Clinical Adjustment of Zirconia-Reinforced Lithium Silicate and Lithium Disilicate Restorations Should Be Performed Before Crystallization
Highlights
- Lithium silicate derivate ceramics as sensible to surface alterations.
- Roughness of lithium silicate derivate is enhanced by diamond bur abrasion.
- Lithium silicate derivate ceramics benefit from adjustment before crystallization.
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
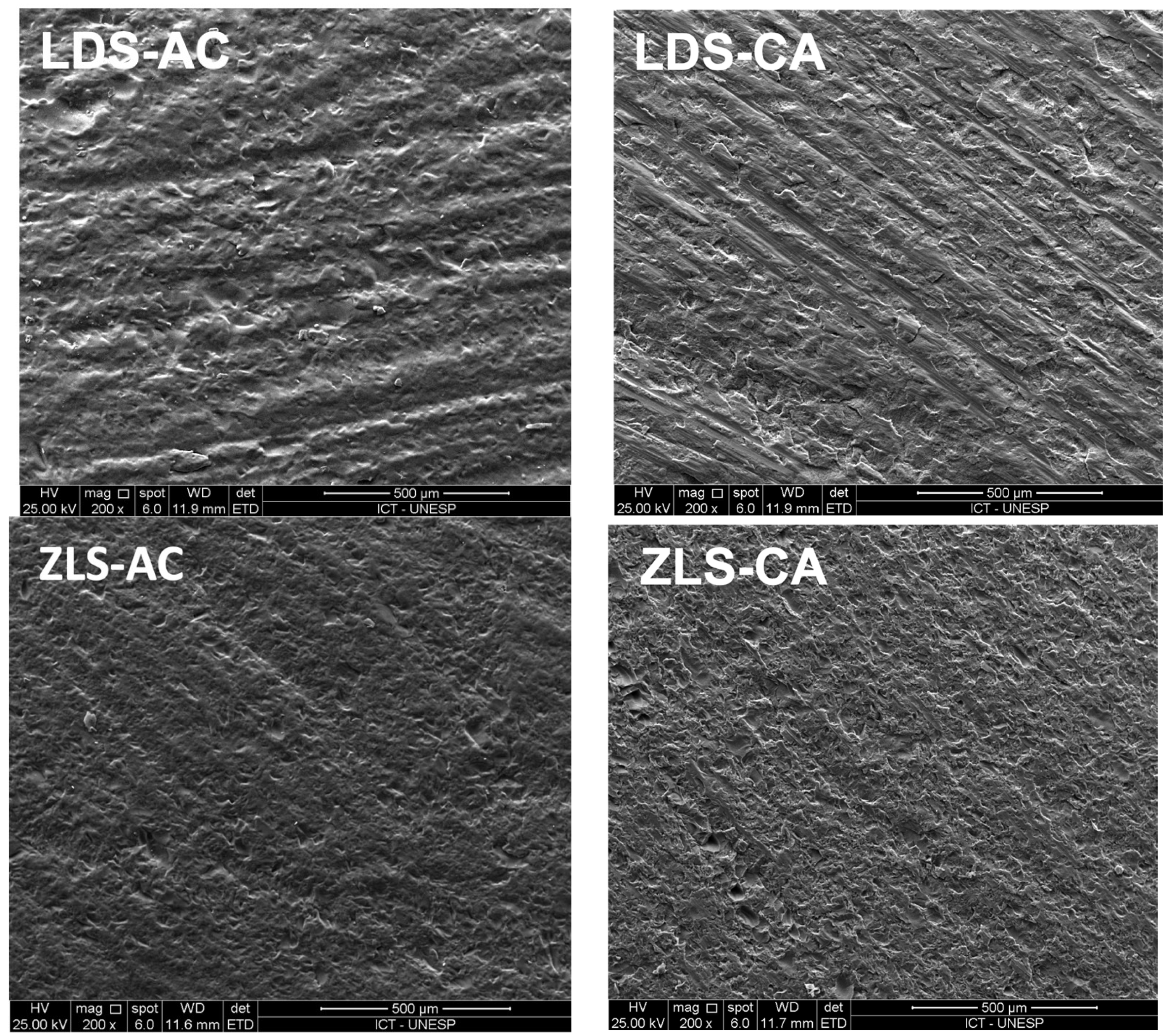
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Spitznagel, F.A.; Balmer, M.; Wiedemeier, D.B.; Jung, R.E.; Gierthmuehlen, P.C. Clinical outcomes of all-ceramic single crowns and fixed dental prostheses supported by ceramic implants: A systematic review and meta-analyses. Clin. Oral Implant. Res. 2022, 33, 1–20. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lempel, E.; Gyulai, S.; Lovász, B.V.; Jeges, S.; Szalma, J. Clinical evaluation of lithium disilicate versus indirect resin composite partial posterior restorations—A 7.8-year retrospective study. Dent. Mater. 2023, 39, 1095–1104. [Google Scholar] [CrossRef] [PubMed]
- Salem, B.O.; Elshehawi, D.M.; Elnaggar, G.A. Fracture resistance of pressed ZLS crowns versus pressed LD crowns under thermo-mechanical cycling. Braz. Dent. J. 2022, 33, 103–109. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zarone, F.; Ruggiero, G.; Leone, R.; Breschi, L.; Leuci, S.; Sorrentino, R. Zirconia-reinforced lithium silicate (ZLS) mechanical and biological properties: A literature review. J. Dent. 2021, 109, 103661. [Google Scholar] [CrossRef] [PubMed]
- Son, K.; Yu, B.Y.; Lee, J.H.; Son, Y.T.; Lee, K.B. Comparison of Intaglio Surface Adjustment in the Oral Cavity for Lithium Disilicate Crowns Fabricated Using Different Scanners. J. Prosthodont. 2021, 30, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Gorman, C.M.; de Faoite, D.; Flannery, D.; Ratajczak, M.; Kelly, T.; Stanton, K.T. Alteration of the intaglio surface of lithium disilicate glass-ceramic. J. Prosthet. Dent. 2019, 122, 411.e1–411.e10. [Google Scholar] [CrossRef] [PubMed]
- Venturini, A.B.; Bohrer, T.C.; Fontana, P.E.; Fröhlich, T.T.; May, L.G.; Valandro, L.F. Step-stress vs. staircase fatigue tests to evaluate the effect of intaglio adjustment on the fatigue behavior of simplified lithium disilicate glass-ceramic restorations. J. Mech. Behav. Biomed. Mater. 2021, 113, 104091. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.X.; Hong, D.W.; Zheng, M.; Yu, H. Is the bond strength of zirconia-reinforced lithium silicate lower than that of lithium disilicate?—A systematic review and meta-analysis. J. Prosthodont. Res. 2022, 66, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Ramos Nde, C.; Campos, T.M.; Paz, I.S.; Machado, J.P.; Bottino, M.A.; Cesar, P.F.; Melo, R.M. Microstructure characterization and SCG of newly engineered dental ceramics. Dent. Mater. 2016, 32, 870–878. [Google Scholar] [CrossRef] [PubMed]
