Biosimilars in Oncology: Latest Trends and Regulatory Status
Abstract
:1. Introduction
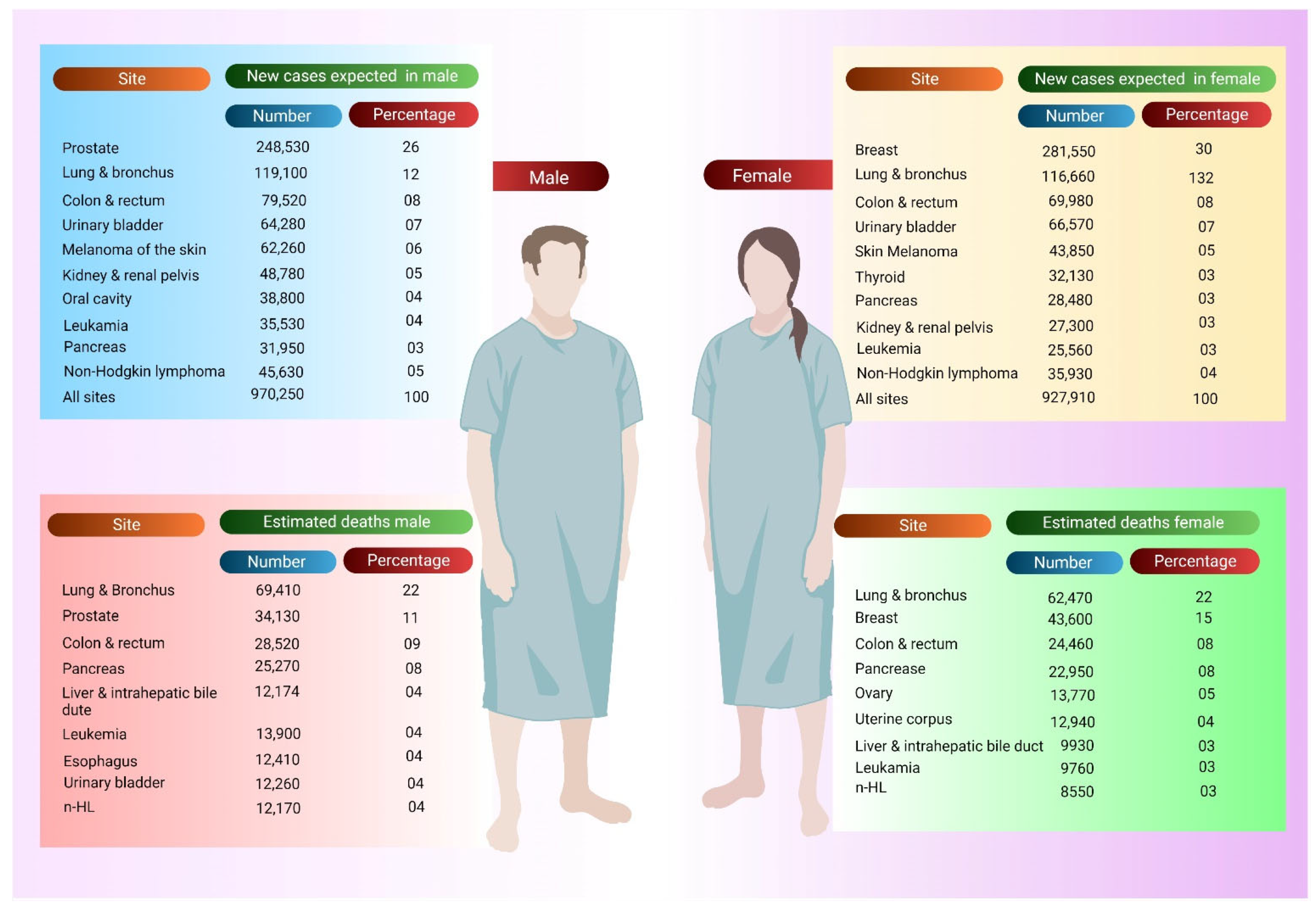
2. Healthcare Burden of Cancer
2.1. Incidence and Prevalence
2.2. Risk Factors
2.3. Treatment
3. Pharmacoeconomics of Biosimilars
4. Current Impact of Biosimilars in Cancer Care
5. Current Biosimilars Used in Oncology Globally
6. Biosimilars in Oncology Approved by Various Regulatory Authorities
6.1. Epoetin
6.2. Filgrastim and Pegfilgrastim
6.3. Rituximab
6.4. Trastuzumab
6.5. Bevacizumab
6.6. Recombinant Human Interferon-α-2α




7. Regulatory Guidelines Associated with Biosimilars Globally
7.1. Europe
7.2. World Health Organization (WHO) Guidelines
7.3. USA
7.4. Australia
7.5. Canada
7.6. Japan
7.7. South Korea
7.8. India
7.9. Other Countries
8. Adverse Events Associated with the Biosimilars
9. Traceability of Biosimilars in the Post-Marketing Phase
10. Conclusions
11. Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sandow, J.; Landgraf, W.; Becker, R.; Seipke, G. Equivalent Recombinant Human Insulin Preparations and their Place in Therapy. Eur. Endocrinol. 2015, 11, 10–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mellstedt, H. Clinical considerations for biosimilar antibodies. EJC Suppl. 2013, 11, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Isaacs, J.D.; Cutolo, M.; Keystone, E.C.; Park, W.; Braun, J. Biosimilars in immune-mediated inflammatory diseases: Initial lessons from the first approved biosimilar anti-tumour necrosis factor monoclonal antibody. J. Intern. Med. 2016, 279, 41–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mestre-Ferrandiz, J.; Towse, A.; Berdud, M. Biosimilars: How Can Payers Get Long-Term Savings? Pharmacoeconomics 2016, 34, 609–616. [Google Scholar] [CrossRef] [Green Version]
- Kaida, Y.F.; Deshpande, K.; Saran, T.; Vyas, D. Biosimilars: Review of current applications, obstacles, and their future in medicine. World J. Clin. Cases 2018, 6, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Janjigian, Y.Y.; Bissig, M.; Curigliano, G.; Coppola, J.; Latymer, M. Talking to patients about Biosimilars. Future Oncol. 2018, 14, 2403–2414. [Google Scholar] [CrossRef]
- Patel, D.; Gillis, C.; Naggar, J.; Mistry, A.; Mantzoros, C.S. The rise of Biosimilars: How they got here and where they are going. Metabolism 2017, 75, 45–53. [Google Scholar] [CrossRef]
- The Global Economic Growth of Cancer: American Cancer Society. Available online: http://phrma-docs.phrma.org/sites/default/files/pdf/08-17-2010_economic_impact_study.pdf (accessed on 20 September 2022).
