New Approaches in Nanomedicine for Ischemic Stroke
Abstract
:1. Introduction
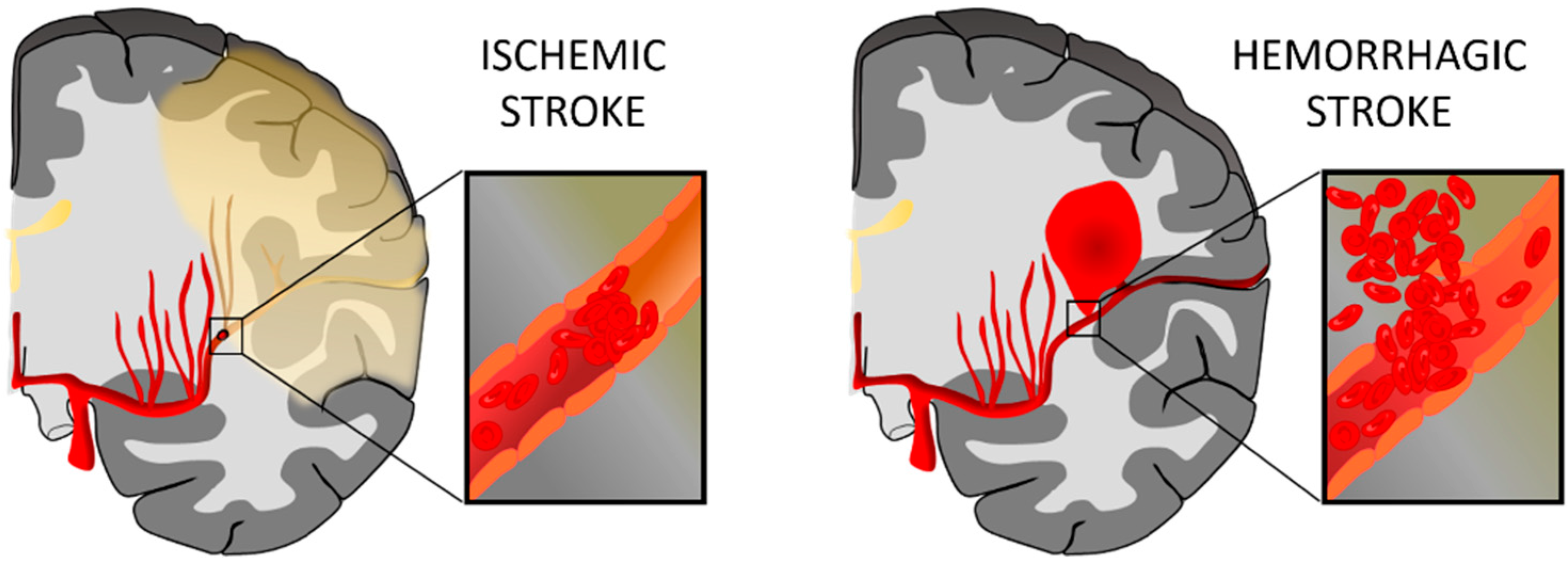
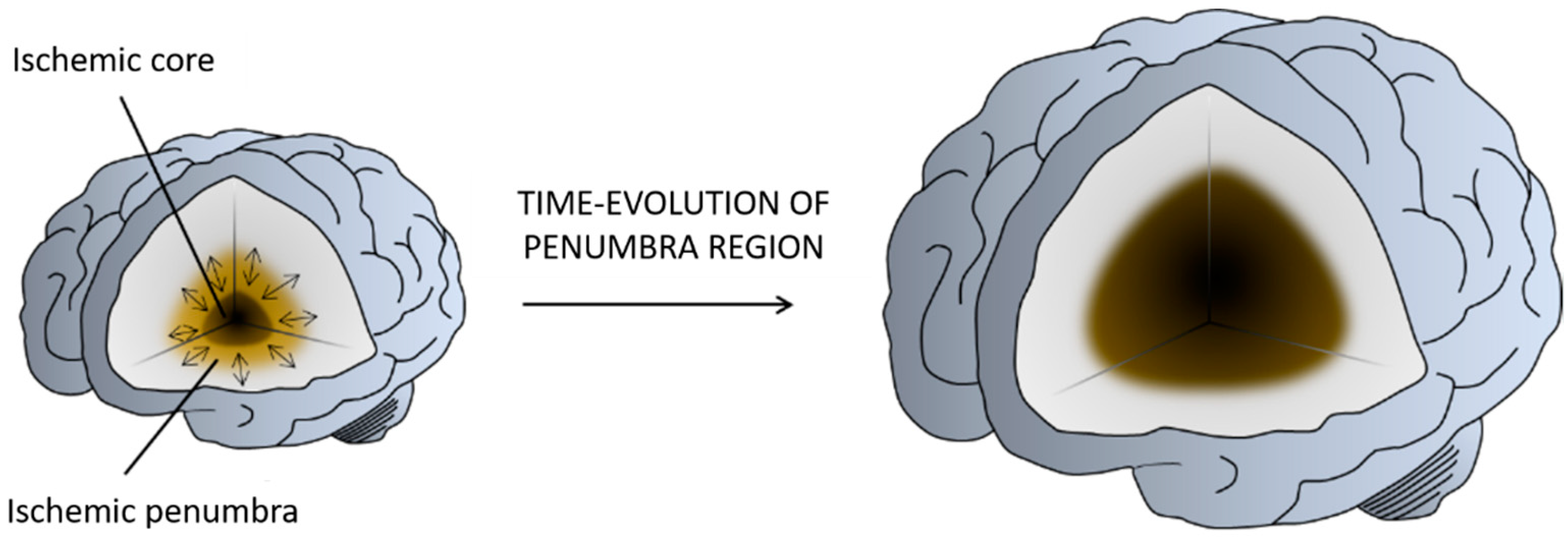
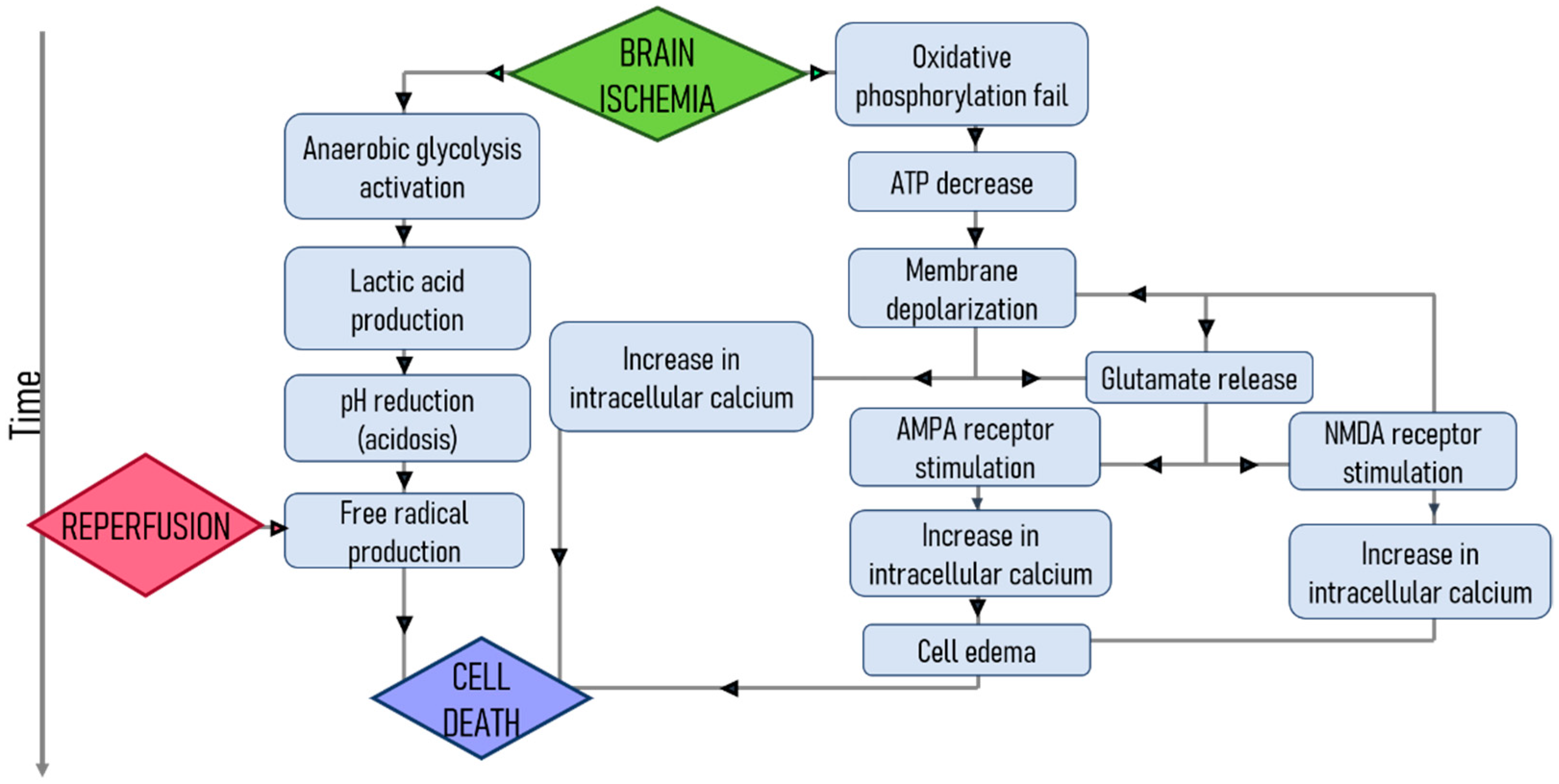
1.1. Stroke
1.2. Nanomedicine
2. Nanomedicine for Stroke Diagnosis
3. Nanoparticles for Recanalization Therapies
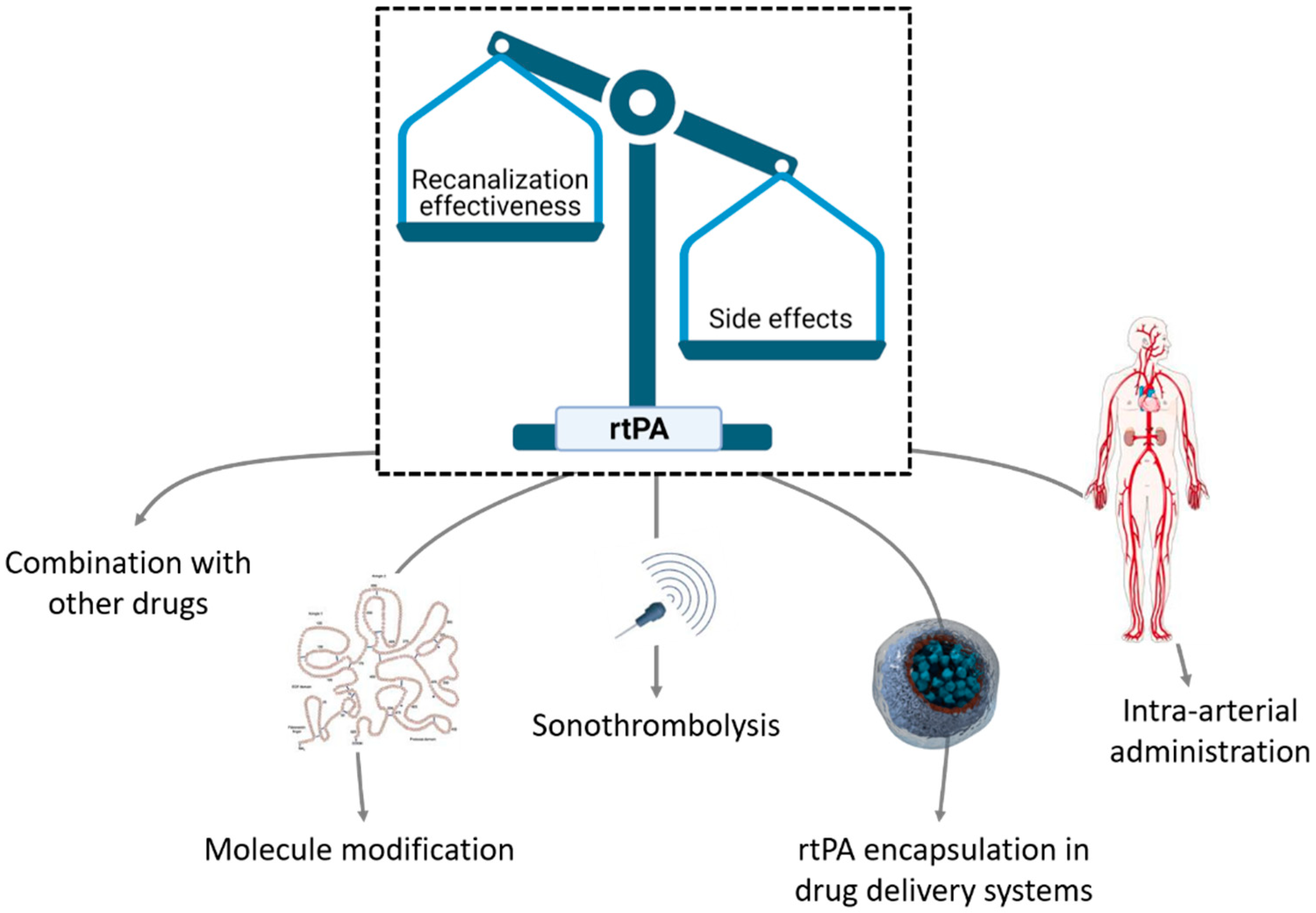
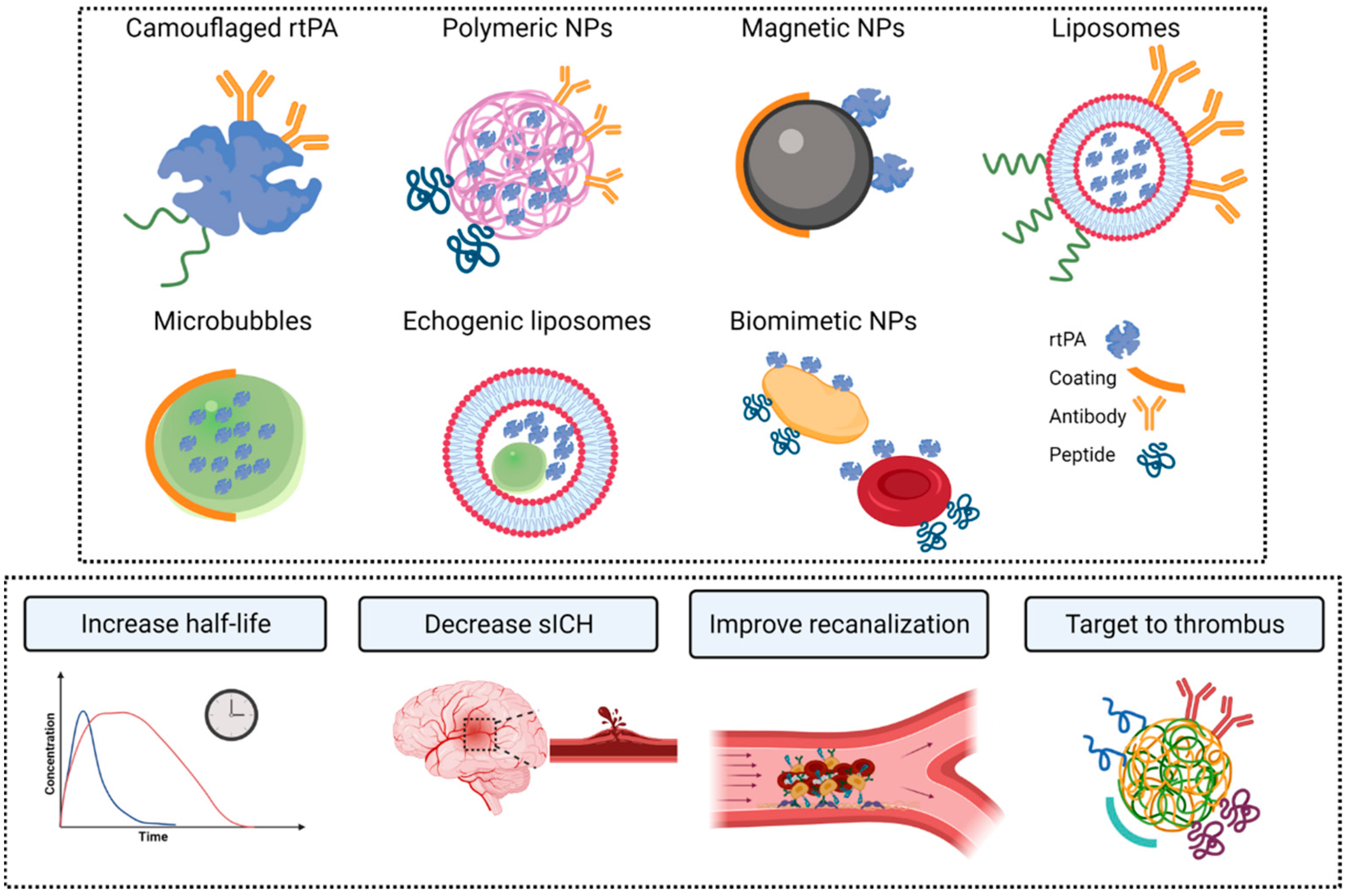
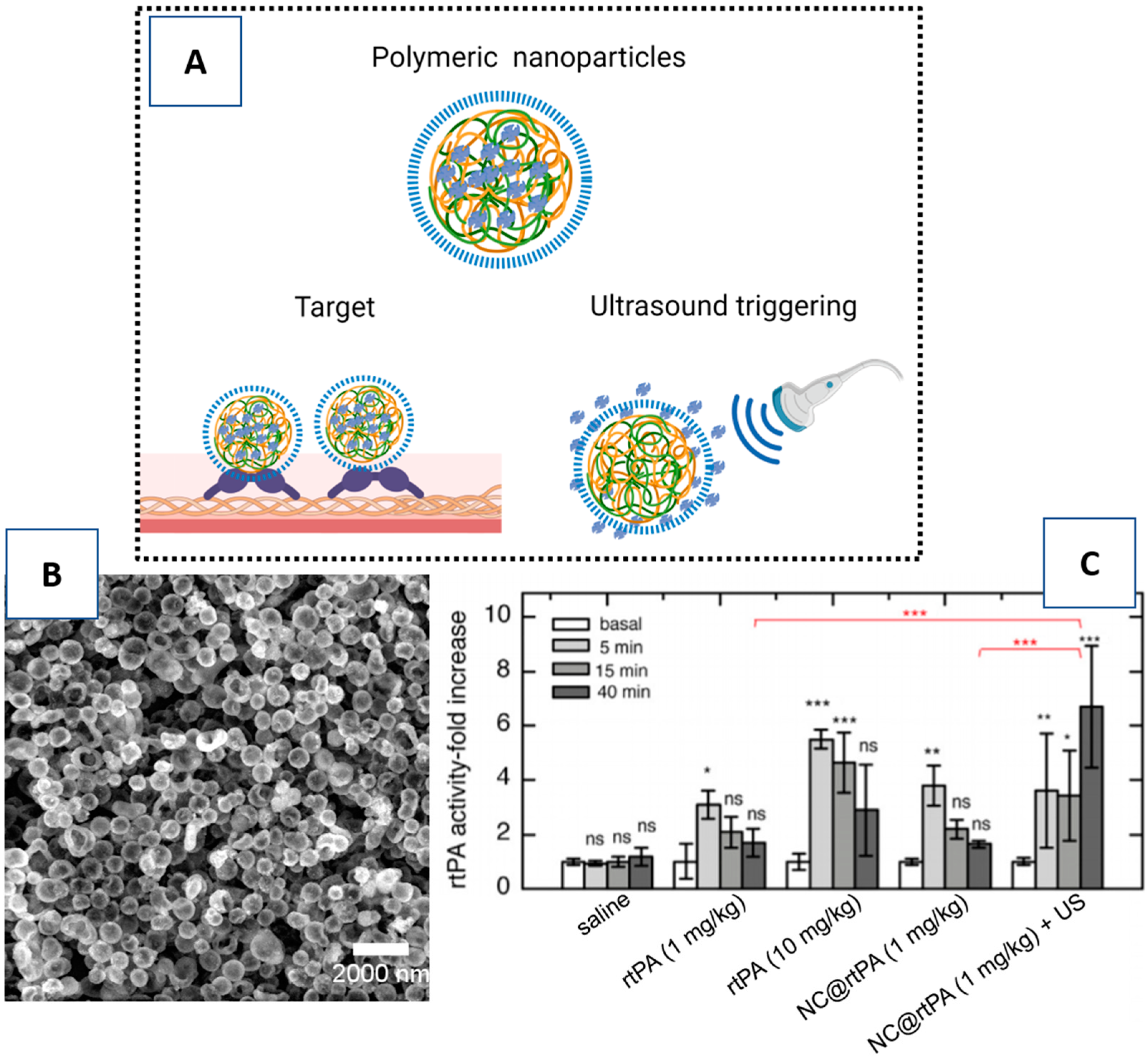
3.1. Nanocarriers for rtPA
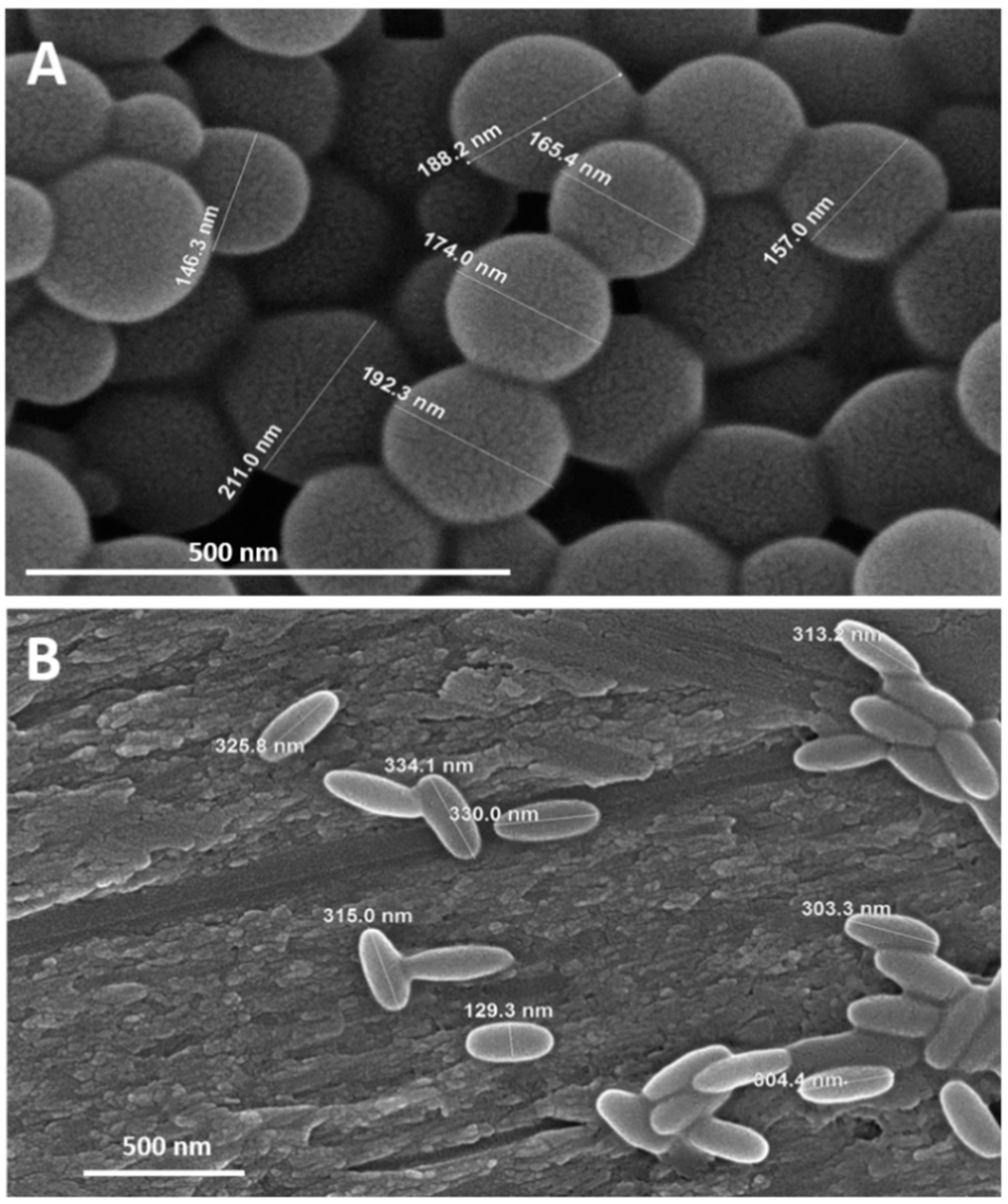
3.2. Clot Targets for rtPA Nanocarrier Vectorization
3.3. Triggering Controlled Release
4. Nanoparticles as a Therapy for Ischemic Brain Protection
4.1. Inflammation
4.2. Oxidative Stress
4.3. Glutamate Excitotoxicity
4.4. Combination of Thrombolytics and Neuroprotectants in Nanomedicine
5. Nanomedicine for Stroke Recovery Therapies
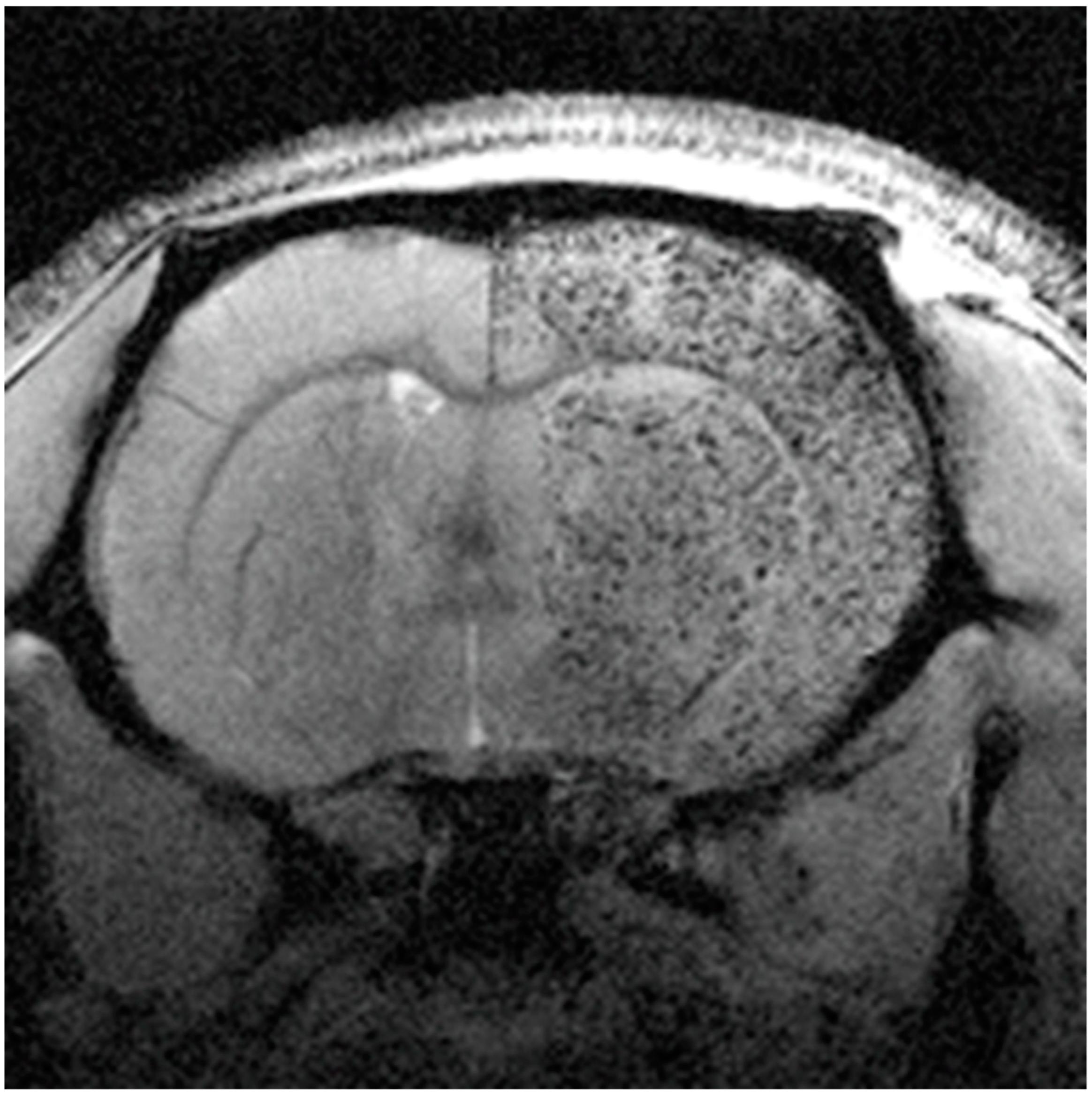
5.1. MRI Contrast Cell Agents
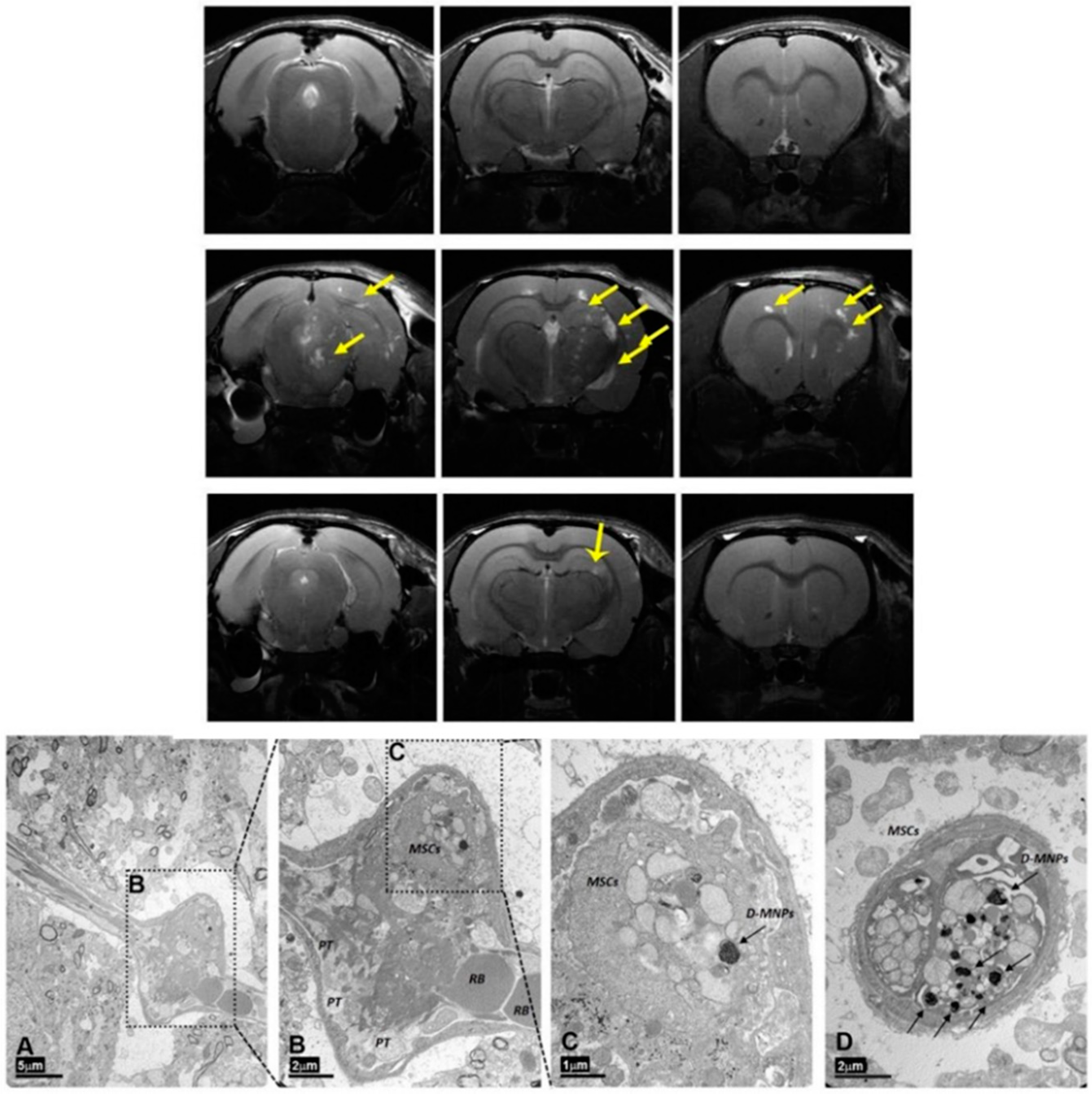
5.2. MNPs for MRI Cell Tracking in Stroke
5.3. Magnetic Vectorization
6. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef]
- Campbell, B.C.V.; De Silva, D.A.; MacLeod, M.R.; Coutts, S.B.; Schwamm, L.H.; Davis, S.M.; Donnan, G.A. Ischaemic stroke. Nat. Rev. Dis. Prim. 2019, 5, 1–22. [Google Scholar] [CrossRef]
- Da Silva-Candal, A.; Argibay, B.; Iglesias-Rey, R.; Vargas, Z.; Vieites-Prado, A.; López-Arias, E.; Rodríguez-Castro, E.; López-Dequidt, I.; Rodríguez-Yáñez, M.; Piñeiro, Y.; et al. Vectorized nanodelivery systems for ischemic stroke: A concept and a need. J. Nanobiotechnol. 2017, 15, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Lo, E.H. A new penumbra: Transitioning from injury into repair after stroke. Nat. Med. 2008, 14, 497–500. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Cabrer, P.; Campos, F.; Sobrino, T.; Castillo, J. Targeting the Ischemic Penumbra. Stroke 2010, 42, S7–S11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baron, J.-C. Protecting the ischaemic penumbra as an adjunct to thrombectomy for acute stroke. Nat. Rev. Neurol. 2018, 14, 325–337. [Google Scholar] [CrossRef]
- Zi, W.; Qiu, Z.; Li, F.; Sang, H.; Wu, D.; Luo, W.; Liu, S.; Yuan, J.; Song, J.; Shi, Z.; et al. Effect of endovascular treatment alone vs intravenous alteplase plus endovascular treatment on functional independence in patients with acute ischemic stroke: The devt randomized clinical trial. JAMA 2021, 325, 234. [Google Scholar] [CrossRef]
- Chamorro, Á.; Dirnagl, U.; Urra, X.; Planas, A.M. Neuroprotection in acute stroke: Targeting excitotoxicity, oxidative and nitrosative stress, and inflammation. Lancet Neurol. 2016, 15, 869–881. [Google Scholar] [CrossRef]
- Laso-García, F.; Diekhorst, L.; Frutos, M.C.G.-D.; Otero-Ortega, L.; Fuentes, B.; Ruiz-Ares, G.; Díez-Tejedor, E.; Gutiérrez-Fernández, M. Cell-Based Therapies for Stroke: Promising Solution or Dead End? Mesenchymal Stem Cells and Comorbidities in Preclinical Stroke Research. Front. Neurol. 2019, 10, 332. [Google Scholar] [CrossRef]
- Dilnawaz, F.; Acharya, S.; Sahoo, S.K. Recent trends of nanomedicinal approaches in clinics. Int. J. Pharm. 2018, 538, 263–278. [Google Scholar] [CrossRef]
- Pelaz, B.; Alexiou, C.; Alvarez-Puebla, R.A.; Alves, F.; Andrews, A.M.; Ashraf, S.; Balogh, L.P.; Ballerini, L.; Bestetti, A.; Brendel, C.; et al. Diverse Applications of Nanomedicine. ACS Nano 2017, 11, 2313–2381. [Google Scholar] [CrossRef] [Green Version]
- Belliere, J.; De Lizarrondo, S.M.; Choudhury, R.P.; Quenault, A.; Le Béhot, A.; Delage, C.; Chauveau, D.; Schanstra, J.P.; Bascands, J.-L.; Vivien, D.; et al. Unmasking Silent Endothelial Activation in the Cardiovascular System Using Molecular Magnetic Resonance Imaging. Theranostics 2015, 5, 1187–1202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gauberti, M.; Montagne, A.; Quenault, A.; Vivien, D. Molecular magnetic resonance imaging of brain-immune interactions. Front. Cell. Neurosci. 2014, 8, 389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gauberti, M.; Fournier, A.P.; Docagne, F.; Vivien, D.; De Lizarrondo, S.M. Molecular Magnetic Resonance Imaging of Endothelial Activation in the Central Nervous System. Theranostics 2018, 8, 1195–1212. [Google Scholar] [CrossRef]
- Shapiro, E.M.; Skrtic, S.; Koretsky, A.P. Sizing it up: Cellular MRI using micron-sized iron oxide particles. Magn. Reson. Med. 2005, 53, 329–338. [Google Scholar] [CrossRef]
