Novel Pullulan/Gellan Gum Bilayer Film as a Vehicle for Silibinin-Loaded Nanocapsules in the Topical Treatment of Atopic Dermatitis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Preparation of Nanocapsule Suspensions and Bilayer Films
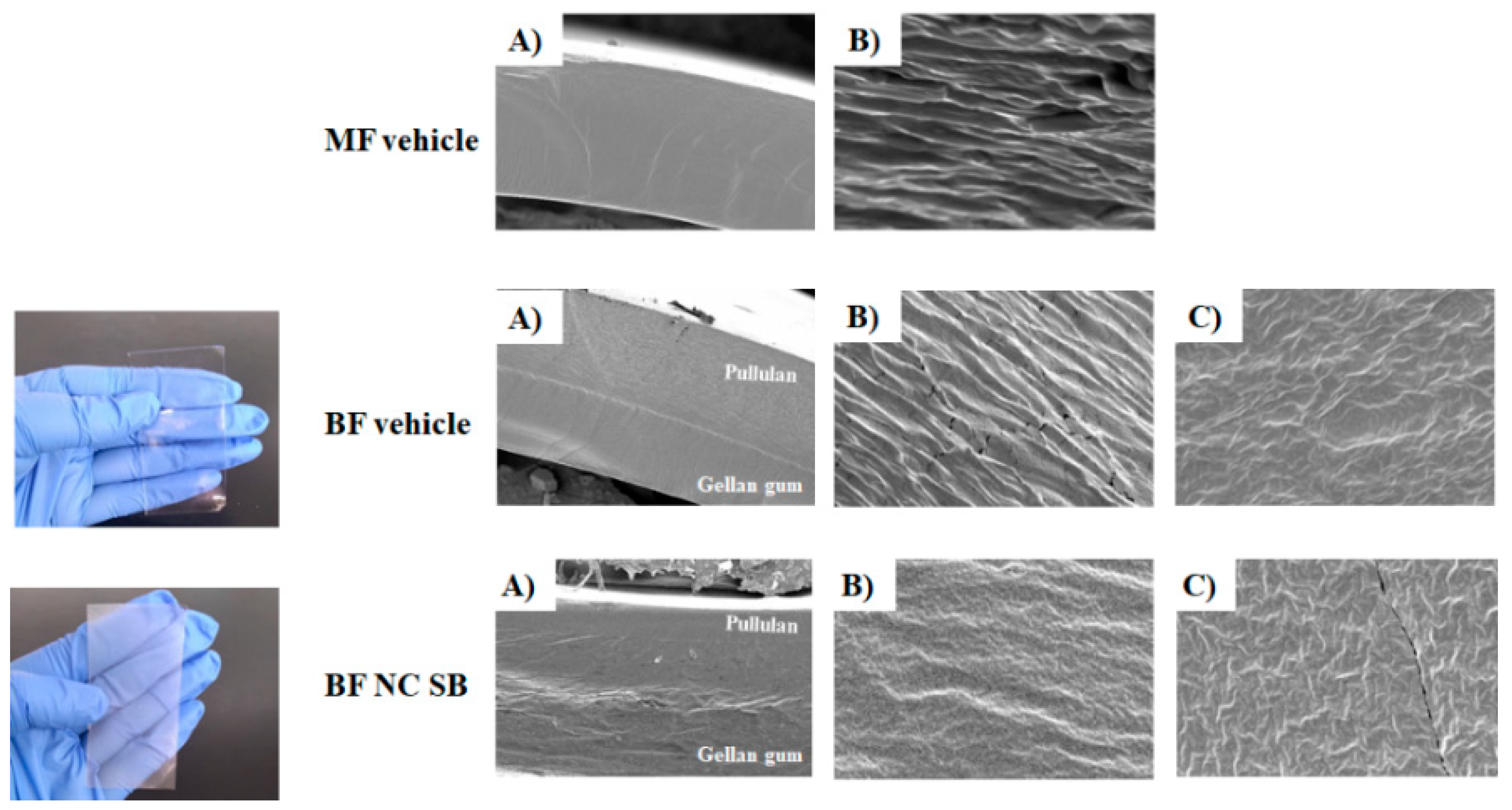
2.2.2. Scanning Electron Microscopy
2.2.3. Bilayer Films Characterization
2.2.4. Folding Endurance and Mechanical Properties
2.2.5. In vitro Studies
Occlusion Test
Skin Preparation
Bioadhesive Strength
SB Release and Skin Permeation/Penetration Study
Free Radical Scavenging Activity
Hemocompatibility Evaluation of Formulations
2.2.6. In Vivo Study
Animals
Experimental Design
2.2.7. AD-like Clinical Signs
Scratching Behavior
Clinical Skin Severity Scores
2.2.8. Evaluation of the Inflammation Markers
Ear Swelling
NOx Content
2.2.9. Evaluation of the Immune Function
Spleen Index
2.2.10. Evaluation of the Oxidative Stress Markers
Tissue Preparation
Protein Concentration
TBARS Levels
NPSH Levels
CAT Activity
2.2.11. Statistical Analysis
3. Results
3.1. The Bilayer Films Presented Suitable Physicochemical Characteristics
3.2. The Nanocapsules Improved the Occlusive Potential of Bilayer Film
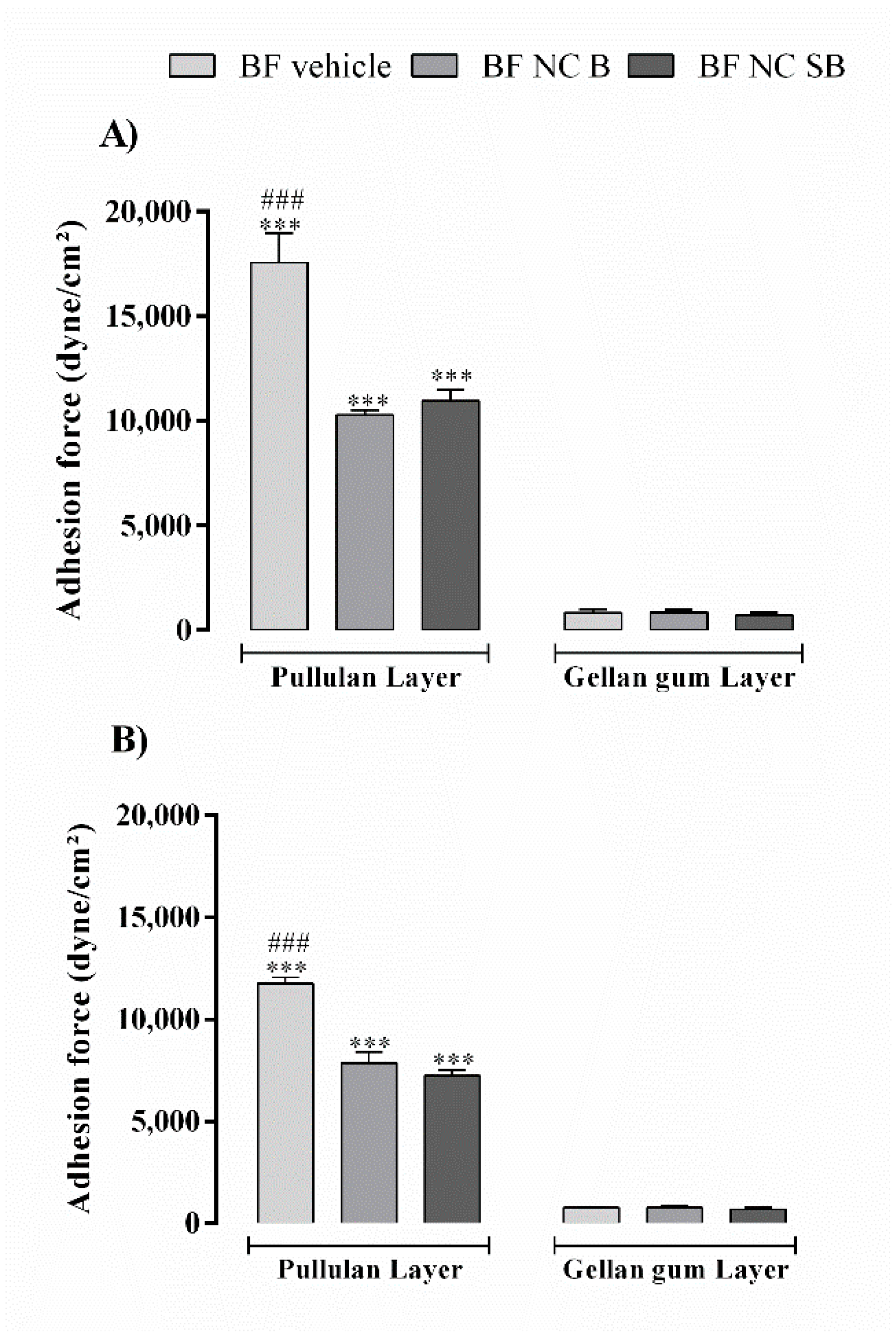
3.3. The Pullulan Layer Confers Bioadhesion to the Film
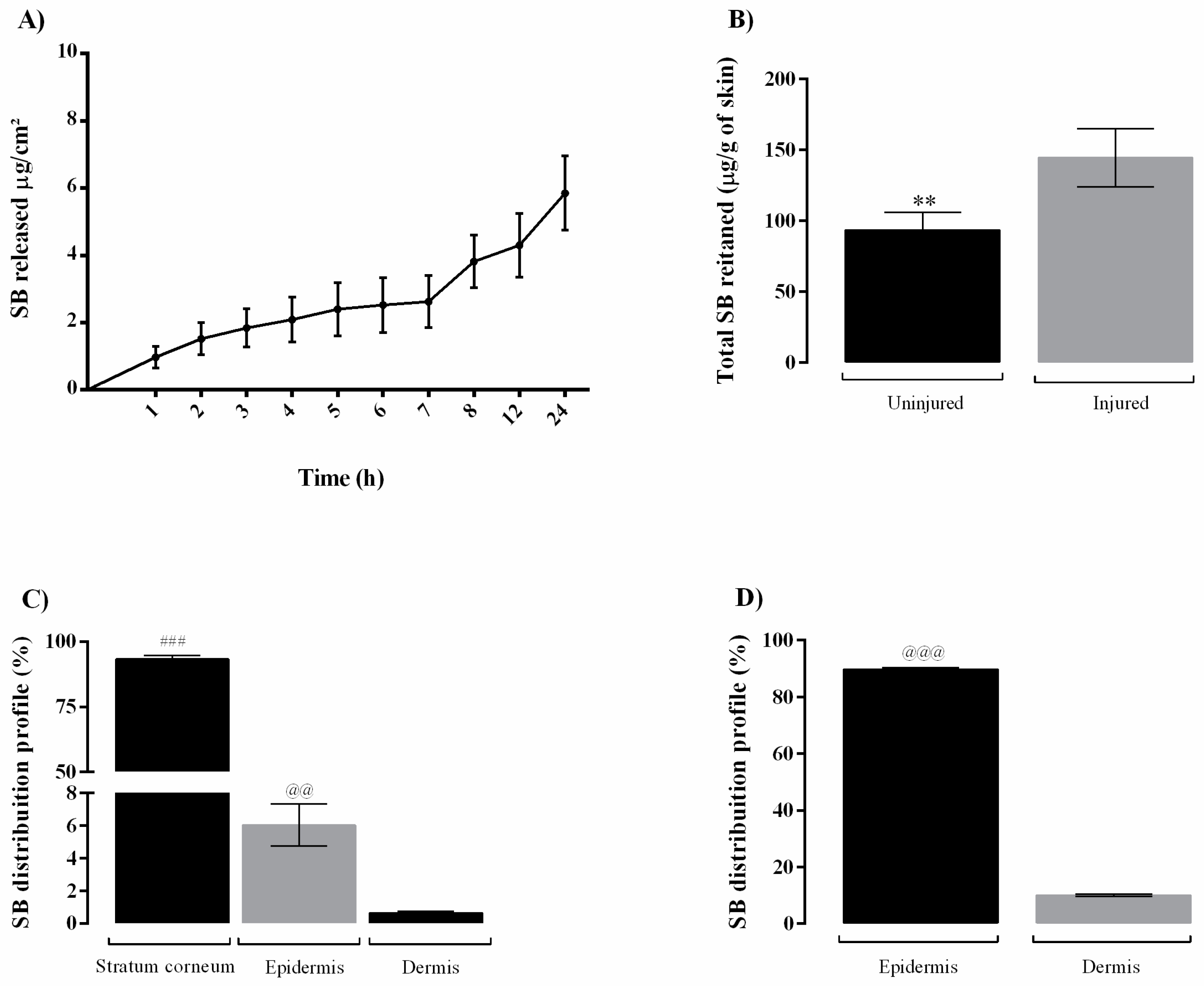
3.4. The BF NC SB Slowly Releases SB and Retains it in the Skin
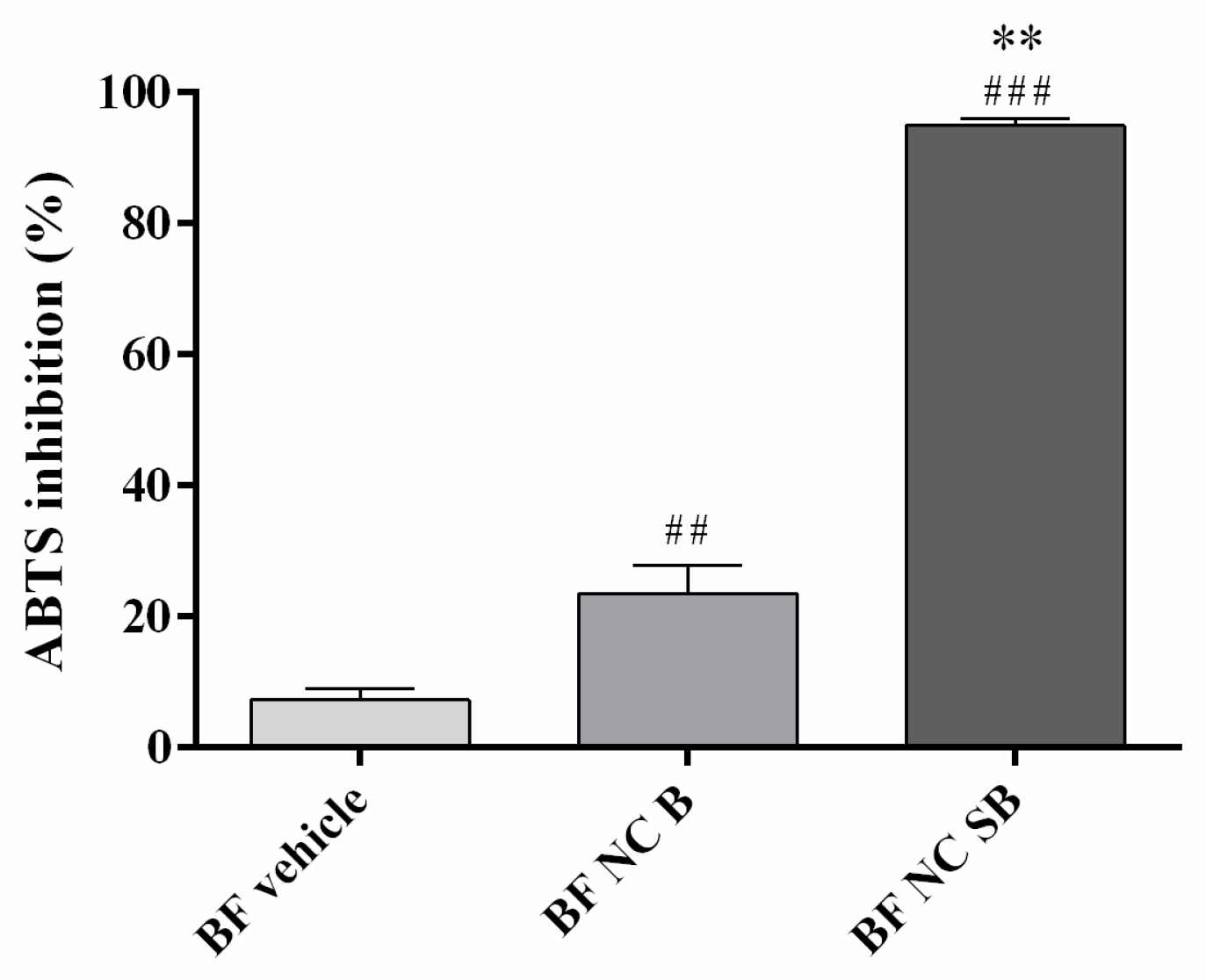
3.5. The BF NC SB Neutralized the ABTS+ Radical
3.6. The Bilayer Films Are Hemocompatible
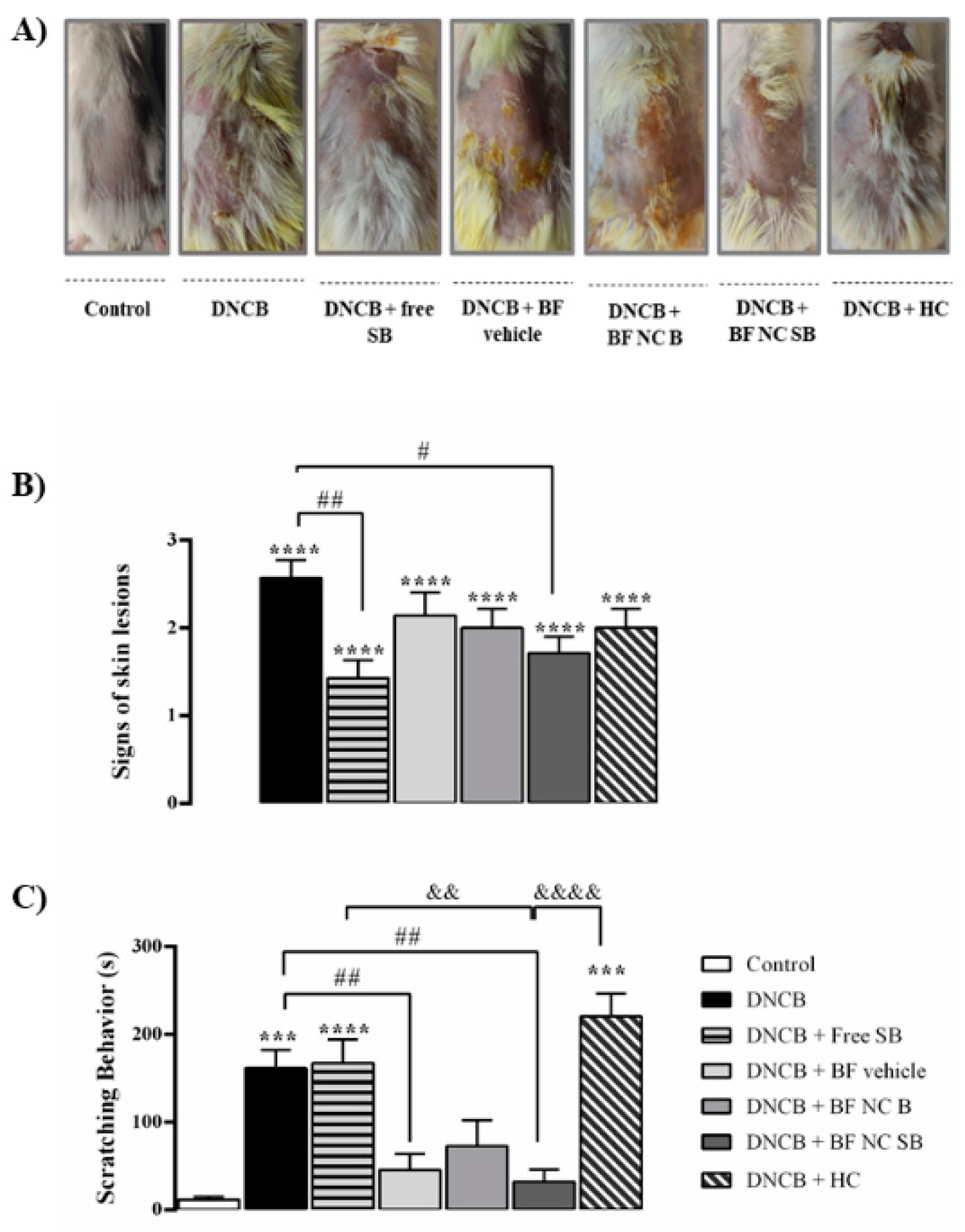
3.7. The BF NC SB Treatment Attenuated the AD-like Clinical Signs Induced by DNCB in Mice
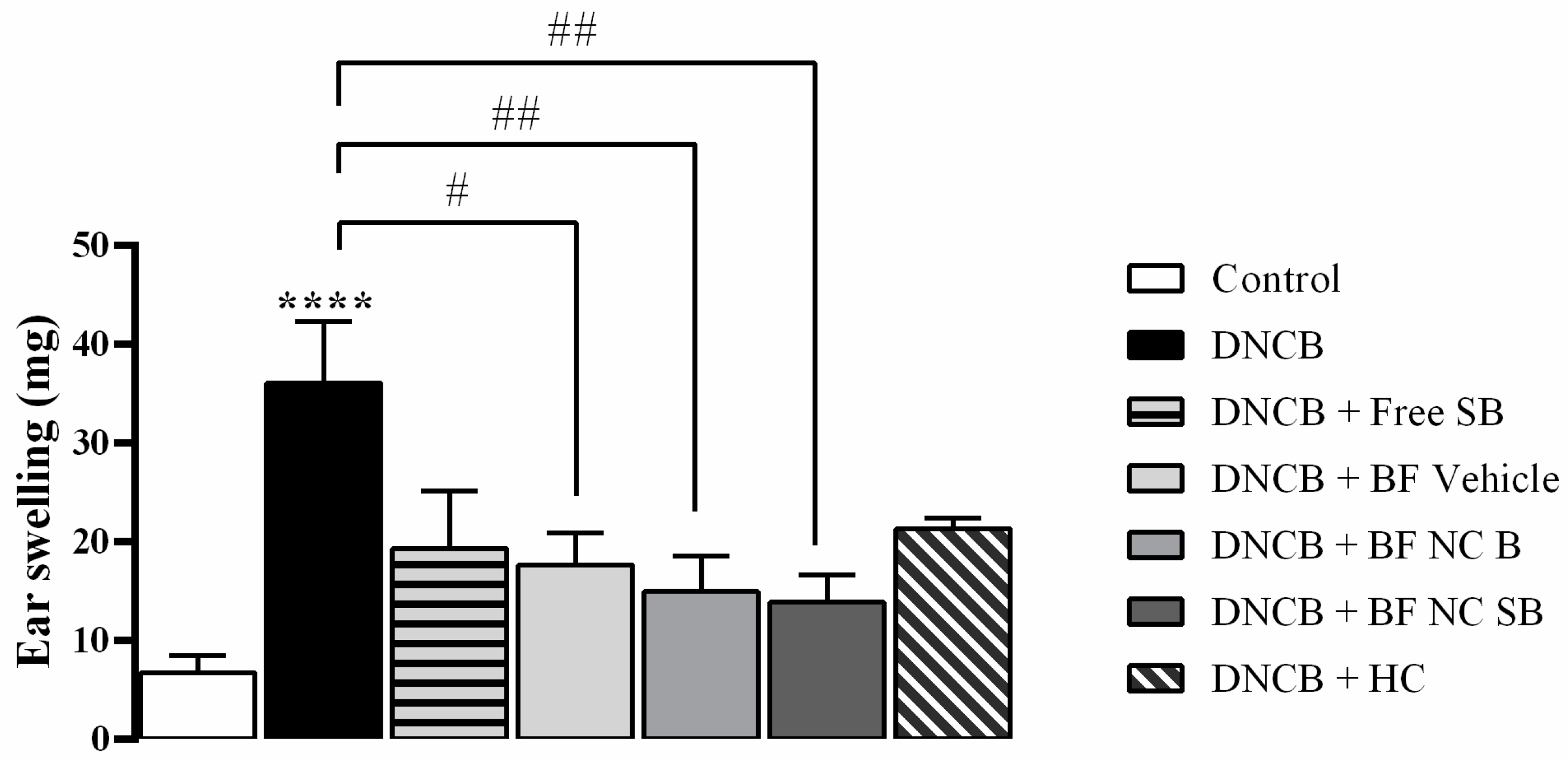
3.8. The BF NC SB Treatment Suppressed the Ear Swelling Induced by DNCB in Mice
3.9. The BF NC SB Treatment Did Not Alter the Spleen Index after DNCB Exposure in Mice
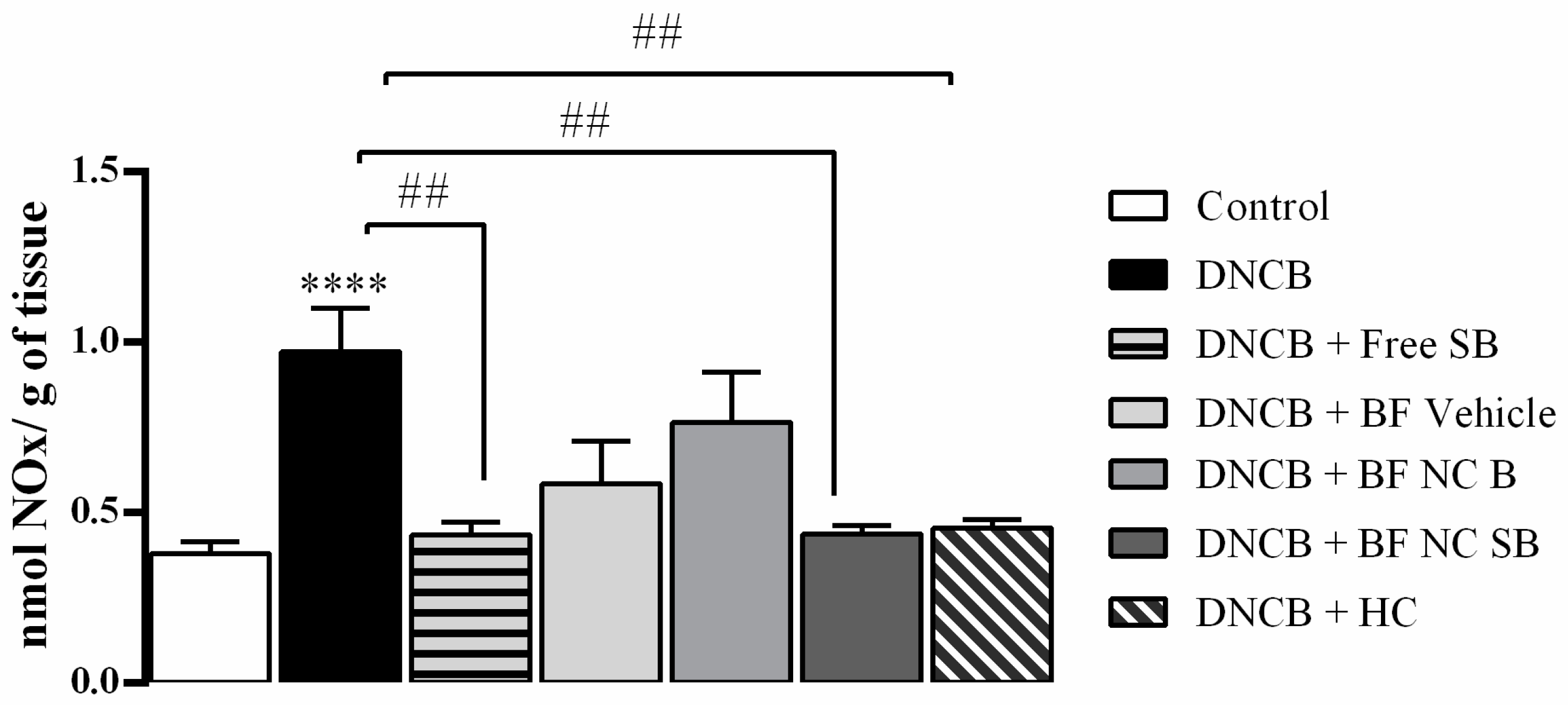
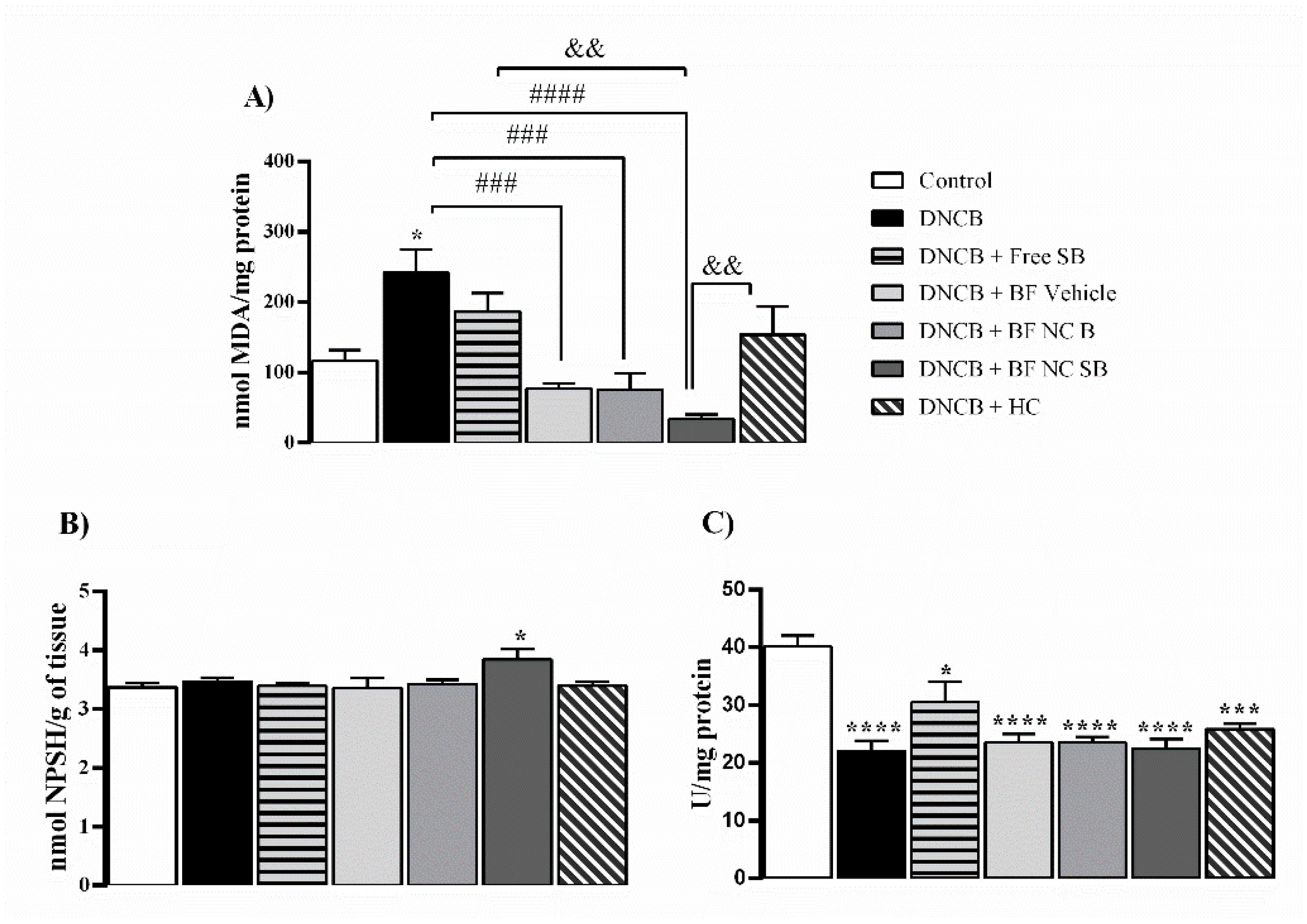
3.10. The BF NC SB Treatment Modulated Some Markers of Oxidative Stress and Inflammation in the Dorsal Skin of Mice Exposed to DNCB
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Malik, K.; Heitmiller, K.D. An Update on the Pathophysiology of Atopic Dermatitis. Dermatol. Clin. 2017, 35, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Rerknimitr, P.; Otsuka, A.; Nakashima, C.; Kabashima, K. The Etiopathogenesis of Atopic Dermatitis: Barrier Disruption, Immunological Derangement, and Pruritus. Inflamm. Regen. 2017, 37, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mancuso, J.B.; Lee, S.S.; Paller, A.S.; Ohya, Y. Management of Severe Atopic Dermatitis in Pediatric Patients. J. Allergy Clin. Immunol. Pract. 2021, 9, 1462–1471. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Pang, Y.; He, Y.; Zhang, X.; Peng, L.; Guo, J.; Zeng, J. A Comprehensive Review of Natural Products against Atopic Dermatitis: Flavonoids, Alkaloids, Terpenes, Glycosides and Other Compounds. Biomed. Pharmacother. 2021, 140, 111741. [Google Scholar] [CrossRef]
