Evaluating and Improving Neonatal Gentamicin Pharmacokinetic Models Using Aggregated Routine Clinical Care Data
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
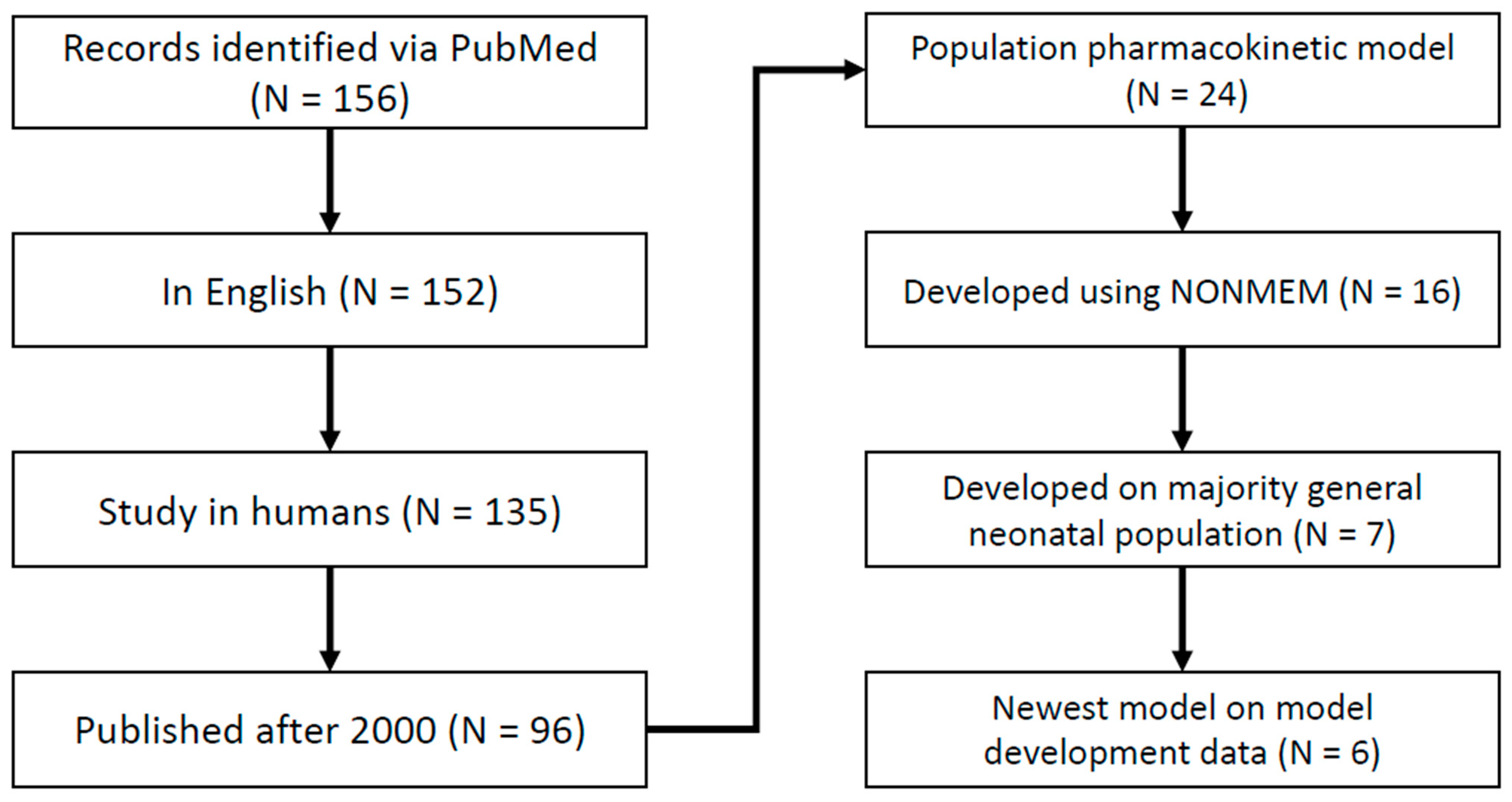
2.2. Population Pharmacokinetic Model Literature Review
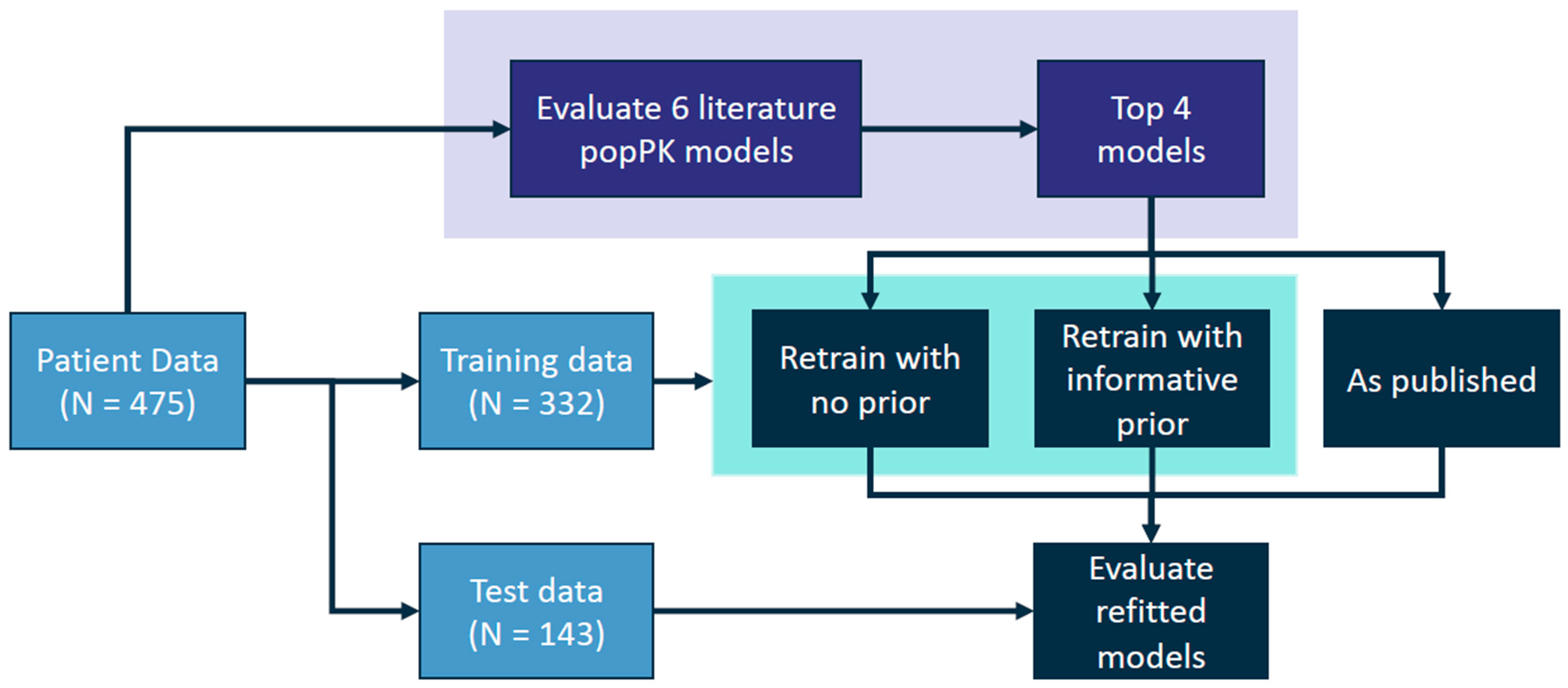
2.3. Population Pharmacokinetic Model Refitting and Evaluation
2.4. Statistics and Error Metrics
3. Results
3.1. Patients and Data Collection
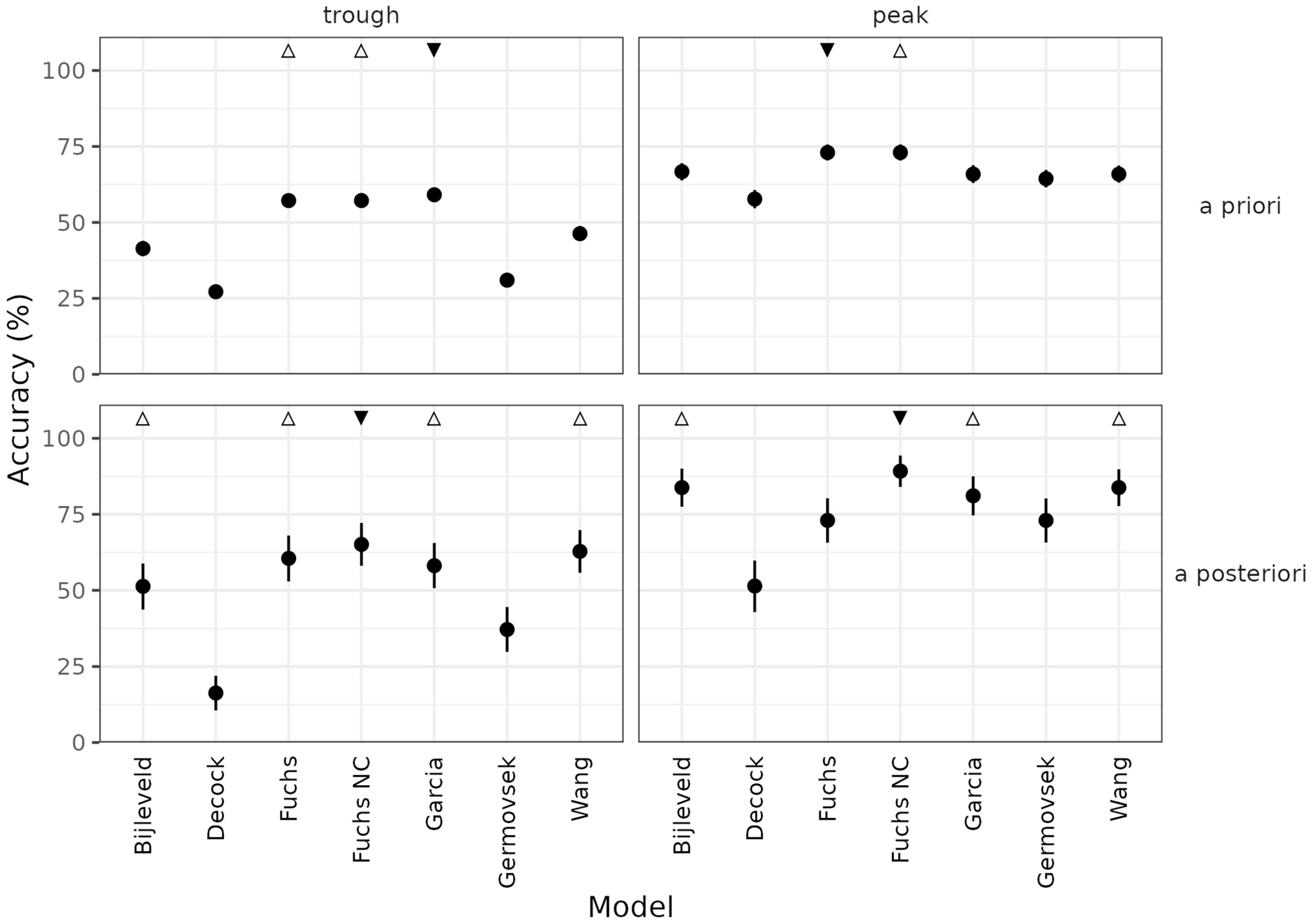
3.2. Evaluation of the Literature Models
3.3. Model Re-Estimation
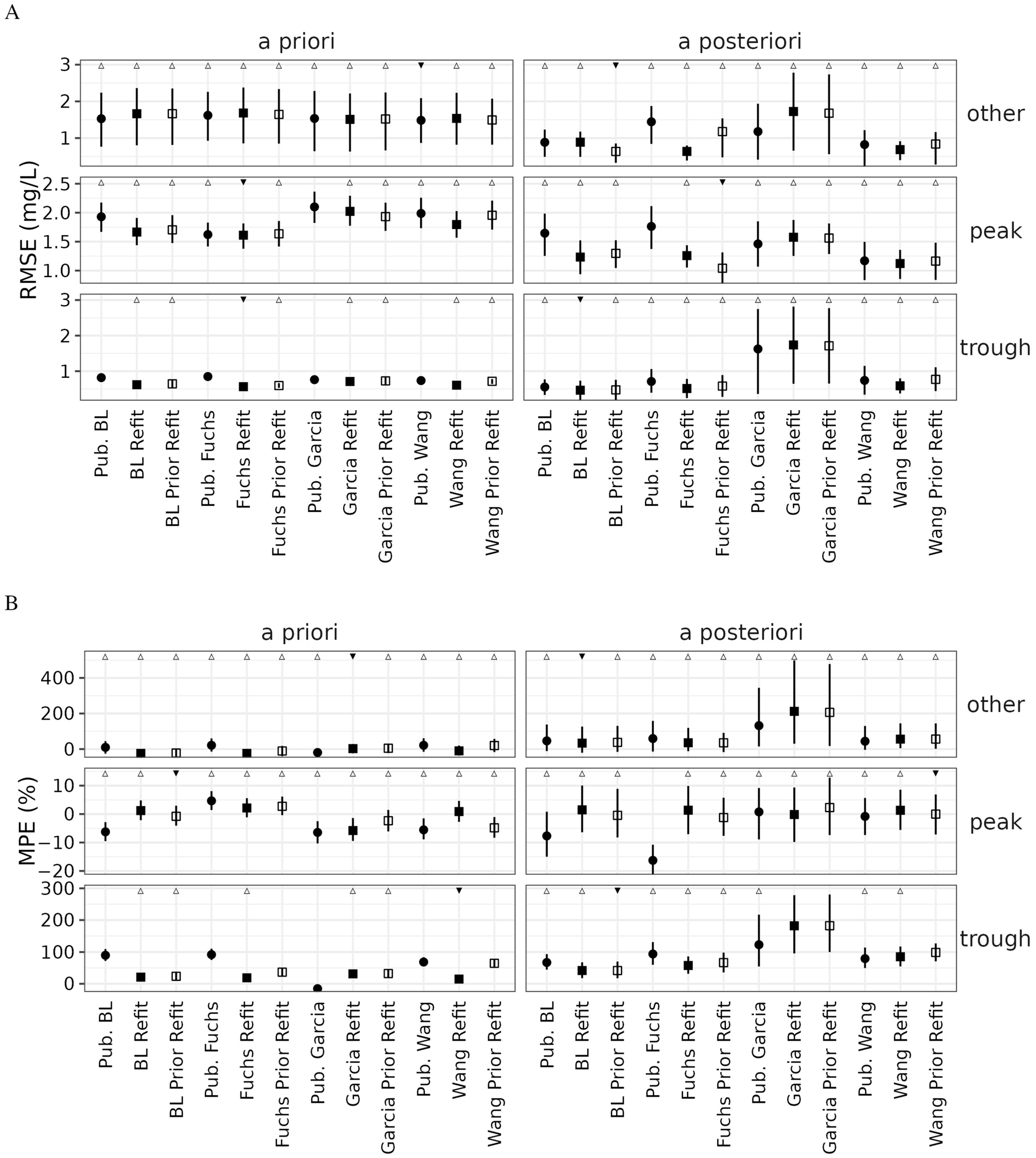
3.4. Re-Estimated Model Evaluation
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stocker, M.; Berger, C.; McDougall, J.; Giannoni, E. Recommendations for Term and Late Preterm Infants at Risk for Perinatal Bacterial Infection. Swiss Med. Wkly. 2013, 143, w13873. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Polin, R.A.; The Committee on Fetus and Newborn; Papile, L.-A.; Baley, J.E.; Bhutani, V.K.; Carlo, W.A.; Cummings, J.; Kumar, P.; Tan, R.C.; Wang, K.S.; et al. Management of Neonates with Suspected or Proven Early-Onset Bacterial Sepsis. Pediatrics 2012, 129, 1006–1015. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Novoa, J.M.; Quiros, Y.; Vicente, L.; Morales, A.I.; Lopez-Hernandez, F.J. New Insights into the Mechanism of Aminoglycoside Nephrotoxicity: An Integrative Point of View. Kidney Int. 2011, 79, 33–45. [Google Scholar] [CrossRef] [PubMed]