- Zinnhardt, B.; Wiesmann, M.; Honold, L.; Barca, C.; Schäfers, M.; Kiliaan, A.J.; Jacobs, A.H. In vivo imaging biomarkers of neuroinflammation in the development and assessment of stroke therapies—towards clinical translation. Theranostics 2018, 8, 2603–2620. [Google Scholar] [CrossRef] [PubMed]
- Iadecola, C.; Anrather, J. The immunology of stroke: From mechanisms to translation. Nat. Med. 2011, 17, 796–808. [Google Scholar] [CrossRef] [PubMed]
- Gauberti, M.; Montagne, A.; Marcos-Contreras, O.A.; Le Béhot, A.; Maubert, E.; Vivien, D. Ultra-Sensitive Molecular MRI of Vascular Cell Adhesion Molecule-1 Reveals a Dynamic Inflammatory Penumbra After Strokes. Stroke 2013, 44, 1988–1996. [Google Scholar] [CrossRef] [Green Version]
- Deddens, L.H.; van Tilborg, G.A.; van der Toorn, A.; van der Marel, K.; Paulis, L.E.; van Bloois, L.; Storm, G.; Strijkers, G.J.; Mulder, W.J.; de Vries, H.E.; et al. Mri of icam-1 upregulation after stroke: The importance of choosing the appropriate target-specific particulate contrast agent. Mol. Imaging Biol. 2013, 15, 411. [Google Scholar] [CrossRef]
- Quenault, A.; De Lizarrondo, S.M.; Etard, O.; Gauberti, M.; Orset, C.; Haelewyn, B.; Segal, H.C.; Rothwell, P.M.; Vivien, D.; Touzé, E.; et al. Molecular magnetic resonance imaging discloses endothelial activation after transient ischaemic attack. Brain 2017, 140, 146–157. [Google Scholar] [CrossRef]
- McAteer, M.A.; Schneider, J.E.; Ali, Z.A.; Warrick, N.; Bursill, C.A.; Muhlen, C.V.Z.; Greaves, D.R.; Neubauer, S.; Channon, K.M.; Choudhury, R.P. Magnetic Resonance Imaging of Endothelial Adhesion Molecules in Mouse Atherosclerosis Using Dual-Targeted Microparticles of Iron Oxide. Arter. Thromb. Vasc. Biol. 2008, 28, 77–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.-Y.; Ryu, J.H.; Schellingerhout, D.; Sun, I.-C.; Lee, S.-K.; Jeon, S.; Kim, J.; Kwon, I.C.; Nahrendorf, M.; Ahn, C.-H.; et al. Direct Imaging of Cerebral Thromboemboli Using Computed Tomography and Fibrin-targeted Gold Nanoparticles. Theranostics 2015, 5, 1098–1114. [Google Scholar] [CrossRef] [Green Version]
- Perez-Balderas, F.; Van Kasteren, S.I.; Aljabali, A.A.A.; Wals, K.; Serres, S.; Jefferson, A.; Soto, M.S.; Khrapitchev, A.A.; Larkin, J.R.; Bristow, C.; et al. Covalent assembly of nanoparticles as a peptidase-degradable platform for molecular MRI. Nat. Commun. 2017, 8, 14254. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart disease and stroke statistics-2019 update: A report from the american heart association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef]
- Chapin, J.C.; Hajjar, K.A. Fibrinolysis and the control of blood coagulation. Blood Rev. 2015, 29, 17. [Google Scholar] [CrossRef] [Green Version]
- Lesept, F.; Chevilley, A.; Jezequel, J.; Ladépêche, L.; Macrez, R.; Aimable, M.; Lenoir, S.; Bertrand, T.; Rubrecht, L.; Galea, P.; et al. Tissue-type plasminogen activator controls neuronal death by raising surface dynamics of extrasynaptic NMDA receptors. Cell Death Dis. 2016, 7, e2466. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, R.; Hill, M.D.; Shobha, N.; Menon, B.; Bal, S.; Kochar, P.; Watson, T.; Goyal, M.; Demchuk, A.M. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke: Real-world experience and a call for action. Stroke 2010, 41, 2254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mican, J.; Toul, M.; Bednar, D.; Damborsky, J. Structural Biology and Protein Engineering of Thrombolytics. Comput. Struct. Biotechnol. J. 2019, 17, 917–938. [Google Scholar] [CrossRef]
- Go, A.S.; Mozaffarian, D.; Roger, V.L.; Benjamin, E.J.; Berry, J.D.; Blaha, M.J.; Dai, S.; Ford, E.S.; Fox, C.S.; Franco, S.; et al. Heart Disease and Stroke Statistics--2014 Update: A Report from the American Heart Association. Circulation 2013, 129, e28–e292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Badhiwala, J.H.; Nassiri, F.; Alhazzani, W.; Selim, M.H.; Farrokhyar, F.; Spears, J.; Kulkarni, A.V.; Singh, S.; Alqahtani, A.; Rochwerg, B.; et al. Endovascular thrombectomy for acute ischemic stroke: A meta-analysis. JAMA 2015, 314, 1832. [Google Scholar] [CrossRef]
