Characterizing the Physicochemical Properties of Two Weakly Basic Drugs and the Precipitates Obtained from Biorelevant Media
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Equilibrium Solubility of API in Different Media
2.3. Preparation of Precipitates
2.4. Recovery of Precipitates
2.5. X-ray Diffraction of Precipitates and API
2.6. Crystal Morphology of Precipitates and API
2.7. Fourier Transform Infrared Spectroscopy
2.8. Differential Scanning Calorimetry
2.9. Equilibrium Solubility of Precipitates and API in pH 6.5 Aqueous Buffer
2.10. Intrinsic Dissolution Rate of Precipitates and API
2.11. Permeability Assay of Precipitates and API in Different Media
2.12. Statistical Analyses
3. Results
3.1. Solubility of the API in Different Media
3.2. Recovery of Precipitates
3.3. X-ray Diffraction Results of Precipitates and API
3.4. Scanning Electron Microscopy Analyses
3.5. Fourier Transform Infrared Spectroscopy Analysis
3.6. Differential Scanning Calorimetry Analysis
3.7. Equilibrium Solubility of Different Precipitates and API in the Same Medium
3.8. Intrinsic Dissolution Rate
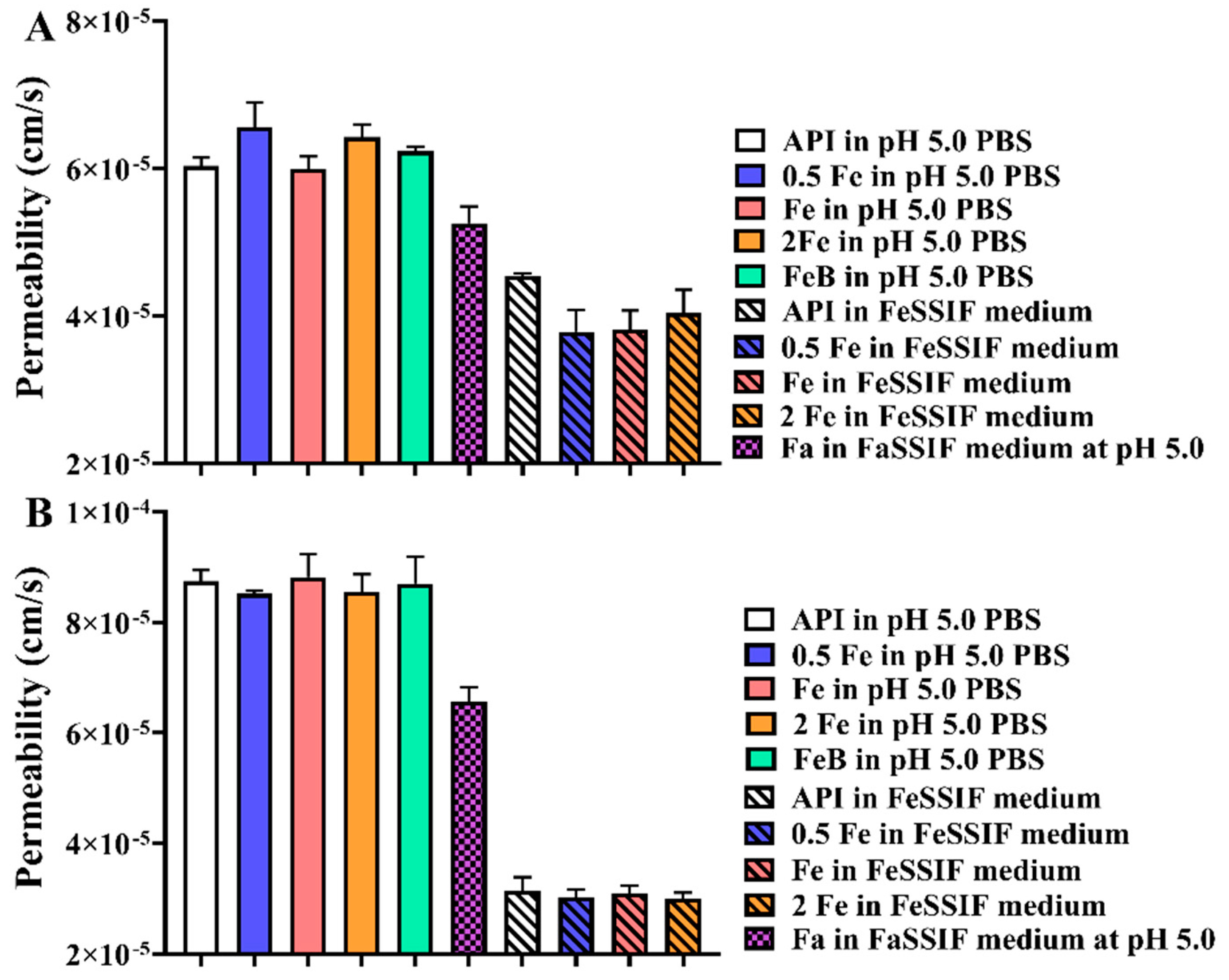
3.9. Permeability Assay
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| APIs | active pharmaceutical ingredients |
| DSC | differential scanning calorimetry |
| Fa | FaSSIF |
| FaB | FaSSIF buffer |
| Fe | FeSSIF |
| 0.5 Fe | double diluted FeSSIF medium |
| 2 Fe | double concentrated FeSSIF medium |
| FeB | FeSSIF buffer |
| FTIS | Fourier transform infrared spectroscope |
| GI | gastrointestinal |
| HPLC | high-performance liquid chromatography |
| IDR | intrinsic dissolution rate |
| PAMPA | Parallel artificial membrane permeability assay |
| PBPK | Physiologically based pharmacokinetic |
| PBS | phosphate buffer solution |
| SEM | scanning electron microscopy |
| XRD | X-ray diffraction |
References
- Li, M.; Zhao, P.; Pan, Y.; Wagner, C. Predictive Performance of Physiologically Based Pharmacokinetic Models for the Effect of Food on Oral Drug Absorption: Current Status. CPT Pharmacomet. Syst. Pharmacol. 2018, 7, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Riedmaier, A.E.; DeMent, K.; Huckle, J.; Bransford, P.; Stillhart, C.; Lloyd, R.; Alluri, R.; Basu, S.; Chen, Y.; Dhamankar, V.; et al. Use of Physiologically Based Pharmacokinetic (PBPK) Modeling for Predicting Drug-Food Interactions: An Industry Perspective. AAPS J. 2020, 22, 123. [Google Scholar] [CrossRef]
- Zhang, L.; Wu, F.; Lee, S.C.; Zhao, H.; Zhang, L. pH-dependent drug-drug interactions for weak base drugs: Potential implications for new drug development. Clin. Pharmacol. Ther. 2014, 96, 266–277. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Zhu, X.; Chen, Z.; Fan, C.H.; Kwan, H.S.; Wong, C.H.; Shek, K.Y.; Zuo, Z.; Lam, T.N. A Review of Food-Drug Interactions on Oral Drug Absorption. Drugs 2017, 77, 1833–1855. [Google Scholar] [CrossRef] [PubMed]
