Multifaceted Factors Causing Conflicting Outcomes in Herb-Drug Interactions
Abstract
1. Introduction
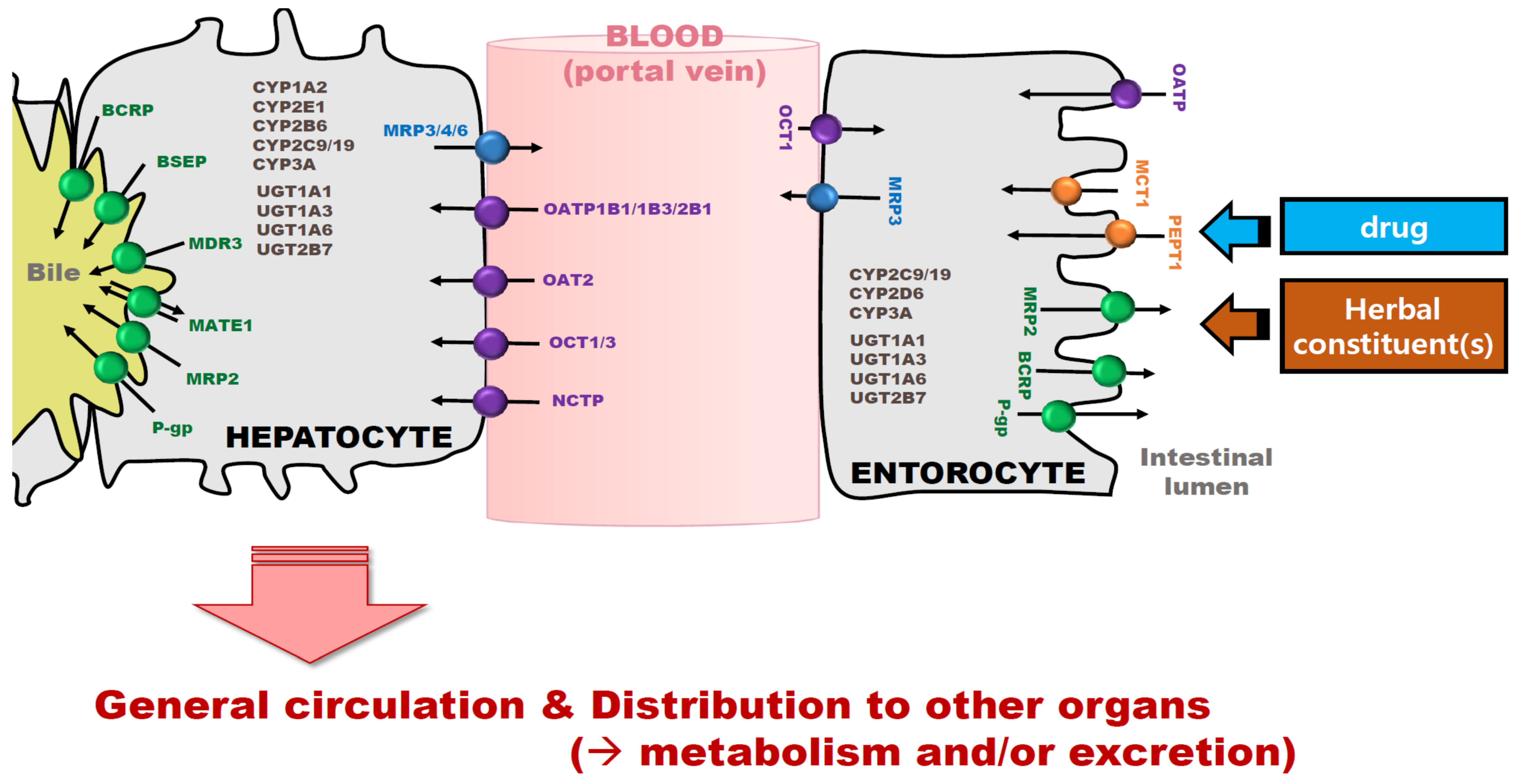
2. Main Pathways Causing HDIs: Metabolic Enzyme- and Transporter-Mediated HDIs
3. Challenging Issues in the Evaluation and Interpretation of PK-Based HDIs
3.1. The Complex Nature of Herbal Products
3.2. Responses of a Drug’s or Herbal Product’s Exposure to Different Assay Systems
3.3. Multifaceted Factors in Study Designs (E.g., Administration Route, Dose, Treatment Period, Etc.)
4. Future Perspectives and Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roe, A.L.; McMillan, D.A.; Mahony, C. A Tiered Approach for the Evaluation of the Safety of Botanicals Used as Dietary Supplements: An Industry Strategy. Clin. Pharmacol. Ther. 2018, 104, 446–457. [Google Scholar] [CrossRef]
- Meng, Q.; Liu, K. Pharmacokinetic interactions between herbal medicines and prescribed drugs: Focus on drug metabolic enzymes and transporters. Curr. Drug Metab. 2014, 15, 791–807. [Google Scholar] [CrossRef]
- Grimstein, M.; Huang, S.M. A regulatory science viewpoint on botanical-drug interactions. J. Food Drug Anal. 2018, 26, S12–S25. [Google Scholar] [CrossRef]
- Tsai, H.H.; Lin, H.W.; Simon Pickard, A.; Tsai, H.Y.; Mahady, G.B. Evaluation of documented drug interactions and contraindications associated with herbs and dietary supplements: A systematic literature review. Int. J. Clin. Pract. 2012, 66, 1056–1078. [Google Scholar] [CrossRef]
- Haefeli, W.E.; Carls, A. Drug interactions with phytotherapeutics in oncology. Expert Opin. Drug Metab. Toxicol. 2014, 10, 359–377. [Google Scholar] [CrossRef]
- Fasinu, P.S.; Gurley, B.J.; Walker, L.A. Clinically Relevant Pharmacokinetic Herb-drug Interactions in Antiretroviral Therapy. Curr. Drug Metab. 2015, 17, 52–64. [Google Scholar] [CrossRef]
- Dechanont, S.; Maphanta, S.; Butthum, B.; Kongkaew, C. Hospital admissions/visits associated with drug-drug interactions: A systematic review and meta-analysis. Pharmacoepidemiol. Drug Saf. 2014, 23, 489–497. [Google Scholar] [CrossRef]
- Huang, S.M.; Strong, J.M.; Zhang, L.; Reynolds, K.S.; Nallani, S.; Temple, R.; Abraham, S.; Habet, S.A.; Baweja, R.K.; Burckart, G.J.; et al. New era in drug interaction evaluation: US Food and Drug Administration update on CYP enzymes, transporters, and the guidance process. J. Clin. Pharmacol. 2008, 48, 662–670. [Google Scholar] [CrossRef]
- Choi, Y.H. Interpretation of Drug Interaction Using Systemic and Local Tissue Exposure Changes. Pharmaceutics 2020, 12, 417. [Google Scholar] [CrossRef]
- Yu, J.J.; Zhou, Z.; Tay-Sontheimer, J.; Levy, R.H.; Ragueneau-Majlessi, I. Intestinal Drug Interactions Mediated by OATPs: A Systematic Review of Preclinical and Clinical Findings. J. Pharm. Sci. 2017, 106, 2312–2325. [Google Scholar] [CrossRef]
- Yoshida, K.; Zhao, P.; Zhang, L.; Abernethy, D.R.; Rekic, D.; Reynolds, K.S.; Galetin, A.; Huang, S.M. In Vitro-In Vivo Extrapolation of Metabolism- and Transporter-Mediated Drug-Drug Interactions-Overview of Basic Prediction Methods. J. Pharm. Sci. 2017, 106, 2209–2213. [Google Scholar] [CrossRef] [PubMed]
