Dual-Drug Delivery via Zein In Situ Forming Implants Augmented with Titanium-Doped Bioactive Glass for Bone Regeneration: Preparation, In Vitro Characterization, and In Vivo Evaluation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Zein In Situ Forming Implants (ZIFIs)
2.3. In Vitro Characterization of the Prepared Zein In Situ Forming Implants (ZIFIs)
2.3.1. In Vitro Solidification Time
2.3.2. Rheological Properties
2.3.3. Injectability Test
2.3.4. In Vitro Release Study
2.4. Preparation and Evaluation of Zein In Situ Forming Implants Loaded with Bioactive Glass Nanoparticles (BG-ZIFI)
2.4.1. Preparation of Bioactive Glass (BG) Nanoparticles
2.4.2. Evaluation of Bioactive Glass Nanoparticles by Transmission Electron Microscope (TEM)
2.4.3. Loading Zein In Situ Forming Implants with Bioactive Glass Nanoparticles
2.4.4. In Vitro Release Study
2.5. Preparation of Dual-Medicated Zein In Situ Forming Implants (D-ZIFI)
2.6. Characterization of Dual-Medicated Zein In Situ Forming Implants (D-ZIFI)
2.6.1. In Vitro Release Study
2.6.2. Fourier-Transform Infrared (FTIR) Spectroscopy
2.6.3. Differential Scanning Calorimetry (DSC)
2.6.4. Morphological Examination
2.6.5. Effect of Gamma Sterilization
2.7. Statistical Analysis
2.8. In Vivo Animal Study
2.8.1. Animals
2.8.2. Surgical Procedures
2.8.3. Dosing the Formulations
2.8.4. Histological Assay
3. Results and Discussion
3.1. Preparation of Zein In Situ Forming Implants (ZIFIs)
3.2. In Vitro Characterization of the Prepared Zein In Situ Forming Implants (ZIFIs)
3.2.1. In Vitro Solidification Time
3.2.2. Rheological Properties
3.2.3. Injectability Test
3.2.4. In Vitro Release Study
3.3. Preparation and Evaluation of Zein In Situ Forming Implants Loaded with Bioactive Glass Nanoparticles (BG-ZIFI)
3.3.1. Evaluation of Bioactive Glass Nanoparticles by Transmission Electron Microscope (TEM)
3.3.2. In Vitro Release Study
3.4. Preparation of Dual-Medicated Zein In Situ Forming Implant (D-ZIFI)
3.5. Characterization of Dual-Medicated Zein In Situ Forming Implant (D-ZIFI)
3.5.1. In Vitro Solidification Time
3.5.2. Rheological Properties
3.5.3. Injectability Test
3.5.4. In Vitro Release Study
3.5.5. Fourier-Transform Infrared (FTIR) Spectroscopy
3.5.6. Differential Scanning Calorimetry (DSC)
3.5.7. Morphological Examination
3.5.8. Effect of Gamma Sterilization
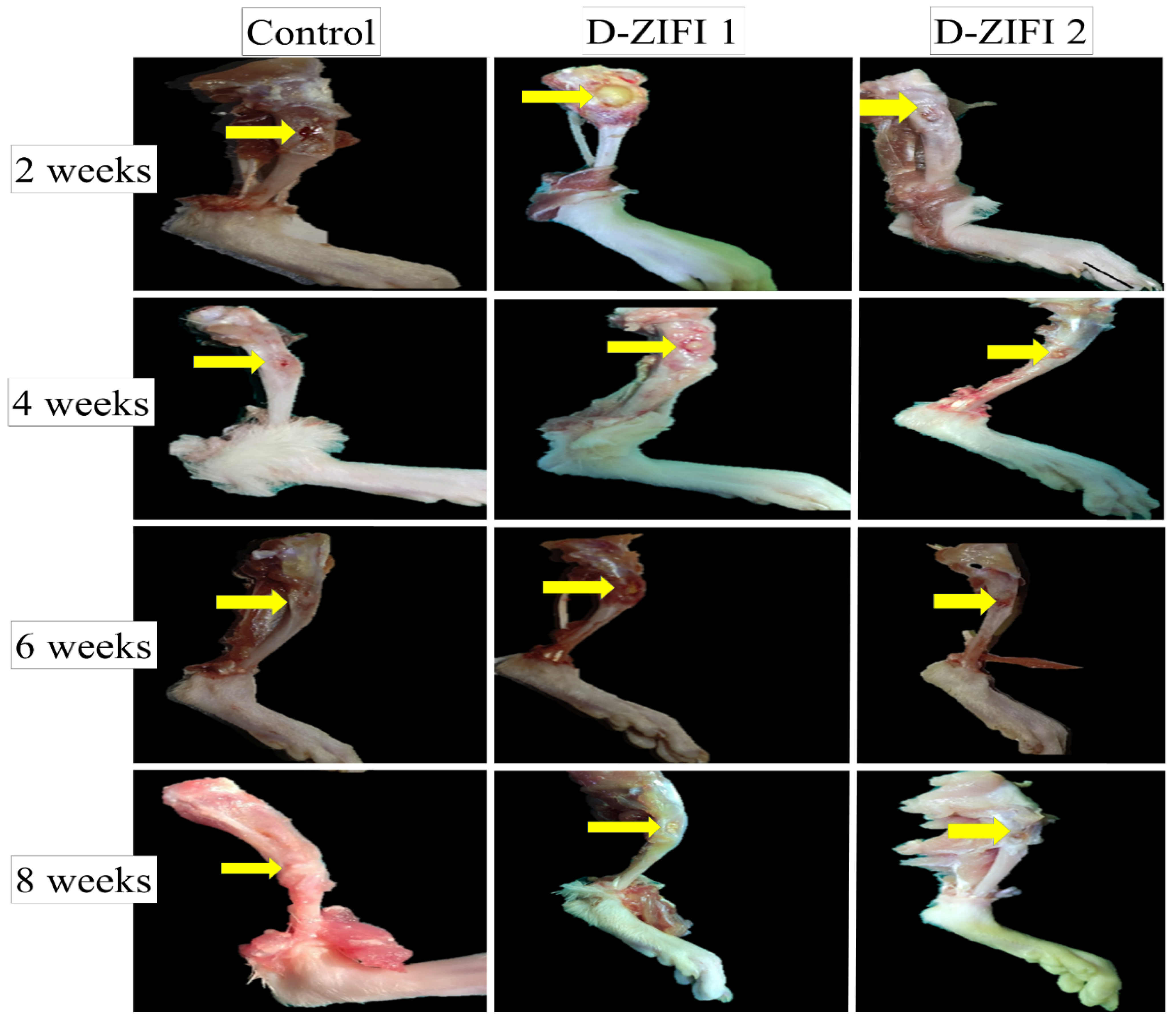
3.6. In Vivo Animal Study
Histological Assay
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Qu, H.; Fu, H.; Han, Z.; Sun, Y. Biomaterials for bone tissue engineering scaffolds: A review. RSC Adv. 2019, 9, 26252–26262. [Google Scholar] [CrossRef] [Green Version]
- Elkasabgy, N.A.; Mahmoud, A.A. Fabrication Strategies of Scaffolds for Delivering Active Ingredients for Tissue Engineering. AAPS PharmSciTech 2019, 20, 256. [Google Scholar] [CrossRef]
- Singh, B.N.; Veeresh, V.; Mallick, S.P.; Sinha, S.; Rastogi, A.; Srivastava, P. Generation of scaffold incorporated with nanobioglass encapsulated in chitosan/chondroitin sulfate complex for bone tissue engineering. Int. J. Biol. Macromol. 2020, 153, 1–16. [Google Scholar] [CrossRef]
- Grewal, B.S.; Keller, B.; Weinhold, P.; Dahners, L.E. Evaluating effects of deferoxamine in a rat tibia critical bone defect model. J. Orthop. 2014, 11, 5–9. [Google Scholar] [CrossRef] [Green Version]