- Song, X.; Zhou, B.; Cui, L.; Lei, D.; Zhang, P.; Yao, G.; Xia, M.; Hayashi, T.; Hattori, S.; Ushiki-Kaku, Y.; et al. Silibinin Ameliorates Aβ25-35-Induced Memory Deficits in Rats by Modulating Autophagy and Attenuating Neuroinflammation as Well as Oxidative Stress. Neurochem. Res. 2017, 42, 1073–1083. [Google Scholar] [CrossRef] [PubMed]
- Samanta, R.; Pattnaik, A.; Pradhan, K.; Mehta, B.; Pattanayak, S.; Banerjee, S. Wound Healing Activity of Silibinin in Mice. Pharmacogn. Res. 2016, 8, 298. [Google Scholar] [CrossRef] [Green Version]
- Rigon, C.; Crivellaro, M.; Marchiori, L.; Jardim, S.; Schopf, N.; Chaves, S.; Callegaro, M.; Carlos, R.; Beck, R.; Ferreira, A.; et al. Hydrogel Containing Silibinin Nanocapsules Presents Effective Anti- Inflammatory Action in a Model of Irritant Contact Dermatitis in Mice. Eur. J. Pharm. Sci. 2019, 137, 104969. [Google Scholar] [CrossRef]
- Shrotriya, S.N.; Vidhate, B.V.; Shukla, M.S. Formulation and Development of Silybin Loaded Solid Lipid Nanoparticle Enriched Gel for Irritant Contact Dermatitis. J. Drug Deliv. Sci. Technol. 2017, 41, 164–173. [Google Scholar] [CrossRef]
- Atrux-Tallau, N.; Romagny, C.; Padois, K.; Denis, A.; Haftek, M.; Falson, F.; Pirot, F.; Maibach, H.I. Effects of Glycerol on Human Skin Damaged by Acute Sodium Lauryl Sulphate Treatment. Arch. Dermatol. Res. 2010, 302, 435–441. [Google Scholar] [CrossRef]
- Marchiori, M.C.L.; Rigon, C.; Camponogara, C.; Oliveira, S.M.; Cruz, L. Hydrogel Containing Silibinin-Loaded Pomegranate Oil Based Nanocapsules Exhibits Anti-Inflammatory Effects on Skin Damage UVB Radiation-Induced in Mice. J. Photochem. Photobiol. B Biol. 2017, 170, 25–32. [Google Scholar] [CrossRef]
- Li, G.; Fan, C.; Li, X.; Fan, Y.; Wang, X.; Li, M.; Liu, Y. Preparation and In Vitro Evaluation of Tacrolimus-Loaded Ethosomes. Sci. World J. 2012, 2012, 874053. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Cao, S.; Yu, K.; Yang, F.; Yu, X.; Zhai, Y.; Wu, C.; Xu, Y. Integrating Tacrolimus into Eutectic Oil-Based Microemulsion for Atopic Dermatitis: Simultaneously Enhancing Percutaneous Delivery and Treatment Efficacy with Relieving Side Effects. Int. J. Nanomed. 2019, 14, 5849–5863. [Google Scholar] [CrossRef] [Green Version]
- Badihi, A.; Fru, M.; Soroka, Y.; Benhamron, S.; Tzur, T.; Nassar, T.; Benita, S. Topical Nano-Encapsulated Cyclosporine Formulation for Atopic Dermatitis Treatment. Nanomed. Nanotechnol. Biol. Med. 2020, 24, 102140. [Google Scholar] [CrossRef]
- Mora-Huertas, C.E.; Fessi, H.; Elaissari, A. Polymer-Based Nanocapsules for Drug Delivery. Int. J. Pharm. 2010, 385, 113–142. [Google Scholar] [CrossRef]
