1. Introduction
Skin aging is a progressive and comprehensive process driven by the environment and time. It is associated with aesthetic and functional changes, such as an increase in wrinkles and cutis laxa. Skin aging is a slow and irreversible process. Photoaging occurs due to perennial exposure to ultraviolet light (UV), which causes skin damage [
1]. Long-term UV irradiation induces reactive oxygen species (ROS) generation. Oxygen free radicals destroy DNA, the extracellular matrix and membrane lipids of skin cells and cause the development of wrinkles [
2]. In addition, cellular damage (e.g., DNA damage due to ROS generation) induces skin cells to overexpress matrix metalloproteinases, which destroy the skin matrix tissue [
3,
4]. Histological studies have shown that major damage occurs in skin connective tissue upon UV irradiation [
5].
Vitamin D
3 (VD
3) is known for its capacity to maintain bone health. VD
3 has an impact on the skin, although it is produced in the skin. Recent studies have shown that VD
3 could repair skin cell damage caused by UV. The main damage by UV is to the DNA by the induction of cyclobutane pyrimidine dimers (CPDs) [
6,
7]. VD
3 significantly reduces the induction of CPDs through increasing two nucleotide excision repair by inducing expression of damage-specific DNA binding protein 2 and xeroderma pigmentosum complementation group C [
8]. In addition, VD
3 increases the expression of p53 protein, which enhances DNA repair by blocking the progression of the cell cycle [
9,
10]. UV also induces an increased level of ROS and NO in skin cells, which increases oxidative damages, such as DNA strand breaks, oxidation of purine or pyrimidine, and lipid peroxidation. VD
3 could reduce ROS and NO generation induced by UV. Furthermore, it protects keratinocytes against UV damage [
10,
11,
12,
13]. The idea of sunburn and VD
3 preventing photoaging may seem counter-intuitive, however, skin exposed to UV is the major mechanism to obtain VD
3 for humans. But the VD
3 photosynthesis, erythema, and CPD formation are all in the same spectral range of UVB. Therefore, the photosynthesis of VD
3 can not be dissociated from photodamage. Although VD
3 could be transformed under UV, it only occurs in the first few minutes upon exposure to UV, and longer exposure adds nothing to VD
3 stores despite increasing DNA damage in a linear fashion. So, naturally occurring VD
3 under UV is insufficient to prevent photoaging. Additional VD
3 needs to be supplied for skin protection [
14].
Photostability and effectiveness are two key parameters of sunscreen products [
2]. Although VD
3 effectively prevents skin photoaging, VD
3 is sensitive to air, light and high temperature, which is not conducive to storage, transportation and use [
2].VD
3 also rapidly degrades in the traditional carrier (water/ethanol) [
15]. Liposomes are commonly used as a carrier to protect drugs from degradation. Liposomes are also used as a protective carrier in cosmetics to enhance the stability of active substances [
16]. The poor solubility of VD
3 impedes uniform distribution in the skin. Liposomes also could improve solubility and control drug release [
17].
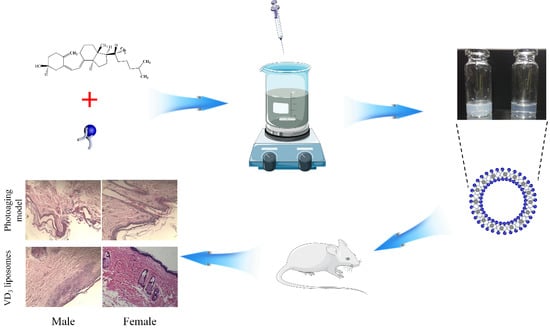
In this study, we optimized the liposomal formulation of VD3 to improve encapsulation efficiency (EE%) and to enhance transdermal absorption and stability of VD3.
2. Materials and Methods
2.1. Materials
Vitamin D3 (crystalline, purity > 99%) was purchased from Shanghai Yuanye Bio-Technology Co., Ltd. (Shanghai, China). Egg phosphatidylcholine (egg PC) was purchased from Jinban Pharmaceutical Co., Ltd. (Shanghai, China). Cholesterol (Chol) was obtained from Beijing Dingguo Changsheng Biotechnology Co., Ltd. (Beijing, China). Other reagents were all of the analytical grade. Aloe-gel was purchased from PERFECT Co., Ltd. (Guangdong, China).
