Dual Angiotensin Receptor and Neprilysin Inhibitor Ameliorates Portal Hypertension in Portal Hypertensive Rats
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animal Model
2.2. Experimental Design
2.3. Measurement of Systemic and Portal Hemodynamics
2.4. Measurement of Portal Venous and Superior Mesentery Arterial Hemodynamics
2.5. Portal-Systemic Shunting Analysis
2.6. Histopathological and Immunohistochemical Staining of Liver
2.7. Western Blot Analysis for Various Protein Expressions
2.8. Drugs
2.9. Data Analysis
3. Results
3.1. Mortality Rates of Control, Valsartan- and LCZ696-Treated PVL, and Sham-Operated Rats
3.2. Hemodynamic Changes of Sham-Operated and PVL Rats after Valsartan and LCZ696 Treatments
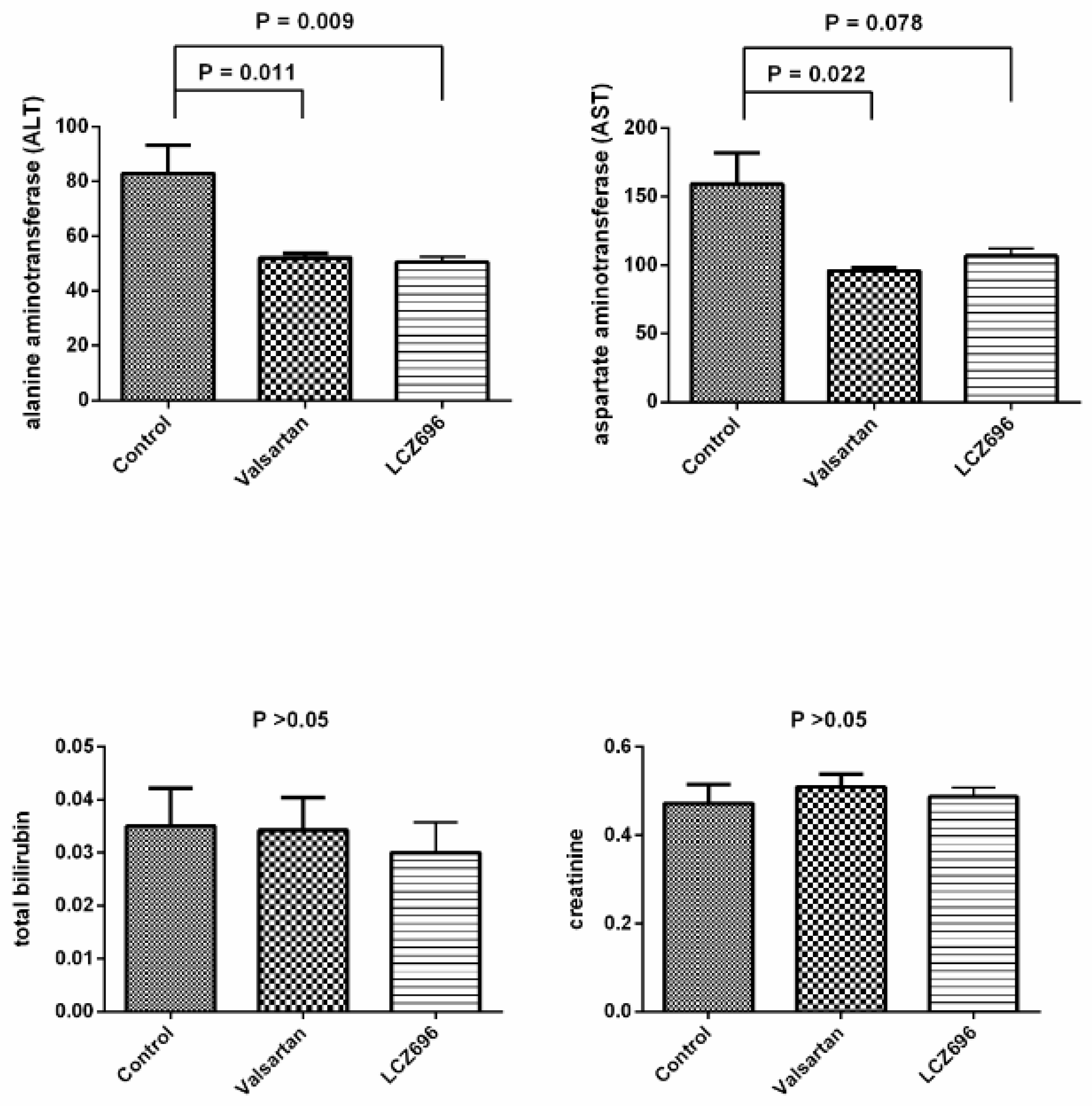
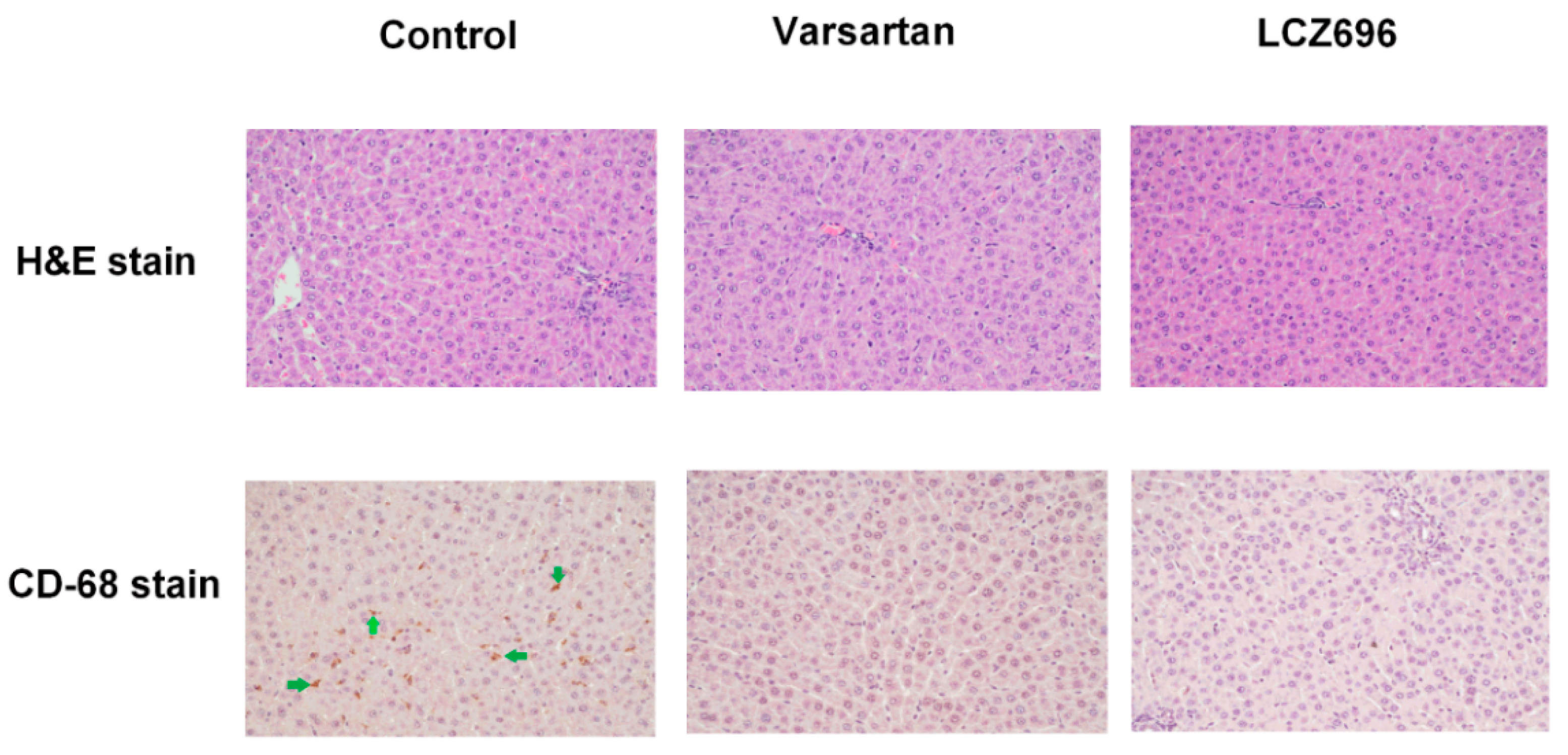
3.3. Effects of Valsartan and LCZ696 Treatment on Biochemistry and Histopathological Changes of Liver in PVL Rats
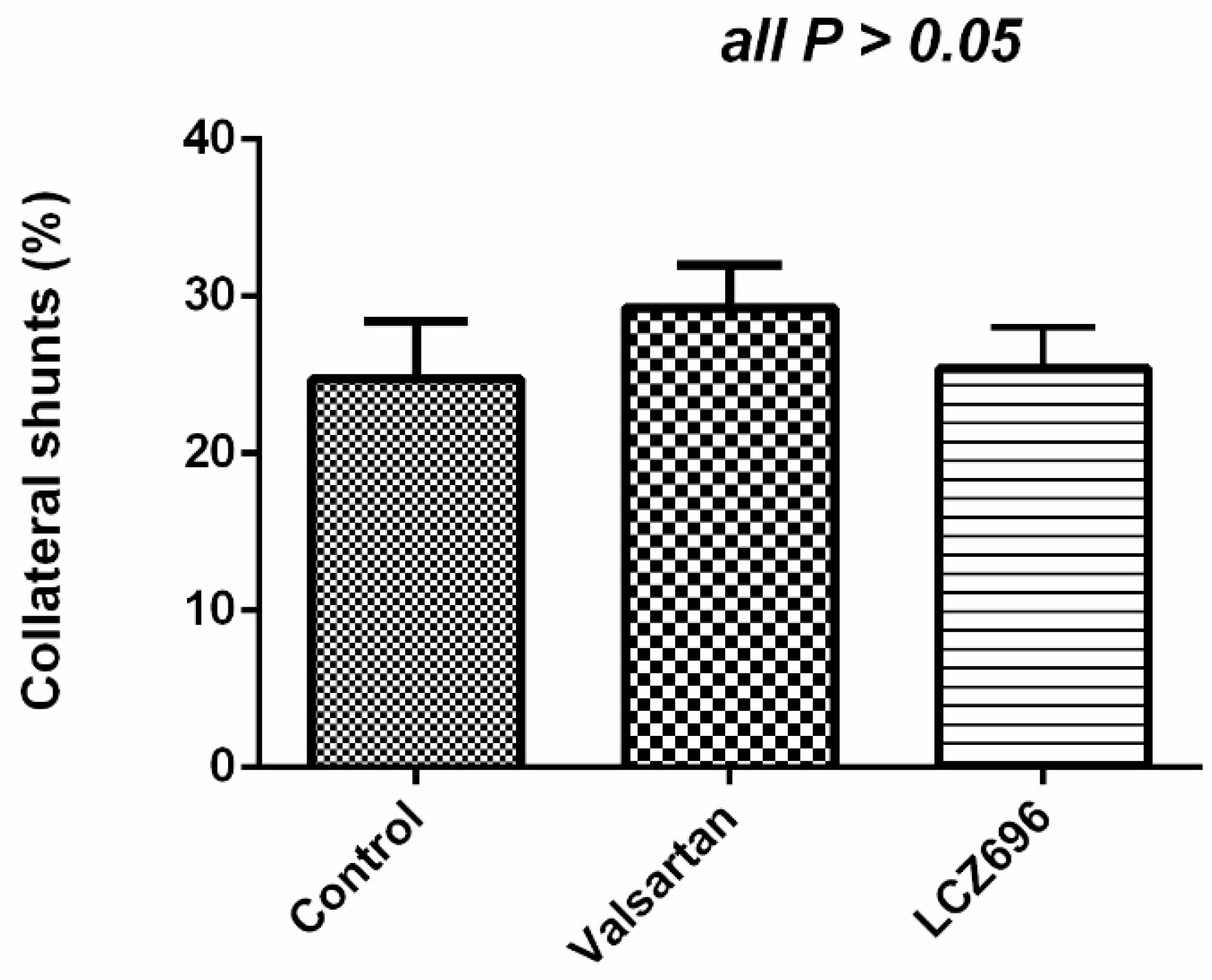
3.4. Portal-Systemic Shunting in the Control (n = 6) and Valsartan- (n = 6) and LCZ696-Treated (n = 6) PVL Rats
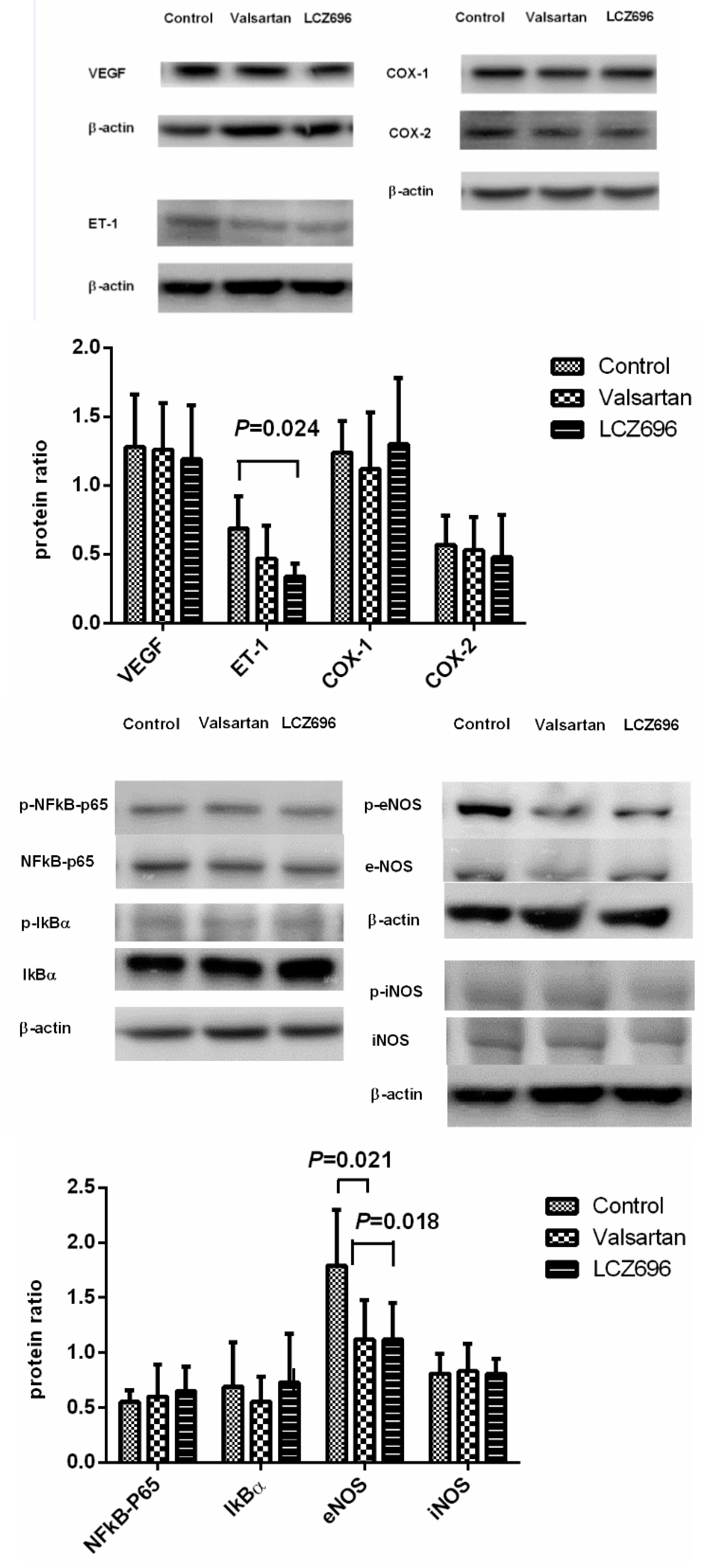
3.5. Protein Expressions in the Liver of PVL Rats Treated by Vehicle (n = 6), Valsartan (n = 8), or LCZ696 (n = 8)
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lubel, J.S.; Angus, P.W. Modern management of portal hypertension. Intern. Med. J. 2005, 35, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Lubel, J.S.; Herath, C.B.; Burrell, L.M.; Angus, P.W. Liver disease and the renin-Angiotensin system: Recent discoveries and clinical implications. J. Gastroenterol. Hepatol. 2008, 23, 1327–1338. [Google Scholar] [CrossRef] [PubMed]
- Tandon, P.; Abraldes, J.G.; Berzigotti, A.; Garcia-Pagan, J.C.; Bosch, J. Renin-Angiotensin-Aldosterone inhibitors in the reduction of portal pressure: A systematic review and meta-Analysis. J. Hepatol. 2010, 53, 273–282. [Google Scholar] [CrossRef]
