Outcomes of Birmingham Hip Resurfacing Based on Clinical Aspects and Retrieval Analysis of Failed Prosthesis
Abstract
:1. Introduction
- To identify the prevalence of failure for Birmingham Hip Prosthesis (BHR) in total hip arthroplasty;
- To analyze the reasons for BHR failure from biomaterials and biofunctional perspectives;
- To conduct a detailed analysis and tests on a series of different BHR-retrieved prostheses after premature failure;
- To analyze relevant clinical data like X-ray investigations and intraoperative images for clinical case studies to better understand all factors involved in BHR prosthesis failure;
- To investigate the importance of surgical technique planning and the cementation procedure in the success rate of BHR prostheses;
- To evaluate patient characteristics and bone quality to minimize the risk of BHR prosthesis failure.
2. Materials and Methods
2.1. The Study Group
2.2. Investigation Methods
3. Results and Discussion
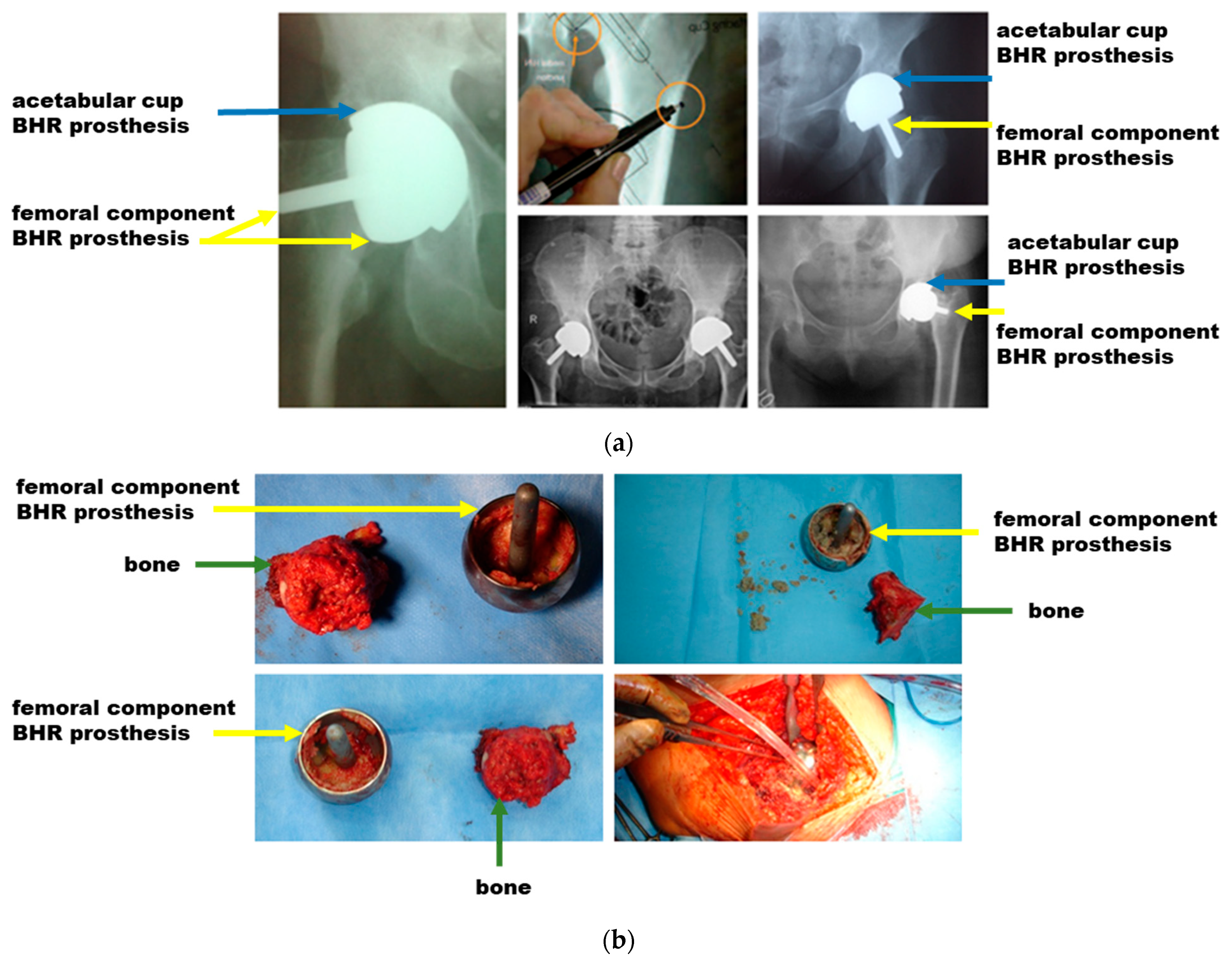
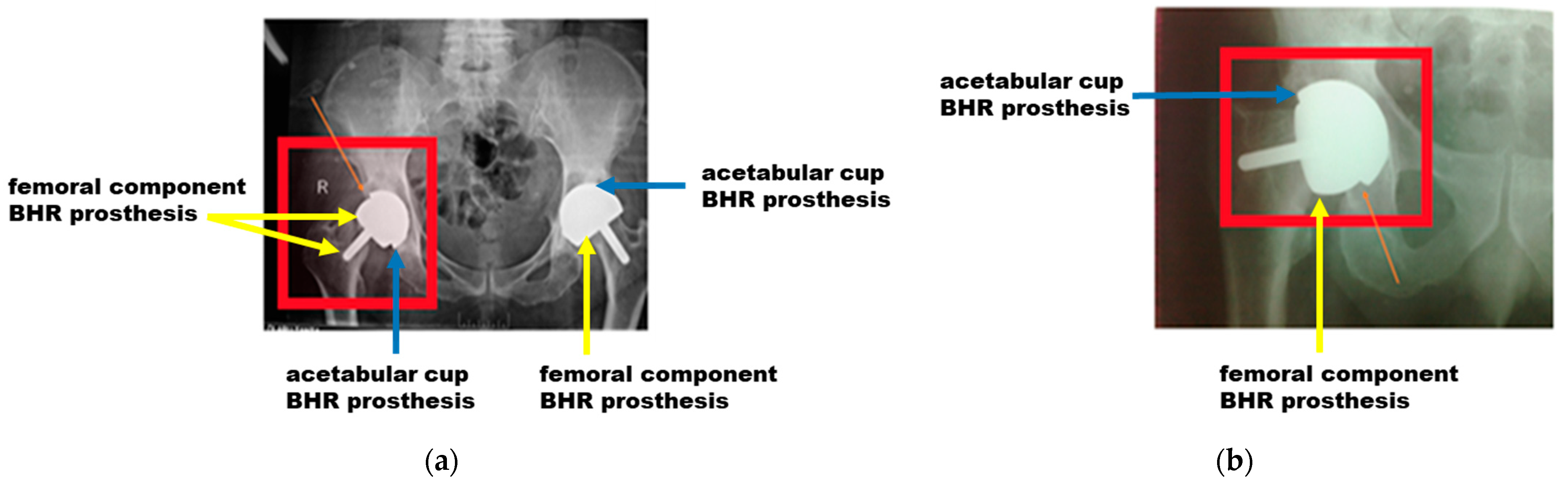
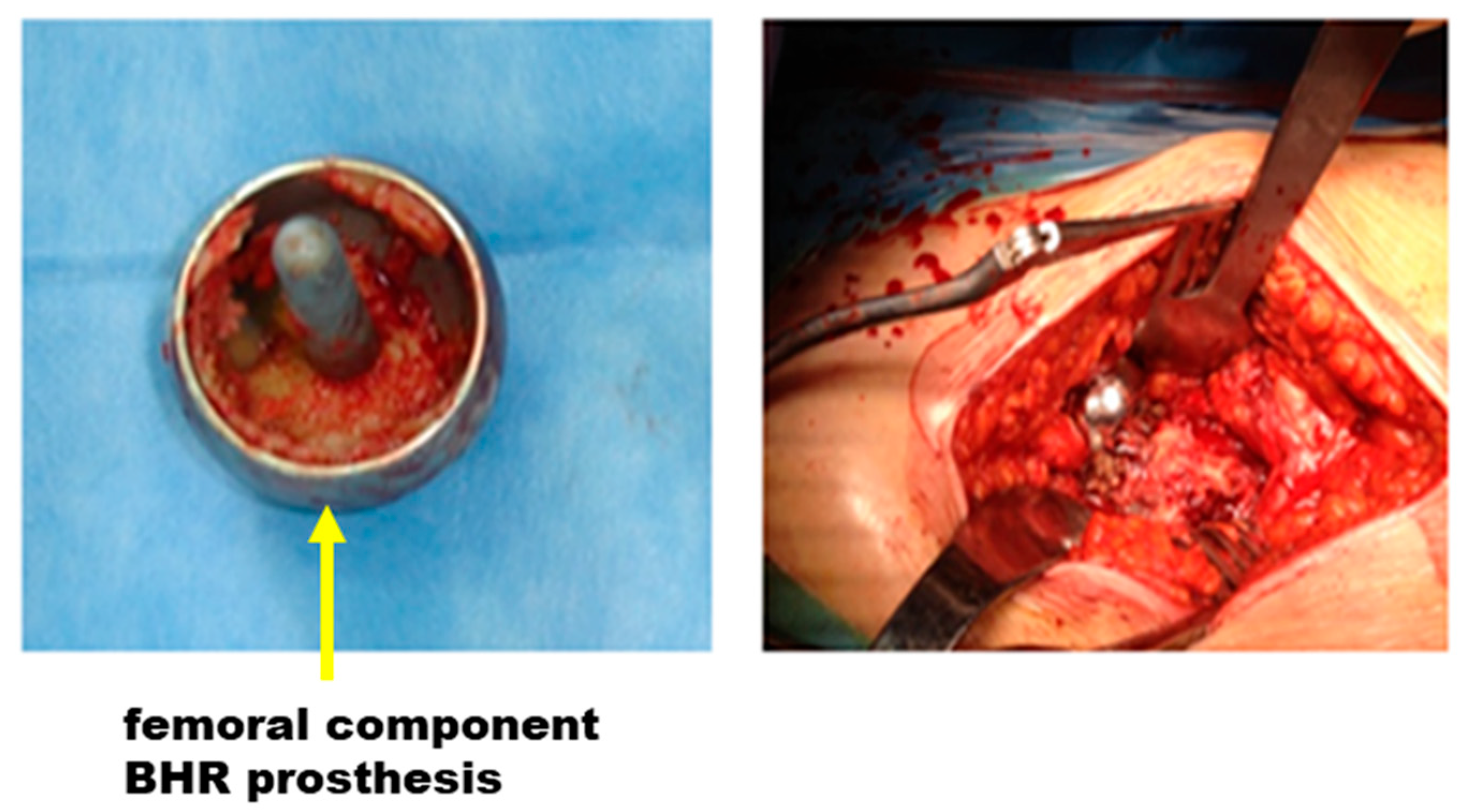
3.1. Clinical Aspects Based on X-rays and Intraoperative Images
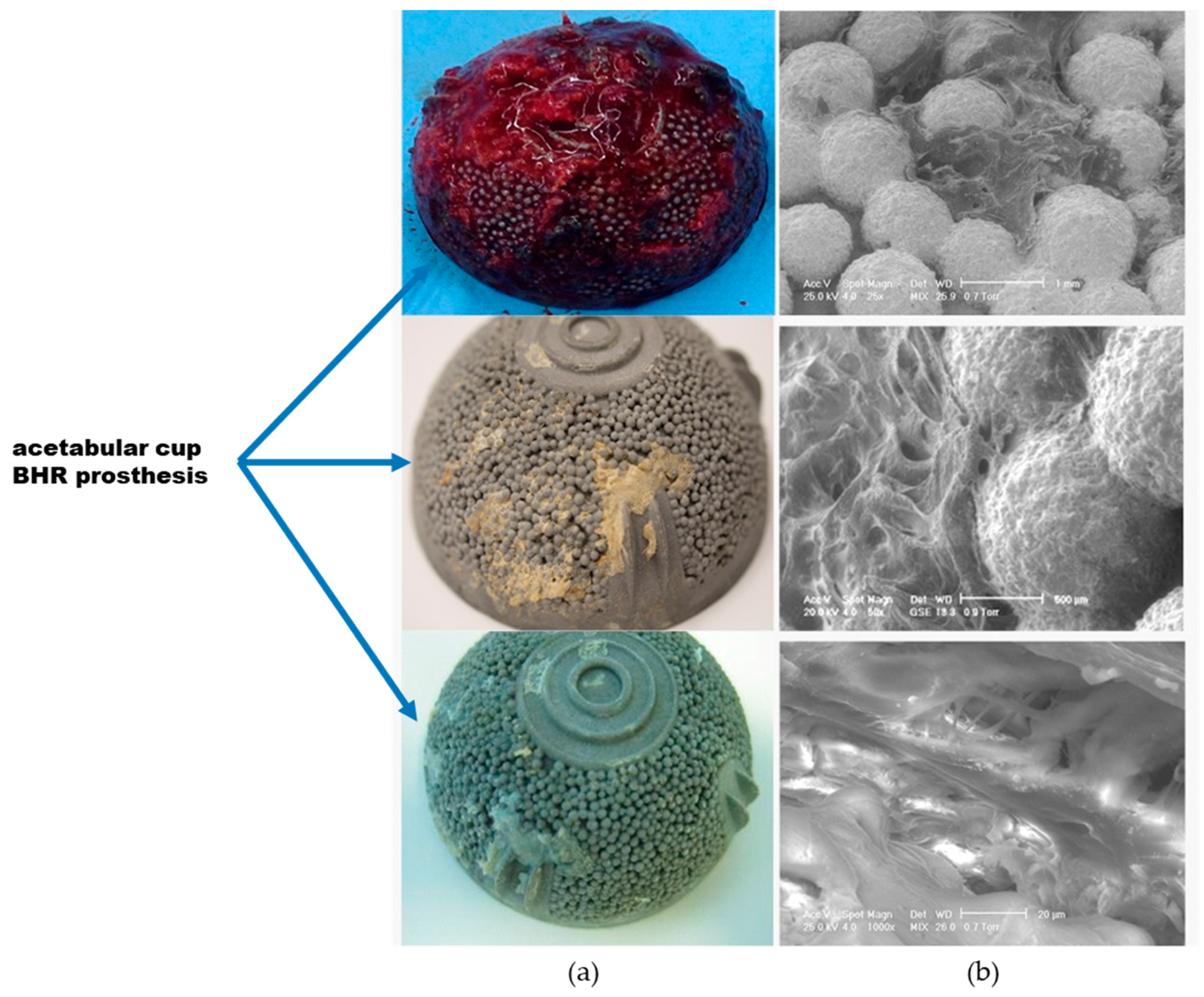
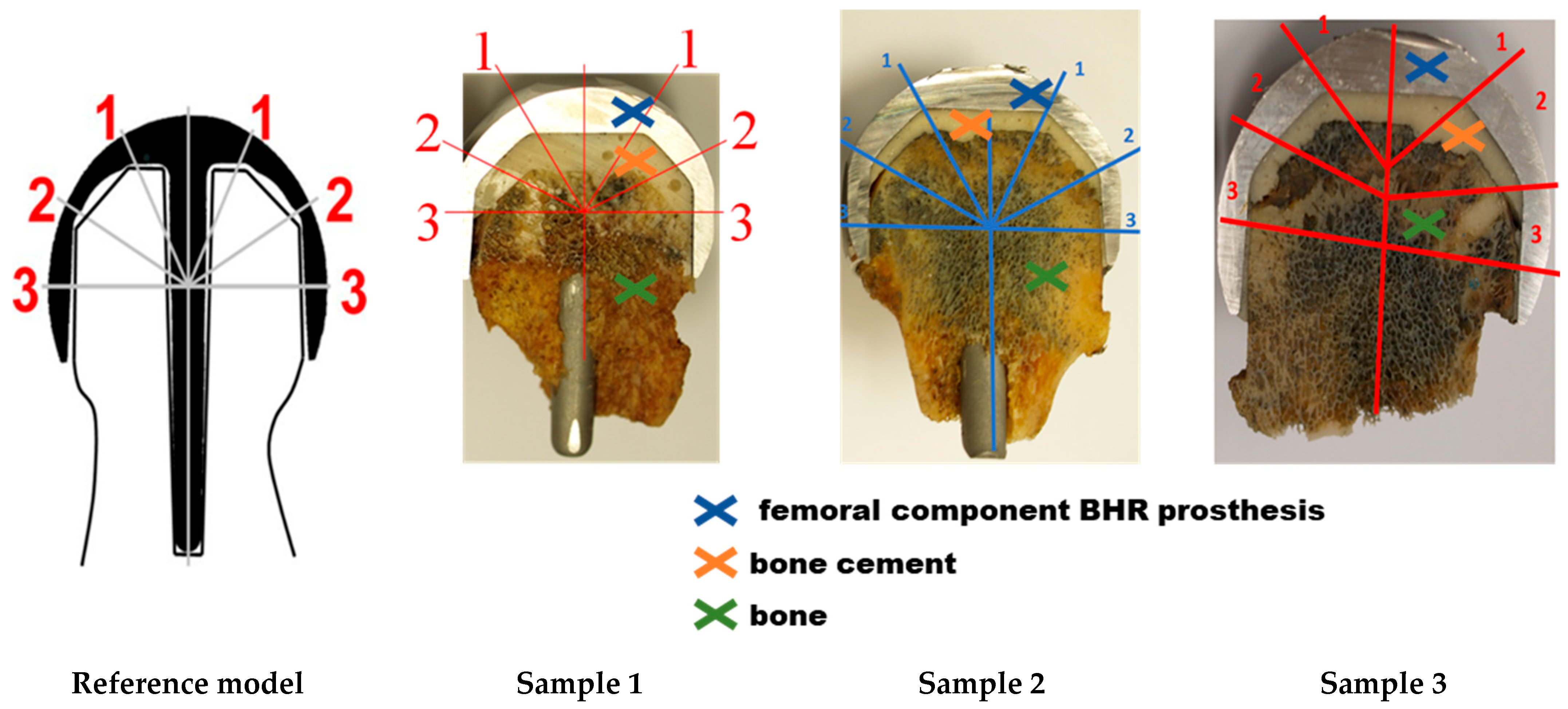
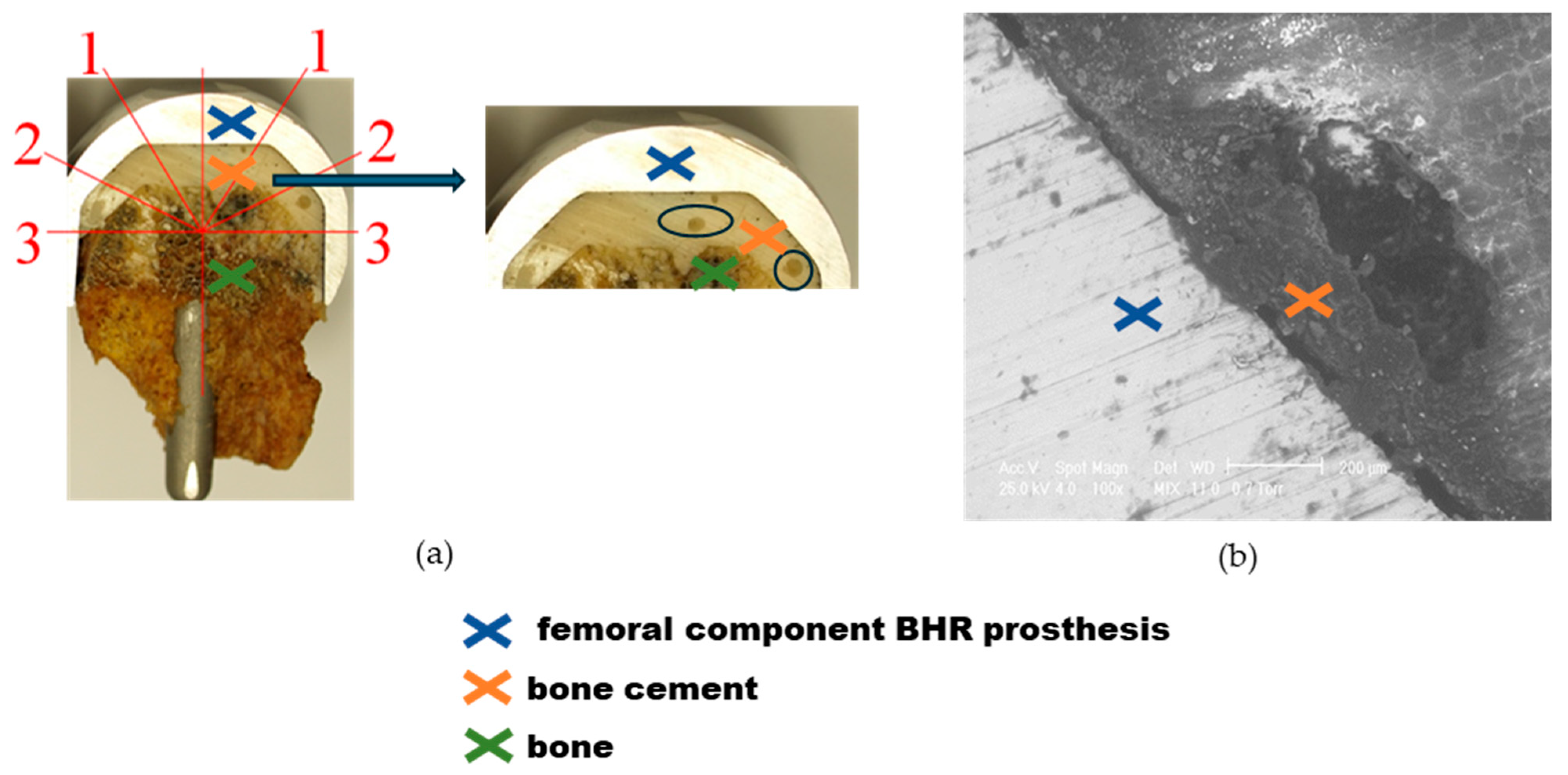
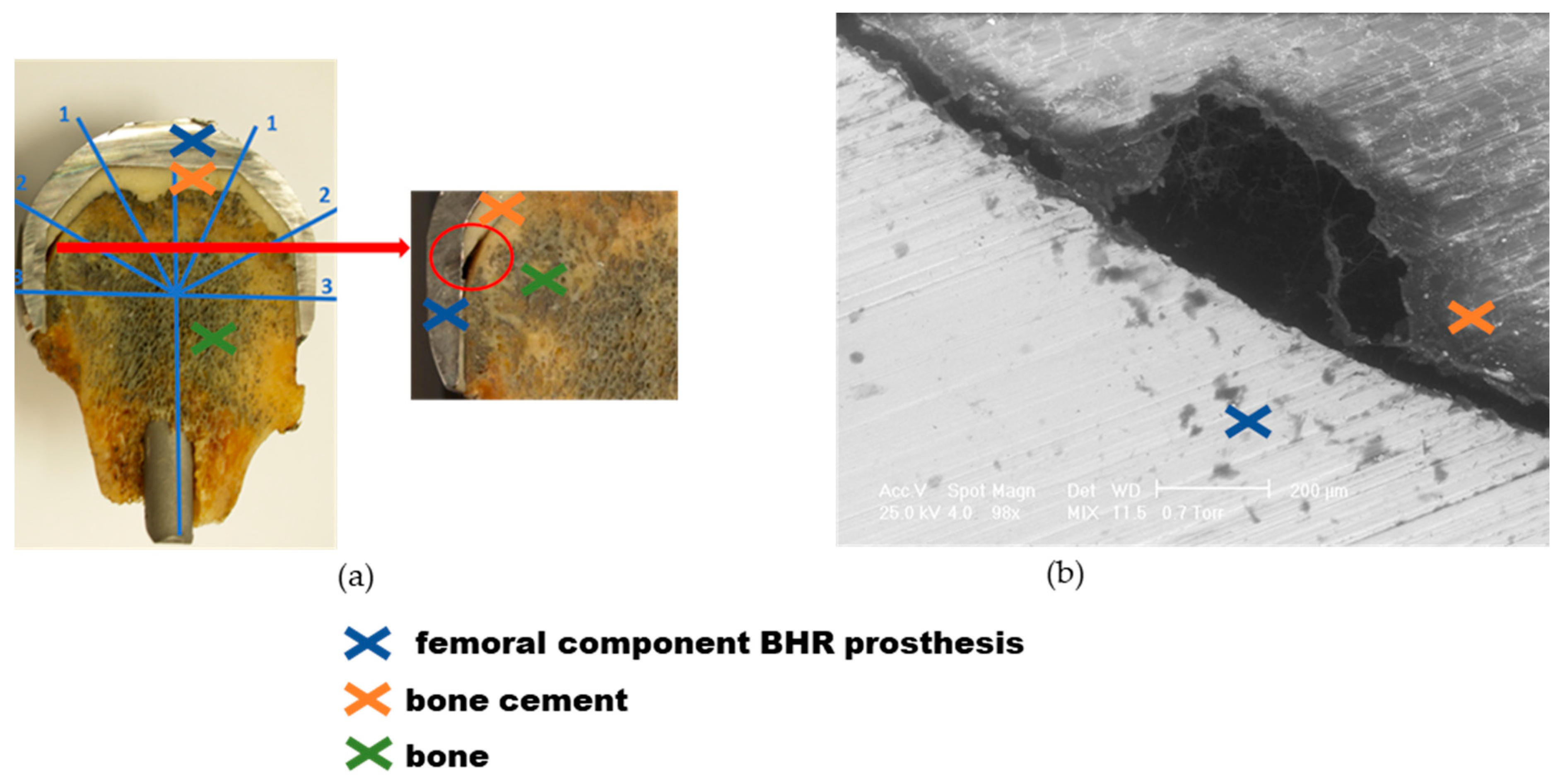
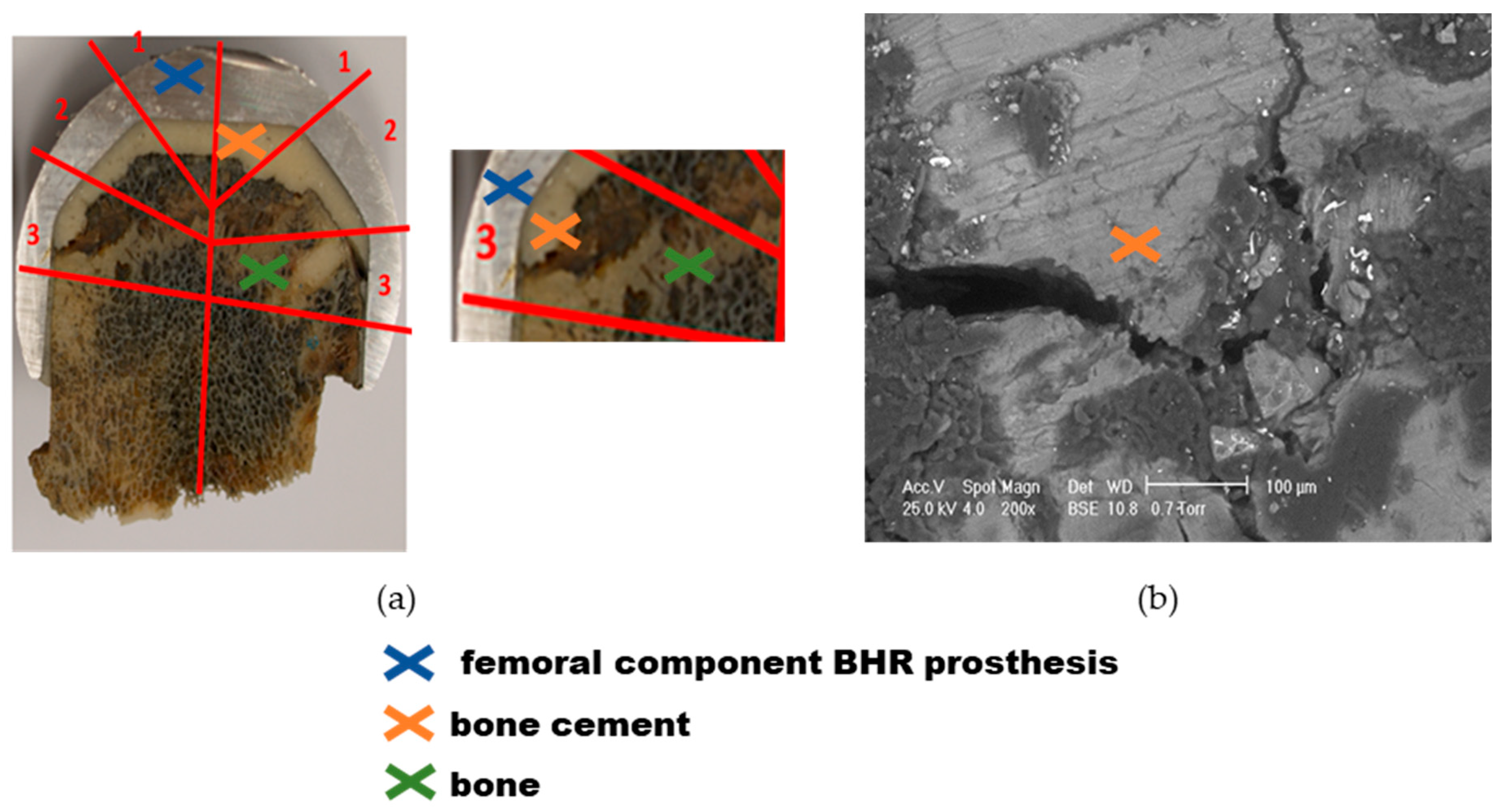
3.2. Explant Analysis
3.3. Limitations of the Study
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pascual-Garrido, C.; Morris, B.L.; Dayton, M.R. Clinical and Functional Outcomes of the Birmingham Hip Resurfacing System. Orthopedics 2016, 39, e236–e239. [Google Scholar] [CrossRef] [PubMed]
- Johanson, P.-E.; Fenstad, A.M.; Furnes, O.; Garellick, G.; Havelin, L.I.; Overgaard, S.; Pedersen, A.B.; Kärrholm, J. Inferior Outcome after Hip Resurfacing Arthroplasty than after Conventional Arthroplasty. Evidence from the Nordic Arthroplasty Register Association (NARA) Database, 1995 to 2007. Acta Orthop. 2010, 81, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.T.; Pasqualini, I.; Mesko, N.; McLaughlin, J.; Brooks, P.J.; Piuzzi, N.S. Conversion Birmingham Hip Resurfacing in Managing Post-Traumatic Arthritis with Retained Femoral Hardware: A Case Report. JBJS Case Connect. 2024, 14. [Google Scholar] [CrossRef] [PubMed]
