Comparative Assessment of the Adhesion Forces of Soft Silicone Materials to the Denture Base Material (PMMA) Conditioned with Sandblasting
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials Subjected to the Tests
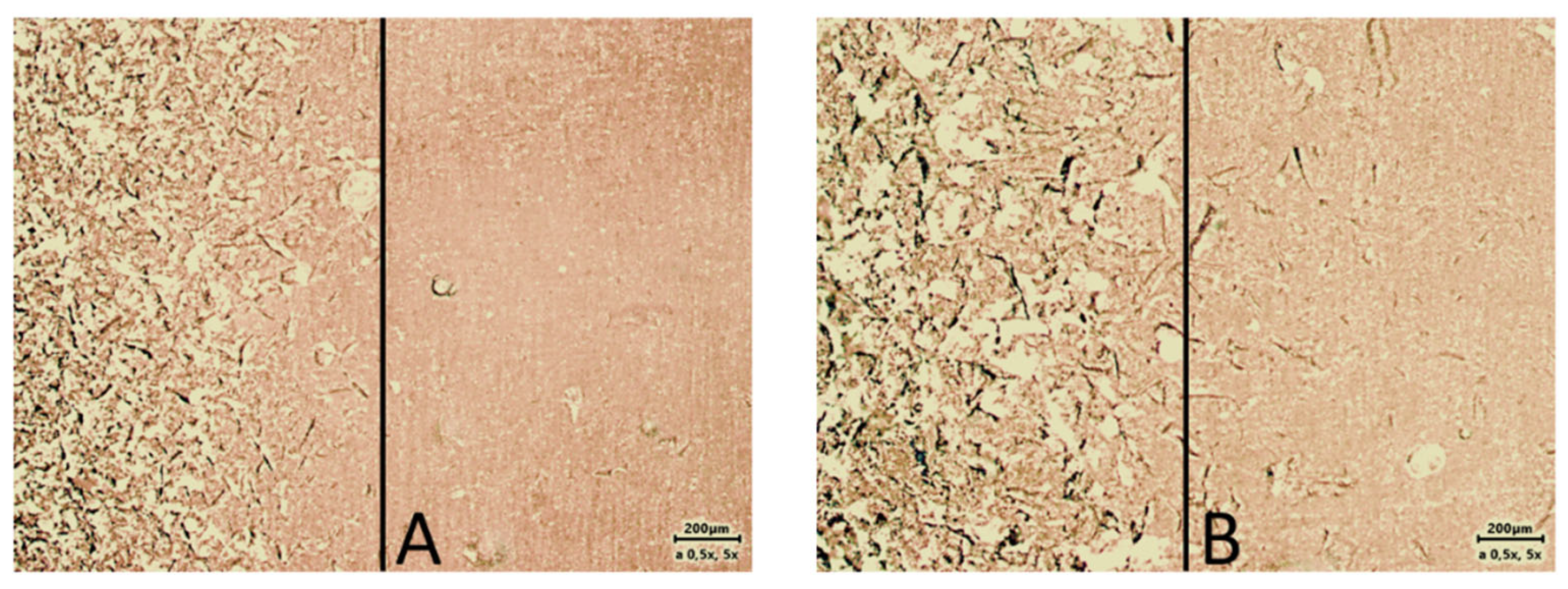
2.2. Preparation of Samples for Testing
2.3. Create Groups of Test Materials
2.4. Strength Tests of Lining Materials
2.5. Statistic Tools
2.5.1. The Kruskal–Wallis Test
2.5.2. The One-Way ANOVA Test
- μ1—mean durability of glue joint for a sample no 1;
- μ2—mean durability of glue joint for a sample no 2;
- μk—mean durability of glue joint for a sample no k;
- K—any number of studied samples.
- -
- Samples are independent.
- -
- Homogeneity of variance in all populations from which the samples are derived—the Brown-Forsythe test is used to verify this assumption.
- -
- Normality of residuals (deviations from the mean)—for this purpose, the Jarque–Bera test is most often used.
2.5.3. The One-Tailed t-Test
2.5.4. Determination of the Size of Differences between Samples (Effect Size)
- n1, n2, …, nk—size of all tested samples.
- —variances of all tested samples.
3. Obtained Results and Analysis
3.1. Results
- Does the strength of the bonded connection depend on the seasoning time of the specimen? In this experiment, specimens were seasoned for either 24 h or six weeks.
- Does the strength of the bonded joint depend on the acrylic surface finish?
