Model-Informed Precision Dosing during Infliximab Induction Therapy Reduces Variability in Exposure and Endoscopic Improvement between Patients with Ulcerative Colitis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population Pharmacokinetic and Exposure-Response Models
2.2. Virtual Population
2.3. Dosing Scenarios
2.4. Evaluation of Dosing Scenarios
2.5. Software
3. Results
3.1. Population Pharmacokinetic and Exposure-Response Models
3.2. Dosing Simulations: Exposure and Efficacy
3.3. Dosing Simulations: Drug Consumption
3.4. Sensitivity Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rutgeerts, P.; Sandborn, W.J.; Feagan, B.G.; Reinisch, W.; Olson, A.; Johanns, J.; Travers, S.; Rachmilewitz, D.; Hanauer, S.B.; Lichtenstein, G.R.; et al. Infliximab for Induction and Maintenance Therapy for Ulcerative Colitis. N. Engl. J. Med. 2005, 353, 2462–2476. [Google Scholar] [CrossRef] [Green Version]
- Brandse, J.F.; Mathôt, R.A.; van der Kleij, D.; Rispens, T.; Ashruf, Y.; Jansen, J.M.; Rietdijk, S.; Löwenberg, M.; Ponsioen, C.Y.; Singh, S.; et al. Pharmacokinetic Features and Presence of Antidrug Antibodies Associate With Response to Infliximab Induction Therapy in Patients With Moderate to Severe Ulcerative Colitis. Clin. Gastroenterol. Hepatol. 2016, 14, 251–258.e2. [Google Scholar] [CrossRef] [PubMed]
- Seow, C.H.; Newman, A.; Irwin, S.P.; Steinhart, A.H.; Silverberg, M.S.; Greenberg, G.R. Trough serum infliximab: A predictive factor of clinical outcome for infliximab treatment in acute ulcerative colitis. Gut 2010, 59, 49–54. [Google Scholar] [CrossRef]
- Papamichael, K.; Van Stappen, T.; Vande Casteele, N.; Gils, A.; Billiet, T.; Tops, S.; Claes, K.; Van Assche, G.; Rutgeerts, P.; Vermeire, S.; et al. Infliximab Concentration Thresholds During Induction Therapy Are Associated With Short-term Mucosal Healing in Patients With Ulcerative Colitis. Clin. Gastroenterol. Hepatol. 2016, 14, 543–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farkas, K.; Rutka, M.; Golovics, P.A.; Végh, Z.; Lovász, B.D.; Nyári, T.; Gecse, K.B.; Kolar, M.; Bortlik, M.; Duricova, D.; et al. Efficacy of infliximab biosimilar CT-P13 induction therapy on mucosal healing in ulcerative colitis. J. Crohns Colitis 2016, 10, 1273–1278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adedokun, O.J.; Sandborn, W.J.; Feagan, B.G.; Rutgeerts, P.; Xu, Z.; Marano, C.W.; Johanns, J.; Zhou, H.; Davis, H.M.; Cornillie, F.; et al. Association between serum concentration of infliximab and efficacy in adult patients with ulcerative colitis. Gastroenterology 2014, 147, 1296–1307.e5. [Google Scholar] [CrossRef] [Green Version]
- Arias, M.T.; Vande Casteele, N.; Vermeire, S.; de Buck van Overstraeten, A.; Billiet, T.; Baert, F.; Wolthuis, A.; Van Assche, G.; Noman, M.; Hoffman, I.; et al. A panel to predict long-term outcome of infliximab therapy for patients with ulcerative colitis. Clin. Gastroenterol. Hepatol. 2015, 13, 531–538. [Google Scholar] [CrossRef]
- Kobayashi, T.; Suzuki, Y.; Motoya, S.; Hirai, F.; Ogata, H.; Ito, H.; Sato, N.; Ozaki, K.; Watanabe, M.; Hibi, T. First trough level of infliximab at week 2 predicts future outcomes of induction therapy in ulcerative colitis—results from a multicenter prospective randomized controlled trial and its post hoc analysis. J. Gastroenterol. 2016, 51, 241–251. [Google Scholar] [CrossRef] [Green Version]