- McCulloch, R.A.; Martin, A.; Young, B.C.; Kendrick, B.J.; Alvand, A.; Jeys, L.; Stevenson, J.; Palmer, A.J. Frequent Microbiological Profile Changes Are Seen in Subsequent-Revision Hip and Knee Arthroplasty for Prosthetic Joint Infection. J. Bone Jt. Infect. 2023, 8, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Davey, M.S.; Mohan, K.; Gavin, E.; Power, F.R.; Curtin, W.; Kaar, K.; Murphy, C.G. Birmingham Hip Resurfacing: A Systematic Review of Outcomes at Minimum 10-Years Follow-Up. Acta Orthop. Belg. 2023, 89, 581–586. [Google Scholar] [CrossRef]
- Cao, A.; Ghanem, E.S.; Cichos, K.H.; Lichstein, P.; Arthroplasty for Hip Fracture Consortium; Chen, A.F. Comparison Between Orthopaedic Trauma Versus Arthroplasty Fellowship Training on Outcomes of Total Hip Arthroplasty for Femoral Neck Fracture. J. Arthroplast. 2023, 38, S72–S77. [Google Scholar] [CrossRef] [PubMed]
- Wei, D.H.; Hawker, G.A.; Jevsevar, D.S.; Bozic, K.J. Improving Value in Musculoskeletal Care Delivery: AOA Critical Issues. J. Bone Jt. Surg. Am. 2015, 97, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Beaulé, P.E.; Dorey, F.J.; Le Duff, M.J.; Gruen, T.; Amstutz, H.C. Risk Factors Affecting Outcome of Metal-on-Metal Surface Arthroplasty of the Hip. Clin. Orthop. Relat. Res. 2004, 418, 87–93. [Google Scholar] [CrossRef]
- Nandra, R.S.; Elnahal, W.A.; Mayne, A.; Brash, L.; McBryde, C.W.; Treacy, R.B.C. Birmingham Hip Resurfacing at 25 Years. Bone Jt. J. 2024, 106-B, 540–547. [Google Scholar] [CrossRef]
- McClure, M.; Cooke, B.; Elphingstone, J.; Schick, S.; Paul, K.; Jardaly, A.; Brabston, E.; Momaya, A.; Ponce, B. Orthopedic Consequences of Modern Gladiators: A Systematic Review of Lower Extremity Musculoskeletal Issues in Retired NFL Players. Phys. Sportsmed. 2023, 51, 539–548. [Google Scholar] [CrossRef]
