Impact of Compression Force on Mechanical, Textural, Release and Chewing Perception Properties of Compressible Medicated Chewing Gums
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Medicated Chewing Gums
2.3. Evaluation of Prepared MCGs
2.3.1. Geometrical Parameters of MCGs
2.3.2. Mechanical Resistance of MCGs
2.3.3. Surface and Internal Structure Characterization
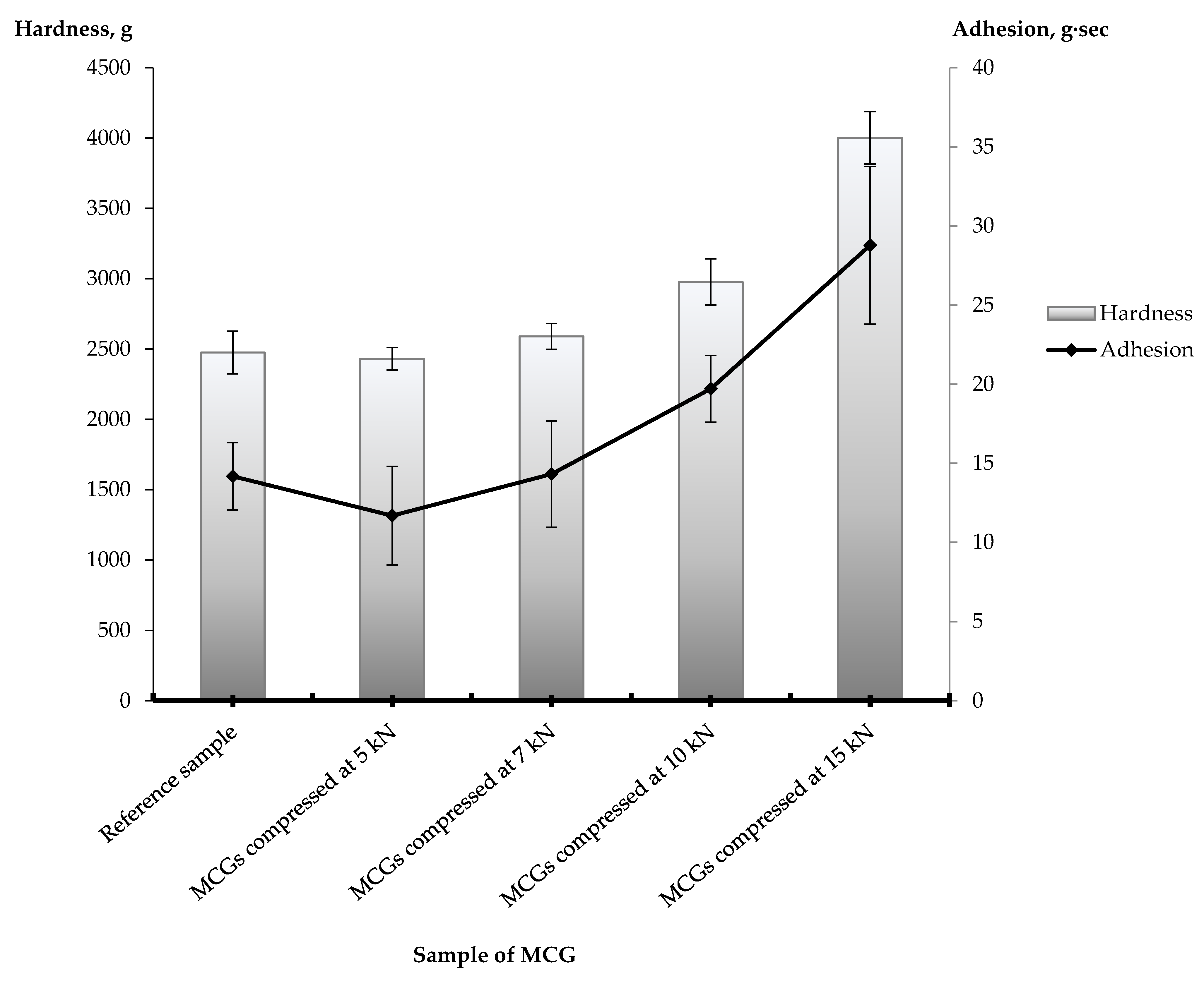
2.3.4. Texture Profile Analysis
2.3.5. In Vitro Drug Release Study
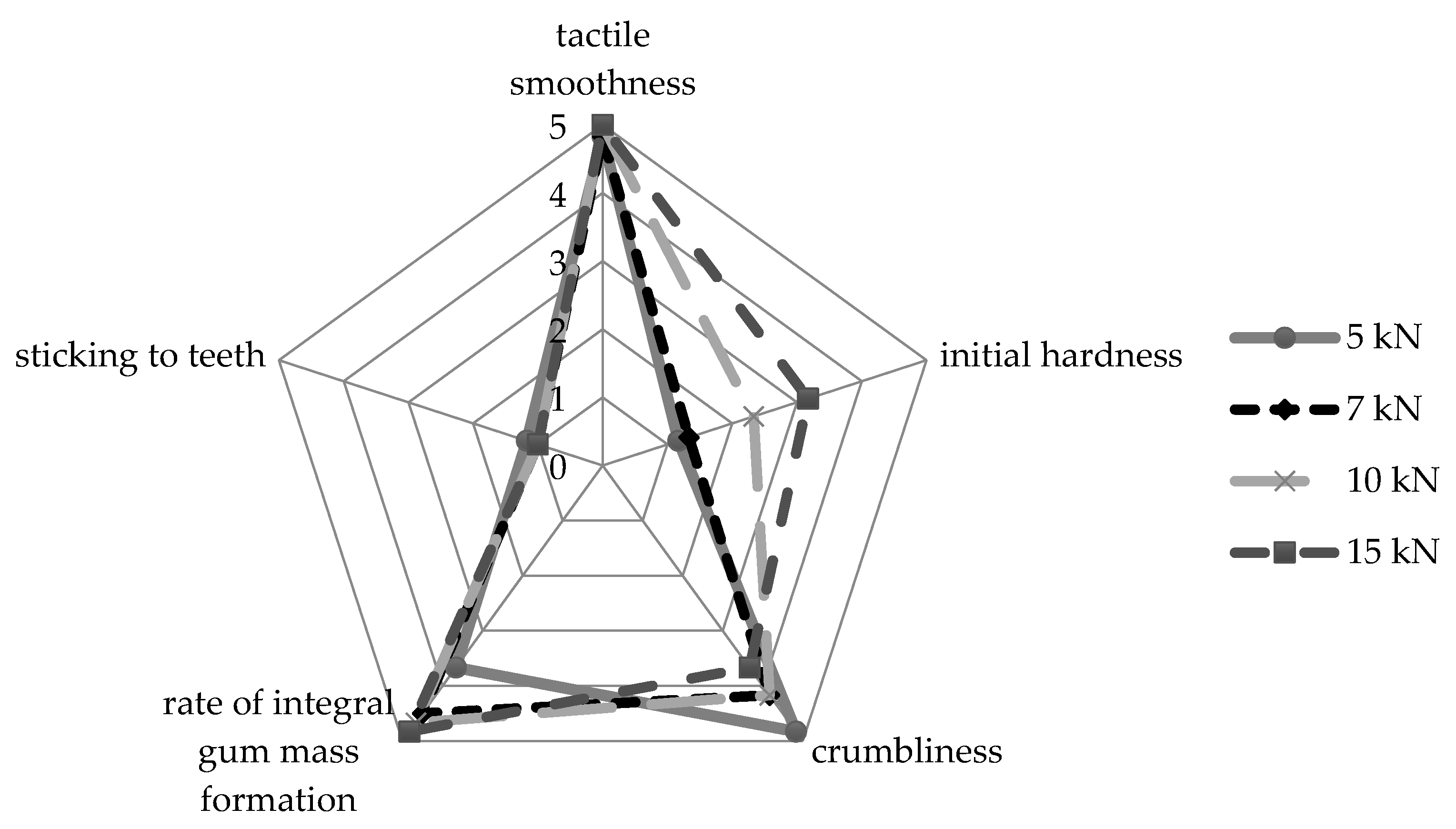
2.3.6. Chewing Perception Assessment
2.4. Statistical Analysis
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kubo, K.Y.; Iinuma, M.; Chen, H. Mastication as a Stress-Coping Behavior. BioMed Res. Int. 2015, 2015, 876409. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.P. Chewing gum and stress reduction. J. Clin. Transl. Res. 2016, 2, 52–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marzouk, M.A.; Darwish, M.K.; Abd El-Fattah, M.A. Development of medicated chewing gum of taste masked levocetirizine dihydrochloride using different gum bases: In vitro and in vivo evaluation. Drug Dev. Ind. Pharm. 2020, 46, 395–402. [Google Scholar] [CrossRef]
- Mostafavi, S.A.; Varshosaz, J.; Arabian, S. Formulation development and evaluation of metformin chewing gum with bitter taste masking. Adv. Biomed. Res. 2014, 3, 92. [Google Scholar] [CrossRef]
- Akbal, O.; Cevher, E.; Araman, A.O. The development and in vitro evaluation of benzydamine hydrochloride medicated chewing gum formulations. Istanb. J. Pharm. 2017, 47, 45–51. [Google Scholar] [CrossRef]
- Wessel, S.W.; van der Mei, H.C.; Maitra, A.; Dodds, M.W.; Busscher, H.J. Potential benefits of chewing gum for the delivery of oral therapeutics and its possible role in oral healthcare. Expert Opin. Drug Deliv. 2016, 13, 1421–1431. [Google Scholar] [CrossRef] [PubMed]
