Burden of Influenza and Respiratory Syncytial Viruses in Suspected COVID-19 Patients: A Cross-Sectional and Meta-Analysis Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Cross-Sectional Study, Specimen Collection, and Processing
2.3. Systematic Review and Meta-Analysis
2.3.1. Search Strategy
2.3.2. Data Analysis
2.3.3. Statistical Analyses
3. Results
3.1. Cross-Sectional Study
3.2. Systematic Review and Meta-Analysis: Characteristics of the Included Studies
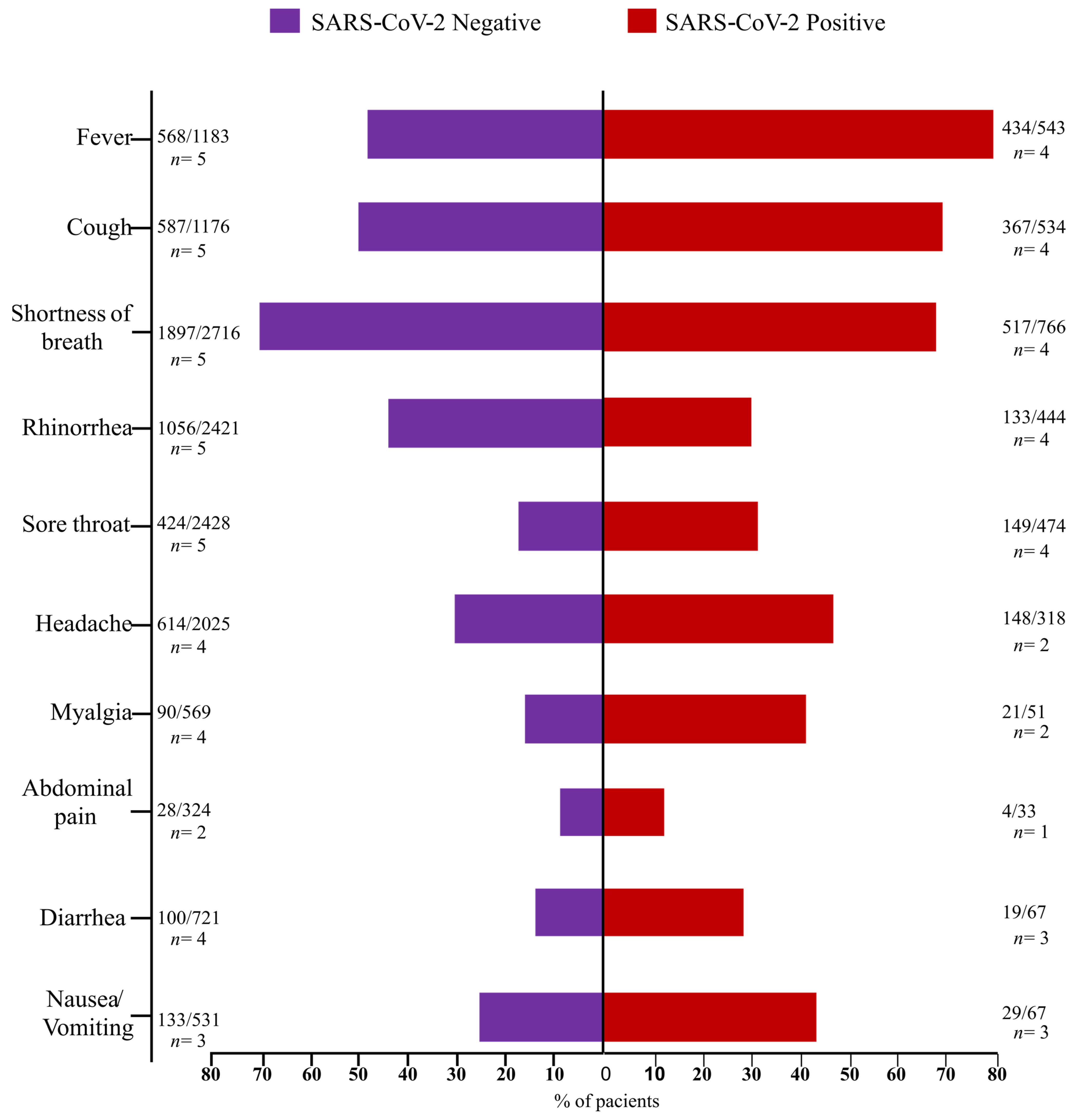
3.3. Clinical Features in the SCNG and SARS-CoV-Positive Group (SCPG)
3.4. A Meta-Analysis to Estimate the Pooled Prevalence of FluAV/FluBV and RSV in the SCNG
3.5. FluV and RSV Co-Infection: Epidemic Trends of FluV and RSV Infection
3.6. Publication Bias and Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Forni, D.; Cagliani, R.; Clerici, M.; Sironi, M. Disease-causing human viruses: Novelty and legacy. Trends Microbiol. 2022, 25, 1232–1242. [Google Scholar] [CrossRef]
- Leung, N.H.L. Transmissibility and transmission of respiratory viruses. Nat. Rev. Microbiol. 2021, 19, 528–545. [Google Scholar] [CrossRef]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 19, 157–160. [Google Scholar] [CrossRef]
- Li, J.; Lai, S.; Gao, G.F.; Shi, W. The emergence, genomic diversity and global spread of SARS-CoV-2. Nature 2021, 600, 408–418. [Google Scholar] [CrossRef]
- JHU, Johns Hopkins University of Medicine. Coronavirus Resource Center. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available online: https://coronavirus.jhu.edu/map.html. (accessed on 26 February 2023).