- Ferreira, L.M.; Sari, M.H.M.; Azambuja, J.H.; da Silveira, E.F.; Cervi, V.F.; Marchiori, M.C.L.; Maria-Engler, S.S.; Wink, M.R.; Azevedo, J.G.; Nogueira, C.W.; et al. Xanthan Gum-Based Hydrogel Containing Nanocapsules for Cutaneous Diphenyl Diselenide Delivery in Melanoma Therapy. Investig. New Drugs 2019, 38, 662–674. [Google Scholar] [CrossRef]
- Jeong, J.H.; Back, S.K.; An, J.H.; Lee, N.; Kim, D.; Na, C.S.; Jeong, Y.; Han, S.Y. Topical Film Prepared with Rhus Verniciflua Extract-Loaded Pullulan Hydrogel for Atopic Dermatitis Treatment. J. Biomed. Mater. Res. 2019, 107, 1–10. [Google Scholar] [CrossRef]
- Alves, N.O.; Gabriela, T.; Weber, D.M.; Luchese, C.; Wilhelm, E.A.; Fajardo, A.R. Chitosan/Poly (Vinyl Alcohol)/Bovine Bone Powder Biocomposites: A Potential Biomaterial for the Treatment of Atopic Dermatitis-like Skin Lesions. Carbohydr. Polym. 2016, 148, 115–124. [Google Scholar] [CrossRef]
- Cervi, V.F.; Saccol, C.P.; Sari, M.H.M.; Martins, C.C.; Da Rosa, L.S.; Ilha, B.D.; Soares, F.Z.; Luchese, C.; Wilhelm, E.A.; Cruz, L. Pullulan Film Incorporated with Nanocapsules Improves Pomegranate Seed Oil Anti-Inflammatory and Antioxidant Effects in the Treatment of Atopic Dermatitis in Mice. Int. J. Pharm. 2021, 609, 121144. [Google Scholar] [CrossRef]
- Karki, S.; Kim, H.; Na, S.; Shin, D.; Jo, K.; Lee, J. Thin Films as an Emerging Platform for Drug Delivery. Asian J. Pharm. Sci. 2016, 11, 559–574. [Google Scholar] [CrossRef] [Green Version]
- Ismail, N.A.; Amin, K.A.M.; Majid, F.A.A.; Razali, M.H. Gellan Gum Incorporating Titanium Dioxide Nanoparticles Biofilm as Wound Dressing: Physicochemical, Mechanical, Antibacterial Properties and Wound Healing Studies. Mater. Sci. Eng. C 2019, 103, 109770. [Google Scholar] [CrossRef]
- Razali, M.H.; Ismail, N.A.; Amin, K.A.M. Nanotubos de dióxido de titânio incorporaram filme bio-nanocompósito de goma gelana para cicatrização de feridas: Efeito da concentração de nanotubos de TiO2. Int. J. Biol. Macromol. 2020, 153, 1117–1135. [Google Scholar] [CrossRef] [PubMed]
- Cervi, V.F.; Saccol, C.P.; Da Rosa Pinheiro, T.; Santos, R.C.V.; Cruz, L.; Sari, M.H.M. A Novel Nanotechnological Mucoadhesive and Fast-Dissolving Film for Vaginal Delivery of Clotrimazole: Design, Characterization, and In Vitro Antifungal Action. Drug Deliv. Transl. Res. 2022, 5, 1–13. [Google Scholar] [CrossRef]
- Contardi, M.; Russo, D.; Suarato, G.; Heredia-Guerrero, J.A.; Ceseracciu, L.; Penna, I.; Margaroli, N.; Summa, M.; Spanò, R.; Tassistro, G.; et al. Polyvinylpyrrolidone/Hyaluronic Acid-Based Bilayer Constructs for Sequential Delivery of Cutaneous Antiseptic and Antibiotic. Chem. Eng. J. 2019, 358, 912–923. [Google Scholar] [CrossRef]
