Virus Infections Play Crucial Roles in the Pathogenesis of Sjögren’s Syndrome
Abstract
1. Introduction
2. Autoimmunity and Viral Infection
3. Sjögren’s Syndrome and Viral Infection
4. Epstein-Barr Virus and Sjögren’s Syndrome
4.1. EBV and Its Clinical Siginificance
4.2. Molecular Pathogenesis of EBV-Associated Sjögren’s Syndrome
5. Animal Models of Virus Infection-Associated SS
6. Future Perspectives
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Seror, R.; Nocturne, G.; Mariette, X. Current and future therapies for primary Sjögren syndrome. Nat. Rev. Rheumatol. 2021, 17, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Verstappen, G.M.; Pringle, S.; Bootsma, H.; Kroese, F.G.M. Epithelial-immune cell interplay in primary Sjögren syndrome salivary gland pathogenesis. Nat. Rev. Rheumatol. 2021, 17, 333–348. [Google Scholar] [CrossRef] [PubMed]
- Nocturne, G.; Mariette, X. Advances in understanding the pathogenesis of primary Sjögren’s syndrome. Nat. Rev. Rheumatol. 2013, 9, 544–556. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Zheng, W.; Cao, W.; Yang, X.; Zhao, L.; Chen, Y. Acute fibrinous and organizing pneumonia in a patient with Sjögren’s syndrome and Legionella pneumonia: A case report and literature review. BMC Pulm. Med. 2022, 22, 205. [Google Scholar] [CrossRef] [PubMed]
- Francois, H.; Mariette, X. Renal involvement in primary Sjögren syndrome. Nat. Rev. Nephrol. 2016, 12, 82–93. [Google Scholar] [CrossRef]
- Weerasinghe, W.S.; Jayasinghe, C. Overlapping rheumatoid arthritis and antisynthetase syndrome with secondary Sjogren’s syndrome: A case report and review of the literature. J. Med. Case Rep. 2022, 16, 132. [Google Scholar] [CrossRef]
- Baldini, C.; Talarico, R.; Tzioufas, A.G.; Bombardieri, S. Classification criteria for Sjögren’s syndrome: A critical review. J. Autoimmun. 2012, 39, 9–14. [Google Scholar] [CrossRef]
- Sebastian, A.; Szachowicz, A.; Wiland, P. Classification criteria for secondary Sjögren’s syndrome. Current state of knowledge. Reumatologia 2019, 57, 277–280. [Google Scholar] [CrossRef]
- Conforti, A.; Di Cola, I.; Pavlych, V.; Ruscitti, P.; Berardicurti, O.; Ursini, F.; Giacomelli, R.; Cipriani, P. Beyond the joints, the extra-articular manifestations in rheumatoid arthritis. Autoimmun. Rev. 2021, 20, 102735. [Google Scholar] [CrossRef]
- Kollert, F.; Fisher, B.A. Equal rights in autoimmunity: Is Sjögren’s syndrome ever ‘secondary’? Rheumatology 2020, 59, 1218–1225. [Google Scholar] [CrossRef]
- Pasoto, S.G.; Adriano de Oliveira Martins, V.; Bonfa, E. Sjögren’s syndrome and systemic lupus erythematosus: Links and risks. Open Access Rheumatol. 2019, 11, 33–45. [Google Scholar] [CrossRef] [PubMed]