- Schultze, R.G.; Winters, R.E.; Kauffman, H. Possible Nephrotoxicity of Gentamicin. J. Infect. Dis. 1971, 124, S145–S147. [Google Scholar] [CrossRef]
- Wilfert, J.N.; Burke, J.P.; Bloomer, H.A.; Smith, C.B. Renal Insufficiency Associated with Gentamicin Therapy. J. Infect. Dis. 1971, 124, S148–S155. [Google Scholar] [CrossRef] [PubMed]
- Borradori, C.; Fawer, C.L.; Buclin, T.; Calame, A. Risk Factors of Sensorineural Hearing Loss in Preterm Infants. Neonatology 1997, 71, 1–10. [Google Scholar] [CrossRef]
- Pacifici, G.M. Clinical Pharmacokinetics of Aminoglycosides in the Neonate: A Review. Eur. J. Clin. Pharmacol. 2009, 65, 419–427. [Google Scholar] [CrossRef]
- Touw, D.J.; Westerman, E.M.; Sprij, A.J. Therapeutic Drug Monitoring of Aminoglycosides in Neonates. Clin. Pharmacokinet. 2009, 48, 71–88. [Google Scholar] [CrossRef]
- Keizer, R.J.; ter Heine, R.; Frymoyer, A.; Lesko, L.J.; Mangat, R.; Goswami, S. Model-Informed Precision Dosing at the Bedside: Scientific Challenges and Opportunities. CPT Pharmacomet. Syst. Pharmacol. 2018, 7, 785–787. [Google Scholar] [CrossRef]
- Fuchs, A.; Guidi, M.; Giannoni, E.; Werner, D.; Buclin, T.; Widmer, N.; Csajka, C. Population Pharmacokinetic Study of Gentamicin in a Large Cohort of Premature and Term Neonates: Population Pharmacokinetics of Gentamicin in Newborns. Br. J. Clin. Pharmacol. 2014, 78, 1090–1101. [Google Scholar] [CrossRef]