- Uyeki, T.M.; Hui, D.S.; Zambon, M.; Wentworth, D.E.; Monto, A.S. Influenza. Lancet 2022, 400, 693–706. [Google Scholar] [CrossRef]
- Krammer, F.; Smith, G.J.D.; Fouchier, R.A.M.; Peiris, M.; Kedzierska, K.; Doherty, P.C.; Palese, P.; Shaw, M.L.; Treanor, J.; Webster, R.G.; et al. Influenza. Nat. Rev. Dis. Primers 2018, 4, 3. [Google Scholar] [CrossRef]
- Iuliano, A.D.; Roguski, K.M.; Chang, H.H.; Muscatello, D.J.; Palekar, R.; Tempia, S.; Cohen, C.; Gran, J.M.; Schanzer, D.; Cowling, B.J.; et al. Global Seasonal Influenza-associated Mortality Collaborator Network. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study. Lancet 2018, 391, 1285–1300. [Google Scholar] [CrossRef]
- Busack, B.; Shorr, A.F. Going Viral-RSV as the Neglected Adult Respiratory Virus. Pathogens 2022, 11, 1324. [Google Scholar] [CrossRef]
- Nam, H.H.; Ison, M.G. Respiratory syncytial virus infection in adults. BMJ 2019, 366, l5021. [Google Scholar] [CrossRef]
- Meissner, H.C. Viral bronchiolitis in children. N. Engl. J. Med. 2016, 374, 62–72. [Google Scholar] [CrossRef]
- Savic, M.; Penders, Y.; Shi, T.; Branche, A.; Pirçon, J.Y. Respiratory syncytial virus disease burden in adults aged 60 years and older in high-income countries: A systematic literature review and meta-analysis. Influenza Other Respir. Viruses 2022, 17, e13031. [Google Scholar] [CrossRef]
- Wang, C.C.; Prather, K.A.; Sznitman, J.; Jimenez, J.L.; Lakdawala, S.S.; Tufekci, Z.; Marr, L.C. Airborne transmission of respiratory viruses. Science 2021, 373, eabd9149. [Google Scholar] [CrossRef]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 26, 1199–1207. [Google Scholar] [CrossRef]
- Lessler, J.; Reich, N.G.; Brookmeyer, R.; Perl, T.M.; Nelson, K.E.; Cummings, D.A. Incubation periods of acute respiratory viral infections: A systematic review. Lancet Infect. Dis. 2009, 9, 291–300. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/flu/symptoms/flu-vs-covid19.htm (accessed on 25 November 2022).
