Designing of Co0.5Ni0.5GaxFe2−xO4 (0.0 ≤ x ≤ 1.0) Microspheres via Hydrothermal Approach and Their Selective Inhibition on the Growth of Cancerous and Fungal Cells
Abstract
:1. Introduction
2. Materials and Methods
2.1. Synthesis and Characterizations of MCs
2.2. Anti-Cancer Activity
2.2.1. Cell Culture and Testing of Nanoparticles Using MTT Method
2.2.2. DAPI Staining for DNA Analysis
2.3. Anti-Candidal Activity
2.3.1. Preparation of Inoculum and Nanomaterial
2.3.2. Study of CFU and Morphogenesis of C. albicans
3. Results and Discussion
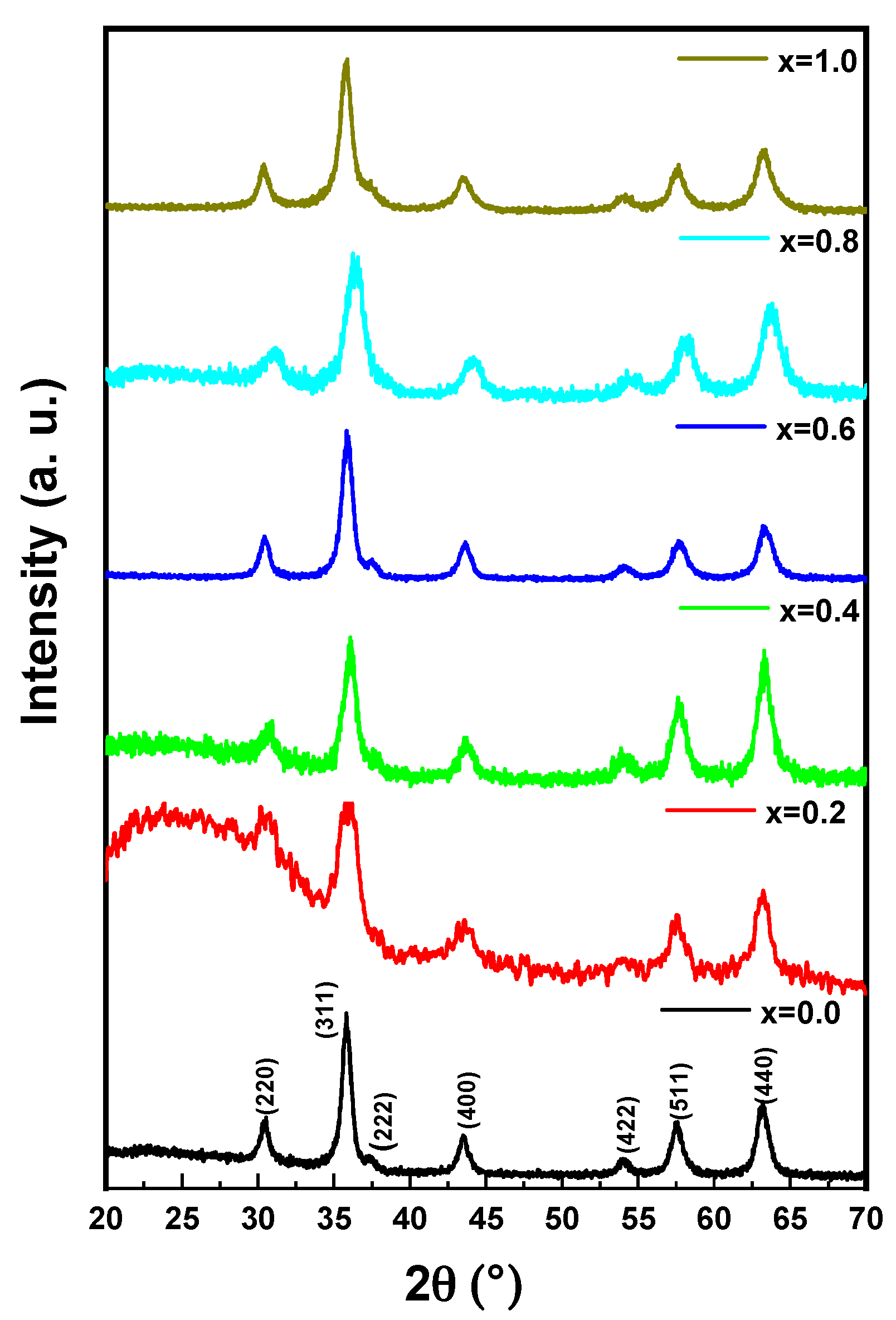
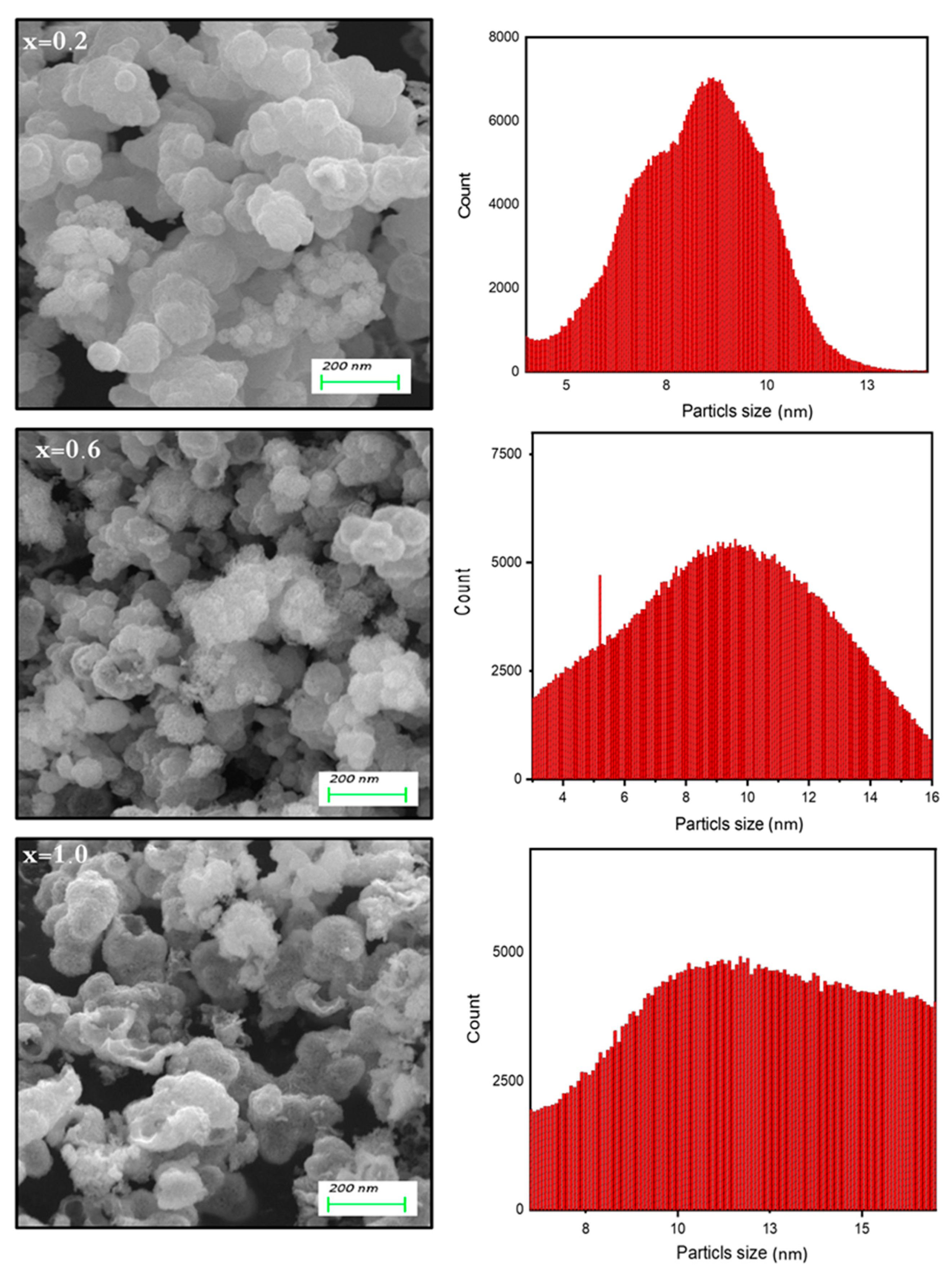
3.1. Microstructural Analysis of Co0.5Ni0.5GaxFe2−xO4 (0.0 ≤ x ≤ 1.0) MCs
3.2. Biological Activities
3.2.1. Impact of Co0.5Ni0.5GaxFe2−xO4 (0.0 ≤ x ≤ 1.0) MCs on Cancer Cell Viability
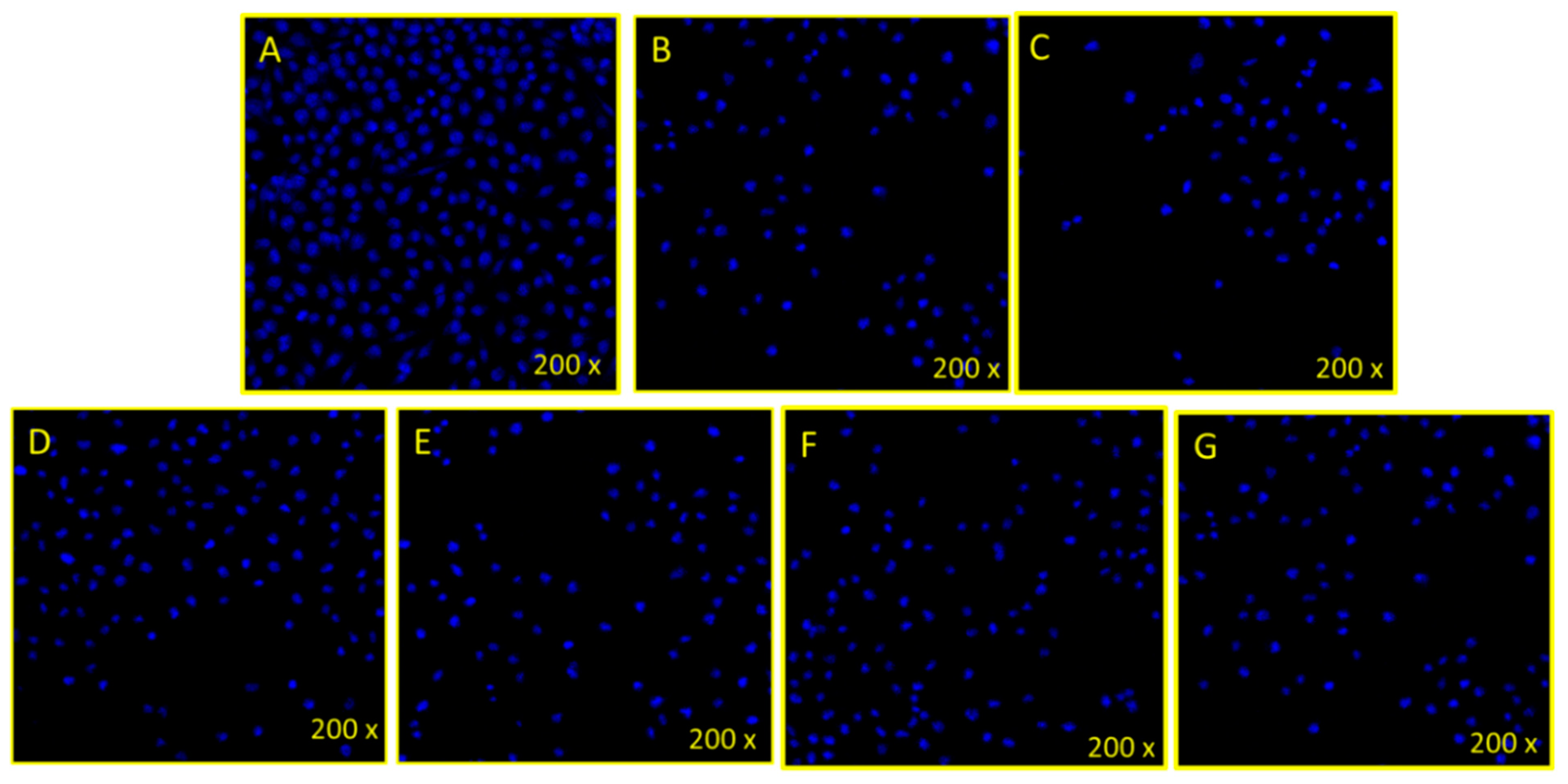
3.2.2. Disintegration of Cancer Cell DNA
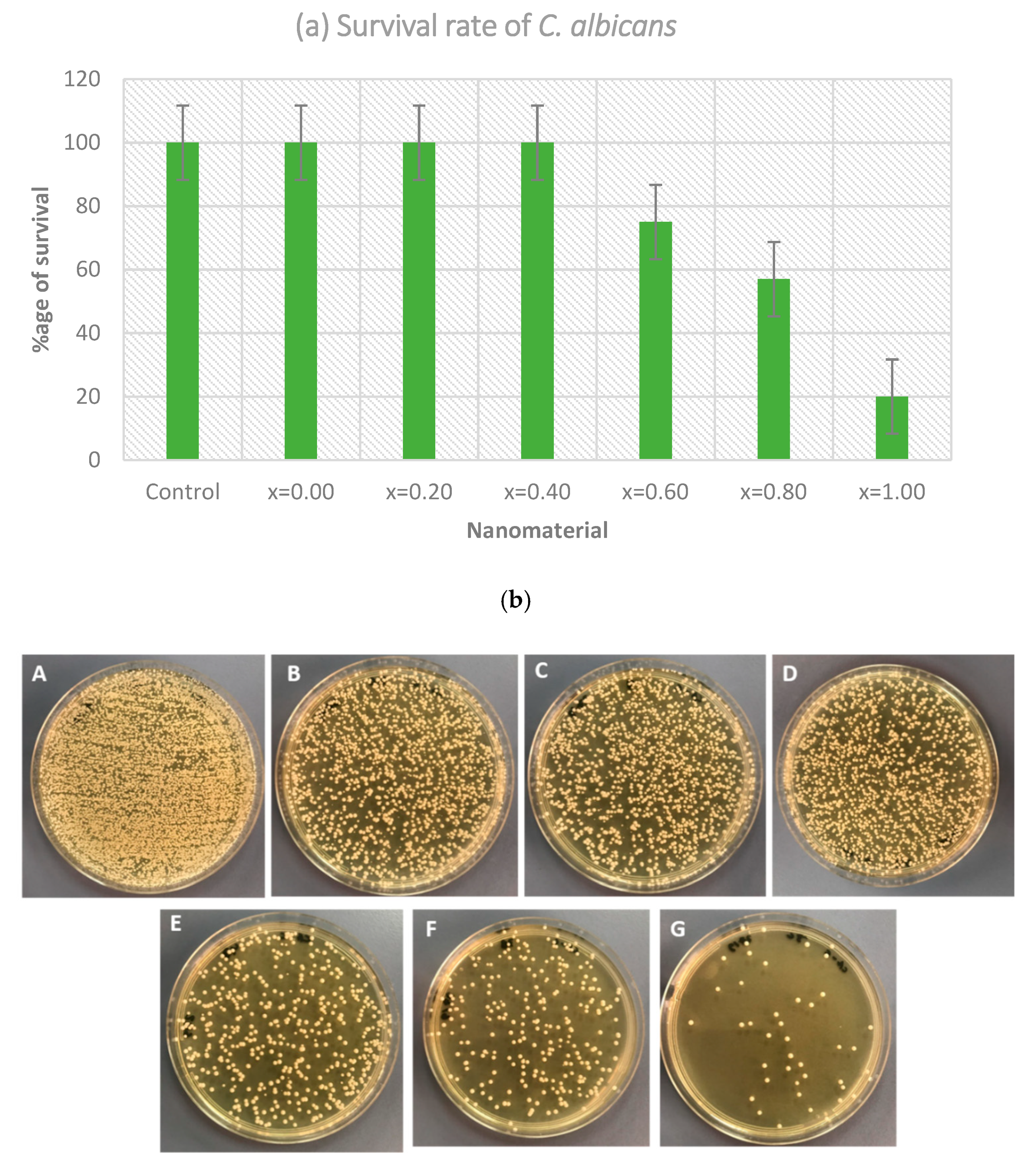
3.2.3. Anti-Fungal Activity
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dilruba, S.; Kalayda, G.V. Platinum-based drugs: Past, present and future. Cancer Chemother. Pharmacol. 2016, 77, 1103–1124. [Google Scholar] [CrossRef]
- Zeng, L.; Chen, Y.; Liu, J.; Huang, H.; Guan, R.; Ji, L.; Chao, H. Ruthenium (II) complexes with 2-phenylimidazo [4,5-f][1,10] phenanthroline derivatives that strongly combat cisplatin-resistant tumor cells. Sci. Rep. 2016, 6, 19449. [Google Scholar] [CrossRef] [PubMed]
- Qin, J.-L.; Shen, W.-Y.; Chen, Z.-F.; Zhao, L.-F.; Qin, Q.-P.; Yu, Y.-C.; Liang, H. Oxoaporphine Metal Complexes (CoII, NiII, ZnII) with High Antitumor Activity by Inducing Mitochondria-Mediated Apoptosis and S-phase Arrest in HepG2. Sci. Rep. 2017, 7, 46056. [Google Scholar] [CrossRef] [Green Version]
- Tombuloglu, H.; Khan, F.A.; Almessiere, M.A.; Aldakheel, S.; Baykal, A. Synthesis of niobium substituted cobalt-nickel nano-ferrite (Co0.5Ni0.5NbxFe2−xO4 (x ≤ 0.1) by hydrothermal approach show strong anti-colon cancer activities. J. Biomol. Struct. Dyn. 2020, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.Y.; Li, J.R.; Li, X.C.; Jiang, L. A new step to the mechanism of the enhancement effect of gold nanoparticles on glucose oxidase. Biochem. Biophys. Res. Commun. 1998, 245, 352–355. [Google Scholar] [CrossRef]