3.2. Thesis I. The Seasoning Time of the Glueing Joint Causes a Change in the Adhesive Strength
3.3. Thesis II. The Surface Finish Increases the Glued Joint Durability
4. Discussion
5. Limitations of the Study
6. Conclusions
- Sandblasting of acrylic plastic improves adhesion to selected relining silicones.
- The size of the abrasive used affects the adhesion of acrylic and silicone. The use of too large an abrasive can weaken the strength of adhesion.
- For some relining systems (Mucopren), sandblasting reduces the bond strength of the silicone to PMMA.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Warnakulasuriya, S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009, 45, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Kwaśniewska, A.; Wawrzeńczyk, A.; Brus-Sawczuk, K.; Ganowicz, E.; Strużycka, I. Preliminary results of screening for pathological lesions in oral mucosa and incidence of oral cancer risk factors in adult population. Epidemiol. Rev. 2019, 73, 81–92. [Google Scholar] [CrossRef]
- Didkowska, J.; Wojciechowska, U.; Czaderny, K.; Olasek, P.; Ciuba, A. Cancer in Poland 2017. Natl. Cancer Regist. 2019. ISSN 0867-8251. [Google Scholar]
- Chaturvedi, A.K.; Graubard, B.I.; Broutian, T.; Pickard, R.K.; Tong, Z.Y.; Xiao, W.; Kahle, L.; Gillison, M.L. Effect of Prophylactic Human Papillomavirus (HPV) Vaccination on Oral HPV Infections Among Young Adults in the United States. Am. J. Clin. Oncol. 2018, 36, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Forgie, A.H.; Scott, B.J.; Davis, D.M. A study to compare the oral health impact profile and satisfaction before and after having replacement complete dentures in England and Scotland. Gerodontology 2005, 22, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Palla, E.S.; Karaoglani, E.; Naka, O.; Anastassiadou, V. Soft denture liners’ effect on the masticatory function in patients wearing complete dentures: A systematic review. J. Dent. 2015, 43, 1403–1410. [Google Scholar] [CrossRef]
- Marzola, R.; Scotti, R.; Fazi, G.; Schincaglia, G. Immediate loading of two implants supporting a ball attachment-retained mandibular overdenture: A prospective clinical study. Clin. Implant Dent. Relat. Res. 2007, 9, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Kimoto, S.; So, K.; Yamamoto, S.; Ohno, Y.; Shinomiya, M.; Ogura, K.; Kobayashi, K. Randomized controlled clinical trial for verifying the effect of silicone-based resilient denture liner on the masticatory function of complete denture wearers. Int. J. Prosthodont. 2006, 19, 593–600. [Google Scholar] [PubMed]
- MacEntee, M.I.; Nolan, A.; Thomason, J.M. Oral mucosal and osseous disorders in frail elders. Gerodontology 2004, 21, 78–84. [Google Scholar] [CrossRef]
- Craig, R.G.; Gibbons, P. Properties of resilient denture liners. J. Am. Dent. Assoc. 1961, 63, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Pisani, M.X.; Malheiros-Segundo, A.D.; Balbino, K.L.; Souza, R.D.F.; Paranhos, H.D.F.O.; Lovato da Silva, C.H. Oral health related quality of life of edentulous patients after denture relining with a siliconebased soft liner. Gerodontology 2012, 29, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Jankowa, M.; Yordanow, B.; Dimova-Gabrovska, M.; Apostolov, N. Resilient lining materials for removable dentures: Types, composition and technology. J. IMAB 2019, 25, 2632–2639. [Google Scholar] [CrossRef]
- Kim, B.J.; Yang, H.S.; Chun, M.G.; Park, Y.J. Shore hardness and tensile bond strength of long-term soft denture lining materials. J. Prosthet. Dent. 2014, 112, 1289–1297. [Google Scholar] [CrossRef] [PubMed]
- Iwaki, M.; Akiba, N.; Minakuchi, S.; Takahashi, H. Influence of methyl mercaptan at early setting stages on the properties of self curing addition silicone resilient denture lining materials. J. Prosthodont. Res. 2009, 53, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, D.N.; Goiato, M.C.; Zuccolotti, B.C.; Moreno, A.; dos Santos, D.M.; Pesqueira, A.A. Effect of thermocycling on hardness, absorption, solubility and colour change of soft lines. Gerodontology 2012, 29, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Niarchou, A.; Ntala, P.; Pantopoulos, A.; Polyzois, G.; Frangou, M. Effect of immersion cleansing in color stability and hardness of soft denture reliners. J. Craniofac. Surg. 2012, 23, 426–429. [Google Scholar] [CrossRef]
- Brożek, R.; Koczorowski, R.; Rogalewicz, R.; Voelkel, A.; Czarnecka, B.; Nicholson, J.W. Effect of denture cleansers on chemical and mechanical behavior of selected soft lining materials. Dent. Mater. 2011, 27, 281–290. [Google Scholar] [CrossRef]
- Rodrigues, S.; Shenoy, V.; Shetty, T. Resilient liners: A review. J. Indian Prosthodont. Soc. 2013, 13, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Hristov, I.; Slavchev, D.; Zlatev, S.; Alexandrov, S. Visco-elastic properties of soft relining materials—Review. J. IMAB 2017, 23, 1571–1574. [Google Scholar] [CrossRef]
- Chladek, G.; Mertas, A.; Barszczewska-Rybarek, I.; Nalewajek, T.; Żmudzki, J.; Król, W.; Łukaszczyk, J. Antifungal Activity of Denture Soft Lining Material Modified by Silver Nanoparticles—A Pilot Study. Int. J. Mol. Sci. 2011, 12, 4735–4744. [Google Scholar] [CrossRef]
- ISO 10139-2:2009; Dentistry—Soft Lining Materials for Removable Dentures—Part 2: Materials for Long-Term Use. International Organization for Standardization ISO: Geneva, Switzerland, 2009.