- World Health Organization. Early Cancer Diagnosis Saves Lives, Cuts Treatment Costs. Available online: https://www.who.int/news/item/03-02-2017-early-cancer-diagnosis-saves-lives-cuts-treatment-costs (accessed on 20 September 2022).
- List of Licensed Biological Products with (1) Reference Product Exclusivity and (2) Biosimilarity or Interchangeability Evaluations to Date: FDA. Available online: https://www.fda.gov/media/89589/download (accessed on 18 September 2022).
- Heinemann, L.; Khatami, H.; McKinnon, R.; Home, P. An Overview of Current Regulatory Requirements for Approval of Biosimilar Insulins. Diabetes Technol. Ther. 2015, 17, 510–526. [Google Scholar] [CrossRef] [Green Version]
- 10 Years of Biosimilar Medicines: Transforming Healthcare: Medicines for Europe. Available online: https://www.medicinesforeurope.com/news/10-years-of-biosimilar-medicines-transforming-healthcare/ (accessed on 20 September 2022).
- Cook, J.W.; McGrath, M.K.; Dixon, M.D.; Switchenko, J.M.; Harvey, R.D.; Pentz, R.D. Academic oncology clinicians’ understanding of Biosimilars and information needed before prescribing. Ther. Adv. Med. Oncol. 2019, 11, 1758835918818335. [Google Scholar] [CrossRef]
- Rugo, H.S.; Rifkin, R.M.; Declerck, P.; Bair, A.H.; Morgan, G. Demystifying Biosimilars: Development, regulation and clinical use. Future Oncol. 2019, 15, 777–790. [Google Scholar] [CrossRef]
- Farfan-Portet, M.I.; Gerkens, S.; Lepage-Nefkens, I.; Vinck, I.; Hulstaert, F. Are Biosimilars the next tool to guarantee cost-containment for pharmaceutical expenditures? Eur. J. Health Econ. 2014, 15, 223–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leonard, E.; Wascovich, M.; Oskouei, S.; Gurz, P.; Carpenter, D. Factors affecting health care provider knowledge and acceptance of biosimilar medicines: A systematic review. J. Manag. Care Spec. Pharm. 2019, 25, 102–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2021. CA A Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 20 September 2022).
- Liu, Y. Utilizing oncology Biosimilars to minimize the economic burden associated with cancer treatment: Managed care considerations. Am. J. Manag. Care 2021, 27 (Suppl. 14). [Google Scholar] [CrossRef]
- Kvien, T.K.; Patel, K.; Strand, V. The cost savings of biosimilars can help increase patient access and lift the financial burden of health care systems. Semin Arthritis Rheum. 2022, 52, 151939. [Google Scholar] [CrossRef]
- IQVIA Institute. Biosimilars in the United States 2020–2024. Available online: https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/iqvia-institute-Biosimilars-in-the-united-states.pdf (accessed on 15 September 2022).
- Generics And Biosimilar Initiative. The Cost-Effectiveness of Biosimilars. Available online: https://gabionline.net/Biosimilars/research/The-cost-effectiveness-of-Biosimilars (accessed on 2 September 2022).
- Huang, H.Y.; Liu, C.C.; Yu, Y.; Wang, L.; Wu, D.W.; Guo, L.W.; Wang, S.H.; Fang, H.; Bai, Y.; Fang, Y.; et al. Pharmacoeconomic evaluation of cancer Biosimilars worldwide: A systematic review. Front. Pharmacol. 2020, 11, 1749. [Google Scholar] [CrossRef]
- Nahleh, Z.; Lyman, G.H.; Schilsky, R.L.; Peterson, D.E.; Tagawa, S.T.; Chavez-MacGregor, M.; Rumble, R.B.; Gupta, S. Use of Biosimilar Medications in Oncology. JCO Oncol. Pract. 2022, 18, 177–186. [Google Scholar] [CrossRef]
- Cornes, P.; Aapro, M. The impact of Biosimilars in supportive care in cancer. Eur. Oncol. Haematol. 2018, 14, 20–32. [Google Scholar] [CrossRef]
- Bhardwaja, B.; Klocke, S.; Ekinci, E.; Jackson, A.; Kono, S.; Olson, K.L. Switching from Biologic to Biosimilar Products: Insight from an Integrated Health Care System. BioDrugs 2022, 36, 1–11. [Google Scholar] [CrossRef]
- Patel, K.B.; Arantes, L.H.; Tang, W.Y.; Fung, S. The role of Biosimilars in value-based oncology care. Cancer Manag. Res. 2018, 10, 4591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulcahy, A.; Buttorff, C.; Finegold, K.; El-Kilani, Z.; Oliver, J.F.; Murphy, S.; Jessup, A. Projected US savings from biosimilars, 2021–2025. Am. J. Manag. Care 2022, 28, 329–335. [Google Scholar] [PubMed]
- Aapro, M.; Krendyukov, A.; Schiestl, M.; Gascon, P. Epoetin Biosimilars in the Treatment of Chemotherapy-Induced Anemia: 10 Years’ Experience Gained. BioDrugs: Clin. Immunother. Biopharm. Gene Ther. 2018, 32, 129–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ludwig, H.; Bokemeyer, C.; Aapro, M.; Boccadoro, M.; Gascon, P.; Denhaerynck, K. Chemotherapy-induced neutropenia/febrile neutropenia prophylaxis with biosimilar filgrastim in solid tumors versus hematological malignancies: MONITOR-GCSF study. Future Oncol. 2019, 15, 897–907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karalis, V.D. From Bioequivalence to Biosimilarity: The Rise of a Novel Regulatory Framework. Drug Res. 2016, 66, 1–6. [Google Scholar] [CrossRef]
- Declerck, P.; Bakalos, G.; Zintzaras, E.; Barton, B.; Schreitmuller, T. Monoclonal Antibody Biosimilars in Oncology: Critical Appraisal of Available Data on Switching. Clin. Ther. 2018, 40, 798–809.e2. [Google Scholar] [CrossRef]
- Matti, A.M. Biosimilars in oncology. Curr. Future Perspect. 2013, 2, 91–93. [Google Scholar] [CrossRef] [Green Version]
- Nabhan, C.; Valley, A.; Feinberg, B.A. Barriers to Oncology Biosimilars Uptake in the United States. Oncologist 2018, 23, 1261–1265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abseamed, EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/abseamed (accessed on 20 September 2022).