- Neto, R.J.G.; Maria, G.; De Almeida, L.; Santos, P.; Agostini, M.; Moraes, D.; Masumi, M. Characterization and in Vitro Evaluation of Chitosan/Konjac Glucomannan Bilayer Film as a Wound Dressing. Carbohydr. Polym. 2019, 212, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Dhal, C.; Mishra, R. In Vitro and in Vivo Evaluation of Gentamicin Sulphate-Loaded PLGA Nanoparticle-Based Film for the Treatment of Surgical Site Infection. Drug Deliv. Transl. Res. 2020, 10, 1032–1043. [Google Scholar] [CrossRef]
- Shahzad, A.; Khan, A.; Afzal, Z.; Farooq, M.; Khan, J.; Majid, G. Formulation Development and Characterization of Cefazolin Nanoparticles-Loaded Cross-Linked Films of Sodium Alginate and Pectin as Wound Dressings. Int. J. Biol. Macromol. 2019, 124, 255–269. [Google Scholar] [CrossRef]
- Gehrcke, M.; Brum, T.B.; Rosa, L.S.; Ilha, B.D.; Soares, F.Z.M.; Cruz, L. Incorporation of Nanocapsules into Gellan Gum Films: A Strategy to Improve the Stability and Prolong the Cutaneous Release of Silibinin. Mater. Sci. Eng. C 2021, 119, 111624. [Google Scholar] [CrossRef]
- Fessi, H.; Puisieux, F.; Devissaguet, J.P.; Ammoury, N.; Benita, S. Nanocapsule Formation by Interfacial Polymer Deposition Following Solvent Displacement. Int. J. Pharm. 1989, 55, R1–R4. [Google Scholar] [CrossRef]
- ASTM. Standard Test Method for Tensile Properties of Thin Plastic Sheeting-D882-02; ASTM International: West Conshohocken, PA, USA, 2002. [Google Scholar]
- Schlupp, P.; Weber, M.; Schmidts, T.; Geiger, K.; Runkel, F. Development and Validation of an Alternative Disturbed Skin Model by Mechanical Abrasion to Study Drug Penetration. Results Pharma. Sci. 2014, 4, 26–33. [Google Scholar] [CrossRef] [Green Version]
- Osmari, B.F.; Giuliani, L.M.; Reolon, J.B.; Rigo, G.V.; Tasca, T.; Cruz, L. Gellan Gum-Based Hydrogel Containing Nanocapsules for Vaginal Indole-3- Carbinol Delivery in Trichomoniasis Treatment. Eur. J. Pharm. Sci. 2020, 151, 105379. [Google Scholar] [CrossRef]
- Yang, N.; Jia, X.; Wang, D.; Wei, C.; He, Y.; Chen, L.; Zhao, Y. Silibinin as a Natural Antioxidant for Modifying Polysulfone Membranes to Suppress Hemodialysis-Induced Oxidative Stress. J. Memb. Sci. 2019, 574, 86–99. [Google Scholar] [CrossRef]
- ASTM. Standard Practice for Assessment of Hemolytic Properties of Materials-F 756-00; ASTM International: West Conshohocken, PA, USA, 2020. [Google Scholar]
- Chan, C.C.; Liou, C.J.; Xu, P.Y.; Shen, J.J.; Kuo, M.L.; Len, W.B.; Chang, L.E.; Huang, W.C. Effect of Dehydroepiandrosterone on Atopic Dermatitis-like Skin Lesions Induced by 1-Chloro-2,4-Dinitrobenzene in Mouse. J. Dermatol. Sci. 2013, 72, 149–157. [Google Scholar] [CrossRef]
- Voss, G.T.; Oliveira, R.L.; de Souza, J.F.; Duarte, L.F.B.; Fajardo, A.R.; Alves, D.; Luchese, C.; Wilhelm, E.A. Therapeutic and Technological Potential of 7-Chloro-4-Phenylselanyl Quinoline for the Treatment of Atopic Dermatitis-like Skin Lesions in Mice. Mater. Sci. Eng. C 2018, 84, 90–98. [Google Scholar] [CrossRef]