- Loubeyre, P.; Zhao, S.; Canet, E.; Abidi, H.; Benderbous, S.; Revel, D. Ultrasmall superparamagnetic iron oxide particles (AMI 227) as a blood pool contrast agent for MR angiography: Experimental study in rabbits. J. Magn. Reson. Imaging 1997, 7, 958–962. [Google Scholar] [CrossRef] [PubMed]
- Kumar, D.; Saini, N.; Jain, N.; Sareen, R.; Pandit, V. Gold nanoparticles: An era in bionanotechnology. Expert Opin. Drug Deliv. 2013, 10, 397–409. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Rao, R.; Kumar, A.; Mahant, S.; Nanda, S. Novel Carriers for Coenzyme Q10 Delivery. Curr. Drug Deliv. 2016, 13, 1184–1204. [Google Scholar] [CrossRef] [PubMed]
- Dong, Q.; Ding, Y.; Wen, B.; Wang, F.; Dong, H.; Zhang, S.; Wang, T.; Yang, M. Improvement of thermal stability of polypropylene using DOPO-immobilized silica nanoparticles. Colloid Polym. Sci. 2012, 290, 1371–1380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarkar, D.; Swain, S.K.; Adhikari, S.; Reddy, B.S.; Maiti, H.S. Synthesis, mechanical properties and bioactivity of nanostructured zirconia. Mater. Sci. Eng. C 2013, 33, 3413–3417. [Google Scholar] [CrossRef]
- Qu, M.; Mallidi, S.; Mehrmohammadi, M.; Truby, R.; Homan, K.; Joshi, P.; Chen, Y.-S.; Sokolov, K.; Emelianov, S. Magneto-photo-acoustic imaging. Biomed. Opt. Express 2011, 2, 385–396. [Google Scholar] [CrossRef] [Green Version]
- Chong, H.; Nie, C.; Zhu, C.; Yang, Q.; Liu, L.; Lv, F.; Wang, S. Conjugated Polymer Nanoparticles for Light-Activated Anticancer and Antibacterial Activity with Imaging Capability. Langmuir 2011, 28, 2091–2098. [Google Scholar] [CrossRef] [PubMed]
- Adwin Jose, P.; Sankarganesh, M.; Dhaveethu Raja, J.; Sukkur Saleem, S. Pyrimidine Derivative Schiff Base Ligand Stabilized Copper and Nickel Nanoparticles by Two Step Phase Transfer Method; in Vitro Anticancer, Antioxidant, Anti-Microbial and DNA Interactions. J. Fluoresc. 2020, 30, 471–482. [Google Scholar] [CrossRef]