- Cristofolini, L.; Teutonico, A.S.; Monti, L.; Cappello, A.; Toni, A. Comparative in Vitro Study on the Long Term Performance of Cemented Hip Stems: Validation of a Protocol to Discriminate between “Good” and “Bad” Designs. J. Biomech. 2003, 36, 1603–1615. [Google Scholar] [CrossRef] [PubMed]
- De Benedittis, A.; Mattioli-Belmonte, M.; Krajewski, A.; Fini, M.; Ravaglioli, A.; Giardino, R.; Biagini, G. In Vitro and in Vivo Assessment of Bone-Implant Interface: A Comparative Study. Int. J. Artif. Organs 1999, 22, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.; Hu, X.Q.; Stewart, T.D.; Williams, S.; Tipper, J.L.; Ingham, E.; Stone, M.H.; Davies, C.; Hatto, P.; Bolton, J.; et al. Wear of Surface Engineered Metal-on-Metal Hip Prostheses. J. Mater. Sci. Mater. Med. 2004, 15, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Kinov, P.; Volpin, G.; Sevi, R.; Tanchev, P.P.; Antonov, B.; Hakim, G. Surgical Treatment of Periprosthetic Femoral Fractures Following Hip Arthroplasty: Our Institutional Experience. Injury 2015, 46, 1945–1950. [Google Scholar] [CrossRef] [PubMed]
- Mabilleau, G.; Kwon, Y.-M.; Pandit, H.; Murray, D.W.; Sabokbar, A. Metal-on-Metal Hip Resurfacing Arthroplasty: A Review of Periprosthetic Biological Reactions. Acta Orthop. 2008, 79, 734–747. [Google Scholar] [CrossRef] [PubMed]
- Revell, M.P.; McBryde, C.W.; Bhatnagar, S.; Pynsent, P.B.; Treacy, R.B.C. Metal-on-Metal Hip Resurfacing in Osteonecrosis of the Femoral Head. J. Bone Jt. Surg. Am. 2006, 88 (Suppl. 3), 98–103. [Google Scholar] [CrossRef]
- Engh, C.A.; Bhal, V.; Hopper, R.H. Metal Levels and Glomerular Filtration Rate after Unilateral Birmingham Hip Resurfacing. Bone Jt. J. 2024, 106-B, 44–50. [Google Scholar] [CrossRef]
- Reito, A.; Lainiala, O.; Berryman, F.; Dunlop, D.J.; Eskelinen, A.; Matharu, G.S. Long-Term Changes in Blood Metal Ion Levels in Patients with Hip Resurfacing Implants: Implications for Patient Surveillance after 10 Years Follow-Up. Hip Int. 2023, 33, 864–871. [Google Scholar] [CrossRef] [PubMed]
- Watt Kearns, S.J.; Bourget-Murray, J.; Johnston, K.; Werle, J. Comparing 1-Year and 10-Year Whole Blood Metal Ion Results Following Birmingham Hip Resurfacing for Osteoarthritis. Can. J. Surg. 2022, 65, E504–E511. [Google Scholar] [CrossRef]
