Stabilisation of Recombinant Human Basic Fibroblast Growth Factor (FGF-2) against Stressors Encountered in Medicinal Product Processing and Evaluation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Assessment of Stability of FGF-2 as Received from Manufacturer
2.3. Survey of Excipients for Stabilising FGF-2 Solutions
2.4. Optimisation of FGF-2 Aqueous Solutions to Processing Stressors
2.5. Storage Stability of Lyophilised and Reconstituted FGF-2 Samples
2.6. Data Analysis
3. Results
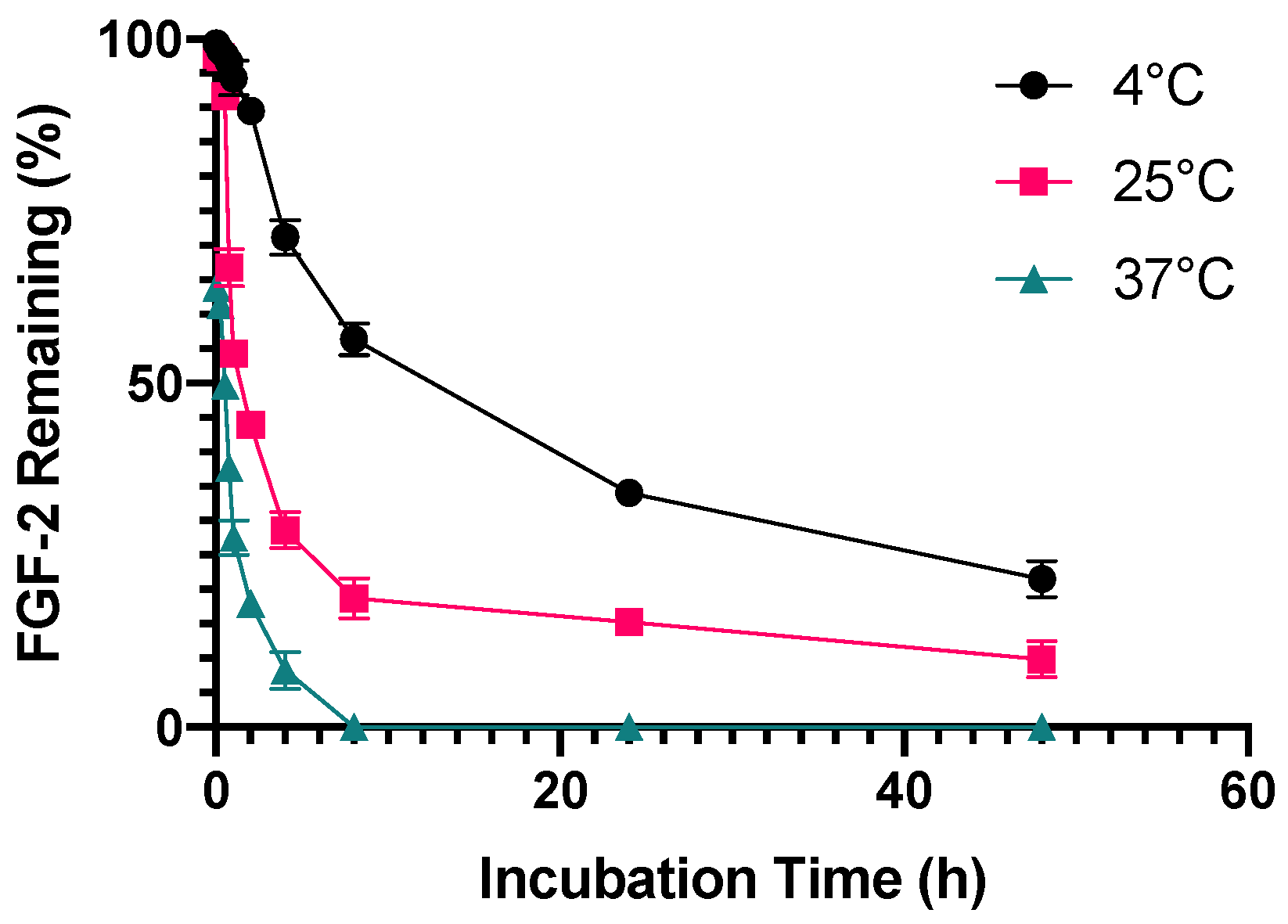
3.1. Stability of FGF-2 as Received from Manufacturer
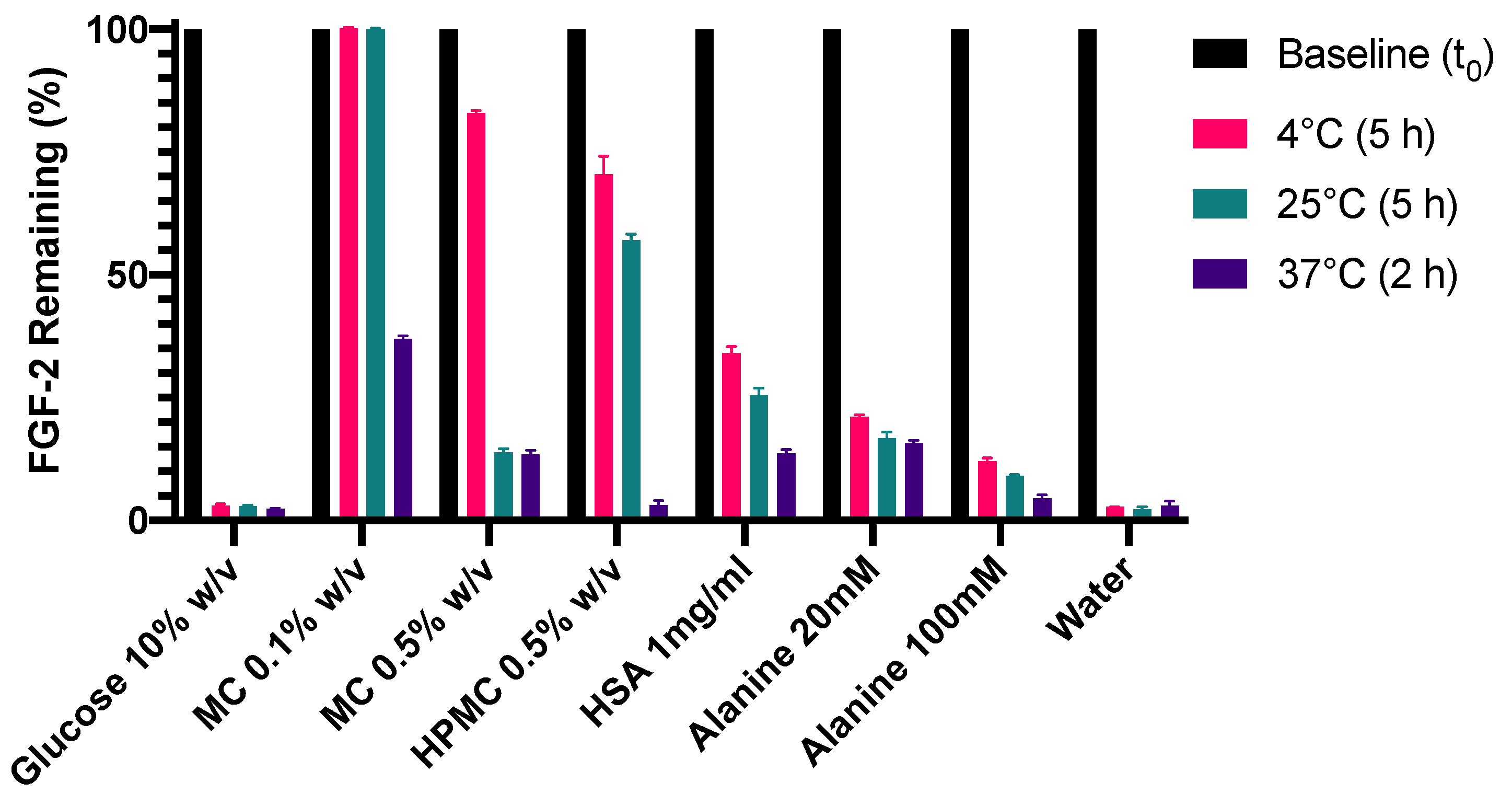
3.2. Identification of Potential Stabilisers for Aqueous FGF-2 Solutions
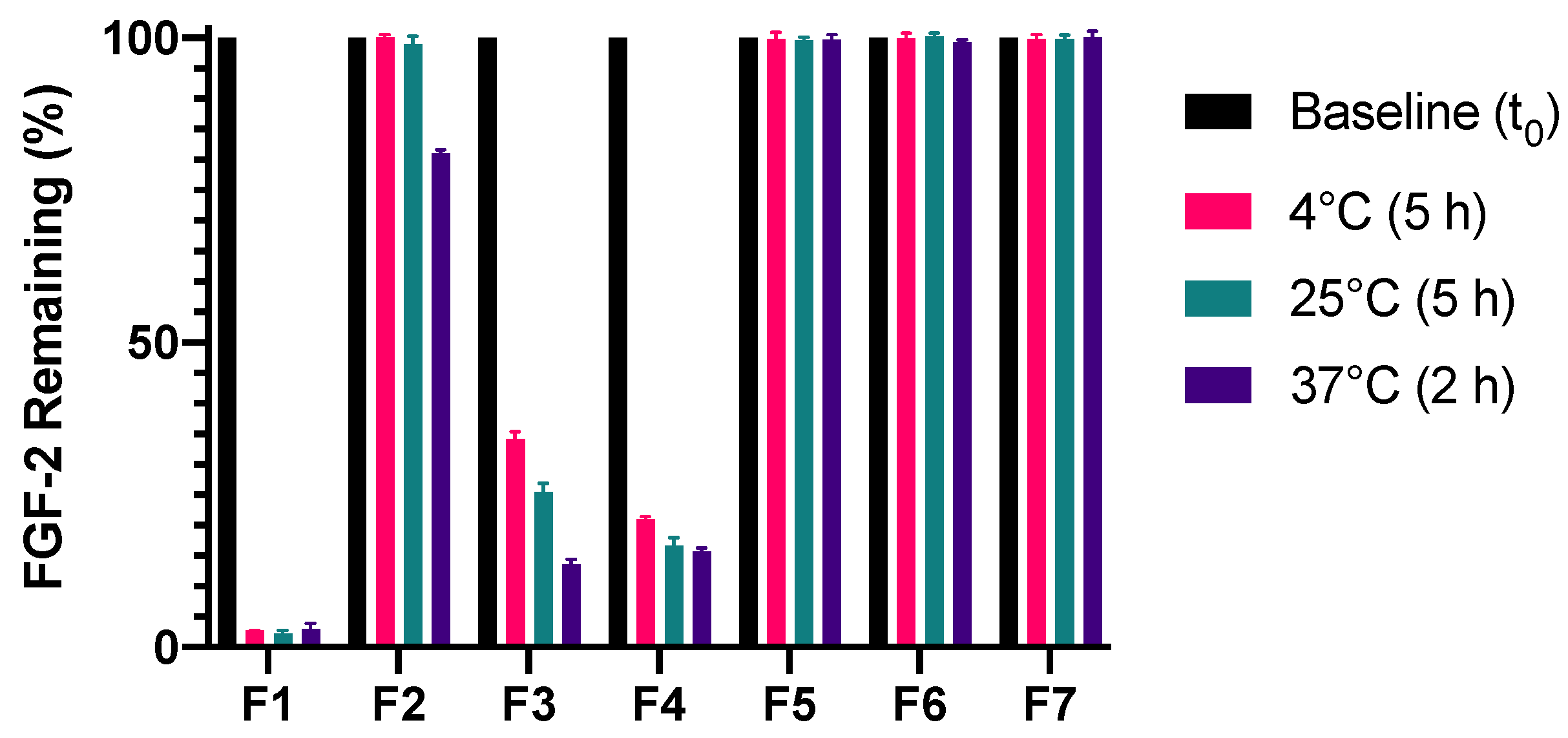
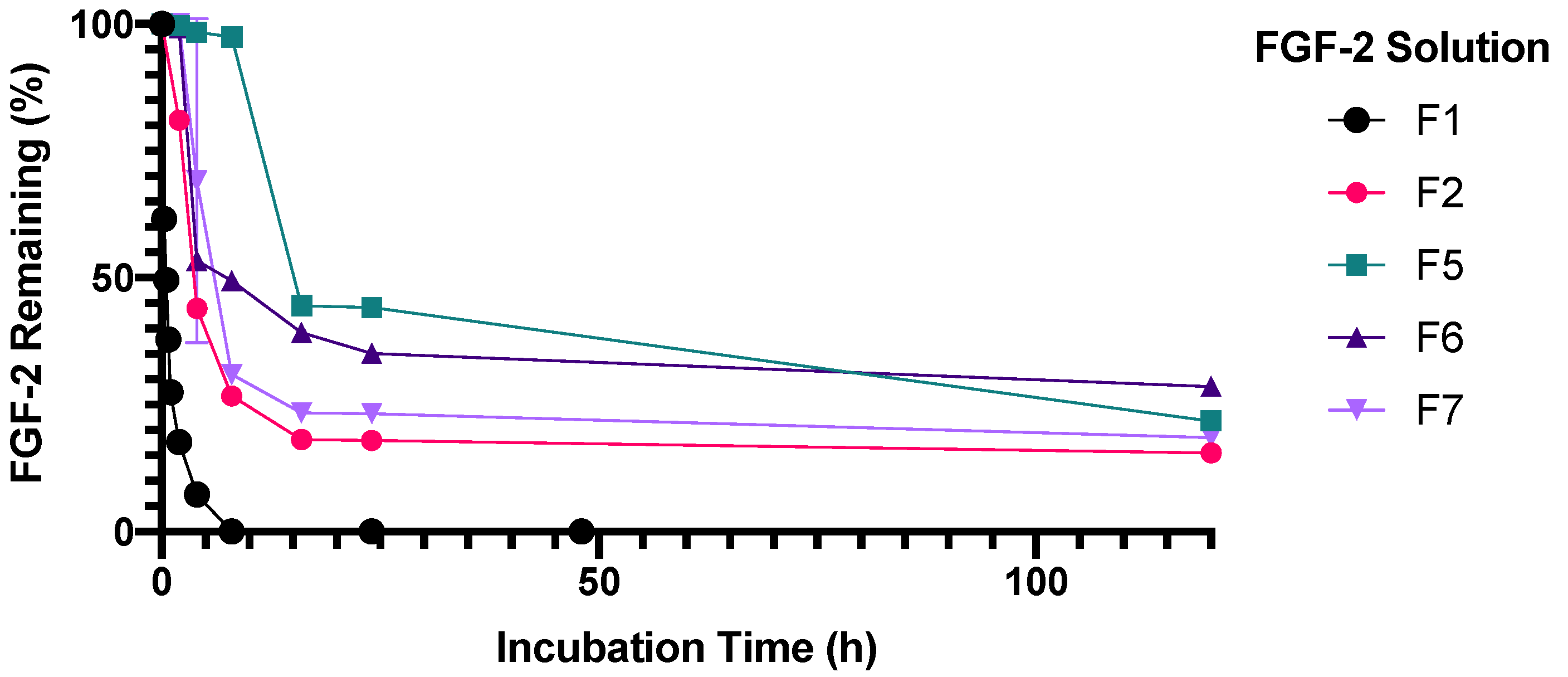
3.3. Stabilisation of FGF-2 Solutions to Temperature Stressors
3.4. Stabilisation of FGF-2 Solutions to Repeat Freeze/Thaw and Lyophilisation Stressors
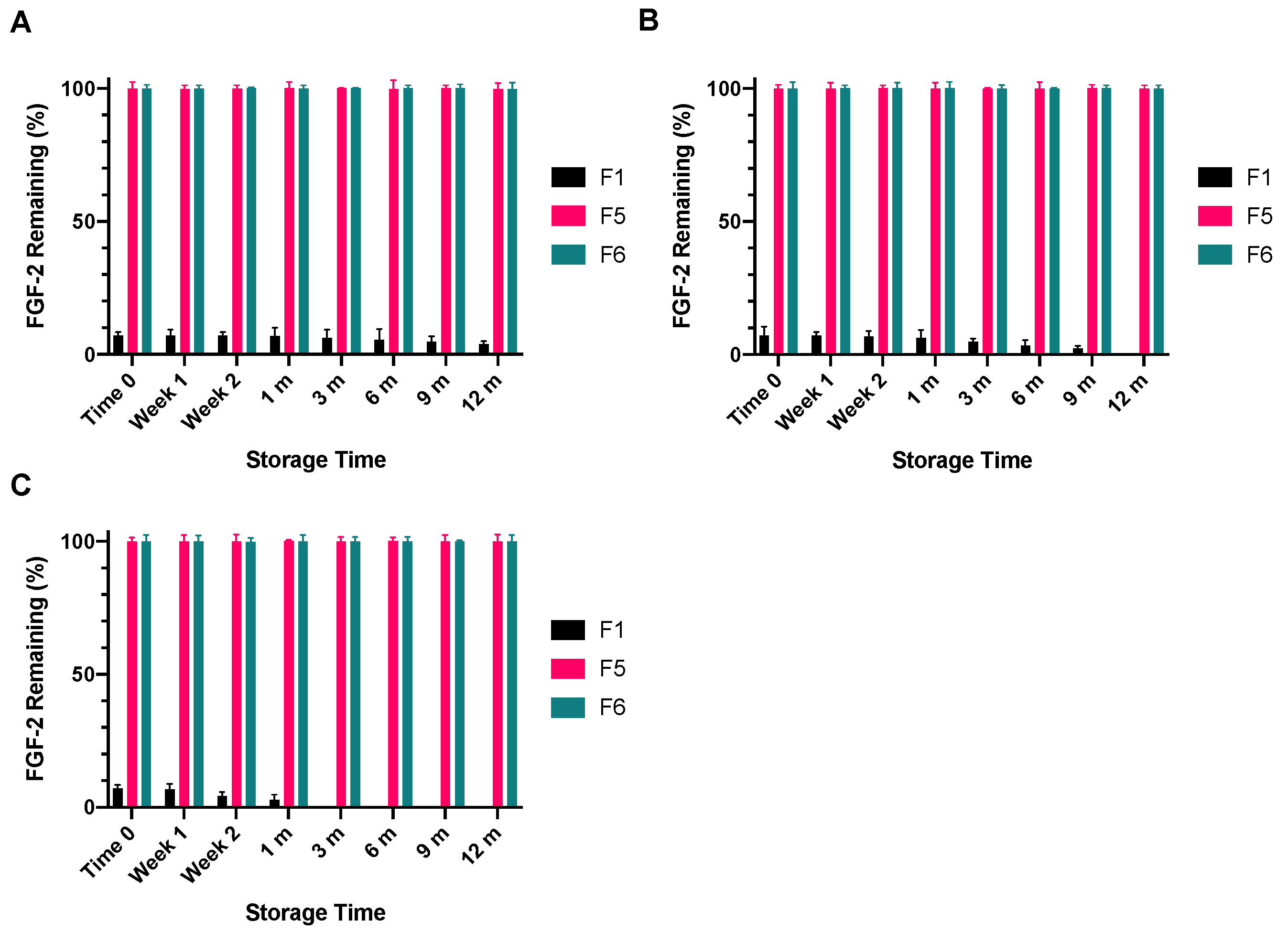
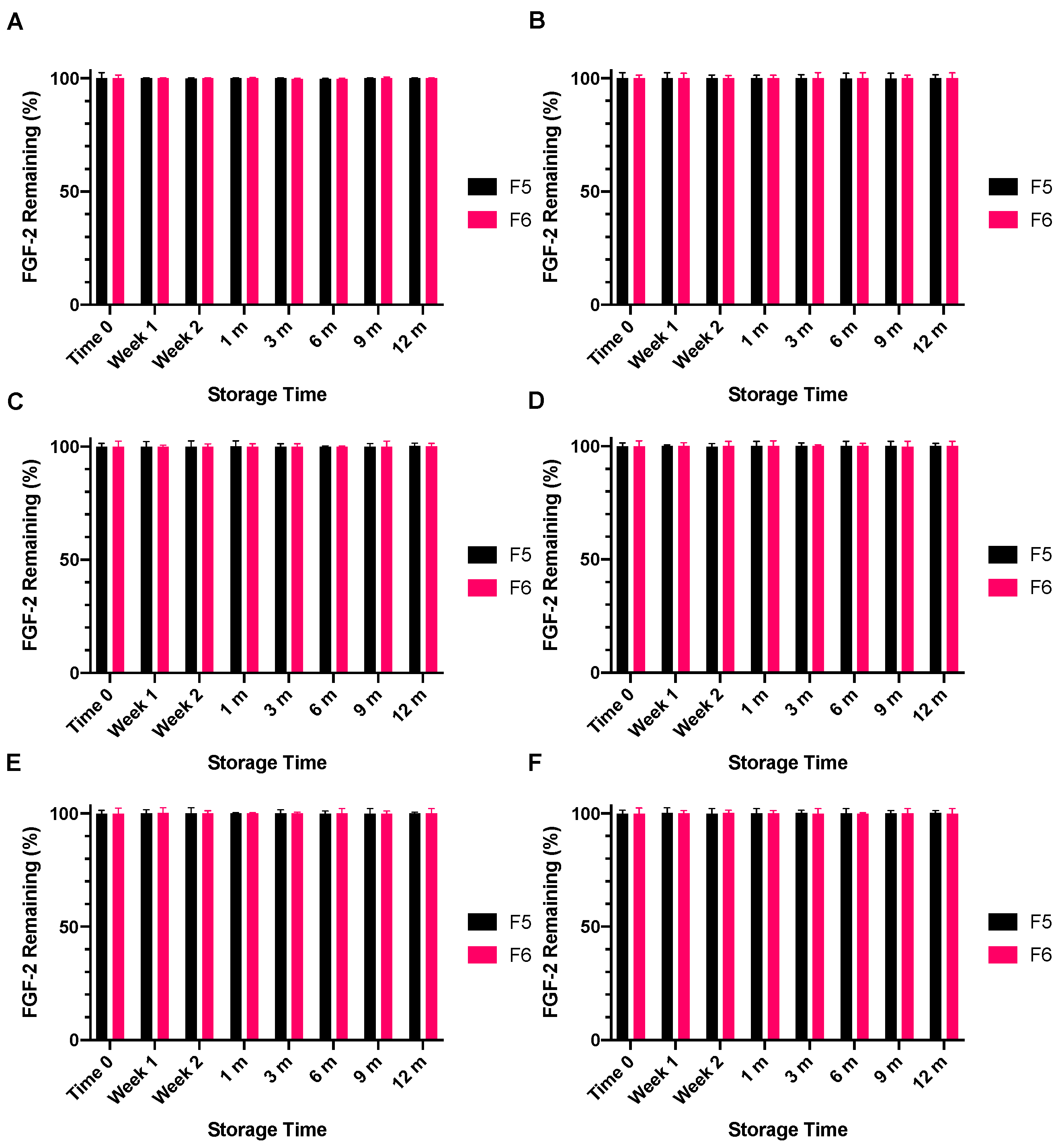
3.5. Storage Stability of Lyophilised and Reconstituted FGF-2 Samples
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beenken, A.; Mohammadi, M. The FGF family: Biology, pathophysiology and therapy. Nat. Rev. Drug Discov. 2009, 8, 235–253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yun, Y.-R.; Won, J.E.; Jeon, E.; Lee, S.; Kang, W.; Jo, H.; Jang, J.-H.; Shin, U.S.; Kim, H.-W. Fibroblast growth factors: Biology, function, and application for tissue regeneration. J. Tissue Eng. 2010, 1, 218142. [Google Scholar] [CrossRef] [PubMed]