- Belli, R.; Lohbauer, U.; Goetz-Neunhoeffer, F.; Hurle, K. Crack-healing during two-stage crystallization of biomedical lithium (di)silicate glass-ceramics. Dent. Mater. 2019, 35, 1130–1145. [Google Scholar] [CrossRef]
- Belli, R.; Wendler, M.; Petschelt, A.; Lohbauer, U. Mixed-mode fracture toughness of texturized LS2 glass-ceramics using the three-point bending with eccentric notch test. Dent. Mater. 2017, 33, 1473–1477. [Google Scholar] [CrossRef] [PubMed]
- Mavriqi, L.; Valente, F.; Murmura, G.; Sinjari, B.; Macrì, M.; Trubiani, O.; Caputi, S.; Traini, T. Lithium disilicate and zirconia reinforced lithium silicate glass-ceramics for CAD/CAM dental restorations: Biocompatibility, mechanical and microstructural properties after crystallization. J. Dent. 2022, 119, 104054. [Google Scholar] [CrossRef] [PubMed]
- Ozdogan, A.; Duymus, Z.Y. Investigating the Effect of Different Surface Treatments on Vickers Hardness and Flexural Strength of Zirconium and Lithium Disilicate Ceramics. J. Prosthodont. 2018, 29, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Rocha, L.S.; Della Bona, A.; Pretto, M.D.; Corazza, P.H.; Borba, M.; Benetti, P. Assessment of the survival and success rates of lithium disilicate crowns after different surface finishing procedures: An in vitro study. J. Prosthet. Dent. 2023, 129, 897–905. [Google Scholar] [CrossRef]
- Furini, G.P.; Pecho, O.E.; Álvarez-Lloret, P.; Benetti, P. Analysis of Topography, Flexural Strength, and Microstructure of a Lithium Disilicate Glass-Ceramic after Surface Finishing. Int. J. Prosthodont. 2024, 37, 439–446. [Google Scholar] [CrossRef] [PubMed]
- May, M.M.; Fraga, S.; May, L.G. Effect of milling, fitting adjustments, and hydrofluoric acid etching on the strength and roughness of CAD-CAM glass-ceramics: A systematic review and meta-analysis. J. Prosthet. Dent. 2022, 128, 1190–1200. [Google Scholar] [CrossRef] [PubMed]
- Mohammadibassir, M.; Rezvani, M.B.; Golzari, H.; Moravej Salehi, E.; Fahimi, M.A.; Kharazi Fard, M.J. Effect of Two Polishing Systems on Surface Roughness, Topography, and Flexural Strength of a Monolithic Lithium Disilicate Ceramic. J. Prosthodont. 2019, 28, e172–e180. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Dal Piva, A.O.; Nedeljkovic, I.; Tribst, J.M.; Feilzer, A.J.; Kleverlaan, C.J. Effect of glazing technique and firing on surface roughness and flexural strength of an advanced lithium disilicate. Clin. Oral Investig. 2023, 27, 3917–3926. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vichi, A.; Zhao, Z.; Paolone, G.; Scotti, N.; Mutahar, M.; Goracci, C.; Louca, C. Factory Crystallized Silicates for Monolithic Metal-Free Restorations: A Flexural Strength and Translucency Comparison Test. Materials 2022, 15, 7834. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- DIN EN 843-5:2007-03; Advanced Technical Ceramics—Monolithic Ceramics—Mechanical Tests at Room Temperature—Part 5: Statistical Analysis. German Institute for Standardisation (Deutsches Institut für Normung): Berlin, Germany, 2007.
- Elsaka, S.E.; Elnaghy, A.M. Mechanical properties of zirconia reinforced lithium silicate glass-ceramic. Dent. Mater. 2016, 32, 908–914. [Google Scholar] [CrossRef]
- Carrabba, M.; Keeling, A.J.; Aziz, A.; Vichi, A.; Fabian Fonzar, R.; Wood, D.; Ferrari, M. Translucent zirconia in the ceramic scenario for monolithic restorations: A flexural strength and translucency comparison test. J. Dent. 2017, 60, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Juntavee, N.; Uasuwan, P. Flexural strength of different monolithic computer-assisted design and computer-assisted manufacturing ceramic materials upon different thermal tempering processes. Eur. J. Dent. 2020, 14, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Beyabanaki, E.; Ashtiani, R.E.; Moradi, M.; Namdari, M.; Mostafavi, D.; Zandinejad, A. Biaxial flexural strength and Weibull characteristics of a resin ceramic material after thermal-cycling. J. Prosthodont. 2023, 32, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Barchetta, N.F.; Amaral, M.; Prochnow, C.; Rodrigues, F.P.; Bottino, M.A.; Valandro, L.F.; de Melo, R.M. Strength of a Zirconia-Reinforced Lithium Silicate Ceramic: Acid-Etching Time and Resin Cement Application Effects. Int. J. Periodontics Restor. Dent. 2019, 39, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Fabian Fonzar, R.; Goracci, C.; Carrabba, M.; Louca, C.; Ferrari, M.; Vichi, A. Influence of Acid Concentration and Etching Time on Composite Cement Adhesion to Lithium-silicate Glass Ceramics. J. Adhes. Dent. 2020, 22, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Osuchukwu, O.A.; Salihi, A.; Ibrahim, A.; Audu, A.A.; Makoyo, M.; Mohammed, S.A.; Lawal, M.Y.; Etinosa, P.O.; Isaac, I.O.; Oni, P.G.; et al. Weibull analysis of ceramics and related materials: A review. Heliyon 2024, 10, e32495. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Group | Initial Roughness | Final Roughness | p-Value |
|---|---|---|---|
| ZLS-AC | 0.763 (0.078) | 2.780 (0.748) | p = 0.000 |
| ZLS-CA | 0.9910 (0.2718) | 2.6849 (0.3678) | p = 0.000 |
| LDS-AC | 0.785 (0.125) | 3.540 (0.911) | p = 0.000 |