- Hogan, A.B.; Anderssen, R.S.; Davis, S.; Moore, H.C.; Lim, F.J.; Fathima, P.; Glass, K. Time series analysis of RSV and bronchiolitis seasonality in temperate and tropical Western Australia. Epidemics 2016, 16, 49–55. [Google Scholar] [CrossRef]
- Cong, B.; Deng, S.; Wang, X.; Li, Y. The role of respiratory co-infection with influenza or respiratory syncytial virus in the clinical severity of COVID-19 patients: A systematic review and meta-analysis. J. Glob. Health 2022, 12, 05040. [Google Scholar] [CrossRef]
- Krumbein, H.; Kümmel, L.S.; Fragkou, P.C.; Thölken, C.; Hünerbein, B.L.; Reiter, R.; Papathanasiou, K.A.; Renz, H.; Skevaki, C. Respiratory viral co-infections in patients with COVID-19 and associated outcomes: A systematic review and meta-analysis. Rev. Med. Virol. 2022, 10, e2365. [Google Scholar] [CrossRef]
- Dao, T.L.; Hoang, V.T.; Colson, P.; Million, M.; Gautret, P. Co-infection of SARS-CoV-2 and influenza viruses: A systematic review and meta-analysis. J. Clin. Virol. Plus 2021, 1, 100036. [Google Scholar] [CrossRef]
- Lansbury, L.; Lim, B.; Baskaran, V.; Lim, W.S. Co-infections in people with COVID-19: A systematic review and meta-analysis. J. Infect. 2020, 81, 266–275. [Google Scholar] [CrossRef]
- Drake, K.; Hore, T.A. Bomb.Bio-SARS-CoV-2 RNA Purification from Nasal/Throat Swabs Collected in Viral Transfer Media. BOMB. Bio. 2020. Available online: https://bomb.bio/protocols/ (accessed on 3 December 2022).
- Corman, V.M.; Landt, O.; Kaiser, M.; Molenkamp, R.; Meijer, A.; Chu, D.K.W.; Bleicker, T.; Brünink, S.; Schneider, J.; Schmidt, M.L.; et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eurosurveillance 2020, 25, 2000045. [Google Scholar] [CrossRef] [PubMed]
- Seegene. Summary of AllplexTM SARS-CoV-2/FluA/FluB/RSV Assay. Available online: https://www.seegene.com/assays/allplex_sars_cov_2_flua_flub_rsv_assay# (accessed on 1 December 2022).
- PRISMA-P Group; Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P.; The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Ottawa Health Research Institute. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 18 November 2022).
- Freeman, M.F.; Tukey, J.W. Transformations related to the angular and the square root. Ann. Math. Statist. 1950, 21, 607–611. [Google Scholar] [CrossRef]
- Barendregt, J.J.; Doi, S.A.; Lee, Y.Y.; Norman, R.E.; Vos, T. Meta-analysis of prevalence. J. Epidemiol. Community Health 2013, 67, 974–978. [Google Scholar] [CrossRef] [PubMed]
- Nyaga, V.N.; Arbyn, M.; Aerts, M. Metaprop: A Stata command to perform meta-analysis of binomial data. Arch. Public Health 2014, 72, 39. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Alpaydin, A.O.; Gezer, N.S.; Simsek, G.O.; Tertemiz, K.C.; Kutsoylu, O.O.E.; Zeka, A.N.; Guzel, I.; Soyturk, M.; Sayiner, A.A.; Oguz, V.A. Clinical and radiological diagnosis of non–SARS-CoV-2 viruses in the era of COVID-19 pandemic. J. Med. Virol. 2021, 93, 1119–1125. [Google Scholar] [CrossRef]
- Babiker, A.; Bradley, H.L.; Stittleburg, V.D.; Ingersoll, J.M.; Key, A.; Kraft, C.S.; Waggoner, J.J.; Piantadosi, A. Metagenomic sequencing to detect respiratory viruses in persons under investigation for COVID-19. J. Clin. Microbiol. 2021, 59, e02142-20. [Google Scholar] [CrossRef]
- Blasco, M.L.; Buesa, J.; Colomina, J.; Forner, M.J.; Galindo, M.J.; Navarro, J.; Noceda, J.; Redón, J.; Signes-Costa, J.; Navarro, D. Co-detection of respiratory pathogens in patients hospitalized with Coronavirus viral disease-2019 pneumonia. J. Clin. Virol. 2020, 92, 1799–1801. [Google Scholar] [CrossRef]
- Castillo, E.M.; Coyne, C.J.; Brennan, J.J.; Tomaszewski, C.A. Rates of coinfection with other respiratory pathogens in patients positive for coronavirus disease 2019 (COVID-19). JACEP Open 2020, 1, 592–596. [Google Scholar] [CrossRef]