- Vande Casteele, N.; Jeyarajah, J.; Jairath, V.; Feagan, B.G.; Sandborn, W.J. Infliximab Exposure-Response Relationship and Thresholds Associated With Endoscopic Healing in Patients With Ulcerative Colitis. Clin. Gastroenterol. Hepatol. 2019, 17, 1814–1821. [Google Scholar] [CrossRef]
- Vande Casteele, N.; Herfarth, H.; Katz, J.; Falck-Ytter, Y.; Singh, S. American Gastroenterological Association Institute Technical Review on the Role of Therapeutic Drug Monitoring in the Management of Inflammatory Bowel Diseases. Gastroenterology 2017, 153, 835–857. [Google Scholar] [CrossRef] [Green Version]
- Harbord, M.; Eliakim, R.; Bettenworth, D.; Karmiris, K.; Katsanos, K.; Kopylov, U.; Kucharzik, T.; Molnár, T.; Raine, T.; Sebastian, S.; et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 2: Current management. J. Crohns Colitis 2017. [Google Scholar] [CrossRef] [Green Version]
- Vande Casteele, N.; Ferrante, M.; Van Assche, G.; Ballet, V.; Compernolle, G.; Van Steen, K.; Simoens, S.; Rutgeerts, P.; Gils, A.; Vermeire, S. Trough concentrations of infliximab guide dosing for patients with inflammatory bowel disease. Gastroenterology 2015, 148, 1320–1329. [Google Scholar] [CrossRef] [PubMed]
- Mitrev, N.; Vande Casteele, N.; Seow, C.H.; Andrews, J.M.; Connor, S.J.; Moore, G.T.; Barclay, M.; Begun, J.; Bryant, R.; Chan, W.; et al. Review article: Consensus statements on therapeutic drug monitoring of anti-tumour necrosis factor therapy in inflammatory bowel diseases. Aliment. Pharmacol. Ther. 2017, 46, 1037–1053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Syversen, S.W.; Goll, G.L.; Jørgensen, K.K.; Sandanger, Ø.; Sexton, J.; Olsen, I.C.; Gehin, J.E.; Warren, D.J.; Brun, M.K.; Klaasen, R.A.; et al. Effect of Therapeutic Drug Monitoring vs Standard Therapy During Infliximab Induction on Disease Remission in Patients With Chronic Immune-Mediated Inflammatory Diseases: A Randomized Clinical Trial. JAMA 2021, 325, 1744–1754. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Dreesen, E. Therapeutic drug monitoring of anti-tumor necrosis factor agents: Lessons learned and remaining issues. Curr. Opin. Pharmacol. 2020, 55, 53–59. [Google Scholar] [CrossRef]
- Keizer, R.J.; ter Heine, R.; Frymoyer, A.; Lesko, L.J.; Mangat, R.; Goswami, S. Model-Informed Precision Dosing at the Bedside: Scientific Challenges and Opportunities. CPT Pharmacomet. Syst. Pharmacol. 2018, 7, 785–787. [Google Scholar] [CrossRef] [PubMed]
- Vermeire, S.; Dreesen, E.; Papamichael, K.; Dubinsky, M.C. How, When, and for Whom Should We Perform Therapeutic Drug Monitoring? Clin. Gastroenterol. Hepatol. 2019. [Google Scholar] [CrossRef]
- Dreesen, E.; Faelens, R.; Van Assche, G.; Ferrante, M.; Vermeire, S.; Gils, A.; Bouillon, T. Optimising infliximab induction dosing for patients with ulcerative colitis. Br. J. Clin. Pharmacol. 2019, 85, 782–795. [Google Scholar] [CrossRef] [Green Version]
- Ben-Horin, S.; Kopylov, U.; Chowers, Y. Optimizing anti-TNF treatments in inflammatory bowel disease. Autoimmun. Rev. 2014, 13, 24–30. [Google Scholar] [CrossRef]
- Sheiner, L.B. Analysis of pharmacokinetic data using parametric models. III. Hypothesis tests and confidence intervals. J. Pharmacokinet. Biopharm. 1986, 14, 539–555. [Google Scholar] [CrossRef]
- Fidler, M.L.; Hallow, M.; Wilkins, J.; Wang, W. RxODE: Facilities for Simulating from ODE-Based Models 2021. R package version 1.1.0. Available online: https://CRAN.R-project.org/package=RxODE (accessed on 20 August 2021).
