A Comparison of the Shear Bond Strength between a Luting Composite Resin and Both Machinable and Printable Ceramic–Glass Polymer Materials
Abstract
1. Introduction
2. Materials and Methods
2.1. Preparation of Substrates
2.2. Application of Luting Composite Resin
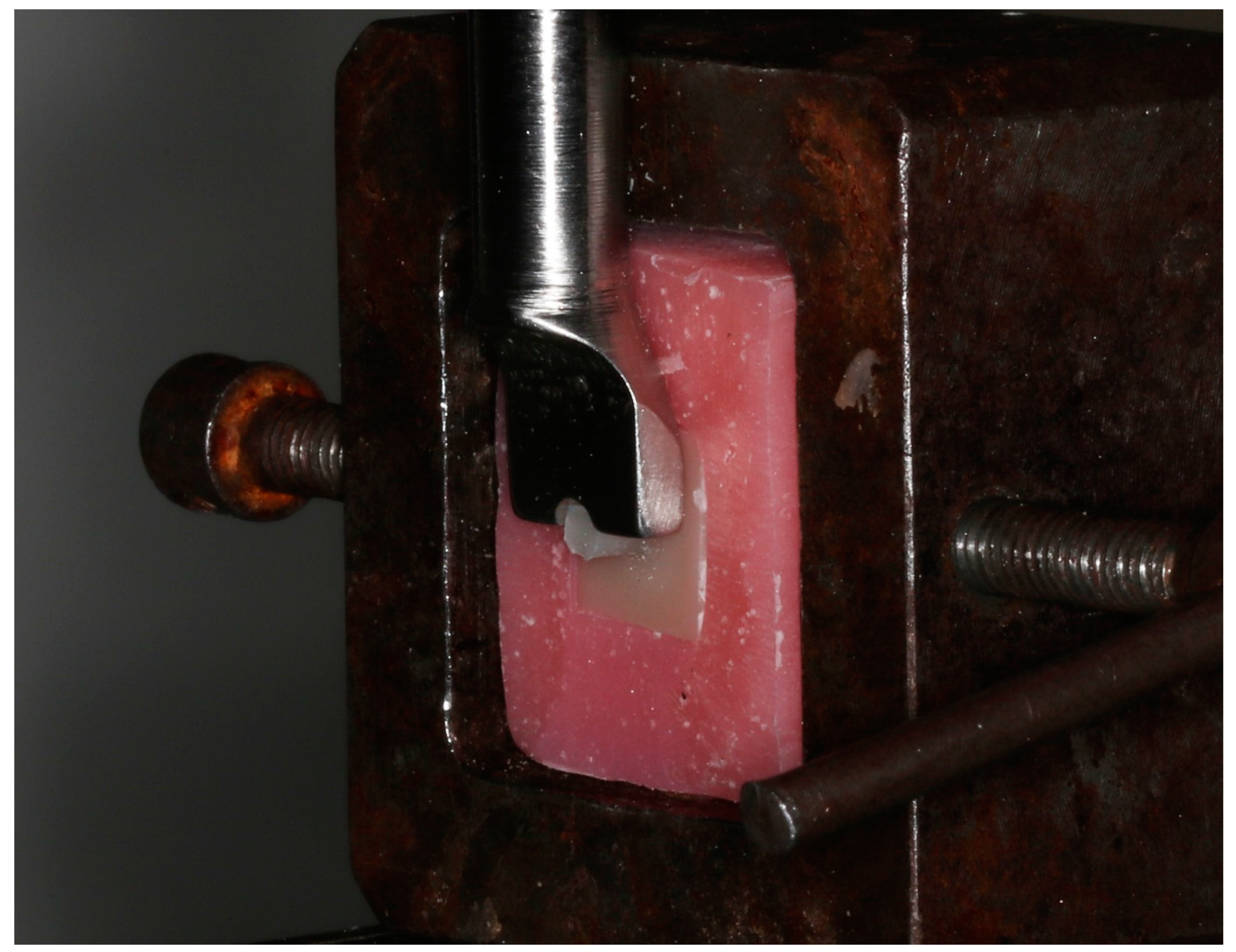
2.3. Shear Bond Strength (SBS) Test
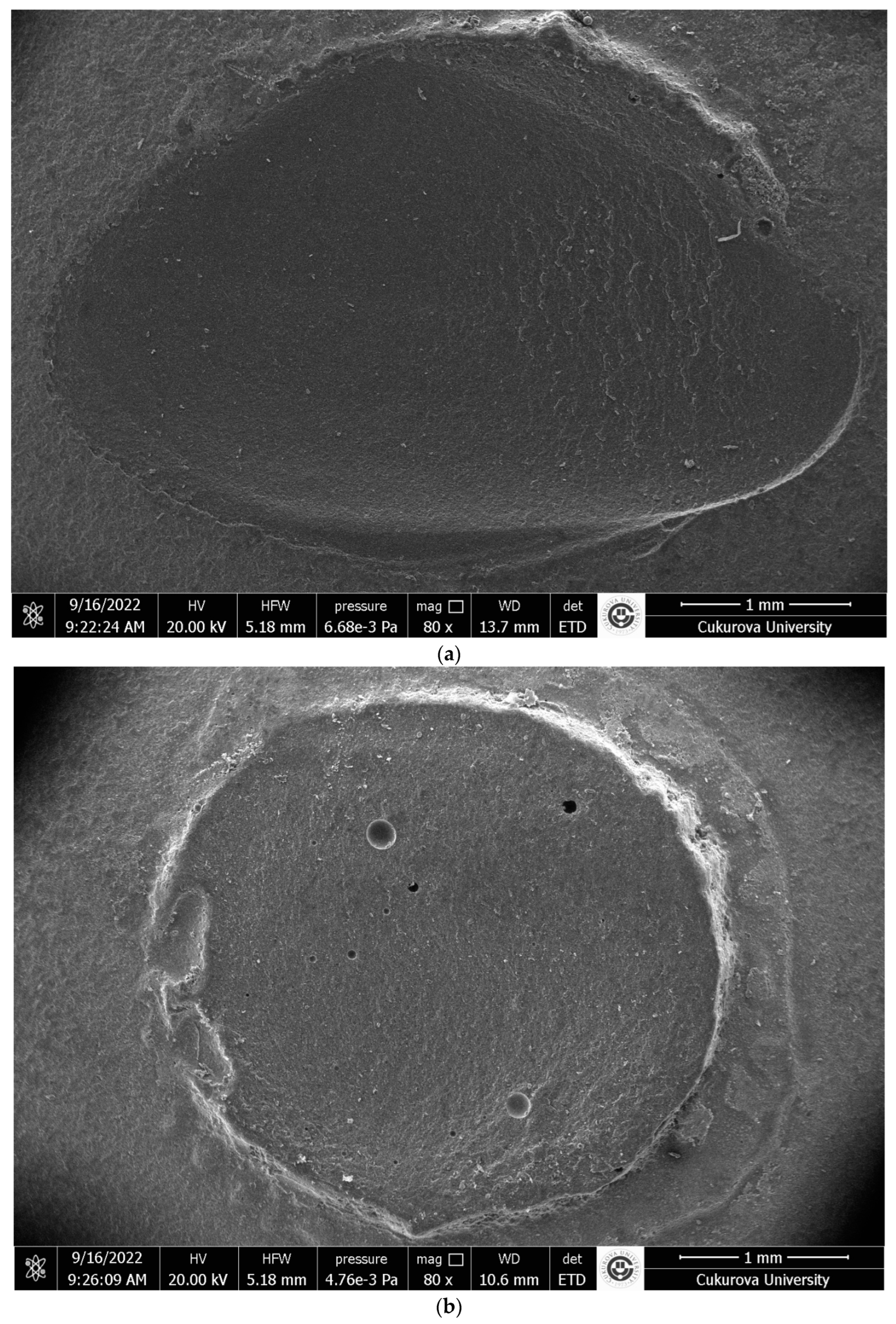
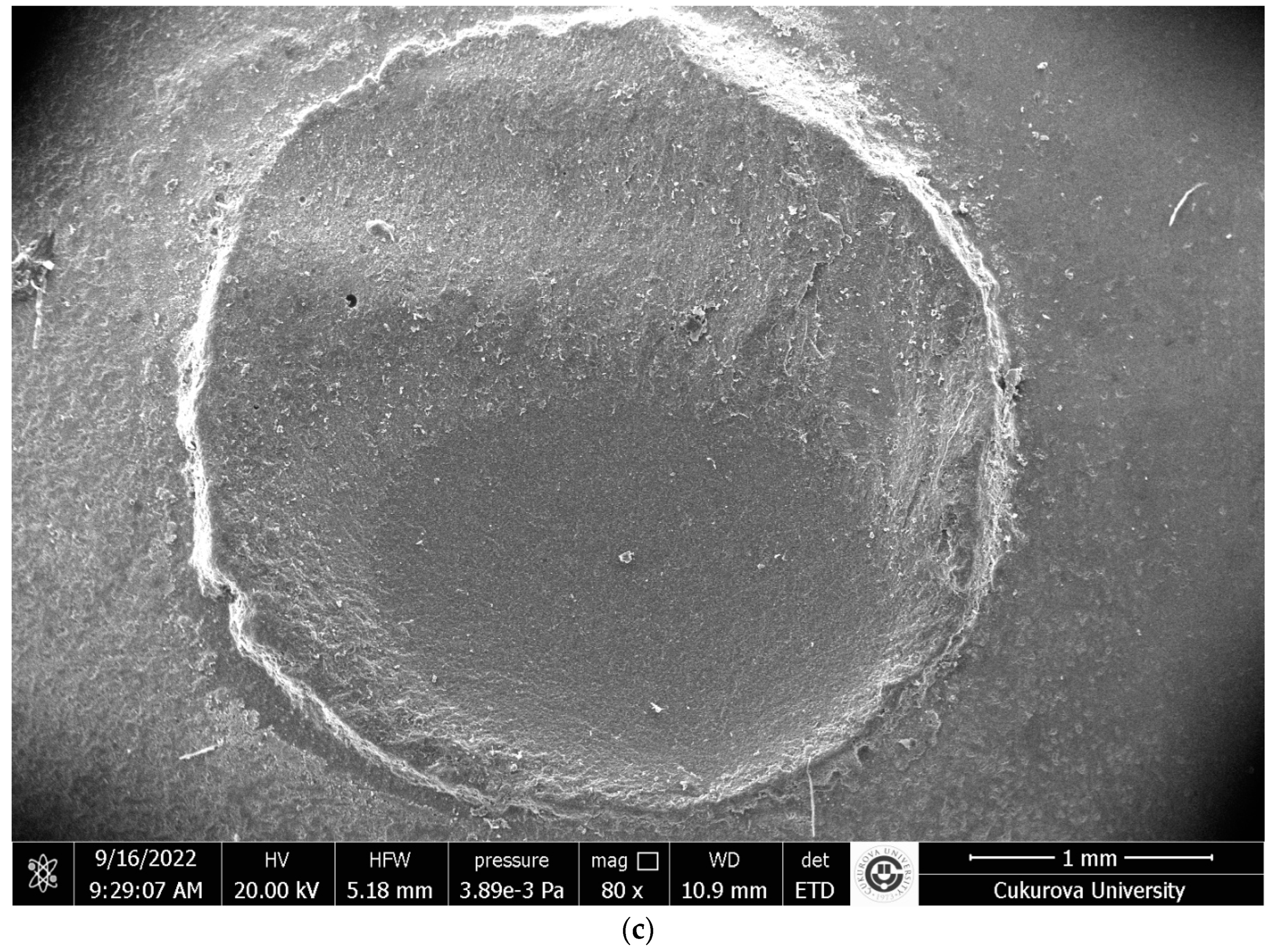
2.4. Microscopic Characterization of Failure Modes
2.5. Statistical Analysis
3. Results
3.1. Shear Bond Strength (SBS) and Weibull Modulus
3.2. Distribution of the Failure Modes
4. Discussion
5. Conclusions
- There is no difference in the SBS of the SLC to both printable 3D-PR and machinable ceramic–glass polymers, VE or CS. SBSs of all tested materials had enough to ensure good clinical performance.