- Weber, D.M.; Voss, G.T.; De Oliveira, R.L.; da Fonseca, C.A.R.; Paltian, J.; Rodrigues, K.C.; Ianiski, F.R.; Vaucher, R.A.; Luchese, C.; Wilhelma, E.A. Topic Application of Meloxicam-Loaded Polymeric Nanocapsules as a Technological Alternative for Treatment of the Atopic Dermatitis in Mice. J. Appl. Biomed. J. 2018, 16, 337–343. [Google Scholar] [CrossRef]
- Kim, H.; Kim, J.R.; Kang, H.; Choi, J.; Yang, H.; Lee, P.; Kim, J.; Lee, K.W. 7,8,4′-Trihydroxyisoflavone Attenuates DNCB-Induced Atopic Dermatitis-like Symptoms in NC/Nga Mice. PLoS ONE 2014, 9, e104938. [Google Scholar] [CrossRef]
- Park, G.; Oh, M.S. Inhibitory Effects of Juglans Mandshurica Leaf on Allergic Dermatitis-like Skin Lesions-Induced by 2,4-Dinitrochlorobenzene in Mice. Exp. Toxicol. Pathol. 2014, 66, 97–101. [Google Scholar] [CrossRef]
- Green, L.C.; Wagner, D.A.; Glogowski, J.; Skipper, P.L.; Wishnok, J.S.; Tannenbaum, S.R. Analysis of Nitrate, Nitrite, and [15N]Nitrate in Biological Fluids. Anal. Biochem. 1982, 126, 131–138. [Google Scholar] [CrossRef]
- Bradford, M.M. A Rapid and Sensitive Method for the Quantitation of Microgram Quantities of Protein Utilizing the Principle of Protein-Dye Binding. Anal. Biochem. 1976, 72, 248–254. [Google Scholar] [CrossRef]
- Ohkawa, H.; Ohishi, N.; Yagi, K. Assay for Lipid Peroxides in Animal Tissues Thiobarbituric Acid Reaction. Anal. Biochem. 1979, 358, 351–358. [Google Scholar] [CrossRef]
- Ellman, G.L. Tissue sulfhydryl groups. Am. J. Anal. Chem. 1959, 82, 70–77. [Google Scholar] [CrossRef]
- Aebi, H. Catalase in vitro. Methods Enzymol. 1984, 105, 121–126. [Google Scholar] [PubMed]
- Dixit, R.P.; Puthli, S.P. Oral Strip Technology: Overview and Future Potential. J. Control. Release 2009, 139, 94–107. [Google Scholar] [CrossRef] [PubMed]
- Machado, A.; Cunha-reis, C.; Araújo, F.; Nunes, R.; Seabra, V.; Ferreira, D.; Sarmento, B. Development and in Vivo Safety Assessment of Tenofovir-Loaded Nanoparticles-in-Film as a Novel Vaginal Microbicide Delivery System. Acta Biomater. 2016, 44, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Ghorbani, M.; Hassani, N.; Raeisi, M. Development of Gelatin Thin Film Reinforced by Modified Gellan Gum and Naringenin-Loaded Zein Nanoparticle as a Wound Dressing. Macromol. Res. 2022, 30, 397–405. [Google Scholar] [CrossRef]
- Evans, N.D.; Oreffo, R.O.C.; Healy, E.; Thurner, P.J.; Hin, Y. Epithelial Mechanobiology, Skin Wound Healing, and the Stem Cell Niche. J. Mech. Behav. Biomed. Mater. 2013, 28, 397–409. [Google Scholar] [CrossRef] [Green Version]
- De Lima, J.A.; Paines, T.C.; Motta, M.H.; Weber, W.B.; Santos, S.S.; Cruz, L.; Silva, C.D.B. Novel Pemulen/Pullulan Blended Hydrogel Containing Clotrimazole-Loaded Cationic Nanocapsules: Evaluation of Mucoadhesion and Vaginal Permeation. Mater. Sci. Eng. C 2017, 79, 886–893. [Google Scholar] [CrossRef]