- Mahyudin, F.; Utomo, D.N.; Suroto, H.; Martanto, T.W.; Edward, M.; Gaol, I.L. Comparative Effectiveness of Bone Grafting Using Xenograft Freeze-Dried Cortical Bovine, Allograft Freeze-Dried Cortical New Zealand White Rabbit, Xenograft Hydroxyapatite Bovine, and Xenograft Demineralized Bone Matrix Bovine in Bone Defect of Femoral Di. Int. J. Biomater. 2017, 2017, 7571523. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, H.; Esfahani, S.N.; Poorganji, B.; Dean, D.; Elahinia, M. Resorbable bone fixation alloys, forming, and post-fabrication treatments. Mater. Sci. Eng. C 2017, 70, 870–888. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chocholata, P.; Kulda, V.; Babuska, V. Fabrication of Scaffolds for Bone-Tissue Regeneration. Materials 2019, 12, 568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adithya, S.P.; Sidharthan, D.S.; Abhinandan, R.; Balagangadharan, K.; Selvamurugan, N. Nanosheets-incorporated bio-composites containing natural and synthetic polymers/ceramics for bone tissue engineering. Int. J. Biol. Macromol. 2020, 164, 1960–1972. [Google Scholar] [CrossRef] [PubMed]
- Khattab, A.; Abouhussein, D.M.N.; Mohammad, F.E. Development of injectable tenoxicam in situ forming microparticles based on sesame oil and poly-DL-lactide: Characterization, efficacy and acute toxicity. J. Drug Deliv. Sci. Technol. 2019, 51, 682–694. [Google Scholar] [CrossRef]
- Falisi, G.; Galli, M.; Vittorini-Velasquez, P.; Gallegos-Rivera, J.C.; Minasi, R.; De Biase, A.; Di Paolo, C. Use of 3D cartilage scaffolds for the stabilization of implants and bone regeneration with the fit-lock technique. Acta Odontol. Latinoam. 2013, 26, 167–172. [Google Scholar] [PubMed]
- Abdel-Salam, F.S.; Elkheshen, S.A.; Mahmoud, A.A.; Basalious, E.B.; Amer, M.S.; Mostafa, A.A.; Elkasabgy, N.A. In-situ forming chitosan implant-loaded with raloxifene hydrochloride and bioactive glass nanoparticles for treatment of bone injuries: Formulation and biological evaluation in animal model. Int. J. Pharm. 2020, 580, 119213. [Google Scholar] [CrossRef] [PubMed]
- Kamel, R.; El-Wakil, N.A.; Dufresne, A.; Elkasabgy, N.A. Nanocellulose: From an agricultural waste to a valuable pharmaceutical ingredient. Int. J. Biol. Macromol. 2020, 163, 1579–1590. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Shen, R.; Komasa, S.; Xue, Y.; Jin, B.; Hou, Y.; Okazaki, J.; Gao, J. Drug-loadable calcium alginate hydrogel system for use in oral bone tissue repair. Int. J. Mol. Sci. 2017, 18, 989. [Google Scholar] [CrossRef] [PubMed]
- Paliwal, R.; Palakurthi, S. Zein in controlled drug delivery and tissue engineering. J. Control. Release 2014, 189, 108–122. [Google Scholar] [CrossRef] [PubMed]
- Ha, T.L.B.; Quan, T.M.; Vu, D.N.; Si, D.M. Naturally Derived Biomaterials: Preparation and Application; Regenerative Medicine and Tissue Engineering; IntechOpen: London, UK, 2013. [Google Scholar] [CrossRef] [Green Version]
- Naseri, S.; Hum, J.; Cole Lepry, W.; Kamal Miri, A.; Najdat Nazhat, S.; Boccaccini, A.R. Fabrication and characterization of zein–bioactive glass scaffolds. Bioinspired. Biomim. Nanobiomaterials 2015, 4, 73–78. [Google Scholar] [CrossRef]
- Lin, T.; Lu, C.; Zhu, L.; Lu, T. The biodegradation of zein in vitro and in vivo and its application in implants. AAPS PharmSciTech 2011, 12, 172–176. [Google Scholar] [CrossRef]
- Nezhad-Mokhtari, P.; Ghorbani, M.; Abdyazdani, N. Reinforcement of hydrogel scaffold using oxidized-guar gum incorporated with curcumin-loaded zein nanoparticles to improve biological performance. Int. J. Biol. Macromol. 2021, 167, 59–65. [Google Scholar] [CrossRef]
- Dong, J.; Sun, Q.; Wang, J.Y. Basic study of corn protein, zein, as a biomaterial in tissue engineering, surface morphology and biocompatibility. Biomaterials 2004, 25, 4691–4697. [Google Scholar] [CrossRef]
- Vogt, L.; Liverani, L.; Roether, J.A.; Boccaccini, A.R. Electrospun zein fibers incorporating poly(glycerol sebacate) for soft tissue engineering. Nanomaterials 2018, 8, 150. [Google Scholar] [CrossRef] [Green Version]
- Lian, H.; Liu, X.; Meng, Z. Enhanced mechanical and osteogenic differentiation performance of hydroxyapatite/zein composite for bone tissue engineering. J. Mater. Sci. 2019, 54, 719–729. [Google Scholar] [CrossRef]