- Binocrit EMA. 2018. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/binocrit (accessed on 20 September 2022).
- Epoetin-α Hexal EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/epoetin-alfa-hexal#:~:text=Epoetin%20Alfa%20Hexal%20is%20used,of%20the%20natural%20hormone%20erythropoietin (accessed on 20 September 2022).
- Retacrit EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/retacrit (accessed on 20 September 2022).
- Silapo EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/silapo (accessed on 20 September 2022).
- Biosimilars Approved in Australia: Generics and Biosimilars Initiative (GaBI). Available online: https://www.gabionline.net/Biosimilars/General/Biosimilars-approved-in-Australia (accessed on 20 September 2022).
- Retacrit Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/125545s000lbl.pdf (accessed on 20 September 2022).
- Ratiograstim EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/ratiograstim (accessed on 20 September 2022).
- Tevagrastim EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/tevagrastim (accessed on 15 September 2022).
- Zarzio EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/zarzio (accessed on 20 September 2022).
- Filgrastim Hexal EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/filgrastim-hexal (accessed on 20 September 2022).
- Nivestim EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/nivestim (accessed on 20 September 2022).
- Grastofil EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/grastofil (accessed on 20 September 2022).
- Accofil EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/accofil (accessed on 20 September 2022).
- Zarxio Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/125553lbl.pdf (accessed on 20 September 2022).
- Biosimilars Approved in Canada: CANADA. Available online: https://www.gabionline.net/Biosimilars/General/Biosimilars-approved-in-Canada (accessed on 20 September 2022).
- Nivestym Label FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761080s000lbl.pdf (accessed on 20 September 2022).
- Udenyca EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/udenyca (accessed on 20 September 2022).
- Fulphila EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/fulphila-0 (accessed on 20 September 2022).
- Pelmeg EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/pelmeg (accessed on 20 September 2022).
- Ziextenzo EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/ziextenzo (accessed on 20 September 2022).
- Ogivri EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/ogivri (accessed on 20 September 2022).
- Fulphila Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761075s000lbl.pdf (accessed on 20 September 2022).
- Udenyca Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761039s000lbl.pdf (accessed on 20 September 2022).
- Nyvepria Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/761111lbl.pdf (accessed on 20 September 2022).
- Truxima EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/truxima (accessed on 20 September 2022).
- Riximyo EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/riximyo (accessed on 20 September 2022).
- Rixathon EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/rixathon (accessed on 20 September 2022).
- Ritemvia EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/ritemvia (accessed on 20 September 2022).
- Blitzima EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/blitzima (accessed on 20 September 2022).
- Truxima Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761088s000lbl.pdf (accessed on 20 September 2022).
- Ruxience Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761103s000lbl.pdf (accessed on 20 September 2022).
- Ontruzant EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/ontruzant (accessed on 20 September 2022).
- Ogivri Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761074s000lbl.pdf (accessed on 20 September 2022).
- Herzuma EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/herzuma (accessed on 20 September 2022).
- Kanjinti EMA: EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/kanjinti (accessed on 20 September 2022).
- Trazimera EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/trazimera (accessed on 20 September 2022).
- Herzuma Label, FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761091s000lbl.pdf (accessed on 20 September 2022).
- Ontruzant Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761100s000lbl.pdf (accessed on 20 September 2022).
- Trazimera Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761081s000lbl.pdf (accessed on 20 September 2022).
- Kanjinti Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761073s000lbl.pdf (accessed on 20 September 2022).
- Mvasi Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/761028s000lbl.pdf (accessed on 20 September 2022).
- Mvasi EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/mvasi (accessed on 20 September 2022).
- Zirabev Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761099s000lbl.pdf (accessed on 20 September 2022).
- Jelkmann, W. Physiology and pharmacology of erythropoietin. Transfus Med. Hemother. 2013, 40, 302–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tonelli, M.; Hemmelgarn, B.; Reiman, T.; Manns, B.; Reaume, M.N.; Lloyd, A. Benefits and harms of erythropoiesis-stimulating agents for anemia related to cancer: A meta-analysis. CMAJ. 2009, 180, E62–E71. [Google Scholar] [CrossRef]
- Xirou, V.; Gkiozos, I.; Grapsa, D.; Dimitroulis, I.; Syrigos, K. P2.01-039 Erythropoiesis-Stimulating Agents for Chemotherapy-Induced Anaemia in Lung Cancer: Efficacy, Toxicity and Effect on Survival. J. Thorac. Oncol. 2017, 12, 2083. [Google Scholar] [CrossRef] [Green Version]
- Irrera, N.; Bitto, A.; Pizzino, G.; Vaccaro, M.; Squadrito, F.; Galeano, M.; d’Alcontres, F.S.; d’Alcontres, F.S.; Buemi, M.; Minutoli, L.; et al. Epoetin Alpha and Epoetin Zeta: A Comparative Study on Stimulation of Angiogenesis and Wound Repair in an Experimental Model of Burn Injury. Biomed. Res. Int. 2015, 2015, 968927. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aapro, M.; Bokemeyer, C.; Ludwig, H.; Gascon, P.; Boccadoro, M.; Denhaerynck, K.; Gorray, M.; Krendyukov, A.; MacDonald, K.; Abraham, I.; et al. Chemotherapy-induced (febrile) neutropenia prophylaxis with biosimilar filgrastim in elderly versus non-elderly cancer patients: Patterns, outcomes, and determinants (MONITOR-GCSF study). J. Geriatr. Oncol. 2017, 8, 86–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenwald, M.; Tesser, J.; Sewell, K.L. Biosimilars Have Arrived: Rituximab. Arthritis 2018, 2018, 3762864. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- FDA Approves First Biosimilar for Treatment of Adult Patients with Non-Hodgkin’s Lymphoma: FDA. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-first-biosimilar-treatment-adult-patients-non-hodgkins-lymphoma#:~:text=The%20U.S.%20Food%20and%20Drug,or%20in%20combination%20with%20chemotherapy (accessed on 20 September 2022).