- Pagano, C.; Rachele, M.; Calarco, P.; Scuota, S.; Conte, C.; Primavilla, S.; Ricci, M.; Perioli, L. Bioadhesive Polymeric Films Based on Usnic Acid for Burn Wound Treatment: Antibacterial and Cytotoxicity Studies. Colloids Surf. B Biointerfaces 2019, 178, 488–499. [Google Scholar] [CrossRef]
- Parisotto-peterle, J.; Bidone, J.; Lucca, L.G.; de Moraes Soares Araújo, G.; Falkembach, M.C.; da Silva Marques, M.; Horn, A.P.; dos Santos, M.K.; da Veiga, V.F.; Limberger, R.P.; et al. Healing Activity of Hydrogel Containing Nanoemulsified β-Caryophyllene. Eur. J. Pharm. Sci. 2020, 148, 105318. [Google Scholar] [CrossRef]
- Mansuri, S.; Kesharwani, P.; Jain, K.; Tekade, R.K.; Jain, N.K. Mucoadhesion: A Promising Approach in Drug Delivery System. React. Funct. Polym. 2016, 100, 151–172. [Google Scholar] [CrossRef]
- Pagano, C.; Latterini, L.; Di Michele, A.; Luzi, F.; Puglia, D.; Ricci, M.; Viseras, A.; Perioli, L. Polymeric Bioadhesive Patch Based on Ketoprofen-Hydrotalcite Hybrid for Local Treatments. Pharmaceutics 2020, 12, 733. [Google Scholar] [CrossRef]
- Timur, S.S.; Yüksel, S.; Akca, G.; Şenel, S. Localized Drug Delivery with Mono and Bilayered Mucoadhesive Films and Wafers for Oral Mucosal Infections. Int. J. Pharm. 2019, 559, 102–112. [Google Scholar] [CrossRef]
- Montenegro, L.; Parenti, C.; Turnaturi, R.; Pasquinucci, L. Resveratrol-Loaded Lipid Nanocarriers: Correlation between in Vitro Occlusion Factor and in Vivo Skin Hydrating Effect. Pharmaceutics 2017, 9, 58. [Google Scholar] [CrossRef] [Green Version]
- Venturini, C.G.; Bruinsmann, F.A.; Oliveira, C.P.; Contri, R.V.; Pohlmann, A.R.; Guterres, S.S. Vegetable Oil-Loaded Nanocapsules: Innovative Alternative for Incorporating Drugs for Parenteral Administration. J. Nanosci. Nanotechnol. 2016, 16, 1310–1320. [Google Scholar] [CrossRef]
- Hussain, Z.; Katas, H.; Cairul, M.; Mohd, I.; Kumulosasi, E.; Sahudin, S. Antidermatitic Perspective of Hydrocortisone as Chitosan Nanocarriers: An Ex Vivo and In Vivo Assessment Using an NC / Nga Mouse Model. J. Pharm. Sci. 2013, 102, 1063–1075. [Google Scholar] [CrossRef]
- Khelifi, I.; Hayouni, E.A.; Cazaux, S.; Ksouri, R.; Bouajila, J. Evaluation of in Vitro Biological Activities: Antioxidant; Anti-Inflammatory; Anti- Cholinesterase; Anti- Xanthine Oxidase, Anti-Superoxyde Dismutase, Anti-α-Glucosidase and Cytotoxic of 19 Bioflavonoids. Cell. Mol. Biol. 2020, 66, 9–19. [Google Scholar] [CrossRef]
- Kabashima, K.; Nomura, T. Revisiting Murine Models for Atopic Dermatitis and Psoriasis with Multipolar Cytokine Axes. Curr. Opin. Immunol. 2017, 48, 99–107. [Google Scholar] [CrossRef]