- The lowest Weibull modulus was seen for the printable 3D-PR, but both printable and machinable materials in the present study have shown a homogenous distribution.
- In the failure modes of both printable and machinable materials in the present study, there is no difference, and the predominant failure mode was mixed mode for 3D-PR, VE, and CS.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Awada, A.; Nathanson, D. Mechanical Properties of Resin-Ceramic CAD/CAM Restorative Materials. J. Prosthet. Dent. 2015, 114, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Alp, G.; Subaşı, M.G.; Johnston, W.M.; Yilmaz, B. Effect of Different Resin Cements and Surface Treatments on the Shear Bond Strength of Ceramic-Glass Polymer Materials. J. Prosthet. Dent. 2018, 120, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Sarahneh, O.; Günal-Abduljalil, B. The Effect of Silane and Universal Adhesives on the Micro-Shear Bond Strength of Current Resin-Matrix Ceramics. J. Adv. Prosthodont. 2021, 13, 292–303. [Google Scholar] [CrossRef]
- Nagasawa, Y.; Eda, Y.; Shigeta, H.; Ferrari, M.; Nakajima, H.; Hibino, Y. Effect of Sandblasting and/or Priming Treatment on the Shear Bond Strength of Self-Adhesive Resin Cement to CAD/CAM Blocks. Odontology 2022, 110, 70–80. [Google Scholar] [CrossRef]
- Çelik, E.; Sahin, S.C.; Dede, D.Ö. Shear Bond Strength of Nanohybrid Composite to the Resin Matrix Ceramics after Different Surface Treatments. Photomed. Laser Surg. 2018, 36, 424–430. [Google Scholar] [CrossRef]
- Cekic-Nagas, I.; Ergun, G.; Egilmez, F.; Vallittu, P.K.; Lassila, L.V.J. Micro-Shear Bond Strength of Different Resin Cements to Ceramic/Glass-Polymer CAD-CAM Block Materials. J. Prosthodont. Res. 2016, 60, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Castro, E.F.; Azevedo, V.L.B.; Nima, G.; de Andrade, O.S.; Dias, C.T.S.; Giannini, M. Adhesion, Mechanical Properties, and Microstructure of Resin-Matrix CAD-CAM Ceramics. J. Adhes. Dent. 2020, 22, 421–431. [Google Scholar] [CrossRef]
- Secilmis, A.; Ustun, O.; Kecik Buyukhatipoglu, I. Evaluation of the Shear Bond Strength of Two Resin Cements on Different CAD/CAM Materials. J. Adhes. Sci. Technol. 2016, 30, 983–993. [Google Scholar] [CrossRef]
- Barutcigil, K.; Barutcigil, Ç.; Kul, E.; Özarslan, M.M.; Buyukkaplan, U.S. Effect of Different Surface Treatments on Bond Strength of Resin Cement to a CAD/CAM Restorative Material. J. Prosthodont. 2019, 28, 71–78. [Google Scholar] [CrossRef]
- Mine, A.; Kabetani, T.; Kawaguchi-Uemura, A.; Higashi, M.; Tajiri, Y.; Hagino, R.; Imai, D.; Yumitate, M.; Ban, S.; Matsumoto, M.; et al. Effectiveness of Current Adhesive Systems When Bonding to CAD/CAM Indirect Resin Materials: A Review of 32 Publications. Jpn. Dent. Sci. Rev. 2019, 55, 41–50. [Google Scholar] [CrossRef]
- Papathanasiou, I.; Kamposiora, P.; Dimitriadis, K.; Papavasiliou, G.; Zinelis, S. In Vitro Evaluation of CAD/CAM Composite Materials. J. Dent. 2023, 136, 104623. [Google Scholar] [CrossRef]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D Printing in Dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