- Al-Qubaisi, M.S.; Rasedee, A.; Flaifel, M.H.; Ahmad, S.H.; Hussein-Al-Ali, S.; Hussein, M.Z.; Eid, E.E.; Zainal, Z.; Saeed, M.; Ilowefah, M.; et al. Cytotoxicity of nickel zinc ferrite nanoparticles on cancer cells of epithelial origin. Int. J. Nanomed. 2013, 8, 2497–2508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qasim, M.; Asghar, K.; Dharmapuri, G.; Das, D. Investigation of novel superparamagnetic Ni0.5Zn0.5Fe2O4@albumen nanoparticles for controlled delivery of anticancer drug. Nanotechnology 2017, 28, 365101. [Google Scholar] [CrossRef] [PubMed]
- Delong, R.K.; Comer, J.; Mathew, E.N.; Jaberi-Douraki, M. Comparative Molecular Immunological Activity of Physiological Metal Oxide Nanoparticle and its Anticancer Peptide and RNA Complexes. Nanomaterials 2019, 9, 1670. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Sayed, E.-S.R.; Abdelhakim, H.K.; Zakaria, Z. Extracellular biosynthesis of cobalt ferrite nanoparticles by Monascus purpureus and their antioxidant, anticancer and antimicrobial activities: Yield enhancement by gamma irradiation. Mater. Sci. Eng. C 2020, 107, 110318. [Google Scholar] [CrossRef]
- Jarestan, M.; Khalatbari, K.; Pouraei, A.; Shandiz, S.A.S.; Beigi, S.; Hedayati, M.; Majlesi, A.; Akbari, F.; Salehzadeh, A. Preparation, characterization, and anticancer efficacy of novel cobalt oxide nanoparticles conjugated with thiosemicarbazide. 3 Biotech 2020, 10, 1–9. [Google Scholar] [CrossRef]
- Dey, C.; Ghosh, A.; Ahir, M.; Ghosh, A.; Goswami, M.M. Improvement of Anticancer Drug Release by Cobalt Ferrite Magnetic Nanoparticles through Combined pH and Temperature Responsive Technique. ChemPhysChem 2018, 19, 2872–2878. [Google Scholar] [CrossRef]
- Park, B.J.; Choi, K.-H.; Nam, K.C.; Ali, A.; Min, J.E.; Son, H.; Uhm, H.S.; Kim, H.-J.; Jung, J.-S.; Choi, E.H. Photodynamic Anticancer Activities of Multifunctional Cobalt Ferrite Nanoparticles in Various Cancer Cells. J. Biomed. Nanotechnol. 2015, 11, 226–235. [Google Scholar] [CrossRef]
- Kandil, E.I.; El-Sonbaty, S.M.; Moawed, F.S.; Khedr, O.M. Anticancer redox activity of gallium nanoparticles accompanied with low dose of gamma radiation in female mice. Tumor Biol. 2018, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Körhegyi, Z.; Rózsa, D.; Hajdu, I.; Bodnár, M.; Kertész, I.; Kerekes, K.; Kun, S.; Kollár, J.; Varga, J.; Garai, I.; et al. Synthesis of 68Ga-Labeled Biopolymer-based Nanoparticle Imaging Agents for Positron-emission Tomography. Anticancer. Res. 2019, 39, 2415–2427. [Google Scholar] [CrossRef]