- Campbell, B.C.; Mitchell, P.J.; Churilov, L.; Yassi, N.; Kleinig, T.J.; Dowling, R.J.; Yan, B.; Bush, S.J.; Dewey, H.M.; Thijs, V.; et al. Tenecteplase versus Alteplase before Thrombectomy for Ischemic Stroke. N. Engl. J. Med. 2018, 378, 1573–1582. [Google Scholar] [CrossRef] [PubMed]
- Bonnard, T.; Gauberti, M.; De Lizarrondo, S.M.; Campos, F.; Vivien, D. Recent Advances in Nanomedicine for Ischemic and Hemorrhagic Stroke. Stroke 2019, 50, 1318–1324. [Google Scholar] [CrossRef]
- Liu, S.; Feng, X.; Jin, R.; Li, G. Tissue plasminogen activator-based nanothrombolysis for ischemic stroke. Expert Opin. Drug Deliv. 2018, 15, 173–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heeremans, J.L.M.; Prevost, R.; E A Bekkers, M.; Los, P.; Emeis, J.J.; Kluft, C.; A Crommelin, D.J. Thrombolytic Treatment with Tissue-type Plasminogen Activator (t-PA) Containing Liposomes in Rabbits: A Comparison with Free t-PA. Thromb. Haemost. 1995, 73, 488–494. [Google Scholar] [CrossRef]
- Cheng, R.; Huang, W.; Huang, L.; Yang, B.; Mao, L.; Jin, K.; Zhuge, Q.; Zhao, Y. Acceleration of Tissue Plasminogen Activator-Mediated Thrombolysis by Magnetically Powered Nanomotors. ACS Nano 2014, 8, 7746–7754. [Google Scholar] [CrossRef]
- Hua, X.; Liu, P.; Gao, Y.-H.; Tan, K.-B.; Zhou, L.-N.; Liu, Z.; Li, X.; Zhou, S.-W.; Gao, Y.-J. Construction of thrombus-targeted microbubbles carrying tissue plasminogen activator and their in vitro thrombolysis efficacy: A primary research. J. Thromb. Thrombolysis 2010, 30, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Hua, X.; Zhou, L.; Liu, P.; He, Y.; Tan, K.; Chen, Q.; Gao, Y.; Gao, Y. In vivo thrombolysis with targeted microbubbles loading tissue plasminogen activator in a rabbit femoral artery thrombus model. J. Thromb. Thrombolysis 2014, 38, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Shekhar, H.; Bader, K.B.; Huang, S.; Peng, T.; Huang, S.; McPherson, D.D.; Holland, C.K. In vitro thrombolytic efficacy of echogenic liposomes loaded with tissue plasminogen activator and octafluoropropane gas. Phys. Med. Biol. 2017, 62, 517. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.S.; Chou, N.K.; Chung, T.W. The t-pa-encapsulated plga nanoparticles shelled with cs or cs-grgd alter both permeation through and dissolving patterns of blood clots compared with t-pa solution: An in vitro thrombolysis study. J. Biomed. Mater. Res. Part A 2009, 91, 753. [Google Scholar] [CrossRef]
- Chung, T.W.; Wang, S.S.; Tsai, W.J. Accelerating thrombolysis with chitosan-coated plasminogen activators encapsulated in poly-(lactide-co-glycolide) (plga) nanoparticles. Biomaterials 2008, 29, 228. [Google Scholar] [CrossRef]
- Zhou, J.; Guo, D.; Zhang, Y.; Wu, W.; Ran, H.; Wang, Z. Construction and evaluation of fe(3)o(4)-based plga nanoparticles carrying rtpa used in the detection of thrombosis and in targeted thrombolysis. ACS Appl. Mater. Interfaces 2014, 6, 5566. [Google Scholar] [CrossRef] [PubMed]
- Juenet, M.; Aid-Launais, R.; Li, B.; Berger, A.; Aerts, J.; Ollivier, V.; Nicoletti, A.; Letourneur, D.; Chauvierre, C. Thrombolytic therapy based on fucoidan-functionalized polymer nanoparticles targeting P-selectin. Biomaterials 2018, 156, 204–216. [Google Scholar] [CrossRef] [PubMed]
- Gunawan, S.T.; Kempe, K.; Bonnard, T.; Cui, J.; Alt, K.; Law, L.S.; Wang, X.; Westein, E.; Such, G.K.; Peter, K.; et al. Multifunctional Thrombin-Activatable Polymer Capsules for Specific Targeting to Activated Platelets. Adv. Mater. 2015, 27, 5153–5157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mihalko, E.; Huang, K.; Sproul, E.; Cheng, K.; Brown, A.C. Targeted Treatment of Ischemic and Fibrotic Complications of Myocardial Infarction Using a Dual-Delivery Microgel Therapeutic. ACS Nano 2018, 12, 7826–7837. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, B.; Agrawal, G.; Vyas, S.P. Functionalized carriers for the improved delivery of plasminogen activators. Int. J. Pharm. 2012, 424, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-A.; Ma, Y.-H.; Hsu, T.-Y.; Chen, J.-P. Preparation of Peptide and Recombinant Tissue Plasminogen Activator Conjugated Poly(Lactic-Co-Glycolic Acid) (PLGA) Magnetic Nanoparticles for Dual Targeted Thrombolytic Therapy. Int. J. Mol. Sci. 2020, 21, 2690. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uesugi, Y.; Kawata, H.; Jo, J.-I.; Saito, Y.; Tabata, Y. An ultrasound-responsive nano delivery system of tissue-type plasminogen activator for thrombolytic therapy. J. Control. Release 2010, 147, 269–277. [Google Scholar] [CrossRef]
