Design and Material Characterization of an Inflatable Vaginal Dilator
Abstract
:1. Introduction
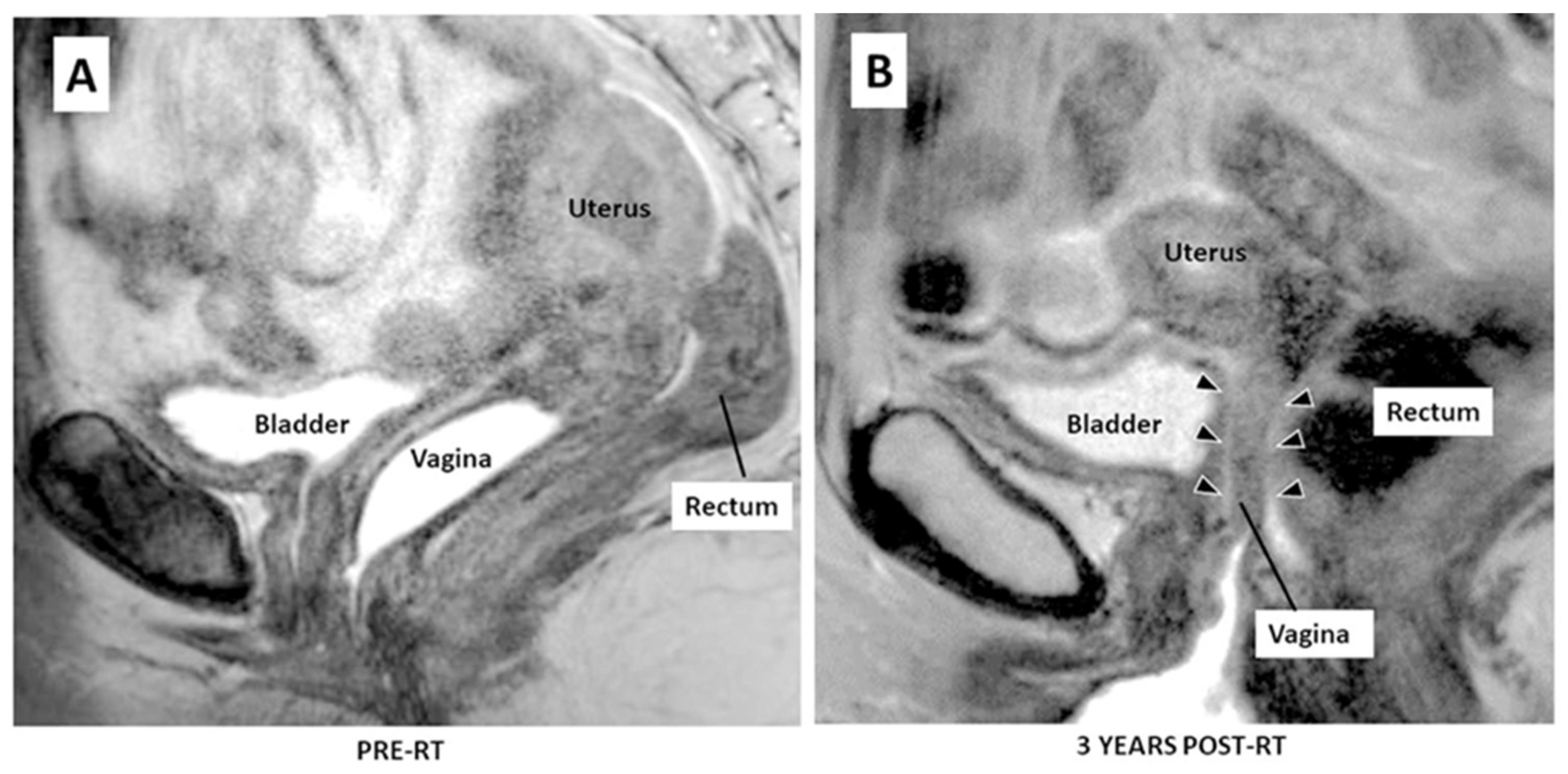
1.1. Medical Background
1.2. Current Standard of Care for VS
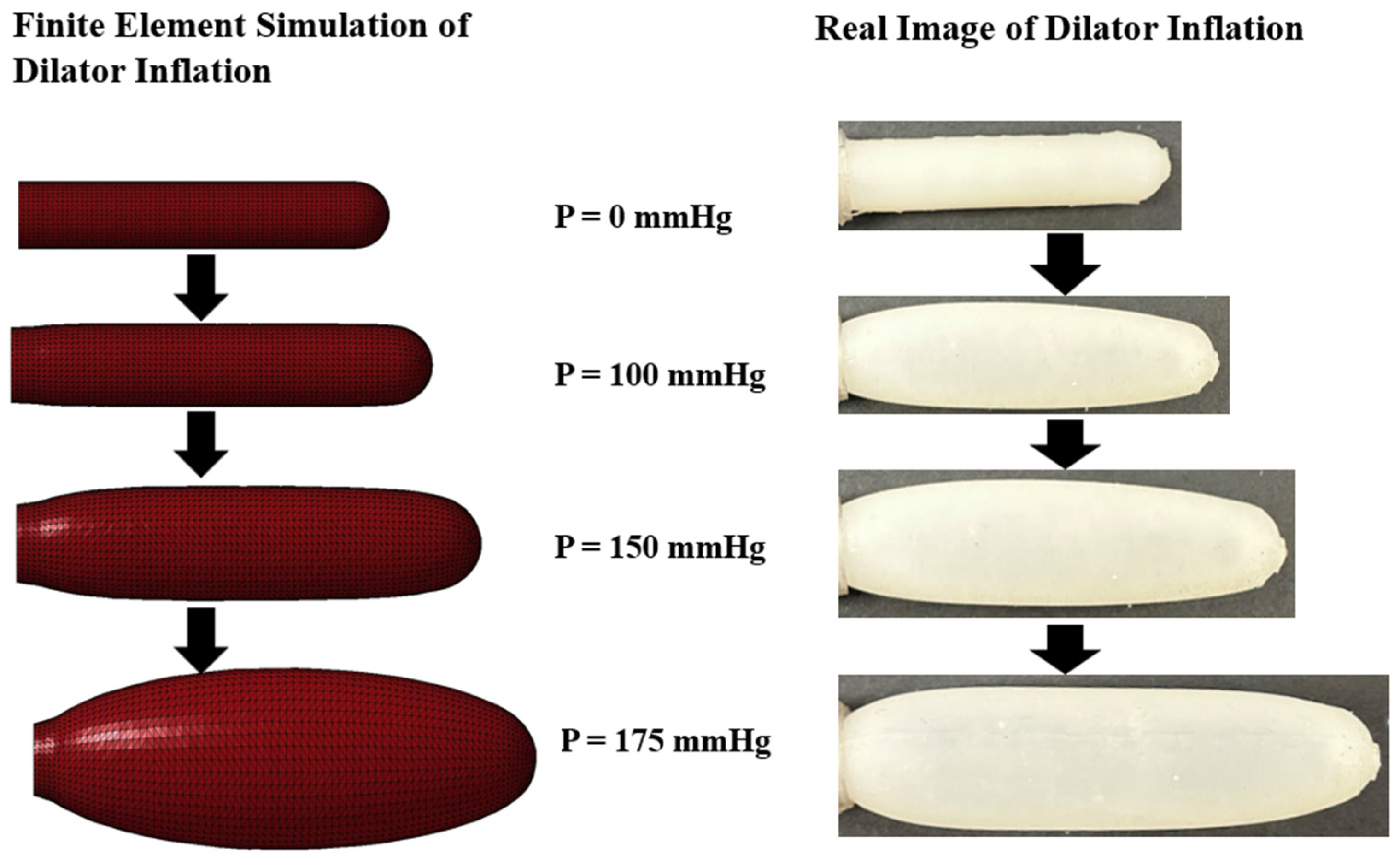