- Nunes, Q.M.; Li, Y.; Sun, C.; Kinnunen, T.K.; Fernig, D.G. Fibroblast growth factors as tissue repair and regeneration therapeutics. PeerJ 2016, 4, e1535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akita, S.; Akino, K.; Imaizumi, T.; Hirano, A. Basic fibroblast growth factor accelerates and improves second-degree burn wound healing. Wound Repair Regen. 2008, 16, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.-W.; Zhang, Y.; Zhang, H.; Lu, K.; Yang, S.-K.; Sun, G.-L. Double-blind, randomized, controlled clinical trial of the effects of diosmectite and basic fibroblast growth factor paste on the treatment of minor recurrent aphthous stomatitis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, 570–575. [Google Scholar] [CrossRef]
- Kawaguchi, H.; Oka, H.; Jingushi, S.; Izumi, T.; Fukunaga, M.; Sato, K.; Matsushita, T.; Nakamura, K. A local application of recombinant human fibroblast growth factor 2 for tibial shaft fractures: A randomized, placebo-controlled trial. J. Bone Miner. Res. 2010, 25, 2735–2743. [Google Scholar] [CrossRef]
- Robson, M.C.; Phillips, L.G.; Lawrence, W.T.; Bishop, J.B.; Youngerman, J.S.; Hayward, P.G.; Broemeling, L.D.; Heggers, J.P. The Safety and Effect of Topically Applied Recombinant Basic Fibroblast Growth Factor on the Healing of Chronic Pressure Sores. Ann. Surg. 1992, 216, 401–408. [Google Scholar] [CrossRef]