- Germovsek, E.; Kent, A.; Metsvaht, T.; Lutsar, I.; Klein, N.; Turner, M.A.; Sharland, M.; Nielsen, E.I.; Heath, P.T.; Standing, J.F. Development and Evaluation of a Gentamicin Pharmacokinetic Model That Facilitates Opportunistic Gentamicin Therapeutic Drug Monitoring in Neonates and Infants. Antimicrob. Agents Chemother. 2016, 60, 4869–4877. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Sherwin, C.; Gobburu, J.V.S.; Ivaturi, V. Population Pharmacokinetic Modeling of Gentamicin in Pediatrics. J. Clin. Pharmacol. 2019, 59, 1584–1596. [Google Scholar] [CrossRef]
- Bijleveld, Y.A.; van den Heuvel, M.E.; Hodiamont, C.J.; Mathôt, R.A.A.; de Haan, T.R. Population Pharmacokinetics and Dosing Considerations for Gentamicin in Newborns with Suspected or Proven Sepsis Caused by Gram-Negative Bacteria. Antimicrob. Agents Chemother. 2017, 61, e01304-16. [Google Scholar] [CrossRef] [PubMed]
- De Cock, R.F.W.; Allegaert, K.; Brussee, J.M.; Sherwin, C.M.T.; Mulla, H.; de Hoog, M.; van den Anker, J.N.; Danhof, M.; Knibbe, C.A.J. Simultaneous Pharmacokinetic Modeling of Gentamicin, Tobramycin and Vancomycin Clearance from Neonates to Adults: Towards a Semi-Physiological Function for Maturation in Glomerular Filtration. Pharm. Res. 2014, 31, 2643–2654. [Google Scholar] [CrossRef] [PubMed]
- Garcia, B.; Barcia, E.; Pérez, F.; Molina, I.T. Population Pharmacokinetics of Gentamicin in Premature Newborns. J. Antimicrob. Chemother. 2006, 58, 372–379. [Google Scholar] [CrossRef]