- Salliot, C.; Mouthon, L.; Ardizzone, M.; Sibilia, J.; Guillevin, L.; Gottenberg, J.E.; Mariette, X. Sjögren’s syndrome is associated with and not secondary to systemic sclerosis. Rheumatology 2007, 46, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, R. Disease mechanisms in Sjögren’s syndrome: What do we know? Scand. J. Immunol. 2022, 95, e13145. [Google Scholar] [CrossRef] [PubMed]
- Theofilopoulos, A.N.; Kono, D.H.; Baccala, R. The multiple pathways to autoimmunity. Nat. Immunol. 2017, 18, 716–724. [Google Scholar] [CrossRef]
- Bluestone, J.A.; Krensky, A.M.; Turka, L.A.; Rotrosen, D.; Matthews, J.B. Ten years of the Immune Tolerance Network: An integrated clinical research organization. Sci. Transl. Med. 2010, 2, 19cm17. [Google Scholar] [CrossRef][Green Version]
- Rouse, B.T.; Sehrawat, S. Immunity and immunopathology to viruses: What decides the outcome? Nat. Rev. Immunol. 2010, 10, 514–526. [Google Scholar] [CrossRef]
- Zacharias, H.; Dubey, S.; Koduri, G.; D’Cruz, D. Rheumatological complications of COVID-19. Autoimmun. Rev. 2021, 20, 102883. [Google Scholar] [CrossRef]
- Tang, K.T.; Hsu, B.C.; Chen, D.Y. Autoimmune and Rheumatic Manifestations Associated With COVID-19 in Adults: An Updated Systematic Review. Front. Immunol. 2021, 12, 645013. [Google Scholar] [CrossRef]
- Casanova, J.L.; Abel, L. Mechanisms of viral inflammation and disease in humans. Science 2021, 374, 1080–1086. [Google Scholar] [CrossRef]
- Matsuoka, M.; Jeang, K.T. Human T-cell leukaemia virus type 1 (HTLV-1) infectivity and cellular transformation. Nat. Rev. Cancer 2007, 7, 270–280. [Google Scholar] [CrossRef]
- Wykes, M.N.; Lewin, S.R. Immune checkpoint blockade in infectious diseases. Nat. Rev. Immunol. 2018, 18, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Munz, C. Cytotoxicity in Epstein Barr virus specific immune control. Curr. Opin. Virol. 2021, 46, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Smatti, M.K.; Cyprian, F.S.; Nasrallah, G.K.; Al Thani, A.A.; Almishal, R.O.; Yassine, H.M. Viruses and Autoimmunity: A Review on the Potential Interaction and Molecular Mechanisms. Viruses 2019, 11, 762. [Google Scholar] [CrossRef]
- Igoe, A.; Scofield, R.H. Autoimmunity and infection in Sjögren’s syndrome. Curr. Opin. Rheumatol. 2013, 25, 480–487. [Google Scholar] [CrossRef]
- Jog, N.R.; James, J.A. Epstein Barr Virus and Autoimmune Responses in Systemic Lupus Erythematosus. Front. Immunol. 2020, 11, 623944. [Google Scholar] [CrossRef] [PubMed]
- Getts, D.R.; Chastain, E.M.; Terry, R.L.; Miller, S.D. Virus infection, antiviral immunity, and autoimmunity. Immunol. Rev. 2013, 255, 197–209. [Google Scholar]
- Fujinami, R.S.; von Herrath, M.G.; Christen, U.; Whitton, J.L. Molecular mimicry, bystander activation, or viral persistence: Infections and autoimmune disease. Clin. Microbiol. Rev. 2006, 19, 80–94. [Google Scholar] [CrossRef]