- Chang, C.C.; Lee, W.S.; Huang, H.C.; Lee, F.Y.; Wang, S.S.; Lin, H.C.; Nong, J.Y.; Lee, S.D. Aliskiren reduces portal pressure in portal hypertensive rats. Eur. J. Clin. Investig. 2012, 42, 526–533. [Google Scholar] [CrossRef] [PubMed]
- Nobakht, N.; Kamgar, M.; Rastogi, A.; Schrier, R.W. Limitations of angiotensin inhibition. Nat. Rev. Nephrol. 2011, 7, 356–359. [Google Scholar] [CrossRef]
- Levin, E.R.; Gardner, D.G.; Samson, W.K. Natriuretic peptides. N. Engl. J. Med. 1998, 30, 321–328. [Google Scholar]
- Ferro, C.J.; Spratt, J.C.; Haynes, W.G.; Webb, D.J. Inhibition of neutral endopeptidase causes vasoconstriction of human resistance vessels in vivo. Circulation 1998, 97, 2323–2330. [Google Scholar] [CrossRef]
- McMurray, J.J.; Packer, M.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.C.; Solomon, S.D.; Swedberg, K.; et al. PARADIGM-HF Investigators and Committees. Angiotensin-Neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 2014, 371, 993–1004. [Google Scholar] [CrossRef] [Green Version]
- Menendez, J.T. The Mechanism of Action of LCZ696. Card Fail Rev. 2016, 2, 40–46. [Google Scholar] [CrossRef] [Green Version]
- Kulmatycki, K.M.; Langenickel, T.; Ng, W.H.; Pal, P.; Zhou, W.; Lin, T.H.; Rajman, I.; Chandra, P.; Sunkara, G. Pharmacokinetics and safety of sacubitril/valsartan (LCZ696) in patients with mild and moderate hepatic impairment. Int. J. Clin. Pharmacol. Ther. 2017, 55, 728–739. [Google Scholar] [CrossRef]
- Shah, V. Cellular and molecular basis of portal hypertension. Clin. Liver. Dis. 2001, 5, 629–644. [Google Scholar] [CrossRef]
- Sansoè, G.; Aragno, M.; Mastrocola, R.; Restivo, F.; Mengozzi, G.; Smedile, A.; Rosina, F.; Danni, O.; Parola, M.; Rizzetto, M. Neutral endopeptidase (EC 3.4.24.11) in cirrhotic liver: A new target to treat portal hypertension? J. Hepatol. 2005, 43, 791–798. [Google Scholar] [CrossRef] [PubMed]