- Pimentel, F.F.; Morgan, G.; Tiezzi, D.G.; de Andrade, J.M. Development of New Formulations of Biologics: Expectations, Immunogenicity, and Safety for Subcutaneous Trastuzumab. Pharmaceut. Med. 2018, 32, 319–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajasekaran, N.; Chester, C.; Yonezawa, A.; Zhao, X.; Kohrt, H.E. Enhancement of antibody-dependent cell mediated cytotoxicity: A new era in cancer treatment. Immunotargets Ther. 2015, 4, 91–100. [Google Scholar] [PubMed] [Green Version]
- Grapsa, D.; Syrigos, K.; Saif, M.W. Bevacizumab in combination with fluoropyrimidine-irinotecan- or fluoropyrimidine-oxaliplatin-based chemotherapy for first-line and maintenance treatment of metastatic colorectal cancer. Expert Rev. Anticancer Ther. 2015, 15, 1267–1281. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Huang, Z.; Mao, W. Bevacizumab treatment for advanced non-small cell lung cancer: A case report. Oncol Lett. 2013, 6, 1779–1783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casak, S.J.; Lemery, S.J.; Chung, J.; Fuchs, C.; Schrieber, S.J.; Chow, E.C.Y.; Yuan, W.; Rodriguez, L.; Gwise, T.; Rowzee, A.; et al. FDA’s Approval of the First Biosimilar to Bevacizumab. Clin. Cancer Res. 2018, 24, 4365–4370. [Google Scholar] [CrossRef] [Green Version]
- Smeeding, J.; Malone, D.C.; Ramchandani, M.; Stolshek, B.; Green, L.; Schneider, P. Biosimilars: Considerations for Payers. P T Peer-Rev. J. Formul. Manag. 2019, 44, 54–63. [Google Scholar]
- Abseamed EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/overview/abseamed-epar-medicine-overview_en.pdf (accessed on 20 September 2022).
- EMA. Binocrit EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/binocrit-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Amsparity EMA SmPC. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/amsparity (accessed on 20 September 2022).
- EMA. Retacrit EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/retacrit-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Silapo EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/silapo-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Ratiograstim EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/ratiograstim-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Tevagrastim EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/tevagrastim-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Zarzio EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/zarzio-epar-product-information_en.pdf (accessed on 20 September 2022).
- Niederwieser, D.; Schmitz, S. Biosimilar agents in oncology/haematology: From approval to practice. Eur. J. Haematol. 2011, 86, 277–288. [Google Scholar] [CrossRef] [PubMed]
- EMA. Grastofil EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/grastofil-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Accofil EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/accofil-epar-product-information_en.pdf (accessed on 20 September 2022).
- Pelgraz EMA: EMA. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/pelgraz (accessed on 20 September 2022).
- EMA. Udenyca EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/udenyca-epar-product-information_en.pdf (accessed on 14 September 2022).
- EMA. Fulphila EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/fulphila-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Ziextenzo EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/ziextenzo-epar-product-information_en.pdf (accessed on 1 September 2022).
- EMA. Ogivri EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/ogivri-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Truxima EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/truxima-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Rixathon EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/rixathon-epar-product-information_en.pdf (accessed on 20 September 2022).
- Riximyo EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/riximyo-epar-product-information_en.pdf (accessed on 5 November 2020).
- EMA. Ritemvia EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/ritemvia-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Blitzima EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/blitzima-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Ontruzant EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/ontruzant-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Herzuma EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/herzuma-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Kanjinti EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/kanjinti-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Trazimera EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/trazimera-epar-product-information_en.pdf (accessed on 20 September 2022).
- EMA. Mvasi EMA SmPC: EMA. Available online: https://www.ema.europa.eu/en/documents/product-information/mvasi-epar-product-information_en.pdf (accessed on 20 September 2022).
- Ingrasciotta, Y.; Cutroneo, P.M.; Marciano, I.; Giezen, T.; Atzeni, F.; Trifiro, G. Safety of Biologics, Including Biosimilars: Perspectives on Current Status and Future Direction. Drug Saf. 2018, 41, 1013–1022. [Google Scholar] [CrossRef] [PubMed]
- Zuniga, L.; Calvo, B. Biosimilars: Pharmacovigilance and risk management. Pharmacoepidemiol. Drug Saf. 2010, 19, 661–669. [Google Scholar] [CrossRef] [PubMed]
- Cutroneo, P.M.; Isgro, V.; Russo, A.; Ientile, V.; Sottosanti, L.; Pimpinella, G.; Conforti, A.; Moretti, U.; Caputi, A.P.; Trifirò, G. Safety profile of biological medicines as compared with non-biologicals: An analysis of the italian spontaneous reporting system database. Drug Saf. 2014, 37, 961–970. [Google Scholar] [CrossRef]
- Renwick, M.; Smolina, K.; Gladstone, E.J.; Weymann, D.; Morgan, S.G. Postmarket policy considerations for biosimilar oncology drugs. Lancet Oncol. 2016, 17, e31–e38. [Google Scholar] [CrossRef]
- Ahmed, I.; Kaspar, B.; Sharma, U. Biosimilars: Impact of biologic product life cycle and European experience on the regulatory trajectory in the United States. Clin. Ther. 2012, 34, 400–419. [Google Scholar] [CrossRef]
- Azevedo, V.F.; Sandorff, E.; Siemak, B.; Halbert, R.J. Potential Regulatory and Commercial Environment for Biosimilars in Latin America. Value Health Reg. Issues 2012, 1, 228–234. [Google Scholar] [CrossRef]
- FDA. Ziextenzo Label: FDA. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761045lbl.pdf (accessed on 20 September 2022).
- Truxima Australia. Available online: https://www.healthdirect.gov.au/medicines/brand/amt,1123851000168105/truxima (accessed on 20 September 2022).