- Kawata, H.; Uesugi, Y.; Soeda, T.; Takemoto, Y.; Sung, J.-H.; Umaki, K.; Kato, K.; Ogiwara, K.; Nogami, K.; Ishigami, K.; et al. A New Drug Delivery System for Intravenous Coronary Thrombolysis with Thrombus Targeting and Stealth Activity Recoverable by Ultrasound. J. Am. Coll. Cardiol. 2012, 60, 2550–2557. [Google Scholar] [CrossRef] [Green Version]
- Vankayala, R.; Corber, S.R.; Mac, J.T.; Rao, M.P.; Shafie, M.; Anvari, B. Erythrocyte-Derived Nanoparticles as a Theranostic Agent for Near-Infrared Fluorescence Imaging and Thrombolysis of Blood Clots. Macromol. Biosci. 2018, 18, e1700379. [Google Scholar] [CrossRef]
- Xu, J.; Wang, X.; Yin, H.; Cao, X.; Hu, Q.; Lv, W.; Xu, Q.; Gu, Z.; Xin, H. Sequentially Site-Specific Delivery of Thrombolytics and Neuroprotectant for Enhanced Treatment of Ischemic Stroke. ACS Nano 2019, 13, 8577–8588. [Google Scholar] [CrossRef]
- Jung, E.; Kang, C.; Lee, J.; Yoo, D.; Hwang, D.W.; Kim, D.; Park, S.-C.; Lim, S.K.; Song, C.; Lee, D. Molecularly Engineered Theranostic Nanoparticles for Thrombosed Vessels: H2O2-Activatable Contrast-Enhanced Photoacoustic Imaging and Antithrombotic Therapy. ACS Nano 2018, 12, 392–401. [Google Scholar] [CrossRef]
- Kang, C.; Gwon, S.; Song, C.; Kang, P.M.; Park, S.-C.; Jeon, J.; Hwang, D.W.; Lee, D. Fibrin-Targeted and H2O2-Responsive Nanoparticles as a Theranostics for Thrombosed Vessels. ACS Nano 2017, 11, 6194–6203. [Google Scholar] [CrossRef] [PubMed]
- Wei, Z.; Xin, G.; Wang, H.; Zheng, H.; Ji, C.; Gu, J.; Ma, L.; Qin, C.; Xing, Z.; Niu, H.; et al. The diosgenin prodrug nanoparticles with ph-responsive as a drug delivery system uniquely prevents thrombosis without increased bleeding risk. Nanomed. Nanotechnol. Biol. Med. 2018, 14, 673. [Google Scholar] [CrossRef] [PubMed]
- Pawlowski, C.L.; Li, W.; Sun, M.; Ravichandran, K.; Hickman, D.; Kos, C.; Kaur, G.; Gupta, A.S. Platelet microparticle-inspired clot-responsive nanomedicine for targeted fibrinolysis. Biomaterals 2017, 128, 94–108. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, J.; Liu, X.; Huo, P.; Zhang, Y.; Chen, H.; Tian, Q.; Zhang, N. MMP-2-responsive gelatin nanoparticles for synergistic tumor therapy. Pharm. Dev. Technol. 2019, 24, 1002–1013. [Google Scholar] [CrossRef]
- Shargh, V.H.; Hondermarck, H.; Liang, M. Gelatin-albumin hybrid nanoparticles as matrix metalloproteinases-degradable delivery systems for breast cancer therapy. Nanomedicine 2017, 12, 977–989. [Google Scholar] [CrossRef]
- Korin, N.; Kanapathipillai, M.; Matthews, B.D.; Crescente, M.; Brill, A.; Mammoto, T.; Ghosh, K.; Jurek, S.; Bencherif, S.A.; Bhatta, D.; et al. Shear-Activated Nanotherapeutics for Drug Targeting to Obstructed Blood Vessels. Science 2012, 337, 738–742. [Google Scholar] [CrossRef] [Green Version]
- Croissant, J.G.; Fatieiev, Y.; Almalik, A.; Khashab, N.M. Mesoporous Silica and Organosilica Nanoparticles: Physical Chemistry, Biosafety, Delivery Strategies, and Biomedical Applications. Adv. Heal. Mater. 2018, 7, 7. [Google Scholar] [CrossRef] [Green Version]
- Zhang, F.; Liu, Y.; Lei, J.; Wang, S.; Ji, X.; Liu, H.; Yang, Q. Metal-organic-framework-derived carbon nanostructures for site-specific dual-modality photothermal/photodynamic thrombus therapy. Adv. Sci. 2019, 6, 1901378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, C.-H.; Hsu, H.-L.; Chen, J.-P.; Wu, T.; Ma, Y.-H. Thrombolysis induced by intravenous administration of plasminogen activator in magnetoliposomes: Dual targeting by magnetic and thermal manipulation. Nanomed. Nanotechnol. Biol. Med. 2019, 20, 101992. [Google Scholar] [CrossRef]
- Chen, J.-P.; Liu, C.-H.; Hsu, H.-L.; Wu, T.; Lu, Y.-J.; Ma, Y.-H. Magnetically controlled release of recombinant tissue plasminogen activator from chitosan nanocomposites for targeted thrombolysis. J. Mater. Chem. B 2016, 4, 2578–2590. [Google Scholar] [CrossRef]
- Cervadoro, A.; Cho, M.; Key, J.; Cooper, C.; Stigliano, C.; Aryal, S.; Brazdeikis, A.; Leary, J.F.; Decuzzi, P. Synthesis of Multifunctional Magnetic NanoFlakes for Magnetic Resonance Imaging, Hyperthermia, and Targeting. ACS Appl. Mater. Interfaces 2014, 6, 12939–12946. [Google Scholar] [CrossRef] [Green Version]