- Cohen, J. Routledge Statistical Power Analysis for the Behavioral Sciences; T&F eBooks: New York, NY, USA, 1988. [Google Scholar] [CrossRef]
- Sawilowsky, S. New effect size rules of thumb. J. Mod. Appl. Stat. Methods 2009, 8, 2. [Google Scholar] [CrossRef]
- Krishnamurthy, S.; Hallikerimath, R.B. An In-vitro Evaluation of Retention, Colonization and Penetration of Commonly Used Denture Lining Materials By Candida albicans. J. Clin. Diagn. Res. 2016, 10, 84–88. [Google Scholar] [CrossRef]
- Gedik, H.; Ozkan, Y.K. The effect of Surface roughness of silicone-based resilient liner materials on the adherence of Candida albicans and inhibition of Candida albicans with different disinfectans. Oral Health Prev. Dent. 2009, 7, 347–353. [Google Scholar] [PubMed]
- Saracx, Y.S.; Başoğlu, T.; Ceylan, G.K.; Saracx, D.; Yapici, O. Effect of denture base surface pretreatment on microleakage of a silicone-based resilient liner. J. Prosthet. Dent. 2004, 92, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Sarac, D.; Sarac, Y.S.; Basoglu, T.; Yapici, O.; Yuzbasioglu, E. The Evaluation of Microleakage and Bond Strength of a Silicone-Based Resilient Liner Following Denture Base Surface Pretreatment. J. Prosthet. Dent. 2006, 95, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Mese, A.; Guzel, K.G. Effect of Storage Duration on the Hardness and Tensile Bond Strength of Silico-ne- and Acrylic Resin-Based Resilient Denture Liners to a Processed Denture Base Acrylic Resin. J. Prosthet. Dent. 2008, 99, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Bayati, O.H.; Yunus, N.; Ahmad, S.F. Tensile Bond Strengths of Silicone Soft Liners to Two Chemically Different Denture Base Resins. Int. J. Adhes. Adhes. 2012, 34, 32–37. [Google Scholar] [CrossRef]
- Wyszyńska, M.; Białozyt-Bujak, E.; Chladek, G.; Czelakowska, A.; Rój, R.; Białozyt, A.; Gruca, O.; Nitsze-Wierzba, M.; Kasperski, J.; Skucha-Nowak, M. Analysis of Changes in the Tensile Bond Strenght of Soft Relining Material with Acrylic Denture Material. Materials 2021, 14, 6868. [Google Scholar] [CrossRef] [PubMed]
- Saadet, A.; Yasemin, K. Effect of silica coating and silane surface treatment on the bond strength of soft denture liner to denture base material. J. Appl. Oral Sci. 2013, 21, 300–306. [Google Scholar] [CrossRef]
- Surapaneni, H.; Ariga, P.; Haribabu, R.; Ravi Shankar, Y.; Kumar, V.H.C.; Attil, S. Comparative Evaluation of Tensile Bond Strength between Silicon Soft Liners and Processed Denture Base Resin Conditioned by Three Modes of Surface Treatment: An Invitro Study. J. Indian Prosthodont. Soc. 2013, 13, 274–280. [Google Scholar] [CrossRef]
- Cavalcanti, Y.W.; Bertolini, M.M.; Cury, A.A.; da Silva, W.J. The effect of poly(methyl methacrylate) surface treatments on the adhesion of silicone-based resilient denture liners. J. Prosthet. Dent. 2014, 112, 1539–1544. [Google Scholar] [CrossRef] [PubMed]