- Rojas, M.; Restrepo-Jimenez, P.; Monsalve, D.M.; Pacheco, Y.; Acosta-Ampudia, Y.; Ramirez-Santana, C.; Leung, P.S.C.; Ansari, A.A.; Gershwin, M.E.; Anaya, J.M. Molecular mimicry and autoimmunity. J. Autoimmun. 2018, 95, 100–123. [Google Scholar] [CrossRef]
- Hiemstra, H.S.; Schloot, N.C.; van Veelen, P.A.; Willemen, S.J.; Franken, K.L.; van Rood, J.J.; de Vries, R.R.; Chaudhuri, A.; Behan, P.O.; Drijfhout, J.W.; et al. Cytomegalovirus in autoimmunity: T cell crossreactivity to viral antigen and autoantigen glutamic acid decarboxylase. Proc. Natl. Acad. Sci. USA 2001, 98, 3988–3991. [Google Scholar] [CrossRef]
- Eizirik, D.L.; Op de Beeck, A. Coxsackievirus and Type 1 Diabetes Mellitus: The Wolf’s Footprints. Trends Endocrinol. Metab. 2018, 29, 137–139. [Google Scholar] [CrossRef]
- Nakamura, H.; Shimizu, T.; Kawakami, A. Role of Viral Infections in the Pathogenesis of Sjögren’s Syndrome: Different Characteristics of Epstein-Barr Virus and HTLV-1. J. Clin. Med. 2020, 9, 1459. [Google Scholar] [CrossRef] [PubMed]
- Tsuboi, H.; Matsumoto, I.; Hagiwara, S.; Hirota, T.; Takahashi, H.; Ebe, H.; Yokosawa, M.; Yagishita, M.; Takahashi, H.; Kurata, I.; et al. Effectiveness of abatacept for patients with Sjögren’s syndrome associated with rheumatoid arthritis. An open label, multicenter, one-year, prospective study: ROSE (Rheumatoid Arthritis with Orencia Trial toward Sjogren’s syndrome Endocrinopathy) trial. Mod. Rheumatol. 2016, 26, 891–899. [Google Scholar] [CrossRef] [PubMed]
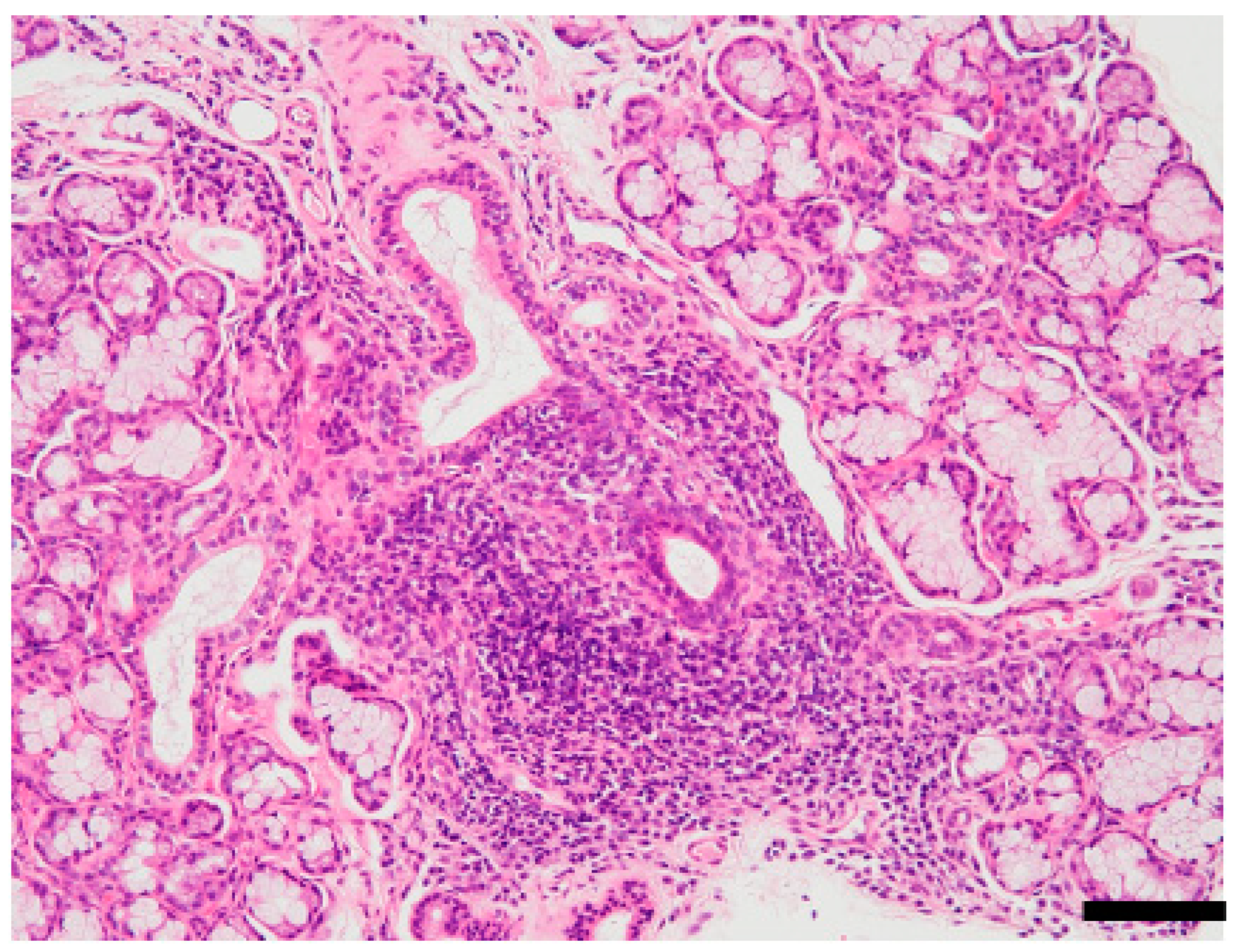
- Ushio, A.; Arakaki, R.; Otsuka, K.; Yamada, A.; Tsunematsu, T.; Kudo, Y.; Aota, K.; Azuma, M.; Ishimaru, N. CCL22-Producing Resident Macrophages Enhance T Cell Response in Sjögren’s Syndrome. Front. Immunol. 2018, 9, 2594. [Google Scholar] [CrossRef] [PubMed]
- Munz, C.; Lunemann, J.D.; Getts, M.T.; Miller, S.D. Antiviral immune responses: Triggers of or triggered by autoimmunity? Nat. Rev. Immunol. 2009, 9, 246–258. [Google Scholar] [CrossRef]
- Gugliesi, F.; Pasquero, S.; Griffante, G.; Scutera, S.; Albano, C.; Pacheco, S.F.C.; Riva, G.; Dell’Oste, V.; Biolatti, M. Human Cytomegalovirus and Autoimmune Diseases: Where Are We? Viruses 2021, 13, 260. [Google Scholar] [CrossRef]
- Scully, C. Apects of human disease. Human disease. 56. Sjogren’s syndrome. Dent. Update 2010, 37, 413. [Google Scholar] [CrossRef]
- Venables, P.J.; Ross, M.G.; Charles, P.J.; Melsom, R.D.; Griffiths, P.D.; Maini, R.N. A seroepidemiological study of cytomegalovirus and Epstein-Barr virus in rheumatoid arthritis and sicca syndrome. Ann. Rheum. Dis. 1985, 44, 742–746. [Google Scholar] [CrossRef]
- Ferreiro, M.C.; Prieto, M.H.; Rodriguez, S.B.; Vazquez, R.L.; Iglesias, A.C.; Dios, P.D. Whole stimulated salivary flow in patients with chronic hepatitis C virus infection. J. Oral Pathol. Med. 2002, 31, 117–120. [Google Scholar] [CrossRef]