- Crcek, M.; Zdovc, J.; Kos, M.K. A Review of Population Pharmacokinetic Models of Gentamicin in Paediatric Patients. J. Clin. Pharm. Ther. 2019, 44, 659–674. [Google Scholar] [CrossRef]
- Hughes, J.H.; Tong, D.M.H.; Lucas, S.S.; Faldasz, J.D.; Goswami, S.; Keizer, R.J. Continuous Learning in Model-Informed Precision Dosing: A Case Study in Pediatric Dosing of Vancomycin. Clin. Pharmacol. Ther. 2021, 109, 233–242. [Google Scholar] [CrossRef]
- Shukla, P.; Goswami, S.; Keizer, R.J.; Winger, B.A.; Kharbanda, S.; Dvorak, C.C.; Long-Boyle, J. Assessment of a Model-Informed Precision Dosing Platform Use in Routine Clinical Care for Personalized Busulfan Therapy in the Pediatric Hematopoietic Cell Transplantation (HCT) Population. Front. Pharmacol. 2020, 11, 888. [Google Scholar] [CrossRef]
- Maier, C.; de Wiljes, J.; Hartung, N.; Kloft, C.; Huisinga, W. A Continued Learning Approach for Model-Informed Precision Dosing: Updating Models in Clinical Practice. CPT Pharmacomet. Syst. Pharmacol. 2022, 11, 185–198. [Google Scholar] [CrossRef]
- Bauer, R.J. NONMEM Users Guide: Introduction to NONMEM 7.2.0; ICON Development Solutions: Ellicott City, MD, USA, 2011. [Google Scholar]
- Bonate, P.L. Pharmacokinetic-Pharmacodynamic Modeling and Simulation, 2nd ed.; Springer: New York, NY, USA, 2011. [Google Scholar]
- Mould, D.; Upton, R. Basic Concepts in Population Modeling, Simulation, and Model-Based Drug Development. CPT Pharmacomet. Syst. Pharmacol. 2012, 1, 6. [Google Scholar] [CrossRef]