- Hazra, A.; Collison, M.; Pisano, J.; Kumar, M.; Oehler, C.; Ridgway, J.P. Coinfections with SARS-CoV-2 and other respiratory pathogens. Infect. Control. Hosp. Epidemiol. 2020, 41, 1228–1236. [Google Scholar] [CrossRef]
- Hirotsu, Y.; Maejima, M.; Shibusawa, M.; Amemiya, K.; Nagakubo, Y.; Hosaka, K.; Sueki, H.; Mochizuki, H.; Tsutsui, T.; Kakizaki, Y.; et al. Analysis of Covid-19 and non-Covid-19 viruses, including influenza viruses, to determine the influence of intensive preventive measures in Japan. J. Clin. Virol. 2020, 129, 104543. [Google Scholar] [CrossRef]
- Hsih, W.-H.; Cheng, M.-Y.; Ho, M.-W.; Chou, C.-H.; Lin, P.-C.; Chi, C.-Y.; Liao, W.-C.; Chen, C.-Y.; Leong, L.-Y.; Tien, N.; et al. Featuring COVID-19 cases via screening symptomatic patients with epidemiologic link during flu season in a medical center of central Taiwan. J. Microbiol. Immunol. Infect. 2020, 53, 459–466. [Google Scholar] [CrossRef]
- Kim, D.; Quinn, J.; Pinsky, B.; Shah, N.H.; Brown, I. Rates of co-infection between SARS-CoV-2 and other respiratory pathogens. JAMA 2020, 20, 2085–2086. [Google Scholar] [CrossRef]
- Matos, A.D.R.; Motta, F.C.; Caetano, B.C.; Ogrzewalska, M.; Garcia, C.C.; Lopes, J.C.O.; Miranda, M.; Livorati, M.T.F.P.; Abreu, A.; Brown, D.; et al. Identification of SARS-CoV-2 and additional respiratory pathogens cases under the investigation of COVID-19 initial phase in a Brazilian reference laboratory. Mem. Inst. Oswaldo Cruz 2020, 115, e200232. [Google Scholar] [CrossRef]
- Nowak, M.D.; Sordillo, E.M.; Gitman, M.R.; Mondolfi, A.E.P. Coinfection in SARS-CoV-2 infected patients: Where are influenza virus and rhinovirus/enterovirus? J. Med. Virol. 2020, 92, 1699–1700. [Google Scholar] [CrossRef]
- Shah, S.J.; Barish, P.N.; Prasad, P.A.; Kistler, A.; Neff, N.; Kamm, J.; Li, L.M.; Chiu, C.Y.; Babik, J.M.; Fang, M.C.; et al. Clinical features, diagnostics, and outcomes of patients presenting with acute respiratory illness: A retrospective cohort study of patients with and without COVID-19. Eclinicalmedicine 2020, 27, 100518. [Google Scholar] [CrossRef]
- Akhtar, Z.; Islam, M.A.; Aleem, M.A.; Mah-E-Muneer, S.; Ahmmed, M.K.; Ghosh, P.K.; Rahman, M.; Rahman, M.Z.; Sumiya, M.K.; Rahman, M.M.; et al. SARS-CoV-2 and influenza virus coinfection among patients with severe acute respiratory infection during the first wave of COVID-19 pandemic in Bangladesh: A hospital-based descriptive study. BMJ Open 2021, 11, e053768. [Google Scholar] [CrossRef]
- Chekuri, S.; A Szymczak, W.; Goldstein, D.Y.; Nori, P.; Rolon, R.M.; Spund, B.; Singh-Tan, S.; Mohrmann, L.; Assa, A.; Southern, W.N.; et al. SARS-CoV-2 coinfection with additional respiratory virus does not predict severe disease: A retrospective cohort study. J. Antimicrob. Chemother. 2021, 76, iii12–iii19. [Google Scholar] [CrossRef]
- Eisen, A.K.A.; Gularte, J.S.; Demoliner, M.; Pereira, V.M.A.G.; Heldt, F.H.; Filippi, M.; Almeida, P.R.; Hansen, A.W.; Fleck, J.D.; Spilki, F.R. Low circulation of Influenza A and coinfection with SARS-CoV-2 among other respiratory viruses during the COVID-19 pandemic in a region of southern Brazil. J. Med. Virol. 2021, 93, 4392–4398. [Google Scholar] [CrossRef]
- Freeman, C.L.; Miller, N.M.; Bastarache, L.; Peterson, J.; Self, W.H.; Barrett, T.W.; Ward, M.J. Co-detection of SARS-CoV-2 with Secondary Respiratory Pathogen Infections. J. Gen. Intern. Med. 2021, 36, 1159–1160. [Google Scholar] [CrossRef]
