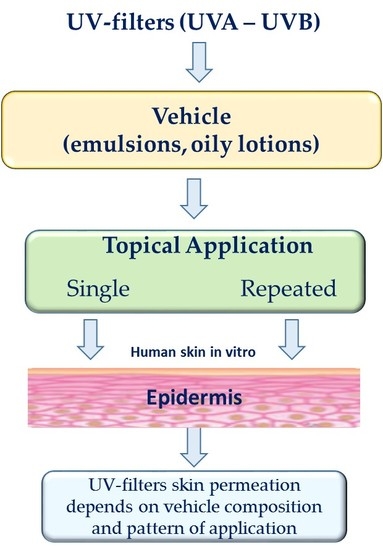
In Vitro Evaluation of Sunscreen Safety: Effects of the Vehicle and Repeated Applications on Skin Permeation from Topical Formulations
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Emulsions 1–3
2.3. Preparation of Oil Vehicles 4–6
2.4. In Vitro Release Experiments
2.5. In Vitro Skin Permeation Experiments
2.6. High Performance Liquid Chromatography (HPLC) Analyses
2.7. Data Analysis
3. Results and Discussion
3.1. In Vitro Release Experiments
3.2. In Vitro Skin Permeation Experiments
4. Conclusions
Author Contributions
Conflicts of Interest
References
- Lautenschlager, S.; Wulf, H.C.; Pittelkow, M.R. Photoprotection. Lancet 2007, 370, 528–537. [Google Scholar] [CrossRef]
- Varvaresou, A. Percutaneous absorption of organic sunscreens. J. Cosmet. Dermatol. 2006, 5, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Hayden, C.G.J.; Roberts, M.S.; Benson, H.E.A. Systemic absorption of sunscreen after topical application. Lancet 1997, 350, 863–864. [Google Scholar] [CrossRef]
- Gustavsson, G.H.; Farbrot, A.; Larko, O. Percutaneous absorption of benzophenone-3, a common component of topical sunscreens. Clin. Exp. Dermatol. 2002, 27, 691–694. [Google Scholar] [CrossRef]
- Okereke, C.S.; Barat, S.A.; Abdel-Rahman, M.S. Safety evaluation of benzophenone-3 after dermal administration in rats. Toxicol. Lett. 1995, 80, 61–67. [Google Scholar] [CrossRef]
- Kasichayanula, S.; House, J.D.; Wang, T.; Gu, X. Percutaneous characterization of the insect repellent DEET and the sunscreen oxybenzone from topical skin application. Toxicol. Appl. Pharmacol. 2007, 223, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Janjua, N.R.; Mogensen, B.; Andersson, A.M.; Petersen, J.H.; Henriksen, M.; Skakkebæk, E.; Wulf, H.C. Systemic absorption of the sunscreens benzophenone-3, octyl-methoxycinnamate, and 3-(4-methyl-benzylidene) camphor after whole-body topical application and reproductive hormone levels in humans. J. Investig. Dermatol. 2004, 123, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Klammer, H.; Schlecht, C.; Wuttke, W.; Jarry, H. Multi-organic risk assessment of estrogenic properties of octyl-methoxycinnamate in vivo. A 5-day sub-acute pharmacodynamic study with ovariectomized rats. Toxicology 2005, 215, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Kunz, P.Y.; Fent, K. Estrogenic activity of UV filter mixtures. Toxicol. Appl. Pharmacol. 2006, 217, 86–99. [Google Scholar] [CrossRef] [PubMed]
- Seidlová-Wuttke, D.; Christoffel, J.; Rimoldi, G.; Jarry, H.; Wuttke, W. Comparison of effects of estradiol with those of octylmethoxycinnamate and 4-methylbenzylidene camphor on fat tissue, lipids and pituitary hormones. Toxicol. Appl. Pharmacol. 2006, 214, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Nohynek, G.J.; Schaefer, H. Benefit and Risk of Organic Ultraviolet Filters. Regul. Toxicol. Pharmacol. 2001, 33, 285–299. [Google Scholar] [CrossRef] [PubMed]
- Nash, J.F. Human safety and efficacy of ultraviolet filters and sunscreen products. Dermatol. Clin. 2006, 24, 35–51. [Google Scholar] [CrossRef] [PubMed]