- Uchi, H.; Igarashi, A.; Urabe, K.; Koga, T.; Nakayama, J.; Kawamori, R.; Tamaki, K.; Hirakata, H.; Ohura, T.; Furue, M. Clinical efficacy of basic fibroblast growth factor (bFGF) for diabetic ulcer. Eur. J. Dermatol. 2009, 19, 461–468. [Google Scholar] [CrossRef]
- Kumagai, M.; Marui, A.; Tabata, Y.; Takeda, T.; Yamamoto, M.; Yonezawa, A.; Tanaka, S.; Yanagi, S.; Ito-Ihara, T.; Ikeda, T.; et al. Safety and efficacy of sustained release of basic fibroblast growth factor using gelatin hydrogel in patients with critical limb ischemia. Heart Vessel. 2016, 31, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Levy, Y.; Hershfield, M.S.; Fernandez-Mejia, C.; Polmar, S.H.; Scudiery, D.; Berger, M.; Sorensen, R.U. Adenosine deaminase deficiency with late onset of recurrent infections: Response to treatment with polyethylene glycol-modified adenosine deaminase. J. Pediatrics 1988, 113, 312–317. [Google Scholar] [CrossRef]
- Ringsdorf, H. Structure and properties of pharmacologically active polymers. J. Polym. Sci. Polym. Symp. 1975, 51, 135–153. [Google Scholar] [CrossRef]
- Kato, M.; Jackler, R.K. Repair of chronic tympanic membrane perforations with fibroblast growth factor. Otolaryngol. Head Neck Surg. 1996, 115, 538–547. [Google Scholar] [CrossRef]