- Oxblom, A.; Hedlund, H.; Itayem, R.; Felländer-Tsai, L.; Vidgren, M.; Rolfson, O.; Brismar, H. Careful Patient Selection Together with Optimal Implant Positioning May Reduce but Does Not Eliminate the Risk of Elevated Serum Cobalt and Chrome Levels Following Metal-on-Metal Hip Resurfacing. Hip Int. 2023, 33, 872–879. [Google Scholar] [CrossRef]
- Skinner, J.A.; Todo, S.; Taylor, M.; Wang, J.S.; Pinskerova, V.; Scott, G. Should the Cement Mantle around the Femoral Component Be Thick or Thin? J. Bone Jt. Surg. Br. 2003, 85, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Ramaniraka, N.A.; Rakotomanana, L.R.; Leyvraz, P.-F. The Fixation of the Cemented Femoral Component: Effects of stem stiffness, cement thickness and roughness of the cement-bone surface. J. Bone Jt. Surg. Br. 2000, 82-B, 297–303. [Google Scholar] [CrossRef]
- Lindahl, H.; Malchau, H.; Herberts, P.; Garellick, G. Periprosthetic Femoral Fractures Classification and Demographics of 1049 Periprosthetic Femoral Fractures from the Swedish National Hip Arthroplasty Register. J Arthroplast. 2005, 20, 857–865. [Google Scholar] [CrossRef]
- Ni, G.X.; Lu, W.W.; Chiu, K.Y.; Li, Z.Y.; Fong, D.Y.T.; Luk, K.D.K. Strontium-Containing Hydroxyapatite (Sr-HA) Bioactive Cement for Primary Hip Replacement: An in Vivo Study. J. Biomed. Mater. Res. Part B Appl. Biomater. 2006, 77, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.T.; Chen, Q.Z.; Lu, W.W.; Leong, J.C.Y.; Chan, W.K.; Cheung, K.M.C.; Luk, K.D.K. Ultrastructural Study of Mineralization of a Strontium-Containing Hydroxyapatite (Sr-HA) Cement in Vivo. J. Biomed. Mater. Res. Part A 2004, 70, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Robu, A.; Antoniac, A.; Ciocoiu, R.; Grosu, E.; Rau, J.V.; Fosca, M.; Krasnyuk, I.I.; Pircalabioru, G.G.; Manescu Paltanea, V.; Antoniac, I.; et al. Effect of the Antimicrobial Agents Peppermint Essential Oil and Silver Nanoparticles on Bone Cement Properties. Biomimetics 2022, 7, 137. [Google Scholar] [CrossRef]