- Herzuma Australia. Available online: https://www.healthdirect.gov.au/medicines/brand/amt,1402181000168107/herzuma (accessed on 20 September 2022).
- Ogivri Australia. Available online: https://www.healthdirect.gov.au/medicines/brand/amt,1265391000168104/ogivri (accessed on 20 September 2022).
- Kanjinti Australia. Available online: https://www.healthdirect.gov.au/medicines/brand/amt,1417821000168103/kanjinti (accessed on 20 September 2022).
- Ontruzant Australia. Available online: https://www.healthdirect.gov.au/medicines/brand/amt,1252911000168105/ontruzant (accessed on 20 September 2022).
- Trazimera Australia. Available online: https://www.healthdirect.gov.au/medicines/brand/amt,1459271000168102/trazimera (accessed on 20 September 2022).
- Canada H. Grastofil Canada Monograph: Health Canada. Available online: https://pdf.hres.ca/dpd_pm/00043738.PDF (accessed on 20 September 2022).
- Malhotra, H. Biosimilars and non-innovator biotherapeutics in India: An overview of the current situation. Biol. J. Int. Assoc. Biol. Stand. 2011, 39, 321–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canada H. Riximyo Canada Monograph: Health Canada. Available online: https://www.sandoz.ca/sites/www.sandoz.ca/files/Riximyo-Product-Monograph.pdf (accessed on 20 September 2022).
- Canada H. Ruxience Canada Monograph: Health Canada. Available online: https://www.pfizer.ca/sites/default/files/202007/RUXIENCE_PM_239138_8July2020_EN.pdf (accessed on 20 September 2022).
- Canada H. Herzuma Canada Monograph: Health Canada. Available online: https://pdf.hres.ca/dpd_pm/00058447.PDF (accessed on 20 September 2022).
- Kanjinti Canada Monograph. Available online: https://pdf.hres.ca/dpd_pm/00055185.PDF (accessed on 20 September 2022).
- Tsiftsoglou, A.S.; Ruiz, S.; Schneider, C.K. Development and regulation of Biosimilars: Current status and future challenges. BioDrugs Clin. Immunother. Biopharm. Gene Ther. 2013, 27, 203–211. [Google Scholar] [CrossRef]
- Bennett, C.L.; Chen, B.; Hermanson, T.; Wyatt, M.D.; Schulz, R.M.; Georgantopoulos, P.; Kessler, S.; Raisch, D.W.; Qureshi, Z.P.; Lu, Z.K. Regulatory and clinical considerations for biosimilar oncology drugs. Lancet Oncol. 2014, 15, e594–e605. [Google Scholar] [CrossRef] [Green Version]
- Minghetti, P.; Rocco, P.; Schellekens, H. The constrained prescription, interchangeability and substitution of Biosimilars. Nat. Biotechnol. 2015, 33, 688–689. [Google Scholar] [CrossRef] [PubMed]
- EMA. Multidisciplinary: Biosimilar. EMA. Available online: https://www.ema.europa.eu/en/human-regulatory/research-development/scientific-guidelines/multidisciplinary/multidisciplinary-biosimilar (accessed on 20 September 2022).
- EMA. Guideline on Similar Biological Medicinal Products Containing Recombinant Granulocyte-Colony Stimulating Factor (rG-CSF); EMA: Amsterdam, The Netherlands, 2018. [Google Scholar]
- WHO. Available online: https://www.who.int/medicines/access/biotherapeutics/FINAL_Report-improving-access-to-and-use-of-biotherapeutics_October2017.pdf (accessed on 20 September 2022).
- Quality Considerations in Demonstrating Biosimilarity of a Therapeutic Protein Product to a Reference Product Guidance for Industry. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/quality-considerations-demonstrating-biosimilarity-therapeutic-protein-product-reference-product (accessed on 20 September 2022).
- Scientific Considerations in Demonstrating Biosimilarity to a Reference Product: FDA. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/scientific-considerations-demonstrating-biosimilarity-reference-product (accessed on 20 September 2022).
- Joshi, D.; Sharma, I.; Gupta, S.; Singh, T.G.; Dhiman, S.; Prashar, A.; Gulati, M.; Kumar, B.; Vishwas, S.; Chellappan, D.K.; et al. A global comparison of implementation and effectiveness of materiovigilance program: Overview of regulations. Environ. Sci. Pollut. Res. Int. 2021, 28, 59608–59629. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, T.; Arato, T. Quality, safety and efficacy of follow-on biologics in Japan. Biol. J. Int. Assoc. Biol. Stand. 2011, 39, 328–332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.J.; Han, E.; Kim, H. Comparison of Utilization Trends between Biosimilars and Generics: Lessons from the Nationwide Claims Data in South Korea. Appl. Health Econ. Health Policy 2020, 18, 557–566. [Google Scholar] [CrossRef] [PubMed]
- Imran, M.; Najmi, A.K.; Rashid, M.F.; Tabrez, S.; Shah, M.A. Clinical research regulation in India-history, development, initiatives, challenges and controversies: Still long way to go. J. Pharm. Bioallied Sci. 2013, 5, 2–9. [Google Scholar] [CrossRef]
- EMA. Human Regulatory. Available online: https://www.ema.europa.eu/en/human-regulatory/overview/pharmacovigilance-overview (accessed on 23 December 2020).
- Information and Submission Requirements for Biosimilar Biologic Drugs (2010, revised 2016). Available online: https://www.google.com/search?q=canada+pharmacovigilance&rlz=1C1CHBF_enIN916IN916&oq=canada+pharmacovigila&aqs=chrome.2.0i457j69i57j0j0i22i30l7.27142j0j15&sourceid=chrome&ie=UTF-8 (accessed on 26 October 2022).
- Labeling for Biosimilar Products; Guidance for Industry (2016). Available online: https://www.fda.gov/media/96894/download (accessed on 25 December 2020).
- Pharmacovigilance Responsibilities of Medicine Sponsors: Australian Recommendations and Requirements. Available online: https://www.nps.org.au/australian-prescriber/articles/pharmacovigilance-and-expedited-drug-approvals#:~:text=Pharmacovigilance%20is%20the%20detection%20and,suspicious%20of%20an%20adverse%20event (accessed on 6 September 2022).