- Hu, J.; Huang, S.; Zhu, L.; Huang, W.; Zhao, Y.; Jin, K.; Zhuge, Q. Tissue Plasminogen Activator-Porous Magnetic Microrods for Targeted Thrombolytic Therapy after Ischemic Stroke. ACS Appl. Mater. Interfaces 2018, 10, 32988–32997. [Google Scholar] [CrossRef]
- Laing, S.T.; Moody, M.R.; Kim, H.; Smulevitz, B.; Huang, S.-L.; Holland, C.K.; McPherson, D.D.; Klegerman, M.E. Thrombolytic efficacy of tissue plasminogen activator-loaded echogenic liposomes in a rabbit thrombus model. Thromb. Res. 2012, 130, 629–635. [Google Scholar] [CrossRef] [Green Version]
- Correa-Paz, C.; Poupard, M.F.N.; Polo, E.; Pérez, M.R.; Taboada, P.; Iglesias-Rey, R.; Hervella, P.; Sobrino, T.; Vivien, D.; Castillo, J.; et al. In vivo ultrasound-activated delivery of recombinant tissue plasminogen activator from the cavity of sub-micrometric capsules. J. Control. Release 2019, 308, 162–171. [Google Scholar] [CrossRef]
- Ginsberg, M.D. Neuroprotection for ischemic stroke: Past, present and future. Neuropharmacology 2008, 55, 363–389. [Google Scholar] [CrossRef] [Green Version]
- Tian, X.; Fan, T.; Zhao, W.; Abbas, G.; Han, B.; Zhang, K.; Li, N.; Liu, N.; Liang, W.; Huang, H.; et al. Recent advances in the development of nanomedicines for the treatment of ischemic stroke. Bioact. Mater. 2021, 6, 2854–2869. [Google Scholar] [CrossRef]
- Shekhar, S.; Cunningham, M.W.; Pabbidi, M.R.; Wang, S.; Booz, G.W.; Fan, F. Targeting vascular inflammation in ischemic stroke: Recent developments on novel immunomodulatory approaches. Eur. J. Pharmacol. 2018, 833, 531–544. [Google Scholar] [CrossRef] [PubMed]
- Malone, K.; Amu, S.; Moore, A.C.; Waeber, C. Immunomodulatory Therapeutic Strategies in Stroke. Front. Pharmacol. 2019, 10, 630. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siniscalchi, A.; Iannacchero, R.; Anticoli, S.; Pezzella, F.R.; De Sarro, G.; Gallelli, L. Anti-inflammatory strategies in stroke: A potential therapeutic target. Curr. Vasc. Pharmacol. 2015, 14, 98–105. [Google Scholar] [CrossRef]
- Tian, T.; Zhang, H.-X.; He, C.-P.; Fan, S.; Zhu, Y.-L.; Qi, C.; Huang, N.-P.; Xiao, Z.-D.; Lu, Z.-H.; Tannous, B.A.; et al. Surface functionalized exosomes as targeted drug delivery vehicles for cerebral ischemia therapy. Biomaterals 2018, 150, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Feng, L.; Dou, C.; Xia, Y.; Li, B.; Zhao, M.; Yu, P.; Zheng, Y.; El-Toni, A.M.; Atta, N.F.; Galal, A.; et al. Neutrophil-like Cell-Membrane-Coated Nanozyme Therapy for Ischemic Brain Damage and Long-Term Neurological Functional Recovery. ACS Nano 2021, 15, 2263–2280. [Google Scholar] [CrossRef] [PubMed]
- Gholizadeh, S.; Kamps, J.A.; Hennink, W.E.; Kok, R.J. PLGA-PEG nanoparticles for targeted delivery of the mTOR/PI3kinase inhibitor dactolisib to inflamed endothelium. Int. J. Pharm. 2018, 548, 747–758. [Google Scholar] [CrossRef] [PubMed]
- Jin, K.; Luo, Z.; Zhang, B.; Pang, Z. Biomimetic nanoparticles for inflammation targeting. Acta Pharm. Sin. B 2018, 8, 23–33. [Google Scholar] [CrossRef]
- Paulis, L.L.; Jacobs, I.I.; Akker, N.M.V.D.; Geelen, T.T.; Molin, D.G.; E Starmans, L.W.; Nicolay, K.; Strijkers, G.G. Targeting of ICAM-1 on vascular endothelium under static and shear stress conditions using a liposomal Gd-based MRI contrast agent. J. Nanobiotechnol. 2012, 10, 25. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.R.; Huh, J.H.; Seo, J.W.; Suk, C.J.; Jeong, H.M.; Kim, E.K. Time-dependent expression of icam-1 & vcam-1 on coronaries of the heterotopically transplanted mouse heart. J. Korean Med Sci. 1999, 14, 245. [Google Scholar]
- Manthe, R.L.; Muro, S. ICAM-1-targeted nanocarriers attenuate endothelial release of soluble ICAM-1, an inflammatory regulator. Bioeng. Transl. Med. 2017, 2, 109–119. [Google Scholar] [CrossRef] [Green Version]
- Verma, A.; Stellacci, F. Effect of surface properties on nanoparticle-cell interactions. Small 2010, 6, 12. [Google Scholar] [CrossRef]
- Muro, S.; Garnacho, C.; A Champion, J.; Leferovich, J.; Gajewski, C.; Schuchman, E.H.; Mitragotri, S.; Muzykantov, V.R. Control of Endothelial Targeting and Intracellular Delivery of Therapeutic Enzymes by Modulating the Size and Shape of ICAM-1-targeted Carriers. Mol. Ther. 2008, 16, 1450–1458. [Google Scholar] [CrossRef]