- United States Food and Drug Administration. Guidance for Industry: Population Pharmacokinetics. 1999. Available online: https://www.fda.gov/media/71364/download (accessed on 8 September 2022).
- Chan Kwong, A.H.-X.P.; Calvier, E.A.M.; Fabre, D.; Gattacceca, F.; Khier, S. Prior Information for Population Pharmacokinetic and Pharmacokinetic/Pharmacodynamic Analysis: Overview and Guidance with a Focus on the NONMEM PRIOR Subroutine. J. Pharmacokinet. Pharmacodyn. 2020, 47, 431–446. [Google Scholar] [CrossRef] [PubMed]
- Lindbom, L.; Pihlgren, P.; Jonsson, N. PsN-Toolkit—A Collection of Computer Intensive Statistical Methods for Non-Linear Mixed Effect Modeling Using NONMEM. Comput. Methods Programs Biomed. 2005, 79, 241–257. [Google Scholar] [CrossRef] [PubMed]
- ter Heine, R.; Keizer, R.J.; van Steeg, K.; Smolders, E.J.; van Luin, M.; Derijks, H.J.; Jager, C.P.C.; Frenzel, T.; Brüggemann, R. Prospective Validation of a Model-informed Precision Dosing Tool for Vancomycin in Intensive Care Patients. Br. J. Clin. Pharmacol. 2020, 86, 2497–2506. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, H.; Dirks, N.L.; Rosario, M.; Hori, T.; Hibi, T. Population Pharmacokinetics of Vedolizumab in Asian and Non-Asian Patients with Ulcerative Colitis and Crohn’s Disease. Intest. Res. 2021, 19, 95–105. [Google Scholar] [CrossRef]