- Hayden, C.G.J.; Cross, S.E.; Anderson, C.; Saunders, N.A.; Roberts, M.S. Sunscreen penetration of human skin and related keratinocyte toxicity after topical application. Skin Pharmacol. Appl. Skin Physiol. 2005, 18, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Chatelain, E.; Gabard, B.; Surber, C. Skin Penetration and Sun Protection Factor of Five UV Filters: Effect of the Vehicle. Skin Pharmacol. Appl. Skin Physiol. 2003, 16, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Kurul, E.; Hekimoglu, S. Skin permeation of two different benzophenone derivatives from various vehicles. Int. J. Cosmet. Sci. 2001, 23, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Montenegro, L.; Carbone, C.; Condorelli, G.; Drago, R.; Puglisi, G. Effect of oil phase lipophilicity on in vitro drug release from o/w microemulsion with low surfactant content. Drug Dev. Ind. Pharm. 2006, 32, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Treffel, P.; Gabard, B. Skin penetration and sun protection factor of ultra-violet filters from two vehicles. Pharm. Res. 1996, 13, 770–774. [Google Scholar] [CrossRef] [PubMed]
- Montenegro, L.; Carbone, C.; Paolino, D.; Drago, R.; Stancampiano, A.H.; Puglisi, G. In vitro skin permeation of sunscreen agents from O/W emulsions. Int. J. Cosmet. Sci. 2008, 30, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Montenegro, L.; Carbone, C.; Puglisi, G. Vehicle effects on in vitro release and skin permeation of octylmethoxycinnamate from microemulsions. Int. J. Pharm. 2011, 405, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Montenegro, L.; Puglisi, G. Evaluation of sunscreen safety by in vitro skin permeation studies: Effects of vehicle composition. Pharmazie 2013, 68, 34–40. [Google Scholar] [PubMed]
- Hojerová, J.; Peráčková, Z.; Beránková, M. Margin of safety for two UV filters estimated by in vitro permeation studies mimicking consumer habits: Effects of skin shaving and sunscreen reapplication. Food Chem. Toxicol. 2017, 103, 66–78. [Google Scholar] [CrossRef] [PubMed]
- Hilton, J.; Woollen, B.H.; Scott, R.C.; Auton, T.R.; Trebilcock, K.L.; Wilks, M.F. Vehicle effects on in vitro percutaneous absorption through rat and human skin. Pharm. Res. 1994, 11, 1396–1400. [Google Scholar] [CrossRef] [PubMed]
- Brinon, L.; Geiger, S.; Alard, V.; Doucet, J.; Tranchant, J.F.; Couarraze, G. Percutaneous absorption of sunscreens from liquid crystalline phases. J. Control. Release 1999, 60, 67–76. [Google Scholar] [CrossRef]
- Fernandez, C.; Marti-Mestres, G.; Ramos, J.; Maillols, H. LC analysis of benzophenone-3: II application to determination of ‘in vitro’ and ‘in vivo’ skin penetration from solvents, coarse and submicron emulsions. J. Pharm. Biomed. Anal. 2000, 24, 155–165. [Google Scholar] [CrossRef]
- Roberts, M.S.; Harlock, E. Effect of repeated skin application on percutaneous absorption of salicylic acid. J. Pharm. Sci. 1978, 67, 1685–1687. [Google Scholar] [CrossRef] [PubMed]
- Shah, V.P.; Elkins, J.; Lam, S.Y.; Skelly, J.P. Determination of in vitro drug release from hydrocortisone creams. Int. J. Pharm. 1989, 53, 53–59. [Google Scholar] [CrossRef]
- Organisation for Economic Co-operation and Development (OECD). Guidance Notes on Dermal Absorption; Series on Testing and Assessment No. 156; OECD Press: Paris, France, 2011. [Google Scholar]
- Kligman, A.M.; Christophers, E. Preparation of isolated sheets of human skin. Arch. Dermatol. 1963, 88, 702–705. [Google Scholar] [CrossRef] [PubMed]
- Bronaugh, R.L.; Stewart, R.F. Methods for in vitro percutaneous absorption studies. III. Hydrophobic compounds. J. Pharm. Sci. 1984, 73, 1255–1258. [Google Scholar] [CrossRef] [PubMed]
- Huong, S.P.; Bun, H.; Fourneron, J.D.; Reynier, J.P.; Andrieu, V. Use of various models for in vitro percutaneous absorption studies of ultraviolet filters. Skin Res. Technol. 2009, 15, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Swarbrick, J.; Lee, G.; Brom, J. Drug permeation through human-skin. 1. Effect of storage-conditions of skin. J. Investig. Dermatol. 1982, 78, 63–66. [Google Scholar] [CrossRef] [PubMed]