- Letafi, A.; Aghamirmohammadali, F.S.; Rahimi-Foroushani, A.; Hasani, S.A.; Mokhtari-Azad, T.; Yavarian, J. No human respiratory syncytial virus but SARS-CoV-2 found in children under 5 years old referred to ChildrenMedical Center in 2021, Tehran, Iran. J. Med. Virol. 2022, 94, 3096–3100. [Google Scholar] [CrossRef]
- Marshall, N.C.; Kariyawasam, R.M.; Zelyas, N.; Kanji, J.N.; Diggle, M.A. Broad respiratory testing to identify SARS-CoV-2 viral co-circulation and inform diagnostic stewardship in the COVID-19 pandemic. Virol. J. 2021, 18, 93. [Google Scholar] [CrossRef]
- Schirmer, P.; Lucero-Obusan, C.; Sharma, A.; Sohoni, P.; Oda, G.; Holodniy, M. Respiratory co-infections with COVID-19 in the Veterans Health Administration, 2020. Diagn. Microbiol. Infect. Dis. 2021, 100, 115312. [Google Scholar] [CrossRef]
- Schneider, J.G.; Relich, R.F.; Datta, D.; Bond, C.; Goings, M.; Hall, D.; Lei, G.-S.; Kedra, J.; John, C.C. Identifying Risk Factors that distinguish symptomatic severe acute respiratory syndrome coronavirus 2 infection from common upper respiratory infections in children. Cureus 2021, 13, e13266. [Google Scholar] [CrossRef]
- Singh, V.; Upadhyay, P.; Reddy, J.; Granger, J. SARS-CoV-2 respiratory co-infections: Incidence of viral and bacterial co-pathogens. Int. J. Infect. Dis. 2021, 105, 617–620. [Google Scholar] [CrossRef]
- Stowe, J.; Tessier, E.; Zhao, H.; Guy, R.; Muller-Pebody, B.; Zambon, M.; Andrews, N.; Ramsay, M.; Bernal, J.L. Interactions between SARS-CoV-2 and influenza, and the impact of coinfection on disease severity: A test-negative design. Int. J. Epidemiol. 2021, 50, 1124–1133. [Google Scholar] [CrossRef]
- Varela, F.H.; Scotta, M.C.; Polese-Bonatto, M.; Sartor, I.T.S.; Ferreira, C.F.; Fernandes, I.R.; Zavaglia, G.O.; Ferreira de Almeida, W.A.; Arakaki-Sanchez, D.; Pinto, L.A.; et al. Absence of detection of RSV and influenza during the COVID-19 pandemic in a Brazilian cohort: Likely role of lower transmission in the community. J. Glob. Health 2021, 11, 05007. [Google Scholar] [CrossRef]
- Boschiero, M.N.; Duarte, A.; Palamim, C.V.C.; Alvarez, A.E.; Mauch, R.M.; Marson, F.A.L. Frequency of respiratory pathogens other than SARS-CoV-2 detected during COVID-19 testing. Diagn. Microbiol. Infect. Dis. 2022, 102, 115576. [Google Scholar] [CrossRef]
- Kriger, O.; Gefen-Halevi, S.; Leshem, E.; Smollan, G.; Belausov, N.; Egbarye, A.; Khashab, R.; Odeh, M.; Saffia, A.; Barak, Y.; et al. Viral co-pathogens in COVID-19 acute respiratory syndrome—What did we learn from the first year of pandemic? Int. J. Infect. Dis. 2022, 116, 226–229. [Google Scholar] [CrossRef]
- Muruganandam, N.; Roy, A.; Sivanandam, N.; Vins, A.; Beniwal, N.; Kaur, H.; Potdar, V.; Parvez, R. Respiratory viruses among ethnic Nicobarese during COVID-19 pandemic. BMC Infect. Dis. 2022, 22, 463. [Google Scholar] [CrossRef]
- Zhang, D.D.; Acree, M.E.; Ridgway, J.P.; Shah, N.; Hazra, A.; Ravichandran, U.; Kumar, M. Characterization coinfection in children with COVID-19: A dual center retrospective analysis. Infect. Control. Hosp. Epidemiol. 2020, 42, 1160–1162. [Google Scholar] [CrossRef]
- Chung, H.-Y.; Jian, M.-J.; Chang, C.-K.; Lin, J.-C.; Yeh, K.-M.; Chen, C.-W.; Chiu, S.-K.; Wang, Y.-H.; Liao, S.-J.; Li, S.-Y.; et al. Novel dual multiplex real-time RT-PCR assay for the rapid detection of SARS-CoV-2, influenza A/B, and respiratory syncytial virus using the BD MAX open system. Emerg. Microb. Infect. 2021, 10, 161–166. [Google Scholar] [CrossRef]
- Ministério da Saúde. Secretaria de Vigilância em Saúde. Boletim Epidemiológico Especial. Semana Epidemiológica 52 (20 a 26 December 2020). Available online: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/boletins/epidemiologicos/covid-19/2020/boletim_epidemiologico_covid_43_final_coe.pdf (accessed on 5 January 2023).