- Tang, L.; Li, X.L.; Deng, Z.X.; Xiao, Y.; Cheng, Y.H.; Li, J.; Ding, H. Conjugated Linoleic Acid Attenuates 2,4-Dinitrofluorobenzene-Induced Atopic Dermatitis in Mice through Dual Inhibition of COX-2/5-LOX and TLR4/NF-ΚB Signaling. J. Nutr. Biochem. 2020, 81, 108379. [Google Scholar] [CrossRef]
- Saini, S.; Pansare, M. New Insights and Treatments in Atopic Dermatitis. Immunol. Allergy Clin. N. Am. 2021, 41, 653–665. [Google Scholar] [CrossRef]
- Fan, P.; Yang, Y.; Liu, T.; Lu, X.; Huang, H.; Chen, L.; Kuang, Y. Anti-Atopic Effect of Viola Yedoensis Ethanol Extract against 2,4-Dinitrochlorobenzene-Induced Atopic Dermatitis-like Skin Dysfunction. J. Ethnopharmacol. 2021, 280, 114474. [Google Scholar] [CrossRef]
- Pelle, E.; Mammone, T.; Maes, D.; Frenkel, K. Keratinocytes Act as a Source of Reactive Oxygen Species by Transferring Hydrogen Peroxide to Melanocytes. J. Investig. Dermatol. 2005, 124, 793–797. [Google Scholar] [CrossRef]
- Rodriguez, K.J.; Wong, H.K.; Oddos, T.; Southall, M.; Frei, B.; Kaur, S. A Purified Feverfew Extract Protects from Oxidative Damage by Inducing DNA Repair in Skin Cells via a PI3-Kinase-Dependent Nrf2/ARE Pathway. J. Dermatol. Sci. 2013, 72, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Steullet, P.; Cabungcal, J.H.; Monin, A.; Dwir, D.; O’Donnell, P.; Cuenod, M.; Do, K.Q. Redox Dysregulation, Neuroinflammation, and NMDA Receptor Hypofunction: A “Central Hub” in Schizophrenia Pathophysiology? Schizophr. Res. 2016, 176, 41–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, W.; Wu, X.; Xu, X.; Wang, W.; Song, S.; Liang, K.; Yang, M.; Guo, L.; Zhao, Y.; Li, R. Coenzyme Q10 Suppresses TNF-α-Induced Inflammatory Reaction In Vitro and Attenuates Severity of Dermatitis in Mice. Inflammation 2016, 39, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Wink, D.A.; Hines, H.B.; Cheng, R.Y.S.; Switzer, C.H.; Flores-Santana, W.; Vitek, M.P.; Ridnour, L.A.; Colton, C.A. Nitric Oxide and Redox Mechanisms in the Immune Response. J. Leukoc. Biol. 2011, 89, 873–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barnes, L.; Kaya, G.; Rollason, V. Topical Corticosteroid-Induced Skin Atrophy: A Comprehensive Review. Drug Saf. 2015, 38, 493–509. [Google Scholar] [CrossRef] [PubMed]
- Slater, N.A.; Morrell, D.S. Systemic Therapy of Childhood Atopic Dermatitis. Clin. Dermatol. 2015, 33, 289–299. [Google Scholar] [CrossRef]
- Danby, S.G.; Draelos, Z.D.; Gold, L.F.S.; Cha, A.; Aikman, L.; Sanders, P.; Wu-linhares, D.; Cork, M.J.; Danby, S.G.; Draelos, Z.D.; et al. Vehicles for Atopic Dermatitis Therapies: More than Just a Placebo. J. Dermatolog. Treat. 2022, 33, 685–698. [Google Scholar] [CrossRef]
- Mcdaniel, M.L.; Kwon, G.; Hill, J.R.; Marshall, C.A.; Corbett, J.A. Cytokines and Nitric Oxide in Islet Inflammation and Diabetes (43950D). Exp. Biol. Med. 1996, 211, 24–32. [Google Scholar] [CrossRef]