- Baert, B.; Boonen, J.; Burvenich, C.; Roche, N.; Stillaert, P.; Blondeel, P.; Van Bocxlaer, J.; De Spiegeleer, B. A new discriminative criterion for the development of Franz diffusion tests for transdermal pharmaceuticals. J. Pharm. Sci. 2010, 13, 218–230. [Google Scholar] [CrossRef]
- Bronaugh, R.L.; Stewart, R.F.; Simon, M. Methods for in vitro percutaneous absorption studies VII: Use of the excised human skin. J. Pharm. Sci. 1986, 75, 1094–1097. [Google Scholar] [CrossRef] [PubMed]
- Scott, R.C.; Walker, M.; Dugard, P.H. In vitro percutaneous absorption experiments: A technique for the production of intact epidermal membranes from rat skin. J. Soc. Cosmet. Chem. 1986, 37, 35–41. [Google Scholar]
- Søeborg, T.; Basse, L.H.; Halling-Sørensen, B. Risk assessment of topically applied products. Toxicology 2007, 236, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Scientific Committee on Consumer Safety (SCCS). The SCCS Notes of Guidance for the Testing of Cosmetic Ingredients and Their Safety Evaluation, 9th ed.; SCCS/1564/15; European Commission: Brussels, Belgium, 2016; p. 151.
- Levy, S.B. UV filters. In Handbook of Cometic Science, 4th ed.; Barel, A.O., Paye, M., Maibach, H.I., Eds.; CRC Press: Boca Raton, FL, USA, 2014; pp. 279–286. ISBN 13:978-1-84214-565-4. [Google Scholar]
- Sparr, E.; Millecamps, D.; Isoir, M.; Burnier, V.; Larsson, A.; Cabane, B. Controlling the hydration of the skin though the application of occluding barrier creams. J. R. Soc. Interface 2013, 10. [Google Scholar] [CrossRef] [PubMed]
- Nash, J.F.; Tanner, P.R. The Controversy of Sunscreen Product Exposure: Too Little, Too Much, or Just Right. In Principles and Practice of Photoprotection; Wang, S.Q., Lim, H., Eds.; Adis International (Springer Nature): Berlin, Germany, 2016; pp. 125–139. ISBN 978-3-319-29381-3. [Google Scholar]
- Montenegro, L.; Paolino, D.; Puglisi, G. Effects of silicone emulsifiers on in vitro skin permeation of sunscreens from cosmetic emulsions. J. Cosmet. Sci. 2004, 55, 509–518. [Google Scholar] [PubMed]
- Walters, K.A.; Brain, K.R.; Howes, D.; James, V.J.; Kraus, A.L.; Teetsel, N.M.; Toulon, M.; Watkinson, A.C.; Gettings, S.D. Percutaneous penetration of octyl salicylate from representative sunscreen formulations through human skin in vitro. Food Chem. Toxicol. 1997, 35, 1219–1225. [Google Scholar] [CrossRef]
- Wester, R.C.; Maibach, H.I. Cutaneous pharmacokinetics: 10 steps to percutaneous absorption. Drug Metab. Rev. 1983, 14, 169–205. [Google Scholar] [CrossRef] [PubMed]
- Trotta, M. Influence of phase transformation on indomethacin release from microemulsions. J. Control. Release 1999, 60, 399–405. [Google Scholar] [CrossRef]
- Watkinson, A.C.; Brain, K.R.; Walters, K.A.; Hadgraft, J. Prediction of the percutaneous penetration of ultra-violet filters used in sunscreen formulations. Int. J. Cosmet. Sci. 1992, 14, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Ates, G.; Steinmetz, F.P.; Doktorova, T.Y.; Madden, J.C.; Rogiers, V. Linking existing in vitro dermal absorption data to physicochemical properties: Contribution to the design of a weight-of-evidence approach for the safety evaluation of cosmetic ingredients with low dermal bioavailability. Regul. Toxicol. Pharmacol. 2016, 76, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Pubchem, 2017. PubChem Substance Database. Available online: www.ncbi.nlm.nih.gov/pcsubstance (accessed on 14 December 2017).