- Weber, D.E.; Semaan, M.T.; Wasman, J.K.; Beane, R.; Bonassar, L.J.; Megerian, C.A. Tissue-engineered calcium alginate patches in the repair of chronic chinchilla tympanic membrane perforations. Laryngoscope 2006, 116, 700–704. [Google Scholar] [CrossRef] [PubMed]
- Wieland, A.M.; Sundback, C.A.; Hart, A.; Kulig, K.; Masiakos, P.T.; Hartnick, C.J. Poly(glycerol sebacate)-engineered plugs to repair chronic tympanic membrane perforations in a chinchilla model. Otolaryngol. Head Neck Surg. Off. J. Am. Acad. Otolaryngol. Head Neck Surg. 2010, 143, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Andreopoulos, F.M.; Persaud, I. Delivery of basic fibroblast growth factor (bFGF) from photoresponsive hydrogel scaffolds. Biomaterials 2006, 27, 2468–2476. [Google Scholar] [CrossRef]
- Freudenberg, U.; Hermann, A.; Welzel, P.B.; Stirl, K.; Schwarz, S.C.; Grimmer, M.; Zieris, A.; Panyanuwat, W.; Zschoche, S.; Meinhold, D.; et al. A star-PEG–heparin hydrogel platform to aid cell replacement therapies for neurodegenerative diseases. Biomaterials 2009, 30, 5049–5060. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.J.; Shahrokh, Z.; Vemuri, S.; Eberlein, G.; Beylin, I.; Busch, M. Characterization, stability, and formulations of basic fibroblast growth factor. In Formulation, Characterization, and Stability of Protein Drugs: Case Histories; Pearlman, R., Wang, J.Y., Eds.; Springer Science and Business Media LLC: New York, NY, USA, 2002; pp. 141–180. [Google Scholar]