- Abend, A.; Curran, D.; Kuiper, J.; Lu, X.; Li, H.; Hermans, A.; Kotwal, P.; Diaz, D.A.; Cohen, M.J.; Zhang, L.; et al. Dissolution Testing in Drug Product Development: Workshop Summary Report. AAPS J. 2019, 21, 21. [Google Scholar] [CrossRef] [PubMed]
- Pentafragka, C.; Symillides, M.; McAllister, M.; Dressman, J.; Vertzoni, M.; Reppas, C. The impact of food intake on the luminal environment and performance of oral drug products with a view to in vitro and in silico simulations: A PEARRL review. J. Pharm. Pharmacol. 2019, 71, 557–580. [Google Scholar] [CrossRef] [Green Version]
- Hsieh, Y.L.; Ilevbare, G.A.; Van Eerdenbrugh, B.; Box, K.J.; Sanchez-Felix, M.V.; Taylor, L.S. pH-Induced precipitation behavior of weakly basic compounds: Determination of extent and duration of supersaturation using potentiometric titration and correlation to solid state properties. Pharm. Res. 2012, 29, 2738–2753. [Google Scholar] [CrossRef]
- Indulkar, A.S.; Box, K.J.; Taylor, R.; Ruiz, R.; Taylor, L.S. pH-Dependent Liquid-Liquid Phase Separation of Highly Supersaturated Solutions of Weakly Basic Drugs. Mol. Pharm. 2015, 12, 2365–2377. [Google Scholar] [CrossRef]
- Avdeef, A. Cocrystal solubility product analysis—Dual concentration-pH mass action model not dependent on explicit solubility equations. Eur. J. Pharm. Sci. 2017, 110, 2–18. [Google Scholar] [CrossRef]
- Pepin, X.; Dressman, J.; Parrott, N.; Delvadia, P.; Mitra, A.; Zhang, X.; Babiskin, A.; Kolhatkar, V.; Seo, P.; Taylor, L.S.; et al. In Vitro Biopredictive Methods: A Workshop Summary Report. J. Pharm. Sci. 2021, 110, 567–583. [Google Scholar] [CrossRef]
- Psachoulias, D.; Vertzoni, M.; Goumas, K.; Kalioras, V.; Beato, S.; Butler, J.; Reppas, C. Precipitation in and supersaturation of contents of the upper small intestine after administration of two weak bases to fasted adults. Pharm. Res. 2011, 28, 3145–3158. [Google Scholar] [CrossRef] [PubMed]
- Rubbens, J.; Brouwers, J.; Tack, J.; Augustijns, P. Gastrointestinal dissolution, supersaturation and precipitation of the weak base indinavir in healthy volunteers. Eur. J. Pharm. Biopharm. 2016, 109, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Hens, B.; Masuy, I.; Deloose, E.; Mols, R.; Tack, J.; Augustijns, P. Exploring the impact of real-life dosing conditions on intraluminal and systemic concentrations of atazanavir in parallel with gastric motility recording in healthy subjects. Eur. J. Pharm. Biopharm. 2020, 150, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Abend, A.; Heimbach, T.; Cohen, M.; Kesisoglou, F.; Pepin, X.; Suarez-Sharp, S. Dissolution and Translational Modeling Strategies Enabling Patient-Centric Drug Product Development: The M-CERSI Workshop Summary Report. AAPS J. 2018, 20, 60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, F.; Shah, H.; Li, M.; Duan, P.; Zhao, P.; Suarez, S.; Raines, K.; Zhao, Y.; Wang, M.; Lin, H.P.; et al. Biopharmaceutics Applications of Physiologically Based Pharmacokinetic Absorption Modeling and Simulation in Regulatory Submissions to the U.S. Food and Drug Administration for New Drugs. AAPS J. 2021, 23, 31. [Google Scholar] [CrossRef]