- Gu, C.; Li, C.; Zhang, J.; Li, X.; Wang, L.; Ju, Y.; Liu, Y.; Xu, Y. Ultra-effective near-infrared Photothermal therapy for the prostate cancer Nursing care through novel intended and surface tailored photo-responsive Ga-Au@MPS nanovesicles. J. Photochem. Photobiol. B Biol. 2020, 202, 111685. [Google Scholar] [CrossRef]
- Douziech-Eyrolles, L.; Marchais, H.; Hervé, K.; Munnier, E.; Soucé, M.; Linassier, C.; Dubois, P.; Chourpa, I. Nanovectors for anticancer agents based on superparamagnetic iron oxide nanoparticles. Int. J. Nanomed. 2007, 2, 541–550. [Google Scholar]
- Jahanbani, J.; Ghotbi, M.; Shahsavari, F.; Seydi, E.; Rahimi, S.; Pourahmad, J. Selective anticancer activity of superparamagnetic iron oxide nanoparticles (SPIONs) against oral tongue cancer using in vitro methods: The key role of oxidative stress on cancerous mitochondria. J. Biochem. Mol. Toxicol. 2020, 34, e22557. [Google Scholar] [CrossRef] [PubMed]
- Shetake, N.G.; Kumar, A.; Pandey, B.N. Iron-oxide nanoparticles target intracellular HSP90 to induce tumor radio-sensitization. Biochim. Biophys. Acta Gen. Subj. 2019, 1863, 857–869. [Google Scholar] [CrossRef]
- Akhtar, S.; Rehman, S.; Almessiere, M.A.; Alam Khan, F.; Slimani, Y.; Baykal, A. Synthesis of Mn0.5Zn0.5SmxEuxFe1.8−2xO4 Nanoparticles via the Hydrothermal Approach Induced Anti-Cancer and Anti-Bacterial Activities. Nanomaterials 2019, 9, 1635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rehman, S.; Asiri, S.M.; Khan, F.A.; Jermy, B.R.; Khan, H.; Akhtar, S.; Jindan, R.A.; Khan, K.M.; Qurashi, A. Biocompatible Tin Oxide Nanoparticles: Synthesis, Antibacterial, Anticandidal and Cytotoxic Activities. Chemistry 2019, 4, 4013–4017. [Google Scholar] [CrossRef]
- AlAhmari, F.; Rehman, S.; Almessiere, M.; A Khan, F.; Slimani, Y.; Baykal, A. Synthesis of Ni0.5Co0.5−xCdxFe1.78Nd0.02O4 (x ≤ 0.25) nanofibers by using electrospinning technique induce anti-cancer and anti-bacterial activities. J. Biomol. Struct. Dyn. 2020, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Almessiere, M.; Slimani, Y.; Rehman, S.; Khan, F.A.; Polat, E.G.; Sadaqat, A.; Shirsath, S.E.; Baykal, A. Synthesis of Dy-Y co-substituted manganese-zinc spinel nanoferrites induced anti-bacterial and anti-cancer activities: Comparison between sonochemical and sol-gel auto-combustion methods. Mater. Sci. Eng. C 2020, 116, 111186. [Google Scholar] [CrossRef]