- El-Rashidy, A.A.; Waly, G.; Gad, A.; Roether, J.A.; Hum, J.; Yang, Y.; Detsch, R.; Hashem, A.A.; Sami, I.; Goldmann, W.H.; et al. Antibacterial activity and biocompatibility of zein scaffolds containing silver-doped bioactive glass. Biomed. Mater. 2018, 13, 65006. [Google Scholar] [CrossRef]
- Li, Y.; Yao, C. Mineralization of hydroxyapatite crystallites on zein microspheres. Polym. Compos. 2012, 33, 961–966. [Google Scholar] [CrossRef]
- Liu, Y.; Miao, Y.-L.; Qin, F.; Cao, C.; Yu, X.-L.; Wu, Y.-H.; Wang, T.-L.; Xu, R.-G.; Zhao, L.; Wu, F. Electrospun poly (aspartic acid)-modified zein nanofibers for promoting bone regeneration. Int. J. Nanomed. 2019, 14, 9497. [Google Scholar] [CrossRef] [Green Version]
- Zou, Y.; Zhang, L.; Yang, L.; Zhu, F.; Ding, M.; Lin, F.; Wang, Z.; Li, Y. “Click” chemistry in polymeric scaffolds: Bioactive materials for tissue engineering. J. Control. Release 2018, 273, 160–179. [Google Scholar] [CrossRef]
- Rodríguez-Arco, L.; Poma, A.; Ruiz-Pérez, L.; Scarpa, E.; Ngamkham, K.; Battaglia, G. Molecular bionics–engineering biomaterials at the molecular level using biological principles. Biomaterials 2019, 192, 26–50. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Ramaswamy, Y.; Zhu, Y.; Zheng, R.; Appleyard, R.; Howard, A.; Zreiqat, H. The effect of mesoporous bioactive glass on the physiochemical, biological and drug-release properties of poly(dl-lactide-co-glycolide) films. Biomaterials 2009, 30, 2199–2208. [Google Scholar] [CrossRef]
- Wu, S.; Liu, X.; Yeung, K.W.K.; Liu, C.; Yang, X. Biomimetic porous scaffolds for bone tissue engineering. Mater. Sci. Eng. R Reports 2014, 80, 1–36. [Google Scholar] [CrossRef]
- Katagiri, T.; Watabe, T. Bone morphogenetic proteins. Cold Spring Harb. Perspect. Biol. 2016, 8, 1–28. [Google Scholar] [CrossRef] [Green Version]
- Cundy, T.; Reid, I.R.; Grey, A. Metabolic bone disease. In Clinical Biochemistry: Metabolic and Clinical Aspects, 3rd ed.; Elsevier: Amsterdam, The Netherlands, 2014; pp. 604–635. [Google Scholar] [CrossRef]
- Szulc, P.; Bauer, D.C. Biochemical Markers of Bone Turnover in Osteoporosis. In Osteoporosis, 4th ed.; Elsevier: Amsterdam, The Netherlands, 2013; pp. 1573–1610. [Google Scholar] [CrossRef]
- Boskey, A.L.; Robey, P.G. The Regulatory Role of Matrix Proteins in Mineralization of Bone. In Osteoporosis, 4th ed.; Elsevier: Amsterdam, The Netherlands, 2013; pp. 235–255. [Google Scholar] [CrossRef]
- Moser, S.C.; van der Eerden, B.C.J. Osteocalcin—A versatile bone-derived hormone. Front. Endocrinol. 2019, 10, 4–9. [Google Scholar] [CrossRef] [Green Version]
- Coxon, F.P.; Helfrich, M.H.; Van’t Hof, R.; Sebti, S.; Ralston, S.H.; Hamilton, A.; Rogers, M.J. Protein geranylgeranylation is required for osteoclast formation, function, and survival: Inhibition by bisphosphonates and GGTI-298. J. Bone Miner. Res. 2000, 15, 1467–1476. [Google Scholar] [CrossRef]
- Juvekar, S.; Kathpalia, H. Solvent removal precipitation based in situ forming implant for controlled drug delivery in periodontitis. J. Control. Release 2017, 251, 75–81. [Google Scholar] [CrossRef]
- Elkasabgy, N.A.; Abdel-Salam, F.S.; Mahmoud, A.A.; Basalious, E.B.; Amer, M.S.; Mostafa, A.A.; Elkheshen, S.A. Long lasting in-situ forming implant loaded with raloxifene HCl: An injectable delivery system for treatment of bone injuries. Int. J. Pharm. 2019, 571, 118703. [Google Scholar] [CrossRef]
- Rawlins, E. Bentley’s Textbook of Pharmaceutics; Elsevier Health Sciences: Amsterdam, The Netherlands, 1977. [Google Scholar]
- Leroux, L.; Hatim, Z.; Frèche, M.; Lacout, J.L. Effects of various adjuvants (lactic acid, glycerol, and chitosan) on the injectability of a calcium phosphate cement. Bone 1999, 25, 31S–34S. [Google Scholar] [CrossRef]