- Maldonado, J.O.; Beach, M.E.; Wang, Y.; Perez, P.; Yin, H.; Pelayo, E.; Fowler, S.; Alevizos, I.; Grisius, M.; Baer, A.N.; et al. HCV Infection Alters Salivary Gland Histology and Saliva Composition. J. Dent. Res. 2022, 101, 534–541. [Google Scholar] [CrossRef]
- Nakamura, H.; Horai, Y.; Tokuyama, A.; Yoshimura, S.; Nakajima, H.; Ichinose, K.; Yamasaki, S.; Nakamura, T.; Hayashi, T.; Kawakami, A. HTLV-I virological and histopathological analysis in two cases of anti-centromere-antibody-seropositive Sjogren’s syndrome. Mod. Rheumatol. 2013, 23, 133–139. [Google Scholar] [CrossRef]
- Nakamura, H.; Tsukamoto, M.; Nagasawa, Y.; Kitamura, N.; Shimizu, T.; Kawakami, A.; Nagata, K.; Takei, M. Does HTLV-1 Infection Show Phenotypes Found in Sjogren’s Syndrome? Viruses 2022, 14, 100. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Lee, J.S.; Shin, M.G.; Tanaka, Y.; Park, D.J.; Kim, T.J.; Park, Y.W.; Lee, S.S. Detection of HTLV-1 in the labial salivary glands of patients with Sjogren’s syndrome: A distinct clinical subgroup? J. Rheumatol. 2012, 39, 809–815. [Google Scholar] [PubMed]
- Ittah, M.; Miceli-Richard, C.; Gottenberg, J.E.; Sellam, J.; Eid, P.; Lebon, P.; Pallier, C.; Lepajolec, C.; Mariette, X. Viruses induce high expression of BAFF by salivary gland epithelial cells through TLR- and type-I IFN-dependent and -independent pathways. Eur. J. Immunol. 2008, 38, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Liu, L.; Wang, Y. Viral proteins recognized by different TLRs. J. Med. Virol. 2021, 93, 6116–6123. [Google Scholar] [CrossRef] [PubMed]
- Gilliet, M.; Cao, W.; Liu, Y.J. Plasmacytoid dendritic cells: Sensing nucleic acids in viral infection and autoimmune diseases. Nat. Rev. Immunol. 2008, 8, 594–606. [Google Scholar] [CrossRef]
- Nordmark, G.; Eloranta, M.L.; Ronnblom, L. Primary Sjogren’s syndrome and the type I interferon system. Curr. Pharm. Biotechnol. 2012, 13, 2054–2062. [Google Scholar] [CrossRef]
- Routsias, J.G.; Tzioufas, A.G. Autoimmune response and target autoantigens in Sjögren’s syndrome. Eur. J. Clin. Investig. 2010, 40, 1026–1036. [Google Scholar] [CrossRef]
- Ishimaru, N.; Arakaki, R.; Yoshida, S.; Yamada, A.; Noji, S.; Hayashi, Y. Expression of the retinoblastoma protein RbAp48 in exocrine glands leads to Sjögren’s syndrome-like autoimmune exocrinopathy. J. Exp. Med. 2008, 205, 2915–2927. [Google Scholar] [CrossRef]
- Mavragani, C.P.; Sagalovskiy, I.; Guo, Q.; Nezos, A.; Kapsogeorgou, E.K.; Lu, P.; Liang Zhou, J.; Kirou, K.A.; Seshan, S.V.; Moutsopoulos, H.M.; et al. Expression of Long Interspersed Nuclear Element 1 Retroelements and Induction of Type I Interferon in Patients with Systemic Autoimmune Disease. Arthritis Rheumatol. 2016, 68, 2686–2696. [Google Scholar] [CrossRef]