- Zaraket, H.; Hurt, A.C.; Clinch, B.; Barr, I.; Lee, N. Burden of influenza B virus infection and considerations for clinical management. Antivir. Res. 2021, 185, 104970. [Google Scholar] [CrossRef]
- Caini, S.; Kusznierz, G.; Garate, V.V.; Wangchuk, S.; Thapa, B.; Júnior, F.J.D.P.; De Almeida, W.A.F.; Njouom, R.; Fasce, R.A.; Bustos, P.; et al. The epidemiological signature of influenza B virus and its B/Victoria and B/Yamagata lineages in the 21st century. PLoS ONE 2019, 14, e0222381. [Google Scholar] [CrossRef]
- van de Sandt, C.E.; Bodewes, R.; Rimmelzwaan, G.F.; de Vries, R.D. Influenza B viruses: Not to be discounted. Future Microbiol. 2015, 10, 1447–1465. [Google Scholar] [CrossRef]
- Htar, M.T.T.; Yerramalla, M.S.; Moïsi, J.C.; Swerdlow, D.L. The burden of respiratory syncytial virus in adults: A systematic review and meta-analysis. Epidemiol. Infect. 2020, 148, e48. [Google Scholar] [CrossRef]
- Mufson, M.A.; Orvell, C.; Rafnar, B.; Norrby, E. Two distinct subtypes of human respiratory syncytial virus. J. Gen. Virol. 1985, 66, 2111–2124. [Google Scholar] [CrossRef] [PubMed]
- Borchers, A.T.; Chang, C.; Gershwin, M.E.; Gershwin, L.J. Respiratory syncytial virus-a comprehensive review. Clin. Rev. Allergy Immunol. 2013, 45, 331–379. [Google Scholar] [CrossRef]
- Walsh, E.E.; McConnochie, K.M.; Long, C.E.; Hall, C.B. Severity of respiratory syncytial virus infection is related to virus strain. J. Infect. Dis. 1997, 175, 814–820. [Google Scholar] [CrossRef]
- Sullender, W.M. Respiratory syncytial virus genetic and antigenic diversity. Clin. Microbiol. Rev. 2000, 13, 1–15. [Google Scholar] [CrossRef]
- Prifert, C.; Streng, A.; Krempl, C.D.; Liese, J.; Weissbrich, B. Novel respiratory syncytial virus a genotype, Germany, 2011–2012. Emerg. Infect. Dis. 2013, 19, 1029–1030. [Google Scholar] [CrossRef] [PubMed]
- Eshaghi, A.; Duvvuri, V.R.; Lai, R.; Nadarajah, J.T.; Li, A.; Patel, S.N.; Low, D.E.; Gubbay, J.B. Genetic variability of human respiratory syncytial virus A strains circulating in Ontario: A novel genotype with a 72 nucleotide G gene duplication. PLoS ONE 2012, 7, e32807. [Google Scholar] [CrossRef]
- Streng, A.; Goettler, D.; Haerlein, M.; Lehmann, L.; Ulrich, K.; Prifert, C.; Krempl, C.; Weißbrich, B.; Liese, J.G. Spread and clinical severity of respiratory syncytial virus A genotype ON1 in Germany, 2011–2017. BMC Infect. Dis. 2019, 19, 613. [Google Scholar] [CrossRef] [PubMed]
- Swets, M.C.; Russell, C.D.; Harrison, E.M.; Docherty, A.B.; Lone, N.; Girvan, M.; E Hardwick, H.; Visser, L.G.; Openshaw, P.J.M.; Groeneveld, G.H.; et al. SARS-CoV-2 co-infection with influenza viruses, respiratory syncytial virus, or adenoviruses. Lancet 2022, 399, 1463–1464. [Google Scholar] [CrossRef]