- Moreau, R.; Tazi, K.A.; Komeichi, H.; Pussard, E.; Lebrec, D. Haemodynamic responses to a ring-Deleted analogue of atrial natriuretic peptide in rats with cirrhosis. Liver 2000, 20, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Albillos, A.; Colombato, L.A.; Groszmann, R.J. Vasodilatation and sodium retention in prehepatic portal hypertension. Gastroenterology 1992, 102, 931–935. [Google Scholar] [CrossRef]
- Abraldes, J.G.; Iwakiri, Y.; Loureiro-Silva, M.; Haq, O.; Sessa, W.C.; Groszmann, R.J. Mild increases in portal pressure upregulate vascular endothelial growth factor and endothelial nitric oxide synthase in the intestinal microcirculatory bed, leading to a hyperdynamic state. Am. J. Physiol. 2006, 290, G980–G987. [Google Scholar] [CrossRef] [Green Version]
- Huang, H.C.; Wang, S.S.; Chan, C.C.; Lee, F.Y.; Chang, F.Y.; Lin, H.C.; Hou, M.C.; Tai, C.C.; Lai, I.N.; Lee, S.D. Chronic inhibition of nitric oxide increases the collateral vascular responsiveness to vasopressin in portal hypertensive rats. J. Hepatol. 2004, 40, 234–238. [Google Scholar] [CrossRef]
- Thenappan, T.; Goel, A.; Marsboom, G.; Fang, Y.H.; Toth, P.T.; Zhang, H.J.; Kajimoto, H.; Hong, Z.; Paul, J.; Wietholt, C.; et al. A central role for CD68 (+) macrophages in hepatopulmonary syndrome. Reversal by macrophage depletion. Am. J. Respir. Crit. Care Med. 2011, 183, 1080–1091. [Google Scholar] [CrossRef] [Green Version]
- Chrysant, S.G. Pharmacokinetic, pharmacodynamic, and antihypertensive effects of the neprilysin inhibitor LCZ-696: Sacubitril/valsartan. J. Am. Soc. Hypertens. 2017, 11, 461–468. [Google Scholar] [CrossRef]
- Roksnoer, L.C.; van Veghel, R.; de Vries, R.; Garrelds, I.M.; Bhaggoe, U.M.; Friesema, E.C.; Leijten, F.P.; Poglitsch, M.; Domenig, O.; Clahsen-van Groningen, M.C.; et al. Optimum AT1 receptor-Neprilysin inhibition has superior cardioprotective effects compared with AT1 receptor blockade alone in hypertensive rats. Kidney Int. 2015, 88, 109–120. [Google Scholar] [CrossRef] [Green Version]