2.2. VD3 Liposomes Preparation
Particle size and EE% were used as assessment criteria to evaluate two common liposomes preparation methods of VD3 (ethanol injection, film dispersion-homogenization method). A mixture of 30 mg of phospholipids, 10 mg of Chol and 10 mg of VD3 was dissolved in 5 mL ethanol as the lipid phase.
Ethanol injection method: The lipid solution was fast injected into 200 mL phosphate buffer solution (pH 6.8, PBS) under vortex mixing for 30 s. Then ethanol was removed by rotary evaporation and the liposomes were condensed to 100 mL under 35 °C. Finally, the liposomes of VD3 were sonicated for 5 min with an ice-bath.
Film dispersion-homogenization method: The lipid solution was dried by rotary evaporation at 35 °C to form a film. Then, 200 mL of PBS was used to hydrate lipid and liposomes were also condensed to 100 mL. Finally, liposomes were sonicated for 5 min in an ice-bath and were subjected to high-pressure homogenization (150 MPa) three times.
2.3. Encapsulation Efficiency
The EE% of VD3 was measured by filter method. Free VD3 was separated from liposomes by ultrafiltration centrifuge tube. Briefly, methanol was used to release and determine total VD3 (Wtotal) in liposomes. On the other hand, an ultrafiltration centrifuge filter (cut off MW of 10 kDa) was used to separate free VD3 (Wfree) from liposomes. The concentrations of Wtotal and Wfree were then measured by high-performance liquid chromatography (HPLC) method.
The concentration of VD3 was determined by HPLC at an absorption wavelength of 204 nm with 1 mL/min methanol as the mobile phase using a C18 reversed-phase column (4.6 × 250 mm, 5 μm).
2.4. Characterization of VD3 Liposomes
The particle size of VD3 liposomes was measured by Zetasizer Nano ZS 90 from Malvern Instruments, Ltd. (Malvern, U.K.). The size was shown by intensity-weighted distribution in Gaussian mode. A JEOL, JSM-6700F field emission scanning electron microscope (SEM) (Tokyo, Japan) was used to evaluate the surface morphology of VD3 liposomes at 3 kV accelerating voltage. VD3 liposomes were directly dropped on a clean silicon slice to dry naturally at room temperature overnight.
2.5. Optimization of Liposomes Formulation
On basis of single-factor experiments, we chose three interrelated factors
X1 (the amount of egg PC),
X2 (the mass ratio of egg PC to Chol), and
X3 (the mass ratio of lipid to the drug) to optimize the liposomes formulation using drug EE% as an evaluation indicator. We designed 17 experiments of three-factor, three-coded level using Box-Behnken design (BBD) to obtain the optimal VD
3 liposomes formulation. Liposomes were prepared by the ethanol injection method. The influence of factors on EE% were shown by response surface method. The factor-level table was listed in
Table 1. The optimal formulation of VD
3 liposomes was calculated by fitting the equation between EE% and three factors. The optimal formulation of VD
3 liposomes was verified three times in repetitive experiments.
2.6. Stability of VD3 in Liposomes
The stability of VD3 liposomes was evaluated in different conditions, including variations in time elapsed, variations in temperature, light exposure and after freezing and thawing. EE% and drug-content were used to estimate the stability of VD3 liposomes. We prepared 100 μg/mL of VD3 liposomes to compare with VD3 solution.
Samples were placed under 4, 25 and 40 °C in darkness and evaluated after storing for 1, 3, 5, 7 or 9 days. To study the effect of light on the stability of liposomes, 4500 Lx light was used to irradiate liposomes for 10 days at 25 °C. At each sampling time (1, 3, 5, 7 or 9 days), we analyzed the evaluation index of VD3 liposomes to study stability. Finally, VD3 liposomes were measured after freezing at −70 °C and thawing at 25 °C.