- Shin, J.Y.; Jung, S.Y.; Ahn, S.H.; Lee, S.H.; Kim, S.J.; Seong, J.M.; Chung, S.Y.; Park, B.J. New initiatives for pharmacovigilance in South Korea: Introducing the Korea Institute of Drug Safety and Risk Management (KIDS). Pharmacoepidemiol. Drug Saf. 2014, 23, 1115–1122. [Google Scholar] [CrossRef] [PubMed]
- Halimi, V.; Daci, A.; Ancevska Netkovska, K.; Suturkova, L.; Babar, Z.U.; Grozdanova, A. Clinical and Regulatory Concerns of Biosimilars: A Review of Literature. Int. J. Environ. Res. Public Health 2020, 17, 5800. [Google Scholar] [CrossRef]
- Antitrust and the Biopharmaceutical Industry: Lessons from Hatch-Waxman and an Early Evaluation of the Biologics Price Competition and Innovation Act of 2009. Available online: https://core.ac.uk/download/pdf/51081943.pdf (accessed on 6 October 2022).
- Schellekens, H.; Smolen, J.S.; Dicato, M.; Rifkin, R.M. Safety and efficacy of Biosimilars in oncology. Lancet Oncol. 2016, 17, e502–e509. [Google Scholar] [CrossRef]
- Kooijman, M.; van Meer, P.J.; Moors, E.H.; Schellekens, H. Thirty years of preclinical safety evaluation of biopharmaceuticals: Did scientific progress lead to appropriate regulatory guidance? Expert Opin. Drug Saf. 2012, 11, 797–801. [Google Scholar] [CrossRef] [Green Version]
- Liu, P.M.; Zou, L.; Sadhu, C.; Shen, W.D.; Nock, S. Comparative immunogenicity assessment: A critical consideration for biosimilar development. Bioanalysis 2015, 7, 373–381. [Google Scholar] [CrossRef]
- Ben-Horin, S.; Heap, G.A.; Ahmad, T.; Kim, H.; Kwon, T.; Chowers, Y. The immunogenicity of biosimilar infliximab: Can we extrapolate the data across indications? Expert Rev. Gastroenterol. Hepatol. 2015, 9 (Suppl. 1), 27–34. [Google Scholar] [CrossRef] [PubMed]
- Ben-Horin, S.; Yavzori, M.; Benhar, I.; Fudim, E.; Picard, O.; Ungar, B.; Lee, S.; Kim, S.; Eliakim, R.; Chowers, Y. Cross-immunogenicity: Antibodies to infliximab in Remicade-treated patients with IBD similarly recognise the biosimilar Remsima. Gut 2016, 65, 1132–1138. [Google Scholar] [CrossRef]
- Bennett, C.L.; Luminari, S.; Nissenson, A.R.; Tallman, M.S.; Klinge, S.A.; McWilliams, N.; McKoy, J.M.; Kim, B.; Lyons, E.A.; Trifilio, S.M.; et al. Pure red-cell aplasia and epoetin therapy. N. Engl. J. Med. 2004, 351, 1403–1408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, W.; Yoo, D.H.; Miranda, P.; Brzosko, M.; Wiland, P.; Gutierrez-Urena, S.; Mikazane, H.; Lee, Y.A.; Smiyan, S.; Lim, M.J.; et al. Efficacy and safety of switching from reference infliximab to CT-P13 compared with maintenance of CT-P13 in ankylosing spondylitis: 102-week data from the PLANETAS extension study. Ann. Rheum. Dis. 2017, 76, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Yoo, D.H.; Prodanovic, N.; Jaworski, J.; Miranda, P.; Ramiterre, E.; Lanzon, A.; Baranauskaite, A.; Wiland, P.; Abud-Mendoza, C.; Oparanov, B.; et al. Efficacy and safety of CT-P13 (biosimilar infliximab) in patients with rheumatoid arthritis: Comparison between switching from reference infliximab to CT-P13 and continuing CT-P13 in the PLANETRA extension study. Ann. Rheum. Dis. 2017, 76, 355–363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papp, K.; Bachelez, H.; Costanzo, A.; Foley, P.; Gooderham, M.; Kaur, P.; Narbutt, J.; Philipp, S.; Spelman, L.; Weglowska, J.; et al. Clinical similarity of biosimilar ABP 501 to adalimumab in the treatment of patients with moderate to severe plaque psoriasis: A randomized, double-blind, multicenter, phase III study. J. Am. Acad. Dermatol. 2017, 76, 1093–1102. [Google Scholar] [CrossRef] [Green Version]
- Smolen, J.S.; Choe, J.Y.; Prodanovic, N.; Niebrzydowski, J.; Staykov, I.; Dokoupilova, E.; Baranauskaite, A.; Yatsyshyn, R.; Mekic, M.; Porawska, W.; et al. Safety, immunogenicity and efficacy after switching from reference infliximab to biosimilar SB2 compared with continuing reference infliximab and SB2 in patients with rheumatoid arthritis: Results of a randomised, double-blind, phase III transition study. Ann. Rheum. Dis. 2018, 77, 234–240. [Google Scholar] [CrossRef] [Green Version]
- Blackwell, K.; Semiglazov, V.; Krasnozhon, D.; Davidenko, I.; Nelyubina, L.; Nakov, R.; Stiegler, G.; Singh, P.; Schwebig, A.; Kramer, S.; et al. Comparison of EP2006, a filgrastim biosimilar, to the reference: A phase III, randomized, double-blind clinical study in the prevention of severe neutropenia in patients with breast cancer receiving myelosuppressive chemotherapy. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2015, 26, 1948–1953. [Google Scholar] [CrossRef]
- Ventola, C.L. Biosimilars: Part 1: Proposed regulatory criteria for FDA approval. P T Peer-Rev. J. Formul. Manag. 2013, 38, 270–287. [Google Scholar]