- Brantley, S.J.; Argikar, A.A.; Lin, Y.S.; Nagar, S.; Paine, M.F. Herb-drug interactions: Challenges and opportunities for improved predictions. Drug Metab. Dispos. 2014, 42, 301–317. [Google Scholar] [CrossRef] [PubMed]
- Houston, J.B.; Galetin, A. Methods for predicting in vivo pharmacokinetics using data from in vitro assays. Curr. Drug Metab. 2008, 9, 940–951. [Google Scholar] [CrossRef] [PubMed]
- De Smet, P.A.; Floor-Schreudering, A.; Bouvy, M.L.; Wensing, M. Clinical risk management of interactions between natural products and drugs. Curr. Drug Metab. 2008, 9, 1055–1062. [Google Scholar] [CrossRef] [PubMed]
- Ma, B.L.; Ma, Y.M. Pharmacokinetic herb-drug interactions with traditional Chinese medicine: Progress, causes of conflicting results and suggestions for future research. Drug Metab. Rev. 2016, 48, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wu, W.Y.; Jiang, B.H.; Yang, M.; Guo, D.A. Pharmacological tools for the development of traditional Chinese medicine. Trends Pharmacol. Sci. 2013, 34, 620–628. [Google Scholar] [CrossRef] [PubMed]
- Tornio, A.; Filppula, A.M.; Niemi, M.; Backman, J.T. Clinical Studies on Drug-Drug Interactions Involving Metabolism and Transport: Methodology, Pitfalls, and Interpretation. Clin Pharmacol. Ther. 2019, 105, 1345–1361. [Google Scholar] [CrossRef]
- Gessner, A.; Konig, J.; Fromm, M.F. Clinical Aspects of Transporter-Mediated Drug-Drug Interactions. Clin Pharmacol. Ther. 2019, 105, 1386–1394. [Google Scholar] [CrossRef]
- Yu, J.; Petrie, I.D.; Levy, R.H.; Ragueneau-Majlessi, I. Mechanisms and Clinical Significance of Pharmacokinetic-Based Drug-Drug Interactions with Drugs Approved by the U.S. Food and Drug Administration in 2017. Drug Metab. Dispos. 2019, 47, 135–144. [Google Scholar] [CrossRef]
- Hermann, R.; von Richter, O. Clinical evidence of herbal drugs as perpetrators of pharmacokinetic drug interactions. Planta Med. 2012, 78, 1458–1477. [Google Scholar] [CrossRef]
- Sun, S.; Wang, Y.; Wu, A.; Ding, Z.; Liu, X. Influence Factors of the Pharmacokinetics of Herbal Resourced Compounds in Clinical Practice. Evid. Based Complement. Altern. Med. 2019, 2019, 1983780. [Google Scholar] [CrossRef] [PubMed]
- Sprouse, A.A.; van Breemen, R.B. Pharmacokinetic Interactions between Drugs and Botanical Dietary Supplements. Drug Metab. Dispos. 2016, 44, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Stieger, B.; Mahdi, Z.M.; Jager, W. Intestinal and Hepatocellular Transporters: Therapeutic Effects and Drug Interactions of Herbal Supplements. Annu. Rev. Pharmacol. Toxicol. 2017, 57, 399–416. [Google Scholar] [CrossRef] [PubMed]
- Shitara, Y.; Horie, T.; Sugiyama, Y. Transporters as a determinant of drug clearance and tissue distribution. Eur. J. Pharm. Sci. 2006, 27, 425–446. [Google Scholar] [CrossRef] [PubMed]
- Shitara, Y.; Maeda, K.; Ikejiri, K.; Yoshida, K.; Horie, T.; Sugiyama, Y. Clinical significance of organic anion transporting polypeptides (OATPs) in drug disposition: Their roles in hepatic clearance and intestinal absorption. Biopharm. Drug Dispos. 2013, 34, 45–78. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.A.; Di, L.; Kerns, E.H. The effect of plasma protein binding on in vivo efficacy: Misconceptions in drug discovery. Nat. Rev. Drug Discov. 2010, 9, 929–939. [Google Scholar] [CrossRef]