- Riethorst, D.; Mols, R.; Duchateau, G.; Tack, J.; Brouwers, J.; Augustijns, P. Characterization of Human Duodenal Fluids in Fasted and Fed State Conditions. J. Pharm. Sci. 2016, 105, 673–681. [Google Scholar] [CrossRef] [Green Version]
- Lu, J.; Ormes, D.O.; Lowinger, M.; Mann, A.K.P.; Xu, W.; Litster, J.D.; Taylor, L.S. Maintaining Supersaturation of Active Pharmaceutical Ingredient Solutions with Biologically Relevant Bile Salts. Cryst. Growth Des. 2017, 17, 2782–2791. [Google Scholar] [CrossRef]
- Bermejo, M.; Kuminek, G.; Al-Gousous, J.; Ruiz-Picazo, A.; Tsume, Y.; Garcia-Arieta, A.; González-Alvarez, I.; Hens, B.; Amidon, G.E.; Rodriguez-Hornedo, N.; et al. Exploring Bioequivalence of Dexketoprofen Trometamol Drug Products with the Gastrointestinal Simulator (GIS) and Precipitation Pathways Analyses. Pharmaceutics 2019, 11, 122. [Google Scholar] [CrossRef] [Green Version]
- Stappaerts, J.; Augustijns, P. Displacement of itraconazole from cyclodextrin complexes in biorelevant media: In vitro evaluation of supersaturation and precipitation behavior. Int. J. Pharm. 2016, 511, 680–687. [Google Scholar] [CrossRef]
- Bevernage, J.; Brouwers, J.; Brewster, M.E.; Augustijns, P. Evaluation of gastrointestinal drug supersaturation and precipitation: Strategies and issues. Int. J. Pharm. 2013, 453, 25–35. [Google Scholar] [CrossRef]
- Sodhi, I.; Sangamwar, A.T. Microarray Plate Method for Estimation of Precipitation Kinetics of Celecoxib under Biorelevant Conditions and Precipitate Characterization. Mol. Pharm. 2018, 15, 2423–2436. [Google Scholar] [CrossRef] [PubMed]
- Mutalik, S.; Usha, N.; Ranjith, A.K.; Umesh, S.; Musmade, P.; Anup, N. Preparation and physicochemical and preclinical evaluations of recrystallized celecoxib. PDA J. Pharm. Sci. Technol. 2007, 61, 362–374. [Google Scholar] [PubMed]
- Lijie, Y.; Hui, L.; Benxia, Y.; Zidong, Z. Determination of rivaroxaban tablets and related substances by HPLC. Chin. J. Pharm. Analysis. 2015, 35, 699–704. [Google Scholar]
- Ota, S.; Singh, A.; Srikanth, N.; Sreedhar, B.; Ruknuddin, G.; Dhiman, K.S. Chemical Characterization of an Ayurvedic Herbo-Mineral Formulation—Vasantakusumākara Rasa: A Potential Tool for Quality Assurance. Anc. Sci. Life 2017, 36, 207–214. [Google Scholar] [CrossRef]
- Kurakula, M.; El-Helw, A.M.; Sobahi, T.R.; Abdelaal, M.Y. Chitosan based atorvastatin nanocrystals: Effect of cationic charge on particle size, formulation stability, and in-vivo efficacy. Int. J. Nanomed. 2015, 10, 321–334. [Google Scholar] [CrossRef] [Green Version]