- Kivity, S.; Arango, M.T.; Ehrenfeld, M.; Tehori, O.; Shoenfeld, Y.; Anaya, J.M.; Agmon-Levin, N. Infection and autoimmunity in Sjogren’s syndrome: A clinical study and comprehensive review. J. Autoimmun. 2014, 51, 17–22. [Google Scholar] [CrossRef]
- Sanosyan, A.; Daien, C.; Nutz, A.; Bollore, K.; Bedin, A.S.; Morel, J.; Zimmermann, V.; Nocturne, G.; Peries, M.; Guigue, N.; et al. Discrepancy of Serological and Molecular Patterns of Circulating Epstein-Barr Virus Reactivation in Primary Sjögren’s Syndrome. Front. Immunol. 2019, 10, 1153. [Google Scholar] [CrossRef] [PubMed]
- Zhong, H.; Liu, S.; Wang, Y.; Xu, D.; Li, M.; Zhao, Y.; Zeng, X. Primary Sjögren’s syndrome is associated with increased risk of malignancies besides lymphoma: A systematic review and meta-analysis. Autoimmun. Rev. 2022, 21, 103084. [Google Scholar] [CrossRef] [PubMed]
- Saito, I.; Servenius, B.; Compton, T.; Fox, R.I. Detection of Epstein-Barr virus DNA by polymerase chain reaction in blood and tissue biopsies from patients with Sjögren’s syndrome. J. Exp. Med. 1989, 169, 2191–2198. [Google Scholar] [CrossRef] [PubMed]
- Saito, S.; Takeuchi, T. Immune response in LPD during methotrexate administration (MTX-LPD) in rheumatoid arthritis patients. J. Clin. Exp. Hematop. 2019, 59, 145–155. [Google Scholar] [CrossRef]
- Seo, S.; Hong, J.Y.; Yoon, S.; Yoo, C.; Park, J.H.; Lee, J.B.; Park, C.S.; Huh, J.; Lee, Y.; Kim, K.W.; et al. Prognostic significance of serum beta-2 microglobulin in patients with diffuse large B-cell lymphoma in the rituximab era. Oncotarget 2016, 7, 76934–76943. [Google Scholar] [CrossRef]
- Yoshimoto, K.; Tanaka, M.; Kojima, M.; Setoyama, Y.; Kameda, H.; Suzuki, K.; Tsuzaka, K.; Ogawa, Y.; Tsubota, K.; Abe, T.; et al. Regulatory mechanisms for the production of BAFF and IL-6 are impaired in monocytes of patients of primary Sjögren’s syndrome. Arthritis Res. Ther. 2011, 13, R170. [Google Scholar] [CrossRef]
- Ishimaru, N.; Takagi, A.; Kohashi, M.; Yamada, A.; Arakaki, R.; Kanno, J.; Hayashi, Y. Neonatal exposure to low-dose 2,3,7,8-tetrachlorodibenzo-p-dioxin causes autoimmunity due to the disruption of T cell tolerance. J. Immunol. 2009, 182, 6576–6586. [Google Scholar] [CrossRef]
- Inoue, H.; Mishima, K.; Yamamoto-Yoshida, S.; Ushikoshi-Nakayama, R.; Nakagawa, Y.; Yamamoto, K.; Ryo, K.; Ide, F.; Saito, I. Aryl hydrocarbon receptor-mediated induction of EBV reactivation as a risk factor for Sjögren’s syndrome. J. Immunol. 2012, 188, 4654–4662. [Google Scholar] [CrossRef]
- Lerner, M.R.; Andrews, N.C.; Miller, G.; Steitz, J.A. Two small RNAs encoded by Epstein-Barr virus and complexed with protein are precipitated by antibodies from patients with systemic lupus erythematosus. Proc. Natl. Acad. Sci. USA 1981, 78, 805–809. [Google Scholar] [CrossRef]
- McClain, M.T.; Heinlen, L.D.; Dennis, G.J.; Roebuck, J.; Harley, J.B.; James, J.A. Early events in lupus humoral autoimmunity suggest initiation through molecular mimicry. Nat. Med. 2005, 11, 85–89. [Google Scholar] [CrossRef]