- Mabrouk, A.; Feathers, J.R.; Mahmood, A.; West, R.; Pandit, H.; Lamb, J.N. Systematic Review and Meta-Analysis of Studies Comparing the Rate of Post-Operative Periprosthetic Fracture Following Hip Arthroplasty with a Polished Taper Slip versus Composite Beam Stem. J. Arthroplast. 2024, 39, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, J.; Rapuri, V.R.; Purtill, J.J.; Sharkey, P.F.; Rothman, R.H.; Hozack, W.J. Treatment Protocol for Proximal Femoral Periprosthetic Fractures. J. Bone Jt. Surg. Am. 2004, 86-A (Suppl. 2), 8–16. [Google Scholar] [CrossRef]
- Tsiridis, E.; Gie, G.A. Mal-United Femoral Fractures Adjacent to Loose Total Hip Arthroplasties. Salvage with Impaction Grafting. A Case Report. Injury 2002, 33, 81–83. [Google Scholar] [CrossRef]
- Robu, A.; Ciocoiu, R.; Antoniac, A.; Antoniac, I.; Raiciu, A.D.; Dura, H.; Forna, N.; Cristea, M.B.; Carstoc, I.D. Bone Cements Used for Hip Prosthesis Fixation: The Influence of the Handling Procedures on Functional Properties Observed during In Vitro Study. Materials 2022, 15, 2967. [Google Scholar] [CrossRef]
- Breusch, S.; Malchau, H. The Well-Cemented Total Hip Arthroplasty; Springer: Berlin/Heidelberg, Germany, 2005; ISBN 978-3-540-24197-3. [Google Scholar]
- Ramanathan, S.; Lin, Y.-C.; Thirumurugan, S.; Hu, C.-C.; Duann, Y.-F.; Chung, R.-J. Poly(Methyl Methacrylate) in Orthopedics: Strategies, Challenges, and Prospects in Bone Tissue Engineering. Polymers 2024, 16, 367. [Google Scholar] [CrossRef] [PubMed]
- Vaishya, R.; Chauhan, M.; Vaish, A. Bone Cement. J. Clin. Orthop. Trauma 2013, 4, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Hoey, D.; Taylor, D. Comparison of the Fatigue Behaviour of Two Different Forms of PMMA. Fatigue Fract. Eng. Mater. Struct. 2009, 32, 261–269. [Google Scholar] [CrossRef]
- Wang, Z.; Luo, S.; Yang, L.; Wu, Z.; Zhang, C.; Teng, J.; Zou, Z.; Ye, C. Intelligent and Bioactive Osseointegration of the Implanted Piezoelectric Bone Cement with the Host Bone Is Realized by Biomechanical Energy. ACS Appl. Mater. Interfaces 2024, 16, 20157–20168. [Google Scholar] [CrossRef] [PubMed]
- ISO 5833 (2002); Implants For Surgery—Acrylic Resin Cements. ISO: Geneva, Switzerland, 2022.