- Paul, S.; Hoey, M.F.; Egbert, J.E. Pressure measurements during injection of corticosteroids: In vivo studies. Med. Biol. Eng. Comput. 1999, 37, 645–651. [Google Scholar] [CrossRef]
- Korsmeyer, R.W.; Gurny, R.; Doelker, E.; Buri, P.; Peppas, N.A. Mechanisms of solute release from porous hydrophilic polymers. Int. J. Pharm. 1983, 15, 25–35. [Google Scholar] [CrossRef]
- Peppas, N.A. Analysis of Fickian and non-Fickian drug release from polymers. Pharm. Acta Helv. 1985, 60, 110–111. [Google Scholar]
- Mabrouk, M.; Beherei, H.H.; Tanaka, Y.; Tanaka, M. Investigating the Intermediate Water Feature of Hydrated Titanium Containing Bioactive Glass. Int. J. Mol. Sci. 2021, 22, 8038. [Google Scholar] [CrossRef]
- Emad Eldeeb, A.; Salah, S.; Ghorab, M. Proniosomal gel-derived niosomes: An approach to sustain and improve the ocular delivery of brimonidine tartrate; formulation, in-vitro characterization, and in-vivo pharmacodynamic study. Drug Deliv. 2019, 26, 509–521. [Google Scholar] [CrossRef] [Green Version]
- El-Gindy, A.; El-Zeany, B.; Awad, T.; Shabana, M.M. Spectrophotometric determination of trifluoperazine HCl and isopropamide iodide in binary mixture using second derivative and second derivative of the ratio spectra methods. J. Pharm. Biomed. Anal. 2001, 26, 203–210. [Google Scholar] [CrossRef]
- Eldeeb, A.E.; Salah, S.; Ghorab, M. Formulation and evaluation of cubosomes drug delivery system for treatment of glaucoma: Ex-vivo permeation and in-vivo pharmacodynamic study. J. Drug Deliv. Sci. Technol. 2019, 52, 236–247. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, W.Y.; Lan, R.; Wang, J.Y. Quality Monitoring of Porous Zein Scaffolds: A Novel Biomaterial. Engineering 2017, 3, 130–135. [Google Scholar] [CrossRef]
- Flanner, M.; Moore, J.W.; Planner, H.H. Mathematical Comparison of Dissolution Profiles. Pharm. Technol. 1996, 20, 64–74. [Google Scholar] [CrossRef] [Green Version]
- Flecknell, P. Laboratory Animal Anaesthesia, 4th ed.; Academic Press: Cambridge, MA, USA, 2015; pp. 1–321. [Google Scholar]
- Zhang, X.; Zhu, L.; Lv, H.; Cao, Y.; Liu, Y.; Xu, Y.; Ye, W.; Wang, J. Repair of rabbit femoral condyle bone defects with injectable nanohydroxyapatite/chitosan composites. J. Mater. Sci. Mater. Med. 2012, 23, 1941–1949. [Google Scholar] [CrossRef]
- Bancroft, J.D.; Gamble, M. Bancroft’s Theory and Practice of Histological Techniques; Elsevier Health Sciences: Amsterdam, The Netherlands, 2019; ISBN 0443102791. [Google Scholar] [CrossRef]
- Thakur, R.R.S.; McMillan, H.L.; Jones, D.S. Solvent induced phase inversion-based in situ forming controlled release drug delivery implants. J. Control. Release 2014, 176, 8–23. [Google Scholar] [CrossRef]
- Kumar, G.P.; Rajeshwarrao, P. Nonionic surfactant vesicular systems for effective drug delivery—An overview. Acta Pharm. Sin. B 2011, 1, 208–219. [Google Scholar] [CrossRef] [Green Version]
- Ibrahim, T.M.; El-Megrab, N.A.; El-Nahas, H.M. Optimization of injectable PLGA in-situ forming implants of anti-psychotic risperidone via Box-Behnken Design. J. Drug Deliv. Sci. Technol. 2020, 58, 101803. [Google Scholar] [CrossRef]
- Dealy, J.M.; Wissbrun, K.F. Introduction to Rheology. In Melt Rheology and Its Role in Plastics Processing; Springer: Dordrecht, The Netherlands, 1999; pp. 1–41. [Google Scholar] [CrossRef]
- Wei, Y.; Hu, L.; Yao, J.; Shao, Z.; Chen, X. Facile Dissolution of Zein Using a Common Solvent Dimethyl Sulfoxide. Langmuir 2019, 35, 6640–6649. [Google Scholar] [CrossRef]
- Lee, C.H.; Moturi, V.; Lee, Y. Thixotropic property in pharmaceutical formulations. J. Control. Release 2009, 136, 88–98. [Google Scholar] [CrossRef]