- Vemuri, S.; Beylin, I.; Sluzky, V.; Stratton, P.; Eberlein, G.; Wang, Y.J. The stability of bFGF against thermal denaturation. J. Pharm. Pharmacol. 1994, 46, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Furue, M.; Na, J.; Jackson, J.P.; Okamoto, T.; Jones, M.; Baker, D.; Hata, R.-I.; Moore, H.D.; Sato, J.D.; Andrews, P.W. Heparin Promotes the Growth of Human Embryonic Stem Cells in a Defined Serum-Free Medium. Proc. Natl. Acad. Sci. USA 2008, 105, 13409–13414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benington, L.; Rajan, G.; Locher, C.; Lim, L.Y. Fibroblast Growth Factor 2-A Review of Stabilisation Approaches for Clinical Applications. Pharmaceutics 2020, 12, 508. [Google Scholar] [CrossRef] [PubMed]
- Lou, Z.; Huang, P.; Yang, J.; Xiao, J.; Chang, J. Direct application of bFGF without edge trimming on human subacute tympanic membrane perforation. Am. J. Otolaryngol. 2016, 37, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Chu, H.; Gao, J.; Chen, W.C.; Huard, J.; Wang, Y. Injectable fibroblast growth factor-2 coacervate for persistent angiogenesis. Proc. Natl. Acad. Sci. USA 2011, 108, 13444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dvořák, P.; Bednar, D.; Vanacek, P.; Balek, L.; Eiselleova, L.; Stepankova, V.; Sebestova, E.; Bosakova, M.K.; Konecna, Z.; Mazurenko, S.; et al. Computer-assisted engineering of hyperstable fibroblast growth factor 2. Biotechnol. Bioeng. 2017, 115, 850–862. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.-Y.; Kim, J.-J.; El-Fiqi, A.; Jang, J.-H.; Kim, H.-W. Ultrahigh protein adsorption capacity and sustained release of nanocomposite scaffolds: Implication for growth factor delivery systems. RSC Adv. 2017, 7, 16453–16459. [Google Scholar] [CrossRef] [Green Version]
- Cold Spring Harbor Protocols. Table 7. Solvent Additives That Stabilize or Destabilize Proteins in Solution 2010 [Updated 1 May 2010]. Available online: http://cshprotocols.cshlp.org/content/2010/5/pdb.tab7top79.short (accessed on 9 September 2017).
- Ohtake, S.; Kita, Y.; Arakawa, T. Interactions of formulation excipients with proteins in solution and in the dried state. Adv. Drug Deliv. Rev. 2011, 63, 1053–1073. [Google Scholar] [CrossRef] [PubMed]
- Hawe, A.; Friess, W. Stabilization of a hydrophobic recombinant cytokine by human serum albumin. J. Pharm. Sci. 2007, 96, 2987–2999. [Google Scholar] [CrossRef] [PubMed]
- Scientific TF. Human FGF Basic ELISA Kit [Product Information Sheet]. Frederick, MD: Life Technologies Corporation; 2015 [Updated 12/9/2015]. Available online: https://www.thermofisher.com/elisa/product/FGF2-Human-ELISA-Kit/KHG0022 (accessed on 10 July 2018).
- Zhuhai Essex Bio-Pharmaceutical Co. L. Recombinant Bovine Basic Fibroblast Growth Factor Eye Drops Zhuhai, China 2017. Available online: http://www.essexbio.com/products-detail/i-1.html (accessed on 8 August 2016).