- Singh, J.S.S.; Burrell, L.M.; Cherif, M.; Squire, I.B.; Clark, A.L.; Lang, C.C. Sacubitril/valsartan: Beyond natriuretic peptides. Heart 2017, 103, 1569–1577. [Google Scholar] [CrossRef] [Green Version]
- Roksnoer, L.C.W.; Uijl, E.; de Vries, R.; Garrelds, I.M.; Jan Danser, A.H. Neprilysin inhibition and endothelin-1 elevation: Focus on the kidney. Eur. J. Pharmacol. 2018, 824, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Clements, R.T.; Vang, A.; Fernandez-Nicolas, A.; Kue, N.R.; Mancini, T.J.; Morrison, A.R.; Mallem, K.; McCullough, D.J.; Choudhary, G. Treatment of Pulmonary Hypertension with Angiotensin II Receptor Blocker and Neprilysin Inhibitor Sacubitril/Valsartan. Circ. Heart Fail. 2019, 12, e005819. [Google Scholar] [CrossRef] [PubMed]
- Kusaka, H.; Sueta, D.; Koibuchi, N.; Hasegawa, Y.; Nakagawa, T.; Lin, B.; Ogawa, H.; Kim-Mitsuyama, S. LCZ696, Angiotensin II Receptor-Neprilysin Inhibitor, Ameliorates High-Salt-Induced Hypertension and Cardiovascular Injury More Than Valsartan Alone. Am. J. Hypertens. 2015, 28, 1409–1417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seki, T.; Goto, K.; Kansui, Y.; Ohtsubo, T.; Matsumura, K.; Kitazono, T. Angiotensin II Receptor-Neprilysin Inhibitor Sacubitril/Valsartan Improves Endothelial Dysfunction in Spontaneously Hypertensive Rats. J. Am. Heart Assoc. 2017, 6. [Google Scholar] [CrossRef] [Green Version]
- Reichen, J.; Gerbes, A.L.; Steiner, M.J.; Sägesser, H.; Clozel, M. The effect of endothelin and its antagonist Bosentan on hemodynamics and microvascular exchange in cirrhotic rat liver. J. Hepatol. 1998, 28, 1020–1030. [Google Scholar] [CrossRef]
- Lee, K.C.; Yang, Y.Y.; Huang, Y.T.; Lee, F.Y.; Hou, M.C.; Lin, H.C.; Lee, S.D. Administration of a low dose of sildenafil for 1 week decreases intrahepatic resistance in rats with biliary cirrhosis: The role of NO bioavailability. Clin. Sci. (Lond.) 2010, 119, 45–55. [Google Scholar] [CrossRef]