- Fuhr, U.; Hsin, C.H.; Li, X.; Jabrane, W.; Sorgel, F. Assessment of Pharmacokinetic Drug-Drug Interactions in Humans: In Vivo Probe Substrates for Drug Metabolism and Drug Transport Revisited. Annu. Rev. Pharmacol. Toxicol. 2019, 59, 507–536. [Google Scholar] [CrossRef]
- Han, H.K. Role of transporters in drug interactions. Arch. Pharm. Res. 2011, 34, 1865–1877. [Google Scholar] [CrossRef]
- Han, S.Y.; Chae, H.S.; You, B.H.; Chin, Y.W.; Kim, H.; Choi, H.S.; Choi, Y.H. Lonicera japonica extract increases metformin distribution in the liver without change of systemic exposed metformin in rats. J. Ethnopharmacol. 2019, 238, 111892. [Google Scholar] [CrossRef]
- You, B.H.; Chin, Y.W.; Kim, H.; Choi, H.S.; Choi, Y.H. Houttuynia cordata extract increased systemic exposure and liver concentrations of metformin through OCTs and MATEs in rats. Phytother. Res. 2018, 32, 1004–1013. [Google Scholar] [CrossRef]
- Andersson, T.B.; Bredberg, E.; Ericsson, H.; Sjoberg, H. An evaluation of the in vitro metabolism data for predicting the clearance and drug-drug interaction potential of CYP2C9 substrates. Drug Metab. Dispos. 2004, 32, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Gurley, B.J.; Gardner, S.F.; Hubbard, M.A.; Williams, D.K.; Gentry, W.B.; Khan, I.A.; Shah, A. In vivo effects of goldenseal, kava kava, black cohosh, and valerian on human cytochrome P450 1A2, 2D6, 2E1, and 3A4/5 phenotypes. Clin. Pharmacol. Ther. 2005, 77, 415–426. [Google Scholar] [CrossRef]
- Komoroski, B.J.; Zhang, S.; Cai, H.; Hutzler, J.M.; Frye, R.; Tracy, T.S.; Strom, S.C.; Lehmann, T.; Ang, C.Y.; Cui, Y.Y.; et al. Induction and inhibition of cytochromes P450 by the St. John’s wort constituent hyperforin in human hepatocyte cultures. Drug Metab. Dispos. 2004, 32, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Lu, J.; Paxton, J.W. The Role of ABC and SLC Transporters in the Pharmacokinetics of Dietary and Herbal Phytochemicals and their Interactions with Xenobiotics. Curr. Drug Metab. 2012, 13, 624–639. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.J.; Yoon, I.S. Pharmacokinetic interactions of herbs with cytochrome p450 and p-glycoprotein. Evid. Based Complement. Altern. Med. 2015, 2015, 736431. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Shin, S.; Yoo, S.D.; Shin, B.S. Effects of Phytochemical P-Glycoprotein Modulators on the Pharmacokinetics and Tissue Distribution of Doxorubicin in Mice. Molecules 2018, 23, 349. [Google Scholar] [CrossRef] [PubMed]
- Thu, O.K.; Spigset, O.; Nilsen, O.G.; Hellum, B. Effect of commercial Rhodiola rosea on CYP enzyme activity in humans. Eur. J. Clin. Pharmacol. 2016, 72, 295–300. [Google Scholar] [CrossRef]
- Spanakis, M.; Vizirianakis, I.S.; Batzias, G.; Niopas, I. Pharmacokinetic Interaction between Losartan and Rhodiola rosea in Rabbits. Pharmacology 2013, 91, 112–116. [Google Scholar] [CrossRef]
- De Lima Toccafondo Vieira, M.; Huang, S.M. Botanical-drug interactions: A scientific perspective. Planta Med. 2012, 78, 1400–1415. [Google Scholar] [CrossRef]
- Izzo, A.A.; Hoon-Kim, S.; Radhakrishnan, R.; Williamson, E.M. A Critical Approach to Evaluating Clinical Efficacy, Adverse Events and Drug Interactions of Herbal Remedies. Phytother. Res. 2016, 30, 691–700. [Google Scholar] [CrossRef]