- Wemken, G.; Burkhardt, F.; Spies, B.C.; Kleinvogel, L.; Adali, U.; Sterzenbach, G.; Beuer, F.; Wesemann, C. Bond Strength of Conventional, Subtractive, and Additive Manufactured Denture Bases to Soft and Hard Relining Materials. Dent. Mater. 2021, 37, 928–938. [Google Scholar] [CrossRef] [PubMed]
- Więckiewicz, W.; Kasperski, J.; Więckiewicz, M.; Miernik, M.; Król, W. The Adhesion of Modern Soft Relining Materials to Acrylic Dentures. Adv. Clin. Exp. Med. 2014, 23, 621–625. [Google Scholar] [CrossRef] [PubMed]



| Brand Names (Code) | Manufacturer | Components | Primer/Adhesive | Processing Method |
|---|---|---|---|---|
| Silagum Comfort (SLC) | DMG, Hamburg, Germany | Vinyl polysiloxane, Hydrogen polysiloxane, aerosil, additives | Ethyl acetate, modified polyacrylate, additives Recommended for Silagum AM Comfort. Apply and let solvent dry for 1 min. | Autopolymerizing |
| Elite Soft Relining (ESR) | Zhermack Rovigo Italy | Vinyl polysiloxane (addition silicone) and platinum catalysts | Solution of polyacrylate in dichloromethane (Apply and let solvent dry for 1 min) | Autopolymerizing |
| Ufi Gel SC | VOCO GmbH Cuxhafen Germany | Modified polydimethylsiloxanes + platinum catalyst (addition silicone) | Butanone and methacrylates (Apply and let solvent dry for 60”) | Autopolymerizing |
| Mucopren Soft | Kettenbach GmbH Eschenburg Germany | Silicone polymers (Vinyl polysiloxane, Hydrogenpolysiloxanes) and fillers with platinum-catalyst (addition silicone) | Polymethyl methacrylate Copolymer in ethyl acetate Apply and let solvent dry for 90”. | Autopolymerizing |
| Cohen’s d | Interpretation |
|---|---|
| 0.1 | very small |
| 0.2 | small |
| 0.5 | medium |
| 0.8 | large |
| 1.2 | very large |
| 2.0 | huge |
| System | Surface Finish | Seasoning Time | Sample Size [pcs] | Mean Value [N] | Variance [N] |
|---|---|---|---|---|---|
| Elite Soft | raw | 24 h | 15 | 172.6 | 49.32 |
| raw | 6 weeks | 13 | 145.9 | 73.50 | |
| 100 μm | 24 h | 11 | 125.0 | 60.38 | |
| 100 μm | 6 weeks | 8 | 168.2 | 28.20 | |
| 350 μm | 24 h | 7 | 162.6 | 29.08 | |
| 350 μm | 6 weeks | 7 | 140.0 | 34.34 | |
| Mucopren Soft | raw | 24 h | 14 | 63.2 | 14.45 |
| raw | 6 weeks | 11 | 56.3 | 8.046 | |
| 100 μm | 24 h | 8 | 47.1 | 9.69 | |
| 100 μm | 6 weeks | 15 | 54.1 | 12.43 | |
| 350 μm | 24 h | 8 | 56.8 | 8.8 | |
| 350 μm | 6 weeks | 13 | 45.9 | 8.09 | |
| Silagum Comfort | raw | 24 h | 10 | 153.5 | 38.62 |
| raw | 6 weeks | 9 | 163.6 | 54.23 | |
| 100 μm | 24 h | 7 | 159.9 | 74.57 | |
| 100 μm | 6 weeks | 8 | 220.6 | 45.77 | |
| 350 μm | 24 h | 11 | 204.7 | 32.35 | |
| 350 μm | 6 weeks | 10 | 141.4 | 59.81 | |
| Ufi Gel SC | raw | 24 h | 11 | 126.7 | 12.47 |
| raw | 6 weeks | 10 | 143.7 | 38.2 | |
| 100 μm | 24 h | 11 | 134.6 | 17.01 | |
| 100 μm | 6 weeks | 11 | 107.7 | 30.87 | |
| 350 μm | 24 h | 9 | 120.7 | 45.34 | |
| 350 μm | 6 weeks | 9 | 157.7 | 27.13 |
| Lining System | p-Value |
|---|---|
| Elite Soft | 0.013 |
| Mucopren Soft | 0.0002 |
| Silagum Comfort | 0.0002 |
| Ufi Gel SC | 0.0005 |
| Right-Tailed | Left-Tailed | ||
|---|---|---|---|
| Surface Finish | p-Value | p-Value | |