- Clemmesen, J.O.; Giraldi, A.; Ott, P.; Dalhoff, K.; Hansen, B.A.; Larsen, F.S. Sildenafil does not influence hepatic venous pressure gradient in patients with cirrhosis. World J. Gastroenterol. 2008, 14, 6208–6212. [Google Scholar] [CrossRef]
- Chistiakov, D.A.; Killingsworth, M.C.; Myasoedova, V.A.; Orekhov, A.N.; Bobryshev, Y.V. CD68/macrosialin: Not just a histochemical marker. Lab. Investig. 2017, 97, 4–13. [Google Scholar] [CrossRef] [Green Version]
- Liczek, M.; Panek, I.; Damiański, P.; Jęczeń, O.; Jaźwiec, J.; Kuna, P.; Panek, M. Neprilysin inhibitors as a new approach in the treatment of right heart failure in the course of chronic obstructive pulmonary disease. Adv. Respir. Med. 2018. [Google Scholar] [CrossRef] [Green Version]
- Theuer, J.; Dechend, R.; Muller, D.N.; Park, J.K.; Fiebeler, A.; Barta, P.; Ganten, D.; Haller, H.; Dietz, R.; Luft, F.C. Angiotensin II induced inflammation in the kidney and in the heart of double transgenic rats. BMC Cardiovasc. Disord. 2002, 2, 3. [Google Scholar] [CrossRef] [Green Version]
- Guo, C.; Yuan, L.; Liu, X.; Du, A.; Huang, Y.; Zhang, L. Effect of ARB on expression of CD68 and MCP-1 in adipose tissue of rats on long-Term high fat diet. J. Huazhong. Univ. Sci. Technol. Med. Sci. 2008, 28, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, F.; Azuma, K.; Ogihara, T.; Toyofuku, Y.; Otsuka, A.; Mita, T.; Hirose, T.; Tanaka, Y.; Kawamori, R.; Watada, H. Angiotensin II type 1 receptor blocker reduces monocyte adhesion to endothelial cells in spontaneously hypertensive rats. Endocr. J. 2007, 54, 605–612. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jing, W.; Vaziri, N.D.; Nunes, A.; Suematsu, Y.; Farzaneh, T.; Khazaeli, M.; Moradi, H. LCZ696 (Sacubitril/valsartan) ameliorates oxidative stress, inflammation, fibrosis and improves renal function beyond angiotensin receptor blockade in CKD. Am. J. Transl. Res. 2017, 9, 5473–5484. [Google Scholar] [PubMed]