- Chang, W.T.; Thissen, U.; Ehlert, K.A.; Koek, M.M.; Jellema, R.H.; Hankemeier, T.; van der Greef, J.; Wang, M. Effects of growth conditions and processing on Rehmannia glutinosa using fingerprint strategy. Planta Med. 2006, 72, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.X.; Yi, X.L.; Si, D.Y.; Xiao, X.F.; He, X.; Li, Y.Z. Herb-drug interactions involving drug metabolizing enzymes and transporters. Curr. Drug Metab. 2011, 12, 835–849. [Google Scholar] [CrossRef] [PubMed]
- Tilton, R.; Paiva, A.A.; Guan, J.Q.; Marathe, R.; Jiang, Z.; van Eyndhoven, W.; Bjoraker, J.; Prusoff, Z.; Wang, H.; Liu, S.H.; et al. A comprehensive platform for quality control of botanical drugs (PhytomicsQC): A case study of Huangqin Tang (HQT) and PHY906. Chin. Med. 2010, 5, 30. [Google Scholar] [CrossRef] [PubMed]
- Krochmal, R.; Hardy, M.; Bowerman, S.; Lu, Q.Y.; Wang, H.J.; Elashoff, R.; Heber, D. Phytochemical Assays of Commercial Botanical Dietary Supplements. Evid. Based Complement. Altern. Med. 2004, 1, 305–313. [Google Scholar] [CrossRef]
- Izzo, A.A. Interactions between Herbs and Conventional Drugs: Overview of the Clinical Data. Med. Princ. Pract. 2012, 21, 404–428. [Google Scholar] [CrossRef]
- Zhou, S.; Huang, M.; Xu, A.; Yang, H.; Duan, W.; Paxton, J.W. Prediction of herb-drug metabolic interactions: A simulation study. Phytother. Res. 2005, 19, 464–471. [Google Scholar] [CrossRef]
- Ko, R.J. A U.S. perspective on the adverse reactions from traditional Chinese medicines. J. Chin. Med. Assoc. 2004, 67, 109–116. [Google Scholar]
- Brandon, E.F.; Raap, C.D.; Meijerman, I.; Beijnen, J.H.; Schellens, J.H. An update on in vitro test methods in human hepatic drug biotransformation research: Pros and cons. Toxicol. Appl. Pharmacol. 2003, 189, 233–246. [Google Scholar] [CrossRef]
- Jaiswal, S.; Sharma, A.; Shukla, M.; Vaghasiya, K.; Rangaraj, N.; Lal, J. Novel pre-clinical methodologies for pharmacokinetic drug-drug interaction studies: Spotlight on "humanized’’ animal models. Drug Metab. Rev. 2014, 46, 475–493. [Google Scholar] [CrossRef]
- Plant, N. Strategies for using in vitro screens in drug metabolism. Drug Discov. Today 2004, 9, 328–336. [Google Scholar] [CrossRef]
- Bun, S.S.; Voeurng, V.; Bun, H. Interspecies variability and drug interactions of loxapine metabolism in liver microsomes. Eur. J. Drug Metab. Pharmacokinet. 2003, 28, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Wang, D.D.; Ge, G.B.; Wang, X.L.; Liu, Y.; Yang, L. Ginsenoside Metabolites Inhibit P-Glycoprotein In Vitro and In Situ Using Three Absorption Models. Planta Med. 2014, 80, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhang, J.W.; Li, W.; Ma, H.; Sun, J.; Deng, M.C.; Yang, L. Ginsenoside metabolites, rather than naturally occurring ginsenosides, lead to inhibition of human cytochrome P450 enzymes. Toxicol. Sci. 2006, 91, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Richert, L.; Tuschl, G.; Viollon-Abadie, C.; Blanchard, N.; Bonet, A.; Heyd, B.; Halkic, N.; Wimmer, E.; Dolgos, H.; Mueller, S.O. Species differences in the response of liver drug-metabolizing enzymes to (S)-4-O-tolylsulfanyl-2-(4-trifluormethyl-phenoxy)-butyric acid (EMD 392949) in vivo and in vitro. Drug Metab. Dispos. 