- Alharbi, N.; Wismeijer, D.; Osman, R.B. Additive Manufacturing Techniques in Prosthodontics: Where Do We Currently Stand? A Critical Review. Int. J. Prosthodont. 2017, 30, 474–484. [Google Scholar] [CrossRef]
- Jockusch, J.; Özcan, M. Additive Manufacturing of Dental Polymers: An Overview on Processes, Materials and Applications. Dent. Mater. J. 2020, 39, 345–354. [Google Scholar] [CrossRef]
- Grzebieluch, W.; Kowalewski, P.; Grygier, D.; Rutkowska-Gorczyca, M.; Kozakiewicz, M.; Jurczyszyn, K. Printable and Machinable Dental Restorative Composites for Cad/Cam Application—Comparison of Mechanical Properties, Fractographic, Texture and Fractal Dimension Analysis. Materials 2021, 14, 4919. [Google Scholar] [CrossRef]
- Lim, N.K.; Shin, S.Y. Bonding of Conventional Provisional Resin to 3D Printed Resin: The Role of Surface Treatments and Type of Repair Resins. J. Adv. Prosthodont. 2020, 12, 322–328. [Google Scholar] [CrossRef]
- Tahayeri, A.; Morgan, M.C.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D Printed versus Conventionally Cured Provisional Crown and Bridge Dental Materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef]
- Lankes, V.; Reymus, M.; Liebermann, A.; Stawarczyk, B. Bond Strength between Temporary 3D Printable Resin and Conventional Resin Composite: Influence of Cleaning Methods and Air-Abrasion Parameters. Clin. Oral Investig. 2023, 27, 31–43. [Google Scholar] [CrossRef]
- Schweiger, J.; Edelhoff, D.; Güth, J.F. 3d Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef]
- Çakmak, G.; Oosterveen-Rüegsegger, A.L.; Akay, C.; Schimmel, M.; Yilmaz, B.; Donmez, M.B. Influence of Polishing Technique and Coffee Thermal Cycling on the Surface Roughness and Color Stability of Additively and Subtractively Manufactured Resins Used for Definitive Restorations. J. Prosthodont. 2024, 33, 467–474. [Google Scholar] [CrossRef]
- Demirel, M.; Diken Türksayar, A.A.; Donmez, M.B. Fabrication Trueness and Internal Fit of Hybrid Abutment Crowns Fabricated by Using Additively and Subtractively Manufactured Resins. J. Dent. 2023, 136, 104621. [Google Scholar] [CrossRef]
- Hitz, T.; Stawarczyk, B.; Fischer, J.; Hämmerle, C.H.F.; Sailer, I. Are Self-Adhesive Resin Cements a Valid Alternative to Conventional Resin Cements? A Laboratory Study of the Long-Term Bond Strength. Dent. Mater. 2012, 28, 1183–1190. [Google Scholar] [CrossRef]
- Bayazıt, E.Ö. Microtensile Bond Strength of Self-Adhesive Resin Cements to CAD/CAM Resin-Matrix Ceramics Prepared with Different Surface Treatments. Int. J. Prosthodont. 2019, 32, 433–438. [Google Scholar] [CrossRef]
- Tekçe, N.; Tuncer, S.; Demirci, M. The Effect of Sandblasting Duration on the Bond Durability of Dual-Cure Adhesive Cement to CAD/CAM Resin Restoratives. J. Adv. Prosthodont. 2018, 10, 211–217. [Google Scholar] [CrossRef]
- Malament, K.A.; Socransky, S.S. Survival of Dicor Glass-Ceramic Dental Restorations over 16 Years. Part III: Effect of Luting Agent and Tooth or Tooth-Substitute Core Structure. J. Prosthet. Dent. 2001, 86, 511–519. [Google Scholar] [CrossRef]