- Mashak, A.; Mobedi, H.; Ziaee, F.; Nekoomanesh, M. The effect of aliphatic esters on the formation and degradation behavior of PLGA-based in situ forming system. Polym. Bull. 2011, 66, 1063–1073. [Google Scholar] [CrossRef]
- Kamel, R.; El-Wakil, N.A.; Abdelkhalek, A.F.A.; Elkasabgy, N.A. Nanofibrillated cellulose/cyclodextrin based 3D scaffolds loaded with raloxifene hydrochloride for bone regeneration. Int. J. Biol. Macromol. 2020, 156, 704–716. [Google Scholar] [CrossRef]
- Adel, I.M.; ElMeligy, M.F.; Abdelkhalek, A.A.; Elkasabgy, N.A. Design and characterization of highly porous curcumin loaded freeze-dried wafers for wound healing. Eur. J. Pharm. Sci. 2021, 164, 105888. [Google Scholar] [CrossRef] [PubMed]
- Shamma, R.N.; Elkasabgy, N.A.; Mahmoud, A.A.; Gawdat, S.I.; Kataia, M.M.; Abdel Hamid, M.A. Design of novel injectable in-situ forming scaffolds for non-surgical treatment of periapical lesions: In-vitro and in-vivo evaluation. Int. J. Pharm. 2017, 521, 306–317. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Murugavel, S.; Aditya, A.; Boccaccini, A.R. Mesoporous 45S5 bioactive glass: Synthesis, in vitro dissolution and biomineralization behavior. J. Mater. Chem. B 2017, 5, 8786–8798. [Google Scholar] [CrossRef] [PubMed]
- Rahaman, M.N.; Day, D.E.; Sonny Bal, B.; Fu, Q.; Jung, S.B.; Bonewald, L.F.; Tomsia, A.P. Bioactive glass in tissue engineering. Acta Biomater. 2011, 7, 2355–2373. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Dong, C.; Hu, Y.; Gao, M.; Luan, G. Zein as a structural protein in gluten-free systems: An overview. Food Sci. Hum. Wellness 2021, 10, 270–277. [Google Scholar] [CrossRef]
- Bouman, J.; Belton, P.; Venema, P.; Van Der Linden, E.; De Vries, R.; Qi, S. Controlled Release from Zein Matrices: Interplay of Drug Hydrophobicity and pH. Pharm. Res. 2016, 33, 673–685. [Google Scholar] [CrossRef] [Green Version]
- Hariram, B.; Kumar, R.S.; Jaya Shree, A.; Rao, D.V.; Kalyanaraman, L.; Srinivas, K. Ultra-High Performance Method on Superficially Porous Stationary Phase for the Determination of Related Substances in Pitavastatin Calcium by HPLC. Chromatographia 2015, 78, 1017–1029. [Google Scholar] [CrossRef]
- Sergi, R.; Bellucci, D.; Cannillo, V. A review of bioactive glass/natural polymer composites: State of the art. Materials 2020, 13, 5560. [Google Scholar] [CrossRef]
- Mahdy, E.A.; Sahbal, K.M.; Mabrouk, M.; Beherei, H.H.; Abdel-Monem, Y.K. Enhancement of glass-ceramic performance by TiO2 doping: In vitro cell viability, proliferation, and differentiation. Ceram. Int. 2020, 47, 6251–6261. [Google Scholar] [CrossRef]
- Civantos, A.; Martínez-Campos, E.; Ramos, V.; Elvira, C.; Gallardo, A.; Abarrategi, A. Titanium Coatings and Surface Modifications: Toward Clinically Useful Bioactive Implants. ACS Biomater. Sci. Eng. 2017, 3, 1245–1261. [Google Scholar] [CrossRef]
- Rodriguez, O.; Stone, W.; Schemitsch, E.H.; Zalzal, P.; Waldman, S.; Papini, M.; Towler, M.R. Titanium addition influences antibacterial activity of bioactive glass coatings on metallic implants. Heliyon 2017, 3, e00420. [Google Scholar] [CrossRef]
- Johnson, A.M.; Trakhtenberg, S.; Cannon, A.S.; Warner, J.C. Effect of pH on the viscosity of titanium dioxide aqueous dispersions with carboxylic acids. J. Phys. Chem. A 2007, 111, 8139–8146. [Google Scholar] [CrossRef] [PubMed]
- Kopf, A.W. The Distribution of Alkaline Phosphatase in Normal and Pathologic Human Skin. AMA Arch. Dermatol. 1957, 75, 1–37. [Google Scholar] [CrossRef] [PubMed]