- Chang, Z. Template Preparation Transition Metal Oxide Hollow Microsphere by Template Method and Study on Its Properties. Master’s Thesis, Anhui University, Hefei, China, 2011. [Google Scholar]
- Jing, W. Synthesis Several Putamen and Hollow Structure Function Material by Carbon Containing Polysaccharide Microsphere Template Method. Master’s Thesis, Harbin Engineering University, Harbin, China, 2011. [Google Scholar]
- Gu, J.; Wu, G.; Zhao, X. Preparation and performance study of high damping cenosphere/epoxy compo site material. Funct. Mater. 2007, 38, 764–766. [Google Scholar]
- Mu, G.; Pan, X.; Shen, H.; Gu, M. Preparation and magnetic properties of composite powders of hollow microspheres coated with barium ferrite. Mater. Sci. Eng. A 2007, 445, 563–566. [Google Scholar] [CrossRef]
- Wang, C.; Wang, J.; Li, M.; Qu, X.; Zhang, K.; Rong, Z.; Xiao, R.; Wang, S. A rapid SERS method for label-free bacteria detection using polyethylenimine-modified Au-coated magnetic microspheres and Au@Ag nanoparticles. Analyst 2016, 141, 6226–6238. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-F.; Wang, Y.-F.; Yan, X.-P. Amine-functionalized magnetic nanoparticles for rapid capture and removal of bacterial pathogens. Environ. Sci. Technol. 2010, 44, 7908–7913. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Ma, J.; Ruan, J.; Zhuang, X. Using positively charged magnetic nanoparticles to capture bacteria at ultralow concentration. Nanoscale Res. Lett. 2019, 14, 195. [Google Scholar] [CrossRef] [Green Version]
- Rethinasabapathy, M.; Vilian, A.E.; Hwang, S.K.; Kang, S.-M.; Cho, Y.; Han, Y.-K.; Rhee, J.-K.; Huh, Y.S. Cobalt ferrite microspheres as a biocompatible anode for higher power generation in microbial fuel cells. J. Power Sources 2021, 483, 229170. [Google Scholar] [CrossRef]