- Habibi, J.; Aroor, A.R.; Das, N.A.; Manrique-Acevedo, C.M.; Johnson, M.S.; Hayden, M.R.; Nistala, R.; Wiedmeyer, C.; Chandrasekar, B.; DeMarco, V.G. The combination of a neprilysin inhibitor (sacubitril) and angiotensin-II receptor blocker (valsartan) attenuates glomerular and tubular injury in the Zucker Obese rat. Cardiovasc. Diabetol. 2019, 18, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uijl, E.; ’t Hart, D.C.; Roksnoer, L.C.W.; Groningen, M.C.C.; van Veghel, R.; Garrelds, I.M.; de Vries, R.; van der Vlag, J.; Zietse, R.; Nijenhuis, T.; et al. Angiotensin-Neprilysin inhibition confers renoprotection in rats with diabetes and hypertension by limiting podocyte injury. J. Hypertens. 2020, 38, 755–764. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, V.T.; Eken, C.; Avci, A.B.; Duman, A.; Tuna, Y.; Akin, M.; Yildirim, B. Relationship of increased serum brain natriuretic peptide levels with hepatic failure, portal hypertension and treatment in patients with cirrhosis. Turk. J. Gastroenterol. 2010, 21, 381–386. [Google Scholar] [CrossRef] [Green Version]
- Koch, A.; Zimmermann, H.W.; Baeck, C.; Schneider, C.; Yagmur, E.; Trautwein, C.; Tacke, F. Serum NT-pro CNP concentrations are elevated in patients with chronic liver diseases and associated with complications and unfavorable prognosis of cirrhosis. Clin. Biochem. 2012, 45, 429–435. [Google Scholar] [CrossRef]
- Jonas, G.M.; Morgan, T.R.; Morgan, K.; Thillainadarajah, I.; Hornacek, C. Atrial natriuretic peptide in portal vein-Ligated rats: Alterations in cardiac production, plasma level and glomerular receptor density and affinity. Hepatology 1992, 15, 696–701. [Google Scholar] [CrossRef]
- Bloom, S.; Kemp, W.; Lubel, J. Portal hypertension: Pathophysiology, diagnosis and management. Intern. Med. J. 2015, 45, 16–26. [Google Scholar] [CrossRef]