- Azrad, M.; Baum, M.; Rokney, A.; Levi, Y.; Peretz, A. In vitro activity of Tedizolid and Dalbavancin against MRSA strains is dependent on infection source. Int. J. Infect. Dis. 2019, 78, 107–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abad, L.; Tafani, V.; Tasse, J.; Josse, J.; Chidiac, C.; Lustig, S.; Ferry, T.; Diot, A.; Laurent, F.; Valour, F. Evaluation of the ability of linezolid and tedizolid to eradicate intraosteoblastic and biofilm-embedded Staphylococcus aureus in the bone and joint infection setting. J. Antimicrob. Chemother. 2019, 74, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Golub, E.; Boesze-Battaglia, K. The role of alkaline phosphatase in mineralization. Curr. Opin. Orthop. 2007, 18, 444–448. [Google Scholar] [CrossRef]
- Agarwal, G.; Agiwal, S.; Srivastava, A. Hyaluronic acid containing scaffolds ameliorate stem cell function for tissue repair and regeneration. Int. J. Biol. Macromol. 2020, 165, 388–401. [Google Scholar] [CrossRef]
- Choi, S.; Lee, J.S.; Shin, J.; Lee, M.S.; Kang, D.; Hwang, N.S.; Lee, H.; Yang, H.S.; Cho, S.W. Osteoconductive hybrid hyaluronic acid hydrogel patch for effective bone formation. J. Control. Release 2020, 327, 571–583. [Google Scholar] [CrossRef]
- Li, C.; Cao, Z.; Li, W.; Liu, R.; Chen, Y.; Song, Y.; Liu, G.; Song, Z.; Liu, Z.; Lu, C.; et al. A review on the wide range applications of hyaluronic acid as a promising rejuvenating biomacromolecule in the treatments of bone related diseases. Int. J. Biol. Macromol. 2020, 165, 1264–1275. [Google Scholar] [CrossRef]
- El-Saharty, Y.S.; Hassan, N.Y.; Metwally, F.H. Simultaneous determination of terbinafine HCL and triamcinolone acetonide by UV derivative spectrophotometry and spectrodensitometry. J. Pharm. Biomed. Anal. 2002, 28, 569–580. [Google Scholar] [CrossRef]
- Mahalakshmi, K. Formulation and In-Vitro Evaluation of Liquid and Solid Self Microemulsifying Drug Delivery System of Pitavastatin Calcium. Ph.D. Thesis, College of Pharmacy, Madurai Medical College, Madurai, India, 2018. [Google Scholar]
- Paczkowska-walendowska, M.; Rosiak, N.; Tykarska, E.; Michalska, K.; Płazińska, A.; Płaziński, W.; Szymanowska, D.; Cielecka-piontek, J. Tedizolid-cyclodextrin system as delayed-release drug delivery with antibacterial activity. Int. J. Mol. Sci. 2021, 22, 115. [Google Scholar] [CrossRef]
- Shinde, P.; Agraval, H.; Srivastav, A.K.; Yadav, U.C.S.; Kumar, U. Physico-chemical characterization of carvacrol loaded zein nanoparticles for enhanced anticancer activity and investigation of molecular interactions between them by molecular docking. Int. J. Pharm. 2020, 588, 119795. [Google Scholar] [CrossRef] [PubMed]
- Zia, R.; Riaz, M.; Maqsood, S.; Anjum, S.; Kayani, Z.; Hussain, T. Titania doped bioactive ceramics prepared by solid state sintering method. Ceram. Int. 2015, 41, 8964–8972. [Google Scholar] [CrossRef]
- Rezaei, Y.; Moztarzadeh, F.; Shahabi, S.; Tahriri, M. Synthesis, characterization, and in vitro bioactivity of sol-gel-derived SiO2-CaO-P2O5-MgO-SrO bioactive glass. Synth. React. Inorg. Met. Nano-Metal Chem. 2014, 44, 692–701. [Google Scholar] [CrossRef]
- Mukherjee, D.P.; Das, S.K. The influence of TiO2 content on the properties of glass ceramics: Crystallization, microstructure and hardness. Ceram. Int. 2014, 40, 4127–4134. [Google Scholar] [CrossRef]
- Al-Amin, M.; Chandra Dey, S.; Rashid, T.U.; Ashaduzzaman, M.; Shamsuddin, S.M.; Dey, S.C.; Rashid, T.U.; Ashaduzzaman, M.; Shamsuddin, S.M. Solar Assisted Photocatalytic Degradation of Reactive Azo Dyes in Presence of Anatase Titanium Dioxide. Int. J. Latest Res. Eng. Technol. (IJLRET) 2016, 2, 14–21. [Google Scholar]
- Quiñones, J.P.; Brüggemann, O.; Covas, C.P.; Ossipov, D.A. Self-assembled hyaluronic acid nanoparticles for controlled release of agrochemicals and diosgenin. Carbohydr. Polym. 2017, 173, 157–169. [Google Scholar] [CrossRef]
- US20190256469A1—Crystalline Forms of Pitavastatin Calcium—Google Patents, (n.d.). Available online: https://patents.google.com/patent/US20190256469A1/en (accessed on 29 July 2021).