- Chen, P.; Cui, B.; Bu, Y.; Yang, Z.; Wang, Y. Synthesis and characterization of mesoporous and hollow-mesoporous MxFe3−xO4 (M = Mg, Mn, Fe, Co, Ni, Cu, Zn) microspheres for microwave-triggered controllable drug delivery. J. Nanopart. Res. 2017, 19, 398. [Google Scholar] [CrossRef]
- Alam Khan, F.; Akhtar, S.; Almohazey, D.; AlOmari, M.; Almofty, S.; Eliassari, A. Fluorescent magnetic submicronic polymer (FMSP) nanoparticles induce cell death in human colorectal carcinoma cells. Artif. Cells Nanomed. Biotechnol. 2018, 46, S247–S253. [Google Scholar] [CrossRef]
- Alam Khan, F.; Akhtar, S.; Almohazey, D.; AlOmari, M.; Almofty, S. Extracts of Clove (Syzygium aromaticum) Potentiate FMSP-Nanoparticles Induced Cell Death in MCF-7 Cells. Int. J. Biomater. 2018, 2018, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Baig, U.; Ansari, M.A.; Gondal, M.A.; Akhtar, S.; Khan, F.A.; Falath, W.S. Single step production of high-purity copper oxide-titanium dioxide nanocomposites and their effective antibacterial and anti-biofilm activity against drug-resistant bacteria. Mater. Sci. Eng. C 2020, 113, 110992. [Google Scholar] [CrossRef]
- Rehman, S.; Almessiere, M.; Khan, F.; Korkmaz, A.D.; Tashkandi, N.; Slimani, Y.; Baykal, A. Synthesis and biological characterization of Mn0.5Zn0.5EuxDyxFe1.8-2xO4 nanoparticles by sonochemical approach. Mater. Sci. Eng. C 2020, 109, 110534. [Google Scholar] [CrossRef]
- Rehman, S.; Almessiere, M.A.; Tashkandi, N.; Baykal, A.; Slimani, Y.; Jermy, R.; Ravinayagam, V.; Yaman, C. Fabrication of Spinel Cobalt Ferrite (CoFe2O4) Nanoparticles with Unique Earth Element Cerium and Neodymium for Anticandidal Activities. Chemistry 2019, 4, 14329–14334. [Google Scholar] [CrossRef]
- El Rayes, S.M.; Aboelmagd, A.; Gomaa, M.; Ali, I.A.I.; Fathalla, W.; Pottoo, F.H.; Khan, F.A. Convenient Synthesis and Anticancer Activity of Methyl 2-[3-(3-Phenyl-quinoxalin-2-ylsulfanyl)propanamido]alkanoates and N-Alkyl 3-((3-Phenyl-quinoxalin-2-yl)sulfanyl)propanamides. ACS Omega 2019, 4, 18555–18566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aldakheel, R.K.; Rehman, S.; Almessiere, M.A.; Khan, F.A.; Gondal, M.A.; Mostafa, A.; Baykal, A. Bactericidal and In Vitro Cytotoxicity of Moringa oleifera Seed Extract and Its Elemental Analysis Using Laser-Induced Breakdown Spectroscopy. Pharmaceuticals 2020, 13, 193. [Google Scholar] [CrossRef]