- Shenoy, D.; Fu, W.; Li, J.; Crasto, C.; Jones, G.; DiMarzio, C.; Sridhar, S.; Amiji, M. Surface functionalization of gold nanoparticles using hetero-bifunctional poly(ethylene glycol) spacer for intracellular tracking and delivery. Int. J. Nanomed. 2006, 1, 51–58. [Google Scholar] [CrossRef]
- Da Silva-Candal, A.; Brown, T.; Krishnan, V.; Lopez-Loureiro, I.; Ávila-Gómez, P.; Pusuluri, A.; Pérez-Díaz, A.; Correa-Paz, C.; Hervella, P.; Castillo, J.; et al. Shape effect in active targeting of nanoparticles to inflamed cerebral endothelium under static and flow conditions. J. Control. Release 2019, 309, 94–105. [Google Scholar] [CrossRef]
- Zein, R.; Sharrouf, W.; Selting, K. Physical Properties of Nanoparticles That Result in Improved Cancer Targeting. J. Oncol. 2020, 2020, 1–16. [Google Scholar] [CrossRef]
- Ahmadinejad, F.; Møller, S.G.; Hashemzadeh-Chaleshtori, M.; Bidkhori, G.; Jami, M.-S. Molecular Mechanisms behind Free Radical Scavengers Function against Oxidative Stress. Antioxidants 2017, 6, 51. [Google Scholar] [CrossRef]
- Zang, X.; Zhou, J.; Zhang, X.; Han, Y.; Chen, X. Ischemia Reperfusion Injury: Opportunities for Nanoparticles. ACS Biomater. Sci. Eng. 2020, 6, 6528–6539. [Google Scholar] [CrossRef] [PubMed]
- Ashafaq, M.; Alam, M.I.; Khan, A.; Islam, F.; Khuwaja, G.; Hussain, S.; Ali, R.; Alshahrani, S.; Makeen, H.A.; Alhazmi, H.A.; et al. Nanoparticles of resveratrol attenuates oxidative stress and inflammation after ischemic stroke in rats. Int. Immunopharmacol. 2021, 94, 107494. [Google Scholar] [CrossRef]
- Zhou, D.; Fang, T.; Lu, L.-Q.; Yi, L. Neuroprotective potential of cerium oxide nanoparticles for focal cerebral ischemic stroke. Acta Acad. Med. Wuhan 2016, 36, 480–486. [Google Scholar] [CrossRef]
- Castillo, J.; Loza, M.I.; Mirelman, D.; Brea, J.; Blanco, M.; Sobrino, T.; Campos, F. A novel mechanism of neuroprotection: Blood glutamate grabber. Br. J. Pharmacol. 2016, 36, 292–301. [Google Scholar] [CrossRef]
- Savchenko, A.; Braun, G.B.; Molokanova, E. Nanostructured Antagonist of Extrasynaptic NMDA Receptors. Nano Lett. 2016, 16, 5495–5502. [Google Scholar] [CrossRef] [PubMed]
- Thiebaut, A.M.; Gauberti, M.; Ali, C.; De Lizarrondo, S.M.; Vivien, D.; Yepes, M.; Roussel, B.D. The role of plasminogen activators in stroke treatment: Fibrinolysis and beyond. Lancet Neurol. 2018, 17, 1121–1132. [Google Scholar] [CrossRef]
- Fukuta, T.; Asai, T.; Yanagida, Y.; Namba, M.; Koide, H.; Shimizu, K.; Oku, N. Combination therapy with liposomal neuroprotectants and tissue plasminogen activator for treatment of ischemic stroke. FASEB J. 2017, 31, 1879–1890. [Google Scholar] [CrossRef] [Green Version]
- Mei, T.; Kim, A.; Vong, L.B.; Marushima, A.; Puentes, S.; Matsumaru, Y.; Matsumura, A.; Nagasaki, Y. Encapsulation of tissue plasminogen activator in ph-sensitive self-assembled antioxidant nanoparticles for ischemic stroke treatment—Synergistic effect of thrombolysis and antioxidant. Biomaterials 2019, 215, 119209. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Susavila, H.; Bugallo-Casal, A.; Castillo, J.; Campos, F. Adult Stem Cells and Induced Pluripotent Stem Cells for Stroke Treatment. Front. Neurol. 2019, 10, 908. [Google Scholar] [CrossRef]
- Liu, X.; Ye, R.; Yan, T.; Yu, S.P.; Wei, L.; Xu, G.; Fan, X.; Jiang, Y.; Stetler, R.A.; Liu, G.; et al. Cell based therapies for ischemic stroke: From basic science to bedside. Prog. Neurobiol. 2014, 115, 92–115. [Google Scholar] [CrossRef] [Green Version]
- Easo, S.L.; Mohanan, P.V. Dextran stabilized iron oxide nanoparticles: Synthesis, characterization and in vitro studies. Carbohydr. Polym. 2013, 92, 726. [Google Scholar] [CrossRef]
- Laurent, S.; Forge, D.; Port, M.; Roch, A.; Robic, C.; Elst, L.V.; Muller, R.N. Magnetic Iron Oxide Nanoparticles: Synthesis, Stabilization, Vectorization, Physicochemical Characterizations, and Biological Applications. Chem. Rev. 2008, 108, 2064–2110. [Google Scholar] [CrossRef]
- Molday, R.S.; MacKenzie, D. Immunospecific ferromagnetic iron-dextran reagents for the labeling and magnetic separation of cells. J. Immunol. Methods 1982, 52, 353–367. [Google Scholar] [CrossRef]
- Argibay, B.; Trekker, J.; Himmelreich, U.; Beiras, A.; Topete, A.; Taboada, P.; Pérez-Mato, M.; Vieites-Prado, A.; Iglesias-Rey, R.; Rivas, J.; et al. Intraarterial route increases the risk of cerebral lesions after mesenchymal cell administration in animal model of ischemia. Sci. Rep. 2017, 7, 40758. [Google Scholar] [CrossRef]