- Fehrenbach, J.; Münchow, E.A.; Isolan, C.P.; Brondani, L.P.; Bergoli, C.D. Structural Reliability and Bonding Performance of Resin Luting Agents to Dentin and Enamel. Int. J. Adhes. Adhes. 2021, 107, 102863. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; Peumans, M.; Poitevin, A.; Mine, A.; Van Ende, A.; Neves, A.; De Munck, J. Relationship between Bond-Strength Tests and Clinical Outcomes. Dent. Mater. 2010, 26, e100–e121. [Google Scholar] [CrossRef]
- Manso, A.P.; Carvalho, R.M. Dental Cements for Luting and Bonding Restorations: Self-Adhesive Resin Cements. Dent. Clin. N. Am. 2017, 61, 821–834. [Google Scholar] [CrossRef]
- Mair, L.; Padipatvuthikul, P. Variables Related to Materials and Preparing for Bond Strength Testing Irrespective of the Test Protocol. Dent. Mater. 2010, 26, e17–e23. [Google Scholar] [CrossRef]
- Sresthadatta, P.; Sriamporn, T.; Klaisiri, A.; Thamrongananskul, N. Effect of Surface Treatments on Shear Bond Strength of Resin Cement to Hybrid Ceramic Materials. J. Int. Dent. Med. Res. 2021, 14, 125–135. [Google Scholar]
- Quinn, J.B.; Quinn, G.D. A Practical and Systematic Review of Weibull Statistics for Reporting Strengths of Dental Materials. Dent. Mater. 2010, 26, 135–147. [Google Scholar] [CrossRef]
- Scherrer, S.S.; Cesar, P.F.; Swain, M.V. Direct Comparison of the Bond Strength Results of the Different Test Methods: A Critical Literature Review. Dent. Mater. 2010, 26, e78–e93. [Google Scholar] [CrossRef]
- Beyabanaki, E.; Ashtiani, R.E.; Moradi, M.; Namdari, M.; Mostafavi, D.; Zandinejad, A. Biaxial Flexural Strength and Weibull Characteristics of a Resin Ceramic Material after Thermal-Cycling. J. Prosthodont. 2023, 32, 721–727. [Google Scholar] [CrossRef]
- Holmer, L.; Othman, A.; Lührs, A.K.; von See, C. Comparison of the Shear Bond Strength of 3D Printed Temporary Bridges Materials, on Different Types of Resin Cements and Surface Treatment. J. Clin. Exp. Dent. 2019, 11, e367–e372. [Google Scholar] [CrossRef]
- Elsaka, S.E. Bond Strength of Novel CAD/CAM Restorative Materials to Self-Adhesive Resin Cement: The Effect of Surface Treatments. J. Adhes. Dent. 2014, 16, 531–540. [Google Scholar] [CrossRef]
- Günal-Abduljalil, B.; Önöral, Ö.; Ongun, S. Micro-Shear Bond Strengths of Resin-Matrix Ceramics Subjected to Different Surface Conditioning Strategies with or without Coupling Agent Application. J. Adv. Prosthodont. 2021, 13, 180–190. [Google Scholar] [CrossRef]
- Şişmanoğlu, S.; Turunç-oğuzman, R. Microshear Bond Strength of Contemporary Self- Adhesive Resin Cements to CAD/CAM Restorative Materials: Effect of Surface Treatment and Aging. J. Adhes. Sci. Technol. 2020, 34, 2484–2498. [Google Scholar] [CrossRef]
- Yoshihara, K.; Nagaoka, N.; Maruo, Y.; Nishigawa, G.; Irie, M.; Yoshida, Y.; Van Meerbeek, B. Sandblasting May Damage the Surface of Composite CAD—CAM Blocks. Dent. Mater. 2017, 33, e124–e135. [Google Scholar] [CrossRef]