- Khan, F.A.; Lammari, N.; Muhammad Siar, A.S.; Alkhater, K.M.; Asiri, S.; Akhtar, S.; Almansour, I.; Alamoudi, W.; Haroun, W.; Louaer, W.; et al. Quantum dots encapsulated with curcumin inhibit the growth of colon cancer, breast cancer and bacterial cells. Nanomedicine 2020, 15, 969–980. [Google Scholar] [CrossRef]
- Veeralakshmi, S.; Nehru, S.; Sabapathi, G.; Arunachalam, S.; Venuvanalingam, P.; Kumar, P.; Anusha, C.; Ravikumar, V. Single and double chain surfactant–cobalt (III) complexes: The impact of hydrophobicity on the interaction with calf thymus DNA, and their biological activities. RSC Adv. 2015, 5, 31746–31758. [Google Scholar] [CrossRef]
- Nguyen, K.T.; Shukla, K.P.; Moctezuma, M.; Braden, A.R.C.; Zhou, J.; Hu, Z.; Tang, L. Studies of the cellular uptake of hydrogel nanospheres and microspheres by phagocytes, vascular endothelial cells, and smooth muscle cells. J. Biomed. Mater. Res. Part A 2008, 88, 1020–1030. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Do, D.P.; D’Souza, M.J.; Enriquez, G.G.; Rizvi, S.A. Formulation and evaluation of drug-loaded targeted magnetic microspheres for cancer therapy. Int. J. Nanomed. 2013, 8, 1393–1402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos, E.V.R.; Rodriguez-Torres, M.D.P.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018, 16, 1–33. [Google Scholar] [CrossRef] [Green Version]
- Chohan, Z.H.; Khan, K.M.; Supuran, C.T. Synthesis of antibacterial and antifungal cobalt (II), copper (II), nickel (II) and zinc (II) complexes with bis-(1,1′-disubstituted ferrocenyl) thiocarbohydrazone and bis-(1,1′-disubstituted ferrocenyl) carbohydrazone. Appl. Organomet. Chem. 2004, 18, 305–310. [Google Scholar] [CrossRef]
- Shah, A.H.; Rather, M.A. Effect of Thermal Treatment on the Phase Composition and Surface Properties of WO3-TiO2 Nanocomposites Synthesized via Hydro-Thermal Method. Chemistry 2021, 6, 987–994. [Google Scholar]