| Elite Soft | raw | 0.127 | 0.873 |
| 100 μm | 0.961 | 0.039 * | |
| 350 μm | 0.105 | 0.895 | |
| Mucopren Soft | raw | 1 | 0 * |
| 100 μm | 1 | 0 * | |
| 350 μm | 1 | 0 * | |
| Silagum Comfort | 100 μm | 0.334 | 0.666 |
| 350 μm | 0 * | 1 | |
| Ufi Gel SC | 100 μm | 0.194 | 0.807 |
| 350 μm | 0.998 | 0.002 * |
| Surface Finish | Cohen’s d | Interpretation | |
|---|---|---|---|
| Mucopren | raw | 0.6 | medium |
| 100 μm | −0.7 | medium | |
| 350 μm | 1.4 | very large | |
| Silagum | 350 μm | 1.5 | very large |
| Ufigel | 350 μm | −1.1 | large |
| Seasoning Time | p-Value | test | |
|---|---|---|---|
| Elite Soft | 24 h | 0.067 | ANOVA |
| 6 weeks | 0.572 | ANOVA | |
| Mucopren Soft | 24 h | 0.019 * | ANOVA |
| 6 weeks | 0.031 * | ANOVA | |
| Silagum | 24 h | 0.047 * | ANOVA |
| 6 weeks | 0.007 * | Student’s t-test | |
| Ufi gel | 24 h | 0.526 | ANOVA |
| 6 weeks | 0.001 * | Student’s t-test |
| Right-Tailed | Left-Tailed | ||
|---|---|---|---|
| (1)–(2) | p-Value | p-Value | |
| Mucopren | |||
| 24 h | raw–100 μm | 0.006 * | 0.994 |
| raw–μm | 0.133 | 0.867 | |
| 100 μm–350 μm | 0.972 | 0.028 | |
| 6 weeks | raw–100 μm | 0.304 | 0.696 |
| raw–350 μm | 0.002 * | 0.998 | |
| 100 μm–350 μm | 0.026 * | 0.974 | |
| Silagum | |||
| 24 h | raw–100 μm | 0.591 | 0.409 |
| raw–350 μm | 0.998 | 0.002 * | |
| 100 μm–350 μm | 0.952 | 0.048 * | |
| 6 weeks | 100 μm–350 μm | 0.004 * | 0.996 |
| Ufi Gel | |||
| 6 weeks | 100 μm–350 μm | 0.999 | 0.001 * |
| (1)–(2) | Cohen’s d | Interpretation | |
|---|---|---|---|
| Mucopren | |||
| 24 h | raw–100 μm | 1.2 | very large |
| 100 μm–350 μm | −1.1 | large | |
| 6 weeks | raw–350 μm | 1.3 | very large |
| 100 μm–350 μm | 0.8 | large | |
| Silagum | |||
| 24 h | raw–350 μm | −1.4 | very large |
| 100 μm–350 μm | −0.9 | large | |
| 6 weeks | raw–100 μm | 1.5 | very large |
| Ufi Gel | |||
| 6 weeks | 100 μm–350 μm | −1.7 | very large |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuźniarski, A.; Huss, W.; Dąbrowa, T.; Kijak, E. Comparative Assessment of the Adhesion Forces of Soft Silicone Materials to the Denture Base Material (PMMA) Conditioned with Sandblasting. Materials 2024, 17, 3439. https://doi.org/10.3390/ma17143439
Kuźniarski A, Huss W, Dąbrowa T, Kijak E. Comparative Assessment of the Adhesion Forces of Soft Silicone Materials to the Denture Base Material (PMMA) Conditioned with Sandblasting. Materials. 2024; 17(14):3439. https://doi.org/10.3390/ma17143439
Chicago/Turabian StyleKuźniarski, Amadeusz, Weronika Huss, Tomasz Dąbrowa, and Edward Kijak. 2024. "Comparative Assessment of the Adhesion Forces of Soft Silicone Materials to the Denture Base Material (PMMA) Conditioned with Sandblasting" Materials 17, no. 14: 3439. https://doi.org/10.3390/ma17143439
APA StyleKuźniarski, A., Huss, W., Dąbrowa, T., & Kijak, E. (2024). Comparative Assessment of the Adhesion Forces of Soft Silicone Materials to the Denture Base Material (PMMA) Conditioned with Sandblasting. Materials, 17(14), 3439. https://doi.org/10.3390/ma17143439