- Schein, C.H. Solubility as a function of protein structure and solvent components. Biotechnol. J. 1990, 8, 308–317. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Manabe, Y.; Minamoto, N.; Saiki, N.; Fukasem, K. Development of a simple assay system for protein-stabilizing efficiency based on hemoglobin protection against denaturation and measurement of the cooperative effect of mixing protein stabilizers. Biosci. Biotechnol. Biochem. 2016, 80, 1874–1878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choudhary, S.; Save, S.N.; Kishore, N.; Hosur, R.V. Synergistic inhibition of protein fibrillation by proline and sorbitol: Biophysical investigations. PLoS ONE 2016, 11, e0166487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prasanthan, P.; Kishore, N. Combined effect of equimolal osmolytes trehalose and glycine on stability of hen egg-white lysozyme: Quantitative mechanistic aspects. J. Mol. Liq. 2019, 278, 477–483. [Google Scholar] [CrossRef]
- Shah, D. Effect of Various Additives on the Stability of Basic Fibroblast Growth Factor and Development of an Intradermal Injectable Formulation; ProQuest Dissertations Publishing: Kansas City, MO, USA, 1998. [Google Scholar]
- Chen, G.; Gulbranson, D.R.; Yu, P.; Hou, Z.; Thomson, J.A. Thermal stability of fibroblast growth factor protein is a determinant factor in regulating self-renewal, differentiation, and reprogramming in human pluripotent stem cells. Stem Cells 2011, 30, 623–630. [Google Scholar] [CrossRef] [Green Version]
- Davis, J.; Venkataraman, G.; Shriver, Z.; Raj, P.; Sasisekharan, R. Oligomeric self-association of basic fibroblast growth factor in the absence of heparin-like glycosaminoglycans. Biochem. J. 1999, 341, 613–620. [Google Scholar] [CrossRef]
- ICH. Quality of Biotechnological Products: Stability Testing of Biotechnological/Biological Products Q5C 1995. Available online: https://database.ich.org/sites/default/files/Q5C%20Guideline.pdf (accessed on 6 October 2021).
- Bostrom, M.; Tavares, F.W.; Bratko, D.; Ninham, B.W. Specific ion effects in solutions of globular proteins: Comparison between analytical models and simulation. J. Phys. Chem. B 2005, 109, 24489–24494. [Google Scholar] [CrossRef]
- Boardman, N.K.; Partridge, S.M. Separation of neutral proteins on ion-exchange resins. Biochem. J. 1955, 59, 543–552. [Google Scholar] [CrossRef] [Green Version]
- Velayudhan, A.; Horvath, C. On the stoichiometric model of electrostatic interaction chromatography for biopolymers. J. Chromatogr. 1986, 367, 160–162. [Google Scholar] [CrossRef]
- Stahlberg, J.; Jonsson, B.; Horvath, C. Combined effect of coulombic and van der Waals interactions in the chromatography of proteins. Anal. Chem. 1992, 64, 3118–3124. [Google Scholar] [CrossRef]
- Arakawa, T.; Bhat, R.; Timasheff, S.N. Preferential interactions determine protein solubility in three-component solutions: The MgCl2 system. Biochemistry 1990, 29, 1914–1923. [Google Scholar] [CrossRef]
- Arakawa, T.; Timasheff, S.N. Theory of protein solubility. Methods Enzymol. 1985, 114, 49–77. [Google Scholar]
- Traube, J. The theory of attraction pressure. J. Phys. Chem. 2002, 14, 471–475. [Google Scholar] [CrossRef] [Green Version]
- Apetri, A.C.; Surewicz, W.K. Atypical effect of salts on the thermodynamic stability of human prion protein. J. Biol. Chem. 2003, 278, 22187–22192. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.D.; Cousens, L.S.; Barr, P.J.; Sprang, S.R. Three-dimensional structure of human basic fibroblast growth factor, a structural homolog of interleukin 1 beta. Proc. Natl. Acad. Sci. USA 1991, 88, 3446–3450. [Google Scholar] [CrossRef] [Green Version]
- Arakawa, T.; Timasheff, S.N. Stabilization of protein structure by sugars. Biochemistry 1982, 21, 6536–6544. [Google Scholar] [CrossRef]
- Kuznetsova, I.M.; Zaslavsky, B.Y.; Breydo, L.; Turoverov, K.K.; Uversky, V.N. Beyond the excluded volume effects: Mechanistic complexity of the crowded milieu. Molecules 2015, 20, 1377–1409. [Google Scholar] [CrossRef] [Green Version]
- Wu, A.; Gao, Y.; Zheng, L. Zwitterionic amphiphiles: Their aggregation behavior and applications. Green Chem. 2019, 21, 4290–4312. [Google Scholar] [CrossRef]
- Contessi, N.; Altomare, L.; Filipponi, A.; Farè, S. Thermo-responsive properties of methylcellulose hydrogels for cell sheet engineering. Mater Lett. 2017, 207, 157–160. [Google Scholar] [CrossRef]
- Joshi, S.C. Sol-Gel Behavior of Hydroxypropyl Methylcellulose (HPMC) in Ionic Media Including Drug Release. Materials 2011, 4, 1861–1905. [Google Scholar] [CrossRef] [Green Version]