- 147526-32-7 Pitavastatin Calcium AKSci F362, (n.d.). Available online: https://aksci.com/item_detail.php?cat=F362 (accessed on 29 July 2021).
- Cada, D.; Ingram, K.; Baker, D. Formulary drug reviews: Tedizolid phosphate. Hosp. Pharm. 2014, 49, 961–971. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.; Ma, P.; Gui, S. Cubic and hexagonal liquid crystals as drug delivery systems. Biomed. Res. Int. 2014, 2014, 1–12. [Google Scholar] [CrossRef]
- Corradini, E.; Curti, P.S.; Meniqueti, A.B.; Martins, A.F.; Rubira, A.F.; Muniz, E.C. Recent advances in food-packing, pharmaceutical and biomedical applications of zein and zein-based materials. Int. J. Mol. Sci. 2014, 15, 22438–22470. [Google Scholar] [CrossRef] [Green Version]
- Benešová, K.; Pekař, M.; Lapčík, L.; Kučerík, J. Stability evaluation of n-alkyl hyaluronic acid derivates by DSC and TG measurement. J. Therm. Anal. Calorim. 2006, 83, 341–348. [Google Scholar] [CrossRef]
- Elkasabgy, N.A.; Mahmoud, A.A.; Shamma, R.N. Determination of cytocompatibility and osteogenesis properties of in situ forming collagen-based scaffolds loaded with bone synthesizing drug for bone tissue engineering. Int. J. Polym. Mater. Polym. Biomater. 2018, 67, 494–500. [Google Scholar] [CrossRef]
- Adel, I.M.; ElMeligy, M.F.; Abdelrahim, M.E.A.E.A.; Maged, A.; Abdelkhalek, A.A.; Abdelmoteleb, A.M.M.M.; Elkasabgy, N.A. Design and Characterization of Spray-Dried Proliposomes for the Pulmonary Delivery of Curcumin. Int. J. Nanomed. 2021, 16, 2667–2687. [Google Scholar] [CrossRef] [PubMed]
- Peric, M.; Dumic-Cule, I.; Grcevic, D.; Matijasic, M.; Verbanac, D.; Paul, R.; Grgurevic, L.; Trkulja, V.; Bagi, C.M.; Vukicevic, S. The rational use of animal models in the evaluation of novel bone regenerative therapies. Bone 2015, 70, 73–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baldauf, R.; Kanat, I.O. The use of bone wax. J. Foot Surg. 1986, 25, 456–458. [Google Scholar]
- Cho, Y.K.; Kim, C.S.; Kim, S.Y.; Park, J.H.; Kim, H.J.; Park, D.I.; Sohn, C.H.; Jeon, W.K.; Kim, B.I.; Shin, J.H.; et al. The hemostatic effect of endoscopic sodium hyaluronate injection in peptic ulcer bleeding. Hepatogastroenterology 2007, 54, 1276–1279. [Google Scholar]
- Khurana, K.; Guillem-Marti, J.; Soldera, F.; Mücklich, F.; Canal, C.; Ginebra, M.-P. Injectable calcium phosphate foams for the delivery of Pitavastatin as osteogenic and angiogenic agent. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 108, 760–770. [Google Scholar] [CrossRef]
- Wu, Y.J.; Chen, T.; Chen, I.F.; Kuo, S.M.; Chuang, C.W. Developing highly porous collagen scaffolds by using alginate microsphere porogens for stem cell cultures. Mater. Lett. 2018, 223, 120–123. [Google Scholar] [CrossRef]
- Ruiz-Aguilar, C.; Olivares-Pinto, U.; Drew, R.A.L.; Aguilar-Reyes, E.A.; Alfonso, I. Porogen Effect on Structural and Physical Properties of β-TCP Scaffolds for Bone Tissue Regeneration. Irbm 2020, 1, 1–11. [Google Scholar] [CrossRef]
- Abbasi, N.; Hamlet, S.; Love, R.M.; Nguyen, N.T. Porous scaffolds for bone regeneration. J. Sci. Adv. Mater. Devices 2020, 5, 1–9. [Google Scholar] [CrossRef]
- Zhai, P.; Peng, X.; Li, B.; Liu, Y.; Sun, H.; Li, X. The application of hyaluronic acid in bone regeneration. Int. J. Biol. Macromol. 2020, 151, 1224–1239. [Google Scholar] [CrossRef]
- Cui, X.; Huang, C.; Chen, Z.; Zhang, M.; Liu, C.; Su, K.; Wang, J.; Li, L.; Wang, R.; Li, B.; et al. Hyaluronic acid facilitates bone repair effects of calcium phosphate cement by accelerating osteogenic expression. Bioact. Mater. 2021, 6, 3801–3811. [Google Scholar] [CrossRef]