- Feng, D.; Peng, T.; Huang, Z.; Singh, V.; Shi, Y.; Wen, T.; Lu, M.; Quan, G.; Pan, X.; Wu, C. Polymer-Surfactant System Based Amorphous Solid Dispersion: Precipitation Inhibition and Bioavailability Enhancement of Itraconazole. Pharmaceutics 2018, 10, 53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Avdeef, A.; Tsinman, O. Miniaturized rotating disk intrinsic dissolution rate measurement: Effects of buffer capacity in comparisons to traditional wood’s apparatus. Pharm. Res. 2008, 25, 2613–2627. [Google Scholar] [CrossRef]
- Andersson, S.; Alvebratt, C.; Bevernage, J.; Bonneau, D.; da Costa Mathews, C.; Dattani, R.; Edueng, K.; He, Y.; Holm, R.; Madsen, C.; et al. Interlaboratory Validation of Small-Scale Solubility and Dissolution Measurements of Poorly Water-Soluble Drugs. J. Pharm. Sci. 2016, 105, 2864–2872. [Google Scholar] [CrossRef] [Green Version]
- Andersson, S.; Alvebratt, C.; Bergström, C. Controlled Suspensions Enable Rapid Determinations of Intrinsic Dissolution Rate and Apparent Solubility of Poorly Water-Soluble Compounds. Pharm. Res. 2017, 34, 1805–1816. [Google Scholar] [CrossRef] [Green Version]
- Bergström, C.; Box, K.; Holm, R.; Matthews, W.; McAllister, M.; Müllertz, A.; Rades, T.; Schäfer, K.J.; Teleki, A. Biorelevant intrinsic dissolution profiling in early drug development: Fundamental, methodological, and industrial aspects. Eur. J. Pharm. Biopharm. 2019, 139, 101–114. [Google Scholar] [CrossRef]
- Guo, M.; Wang, K.; Qiao, N.; Yardley, V.; Li, M. Investigating Permeation Behavior of Flufenamic Acid Cocrystals Using a Dissolution and Permeation System. Mol. Pharm. 2018, 15, 4257–4272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borbás, E.; Sinkó, B.; Tsinman, O.; Tsinman, K.; Kiserdei, É.; Démuth, B.; Balogh, A.; Bodák, B.; Domokos, A.; Dargó, G.; et al. Investigation and Mathematical Description of the Real Driving Force of Passive Transport of Drug Molecules from Supersaturated Solutions. Mol. Pharm. 2016, 13, 3816–3826. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Nguyen, K.; Kerns, E.; Yan, Z.; Yu, K.R.; Shah, P.; Jadhav, A.; Xu, X. Highly predictive and interpretable models for PAMPA permeability. Bioorg. Med. Chem. 2017, 25, 1266–1276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Dwyer, P.J.; Litou, C.; Box, K.J.; Dressman, J.B.; Kostewicz, E.S.; Kuentz, M.; Reppas, C. In vitro methods to assess drug precipitation in the fasted small intestine—A PEARRL review. J. Pharm. Pharmacol. 2019, 71, 536–556. [Google Scholar] [CrossRef] [Green Version]
- Martinez, M.N.; Amidon, G.L. A mechanistic approach to understanding the factors affecting drug absorption: A review of fundamentals. J. Clin. Pharmacol. 2002, 42, 620–643. [Google Scholar] [CrossRef] [Green Version]