- Dreesen, E. New Tools for Therapeutic Drug Monitoring: Making Big Things out of Small Pieces. J. Crohns Colitis 2021. [Google Scholar] [CrossRef] [PubMed]
- Battat, R.; Hemperly, A.; Truong, S.; Whitmire, N.; Boland, B.S.; Dulai, P.S.; Holmer, A.K.; Nguyen, N.H.; Singh, S.; Vande Casteele, N.; et al. Baseline Clearance of Infliximab Is Associated With Requirement for Colectomy in Patients With Acute Severe Ulcerative Colitis. Clin. Gastroenterol. Hepatol. 2021, 19, 511–518.e6. [Google Scholar] [CrossRef] [PubMed]
- Ding, N.S.; Hart, A.; De Cruz, P. Systematic review: Predicting and optimising response to anti-TNF therapy in Crohn’s disease - Algorithm for practical management. Aliment. Pharmacol. Ther. 2016, 43, 30–51. [Google Scholar] [CrossRef]
- Dreesen, E.; Berends, S.; Laharie, D.; D’Haens, G.; Vermeire, S.; Gils, A.; Mathôt, R. Modelling of the relationship between infliximab exposure, faecal calprotectin and endoscopic remission in patients with Crohn’s disease. Br. J. Clin. Pharmacol. 2020, 87, 106–118. [Google Scholar] [CrossRef] [PubMed]
- Brekkan, A.; Lopez-Lazaro, L.; Yngman, G.; Plan, E.L.; Acharya, C.; Hooker, A.C.; Kankanwadi, S.; Karlsson, M.O. A Population Pharmacokinetic-Pharmacodynamic Model of Pegfilgrastim. AAPS J. 2018, 20, 91. [Google Scholar] [CrossRef] [Green Version]
- Kantasiripitak, W.; Verstockt, B.; Alsoud, D.; Lobatón, T.; Thomas, D.; Gils, A.; Vermeire, S.; Ferrante, M.; Dreesen, E. The effect of aging on infliximab exposure and response in patients with inflammatory bowel diseases. Br. J. Clin. Pharmacol. 2021. [Google Scholar] [CrossRef]
- Bejan-Angoulvant, T.; Ternant, D.; Daoued, F.; Medina, F.; Bernard, L.; Mammou, S.; Paintaud, G.; Mulleman, D. Brief Report: Relationship Between Serum Infliximab Concentrations and Risk of Infections in Patients Treated for Spondyloarthritis. Arthritis Rheumatol. 2017, 69, 108–113. [Google Scholar] [CrossRef] [Green Version]
- Landemaine, A.; Petitcollin, A.; Brochard, C.; Miard, C.; Dewitte, M.; Le, E.; Grainville, T.; Bellissant, E.; Siproudhis, L.; Bouguen, G. Cumulative Exposure to Infliximab, But Not Trough Concentrations, Correlate With Rate of Infection. Clin. Gastroenterol. Hepatol. 2020. [Google Scholar] [CrossRef] [PubMed]
- NIH U.S. Natial Library of Medicine ClinicalTrials.gov. Optimising Infliximab Induction Therapy for Acute Severe Ulcerative Colitis (PREDICT-UC). Available online: https://clinicaltrials.gov/ct2/show/NCT02770040 (accessed on 16 July 2021).