- Barry, B.W. Lipid-protein-partitioning theory of skin penetration enhancement. J. Control. Release 1991, 15, 237–248. [Google Scholar] [CrossRef]
- Montenegro, L. Nanocarriers for skin delivery of cosmetic antioxidants. J. Pharm. Pharmacogn. Res. 2014, 2, 73–92. [Google Scholar]
- Souto, E.; Müller, R.H. Cosmetic features and applications of lipid nanoparticles (SLN, NLC). Int. J. Cosmet. Sci. 2008, 30, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Pardeike, J.; Hommoss, A.; Müller, R.H. Lipid nanoparticles (SLN, NLC) in cosmetic and pharmaceutical dermal products. Int. J. Pharm. 2009, 366, 170–184. [Google Scholar] [CrossRef] [PubMed]

| Ingredient | 1 | 2 |
|---|---|---|
| Phase A | ||
| Myritol 318 | 1.60 | 1.60 |
| IPM | 2.40 | 2.40 |
| Cetiol V | 3.00 | 3.00 |
| Cetiol SN | 5.00 | 5.00 |
| Beeswax | 1.00 | 0.70 |
| OMC | 5.00 | 5.00 |
| BMBM | 1.00 | 1.00 |
| Emulgade SE | 5.50 | 5.00 |
| GMS | 0.50 | 0.35 |
| Phase B | ||
| Disodium EDTA | 0.10 | 0.10 |
| Glycerin | 5.00 | 5.00 |
| Water | q.s.100 | q.s.100 |
| Phase C | ||
| Gram 1 | 0.35 | 0.35 |
| Kathon CG | 0.05 | 0.05 |
| Ingredient | % w/w |
|---|---|
| Phase A | |
| Mineral oil | 13.0 |
| Squalane | 3.00 |
| GMS | 1.00 |
| Sorbitan monostearate | 7.00 |
| BHT | 0.05 |
| OMC | 5.00 |
| BMBM | 1.00 |
| Phase B | |
| Disodium EDTA | 0.10 |
| Water | q.b.100 |
| Glycerin | 5.00 |
| Phase C | |
| Gram 1 | 0.35 |
| Kathon CG | 0.05 |
| Oil | HLBr | Vehicle | ||
|---|---|---|---|---|
| 4 | 5 | 6 | ||
| Mineral oil | 4, 5 | 83.95 | 69.95 | 49.95 |
| Almond oil | 6 | 5.00 | 5.00 | 5.00 |
| Jojoba oil | 6 | 5.00 | 5.00 | 5.00 |
| IPM | 11 | 0.00 | 14.00 | 34.00 |
| Vehicle | UV-Filter | Q24 ± S.D. (μg/cm2) | % Dose | Flux (μg/cm2/h) | Lag Time (h) |
|---|---|---|---|---|---|
| 1 | OMC | 73.41 ± 6.47 | 7.34 | 3.09 ± 0.28 | 0.20 |
| BMBM | 1.36 ± 0.11 | 0.68 | N.DT. | N.DT. | |
| 2 | OMC | 75.83 ± 7.77 | 7.58 | 3.20 ±0.29 | 0.11 |
| BMBM | 1.29 ±0.09 | 0.65 | N.DT. | N.DT. | |
| 3 | OMC | 90.66 ± 8.31 | 9.07 | 3.80 ± 0.35 | 0.15 |
| BMBM | 1.46 ± 0.15 | 0.73 | N.DT. | N.DT. | |
| 4 | OMC | 72.56 ± 8.02 | 7.26 | 3.07 ± 0.35 | 0.41 |
| BMBM | N.D. 1 | N.DT. 2 | N.DT. | N.DT. | |
| 5 | OMC | 95.23 ± 8.99 | 9.52 | 4.02 ± 0.39 | 0.17 |