- Thivya, P.; Durgadevi, M.; Sinija, V.R.N. Biodegradable medicated chewing gum: A modernized system for delivering bioactive compounds. Future Foods 2021, 4, 100054. [Google Scholar] [CrossRef]
- Motwani, N.V.; Suryavanshi, K.A. Medicated Chewing Gum—A Review. Inter. J. Pharma O2 2021, 3, 167–174. [Google Scholar]
- Parmar, V.W.; Thosar, M. A comprehensive review on: Medicated chewing gum. Int. J. Res. Pharm. Biomed. Sci. 2012, 3, 894–907. [Google Scholar]
- Aslani, A.; Rostami, F. Medicated chewing gum, a novel drug delivery system. J. Res. Med. Sci. 2015, 20, 403–411. [Google Scholar]
- Kaushik, P.; Kaushik, D. Medicated Chewing Gums: Recent Patents and Patented Technology Platforms. Recent Pat. Drug Deliv. Formul. 2019, 13, 184–191. [Google Scholar] [CrossRef]
- Al Hagbani, T.; Nazzal, S. Development of postcompressional textural tests to evaluate the mechanical properties of medicated chewing gum tablets with high drug loadings. J. Texture Stud. 2018, 49, 30–37. [Google Scholar] [CrossRef]
- Al Hagbani, T.; Nazzal, S. Medicated Chewing Gums (MCGs): Composition, Production, and Mechanical Testing. AAPS PharmSciTech 2018, 19, 2908–2920. [Google Scholar] [CrossRef]
- Council of Europe. European Pharmacopoeia, 9th ed.; Council of Europe: Strasbourg, France, 2016. [Google Scholar]
- United States Pharmacopeial Convention. The United States Pharmacopeia and National Formulary, 39th ed.; (USP39-NF34); The United States Pharmacopeial Convention: Rockville, MD, USA, 2016. [Google Scholar]
- Paradkar, M.; Gajra, B.; Patel, B. Formulation development and evaluation of medicated chewing gum of anti-emetic drug. Saudi Pharm. J. 2016, 24, 153–164. [Google Scholar] [CrossRef] [Green Version]