2008, 36, 702–714. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Lechon, M.J.; Donato, T.; Ponsoda, X.; Castell, J.V. Human hepatic cell cultures: In vitro and in vivo drug metabolism. Altern. Lab. Anim. 2003, 31, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Xia, C.Q.; Xiao, G.; Liu, N.; Pimprale, S.; Fox, L.; Patten, C.J.; Crespi, C.L.; Miwa, G.; Gan, L.S. Comparison of species differences of P-glycoproteins in beagle dog, rhesus monkey, and human using Atpase activity assays. Mol. Pharm. 2006, 3, 78–86. [Google Scholar] [CrossRef]
- Tahara, H.; Kusuhara, H.; Endou, H.; Koepsell, H.; Imaoka, T.; Fuse, E.; Sugiyama, Y. A species difference in the transport activities of H2 receptor antagonists by rat and human renal organic anion and cation transporters. J. Pharmacol. Exp. Ther. 2005, 315, 337–345. [Google Scholar] [CrossRef]
- Rombola, L.; Scuteri, D.; Marilisa, S.; Watanabe, C.; Morrone, L.A.; Bagetta, G.; Corasaniti, M.T. Pharmacokinetic Interactions between Herbal Medicines and Drugs: Their Mechanisms and Clinical Relevance. Life-Basel 2020, 10, 106. [Google Scholar] [CrossRef]
- Zhao, Q.; Luan, X.; Zheng, M.; Tian, X.H.; Zhao, J.; Zhang, W.D.; Ma, B.L. Synergistic Mechanisms of Constituents in Herbal Extracts during Intestinal Absorption: Focus on Natural Occurring Nanoparticles. Pharmaceutics 2020, 12, 128. [Google Scholar] [CrossRef]
- van Waterschoot, R.A.; Rooswinkel, R.W.; Sparidans, R.W.; van Herwaarden, A.E.; Beijnen, J.H.; Schinkel, A.H. Inhibition and stimulation of intestinal and hepatic CYP3A activity: Studies in humanized CYP3A4 transgenic mice using triazolam. Drug Metab. Dispos. 2009, 37, 2305–2313. [Google Scholar] [CrossRef]
- Yoshioka, M.; Ohnishi, N.; Sone, N.; Egami, S.; Takara, K.; Yokoyama, T.; Kuroda, K. Studies on interactions between functional foods or dietary supplements and medicines. III. Effects of ginkgo biloba leaf extract on the pharmacokinetics of nifedipine in rats. Biol. Pharm. Bull. 2004, 27, 2042–2045. [Google Scholar] [CrossRef] [PubMed]
- Chiang, H.M.; Chao, P.D.; Hsiu, S.L.; Wen, K.C.; Tsai, S.Y.; Hou, Y.C. Ginger significantly decreased the oral bioavailability of cyclosporine in rats. Am. J. Chin. Med. 2006, 34, 845–855. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, N.; Yamaguchi, Y.; Hou, X.L.; Takahashi, K.; Takahashi, K. Experimental Adjustment on Drug Interactions through Intestinal CYP3A Activity in Rat: Impacts of Kampo Medicines Repeat Administered. Evid. Based Complement. Altern. Med. 2011, 2011, 827435. [Google Scholar] [CrossRef] [PubMed]
- Lai, L.; Hao, H.; Wang, Q.; Zheng, C.; Zhou, F.; Liu, Y.; Wang, Y.; Yu, G.; Kang, A.; Peng, Y.; et al. Effects of short-term and long-term pretreatment of Schisandra lignans on regulating hepatic and intestinal CYP3A in rats. Drug Metab. Dispos. 2009, 37, 2399–2407. [Google Scholar] [CrossRef]
- Zhang, W.; Tan, T.M.; Lim, L.Y. Impact of curcumin-induced changes in P-glycoprotein and CYP3A expression on the pharmacokinetics of peroral celiprolol and midazolam in rats. Drug Metab. Dispos. 2007, 35, 110–115. [Google Scholar] [CrossRef]