- Toyoshima, J.; Shibata, M.; Kaibara, A.; Kaneko, Y.; Izutsu, H.; Nishimura, T. Population Pharmacokinetic Analysis of Peficitinib in Patients with Rheumatoid Arthritis. Br. J. Clin. Pharmacol. 2021, 87, 2014–2022. [Google Scholar] [CrossRef]
- Kwong, A.C.; O’Jeanson, A.; Khier, S. Model-Informed Therapeutic Drug Monitoring of Meropenem in Critically Ill Patients: Improvement of the Predictive Ability of Literature Models with the PRIOR Approach. Eur. J. Drug Metab. Pharmacokinet. 2021, 46, 415–426. [Google Scholar] [CrossRef]



| Characteristic | Overall | Training Data | Validation Data |
|---|---|---|---|
| Number of Patients | 475 | 332 | 143 |
| Number of Sites | 9 | 9 | 9 |
| Number of TDMs | 842 (304 peaks, 466 troughs, 72 other) | 590 (210 peaks, 328 troughs, 52 other) | 252 (94 peaks, 138 troughs, 20 other) |
| Age (days) | 1.46 (0.36–81.9) | 1.46 (0.36–81.9) | 1.46 (0.36–41.1) |
| Gestational age (weeks) | 36.7 (23.7–43) | 36.6 (23.9–43) | 37 (23.7–41.4) |
| Serum creatinine (mg/dL) | 0.64 (0.15–2.79) | 0.64 (0.15–2.79) | 0.63 (0.19–2.05) |
| Weight (kg) | 2.76 (0.37–5.44) | 2.67 (0.37–4.94) | 2.86 (0.49–5.44) |
| Model | Pts | Samples | PNA (d) | GA (wk) | WT (kg) | CR (mg/dL) | Model Covariates |
|---|---|---|---|---|---|---|---|
| Bijleveld [13] | 65 | 136 | 1 (0–31) | 32 (25–42) | 1.84 (0.43–4.67) | 0.63 (0.29–1.3) | WT, PMA |
| De Cock [14] | 717 | 1705 | 2 (1–5475) | (23–43) | 2.6 (0.44–80) | 0.82 (0.14–1.18) | WT |
| Fuchs [10] | 1518 | 3039 | 1 (0–94) | 34 (24–42) | 2.2 (0.44–5.5) | NG | WT, GA, PNA, dopamine coadmin |