- Wilson, D.; Frei, H.; Masri, B.A.; Oxland, T.R.; Duncan, C.P. A Biomechanical Study Comparing Cortical Onlay Allograft Struts and Plates in the Treatment of Periprosthetic Femoral Fractures. Clin. Biomech. 2005, 20, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Spina, M.; Rocca, G.; Canella, A.; Scalvi, A. Causes of Failure in Periprosthetic Fractures of the Hip at 1- to 14-Year Follow-Up. Injury 2014, 45 (Suppl. 6), S85–S92. [Google Scholar] [CrossRef] [PubMed]
- Moreta, J.; Aguirre, U.; de Ugarte, O.S.; Jáuregui, I.; Mozos, J.L.M.-D.L. Functional and Radiological Outcome of Periprosthetic Femoral Fractures after Hip Arthroplasty. Injury 2015, 46, 292–298. [Google Scholar] [CrossRef]
- Carrothers, A.D.; Gilbert, R.E.; Richardson, J.B. Birmingham Hip Resurfacing in Patients Who Are Seventy Years of Age or Older. Hip Int. 2011, 21, 217–224. [Google Scholar] [CrossRef]
- Molloy, J.; Handford, C.; Coolican, J.; Molloy, T.; Walter, W. Long-Term Outcomes of Birmingham Hip Resurfacing Arthroplasty: A Systematic Review of Independent Series with At Least 10 Years of Follow-Up. JB JS Open Access 2024, 9, e23.00057. [Google Scholar] [CrossRef]
- Lass, R.; Bechler, U.; Springer, B.; Rueckl, K.; Hanreich, C.; Boettner, F. Midterm Results of the Birmingham Hip Resurfacing: A Single-Surgeon Series. Arch. Orthop. Trauma Surg. 2023, 143, 1041–1048. [Google Scholar] [CrossRef]
- Uemura, K.; Takao, M.; Hamada, H.; Sakai, T.; Ohzono, K.; Sugano, N. Long-Term Results of Birmingham Hip Resurfacing Arthroplasty in Asian Patients. J. Artif. Organs 2018, 21, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Frew, N.; Johnson, G. Survival of the Birmingham Hip Resurfacing in Young Men up to 13 Years Post-Operatively. Acta Orthop. Belg. 2017, 83, 67–73. [Google Scholar] [PubMed]
- Matharu, G.S.; McBryde, C.W.; Revell, M.P.; Pynsent, P.B. Femoral Neck Fracture after Birmingham Hip Resurfacing Arthroplasty: Prevalence, Time to Fracture, and Outcome after Revision. J. Arthroplast. 2013, 28, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Hannon, C.P.; Goodman, S.M.; Austin, M.S.; Yates, A.; Guyatt, G.; Aggarwal, V.K.; Baker, J.F.; Bass, P.; Bekele, D.I.; Dass, D.; et al. 2023 American College of Rheumatology and American Association of Hip and Knee Surgeons Clinical Practice Guideline for the Optimal Timing of Elective Hip or Knee Arthroplasty for Patients with Symptomatic Moderate-to-Severe Osteoarthritis or Advanced Symptomatic Osteonecrosis with Secondary Arthritis for Whom Nonoperative Therapy Is Ineffective. J. Arthroplast. 2023, 38, 2193–2201. [Google Scholar] [CrossRef]
- Dhawan, R.; Young, D.A.; Van Eemeren, A.; Shimmin, A. Birmingham Hip Resurfacing at 20 Years. Bone Jt. J. 2023, 105-B, 946–952. [Google Scholar] [CrossRef]
- Cichos, K.H.; McGwin, G.; Boyd, B.; Arthroplasty for Hip Fracture Consortium; Ghanem, E.S. Direct Anterior Approach Total Hip Arthroplasty Is Associated with Reduced 1-Year Mortality and Surgical Complications After Femoral Neck Fracture. J. Arthroplast. 2023, 38, 2347–2354.e2. [Google Scholar] [CrossRef] [PubMed]
- Dahlgren, N.; Jacob, R.; Cantrell, C.; Sowers, M.; Shah, A.B.; Naranje, S.M. Unusual Arteriovenous Malformation in Total Hip Arthroplasty: Case Report of a Complicated Perioperative Course. Rev. Bras Ortop. 2023, 58, e818–e821. [Google Scholar] [CrossRef]
- Davies, A.P.; Willert, H.G.; Campbell, P.A.; Learmonth, I.D.; Case, C.P. An Unusual Lymphocytic Perivascular Infiltration in Tissues around Contemporary Metal-on-Metal Joint Replacements. J. Bone Jt. Surg. Am. 2005, 87, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Willert, H.-G.; Buchhorn, G.H.; Fayyazi, A.; Flury, R.; Windler, M.; Köster, G.; Lohmann, C.H. Metal-on-Metal Bearings and Hypersensitivity in Patients with Artificial Hip Joints. A Clinical and Histomorphological Study. J. Bone Jt. Surg. Am. 2005, 87, 28–36. [Google Scholar] [CrossRef]
- Witzleb, W.-C.; Hanisch, U.; Kolar, N.; Krummenauer, F.; Guenther, K.-P. Neo-Capsule Tissue Reactions in Metal-on-Metal Hip Arthroplasty. Acta Orthop. 2007, 78, 211–220. [Google Scholar] [CrossRef]
- Pandit, H.; Glyn-Jones, S.; McLardy-Smith, P.; Gundle, R.; Whitwell, D.; Gibbons, C.L.M.; Ostlere, S.; Athanasou, N.; Gill, H.S.; Murray, D.W. Pseudotumours Associated with Metal-on-Metal Hip Resurfacings. J. Bone Jt. Surg. Br. 2008, 90, 847–851. [Google Scholar] [CrossRef]