- Hou, X.; Hong, X.; Ou, M.; Meng, S.; Wang, T.; Liao, S.; He, J.; Yu, H.; Liu, L.; Yin, L.; et al. Analysis of Gene Expression and TCR/B Cell Receptor Profiling of Immune Cells in Primary Sjogren’s Syndrome by Single-Cell Sequencing. J. Immunol. 2022. [Google Scholar] [CrossRef]
- Green, J.E.; Hinrichs, S.H.; Vogel, J.; Jay, G. Exocrinopathy resembling Sjogren’s syndrome in HTLV-1 tax transgenic mice. Nature 1989, 341, 72–74. [Google Scholar] [CrossRef] [PubMed]
- Fleck, M.; Kern, E.R.; Zhou, T.; Lang, B.; Mountz, J.D. Murine cytomegalovirus induces a Sjogren’s syndrome-like disease in C57Bl/6-lpr/lpr mice. Arthritis Rheum. 1998, 41, 2175–2184. [Google Scholar] [CrossRef]
- Ohyama, Y.; Carroll, V.A.; Deshmukh, U.; Gaskin, F.; Brown, M.G.; Fu, S.M. Severe focal sialadenitis and dacryoadenitis in NZM2328 mice induced by MCMV: A novel model for human Sjogren’s syndrome. J. Immunol. 2006, 177, 7391–7397. [Google Scholar] [CrossRef] [PubMed]
- Schuster, I.S.; Wikstrom, M.E.; Brizard, G.; Coudert, J.D.; Estcourt, M.J.; Manzur, M.; O’Reilly, L.A.; Smyth, M.J.; Trapani, J.A.; Hill, G.R.; et al. TRAIL+ NK cells control CD4+ T cell responses during chronic viral infection to limit autoimmunity. Immunity 2014, 41, 646–656. [Google Scholar] [CrossRef]
- Usami, Y.; Hirose, K.; Okumura, M.; Toyosawa, S.; Sakai, T. Brief communication: Immunohistochemical detection of ACE2 in human salivary gland. Oral Sci. Int. 2020, 18, 101–104. [Google Scholar] [CrossRef]
- Huang, N.; Perez, P.; Kato, T.; Mikami, Y.; Okuda, K.; Gilmore, R.C.; Conde, C.D.; Gasmi, B.; Stein, S.; Beach, M.; et al. SARS-CoV-2 infection of the oral cavity and saliva. Nat. Med. 2021, 27, 892–903. [Google Scholar] [CrossRef]
- Serban, A.; Mihai, A.; Dima, A.; Balaban, D.V.; Jinga, M.; Jurcut, C. The impact of the COVID-19 pandemic on patients with primary Sjogren syndrome. Rheumatol. Int. 2021, 41, 1933–1940. [Google Scholar] [CrossRef]
- Chowdhury, F.; Grigoriadou, S.; Bombardieri, M. Severity of COVID-19 infection in primary Sjogren’s syndrome and the emerging evidence of COVID-19-induced xerostomia. Clin. Exp. Rheumatol. 2021, 133, 215–222. [Google Scholar] [CrossRef]
- Xu, J.; Zhong, S.; Liu, J.; Li, L.; Li, Y.; Wu, X.; Li, Z.; Deng, P.; Zhang, J.; Zhong, N.; et al. Detection of severe acute respiratory syndrome coronavirus in the brain: Potential role of the chemokine mig in pathogenesis. Clin. Infect. Dis. 2005, 41, 1089–1096. [Google Scholar] [CrossRef]
- Benedict, C.A.; Norris, P.S.; Ware, C.F. To kill or be killed: Viral evasion of apoptosis. Nat. Immunol. 2002, 3, 1013–1018. [Google Scholar] [CrossRef] [PubMed]
- McCormick, C.; Khaperskyy, D.A. Translation inhibition and stress granules in the antiviral immune response. Nat. Rev. Immunol. 2017, 17, 647–660. [Google Scholar] [CrossRef] [PubMed]