- Sai Nievethitha, S.; Subhapradha, N.; Saravanan, D.; Selvamurugan, N.; Tsai, W.B.; Srinivasan, N.; Murugesan, R.; Moorthi, A. Nanoceramics on osteoblast proliferation and differentiation in bone tissue engineering. Int. J. Biol. Macromol. 2017, 98, 67–74. [Google Scholar] [CrossRef]
- Nokhasteh, S.; Sadeghi-avalshahr, A.; Molavi, A.M.; Khorsand-Ghayeni, M.; Naderi-Meshkin, H. Effect of bioactive glass nanoparticles on biological properties of PLGA/collagen scaffold. Prog. Biomater. 2018, 7, 111–119. [Google Scholar] [CrossRef] [Green Version]
- Farooq, I.; Ali, S.; Husain, S.; Khan, E.; Hill, R.G. Bioactive Glasses—Structure and Applications; Elsevier Ltd.: Amsterdam, The Netherlands, 2019. [Google Scholar] [CrossRef]
- de Dicastillo, C.L.; Correa, M.G.; Martínez, F.B.; Streitt, C.; Galotto, M.J.; López de Dicastillo, C.; Guerrero Correa, M.; Martínez, F.B.; Streitt, C.; José Galotto, M. Antimicrobial effect of titanium dioxide nanoparticles. In Antimicrobial Resistance-a One Health Perspective; IntechOpen: London, UK, 2020. [Google Scholar] [CrossRef] [Green Version]
- Verdier, T.; Coutand, M.; Bertron, A.; Roques, C. Antibacterial activity of TiO 2 photocatalyst alone or in coatings on E. coli: The influence of methodological aspects. Coatings 2014, 4, 670–686. [Google Scholar] [CrossRef]
- Saldana, C.S.; Vyas, D.A.; Wurcel, A.G. Soft Tissue, Bone, and Joint Infections in People Who Inject Drugs. Infect. Dis. Clin. N. Am. 2020, 34, 495–509. [Google Scholar] [CrossRef]








| Formulation Code a | Composition | Characterization | ||||||
|---|---|---|---|---|---|---|---|---|
| Zein (% w/v) | BGT0 (% w/v) | BGT5 (% w/v) | Sodium Hyaluronate (% w/v) | Solidification Time (s) | Flow Rate (mL/min) | Q24h (%) | K (h−1) | |
| ZIFI 1 a | 10 | --- | --- | --- | 104.9 ± 4.9 | 8.6 ± 3.1 | 77.70 ± 0.58 | 39.86 ± 0.03 |
| ZIFI 2 a | 20 | --- | --- | --- | 65.9 ± 2.5 | 2.9 ± 0.4 | 43.15 ± 0.00 | 19.97 ± 0.17 |
| ZIFI 3 a | 30 | --- | --- | --- | 48.9 ± 3.6 | 1.6 ± 0.1 | 36.9 ± 0.40 | 14.23 ± 0.94 |
| BG-ZIFI 1 a | 30 | 1 | 0 | --- | --- | --- | 43.94 ± 0.50 | 21.94 ± 0.37 |
| BG-ZIFI 2 a | 30 | 3 | 0 | --- | --- | --- | 48.88 ± 1.11 | 28.64 ± 1.46 |
| BG-ZIFI 3 a | 30 | 5 | 0 | --- | --- | --- | 52.47 ± 0.69 | 34.76 ± 0.21 |
| BG-ZIFI 4 a | 30 | 10 | 0 | --- | --- | --- | 57.27 ± 0.53 | 36.62 ± 0.20 |
| BG-ZIFI 5 a | 30 | 0 | 1 | --- | --- | --- | 38.84 ± 0.53 | 15.78 ± 0.70 |
| D-ZIFI 1 b | 30 | 0 | 1 | 3 | 52.4 ± 3.1 | 1.2 ± 0.1 | 38.47 ± 0.74 c | 14.29 ± 0.52 c |
| 33.77 ± 0.54 d | 13.34 ± 0.20 d | |||||||
| D-ZIFI 2 b | 30 | 0 | 0 | --- | 43.9 ± 2.5 | 1.5 ± 0.1 | 36.5 ± 0.90 c | 13.85 ± 0.40 c |
| 35.28 ± 1.08 d | 12.42 ± 1.07 d | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eldeeb, A.E.; Salah, S.; Mabrouk, M.; Amer, M.S.; Elkasabgy, N.A. Dual-Drug Delivery via Zein In Situ Forming Implants Augmented with Titanium-Doped Bioactive Glass for Bone Regeneration: Preparation, In Vitro Characterization, and In Vivo Evaluation. Pharmaceutics 2022, 14, 274. https://doi.org/10.3390/pharmaceutics14020274
Eldeeb AE, Salah S, Mabrouk M, Amer MS, Elkasabgy NA. Dual-Drug Delivery via Zein In Situ Forming Implants Augmented with Titanium-Doped Bioactive Glass for Bone Regeneration: Preparation, In Vitro Characterization, and In Vivo Evaluation. Pharmaceutics. 2022; 14(2):274. https://doi.org/10.3390/pharmaceutics14020274
Chicago/Turabian StyleEldeeb, Alaa Emad, Salwa Salah, Mostafa Mabrouk, Mohammed S. Amer, and Nermeen A. Elkasabgy. 2022. "Dual-Drug Delivery via Zein In Situ Forming Implants Augmented with Titanium-Doped Bioactive Glass for Bone Regeneration: Preparation, In Vitro Characterization, and In Vivo Evaluation" Pharmaceutics 14, no. 2: 274. https://doi.org/10.3390/pharmaceutics14020274