- Fishley, W.; Nandra, R.; Carluke, I.; Partington, P.F.; Reed, M.R.; Kramer, D.J.; Wilson, M.J.; Hubble, M.J.W.; Howell, J.R.; Whitehouse, S.L.; et al. Revision of Metal-on-Metal Hip Replacements with Dual-Mobility Bearings and Acetabular Component Retention. Bone Jt. Open 2024, 5, 514–523. [Google Scholar] [CrossRef] [PubMed]
- Akçaalan, S.; Kengil, M.C.; Çağlar, C.; Uğurlu, M. Is There Still an Indication for the Birmingham Hip Resurfacing in Femoral Head Osteonecrosis? Int. Orthop. 2024, 48, 1157–1163. [Google Scholar] [CrossRef] [PubMed]
- Ouwendijk, M.; Van Der Bracht, H.; Jansegers, E. Clinical, Functional and Radiographic Long-Term Follow-Up (7–12 Years) of Birmingham Hip Resurfacing, Including Metal Ions Evaluation: A Single Surgeon Series. Acta Orthop. Belg. 2024, 90, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Nasser, A.A.H.H.; Prakash, R.; Handford, C.; Osman, K.; Chauhan, G.S.; Nandra, R.; Mahmood, A.; Dewan, V.; Davidson, J.; Al-Azzawi, M.; et al. Predictors of Mortality in Periprosthetic Fractures of the Hip: Results from the National PPF Study. Injury 2023, 54, 111152. [Google Scholar] [CrossRef] [PubMed]
- Coulter, G.; Young, D.A.; Dalziel, R.E.; Shimmin, A.J. Birmingham Hip Resurfacing at a Mean of Ten Years: Results from an Independent Centre. J. Bone Jt. Surg. Br. 2012, 94, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Murray, D.W.; Grammatopoulos, G.; Pandit, H.; Gundle, R.; Gill, H.S.; McLardy-Smith, P. The Ten-Year Survival of the Birmingham Hip Resurfacing: An Independent Series. J. Bone Jt. Surg. Br. 2012, 94, 1180–1186. [Google Scholar] [CrossRef]
- Treacy, R.B.C.; McBryde, C.W.; Shears, E.; Pynsent, P.B. Birmingham Hip Resurfacing: A Minimum Follow-Up of Ten Years. J. Bone Jt. Surg. Br. 2011, 93, 27–33. [Google Scholar] [CrossRef] [PubMed]
- McBryde, C.W.; Theivendran, K.; Thomas, A.M.C.; Treacy, R.B.C.; Pynsent, P.B. The Influence of Head Size and Sex on the Outcome of Birmingham Hip Resurfacing. J. Bone Jt. Surg. Am. 2010, 92, 105–112. [Google Scholar] [CrossRef]
- Treacy, R.B.C.; McBryde, C.W.; Pynsent, P.B. Birmingham Hip Resurfacing Arthroplasty. A Minimum Follow-Up of Five Years. J. Bone Jt. Surg. Br. 2005, 87, 167–170. [Google Scholar] [CrossRef]
- McMinn, D.J.W.; Daniel, J.; Ziaee, H.; Pradhan, C. Indications and Results of Hip Resurfacing. Int. Orthop. 2011, 35, 231–237. [Google Scholar] [CrossRef]


| Property | Remarks | Ref. |
|---|---|---|
| Adhesion | The cement must adhere well to the implant to prevent micromotion, which can lead to implant loosening. Surface treatments of implants, such as roughening or coating with bioactive materials, can enhance this adhesion | [32] |
| Load transfer | The cement must allow uniform mechanical load transfer between the bone and the prosthesis. | [33] |
| Mechanical properties | The mechanical properties of the cement must be compatible with the implant and the surrounding bone. The mechanical mismatch between the rigid PMMA and the more elastic bone can lead to stress concentrations, potentially causing microcracks and long-term failure. | [34] |
| Mechanical interlock | To accomplish interlock, the surface of the bones must be rough and irregular. The strength of the cement-bone interaction increases with deeper cement penetration. | [31] |
| Thermal effects | Because of the potential for thermal necrosis of bone tissue resulting from the exothermic reaction of PMMA curing, the ISO 5833 (2002) standard sets a 90 °C restriction on the hardening temperature of bone cement. Controlling the polymerization temperature is crucial to mitigate these effects. | [31,36] |
| Biocompatibility | PMMA is biocompatible, but it can cause a mild inflammatory response. The exothermic polymerization process can determine thermal necrosis. The presence of residual monomer can be cytotoxic. | [32] |
| Osseointegration | Osseointegration relies on mechanical interlock rather than chemical bonding. While PMMA itself is not osteoinductive, the surface texture and porosity can be modified to enhance integration with bone. | [35] |
| Gender | Diagnosis | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| P.C. | N.A.C.F. | S.C. | D.S.P. | B.C. | O.F.H. | O.D. | P.T. | ||
| Women | 25 | 53 | 3 | 16 | 0 | 0 | 0 | 1 | 98 |