1.3. An Alternative Approach
1.4. Inflatable Vaginal Dilator Material
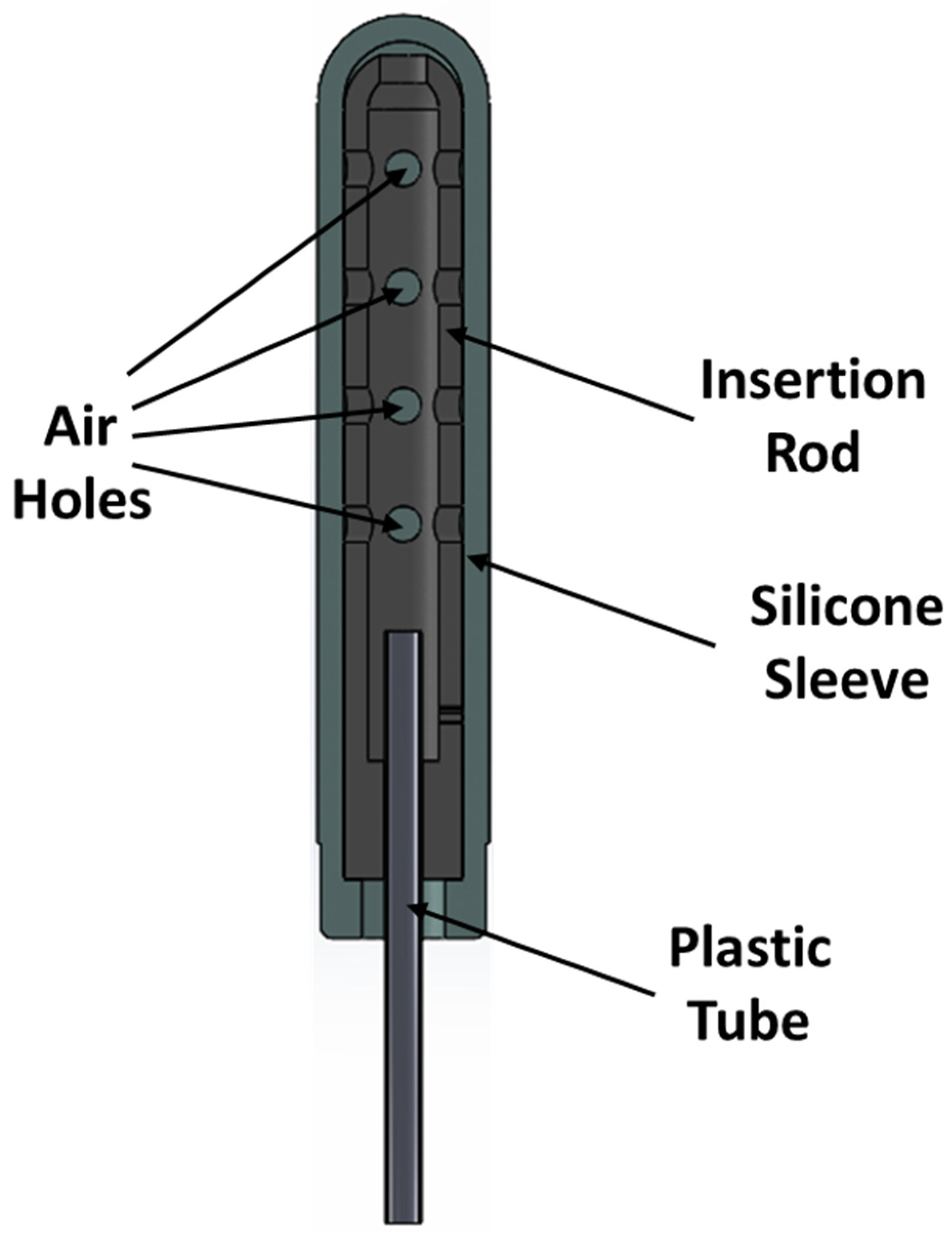
2. Design and Manufacturing of an Inflatable Dilator
3. Material Characterization
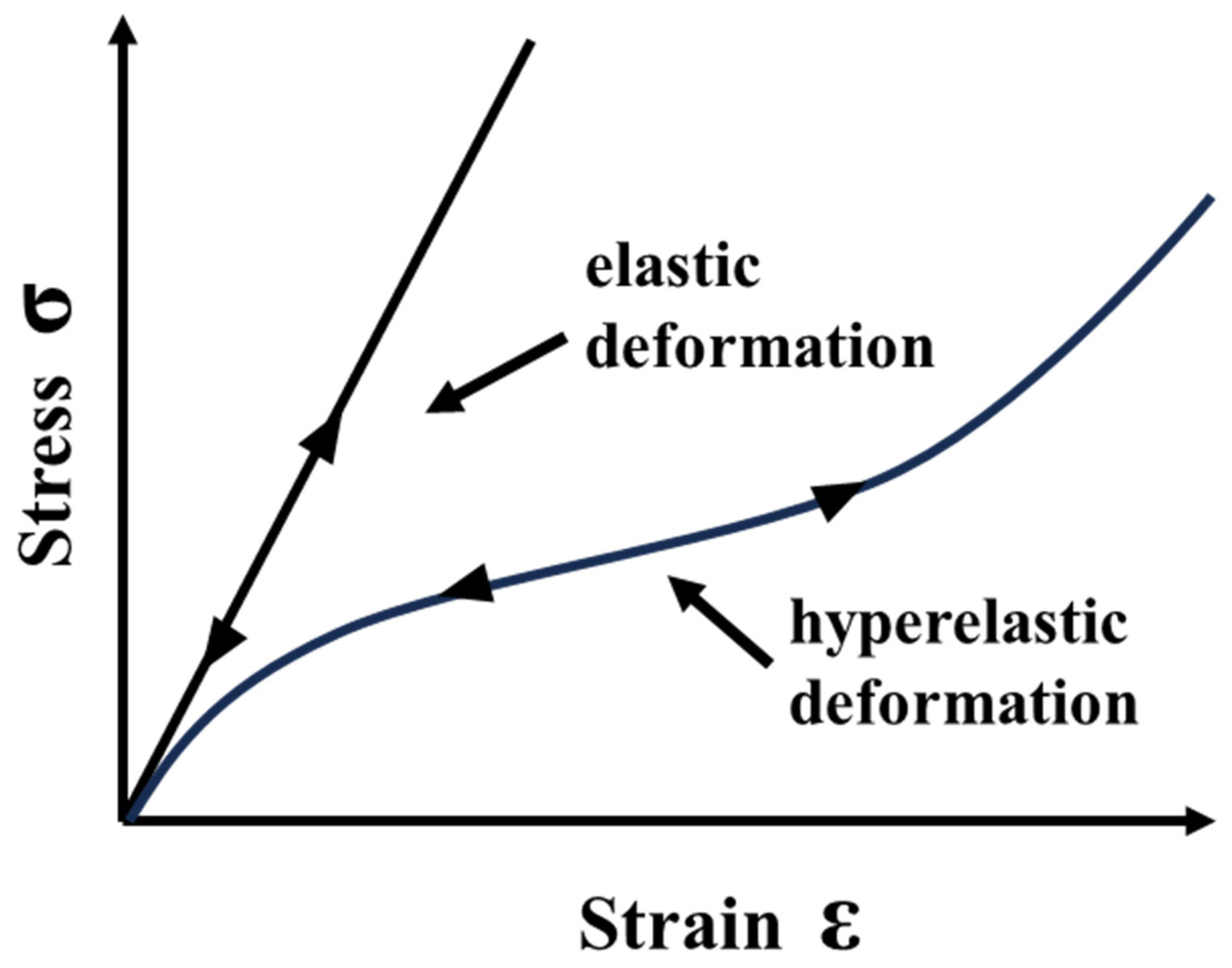
3.1. Silicone and Hyperelasticity