- Maslii, Y.; Ruban, L.; Yevtifieieva, O.; Hrudko, V.; Gureyeva, S.; Goy, A.; Kolisnyk, T. Development and uniformity evaluation of low-dose medicated chewing gums prepared by compression method. Ceska Slov. Farm. 2020, 69, 33–42. [Google Scholar]
- Maslii, Y.; Ruban, O.; Kolisnyk, T. Investigations with the aim of obtaining a mass for pressing medicated chewing gums “Lysodent C”. ScienceRise Pharm. Sci. 2019, 3, 11–16. [Google Scholar] [CrossRef] [Green Version]
- Maslii, Y.; Ruban, O.; Kutsenko, S. Selection of flavour additives and method of their introduction in the composition of compressed medicated chewing gums. EUREKA Health Sci. 2020, 2, 59–66. [Google Scholar] [CrossRef] [Green Version]
- Maslii, Y.S.; Ruban, O.A.; Kolisnyk, T.E.; Liapunova, O.A. The substantiation of the method for introduction of lysozyme hydrochloride and ascorbic acid in the composition of the medicated chewing gum “Lysodent C”. Ukr. Biopharm. J. 2019, 3, 14–22. [Google Scholar] [CrossRef]
- Kása, P.; Jójárt, I.; Kelemen, A.; Pintye-Hódi, K. Formulation study of directly compressible chewable polymers containing ascorbic acid. Pharm. Dev. Technol. 2013, 18, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Jójárt, I.; Kása, P., Jr.; Kelemen, A.; Pintye-Hódi, K. Study of the compressibility of chewing gum and its applicability as an oral drug delivery system. Pharm. Dev. Technol. 2016, 21, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Jójárt, I.; Kelemen, A.; Kása, P., Jr.; Pintye-Hódi, K. Tracking of the postcompressional behaviour of chewing gum tablets. Compos. Part B 2013, 49, 1–5. [Google Scholar] [CrossRef]
- Lysozyme hydrochloride. In The Japanese Pharmacopoeia, 17th ed.; (JP17); Ministry of Health, Labour and Welfare: Tokyo, Japan, 2016; p. 1181.