- Liu, G.; Yang, H.; Zhang, X.M.; Shao, Y.; Jiang, H. MR imaging for the longevity of mesenchymal stem cells labeled with poly-L-lysine-Resovist complexes. Contrast Media Mol. Imaging 2010, 5, 53–58. [Google Scholar] [CrossRef]
- Soenen, S.J.; Himmelreich, U.; Nuytten, N.; De Cuyper, M. Cytotoxic effects of iron oxide nanoparticles and implications for safety in cell labelling. Biomaterals 2011, 32, 195–205. [Google Scholar] [CrossRef]
- Jain, T.K.; Morales, M.A.; Sahoo, S.K.; Leslie-Pelecky, D.L.; Labhasetwar, V. Iron Oxide Nanoparticles for Sustained Delivery of Anticancer Agents. Mol. Pharm. 2005, 2, 194–205. [Google Scholar] [CrossRef] [Green Version]
- Bae, K.H.; Ha, Y.J.; Kim, C.; Lee, K.-R.; Park, T.G. Pluronic/chitosan shell cross-linked nanocapsules encapsulating magnetic nanoparticles. J. Biomater. Sci. Polym. Ed. 2008, 19, 1571–1583. [Google Scholar] [CrossRef] [Green Version]
- Kelly, S.; Bliss, T.M.; Shah, A.K.; Sun, G.H.; Ma, M.; Foo, W.C.; Masel, J.; Yenari, M.A.; Weissman, I.L.; Uchida, N.; et al. Transplanted human fetal neural stem cells survive, migrate, and differentiate in ischemic rat cerebral cortex. Proc. Natl. Acad. Sci. USA 2004, 101, 11839. [Google Scholar] [CrossRef] [Green Version]
- Darsalia, V.; Kallur, T.; Kokaia, Z. Survival, migration and neuronal differentiation of human fetal striatal and cortical neural stem cells grafted in stroke-damaged rat striatum. Eur. J. Neurosci. 2007, 26, 605–614. [Google Scholar] [CrossRef]
- Fischer, U.M.; Harting, M.T.; Jimenez, F.; Monzon-Posadas, W.O.; Xue, H.; Savitz, S.I.; Laine, G.A.; Cox, C.S. Pulmonary Passage is a Major Obstacle for Intravenous Stem Cell Delivery: The Pulmonary First-Pass Effect. Stem Cells Dev. 2009, 18, 683–692. [Google Scholar] [CrossRef]
- Eggenhofer, E.; Benseler, V.; Kroemer, H.; Popp, F.; Geissler, E.; Schlitt, H.; Baan, C.; Dahlke, M.; Hoogduijn, M.J. Mesenchymal stem cells are short-lived and do not migrate beyond the lungs after intravenous infusion. Front. Immunol. 2012, 3, 297. [Google Scholar] [CrossRef] [Green Version]
- Ezquer, F.; Morales, P.; Quintanilla, M.E.; Santapau, D.; Lespay-Rebolledo, C.; Ezquer, M.; Herrera-Marschitz, M.; Israel, Y. Intravenous administration of anti-inflammatory mesenchymal stem cell spheroids reduces chronic alcohol intake and abolishes binge-drinking. Sci. Rep. 2018, 8, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Acosta, S.A.; Tajiri, N.; Hoover, J.; Kaneko, Y.; Borlongan, C.V. Intravenous Bone Marrow Stem Cell Grafts Preferentially Migrate to Spleen and Abrogate Chronic Inflammation in Stroke. Stroke 2015, 46, 2616–2627. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Jiang, Q.; Ding, G.; Zhang, L.; Zhang, Z.G.; Li, Q.; Panda, S.; Lu, M.; Ewing, J.R.; Chopp, M. Effects of Administration Route on Migration and Distribution of Neural Progenitor Cells Transplanted into Rats with Focal Cerebral Ischemia, an MRI Study. Br. J. Pharmacol. 2009, 30, 653–662. [Google Scholar] [CrossRef] [Green Version]
- Vasconcelos-Dos-Santos, A.; Rosado-De-Castro, P.H.; de Souza, S.A.L.; Silva, J.D.C.; Ramos, A.B.; de Freitas, G.R.; da Fonseca, L.M.B.; Gutfilen, B.; Mendez-Otero, R. Intravenous and intra-arterial administration of bone marrow mononuclear cells after focal cerebral ischemia: Is there a difference in biodistribution and efficacy? Stem Cell Res. 2012, 9, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Yang, B.; Migliati, E.; Parsha, K.; Schaar, K.; Xi, X.; Aronowski, J.; Savitz, S.I. Intra-Arterial Delivery Is Not Superior to Intravenous Delivery of Autologous Bone Marrow Mononuclear Cells in Acute Ischemic Stroke. Stroke 2013, 44, 3463–3472. [Google Scholar] [CrossRef] [Green Version]
- Carenza, E.; Barceló, V.; Morancho, A.; Levander, L.; Boada, C.; Laromaine, A.; Roig, A.; Montaner, J.; Rosell, A. In vitro angiogenic performance and in vivo brain targeting of magnetized endothelial progenitor cells for neurorepair therapies. Nanomed. Nanotechnol. Biol. Med. 2014, 10, 225–234. [Google Scholar] [CrossRef]



| Diagnosis | |||
| Imaging Tool | Type of Nanoparticle | Target Triggering | Reference |
| MRI | MPIOs | VCAM-1 | [18] |
| ICAM-1 | [19] | ||