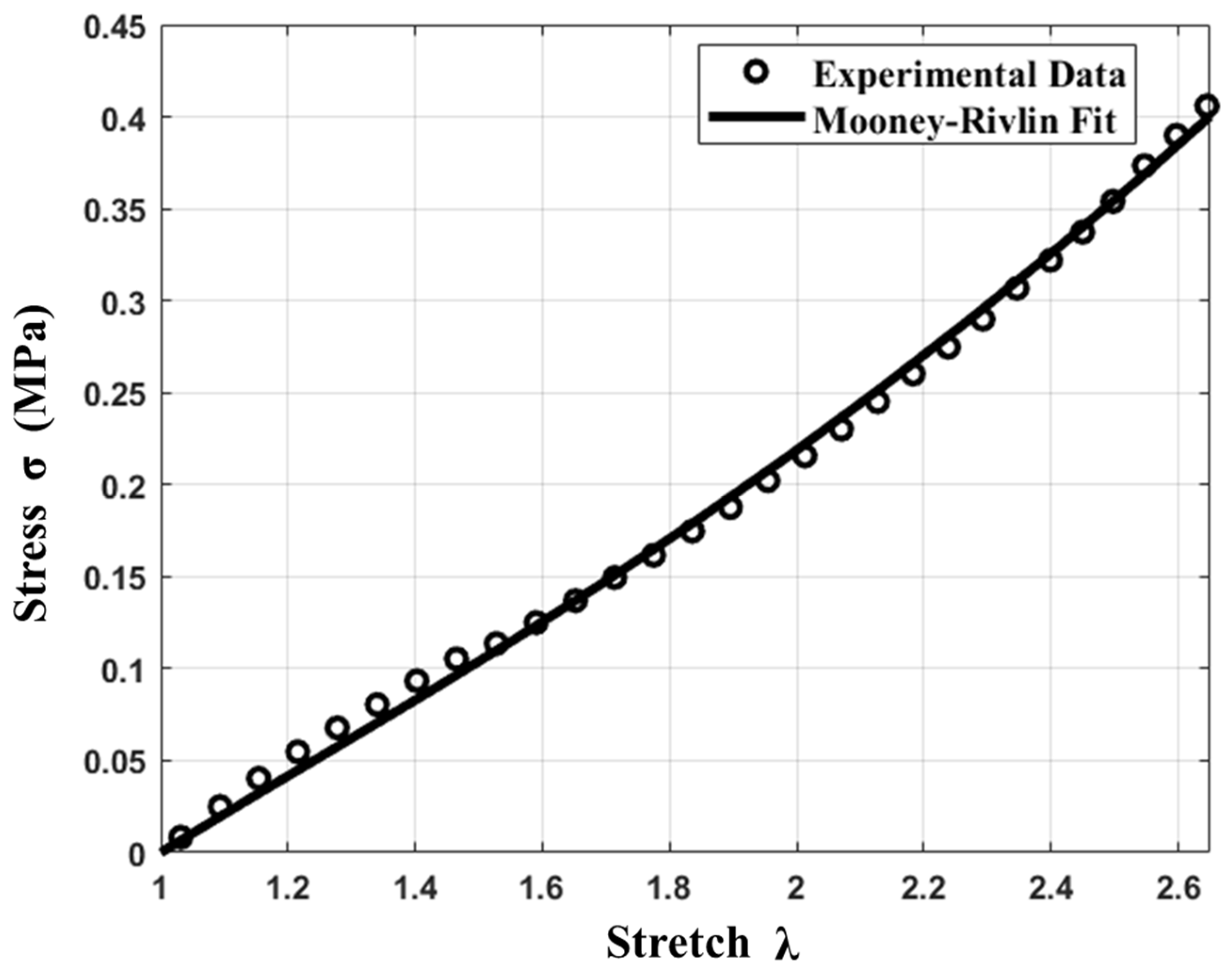
3.2. Mooney–Rivlin Material Model
3.3. Material Testing and Modeling
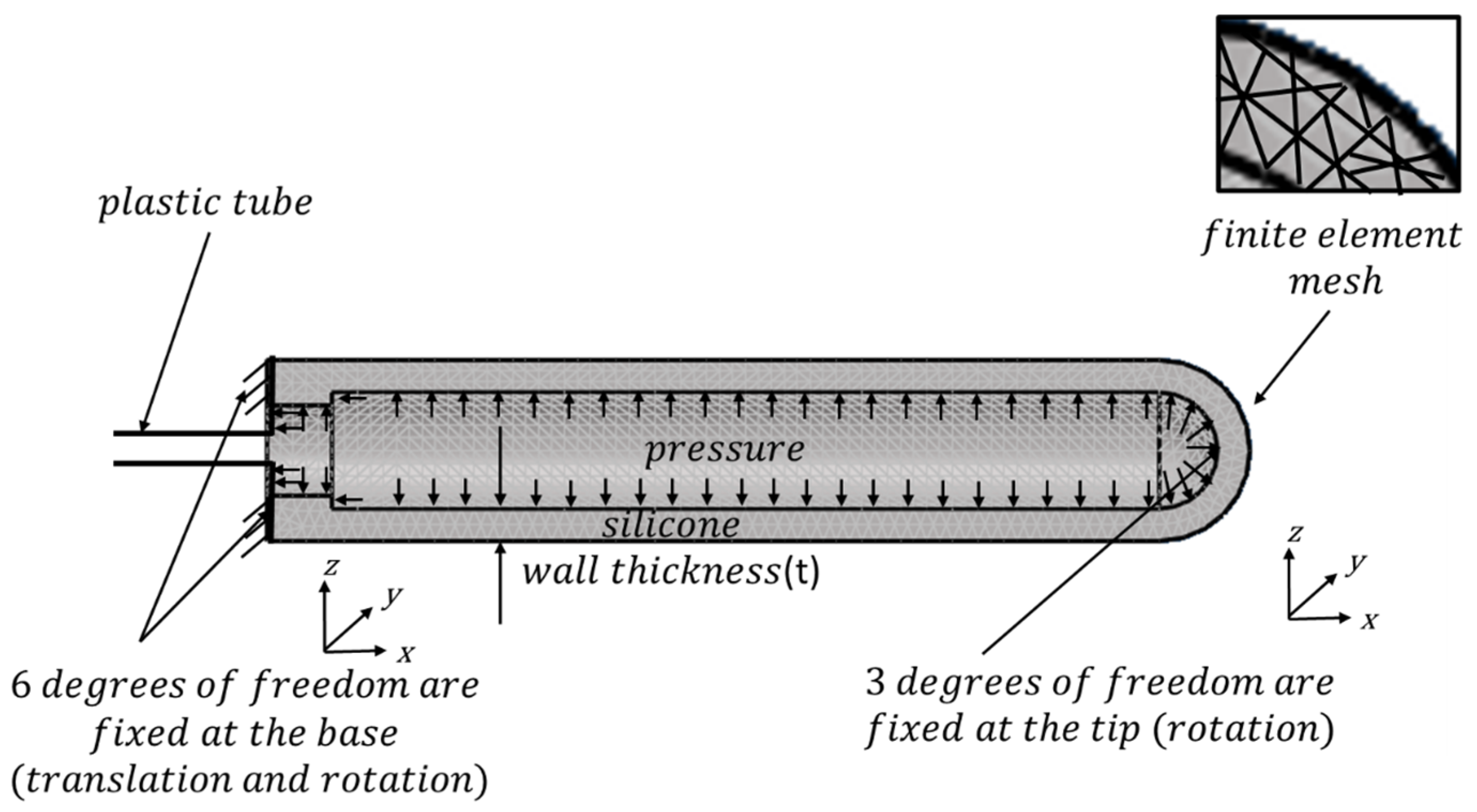
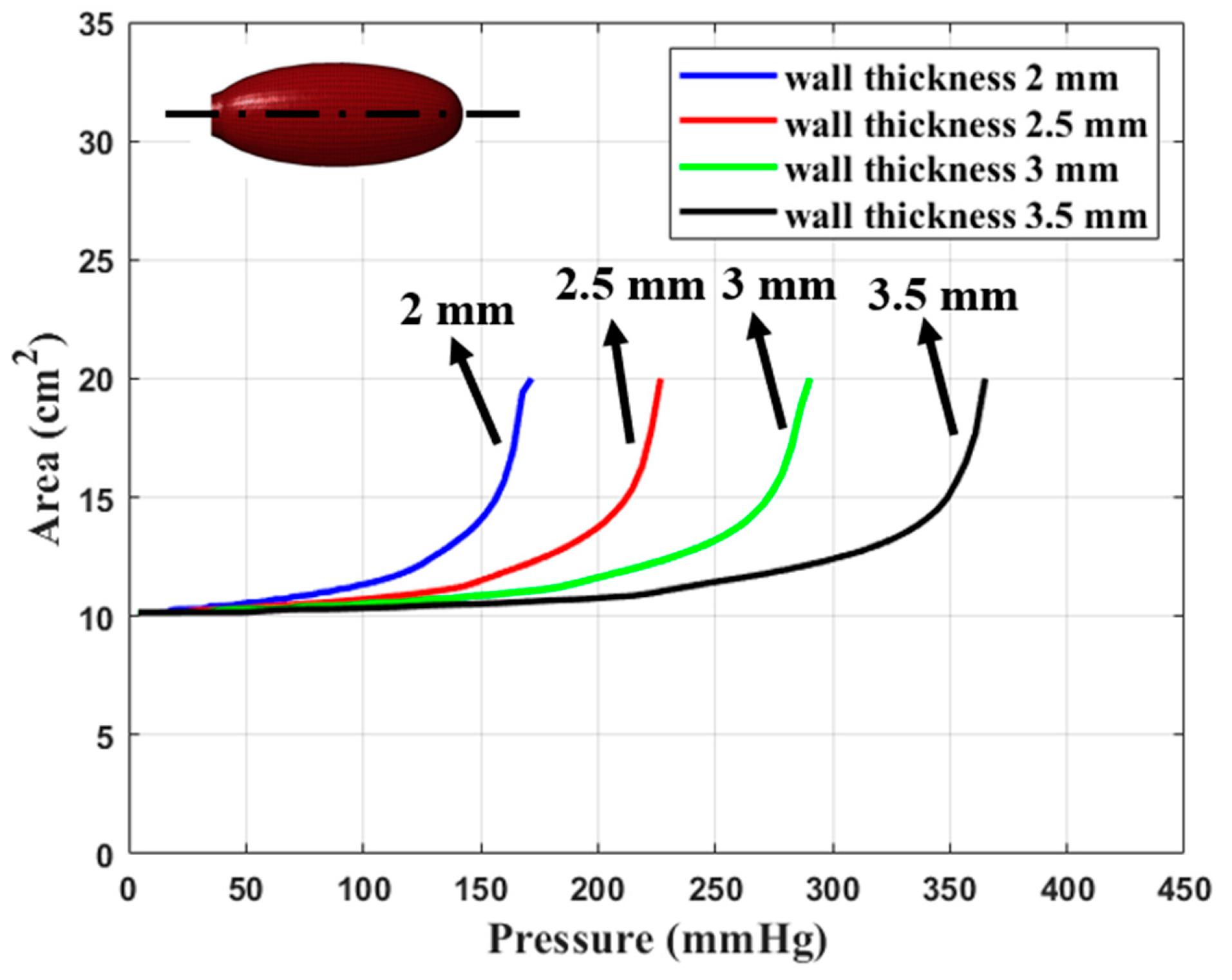
4. Finite Element Modeling
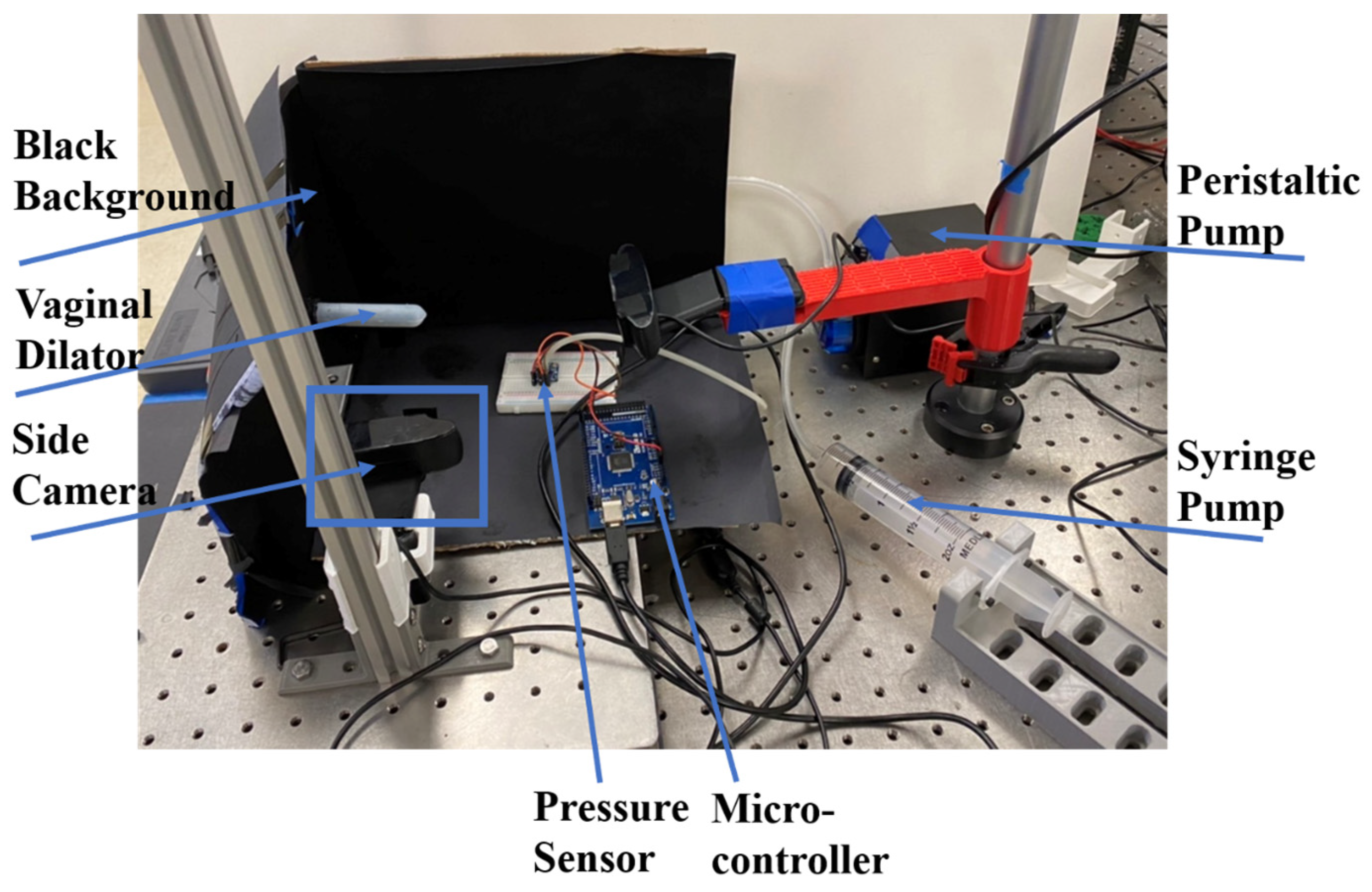
5. Experimental Verification and Comparison
6. Summary and Discussion
7. Conclusions
- Silicone polymers are a good material choice for use in an inflatable dilator to treat vaginal stenosis, as they are soft and reversibly deformable. The stress–stretch characteristics of a typical commercially available silicone can be described using the Mooney–Rivlin model. Large variations in material properties and Mooney–Rivlin parameters are expected depending on the manufacturing process.