| Garcia [15] | 200 | 417 | 5.49 (5.41) | 32.19 (2.97) | 1.68 (0.63) | NG | WT, PNA, CRCL |
| Germovsek [11] | 205 | 1325 | 5.1 (1–66) | 34 (23.3–42.1) | 2.12 (0.53–5.05) | NG | WT, GA, PNA, CR |
| Wang [12] | 2357 | 6359 | 1 (1–6924) | 37 (21–42) | 3.43 (1.1–5.83) | 0.66 (0.14–3.8) | WT, HT, CR, PNA, PMA |
| Current Study Data | 475 | 842 | 1.46 (0.36–81.9) | 36.7 (23.7–43) | 2.76 (0.37–5.44) | 0.64 (0.15–2.79) | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tong, D.M.H.; Hughes, J.H.; Keizer, R.J. Evaluating and Improving Neonatal Gentamicin Pharmacokinetic Models Using Aggregated Routine Clinical Care Data. Pharmaceutics 2022, 14, 2089. https://doi.org/10.3390/pharmaceutics14102089
Tong DMH, Hughes JH, Keizer RJ. Evaluating and Improving Neonatal Gentamicin Pharmacokinetic Models Using Aggregated Routine Clinical Care Data. Pharmaceutics. 2022; 14(10):2089. https://doi.org/10.3390/pharmaceutics14102089
Chicago/Turabian StyleTong, Dominic M. H., Jasmine H. Hughes, and Ron J. Keizer. 2022. "Evaluating and Improving Neonatal Gentamicin Pharmacokinetic Models Using Aggregated Routine Clinical Care Data" Pharmaceutics 14, no. 10: 2089. https://doi.org/10.3390/pharmaceutics14102089
APA StyleTong, D. M. H., Hughes, J. H., & Keizer, R. J. (2022). Evaluating and Improving Neonatal Gentamicin Pharmacokinetic Models Using Aggregated Routine Clinical Care Data. Pharmaceutics, 14(10), 2089. https://doi.org/10.3390/pharmaceutics14102089