- Nagy, M.; Szemán-Nagy, G.; Kiss, A.; Nagy, Z.L.; Tálas, L.; Rácz, D.; Majoros, L.; Tóth, Z.; Szigeti, Z.M.; Pócsi, I.; et al. Antifungal activity of an original amino-isocyanonaphthalene (ICAN) compound family: Promising broad spectrum antifungals. Molecules 2020, 25, 903. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| x | IC50 (HCT-116) Cells (µg/mL) | IC50 (HeLa) Cells (µg/mL) | IC50 (HEK-293) Cells |
|---|---|---|---|
| 0.0 | 25 ± 2 | 35 ± 4 | No inhibition |
| 0.2 | 46 ± 3 | 56 ± 4 | No inhibition |
| 0.4 | 42 ± 4 | 48 ± 5 | No inhibition |
| 0.6 | 29 ± 2 | 50 ± 5 | No inhibition |
| 0.8 | 50 ± 5 | 49 ± 4 | No inhibition |
| 1.0 | 59 ± 5 | 60 ± 5 | No inhibition |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rehman, S.; Almessiere, M.A.; Al-Jameel, S.S.; Ali, U.; Slimani, Y.; Tashkandi, N.; Al-Saleh, N.S.; Manikandan, A.; Khan, F.A.; Al-Suhaimi, E.A.; et al. Designing of Co0.5Ni0.5GaxFe2−xO4 (0.0 ≤ x ≤ 1.0) Microspheres via Hydrothermal Approach and Their Selective Inhibition on the Growth of Cancerous and Fungal Cells. Pharmaceutics 2021, 13, 962. https://doi.org/10.3390/pharmaceutics13070962
Rehman S, Almessiere MA, Al-Jameel SS, Ali U, Slimani Y, Tashkandi N, Al-Saleh NS, Manikandan A, Khan FA, Al-Suhaimi EA, et al. Designing of Co0.5Ni0.5GaxFe2−xO4 (0.0 ≤ x ≤ 1.0) Microspheres via Hydrothermal Approach and Their Selective Inhibition on the Growth of Cancerous and Fungal Cells. Pharmaceutics. 2021; 13(7):962. https://doi.org/10.3390/pharmaceutics13070962
Chicago/Turabian StyleRehman, Suriya, Munirah A. Almessiere, Suhailah S. Al-Jameel, Uzma Ali, Yassine Slimani, Nedaa Tashkandi, Najat S. Al-Saleh, Ayyar Manikandan, Firdos Alam Khan, Ebtesam A. Al-Suhaimi, and et al. 2021. "Designing of Co0.5Ni0.5GaxFe2−xO4 (0.0 ≤ x ≤ 1.0) Microspheres via Hydrothermal Approach and Their Selective Inhibition on the Growth of Cancerous and Fungal Cells" Pharmaceutics 13, no. 7: 962. https://doi.org/10.3390/pharmaceutics13070962
APA StyleRehman, S., Almessiere, M. A., Al-Jameel, S. S., Ali, U., Slimani, Y., Tashkandi, N., Al-Saleh, N. S., Manikandan, A., Khan, F. A., Al-Suhaimi, E. A., & Baykal, A. (2021). Designing of Co0.5Ni0.5GaxFe2−xO4 (0.0 ≤ x ≤ 1.0) Microspheres via Hydrothermal Approach and Their Selective Inhibition on the Growth of Cancerous and Fungal Cells. Pharmaceutics, 13(7), 962. https://doi.org/10.3390/pharmaceutics13070962