- Shmilovich, H.; Ben-Shoshan, J.; Tal, R.; Afek, A.; Barshack, I.; Maysel-Auslander, S.; Harats, D.; Keren, G.; George, J. B-Type natriuretic peptide enhances vasculogenesis by promoting number and functional properties of early endothelial progenitor cells. Tissue Eng. Part A 2009, 15, 2741–2749. [Google Scholar] [CrossRef]
- Doi, K.; Itoh, H.; Komatsu, Y.; Igaki, T.; Chun, T.H.; Takaya, K.; Yamashita, J.; Inoue, M.; Yoshimasa, T.; Nakao, K. Vascular endothelial growth factor suppresses C-type natriuretic peptide secretion. Hypertension 1996, 27 Pt 2, 811–815. [Google Scholar] [CrossRef]
- Almeida, S.A.; Cardoso, C.C.; Orellano, L.A.; Reis, A.M.; Barcelos, L.S.; Andrade, S.P. Natriuretic peptide clearance receptor ligand (C-ANP4-23) attenuates angiogenesis in a murine sponge implant model. Clin. Exp. Pharmacol. Physiol. 2014, 41, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Lara-Castillo, N.; Zandi, S.; Nakao, S.; Ito, Y.; Noda, K.; She, H.; Ahmed, M.; Frimmel, S.; Ablonczy, Z.; Hafezi-Moghadam, A. Atrial natriuretic peptide reduces vascular leakage and choroidal neovascularization. Am. J. Pathol. 2009, 175, 2343–2350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimizu, T.; Okamoto, H.; Chiba, S.; Matsui, Y.; Sugawara, T.; Akino, M.; Nan, J.; Kumamoto, H.; Onozuka, H.; Mikami, T.; et al. VEGF-Mediated angiogenesis is impaired by angiotensin type 1 receptor blockade in cardiomyopathic hamster hearts. Cardiovasc. Res. 2003, 58, 203–212. [Google Scholar] [CrossRef] [Green Version]
- Noguchi, R.; Yoshiji, H.; Ikenaka, Y.; Kaji, K.; Aihara, Y.; Shirai, Y.; Namisaki, T.; Kitade, M.; Douhara, A.; Moriya, K.; et al. Dual blockade of angiotensin-II and aldosterone suppresses the progression of a non-Diabetic rat model of steatohepatitis. Hepatol. Res. 2013, 43, 765–774. [Google Scholar] [CrossRef] [PubMed]
| Control (n = 6) | Valsartan (n = 5) | LCZ696 (n = 5) | |
|---|---|---|---|
| BW (g) | 356 ± 26 | 367 ± 8 | 367 ± 26 |
| MAP (mmHg) | 145 ± 11 | 121 ± 19 * | 104 ± 15 * |