| BMBM | 1.03 ± 0.10 | 0.51 | N.DT. | N.DT. | |
| 6 | OMC | 1.27 ± 0.14 | 0.13 | N.DT. | N.DT. |
| BMBM | N.D. | N.DT. | N.DT. | N.DT. |
| Parameter | OMC | BMBM |
|---|---|---|
| MW (g/mol) | 290.403 | 310.393 |
| TPSA (A2) | 35.5 | 43.4 |
| MP (°C) | −68.3 | 83.5 |
| Water solubility (mg/L) | 0.22–0.75 (at 21 °C) | 2.2 (at 25 °C) |
| Log Kow | 6.10 | 4.51 |
| Vehicle | UV-Filter | Q24 ± S.D. (μg/cm2) | % Dose | Flux (μg/cm2/h) | Lag Time (h) |
|---|---|---|---|---|---|
| 1 | OMC | 27.24 ± 3.23 | 2.72 | 3.09 ± 0.28 | 0.20 |
| BMBM | 1.04 ± 0.10 | 0.52 | N.DT.2 | N.DT. | |
| 2 | OMC | 27.50 ± 3.96 | 2.75 | 3.20 ±0.29 | 0.11 |
| BMBM | 1.06 ±0.09 | 0.53 | N.DT. | N.DT. | |
| 3 | OMC | 29.85 ± 4.14 | 2.99 | 3.80 ± 0.35 | 0.15 |
| BMBM | 0.57 ± 0.15 | 0.28 | N.DT. | N.DT. | |
| 4 | OMC | 16.64 ± 2.37 | 1.66 | 3.07 ± 0.35 | 0.41 |
| BMBM | N.D. 2 | N.DT. | N.DT. | N.DT. | |
| 5 | OMC | 46.63 ± 6.91 | 4.66 | 4.02 ± 0.39 | 0.17 |
| BMBM | 0.73 ± 0.21 | 0.36 | N.DT. | N.DT. | |
| 6 | OMC | N.D. 1 | N.DT. | N.DT. | N.DT. |
| BMBM | N.D. | N.DT. | N.DT. | N.DT. |
| Vehicle | UV-Filter | Q24 ± S.D. (µg/cm2) | % Dose | ||||
|---|---|---|---|---|---|---|---|
| Day 1 | Day 2 | Day 3 | Day 1 | Day 2 | Day 3 | ||
| 1 | OMC | 13.45 ± 1.98 | 16.78 ± 2.03 | 16.23 ± 3.07 | 1.35 | 1.57 | 1.62 |
| BMBM | 0.56 ± 0.03 | 0.70 ± 0.02 | 0.72 ± 0.10 | 0.28 | 0.35 | 0.36 | |
| 2 | OMC | 13.03 ± 2.31 | 17.33 ± 2.97 | 17.46 ± 4.33 | 1.30 | 1.73 | 1.74 |
| BMBM | 0.55 ± 0.02 | 0.72 ± 0.23 | 0.71 ±0.20 | 0.27 | 0.36 | 0.36 | |
| 3 | OMC | 13.99 ± 1.76 | 15.00 ± 2.49 | 15.41 ± 2.98 | 1.40 | 1.50 | 1.54 |
| BMBM | N.D. 1 | N.D. | N.D. | N.DT. 2 | N.DT. | N.DT. | |
| 4 | OMC | 8.09 ± 1.02 | 9.55 ± 2.10 | 8.93 ± 1.29 | 0.81 | 0.95 | 0.89 |
| BMBM | N.D. | N.D. | N.D. | N.DT. | N.DT. | N.DT. | |
| 5 | OMC | 26.44 ± 3.71 | 29.36 ± 5.99 | 28.14 ± 4.15 | 2.64 | 2.93 | 2.81 |
| BMBM | N.D. | N.D. | N.D. | N.DT. | N.DT. | N.DT. | |
| 6 | OMC | N.D. | N.D. | N.D. | N.DT. | N.DT. | N.DT. |
| BMBM | N.D. | N.D. | N.D. | N.DT. | N.DT. | N.DT. | |
| Vehicle | Day 1 | Day 2 | Day 3 |
|---|---|---|---|
| 1 | 4.5 ± 0.5 | 7.7 ± 1.5 | 7.3 ± 1.6 |
| 2 | 3.9 ± 0.3 | 8.3 ± 2.0 | 8.4 ± 1.9 |
| 3 | 4.8 ± 0.4 | 5.8 ± 1.0 | 6.2 ± 1.7 |
| 4 | 3.5 ± 0.4 | 5.0 ± 0.9 | 4.4 ± 1.0 |