- Paul, S.; Sun, C.C. Dependence of Friability on Tablet Mechanical Properties and a Predictive Approach for Binary Mixtures. Pharm. Res. 2017, 34, 2901–2909. [Google Scholar] [CrossRef] [PubMed]
- Swaminathan, S.; Ramey, B.; Hilden, J.; Wassgren, C. Characterizing the powder punch-face adhesive interaction during the unloading phase of powder compaction. Powder Technol. 2017, 315, 410–421. [Google Scholar] [CrossRef]
- Hermans, A.; Abend, A.M.; Kesisoglou, F.; Flanagan, T.; Cohen, M.J.; Diaz, D.A.; Mao, Y.; Zhang, L.; Webster, G.K.; Lin, Y.; et al. Approaches for Establishing Clinically Relevant Dissolution Specifications for Immediate Release Solid Oral Dosage Forms. AAPS J. 2017, 19, 1537–1549. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Dietetic Products, Nutrition and Allergies. Scientific Opinion on the substantiation of a health claim related to sugar free chewing gum and reduction of tooth demineralisation which reduces the risk of dental caries pursuant to Article 14 of Regulation (EC) No 1924/2006. EFSA J. 2010, 8, 1775. [Google Scholar] [CrossRef]
- George, M.K.; Bogosian, A.; Tapper, K. The effect of implementation intentions on use of dental chewing gum. Health Psychol. Open 2019, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morjaria, Y.; Irwin, W.J.; Barnett, P.X.; Chan, R.S.; Conway, B.R. In Vitro Release of Nicotine from Chewing Gum Formulations. Dissolution Technol. 2004, 11, 12–15. [Google Scholar] [CrossRef]
- Sorsa, T.; Tjäderhane, L.; Konttinen, Y.T.; Lauhio, A.; Salo, T.; Lee, H.M.; Golub, L.M.; Brown, D.L.; Mäntylä, P. Matrix metalloproteinases: Contribution to pathogenesis, diagnosis and treatment of periodontal inflammation. Ann. Med. 2006, 38, 306–321. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.C.; Anoop, K.R. Intraperiodontal pocket: An ideal route for local antimicrobial drug delivery. J. Adv. Pharm. Technol. Res. 2012, 3, 9–15. [Google Scholar] [CrossRef]
- Tye, C.K.; Sun, C.C.; Amidon, G.E. Evaluation of the effects of tableting speed on the relationships between compaction pressure, tablet tensile strength, and tablet solid fraction. J. Pharm. Sci. 2005, 94, 465–472. [Google Scholar] [CrossRef]


| Name of Ingredient | Amount, mg/per Gum | Function in the MCG Formulation | Manufacturer |
|---|---|---|---|
| Lysozyme hydrochloride | 10.0 | API | Bouwhuis Enthoven B.V., Raalte, The Netherlands |
| Ascorbic acid | 20.0 | API | Foodchem International Corporation, Shanghai, China |
| Solo Sucralose Non-Micronised NF | 1.5 | Intense sweetener | V.B. Medicare Pvt. Ltd., Hosur, India |
| Nat Apple Flavor Wonf | 20.0 | Taste additive | Kerry Inc., Kuala Lumpur, Malaysia |
| Apple FLV LQD FA-BO2980 | 6.0 | Flavor | Kerry Inc., Kuala Lumpur, Malaysia |
| Syloid® 244FP | 10.0 | Moisture scavenger, carrier for liquid flavor, glidant | Grace GmbH & Co. KG, Worms, Germany |