- Fage, C.; Hénaut, M.; Carbonneau, J.; Piret, J.; Boivin, G. Influenza A(H1N1)pdm09 Virus but Not Respiratory Syncytial Virus Interferes with SARS-CoV-2 Replication during Sequential Infections in Human Nasal Epithelial Cells. Viruses 2022, 14, 395. [Google Scholar] [CrossRef] [PubMed]
- Pizzorno, A.; Padey, B.; Dulière, V.; Mouton, W.; Oliva, J.; Laurent, E.; Milesi, C.; Lina, B.; Traversier, A.; Julien, T.; et al. Interactions Between Severe Acute Respiratory Syndrome Coronavirus 2 Replication and Major Respiratory Viruses in Human Nasal Epithelium. J. Infect. Dis. 2022, 226, 2095–2104. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.-M.; Song, W.-Q.; Liang, F.; Ye, B.-L.; Li, Z.-H.; Zhang, X.-R.; Zhong, W.-F.; Zhang, P.-D.; Liu, D.; Shen, D.; et al. Non-Pharmaceutical Interventions Implemented to Control the COVID-19 Were Associated With Reduction of Influenza Incidence. Front. Public Health 2022, 10, 773271. [Google Scholar] [CrossRef] [PubMed]
- Chow, E.J.; Uyeki, T.M.; Chu, H.Y. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat. Rev. Microbiol. 2023, 21, 195–210. [Google Scholar] [CrossRef] [PubMed]
- Mott, J.A.; Fry, A.M.; Kondor, R.; Wentworth, D.E.; Olsen, S.J. Re-emergence of influenza virus circulation during 2020 in parts of tropical Asia: Implications for other countries. Influenza Other Respir. Viruses. 2021, 15, 415–418. [Google Scholar] [CrossRef] [PubMed]
- Melidou, A.; Ködmön, C.; Nahapetyan, K.; Kraus, A.; Alm, E.; Adlhoch, C.; Mooks, P.; Dave, N.; Carvalho, C.; Meslé, M.M.; et al. Influenza returns with a season dominated by clade 3C.2a1b.2a.2 A(H3N2) viruses, WHO European Region, 2021/22. Euro Surveill. 2022, 27, 2200255. [Google Scholar] [CrossRef]



| Var. | S.s | COVID+ | COVID-N | p * | FluV+/COVID+ | FluV+ | FluV-N | p * | RSV+/COVID+ | RSV+ | RSV-N | p * |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| n (%) | 901 (100) | 168 (18.65) | 733 (81.33) | 3 (1.7) | 18 (1.9) | 883 (98) | 3 (1.7) | 5 (0.5) | 896 (99) | |||
| Sex | ||||||||||||
| Male | 380 (42.3) | 77 (46.67) | 303 (41.33) | 0.2 | 1 (50) | 4 (24) | 376 (42.7) | 0.11 | 1 (33.3) | 1 (20) | 379 (42.4) | 0.31 |
| Female | 518 (57.7) | 88 (53.33) | 430 (58.67) | 1 (50) | 13 (76) | 505 (57.3) | 2 (66.6) | 4 (80) | 514 (57.6) | |||
| Age (Y.) | ||||||||||||
| 0–4 | 53 (5.9) | 8 (4.8) | 45 (6.2) | 0.5 | 0 (0) | 1 (5.5) | 52 (5.9) | 0.99 | 0 (0) | 1 (20) | 52 (5.9) | 0.17 |
| 5–9 | 6 (0.7) | 1 (0.6) | 5 (0.7) | 0.77 | 0 (0) | 0 (0.0) | 6 (0.7) | 0.73 | 0 (0) | 0 (0) | 6 (0.7) | 0.85 |
| 10–19 | 53 (5.9) | 2 (1.2) | 51 (7) | 0.001 | 0 (0) | 2 (11) | 51 (5.8) | 0.29 | 0 (0) | 0 (0) | 53 (6) | 0.57 |
| 20–29 | 174 (19.61) | 41 (24.8) | 133 (18.4) | 0.4 | 2 (66.7) | 6 (33) | 168 (19.3) | 0.09 | 1 (33.3) | 1 (20) | 173 (19.6) | 0.96 |
| 30–39 | 206 (23.2) | 40 (24.2) | 166 (23) | 0.35 | 0 (0) | 3 (16.6) | 203 (23.3) | 0.62 | 1 (33.3) | 1 (20) | 205 (23.2) | 0.87 |
| 40–49 | 178 (20) | 39 (23.6) | 139 (19.2) | 0.93 | 1 (33.3) | 5 (27.7) | 173 (19.9) | 0.23 | 1 (33.3) | 1 (20) | 177 (20) | 0.98 |