- Ali, Z.; Islam, A.; Sherrell, P.; Le-Moine, M.; Lolas, G.; Syrigos, K.; Rafat, M.; Jensen, L.D. Adjustable delivery of pro-angiogenic FGF-2 by alginate:collagen microspheres. Biol. Open. 2018, 7, bio027060. [Google Scholar] [CrossRef] [Green Version]
- Spelzini, D.; Rigatusso, R.; Farruggia, B.; Picó, G. Thermal Aggregation of Methyl Cellulose in Aqueous Solution: A Thermodynamic Study and Protein Partitioning Behaviour. Cellulose 2005, 12, 293–304. [Google Scholar] [CrossRef]
- Pikal, M.J. Freeze-drying of proteins. Part I: Process design. BioPharm 1990, 3, 18–27. [Google Scholar]
- Carpenter, J.F.; Hand, S.C.; Crowe, L.M.; Crowe, J.H. Cryoprotection of phosphofructokinase with organic solutes: Characterization of enhanced protection in the presence of divalent cations. Arch. Biochem. Biophys. 1986, 250, 505–512. [Google Scholar] [CrossRef]
- Carpenter, J.F.; Crowe, L.M.; Crowe, J.H. Stabilization of phosphofructokinase with sugars during freeze-drying: Characterization of enhanced protection in the presence of divalent cations. Biochim. Biophys Acta 1987, 923, 109–115. [Google Scholar] [CrossRef]
- Chang, B.S.; Randall, C.S.; Lee, Y.S. Stabilization of lyophilized porcine pancreatic elastase. Pharm. Res. 1993, 10, 1478–1483. [Google Scholar] [CrossRef] [PubMed]
- Sluzky, V.; Shahrokh, Z.; Stratton, P.; Eberlein, G.; Wang, Y.J. Chromatographic methods for quantitative analysis of native, denatured, and aggregated basic fibroblast growth factor in solution formulations. Pharm. Res. 1994, 11, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Sauer, D.G.; Mosor, M.; Frank, A.-C.; Weiß, F.; Christler, A.; Walch, N.; Jungbauer, A.; Dürauer, A. A two-step process for capture and purification of human basic fibroblast growth factor from E. coli homogenate: Yield versus endotoxin clearance. Protein Expr. Purif. 2019, 153, 70–82. [Google Scholar] [CrossRef]
- Chrusciel, M.; Rekawiecki, R.; Ziecik, A.; Andronowska, A. MRNA and protein expression of FGF-1, FGF-2 and their receptors in the porcine umbilical cord during pregnancy. Folia Histochem. Cytobiol. 2010, 48, 572–580. [Google Scholar] [CrossRef] [PubMed] [Green Version]





| Excipient | Excipient Concentration |
|---|---|
| Sodium chloride (NaCl) | 0.9% w/v |
| Maltodextrin | 1% w/v; 10% w/v |
| Mannitol | 5% w/v; 10% w/v |
| Glucose | 5% w/v; 10% w/v |
| Methylcellulose (MC) | 0.1% w/v; 0.5% w/v |
| Hydroxypropyl methylcellulose (HPMC) | 0.5% w/v; 2% w/v |
| Sodium alginate | 2% w/v |
| Human serum albumin (HSA) | 1 mg/mL; 10 mg/mL |
| Alanine | 20 mM; 100 mM |
| Glycine | 20 mM; 100 mM |
| Excipient(s) | Final Excipient Concentration(s) |
|---|---|
| Glucose | 10% w/v |
| Methylcellulose (MC) | 0.05% w/v; 0.10% w/v; 0.50% w/v |
| Human Serum Albumin (HSA) | 1 mg/mL |
| Alanine | 20 mM |
| MC and alanine | MC 0.05% w/v and alanine 20 mM |
| MC and HSA | MC 0.05% w/v and HSA 1 mg/mL |
| MC and HSA and alanine | MC 0.05% w/v, HSA 1 mg/mL and alanine 20 mM |
| Vehicle ID | Composition of Aqueous Vehicle | Corresponding FGF-2 Sample ID |
|---|---|---|
| 1 | Water (control) | F1 |
| 2 | Methylcellulose (MC; 0.05% w/v) | F2 |
| 3 | Alanine (20 mM) | F3 |
| 4 | Human serum albumin (HSA; 1 mg/mL) | F4 |
| 5 | MC (0.05% w/v) and alanine (20 mM) | F5 |
| 6 | MC (0.05% w/v) and HSA (1 mg/mL) | F6 |
| 7 | MC (0.05% w/v), alanine (20 mM) and HSA (1 mg/mL) | F7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benington, L.R.; Rajan, G.; Locher, C.; Lim, L.Y. Stabilisation of Recombinant Human Basic Fibroblast Growth Factor (FGF-2) against Stressors Encountered in Medicinal Product Processing and Evaluation. Pharmaceutics 2021, 13, 1762. https://doi.org/10.3390/pharmaceutics13111762
Benington LR, Rajan G, Locher C, Lim LY. Stabilisation of Recombinant Human Basic Fibroblast Growth Factor (FGF-2) against Stressors Encountered in Medicinal Product Processing and Evaluation. Pharmaceutics. 2021; 13(11):1762. https://doi.org/10.3390/pharmaceutics13111762
Chicago/Turabian StyleBenington, Leah R., Gunesh Rajan, Cornelia Locher, and Lee Yong Lim. 2021. "Stabilisation of Recombinant Human Basic Fibroblast Growth Factor (FGF-2) against Stressors Encountered in Medicinal Product Processing and Evaluation" Pharmaceutics 13, no. 11: 1762. https://doi.org/10.3390/pharmaceutics13111762
APA StyleBenington, L. R., Rajan, G., Locher, C., & Lim, L. Y. (2021). Stabilisation of Recombinant Human Basic Fibroblast Growth Factor (FGF-2) against Stressors Encountered in Medicinal Product Processing and Evaluation. Pharmaceutics, 13(11), 1762. https://doi.org/10.3390/pharmaceutics13111762