| Magnesium stearate | 15.0 | Lubricant | S.D. Fine Chemicals Ltd., Mumbai, India |
| Health in Gum® PWD 01 | Up to 1000.0 | Chewing gum base | Cafosa Gum SA, Barcelona, Spain |
| Compression Force Value, kN | Geometrical Parameters, mm | Resistance to Crushing, N | Friability, % | |
|---|---|---|---|---|
| Diameter | Thickness | |||
| 5 | 13.02 ± 0.01 | 5.62 ± 0.03 | 71 ± 2 | 0.121 ± 0.001 |
| 7 | 13.01 ± 0.01 | 5.50 ± 0.02 | 78 ± 2 | 0.102 ± 0.001 |
| 10 | 13.01 ± 0.01 | 5.44 ± 0.05 | 80 ± 1 | 0.090 ± 0.001 |
| 15 | 13.00 ± 0.01 | 5.21 ± 0.03 | 92 ± 2 | 0.054 ± 0.001 |
| Compression Force Value, kN | API | Released Amount of APIs, % | ||||
|---|---|---|---|---|---|---|
| Sampling Time, min | ||||||
| 5 | 10 | 15 | 20 | 30 | ||
| 5 | AsA | 81.35 ± 1.90 | 94.87 ± 1.56 | 97.05 ± 2.45 | 98.12 ± 0.82 | 99.08 ± 1.47 |
| LH | 81.25 ± 0.38 | 94.68 ± 0.63 | 97.75 ± 0.48 | 98.55 ± 0.57 | 99.34 ± 0.91 | |
| 7 | AsA | 79.86 ± 2.53 | 93.34 ± 1.80 | 97.65 ± 1.08 | 98.93 ± 1.07 | 99.55 ± 0.52 |
| LH | 82.95 ± 0.56 | 95.83 ± 0.45 | 98.17 ± 0.78 | 98.90 ± 0.45 | 99.71 ± 0.59 | |
| 10 | AsA | 78.19 ± 2.02 | 90.62 ± 1.77 | 92.11 ± 1.41 | 94.90 ± 1.43 | 98.88 ± 1.52 |
| LH | 80.29 ± 0.69 | 88.12 ± 0.31 | 92.21 ± 0.47 | 94.02 ± 0.37 | 97.67 ± 0.56 | |
| 15 | AsA | 75.66 ± 1.55 | 85.58 ± 0.93 | 89.25 ± 2.05 | 93.45 ± 1.48 | 96.11 ± 1.95 |
| LH | 77.13 ± 0.52 | 90.25 ± 0.66 | 91.77 ± 0.48 | 92.45 ± 0.34 | 95.11 ± 0.36 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maslii, Y.; Kolisnyk, T.; Ruban, O.; Yevtifieieva, O.; Gureyeva, S.; Goy, A.; Kasparaviciene, G.; Kalveniene, Z.; Bernatoniene, J. Impact of Compression Force on Mechanical, Textural, Release and Chewing Perception Properties of Compressible Medicated Chewing Gums. Pharmaceutics 2021, 13, 1808. https://doi.org/10.3390/pharmaceutics13111808
Maslii Y, Kolisnyk T, Ruban O, Yevtifieieva O, Gureyeva S, Goy A, Kasparaviciene G, Kalveniene Z, Bernatoniene J. Impact of Compression Force on Mechanical, Textural, Release and Chewing Perception Properties of Compressible Medicated Chewing Gums. Pharmaceutics. 2021; 13(11):1808. https://doi.org/10.3390/pharmaceutics13111808
Chicago/Turabian StyleMaslii, Yuliia, Tetiana Kolisnyk, Olena Ruban, Olga Yevtifieieva, Svitlana Gureyeva, Andriy Goy, Giedre Kasparaviciene, Zenona Kalveniene, and Jurga Bernatoniene. 2021. "Impact of Compression Force on Mechanical, Textural, Release and Chewing Perception Properties of Compressible Medicated Chewing Gums" Pharmaceutics 13, no. 11: 1808. https://doi.org/10.3390/pharmaceutics13111808
APA StyleMaslii, Y., Kolisnyk, T., Ruban, O., Yevtifieieva, O., Gureyeva, S., Goy, A., Kasparaviciene, G., Kalveniene, Z., & Bernatoniene, J. (2021). Impact of Compression Force on Mechanical, Textural, Release and Chewing Perception Properties of Compressible Medicated Chewing Gums. Pharmaceutics, 13(11), 1808. https://doi.org/10.3390/pharmaceutics13111808