| LDS-CA | 0.8282 (0.170) | 3.157 (1.207) | p = 0.000 |
| Increase in Roughness | p-Value | ||
|---|---|---|---|
| Final Ra roughness—initial Ra roughness | ZLS-AC = 2.006 (0.772) | ZLS-CA = 1.651 (0.673) | p = 0.191 |
| LDS-AC = 2.800 (0.980) | LDS-CA = 2.40 (1.35) | p = 0.366 | |
| Material | Moment of Crystallization * | p-Value | |
|---|---|---|---|
| ZLS | AC = 232.1 (56.2) | CA = 115.0 (27.1) | p = 0.000 |
| LDS | AC = 244.3 (35.7) | CA = 135.2 (17.9) | p = 0.000 |
| Source | DF | Adj SS | ADJ MS | F-Vale | p-Value |
|---|---|---|---|---|---|
| Material | 1 | 3939 | 3939 | 2.87 | 0.096 |
| Moment of crystallization | 1 | 191,810 | 191,810 | 139.91 | 0.000 |
| Material Moment of crystallization | 1 | 236 | 236 | 0.17 | 0.680 |
| Error | 56 | 76,772 | 1371 | ||
| Total | 59 | 272,758 |
| Group | N | Mean | Grouping |
|---|---|---|---|
| LDS-AC | 15 | 244.32 | A |
| ZLS-AC | 15 | 232.08 | A |
| LDS-CA | 15 | 135.21 | B |
| ZLS-CA | 15 | 115.03 | B |
| Group | CI (95%) | CI (95%) | ||
|---|---|---|---|---|
| ZLS-AC | 3.741 | (2.160–5.225) | 259.15 | (217.63–308.39) |
| ZLS-CA | 4.254 | (2.456–5.941) | 126.79 | (108.74–147.75) |
| LDS-AC | 7.270 | (4.197–10.154) | 259.36 | (237.08–283.66) |
| LDS-CA | 8.425 | (4.864–11.767) | 143.14 | (132.46–154.64) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baroudi, K.; Almeida, N.R.d.; de Abreu, L.S.; Wandscher, V.F.; Ramos, N.d.C.; Padmanabhan, V.; Bucholz, C.A.; Amaral, M. Clinical Adjustment of Zirconia-Reinforced Lithium Silicate and Lithium Disilicate Restorations Should Be Performed Before Crystallization. Materials 2025, 18, 1944. https://doi.org/10.3390/ma18091944
Baroudi K, Almeida NRd, de Abreu LS, Wandscher VF, Ramos NdC, Padmanabhan V, Bucholz CA, Amaral M. Clinical Adjustment of Zirconia-Reinforced Lithium Silicate and Lithium Disilicate Restorations Should Be Performed Before Crystallization. Materials. 2025; 18(9):1944. https://doi.org/10.3390/ma18091944
Chicago/Turabian StyleBaroudi, Kusai, Nathália Ribeiro de Almeida, Laura Salerno de Abreu, Vinícius Felipe Wandscher, Nathalia de Carvalho Ramos, Vivek Padmanabhan, Caroline Andrade Bucholz, and Marina Amaral. 2025. "Clinical Adjustment of Zirconia-Reinforced Lithium Silicate and Lithium Disilicate Restorations Should Be Performed Before Crystallization" Materials 18, no. 9: 1944. https://doi.org/10.3390/ma18091944
APA StyleBaroudi, K., Almeida, N. R. d., de Abreu, L. S., Wandscher, V. F., Ramos, N. d. C., Padmanabhan, V., Bucholz, C. A., & Amaral, M. (2025). Clinical Adjustment of Zirconia-Reinforced Lithium Silicate and Lithium Disilicate Restorations Should Be Performed Before Crystallization. Materials, 18(9), 1944. https://doi.org/10.3390/ma18091944