- Deng, Y.; Bi, H.C.; Zhao, L.Z.; Wang, X.D.; Chen, J.; Ou, Z.M.; Ding, L.; Xu, L.J.; Guan, S.; Chen, X.; et al. Induction of cytochrome P450 3A by the Ginkgo biloba extract and bilobalides in human and rat primary hepatocytes. Drug Metab. Lett. 2008, 2, 60–66. [Google Scholar] [CrossRef]
- Deng, Y.; Bi, H.C.; Zhao, L.Z.; He, F.; Liu, Y.Q.; Yu, J.J.; Ou, Z.M.; Ding, L.; Chen, X.; Huang, Z.Y.; et al. Induction of cytochrome P450s by terpene trilactones and flavonoids of the Ginkgo biloba extract EGb 761 in rats. Xenobiotica 2008, 38, 465–481. [Google Scholar] [CrossRef]
- Zhao, L.Z.; Huang, M.; Chen, J.; Ee, P.L.; Chan, E.; Duan, W.; Guan, Y.Y.; Hong, Y.H.; Chen, X.; Zhou, S. Induction of propranolol metabolism by Ginkgo biloba extract EGb 761 in rats. Curr. Drug Metab. 2006, 7, 577–587. [Google Scholar] [CrossRef]
- Gyamfi, M.A.; Hokama, N.; Oppong-Boachie, K.; Aniya, Y. Inhibitory effects of the medicinal herb, Thonningia sanguinea, on liver drug metabolizing enzymes of rats. Hum. Exp. Toxicol. 2000, 19, 623–631. [Google Scholar] [CrossRef]
- Zuber, R.; Modriansky, M.; Dvorak, Z.; Rohovsky, P.; Ulrichova, J.; Simanek, V.; Anzenbacher, P. Effect of silybin and its congeners on human liver microsomal cytochrome P450 activities. Phytother. Res. 2002, 16, 632–638. [Google Scholar] [CrossRef]
- Hellum, B.H.; Hu, Z.; Nilsen, O.G. Trade herbal products and induction of CYP2C19 and CYP2E1 in cultured human hepatocytes. Basic Clin. Pharmacol. Toxicol. 2009, 105, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Chien, C.F.; Wu, Y.T.; Lee, W.C.; Lin, L.C.; Tsai, T.H. Herb-drug interaction of Andrographis paniculata extract and andrographolide on the pharmacokinetics of theophylline in rats. Chem. Biol. Interact. 2010, 184, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Sahu, R.; Ahmed, T.; Sangana, R.; Punde, R.; Subudhi, B.B. Effect of Tinospora cordifolia aqua-alcoholic extract on pharmacokinetic of Glibenclamide in rat: An herb-drug interaction study. J. Pharm. Biomed. Anal. 2018, 151, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Paolini, M.; Barillari, J.; Broccoli, M.; Pozzetti, L.; Perocco, P.; Cantelli-Forti, G. Effect of liquorice and glycyrrhizin on rat liver carcinogen metabolizing enzymes. Cancer Lett. 1999, 145, 35–42. [Google Scholar] [CrossRef]
- Ohnishi, N.; Kusuhara, M.; Yoshioka, M.; Kuroda, K.; Soga, A.; Nishikawa, F.; Koishi, T.; Nakagawa, M.; Hori, S.; Matsumoto, T.; et al. Studies on interactions between functional foods or dietary supplements and medicines. I. Effects of Ginkgo biloba leaf extract on the pharmacokinetics of diltiazem in rats. Biol. Pharm. Bull. 2003, 26, 1315–1320. [Google Scholar] [CrossRef][Green Version]
- Kubota, Y.; Kobayashi, K.; Tanaka, N.; Nakamura, K.; Kunitomo, M.; Umegaki, K.; Shinozuka, K. Pretreatment with Ginkgo biloba extract weakens the hypnosis action of phenobarbital and its plasma concentration in rats. J. Pharm. Pharmacol. 2004, 56, 401–405. [Google Scholar] [CrossRef]
- Shi, S.; Klotz, U. Drug interactions with herbal medicines. Clin. Pharmacokinet. 2012, 51, 77–104. [Google Scholar] [CrossRef]
- He, L.; Liu, G.Q. Effects of various principles from Chinese herbal medicine on rhodamine123 accumulation in brain capillary endothelial cells. Acta Pharmacol. Sin. 2002, 23, 591–596. [Google Scholar]