- Perng, Y.C.; Lenschow, D.J. ISG15 in antiviral immunity and beyond. Nat. Rev. Microbiol. 2018, 16, 423–439. [Google Scholar] [CrossRef] [PubMed]
- Krump, N.A.; You, J. Molecular mechanisms of viral oncogenesis in humans. Nat. Rev. Microbiol. 2018, 16, 684–698. [Google Scholar] [CrossRef]
- Wu, S.X.; Ren, X.Y.; Pan, Y.L.; Guan, D.D.; Liu, S.; Zou, X.Y.; Shi, C.G.; Li, Y.Z.; Zhang, Y.Z. Effects of ALA-PDT on HPV16-immortalized cervical epithelial cell. Neoplasma 2017, 64, 175–181. [Google Scholar] [CrossRef]
- Xu, W.; Wu, Y.; Zhao, J.; Chen, J.; Zhang, W. Human immunodeficiency virus type 1 transcription is regulated by thieno [3,4-d]pyrimidine. Exp. Ther. Med. 2020, 19, 3090–3096. [Google Scholar] [CrossRef]
- Loyola, A.; Almouzni, G. Histone chaperones, a supporting role in the limelight. Biochim. Biophys. Acta 2004, 1677, 3–11. [Google Scholar] [CrossRef]
- Allen, H.F.; Wade, P.A.; Kutateladze, T.G. The NuRD architecture. Cell Mol. Life Sci. 2013, 70, 3513–3524. [Google Scholar] [CrossRef]
- Zhang, W.; Tyl, M.; Ward, R.; Sobott, F.; Maman, J.; Murthy, A.S.; Watson, A.A.; Fedorov, O.; Bowman, A.; Owen-Hughes, T.; et al. Structural plasticity of histones H3-H4 facilitates their allosteric exchange between RbAp48 and ASF1. Nat. Struct. Mol. Biol. 2013, 20, 29–35. [Google Scholar] [CrossRef]
- Ishimaru, N.; Arakaki, R.; Omotehara, F.; Yamada, K.; Mishima, K.; Saito, I.; Hayashi, Y. Novel role for RbAp48 in tissue-specific, estrogen deficiency-dependent apoptosis in the exocrine glands. Mol. Cell. Biol. 2006, 26, 2924–2935. [Google Scholar] [CrossRef][Green Version]
- Moutsopoulos, H.M. Sjogren’s syndrome: A forty-year scientific journey. J. Autoimmun. 2014, 51, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Tong, L.; Koh, V.; Thong, B.Y. Review of autoantigens in Sjogren’s syndrome: An update. J. Inflamm. Res. 2017, 10, 97–105. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otsuka, K.; Sato, M.; Tsunematsu, T.; Ishimaru, N. Virus Infections Play Crucial Roles in the Pathogenesis of Sjögren’s Syndrome. Viruses 2022, 14, 1474. https://doi.org/10.3390/v14071474
Otsuka K, Sato M, Tsunematsu T, Ishimaru N. Virus Infections Play Crucial Roles in the Pathogenesis of Sjögren’s Syndrome. Viruses. 2022; 14(7):1474. https://doi.org/10.3390/v14071474
Chicago/Turabian StyleOtsuka, Kunihiro, Mami Sato, Takaaki Tsunematsu, and Naozumi Ishimaru. 2022. "Virus Infections Play Crucial Roles in the Pathogenesis of Sjögren’s Syndrome" Viruses 14, no. 7: 1474. https://doi.org/10.3390/v14071474
APA StyleOtsuka, K., Sato, M., Tsunematsu, T., & Ishimaru, N. (2022). Virus Infections Play Crucial Roles in the Pathogenesis of Sjögren’s Syndrome. Viruses, 14(7), 1474. https://doi.org/10.3390/v14071474