2.7. Transdermal Absorption of VD3 Liposomes
Wistar rats were fed according to the cleanliness class specifications, and 24 h free diet. Before the transdermal absorption experiment, a rat was euthanized with sodium pentobarbital and sacrificed. A piece of rat back skin was harvested without hair and after removing skin moisture with filter paper, the rats using protocol and relevant experimental procedures was approved by the Institutional Animal Care and Use Committee of Jilin University at January, 2017 (Authorization number: 201701005). The rat skin was fitted between the accept pool and supply pool of Franz diffusion pool. The corneous layer-oriented supply pool and diffusion area was 2.54 cm2. One ml of VD3 liposomes or VD3 solution (1 mg/mL) was evenly daubed onto the skin, while the supply pool was covered by plastic wrap. The accept pool was filled with saline solution containing 30% (v/v) ethanol under stirring (400 rpm) and maintained at a constant temperature of 37 °C. The device was placed in darkness. At sampling time of 0.5, 1, 2, and 4 h, we collected 1 mL receiving liquid to test the concentration of VD3, then replaced equivalent fresh liquid to the accept pool.
The residual VD
3 on the skin surface was cleaned, the skin was then cut into pieces. Pieces of skin were homogenized with PBS by a high-speed homogenizer. VD
3 within the skin homogenate solution was extracted by liquid-liquid extraction. Briefly, 200 ul skin homogenate solution was added into 1 mL methanol with vortex for 30s. And then 1 mL of hexane was added to extract VD
3 under oscillation mixture for 2 min [
18]. The mixture was centrifuged at 2000 rpm for 5 min to separate supernatant fluid. The supernatant fluid containing VD
3 was dried by nitrogen at 4 °C. Finally, the sample was dissolved in 200 μL of HPLC initial mobile phase. The skin retention of VD
3 was measured by the HPLC method.
Q: Average cumulative penetration of VD3 (μg/cm2)
Cn: Concentration of VD3 at the nth hour.
Ci: Concentration of VD3 when the ith.
V0: Volume of the accept pool (6.50 cm2)
V: Volume of the sampling
S: Diffusion area
2.8. VD3 Liposomes for Preventing Photoaging
Animal experiments were approved by the Institutional Animal Care and Use Committee of Jilin University at January, 2017 (Authorization number: 201701005). Wistar rats were fed according to the cleanliness class specifications.
Wistar rats were divided into four groups, each group contained eight rats with half female and half male. Rats were normally fed for 7 days with 24 h free diet to adapt to the environment before the experiment.
Back hair of rats in four groups was cleanly shaved in an area of about 3 × 5 cm. Ultraviolet ray was used to illuminate the exposed skin of rats to build a photoaging model. The exposed skin of rats was continuously irradiated for 1 month by 30 W of UVA and UVB ultraviolet lamp placed 30 cm above the cage, each irradiation time was 2 h every two days.
The four photoaging model groups were respectively administrated PBS, 1 mL of 100 μg/mL VD3 solution, VD3 liposomes or 1 mL of aloe-gel twice per day. The rats were continuously treated for 1 month. Apparent properties of the rats’ skin were quantitatively analyzed after treatment using the skin color and scale. And then the four groups of rats were anesthetized and sacrificed to harvest the exposed target skin, the skin was fixed by 4% paraformaldehyde, embedded in paraffin. Finally, the skin tissues were stained by the H&E method to analyze the histology of epidermis, dermis, collagen fibers and elastic fibers.
2.9. Statistical Analysis
A t-test was used to analyze the statistical significance of the data. P values < 0.05 and < 0.01 indicate significant difference and extremely significant difference respectively. The results are shown as mean ± SD.
4. Conclusions
Excessive exposure to sunlight causes skin photoaging. The severity of this complication mainly depends on genetic factors, skin type, and the area of skin exposed to the sun. The skin produces high-level ROS upon UV radiation, which damages skin cells. In addition, UV radiation might directly damage DNA and cause skin cancer.
VD3 was found to have a good protective effect from UV radiation and photoaging. Of course, there are still some remaining issues to be overcome, such as stability and skin uptake of VD3. In 1987, Christian Dior launched the first liposomes cosmetics “Capture”. Since then, this class of cosmetics has received positive attention. About 300 liposomal cosmetics have been commercialized so far. In this study, we prepared VD3 liposomes to prevent photoaging. The VD3 liposomes had high drug EE% and uniform particle size. Liposomes raised the retention amount of VD3 in the skin by transdermal absorption compared to the VD3 solution. Finally, VD3 liposomes could significantly improve skin appearance and repair damage in the histology of photoaging. This suggests that VD3 liposomes warrant further research as a protective agent against photoaging in the skin care field.