- Material properties and topology optimization of design parameters such as wall thicknesses are crucial for obtaining a well-tolerated and functional device. Reliability and manufacturability tests need to be performed to study the failure characteristics of the device.
- Further refinements to optimally translate the dilator design into the clinic are needed, guided by close collaboration with medical professionals and, at later developmental stages, via patient feedback.
- Medical devices such as inflatable dilators clearly have the potential to improve the lives of cervical cancer patients in multiple important ways.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention and National Cancer Institute. United States Cancer Statistics: Data Visualizations. Available online: https://gis.cdc.gov/Cancer/USCS/#/AtAGlance/ (accessed on 9 February 2024).
- National Cancer Institute. Cervical Cancer Prognosis and Survival Rates. Available online: https://www.cancer.gov/types/cervical/survival (accessed on 14 April 2022).
- Tornero-López, A.M.; Guirado, D. Radiobiological Considerations in Combining Doses from External Beam Radiotherapy and Brachytherapy for Cervical Cancer. Rep. Pract. Oncol. Radiother. 2018, 23, 562–573. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.A.; Jhingran, A.; Oaknin, A.; Denny, L. Cervical Cancer. Lancet 2019, 393, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Waggoner, S.E. Cervical Cancer. Lancet 2003, 361, 2217–2225. [Google Scholar] [CrossRef] [PubMed]
- Varytė, G.; Bartkevičienė, D. Pelvic Radiation Therapy Induced Vaginal Stenosis: A Review of Current Modalities and Recent Treatment Advances. Medicina 2021, 57, 336. [Google Scholar] [CrossRef]
- Morris, L.; Do, V.; Chard, J.; Brand, A. Radiation-Induced Vaginal Stenosis: Current Perspectives. Int. J. Womens Health 2017, 9, 273–279. [Google Scholar] [CrossRef]
- Kirchheiner, K.; Fidarova, E.; Nout, R.A.; Schmid, M.P.; Sturdza, A.; Wiebe, E.; Kranz, A.; Polterauer, S.; Pötter, R.; Dörr, W. Radiation-Induced Morphological Changes in the Vagina. Strahlenther. Onkol. 2012, 188, 1010–1019. [Google Scholar] [CrossRef]
- Grigsby, P.W.; Russell, A.; Bruner, D.; Eifel, P.; Koh, W.-J.; Spanos, W.; Stetz, J.; Stitt, J.A.; Sullivan, J. Late Injury of Cancer Therapy on the Female Reproductive Tract. Int. J. Radiat. Oncol. 1995, 31, 1281–1299. [Google Scholar] [CrossRef]
- Fajardo, L.F. The Pathology of Ionizing Radiation as Defined by Morphologic Patterns. Acta Oncol. 2005, 44, 13–22. [Google Scholar] [CrossRef]
- Yoshida, K.; Yamazaki, H.; Nakamura, S.; Masui, K.; Kotsuma, T.; Akiyama, H.; Tanaka, E.; Yoshikawa, N.; Uesugi, Y.; Shimbo, T.; et al. Role of Vaginal Pallor Reaction in Predicting Late Vaginal Stenosis after High-Dose-Rate Brachytherapy in Treatment-Naive Patients with Cervical Cancer. J. Gynecol. Oncol. 2015, 26, 179. [Google Scholar] [CrossRef]
- Mirabeau-Beale, K.; Hong, T.S.; Niemierko, A.; Ancukiewicz, M.; Blaszkowsky, L.S.; Crowley, E.M.; Cusack, J.C.; Drapek, L.C.; Kovalchuk, N.; Markowski, M.; et al. Clinical and Treatment Factors Associated with Vaginal Stenosis after Definitive Chemoradiation for Anal Canal Cancer. Pract. Radiat. Oncol. 2015, 5, e113–e118. [Google Scholar] [CrossRef]
- Simoes-Torigoe, R.; Chen, P.-H.; Li, Y.M.; Kohanfars, M.; Morris, K.; Williamson, C.W.; Makale, M.; Mayadev, J.; Talke, F. Design and Validation of an Automated Dilator Prototype for the Treatment of Radiation Induced Vaginal Injury. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), IEEE, Mexico, 1–5 November 2021; pp. 1562–1565. [Google Scholar]
- Damast, S.; Jeffery, D.D.; Son, C.H.; Hasan, Y.; Carter, J.; Lindau, S.T.; Jhingran, A. Literature Review of Vaginal Stenosis and Dilator Use in Radiation Oncology. Pract. Radiat. Oncol. 2019, 9, 479–491. [Google Scholar] [CrossRef]
- Brand, A.H.; Bull, C.A.; Cakir, B. Vaginal Stenosis in Patients Treated with Radiotherapy for Carcinoma of the Cervix. Int. J. Gynecol. Cancer 2006, 16, 288–293. [Google Scholar] [CrossRef]