- Reymus, M.; Roos, M.; Eichberger, M.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Bonding to New CAD/CAM Resin Composites: Influence of Air Abrasion and Conditioning Agents as Pretreatment Strategy. Clin. Oral Investig. 2019, 23, 529–538. [Google Scholar] [CrossRef]
- Zattera, A.C.A.; Morganti, F.A.; de Souza Balbinot, G.; Della Bona, A.; Collares, F.M. The Influence of Filler Load in 3D Printing Resin-Based Composites. Dent. Mater. 2024, 40, 1041–1046. [Google Scholar] [CrossRef]
- Katheng, A.; Kanazawa, M.; Iwaki, M.; Minakuchi, S. Evaluation of Dimensional Accuracy and Degree of Polymerization of Stereolithography Photopolymer Resin under Different Postpolymerization Conditions: An in Vitro Study. J. Prosthet. Dent. 2021, 125, 695–702. [Google Scholar] [CrossRef]
- Tekçe, N.; Tuncer, S.; Demirci, M.; Kara, D.; Baydemir, C. Microtensile Bond Strength of CAD/CAM Resin Blocks to Dual-Cure Adhesive Cement: The Effect of Different sandblasting procedures. J. Prosthodont. 2019, 28, e485–e490. [Google Scholar] [CrossRef]
- Yano, H.T.; Ikeda, H.; Nagamatsu, Y.; Masaki, C.; Hosokawa, R.; Shimizu, H. Correlation between Microstructure of CAD/CAM Composites and the Silanization Effect on Adhesive Bonding. J. Mech. Behav. Biomed. Mater. 2020, 101, 103441. [Google Scholar] [CrossRef]
- Murillo-gomez, F.; Wanderley, R.B.; De Goes, M.F. Impact of Silane-Containing Universal Adhesive on the Biaxial Flexural Strength of a Resin Cement/Glass-Ceramic System. Oper. Dent. 2019, 44, 200–209. [Google Scholar] [CrossRef]
- Braga, R.R.; Meira, J.B.C.; Boaro, L.C.C.; Xavier, T.A. Adhesion to Tooth Structure: A Critical Review of “Macro” Test Methods. Dent. Mater. 2010, 26, e38–e49. [Google Scholar] [CrossRef]
- Mostafavi, D.M.; Methani, M.M.; Piedra-Cascon, W.; Zandinejad, A.; Att, W.; Revilla-León, M. Influence of the Polymerization Postprocessing Procedures on the Accuracy of Additively Manufactured Dental Model Material. Int. J. Prosthodont. 2023, 36, 479–485. [Google Scholar] [CrossRef]
- Kim, M.J.; Kim, Y.K.; Kim, K.H.; Kwon, T.Y. Shear Bond Strengths of Various Luting Cements to Zirconia Ceramic: Surface Chemical Aspects. J. Dent. 2011, 39, 795–803. [Google Scholar] [CrossRef]
- Lüthy, H.; Loeffel, O.; Hammerle, C.H.F. Effect of Thermocycling on Bond Strength of Luting Cements to Zirconia Ceramic. Dent. Mater. 2006, 22, 195–200. [Google Scholar] [CrossRef]
- Barbon, F.J.; Moraes, R.R.; Isolan, C.P.; Spazzin, A.O.; Boscato, N. Influence of Inorganic Filler Content of Resin Luting Agents and Use of Adhesive on the Performance of Bonded Ceramic. J. Prosthet. Dent. 2019, 122, 566.e1–566.e11. [Google Scholar] [CrossRef]
- Chen, Y.; Yao, C.; Huang, C.; Wang, Y. The Effect of Monowave and Polywave Light-Polymerization Units on the Adhesion of Resin Cements to Zirconia. J. Prosthet. Dent. 2019, 121, 549.e1–549.e7. [Google Scholar] [CrossRef]

| Material | Manufacturer | Composition | Lot Number | |
|---|---|---|---|---|
| Machinable Blocks | (CS) Cerasmart 270 | GC Dental Products, Leuven, Belgium | Organic part: Bis-MEPP, UDMA, DMA Inorganic part: 71 wt% silica (0.02 μm) and barium glass (0.3 μm) nanoparticles | 2102176 |