| 50–59 | 104 (11.7) | 20 (12) | 84 (11.6) | 0.54 | 0 (0) | 0 (0.0) | 104 (12) | 0.13 | 0 (0) | 0 (0) | 104 (11.7) | 0.41 |
| 60–69 | 26 (2.9) | 9 (5.5) | 17 (2.3) | 0.09 | 0 (0) | 0 (0.0) | 26 (3) | 0.47 | 0 (0) | 0 (0) | 26 (2.9) | 0.69 |
| 70–79 | 19 (2.1) | 0 (0.0) | 19 (2.6) | 0.03 | 0 (0) | 0 (0.0) | 19 (2.2) | 0.54 | 0 (0) | 0 (0) | 19 (2.1) | 0.74 |
| 80+ | 7 (0.8) | 1 (0.6) | 6 (0.8) | 0.7 | 0 (0) | 0 (0.0) | 7 (0.8) | 0.71 | 0 (0) | 0 (0) | 7 (0.8) | 0.84 |
| C.p. | ||||||||||||
| May/2020 | 697 (78.1) | 134 (81.7) | 563 (77.3) | 0.4 | 3 (100) | 12 (66) | 685 (78.3) | 0.27 | 3 (100) | 5 (100) | 692 (78) | 0.22 |
| Jun/2020 | 34 (3.8) | 1 (0.6) | 33 (4.5) | 0.01 | 0 (0) | 1 (5.5) | 33 (3.7) | 0.68 | 0 (0) | 0 (0) | 34 (3.8) | 0.65 |
| Jul/2020 | 44 (4.9) | 7 (4.2) | 37 (0.5) | 0.6 | 0 (0) | 4 (22) | 40 (4.5) | <0.001 | 0 (0) | 0 (0) | 44 (4.9) | 0.61 |
| Aug/2020 | 118 (13.2) | 25 (15.2) | 93 (12.7) | 0.45 | 0 (0) | 1 (5.5) | 117 (13.3) | 0.33 | 0 (0) | 0 (0) | 118 (13.3) | 0.38 |
| Sep/2020 | 7 (0.8) | 1 (0.6) | 6 (0.8) | 0.76 | 0 (0) | 0 (0.0) | 7 (0.8) | 0.7 | 0 (0) | 0 (0) | 7 (0.8) | 0.84 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, V.G.d.; Gomes, A.J.C.; Bittar, C.; Geraldini, D.B.; Previdelli da Conceição, P.J.; Cabral, Á.S.; Carvalho, T.; Biselli, J.M.; Provazzi, P.J.S.; Campos, G.R.F.; et al. Burden of Influenza and Respiratory Syncytial Viruses in Suspected COVID-19 Patients: A Cross-Sectional and Meta-Analysis Study. Viruses 2023, 15, 665. https://doi.org/10.3390/v15030665
Costa VGd, Gomes AJC, Bittar C, Geraldini DB, Previdelli da Conceição PJ, Cabral ÁS, Carvalho T, Biselli JM, Provazzi PJS, Campos GRF, et al. Burden of Influenza and Respiratory Syncytial Viruses in Suspected COVID-19 Patients: A Cross-Sectional and Meta-Analysis Study. Viruses. 2023; 15(3):665. https://doi.org/10.3390/v15030665
Chicago/Turabian StyleCosta, Vivaldo Gomes da, Ana Júlia Chaves Gomes, Cíntia Bittar, Dayla Bott Geraldini, Pâmela Jóyce Previdelli da Conceição, Ágata Silva Cabral, Tamara Carvalho, Joice Matos Biselli, Paola Jocelan Scarin Provazzi, Guilherme Rodrigues Fernandes Campos, and et al. 2023. "Burden of Influenza and Respiratory Syncytial Viruses in Suspected COVID-19 Patients: A Cross-Sectional and Meta-Analysis Study" Viruses 15, no. 3: 665. https://doi.org/10.3390/v15030665
APA StyleCosta, V. G. d., Gomes, A. J. C., Bittar, C., Geraldini, D. B., Previdelli da Conceição, P. J., Cabral, Á. S., Carvalho, T., Biselli, J. M., Provazzi, P. J. S., Campos, G. R. F., Sanches, P. R. d. S., Costa, P. I., Nogueira, M. L., Araujo, J. P., Jr., Spilki, F. R., Calmon, M. F., & Rahal, P. (2023). Burden of Influenza and Respiratory Syncytial Viruses in Suspected COVID-19 Patients: A Cross-Sectional and Meta-Analysis Study. Viruses, 15(3), 665. https://doi.org/10.3390/v15030665