| 5 | 11.5 ± 1.8 | 14.5 ± 2.1 | 13.3 ± 1.9 |
| 6 | N.D. | N.D. | N.D. |
| Vehicle | UV-Filter | SED (mg/Kg/day) | MoS | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Single | Repeated | Single | Repeated | ||||||
| Day 1 | Day 2 | Day 3 | Day 1 | Day 2 | Day 3 | ||||
| 1 | OMC | 6.81 | 3.36 | 4.17 | 4.05 | 66 | 134 | 108 | 111 |
| BMBM | 0.26 | 0.14 | 0.17 | 0.18 | 1730 | 3214 | 2647 | 2500 | |
| 2 | OMC | 6.86 | 3.25 | 4.33 | 4.36 | 66 | 138 | 104 | 103 |
| BMBM | 0.27 | 0.14 | 0.18 | 0.18 | 1666 | 3214 | 2500 | 2500 | |
| 3 | OMC | 7.46 | 3.50 | 3.75 | 3.85 | 60 | 129 | 120 | 117 |
| BMBM | 0.14 | N.D. | N.D. | N.D. | 3214 | N.D. | N.D. | N.D. | |
| 4 | OMC | 4.16 | 2.02 | 2.39 | 2.23 | 108 | 223 | 188 | 202 |
| BMBM | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
| 5 | OMC | 11.66 | 6.61 | 7.34 | 7.03 | 39 | 68 | 61 | 64 |
| BMBM | 0.18 | N.D. | N.D. | N.D. | 2500 | N.D. | N.D. | N.D. | |
| 6 | OMC | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. |
| BMBM | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | N.D. | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montenegro, L.; Turnaturi, R.; Parenti, C.; Pasquinucci, L. In Vitro Evaluation of Sunscreen Safety: Effects of the Vehicle and Repeated Applications on Skin Permeation from Topical Formulations. Pharmaceutics 2018, 10, 27. https://doi.org/10.3390/pharmaceutics10010027
Montenegro L, Turnaturi R, Parenti C, Pasquinucci L. In Vitro Evaluation of Sunscreen Safety: Effects of the Vehicle and Repeated Applications on Skin Permeation from Topical Formulations. Pharmaceutics. 2018; 10(1):27. https://doi.org/10.3390/pharmaceutics10010027
Chicago/Turabian StyleMontenegro, Lucia, Rita Turnaturi, Carmela Parenti, and Lorella Pasquinucci. 2018. "In Vitro Evaluation of Sunscreen Safety: Effects of the Vehicle and Repeated Applications on Skin Permeation from Topical Formulations" Pharmaceutics 10, no. 1: 27. https://doi.org/10.3390/pharmaceutics10010027
APA StyleMontenegro, L., Turnaturi, R., Parenti, C., & Pasquinucci, L. (2018). In Vitro Evaluation of Sunscreen Safety: Effects of the Vehicle and Repeated Applications on Skin Permeation from Topical Formulations. Pharmaceutics, 10(1), 27. https://doi.org/10.3390/pharmaceutics10010027