM technology. J. Prosthet. Dent. 2014, 111, 351–355. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, B.J.; Goodacre, C.J. Additive Manufacturing for Complete Denture Fabrication: A Narrative Review. J. Prosthodont. 2022, 31, 47–51. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Alshahrani, F.A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Ateeq, I.S.; Helal, M.A.; Al-Harbi, F.A. Strength and Surface Properties of a 3D-Printed Denture Base Polymer. J. Prosthodont. 2022, 31, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Andreescu, C.F.; Ghergic, D.L.; Botoaca, O.; Hancu, V.; Banateanu, A.M.; Patroi, D.N. Evaluation of different materials used for fabrication of complete digital denture. Mater. Plast. 2018, 55, 124–128. [Google Scholar] [CrossRef]
- Yau, H.T.; Yang, T.J.; Lin, Y.K. Comparison of 3-D Printing and 5-axis Milling for the Production of Dental e-models from Intra-oral Scanning. Comput.-Aided Des. Appl. 2016, 13, 32–38. [Google Scholar] [CrossRef]
- Han, W.; Li, Y.; Zhang, Y.; Lv, Y.; Zhang, Y.; Hu, P.; Liu, H.; Ma, Z.; Shen, Y. Design and fabrication of complete dentures using CAD/CAM technology. Medicine 2017, 96, e5435. [Google Scholar] [CrossRef]
- Madhav, G.V.; Raj, S.; Yadav, N.; Mudgal, I.; Mehta, N.; Tatwadiya, R. Shear bond strength of acrylic teeth to acrylic denture base after different surface conditioning methods. J. Contemp. Dent. Pract. 2013, 14, 892–897. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).