- Patel, P.K.; King, C.R.; Feldman, S.R. Biologics and Biosimilars. J. Dermatol. Treat. 2015, 26, 299–302. [Google Scholar] [CrossRef]
- O’Callaghan, J.; Griffin, B.T.; Morris, J.M.; Bermingham, M. Knowledge of Adverse Drug Reaction Reporting and the Pharmacovigilance of Biological Medicines: A Survey of Healthcare Professionals in Ireland. BioDrugs Clin. Immunother. Biopharm. Gene Ther. 2018, 32, 267–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein, K.; Hazell, L.; Stolk, P.; Shakir, S. The UK BIO-TRAC Study: A Cross-Sectional Study of Product and Batch Traceability for Biologics in Clinical Practice and Electronic Adverse Drug Reaction Reporting in the UK. Drug Saf. 2020, 43, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Socal, M.; Ballreich, J.; Chyr, L.; Anderson, G. Biosimilar Medications—Savings Opportunities for Large Employers; A Report for ERIC—The ERISA Industry Committee; Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health: Baltimore, MD, USA, 2020. [Google Scholar]




| Active Ingredient | Year | Biosimilars | Manufacturer | Country/Regulatory Body | Therapeutic Areas | References |
|---|---|---|---|---|---|---|
| Epoetin alfa | 2007 | Abseamed | Medice Arzneimittel Putter GmbH & Co. Kg | Europe/EMA | Cancer, ANE, CKF | [36] |
| 2007 | Binocrit | Sandoz GmbH | Europe/EMA | ANE, CKF | [37] | |
| 2007 | Epoetin-α Hexal | Hexal Ag | Europe/EMA | ANE, cancer, ANE, CKF | [38] | |
| 2007 | Retacrit | Hospira UK Limited | Europe/EMA | ANE, cancer, ABT, CKF | [39] | |
| 2007 | Silapo | Stada Arzneimittel Ag | Europe/EMA | ANE, cancer, ABT, CKF | [40] | |
| Epoetin lambda | 2010 | Novicrit | Sandoz | Australia/TGA | ANE, cancer, CKF | [41] |
| 2010 | Aczicrit | Sandoz | Australia/TGA | ANE, cancer, CKF | ||
| 2010 | Grandicrit | Sandoz | Australia/TGA | ANE, cancer, CKF | ||
| Epoetin alfa-epbx | 2018 | Retacrit | Hospira Inc. | USA/FDA | ANE (caused by chronic kidney disease, CHM, or patients taking zidovudine), reduction in allogeneic red blood cell transfusions | [42] |
| Filgrastim | 2008 | Ratiograstim | Ratiopharm GmbH | Europe/EMA | Cancer, hematopoietic stem cell transplantation (HSCT), NTP | [43] |
| 2008 | Tevagrastim | Teva GmbH | Europe/EMA | Cancer, HSCT, NTP | [44] | |
| 2009 | Zarzio | Sandoz | Europe/EMA | Cancer, HSCT, NTP | [45] | |
| 2009 | Filgrastimhexal | Hexal Ag | Europe/EMA | Cancer, HSCT, NTP | [46] | |
| 2010 | Nivestim | Hospira UK | Europe/EMA | Cancer, HSCT, NTP | [47] | |
| 2010 | Nivestim | Hospira | Australia/TGA | Cancer, HSCT, NTP | [41] | |
| 2011 | Tevagrastim | Aspen Pharmacare Australia | Australia/TGA | Cancer, HSCT, NTP | [41] | |
| 2013 | Zarzio | Sandoz | Australia/TGA | Cancer, HSCT, NTP | [41] | |
| 2013 | Grastofil | Apotex Europe Bv | Europe/EMA | NTP | [48] | |
| 2014 | Accofil | Accord Healthcare Ltd. | Europe/EMA | NTP | [49] | |
| 2015 | Zarxio | Sandoz Inc. | USA/FDA | BMT, APBPC, NTP, ML | [50] | |
| 2015 | Grastofil | Apotex | Canada/Health Canada | NTP | [51] | |
| Filgrastim-aafi | 2018 | Nivestym | Pfizer Inc. | USA/FDA | BMT, APBPC, cancer, NTP, ML | [52] |
| Pegfilgrastim | 2018 | Udenyca | Coherus | Europe/EMA | NTP | [53] |
| 2018 | Fulphila | Mylan S.A.S. | Europe/EMA | NTP | [54] | |
| 2018 | Pelmeg | Cinfa Biotech S.L. | Europe/EMA | NTP | [55] | |
| 2018 | Ziextenzo | Sandoz GmbH | Europe/EMA | NTP | [56] | |
| 2018 | Ogivri | Mylan S.A.S. | Europe/EMA | MBC, EBC, MGC | [57] | |
| 2020 | Ziextenzo | Sandoz | Australia/TGA | CHM-induced NTP, HSCT | [41] | |
| 2020 | Fulphila | Alphapharm | Australia/TGA | CHM-induced NTP, HSCT | ||
| 2020 | Pelgraz | Accord | Australia/TGA | CHM-induced NTP, HSCT | ||
| 2020 | Ziextenzo | Sandoz | Canada/Health Canada | NTP | [51] | |
| Pegfligrastim-jmdb | 2018 | Fulphila | Mylan/Biocon | USA/FDA | FN | [58] |
| Pegfligrastim-cbqv | 2018 | Udenyca | Coherus Biosciences | USA/FDA | FN | [59] |
| Pegfilgrastim-apgf | 2020 | Nyvepria | Pfizer Inc. | USA/FDA | FN | [60] |
| Rituximab | 2017 | Riximyo | Sandoz Australia | Australia/TGA | Chronic lymphocytic leukemia (CLL), B-cell NHL, MPA, WG, RA | [41] |
| 2017 | Truxima | Celltrion Healthcare Hungary Kft | Europe/EMA | GPA, CLL, MPA, RA, n-HL | [61] | |
| 2017 | Riximyo | Sandoz GmbH | Europe/EMA | B-CLL, n-HL, MPA, WG, RA | [62] | |
| 2017 | Rixathon | Sandoz GmbH | Europe/EMA | MPA, CLL, B-cell n-HL, WG, RA | [63] | |
| 2017 | Ritemvia | Celltrion Healthcare Hungary Kft. | Europe/EMA | WG, n-HL, MPA | [64] | |
| 2017 | Blitzima | Celltrion Healthcare Hungary Kft. | Europe/EMA | B-CLL, n-HL | [65] | |
| 2018 | Truxima | Celltrion | Australia/TGA | B-cell NHL, MPA, CLL, WG, RA | [41] | |
| 2020 | Riximyo | Sandoz | Canada/Health Canada | RA, n-HL, CLL | [51] | |