- Winterbourn, C.C. Revisiting the Reactions of Superoxide with Glutathione and Other Thiols. Arch. Biochem. Biophys. 2016, 595, 68–71. [Google Scholar] [CrossRef]
- Hussain, Z.; Katas, H.; Cairul, M.; Mohd, I.; Kumolosasi, E.; Buang, F.; Sahudin, S. Self-Assembled Polymeric Nanoparticles for Percutaneous Co-Delivery of Hydrocortisone/Hydroxytyrosol: An Ex Vivo and In Vivo Study Using an NC/Nga Mouse Model. Int. J. Pharm. 2013, 444, 109–119. [Google Scholar] [CrossRef]

| BF NC SB | BF NC B | BF Vehicle | |
|---|---|---|---|
| Drug content homogeneity (µg/cm2) | 440.61 ± 5.21 | - | - |
| Thickness (µm) | 43 ± 7 | 42 ± 5 | 40 ± 5 |
| Size (nm) | 117 ± 11 | 137 ± 15 | 514 ± 143 |
| Polydispersity index | 0.28 ± 0.05 | 0.24 ± 0.05 | 0.47 ± 0.11 |
| Swelling index (%) | 106.95 ± 2.56 * | 101.02 ± 6.45 * | 134.42 ± 4.78 |
| Moisture (%) | 13.89 ± 2.01 | 12.83 ± 1.07 | 14.83 ± 2.64 |
| Tensile strength (MPa) | 1.09 ± 0.03 * | 1.13 ± 0.09 * | 0.51 ± 0.05 |
| Elongation (%) | 4.93 ± 0.45 * | 4.61 ± 0.18 * | 7.69 ± 0.15 |
| Young’s modulus (MPa) | 27.25± 5.95 * | 24.25 ± 6.57 * | 7.25 ± 5.95 |
| Formulation | Occlusion Factor (%) | ||
|---|---|---|---|
| 6 h | 24 h | 48 h | |
| BF Vehicle | 20.18 ± 3.66 ** | 28.18 ± 2.05 ** | 29.45 ± 1.47 ** |
| BF NC SB | 51.90 ± 2.01 | 50.16 ± 1.84 | 55.78 ± 2.35 |
| BF NC B | 49.50 ± 4.31 | 52.30 ± 6.09 | 50.26 ± 2.45 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gehrcke, M.; Martins, C.C.; de Bastos Brum, T.; da Rosa, L.S.; Luchese, C.; Wilhelm, E.A.; Soares, F.Z.M.; Cruz, L. Novel Pullulan/Gellan Gum Bilayer Film as a Vehicle for Silibinin-Loaded Nanocapsules in the Topical Treatment of Atopic Dermatitis. Pharmaceutics 2022, 14, 2352. https://doi.org/10.3390/pharmaceutics14112352
Gehrcke M, Martins CC, de Bastos Brum T, da Rosa LS, Luchese C, Wilhelm EA, Soares FZM, Cruz L. Novel Pullulan/Gellan Gum Bilayer Film as a Vehicle for Silibinin-Loaded Nanocapsules in the Topical Treatment of Atopic Dermatitis. Pharmaceutics. 2022; 14(11):2352. https://doi.org/10.3390/pharmaceutics14112352
Chicago/Turabian StyleGehrcke, Mailine, Carolina Cristóvão Martins, Taíne de Bastos Brum, Lucas Saldanha da Rosa, Cristiane Luchese, Ethel Antunes Wilhelm, Fabio Zovico Maxnuck Soares, and Letícia Cruz. 2022. "Novel Pullulan/Gellan Gum Bilayer Film as a Vehicle for Silibinin-Loaded Nanocapsules in the Topical Treatment of Atopic Dermatitis" Pharmaceutics 14, no. 11: 2352. https://doi.org/10.3390/pharmaceutics14112352
APA StyleGehrcke, M., Martins, C. C., de Bastos Brum, T., da Rosa, L. S., Luchese, C., Wilhelm, E. A., Soares, F. Z. M., & Cruz, L. (2022). Novel Pullulan/Gellan Gum Bilayer Film as a Vehicle for Silibinin-Loaded Nanocapsules in the Topical Treatment of Atopic Dermatitis. Pharmaceutics, 14(11), 2352. https://doi.org/10.3390/pharmaceutics14112352