- Ma, B.L.; Ma, Y.M.; Shi, R.; Wang, T.M.; Zhang, N.; Wang, C.H.; Yang, Y. Identification of the toxic constituents in Rhizoma Coptidis. J. Ethnopharmacol. 2010, 128, 357–364. [Google Scholar] [CrossRef]
- Garcia-Fuente, A.; Vazquez, F.; Vieitez, J.M.; Garcia Alonso, F.J.; Martin, J.I.; Ferrer, J. CISNE: An accurate description of dose-effect and synergism in combination therapies. Sci. Rep. 2018, 8, 4964. [Google Scholar] [CrossRef]
- Caesar, L.K.; Cech, N.B. Synergy and antagonism in natural product extracts: When 1 + 1 does not equal 2. Nat. Prod. Rep. 2019, 36, 869–888. [Google Scholar] [CrossRef] [PubMed]
- Roell, K.R.; Reif, D.M.; Motsinger-Reif, A.A. An Introduction to Terminology and Methodology of Chemical Synergy-Perspectives from Across Disciplines. Front. Pharmacol. 2017, 8, 158. [Google Scholar] [CrossRef] [PubMed]
- Qian, Y.; Ye, X.; Du, W.; Ren, J.; Sun, Y.; Wang, H.; Luo, B.; Gao, Q.; Wu, M.; He, J. A computerized system for detecting signals due to drug-drug interactions in spontaneous reporting systems. Br. J. Clin. Pharmacol. 2010, 69, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Sim, S.N.; Levine, M.A. An evaluation of pharmacist and health food store retailer’s knowledge regarding potential drug interactions associated with St. John’s wort. Can. J. Clin. Pharmacol. 2010, 17, e57–e63. [Google Scholar]
- De Smet, P.A. Clinical risk management of herb-drug interactions. Br. J. Clin. Pharmacol. 2007, 63, 258–267. [Google Scholar] [CrossRef]
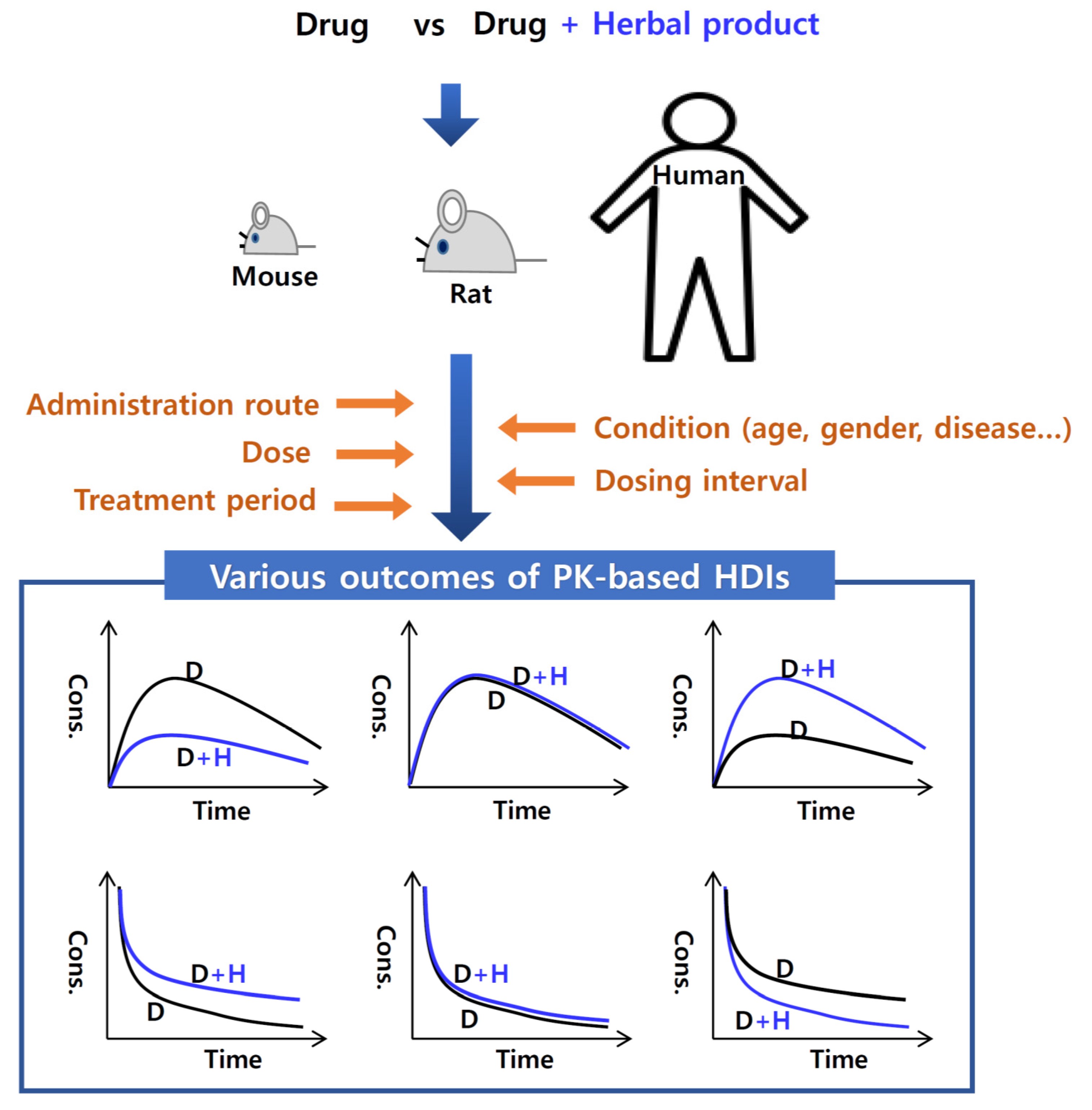
| Factors | Herbal Products | HDI Results | PK-Based HDI Mechanism | Ref |
|---|---|---|---|---|
| Administration route | Ginkgo biloba leaf extract (oral, p.o.) | G. biloba leaf extract only alters the PK of orally, but not intravenously, administered nifedipine in rats | Due to inhibition of CYP3A in intestine, not in liver | [61] |
| Zingiber officinale root juice (p.o.) | Z. officinale juice decreases the oral bioavailability of cyclosporine, but the PK property of intravenous cyclosporine is not altered in rats | Due to inhibition of CYP3A and P-gp in intestine, not in liver | [62] | |
| Echinacea purpurea root (p.o.) | E. purpurea root extract reduced systemic clearance of midazolam following intravenous administration, but oral clearance of midazolam was not altered in rats | Due to inhibition of CYP3A in liver, not in intestine | [77] | |
| Ginseng berry extract (p.o.) | Ginseng berry extract did not affect the PK properties of intravenous administered nifedipine or cyclosporin, but markedly increased the absolute bioavailability of both drugs after oral administration in rats | Due to inhibition of CYP3A in intestine, not in liver | [77] | |
| Schisandra chinensis fruit (p.o.) | S. chinensis fruit extract increased AUC and Cmax of orally administered midazolam, but there was no little change in the PK properties of intravenously administered midazolam in rats | Due to intensive inhibitory effect on CYP3A in intestine, not in liver | [64] | |
| Dose | Andrographis paniculata extract (p.o.) | Low dose of Andrographis Herba extract increases theophylline elimination, whereas high-dose of A. paniculata extract decreases theophylline elimination | Due to induction of CYP1A2 by low-dose treatment of A. paniculata extract, but inhibition of CYP1A2 by its high-dose treatment | [72] |