| 2020 | Ruxience | Pfizer | Canada/Health Canada | RA, n-HL, CLL | ||
| Rituximab-abbs | 2018 | Truxima | Celltrion Inc. | USA/FDA | n-HL | [66] |
| Rituximab-pvvr | 2019 | Ruxience | Pfizer Inc. | USA/FDA | CLL, GPA, n-HL | [67] |
| Trastuzumab | 2017 | Ontruzant | Samsung Bioepis | Europe/EMA | EBC, MGC, MBC | [68] |
| 2017 | Ogivri | Mylan | USA/FDA | HER2 BC, AC, HER2 MGGJ, | [69] | |
| 2018 | Herzuma | Celltrion Healthcare | Australia/TGA | EBC, MGC, MBC | [41] | |
| 2018 | Herzuma | Celltrion Healthcare Hungary Kft. | Europe/EMA | EBC, MGC, MBC | [70] | |
| 2018 | Kanjinti | Amgen Europe | Europe/EMA | EBC, MGC, MBC | [71] | |
| 2018 | Trazimera | Pfizer Europe | Europe/EMA | Stomach neoplasms, breast neoplasms | [72] | |
| 2019 | Herzuma | Celltrion | Canada/Health Canada | BC, GC | [51] | |
| 2019 | Ogivri | Alphapharm | Australia/TGA | BC, GC | [41] | |
| 2019 | Kanjinti | Amgen | Australia/TGA | BC, GC | ||
| 2020 | Ontruzant | Merck Sharp and Dohme | Australia/TGA | BC, GC | ||
| 2020 | Trazimera | Pfizer | Australia/TGA | BC, GC | ||
| 2020 | Kanjinti | Amgen Canada | Canada/Health Canada | EBC, MGC, MBC | [51] | |
| Trastuzumab-pkrb | 2018 | Herzuma | Celltrion Inc. | USA/FDA | BC | [73] |
| Trastuzumab-dttb | 2019 | Ontruzant | Samsung Bioepis | USA/FDA | HER2 BC, HER2 MGGJ, AC | [74] |
| Trastuzumab-qyyp | 2019 | Trazimera | Pfizer Ind. | USA/FDA | HER2 BC, HER2 MGGJ, AC | [75] |
| Trastuzumab-anns | 2019 | Kanjinti | Amgen Inc. | USA/FDA | HER2 BC, HER2 MGGJ, AC | [76] |
| Bevacizumab | 2017 | Mvasi | Amgen, Inc. | USA/FDA | NSCLC, RCC, colorectal neoplasms, breast neoplasms, ovarian neoplasms | [77] |
| 2018 | Mvasi | Amgen Europe B.V. | Europe/EMA | Breast neoplasms, non-small-cell lung carcinoma, fallopian tube neoplasms, peritoneal neoplasms, ovarian neoplasms, RCC | [78] | |
| Bevacizumab-bvzr | 2019 | Zirabev | Pfizer Inc. | USA/FDA | NSCLC, CRC, cervical cancer, breast neoplasms, RCC | [79] |
| Country | Regulatory Bodies | Regulatory Guidelines | Authorities Responsible for Pharmacovigilance | Database | Reference |
|---|---|---|---|---|---|
| Europe | EMA | European Medicines Agency: Similar Biological Medicinal Products (overarching guidelines). CHMP/437/04 Rev. 1 European Medicines Agency: Guideline on Good Pharmacovigilance Practices (GVPs), Product- or Population-Specific considerations II: Biological Medicinal Products. EMA/168402/2014 | European Commission, EudraVigilance Data Analysis System (EVDAS), Good Pharmacovigilance Practices (GVP) | European Database of Suspected Adverse Drug Reaction Reports, European Commission, EudraVigilance Data Analysis System (EVDAS), EudraVigilance Web Trader (EVWEB) | [150] |
| Canada | Biologics and Genetics Therapy Directorate (BGTD), Health Products and Food Branch (HPFB) | Information and Submission Requirements for Biosimilar Biologic Drugs (2010, revised 2016) | Health Canada | Vigilance | [151] |
| USA | FDA | Labeling for Biosimilar Products; Guidance for Industry (2016) Reference Product Exclusivity for Biological Products Filed Under Section 351(a) of the PHS Act (2015) | Center for Drug Evaluation and Research (CDER), Center for Biologics Evaluation and Research (CBER) | FAERS, Sentinel System | [152] |
| Australia | Therapeutic Goods Administration | Pharmacovigilance Responsibilities of Medicine Sponsors: Australian Recommendations and Requirements. Risk Management Plans for Prescription Medicines | Therapeutic Goods Administration | Database of Adverse Event Notification (DAEN) | [153] |
| South Korea | Korean Food and Drug Administration | Guideline on Evaluation of Biosimilar Products Regulation on Marketing Authorization of Biopharmaceutical Products (2007) | Ministry of Food and Drug Safety | Korea Adverse Event Reporting System (KAERS) | [154] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Joshi, D.; Khursheed, R.; Gupta, S.; Wadhwa, D.; Singh, T.G.; Sharma, S.; Porwal, S.; Gauniyal, S.; Vishwas, S.; Goyal, S.; et al. Biosimilars in Oncology: Latest Trends and Regulatory Status. Pharmaceutics 2022, 14, 2721. https://doi.org/10.3390/pharmaceutics14122721
Joshi D, Khursheed R, Gupta S, Wadhwa D, Singh TG, Sharma S, Porwal S, Gauniyal S, Vishwas S, Goyal S, et al. Biosimilars in Oncology: Latest Trends and Regulatory Status. Pharmaceutics. 2022; 14(12):2721. https://doi.org/10.3390/pharmaceutics14122721
Chicago/Turabian StyleJoshi, Deeksha, Rubiya Khursheed, Saurabh Gupta, Diksha Wadhwa, Thakur Gurjeet Singh, Sumit Sharma, Sejal Porwal, Swati Gauniyal, Sukriti Vishwas, Sanjay Goyal, and et al. 2022. "Biosimilars in Oncology: Latest Trends and Regulatory Status" Pharmaceutics 14, no. 12: 2721. https://doi.org/10.3390/pharmaceutics14122721