| PP (mmHg) | 10.4 ± 0.6 | 8.8 ± 2.2 | 9.5 ± 1.1 |
| HR (beats/min) | 352 ± 23 | 359 ± 41 | 353 ± 24 |
| PVf (mL/min/100 g) | 9.8 ± 0.9 | 9.8 ± 4.1 | 8.1 ± 1.6 |
| SMAf (mL/min/100 g) | 6.2 ± 1.1 | 5.4 ± 1.0 | 6.0 ± 1.5 |
| SMAR(mmHg/mL/min/100 g) | 22.6 ± 5.9 | 21.4 ± 6.0 | 16.4 ± 3.8 |
| SVR (mmHg/mL/min/100 g) | 3.9 ± 0.4 | 3.2 ± 0.6 # | 2.7 ± 0.5 * |
| CI (mL/min/100 g) | 37.6 ± 4.4 | 38.8 ± 6.0 | 39.2 ± 7.9 |
| Control (n = 5) | Valsartan (n = 7) | LCZ696 (n = 7) | |
|---|---|---|---|
| BW (g) | 304 ± 20 | 285 ± 16 | 287 ± 30 |
| MAP (mmHg) | 126 ± 5 | 103 ± 16 * | 90 ± 12 * |
| PP (mmHg) | 15.4 ± 1.6 | 14.0 ± 2.3 | 12.0 ± 2.0 * |
| HR (beats/min) | 323 ± 26 | 349 ± 27 | 325 ± 47 |
| PVf (mL/min/100 g) | 3.4 ± 1.4 | 4.8 ± 2.1 | 4.4 ± 1.9 |
| SMAf (mL/min/100 g) | 6.0 ± 0.6 | 7.9 ± 2.7 | 7.3 ± 1.8 |
| SMAR (mmHg/mL/min/100 g) | 18.6 ± 1.8 | 12.9 ± 5.7 | 11.3 ± 3.6 * |
| SVR (mmHg/mL/min/100 g) | 3.9 ± 0.4 | 2.7 ± 1.1 * | 2.3 ± 0.5 * |
| CI (mL/min/100 g) | 32.5 ± 3.6 | 41.2 ± 11.3 | 39.6 ± 5.7 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, S.-J.; Huang, H.-C.; Chuang, C.-L.; Chang, C.-C.; Hou, M.-C.; Lee, F.-Y.; Lee, S.-D. Dual Angiotensin Receptor and Neprilysin Inhibitor Ameliorates Portal Hypertension in Portal Hypertensive Rats. Pharmaceutics 2020, 12, 320. https://doi.org/10.3390/pharmaceutics12040320
Hsu S-J, Huang H-C, Chuang C-L, Chang C-C, Hou M-C, Lee F-Y, Lee S-D. Dual Angiotensin Receptor and Neprilysin Inhibitor Ameliorates Portal Hypertension in Portal Hypertensive Rats. Pharmaceutics. 2020; 12(4):320. https://doi.org/10.3390/pharmaceutics12040320
Chicago/Turabian StyleHsu, Shao-Jung, Hui-Chun Huang, Chiao-Lin Chuang, Ching-Chih Chang, Ming-Chih Hou, Fa-Yauh Lee, and Shou-Dong Lee. 2020. "Dual Angiotensin Receptor and Neprilysin Inhibitor Ameliorates Portal Hypertension in Portal Hypertensive Rats" Pharmaceutics 12, no. 4: 320. https://doi.org/10.3390/pharmaceutics12040320