| Men | 44 | 122 | 12 | 21 | 1 | 1 | 1 | 0 | 202 |
| Total | 69 | 175 | 15 | 37 | 1 | 1 | 1 | 1 | 300 |
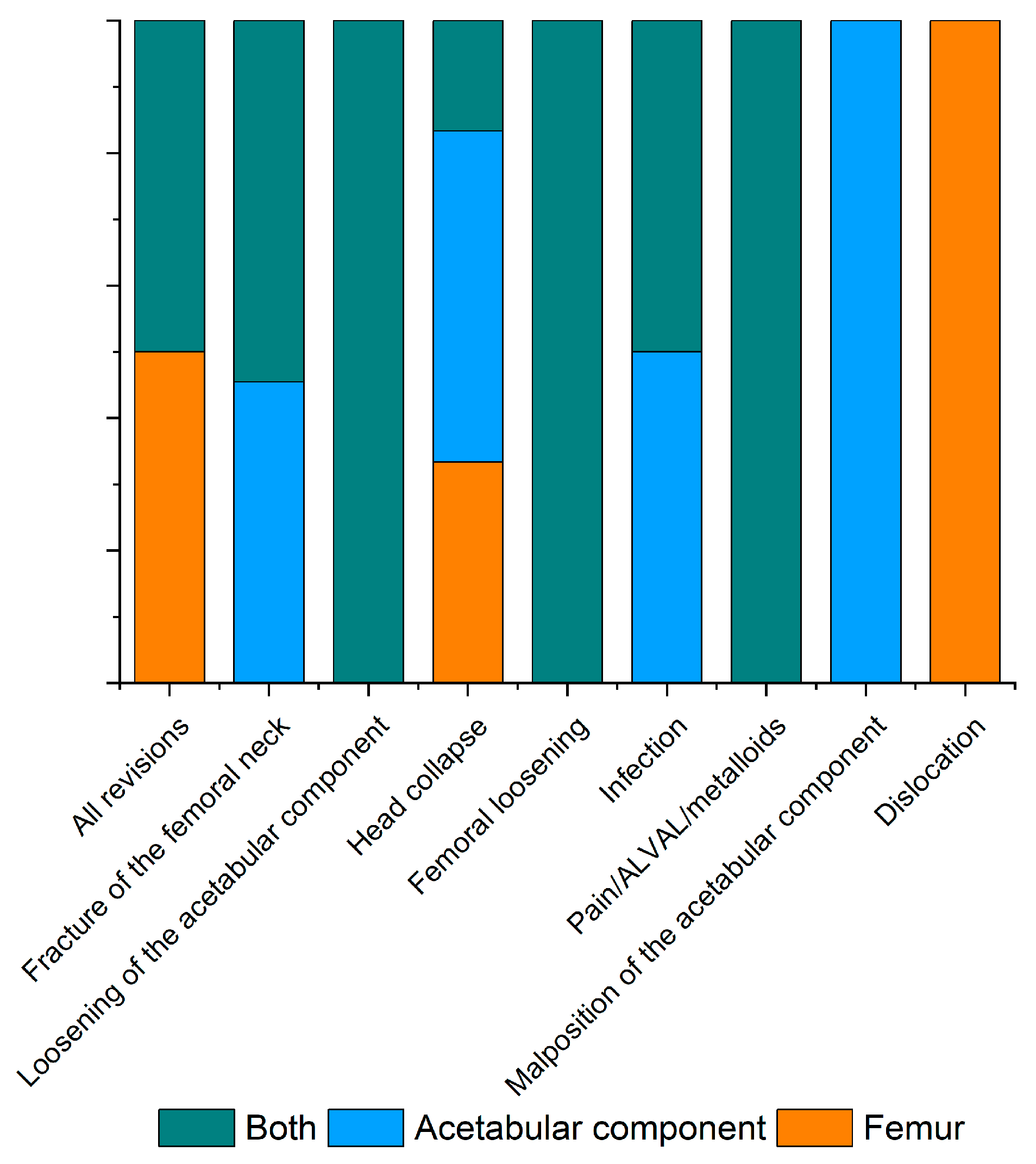
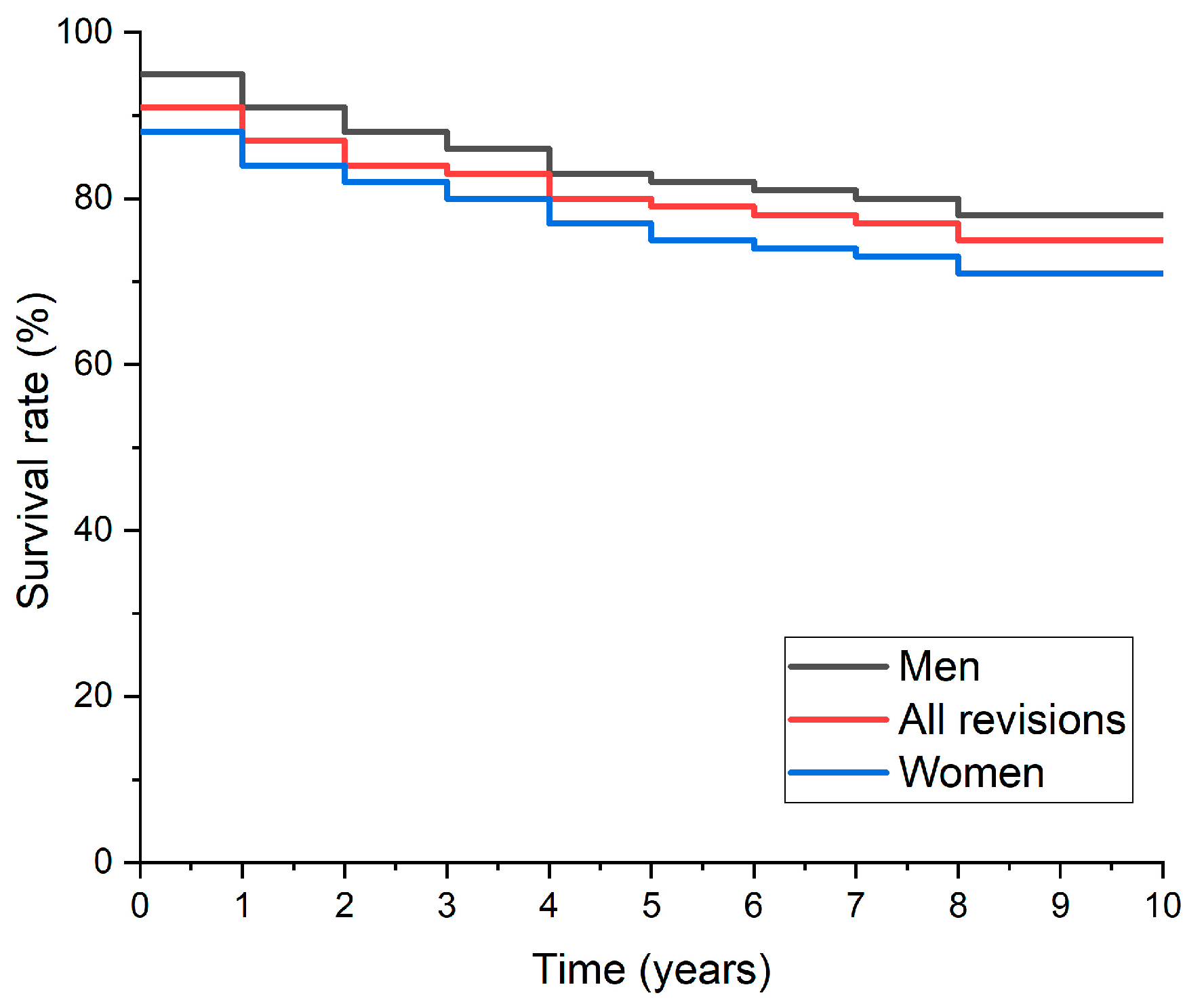
| Mode of Failure | Total (%) | Men | Women | p-Estimated Value |
|---|---|---|---|---|
| All revisions | 30 (10.0) | 20 | 10 | <0.001 |
| Fracture of the femoral neck | 9 (3.0) | 6 | 3 | 0.005 |
| Loosening of the acetabular component | 6 (2.0) | 4 | 2 | 0.02 |
| Head collapse | 5 (1.7) | 3 | 2 | 0.03 |
| Femoral loosening | 3 (1.0) | 2 | 1 | 0.06 |
| Infection | 3 (1.0) | 2 | 1 | 0.06 |
| Pain/(ALVAL)/metalloids | 2 (0.7) | 1 | 1 | 0.11 |
| Malposition of the acetabular component | 1 (0.3) | 1 | 0 | 0.27 |
| Dislocation | 2 (0.7) | 1 | 1 | 0.1 |
| Preoperative Diagnosis | Men | Women | Potential Adverse Effect on Acetabular Component Stability |
|---|---|---|---|
| Osteoarthritis | 10 | 5 | No |
| Acetabular Dysplasia | 1 | 1 | Yes |
| Previous Shelf Procedure for Acetabular Dysplasia | 1 | 1 | Yes |
| Renal Failure | 1 | 1 | Yes |
| Avascular Necrosis of the Femoral Head Following Radiotherapy for Pelvic Osteosarcoma | 1 | 1 | Yes |
| Unknown | 3 | 2 | Unknown |
| Mode of Failure | Total (%) | Men | Women | p Estimated Value |
|---|---|---|---|---|
| All revisions | 2.9 (0.003 ÷ 11.0) | 1.7 (0.04 ÷ 8.2) | 4.5 (0.002 ÷ 11.0) | <0.001 |
| Fracture of the femoral neck | 1.5 (0.02 ÷ 11.0) | 0.5 (0.04 ÷ 3.8) | 3.0 (0.002 ÷ 11.0) | 0.0012 |
| Loosening of the acetabular component | 2.4 (0.01 ÷ 9.7) | 1.4 (0.04 ÷ 3.0) | 3.0 (0.01 ÷ 9.7) | 0.16 |
| Head collapse | 3.9 (0.3 ÷ 9.8) | 3.1 (0.6 ÷ 7.8) | 5.2 (0.3 ÷ 9.8) | 0.28 |
| Femoral loosening | 3.7 (0.1 ÷ 9.1) | 3.0 (0.1 ÷ 5.8) | 4.4 (0.4 ÷ 8.8) | 0.50 |
| Infection | 3.1 (0.5 ÷ 9.6) | 2.2 (0.5 ÷ 4.4) | 4.0 (1.0 ÷ 9.6) | 0.53 |
| Pain/ALVAL/metalloids | 5.2 (1.0 ÷ 10.2) | 3.3 (1.0 ÷ 6.5) | 6.8 (1.7 ÷ 10.2) | 0.16 |
| Malposition of the acetabular component | 4.2 (1.5 ÷ 6.5) | 1.5 (N/A) | 6.0 (1.5 ÷ 6.5) | N/A |
| Dislocation | 3.9 (0.003 ÷ 9.5) | 0 | 3.9 (0.003 ÷ 9.5) | N/A |
| Loosening of both components | 3.4 (0.3 to 5.9) | 1.6 (0.3 to 3.0) | 4.6 (3.4 to 5.9) | 1.0 |
| Surgical Simplex P (Stryker Howmedica Osteonics) | Aminofix 1 (Groupe Lepine) | Aminofix 3 (Groupe Lepine) | ||
|---|---|---|---|---|
| Liquid component | 18.79 g | 14.4 g | 16.4 g | |
| Methyl methacrylate | Monomer | 18.33 | 12.28 | 13.99 |
| Butyl methacrylate | Monomer | - | 1.90 | 2.16 |
| N,N-dimethyl-p-toluidine | Activator | 0.46 | 0.22 | 0.25 |
| Hydroquinone | Inhibitor | 60 ppm | 20 ppm | 20 ppm |
| Powder component | 41 g | 40 g | 40 g | |
| Polymethyl methacrylate | Pre-polymerized polymer | 6.00 | 33.68 | 33.52 |
| Benzoyl peroxide | Initiator | 0.50 | 0.96 | 1.12 |
| Methyl methacrylate-styrene copolymer | Pre-polymerized copolymer | 30.00 | - | - |
| Barium sulphate | Radiopaque agent | 4 | 3.84 | 3.84 |
| Gentamicin sulfate | Antibiotic | - | 1.52 | 1.52 |
| Erytromycin Colistin | Antibiotic | 0.50 | - | - |
| Sulphomethate | Antibiotic | 3.00 million I.U. | - | - |
| Sodium EP viscosity | low | standard | low |
| Sample | Zone | Average Thickness of the Cement Layer (mm) |
|---|---|---|
| Sample 1 | 1 | 24.86 |
| 2 | 15.68 | |
| 3 | 13.92 | |
| Sample 2 | 12.83 | |
| 2 | 7.59 | |
| 3 | 5.90 | |
| Sample 3 | 1 | 13.48 |
| 2 | 12.29 | |
| 3 | 9.43 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antoniac, I.; Valeanu, N.; Niculescu, M.; Antoniac, A.; Robu, A.; Popescu, L.; Manescu, V.; Anusca, D.; Enachescu, C.I. Outcomes of Birmingham Hip Resurfacing Based on Clinical Aspects and Retrieval Analysis of Failed Prosthesis. Materials 2024, 17, 3965. https://doi.org/10.3390/ma17163965
Antoniac I, Valeanu N, Niculescu M, Antoniac A, Robu A, Popescu L, Manescu V, Anusca D, Enachescu CI. Outcomes of Birmingham Hip Resurfacing Based on Clinical Aspects and Retrieval Analysis of Failed Prosthesis. Materials. 2024; 17(16):3965. https://doi.org/10.3390/ma17163965
Chicago/Turabian StyleAntoniac, Iulian, Niculae Valeanu, Marius Niculescu, Aurora Antoniac, Alina Robu, Larisa Popescu, Veronica Manescu (Paltanea), Dan Anusca, and Catalin Ionel Enachescu. 2024. "Outcomes of Birmingham Hip Resurfacing Based on Clinical Aspects and Retrieval Analysis of Failed Prosthesis" Materials 17, no. 16: 3965. https://doi.org/10.3390/ma17163965