- Jambhekar, S.S.; Breen, P.J. Drug dissolution: Significance of physicochemical properties and physiological conditions. Drug Discov. Today 2013, 18, 1173–1184. [Google Scholar] [CrossRef]
- Dalpiaz, A.; Pavan, B.; Ferretti, V. Can pharmaceutical co-crystals provide an opportunity to modify the biological properties of drugs. Drug Discov. Today 2017, 22, 1134–1138. [Google Scholar] [CrossRef]
- Fiolka, T.; Van Den Abeele, J.; Augustijns, P.; Arora, S.; Dressman, J. Biorelevant Two-Stage In Vitro Testing for rDCS Classification and in PBPK Modeling-Case Example Ritonavir. J. Pharm. Sci. 2020, 109, 2512–2526. [Google Scholar] [CrossRef]
- Indulkar, A.S.; Gao, Y.; Raina, S.A.; Zhang, G.; Taylor, L.S. Crystallization from Supersaturated Solutions: Role of Lecithin and Composite Simulated Intestinal Fluid. Pharm. Res. 2018, 35, 158. [Google Scholar] [CrossRef]
- Elkhabaz, A.; Sarkar, S.; Dinh, J.K.; Simpson, G.J.; Taylor, L.S. Variation in Supersaturation and Phase Behavior of Ezetimibe Amorphous Solid Dispersions upon Dissolution in Different Biorelevant Media. Mol. Pharm. 2018, 15, 193–206. [Google Scholar] [CrossRef]
- Brouwers, J.; Brewster, M.E.; Augustijns, P. Supersaturating drug delivery systems: The answer to solubility-limited oral bioavailability. J. Pharm. Sci. 2009, 98, 2549–2572. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Mosquera-Giraldo, L.I.; Ormes, J.D.; Higgins, J.D.; Taylor, L.S. Bile Salts as Crystallization Inhibitors of Supersaturated Solutions of Poorly Water-Soluble Compoun s. Cryst Growth Des. 2015, 15, 2593–2597. [Google Scholar] [CrossRef]
- Ahmed Elkhabaz, D.E.M.; Sreya Sarkar, J.B.; Garth, J.; Simpson, P.A.; Taylor, A.L.S. Crystallization Kinetics in Fasted-State Simulated and Aspirated Human Intestinal Fluids. Cryst Growth Des. 2021, 21, 2807–2820. [Google Scholar] [CrossRef]
- Lind, M.L.; Jacobsen, J.; Holm, R.; Müllertz, A. Development of simulated intestinal fluids containing nutrients as transport media in the Caco-2 cell culture model: Assessment of cell viability, monolayer integrity and transport of a poorly aqueous soluble drug and a substrate of efflux mechanisms. Eur. J. Pharm. Sci. 2007, 32, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Ingels, F.; Deferme, S.; Destexhe, E.; Oth, M.; Van den Mooter, G.; Augustijns, P. Simulated intestinal fluid as transport medium in the Caco-2 cell culture model. Int. J. Pharm. 2002, 232, 183–192. [Google Scholar] [CrossRef]
- Duane, W.C.; Wiegand, D.M.; Sievert, C.E. Bile acid and bile salt disrupt gastric mucosal barrier in the dog by different mechanisms. Am. J. Physiol. 1982, 242, G95–G99. [Google Scholar] [CrossRef] [PubMed]