- Jensen, P.T.; Groenvold, M.; Klee, M.C.; Thranov, I.; Petersen, M.A.; Machin, D. Longitudinal Study of Sexual Function and Vaginal Changes after Radiotherapy for Cervical Cancer. Int. J. Radiat. Oncol. 2003, 56, 937–949. [Google Scholar] [CrossRef] [PubMed]
- Denton, A.S.; Maher, J. Interventions for the Physical Aspects of Sexual Dysfunction in Women Following Pelvic Radiotherapy. Cochrane Database Syst. Rev. 2003, 2015, CD003750. [Google Scholar] [CrossRef] [PubMed]
- Miles, K.; Miles, S. Low Dose, High Frequency Movement Based Dilator Therapy for Dyspareunia: Retrospective Analysis of 26 Cases. Sex. Med. 2021, 9, 100344. [Google Scholar] [CrossRef]
- Macey, K.; Gregory, A.; Nunns, D.; das Nair, R. Women’s Experiences of Using Vaginal Trainers (Dilators) to Treat Vaginal Penetration Difficulties Diagnosed as Vaginismus: A Qualitative Interview Study. BMC Womens Health 2015, 15, 49. [Google Scholar] [CrossRef]
- Law, E.; Kelvin, J.F.; Thom, B.; Riedel, E.; Tom, A.; Carter, J.; Alektiar, K.M.; Goodman, K.A. Prospective Study of Vaginal Dilator Use Adherence and Efficacy Following Radiotherapy. Radiother. Oncol. 2015, 116, 149–155. [Google Scholar] [CrossRef]
- Friedman, L.C.; Abdallah, R.; Schluchter, M.; Panneerselvam, A.; Kunos, C.A. Adherence to Vaginal Dilation Following High Dose Rate Brachytherapy for Endometrial Cancer. Int. J. Radiat. Oncol. 2011, 80, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Bakker, R.M.; Vermeer, W.M.; Creutzberg, C.L.; Mens JW, M.; Nout, R.A.; Ter Kuile, M.M. Qualitative Accounts of Patients’ Determinants of Vaginal Dilator Use after Pelvic Radiotherapy. J. Sex. Med. 2015, 12, 764–773. [Google Scholar] [CrossRef]
- Laganà, A.S.; Garzon, S.; Raffaelli, R.; Ban Frangež, H.; Lukanovič, D.; Franchi, M. Vaginal Stenosis After Cervical Cancer Treatments: Challenges for Reconstructive Surgery. J. Investig. Surg. 2021, 34, 754–755. [Google Scholar] [CrossRef]
- Pruitt, L.; Furmanski, J. Polymeric Biomaterials for Load-Bearing Medical Devices. JOM 2009, 61, 14–20. [Google Scholar] [CrossRef]
- Wu, A.K.; Blaschko, S.D.; Garcia, M.; McAninch, J.W.; Aaronson, D.S. Safer Urethral Catheters: How Study of Catheter Balloon Pressure and Force Can Guide Design: Urethral Catheter Balloon Pressure and Force. BJU Int. 2012, 109, 1110–1114. [Google Scholar] [CrossRef]
- Bhardwaj, R.; Naniwadekar, A.; Whang, W.; Mittnacht, A.J.; Palaniswamy, C.; Koruth, J.S.; Joshi, K.; Sofi, A.; Miller, M.; Choudry, S.; et al. Esophageal Deviation during Atrial Fibrillation Ablation. JACC Clin. Electrophysiol. 2018, 4, 1020–1030. [Google Scholar] [CrossRef]
- Hsiao, J.-H.; Chang, J.-Y.; Cheng, C.-M. Soft Medical Robotics: Clinical and Biomedical Applications, Challenges, and Future Directions. Adv. Robot. 2019, 33, 1099–1111. [Google Scholar] [CrossRef]
- Asfour, H.; Otridge, J.; Thomasian, R.; Larson, C.; Sarvazyan, N. Autofluorescence Properties of Balloon Polymers Used in Medical Applications. J. Biomed. Opt. 2020, 25, 106004. [Google Scholar] [CrossRef] [PubMed]
- Adamson, C.D.; Naik, B.J.; Lynch, D.J. The Vacuum Expandable Condom Mold: A Simple Vaginal Stent for McIndoe-Style Vaginoplasty. Plast. Reconstr. Surg. 2004, 113, 664–666. [Google Scholar] [CrossRef]
- Chen, P.-H. Design and Material Characterization of an Inflatable Vaginal Dilator. Masters Dissertation, University of California, San Diego, CA, USA, 2022. [Google Scholar]
- Visakh, P.M.; Thomas, S.; Chandra, A.K.; Mathew, A.P. (Eds.) Advances in Elastomers I: Blends and Interpenetrating Networks; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Studer, J. Material Q&A: Elastomer and Plastic Materials. Valve Mag, 7 February 2019. [Google Scholar]
- Ahn, J. What Is the Difference between a Hyperelastic Material and an Elastic Material in RecurDyn. Available online: https://support.functionbay.com/en/faq/single/87/difference-hyperelastic-material-elastic-material-recurdyn (accessed on 14 April 2022).
- Hyperelastic Materials. Available online: https://www.simscale.com/docs/simulation-setup/materials/hyperelastic-materials/ (accessed on 14 April 2022).