| (VE) VITA Enamic | VITA Zahnfabrik, Bad Säckingen, Germany | Organic part: UDMA, TEGDMA Inorganic part: 86 wt% glass ceramic (SiO2, Al2O3, Na2O, K2O, and other oxides) | 73340 | |
| Printable Resin | (3D-PR) VarseoSmile Crown Plus is distributed by Formlabs as Permanent Crown | Bego, Bremen, Germany | 4′-isopropylidiphenol, ethoxylated and 2-methylprop-2enoic acid. Silanized dental glass, methyl benzoylformate, diphenyl (2,4,6-trimethylbenzoyl) phosphine oxide, 30–50 wt% inorganic fillers (particle size 0.7 μm) | 600163 |
| Self-adhesive luting composite | (SLC) RelyX™ U200 | 3M ESPE, St. Paul, MN, USA | Base paste: Silane-treated glass filler, 2-propenoic acid, 2-methyl 1,1′-[1-(hydroxymethyl)-1,2-ethanediyl] ester, triethylene dimethacrylate, sodium persulfate andper−3,5,5-trimethylhexanoate t-butyl. Catalyst paste: Silanated filler, dimethacrylate, silane-treated filler, sodium p-toluenesulfonate,1-benzyl-5-phenyl-baric acid, calcium salts, 1,12-dodecane dimethacrylate, calcium hydroxide and titanium dioxide (~70 wt% filler) | 7784355 |
| Material | N | Mean ± SD (MPa) | 95% CI | p |
|---|---|---|---|---|
| 3D-PR (Permanent Crown) | 12 | 9.74 ± 2.88 | [7.91; 11.58] | |
| VE (VITA Enamic) | 12 | 12.03 ± 2.11 | [10.68; 13.37] | 0.129 |
| CS (Cerasmart 270) | 12 | 11.02 ± 2.96 | [9.13; 12.90] |
| Adhesive n (%) | Mixed n (%) | Cohesive-Material n (%) | Cohesive-Luting Composite n (%) | p | |
|---|---|---|---|---|---|
| 3D-PR (Permanent Crown) | 0 (0) | 7 (58.3) | 2 (16.7) | 3 (25) | 0.986 |
| VE (VITA Enamic) | 0 (0) | 8 (66.7) | 2 (16.7) | 2 (16.7) | |
| CS (Cerasmart 270) | 0 (0) | 7 (58.3) | 2 (16.7) | 3 (25) |
| Failure Mode | Mean ± SD (n) | p |
|---|---|---|
| Adhesive | - (0) | |
| Cohesive-Material | 11.1 ± 3 (6) | 0.033 |
| Cohesive-luting composite | 8.9 ± 1.6 (8) | |
| Mixed | 11.6 ± 2.7 (22) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aydin, N.; Celik Oge, S.; Guney, O.; Okbaz, O.; Sertdemir, Y. A Comparison of the Shear Bond Strength between a Luting Composite Resin and Both Machinable and Printable Ceramic–Glass Polymer Materials. Materials 2024, 17, 4697. https://doi.org/10.3390/ma17194697
Aydin N, Celik Oge S, Guney O, Okbaz O, Sertdemir Y. A Comparison of the Shear Bond Strength between a Luting Composite Resin and Both Machinable and Printable Ceramic–Glass Polymer Materials. Materials. 2024; 17(19):4697. https://doi.org/10.3390/ma17194697
Chicago/Turabian StyleAydin, Nazli, Selin Celik Oge, Ogulcan Guney, Onur Okbaz, and Yasar Sertdemir. 2024. "A Comparison of the Shear Bond Strength between a Luting Composite Resin and Both Machinable and Printable Ceramic–Glass Polymer Materials" Materials 17, no. 19: 4697. https://doi.org/10.3390/ma17194697
APA StyleAydin, N., Celik Oge, S., Guney, O., Okbaz, O., & Sertdemir, Y. (2024). A Comparison of the Shear Bond Strength between a Luting Composite Resin and Both Machinable and Printable Ceramic–Glass Polymer Materials. Materials, 17(19), 4697. https://doi.org/10.3390/ma17194697