- Patel, N.; Forbes, B.; Eskola, S.; Murray, J. Use of simulated intestinal fluids with Caco-2 cells and rat ileum. Drug Dev. Ind. Pharm. 2006, 32, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Pathak, S.M.; Ruff, A.; Kostewicz, E.S.; Patel, N.; Turner, D.B.; Jamei, M. Model-Based Analysis of Biopharmaceutic Experiments to Improve Mechanistic Oral Absorption Modeling: An Integrated in Vitro in Vivo Extrapolation Perspective Using Ketoconazole as a Model Drug. Mol. Pharm. 2017, 14, 4305–4320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arora, S.; Pansari, A.; Kilford, P.; Jamei, M.; Gardner, I.; Turner, D.B. Biopharmaceutic In Vitro In Vivo Extrapolation (IVIV_E) Informed Physiologically-Based Pharmacokinetic Model of Ritonavir Norvir Tablet Absorption in Humans Under Fasted and Fed State Conditions. Mol. Pharm. 2020, 17, 2329–2344. [Google Scholar] [CrossRef]







| Media | NaOH | NaH2PO4 | NaCl | CH3COOH | pH | Biorelevant Powder * |
|---|---|---|---|---|---|---|
| (g) | (g) | (g) | (g) | (g) | ||
| FaSSIF buffer (FaB) | 0.42 | 3.44 | 6.19 | - | 6.5 | - |
| FeSSIF buffer (FeB) | 4.04 | - | 11.87 | 8.65 | 5.0 | - |
| FaSSIF (Fa) | 0.42 | 3.44 | 6.19 | - | 6.5 | 2.24 |
| FeSSIF (Fe) | 4.04 | - | 11.87 | 8.65 | 5.0 | 11.2 |
| 0.5 × FeSSIF (0.5 Fe) | 4.04 | - | 11.87 | 8.65 | 5.0 | 5.60 |
| 2 × FeSSIF (2 Fe) | 4.04 | - | 11.87 | 8.65 | 5.0 | 22.4 |
| Model Drugs | pH 1.0 HCl | pH 5.0 PBS | pH 6.5 PBS | pH 8.0 PBS | FaSSIF (μg/mL) | FeSSIF (μg/mL) |
|---|---|---|---|---|---|---|
| (μg/mL) | (μg/mL) | (μg/mL) | (μg/mL) | |||
| Rivaroxaban | 6.84 (±0.20) | 4.85 (±0.11) | 5.85 (±0.02) | 5.87 (±0.04) | 6.17 (±0.13) | 10.6 (±0.14) |
| Drug-A | 42.9 (±0.47) | 11.9 (±0.12) | 11.6 (±0.17) | 11.2 (±0.16) | 12.3 (±0.30) | 13.8 (±0.85) |
| Model Drugs | Organic Solvent | FaSSIF Buffer | FeSSIF Buffer | FaSSIF | 0.5 × FeSSIF | FeSSIF | 2 × FeSSIF |
|---|---|---|---|---|---|---|---|
| Rivaroxaban | 98.7% (±1.59%) | 100% (±0.49%) | 99.0% (±0.96%) | 96.6% (±1.12%) | 98.1% (±1.32%) | 95.2% (±1.38%) | 99.6% (±1.16%) |
| Drug-A | 99.3% (±0.17%) | 99.6% (±0.40%) | 100% (±1.34%) | 101% (±0.91%) | 99. 8% (±1.01%) | 97.3% (±0.99%) | 98.2% (±0.10%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, M.; Wu, B.; Zhang, S.; Wang, L.; Hu, Q.; Liu, D.; Chen, X. Characterizing the Physicochemical Properties of Two Weakly Basic Drugs and the Precipitates Obtained from Biorelevant Media. Pharmaceutics 2022, 14, 330. https://doi.org/10.3390/pharmaceutics14020330
Zhang M, Wu B, Zhang S, Wang L, Hu Q, Liu D, Chen X. Characterizing the Physicochemical Properties of Two Weakly Basic Drugs and the Precipitates Obtained from Biorelevant Media. Pharmaceutics. 2022; 14(2):330. https://doi.org/10.3390/pharmaceutics14020330
Chicago/Turabian StyleZhang, Miao, Bin Wu, Shudong Zhang, Lin Wang, Qin Hu, Dongyang Liu, and Xijing Chen. 2022. "Characterizing the Physicochemical Properties of Two Weakly Basic Drugs and the Precipitates Obtained from Biorelevant Media" Pharmaceutics 14, no. 2: 330. https://doi.org/10.3390/pharmaceutics14020330