| P-selectin | [20] | ||
| VCAM-1 and P-selectin | [21] | ||
| Multimeric magnetite particles | Peptide to intracellular macrophage proteases | [23] | |
| CT | Gold NPs | Fibrin | [22] |
| Thrombolytic Treatment | |||
| Type of Nanoparticle | Target Triggering | Reference | |
| Liposomes | Liposomes | Plasminogen | [33,34] |
| Magnetoliposomes | Thermosensitive and magnetic guidance | [60] | |
| Polymeric NPs | PLGA NPs coated with chitosan | Fibrin | [39,40] |
| Polysaccharide-poly(isobutylcyanoacrylate) nanoparticles | P-selectin | [42] | |
| Layer-by-layer capsules | Glycoprotein (GP) IIb/IIIa Thrombin responsive | [43] | |
| Poly(N-isopropylacrylamide) nanogels | Fibrin | [44] | |
| Near-infrared fluorescent dye-conjugated boronated maltodextrin | Fibrin H2O2 responsive | [51] | |
| NIR fluorescent dye-conjugated boronate antioxidant polymers (fBAP) and fibrin-targeting lipopeptides | Fibrin H2O2 responsive | [52] | |
| Prodrug nanocarriers based on PEG and diosgenin derivatives | pH responsive | [53] | |
| Aggregates of multiple smaller NPs of PLGA | Shear stress responsive | [57] | |
| Layer-by-layer sub-micrometic nanocapsules with gelatin | Von Willebrand factor Ultrasounds | [65] | |
| Near-infrared fluorescent dye-conjugated boronated maltodextrin | Fibrin H2O2 responsive | [51] | |
| Metal NPs | Magnetic rods | Magnetic guidance | [35] |
| Fe3O4-based PLGA | Fibrin | [41] | |
| PLGA magnetic NPs | Fibrin Magnetic guidance | [46] | |
| Metal–organic framework-derived carbon nanostructures | GP IIb/IIIa Hyperthermia and ROS sensitive under NIR laser | [59] | |
| Chitosan nanocomposites with Fe3O4 | Magnetic guidance | [61] | |
| Magnetic nanocubes within a deoxychitosan core | Magnetic guidance | [62] | |
| Magnetic Fe3O4 microrods | Magnetic guidance | [63] | |
| Microbubbles | Fibrin Ultrasounds | [36] | |
| Fibrin Ultrasounds | [37] | ||
| Echogenic liposomes | Ultrasounds | [38] | |
| Ultrasounds | [64] | ||
| Biomimetic NPs | Red blood cells doped with NIR imaging agent | [49] | |
| Nanoplatelet with rtPA and a neuroprotectant (ZL006e) | Thrombin | [50] | |
| Platelet microparticle inspired | GP IIb/IIIa and P-selectin | [54] | |
| Neuroprotection | |||
| Approach | Type of Nanoparticle | Target Triggering | Reference |
| Inflammation | Exosomes loading curcumin | Integrin αvβ3 | [71] |
| Neutrophil-like cell membrane-coated mesoporous nanozyme | Inflamed endothelium | [72] | |
| Spheres and elliptical disks | ICAM-1 | [79] | |
| Gold NPs with coumarin-PEG-thiol | [80] | ||
| Sphere and rod NPs | VCAM-1 | [81] | |
| Oxidative stress | NPs of resveratrol | [85] | |
| Cerium oxide NPs | [86] | ||
| Glutamate excitotoxicity | Gold NPs with memantine | [88] | |
| Combination with rtPA | Liposomes loading rtPA and fasudil | [90] | |
| Self-assembled antioxidant NPs with rtPA | [91] | ||
| Neurorecovery | |||
| Approach | Type of Nanoparticle | Target Triggering | Reference |
| MRI cell tracking | Superparamagnetic iron oxide nanoparticles (SPIONs) | Cell tracking of mesenchymal stem cells (MSCs) | [97] |
| Magnetic vectorization | Superparamagnetic iron oxide nanoparticles (SPIONs) | Cell tracking of endothelial progenitor cells (EPCs) Magnetic guidance | [111] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Correa-Paz, C.; da Silva-Candal, A.; Polo, E.; Parcq, J.; Vivien, D.; Maysinger, D.; Pelaz, B.; Campos, F. New Approaches in Nanomedicine for Ischemic Stroke. Pharmaceutics 2021, 13, 757. https://doi.org/10.3390/pharmaceutics13050757
Correa-Paz C, da Silva-Candal A, Polo E, Parcq J, Vivien D, Maysinger D, Pelaz B, Campos F. New Approaches in Nanomedicine for Ischemic Stroke. Pharmaceutics. 2021; 13(5):757. https://doi.org/10.3390/pharmaceutics13050757
Chicago/Turabian StyleCorrea-Paz, Clara, Andrés da Silva-Candal, Ester Polo, Jérôme Parcq, Denis Vivien, Dusica Maysinger, Beatriz Pelaz, and Francisco Campos. 2021. "New Approaches in Nanomedicine for Ischemic Stroke" Pharmaceutics 13, no. 5: 757. https://doi.org/10.3390/pharmaceutics13050757
APA StyleCorrea-Paz, C., da Silva-Candal, A., Polo, E., Parcq, J., Vivien, D., Maysinger, D., Pelaz, B., & Campos, F. (2021). New Approaches in Nanomedicine for Ischemic Stroke. Pharmaceutics, 13(5), 757. https://doi.org/10.3390/pharmaceutics13050757