- Mooney, M. A Theory of Large Elastic Deformation. J. Appl. Phys. 1940, 11, 582–592. [Google Scholar] [CrossRef]
- Rivlin, R.S.; Saunders, D.W. Large Elastic Deformations of Isotropic Materials; Collected Papers; Rivlin, R.S., Barenblatt, G.I., Joseph, D.D., Eds.; Springer: New York, NY, USA, 1997; pp. 157–194. [Google Scholar]
- Morris, K.; Rosenkranz, A.; Seibert, H.; Ringel, L.; Diebels, S.; Talke, F.E. Uniaxial and Biaxial Testing of 3D Printed Hyperelastic Photopolymers. J. Appl. Polym. Sci. 2020, 137, 48400. [Google Scholar] [CrossRef]
- Lai, W.M.; Rubin, D.; Krempl, E.; Lai, W.M. Introduction to Continuum Mechanics; Butterworth-Heinemann: Oxford, UK, 1996. [Google Scholar]
- Gopesh, T.; Friend, J. Facile Analytical Extraction of the Hyperelastic Constants for the Two-Parameter Mooney–Rivlin Model from Experiments on Soft Polymers. Soft Robot. 2021, 8, 365–370. [Google Scholar] [CrossRef]
- Di Lecce, M.; Onaizah, O.; Lloyd, P.; Chandler, J.H.; Valdastri, P. Evolutionary Inverse Material Identification: Bespoke Characterization of Soft Materials Using a Metaheuristic Algorithm. Front. Robot. AI 2022, 8, 790571. [Google Scholar] [CrossRef] [PubMed]
- Marechal, L.; Balland, P.; Lindenroth, L.; Petrou, F.; Kontovounisios, C.; Bello, F. Toward a Common Framework and Database of Materials for Soft Robotics. Soft Robot 2021, 8, 284–297. [Google Scholar] [CrossRef]
- Apinsathanon, P.; Bhattarai, B.P.; Suphangul, S.; Wongsirichat, N.; Aimjirakul, N. Penetration and Tensile Strength of Various Impression Materials of Vinylsiloxanether, Polyether, and Polyvinylsiloxane Impression Materials. Eur. J. Dent. 2022, 16, 339–345. [Google Scholar] [CrossRef]
- Li, Y.M.; Chen, P.-H.; Simoes-Torigoe, R.; Scott, G.; Hu, S.; Paracuellos, R.; Morris, K.; Mayadev, J.; Makale, M.; Talke, F.E. Digital Image Based Characterization of a Silicone Composite Vaginal Tissue Analog; Toyoda Auditorium of Nagoya University: Nagoya, Japan, 2022; p. 3. [Google Scholar]
- Blaber, J.; Adair, B.; Antoniou, A. Ncorr: Open-Source 2D Digital Image Correlation Matlab Software. Exp. Mech. 2015, 55, 1105–1122. [Google Scholar] [CrossRef]
- Nežerka, V. Ncorr_post: DIC Post-Processing Tool. Available online: https://mech.fsv.cvut.cz/~nezerka/DIC/index.htm (accessed on 11 June 2022).
- Agarwalla, A.; Small, A.J.; Mendelson, A.H.; Scott, F.I.; Kochman, M.L. Risk of Recurrent or Refractory Strictures and Outcome of Endoscopic Dilation for Radiation-Induced Esophageal Strictures. Surg. Endosc. 2015, 29, 1903–1912. [Google Scholar] [CrossRef]
- Francis, D.O.; Hall, E.; Dang, J.H.; Vlacich, G.R.; Netterville, J.L.; Vaezi, M.F. Outcomes of Serial Dilation for High-grade Radiation-related Esophageal Strictures in Head and Neck Cancer Patients. Laryngoscope 2015, 125, 856–862. [Google Scholar] [CrossRef]
- Michaels, A. Cervical Dilator. U.S. Patent US4237893A, 9 December 1980. p. 6. [Google Scholar]
- Cowan, R.K. Single Balloon Device for Cervix. U.S. Patent US5947991A, 7 September 1999. p. 5. [Google Scholar]
- Ochiai, K.; Mizutani, M. Cervical Dilator. U.S. Patent US4018230A, 19 April 1977. p. 7. [Google Scholar]
- Hakim, J.; Dietrich, J.; Smith, P.; Buskmiller, C. Vaginal Stents, Vaginal Dilators, and Methods of Fabricating the Same. U.S. Patent US20180071502A1, 4 April 2016. p. 22. [Google Scholar]
- Zhang, X.S.; Chi, H.; Paulino, G.H. Adaptive Multi-Material Topology Optimization with Hyperelastic Materials under Large Deformations: A Virtual Element Approach. Comput. Methods Appl. Mech. Eng. 2020, 370, 112976. [Google Scholar] [CrossRef]
- James, K.A.; Waisman, H. Layout Design of a Bi-Stable Cardiovascular Stent Using Topology Optimization. Comput. Methods Appl. Mech. Eng. 2016, 305, 869–890. [Google Scholar] [CrossRef]
- Huang, J.; Wei, Z.; Cui, Y.; Liu, J. Clamping Force Manipulation in 2D Compliant Gripper Topology Optimization under Frictionless Contact. Struct. Multidiscip. Optim. 2023, 66, 164. [Google Scholar] [CrossRef]
- Chen, F.; Cao, J.; Zhang, H.; Wang, M.Y.; Zhu, J.; Zhang, Y.F. Programmable Deformations of Networked Inflated Dielectric Elastomer Actuators. IEEE/ASME Trans. Mechatron. 2019, 24, 45–55. [Google Scholar] [CrossRef]
- Chen, S.; Chen, F.; Cao, Z.; Wang, Y.; Miao, Y.; Gu, G.; Zhu, X. Topology Optimization of Skeleton-Reinforced Soft Pneumatic Actuators for Desired Motions. IEEE/ASME Trans. Mechatron. 2021, 26, 1745–1753. [Google Scholar] [CrossRef]
- Huang, J.; Liu, J. Derivable Skeletons in Topology Optimization for Length Scale Control. Comput. Methods Appl. Mech. Eng. 2024, 421, 116778. [Google Scholar] [CrossRef]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, P.-H.; Li, Y.M.; Morris, K.; Makale, M.T.; Mayadev, J.; Talke, F.E. Design and Material Characterization of an Inflatable Vaginal Dilator. Materials 2024, 17, 1050. https://doi.org/10.3390/ma17051050
Chen P-H, Li YM, Morris K, Makale MT, Mayadev J, Talke FE. Design and Material Characterization of an Inflatable Vaginal Dilator. Materials. 2024; 17(5):1050. https://doi.org/10.3390/ma17051050
Chicago/Turabian StyleChen, Po-Han, Yu Ming Li, Karcher Morris, Milan T. Makale, Jyoti Mayadev, and Frank E. Talke. 2024. "Design and Material Characterization of an Inflatable Vaginal Dilator" Materials 17, no. 5: 1050. https://doi.org/10.3390/ma17051050
APA StyleChen, P.-H., Li, Y. M., Morris, K., Makale, M. T., Mayadev, J., & Talke, F. E. (2024). Design and Material Characterization of an Inflatable Vaginal Dilator. Materials, 17(5), 1050. https://doi.org/10.3390/ma17051050