| Tinospora cordifolia aqueous-alcoholic extract (p.o.) | High-dose of T. cordifolia aqueous-alcoholic extract, not low-dose, reduced the clearance and increased bioavailability of glibenclamide, respectively, in rats | Due to the inhibition of CYP2C9, 2D6 and 3A4 in liver by high-dose of T. cordifolia aqua-alcoholic extract, not low-dose | [73] | |
| Treatment period | S. chinensis fruit extract (p.o.) | Long-term treatment of S. chinensis fruit extract reduced AUC and Cmax of orally administered midazolam, but the AUC and Cmax of orally administered midazolam were increased after single treatment of Schisandrae Chinensis Fructus extract | Due to stronger induction of CYP3A in liver and intestine than inhibition of CYP3A in long-term treatment; Due to stronger inhibition of CYP3A in intestine, not in liver after single treatment | [72] |
| G. biloba leaf extract (p.o.) | Single treatment of G. biloba leaf extract increased the intravenously administered diltiazem concentrations in plasma, but long-term treatment of ginkgo biloba leaf extract reduced the intravenously administered diltiazem concentrations in plasma | Due to inhibition of CYP3A in liver in singe treatment of G. biloba leaf extract; due to induction of CYP3A in liver after long-term treatment | [68,76] | |
| Lonicera japonica extract (p.o.) | 28-day treatment of L. japonica extract increased metformin concentration in liver along with the enhancement of glucose tolerance activity of metformin, but single and 7-day treatment of Lonicera japonica extract did not alter metformin concentration in plasma and liver as well as glucose tolerance activity. | Due to reduction in mate1-mediated biliary excretion of metformin by 28-day treatment of Lonicera japonica extract | [29] | |
| Houttuynia cordata extract (p.o.) | 28-day treatment of H. cordata extract increased metformin concentration in plasma, liver and kidneys along with the enhancement of glucose-lowering effect in rats, but there no change of PK and PD of metformin after single and 7-day treatment of Houttuynia cordata extract | Increase in metformin plasma concentrations due to the decrease in renal oct2-mediated renal excretion of metformin and metformin concentration in kidneys; enhancement of glucose tolerance activity due to the increase in oct1-mediated renal uptake of metformin | [30] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, Y.H.; Chin, Y.-W. Multifaceted Factors Causing Conflicting Outcomes in Herb-Drug Interactions. Pharmaceutics 2021, 13, 43. https://doi.org/10.3390/pharmaceutics13010043
Choi YH, Chin Y-W. Multifaceted Factors Causing Conflicting Outcomes in Herb-Drug Interactions. Pharmaceutics. 2021; 13(1):43. https://doi.org/10.3390/pharmaceutics13010043
Chicago/Turabian StyleChoi, Young Hee, and Young-Won Chin. 2021. "Multifaceted Factors Causing Conflicting Outcomes in Herb-Drug Interactions" Pharmaceutics 13, no. 1: 43. https://doi.org/10.3390/pharmaceutics13010043
APA StyleChoi, Y. H., & Chin, Y.-W. (2021). Multifaceted Factors Causing Conflicting Outcomes in Herb-Drug Interactions. Pharmaceutics, 13(1), 43. https://doi.org/10.3390/pharmaceutics13010043