- D’Haens, G.; Vermeire, S.; Lambrecht, G.; Baert, F.; Bossuyt, P.; Pariente, B.; Buisson, A.; Bouhnik, Y.; Filippi, J.; vander Woude, J.; et al. Increasing Infliximab Dose Based on Symptoms, Biomarkers, and Serum Drug Concentrations Does Not Increase Clinical, Endoscopic, and Corticosteroid-Free Remission in Patients With Active Luminal Crohn’s Disease. Gastroenterology 2018, 154, 1343–1351.e1. [Google Scholar] [CrossRef] [PubMed]
- Alihodzic, D.; Broeker, A.; Baehr, M.; Kluge, S.; Langebrake, C.; Wicha, S.G. Impact of Inaccurate Documentation of Sampling and Infusion Time in Model-Informed Precision Dosing. Front. Pharmacol. 2020, 11, 1–12. [Google Scholar] [CrossRef] [Green Version]
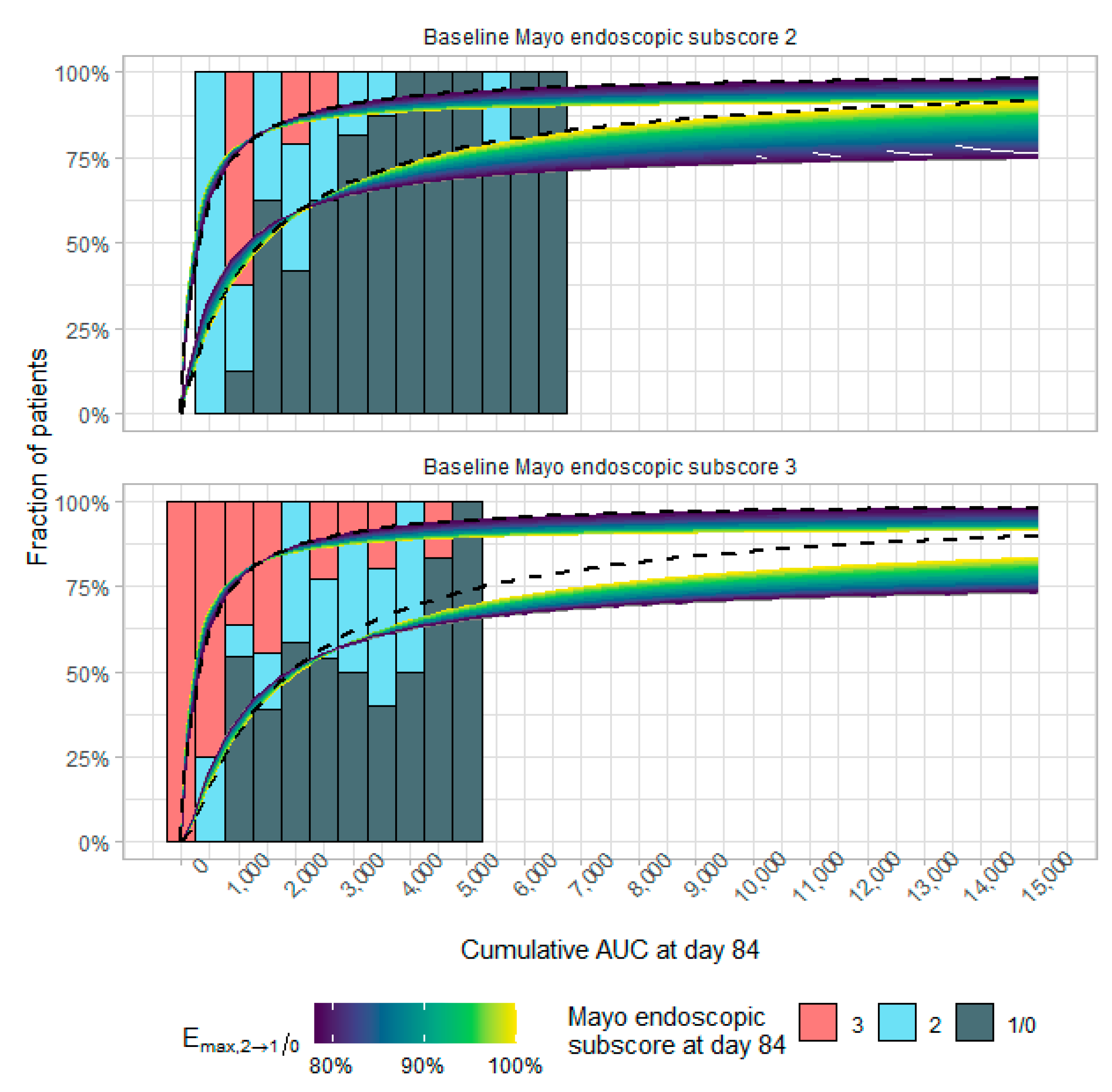



| AUCd84 (mg/L × Day) | pEI (%) | Cumulative Dose (mg) | |||||
|---|---|---|---|---|---|---|---|
| Baseline Mayo Endoscopic Subscore | Dosing scenario | median | [90%PI] | mean | ±sd | mean | ±sd |
| 2 | 5 mg/kg | 2455 | [1215–4805] | 61.2 | ±5.51 | 1090 | ±196 |
| 10 mg/kg | 4910 | [2431–9609] | 68.6 | ±3.60 | 2181 | ±393 | |
| Covariate-based MIPD | 4895 | [2661–8522] | 68.7 | ±3.08 | 2166 | ±443 | |
| Concentration-based MIPD | 5095 | [3683–6879] | 69.3 | ±1.67 | 2298 | ±613 | |
| 3 | 5 mg/kg | 1979 | [953–3990] | 50.3 | ±8.36 | 1078 | ±214 |
| 10 mg/kg | 3958 | [1906–7981] | 61.6 | ±6.05 | 2155 | ±428 | |
| Covariate-based MIPD | 3933 | [2123–7045] | 61.7 | ±5.06 | 2137 | ±417 | |
| Concentration-based MIPD | 4125 | [3056–5431] | 62.8 | ±2.51 | 2287 | ±643 | |
| Combined (2:3; 49%:51%) | 5 mg/kg | 2210 | [1049–4448] | 55.7 | ±8.96 | 1084 | ±205 |
| 10 mg/kg | 4419 | [2098–8895] | 65.1 | ±6.11 | 2168 | ±411 | |
| Covariate-based MIPD | 4372 | [2302–7940] | 65.1 | ±5.46 | 2151 | ±431 | |
| Concentration-based MIPD | 4561 | [3209–6516] | 66.0 | ±3.91 | 2293 | ±628 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faelens, R.; Wang, Z.; Bouillon, T.; Declerck, P.; Ferrante, M.; Vermeire, S.; Dreesen, E. Model-Informed Precision Dosing during Infliximab Induction Therapy Reduces Variability in Exposure and Endoscopic Improvement between Patients with Ulcerative Colitis. Pharmaceutics 2021, 13, 1623. https://doi.org/10.3390/pharmaceutics13101623
Faelens R, Wang Z, Bouillon T, Declerck P, Ferrante M, Vermeire S, Dreesen E. Model-Informed Precision Dosing during Infliximab Induction Therapy Reduces Variability in Exposure and Endoscopic Improvement between Patients with Ulcerative Colitis. Pharmaceutics. 2021; 13(10):1623. https://doi.org/10.3390/pharmaceutics13101623
Chicago/Turabian StyleFaelens, Ruben, Zhigang Wang, Thomas Bouillon, Paul Declerck, Marc Ferrante, Séverine Vermeire, and Erwin Dreesen. 2021. "Model-Informed Precision Dosing during Infliximab Induction Therapy Reduces Variability in Exposure and Endoscopic Improvement between Patients with Ulcerative Colitis" Pharmaceutics 13, no. 10: 1623. https://doi.org/10.3390/pharmaceutics13101623
APA StyleFaelens, R., Wang, Z., Bouillon, T., Declerck, P., Ferrante, M., Vermeire, S., & Dreesen, E. (2021). Model-Informed Precision Dosing during Infliximab Induction Therapy Reduces Variability in Exposure and Endoscopic Improvement between Patients with Ulcerative Colitis. Pharmaceutics, 13(10), 1623. https://doi.org/10.3390/pharmaceutics13101623







