Multi-Strain-Probiotic-Loaded Nanoparticles Reduced Colon Inflammation and Orchestrated the Expressions of Tight Junction, NLRP3 Inflammasome and Caspase-1 Genes in DSS-Induced Colitis Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Preparation of Probiotic Microorganisms
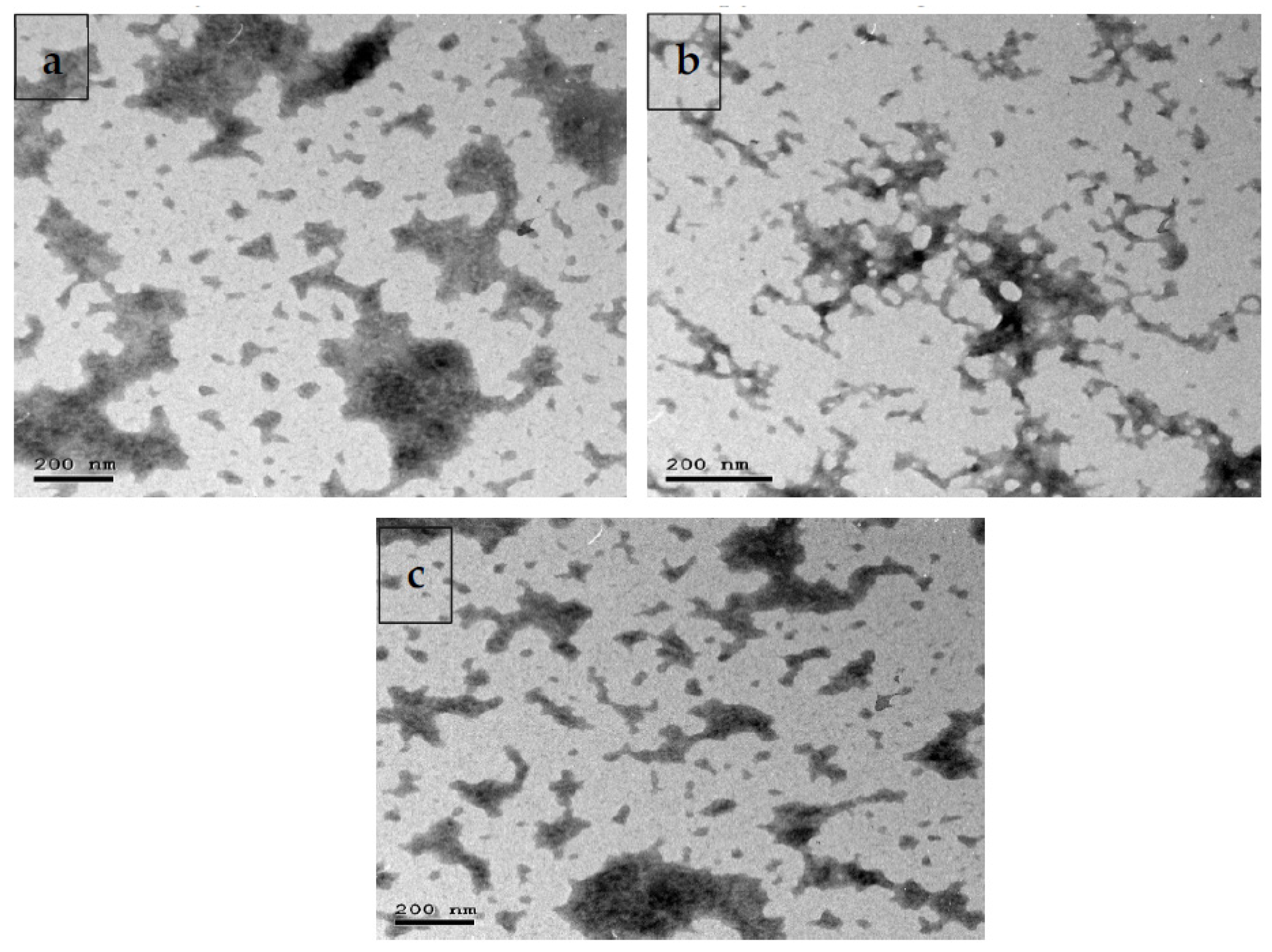
2.2. Formulation and Characterization of Multi-Strain-Probiotic-Loaded Nanoparticles
2.3. Survival of Assay of Probiotic-Cell-Loaded Nanoparticles in Bile Salt Solution and Incubation in Gastric and Intestinal Juice with and without Bile Salt
2.4. Experimental Animals and Colitis-Induced Model
2.5. Sampling
2.6. Scoring by Disease Activity Index (DAI)
2.7. Measurement of Hematological and Serum Indices
2.8. Measurement of Cytokines by Enzyme-Linked Immunosorbent Assay (ELISA)
2.9. Measurement of Colonic Myeloperoxidase and Nitric Oxide
2.10. Quantification of Fecal Calprotectin
2.11. Quantitative Real-Time PCR
2.12. Quantitative DNA-Based Analysis of Abundance of Colon Bacterial Populations
2.13. Histopathological Examination
2.14. Statistical Analysis
3. Results
3.1. Survival of Free and Loaded Multi-Strain Probiotics in Activated Gastric and Intestinal Juice
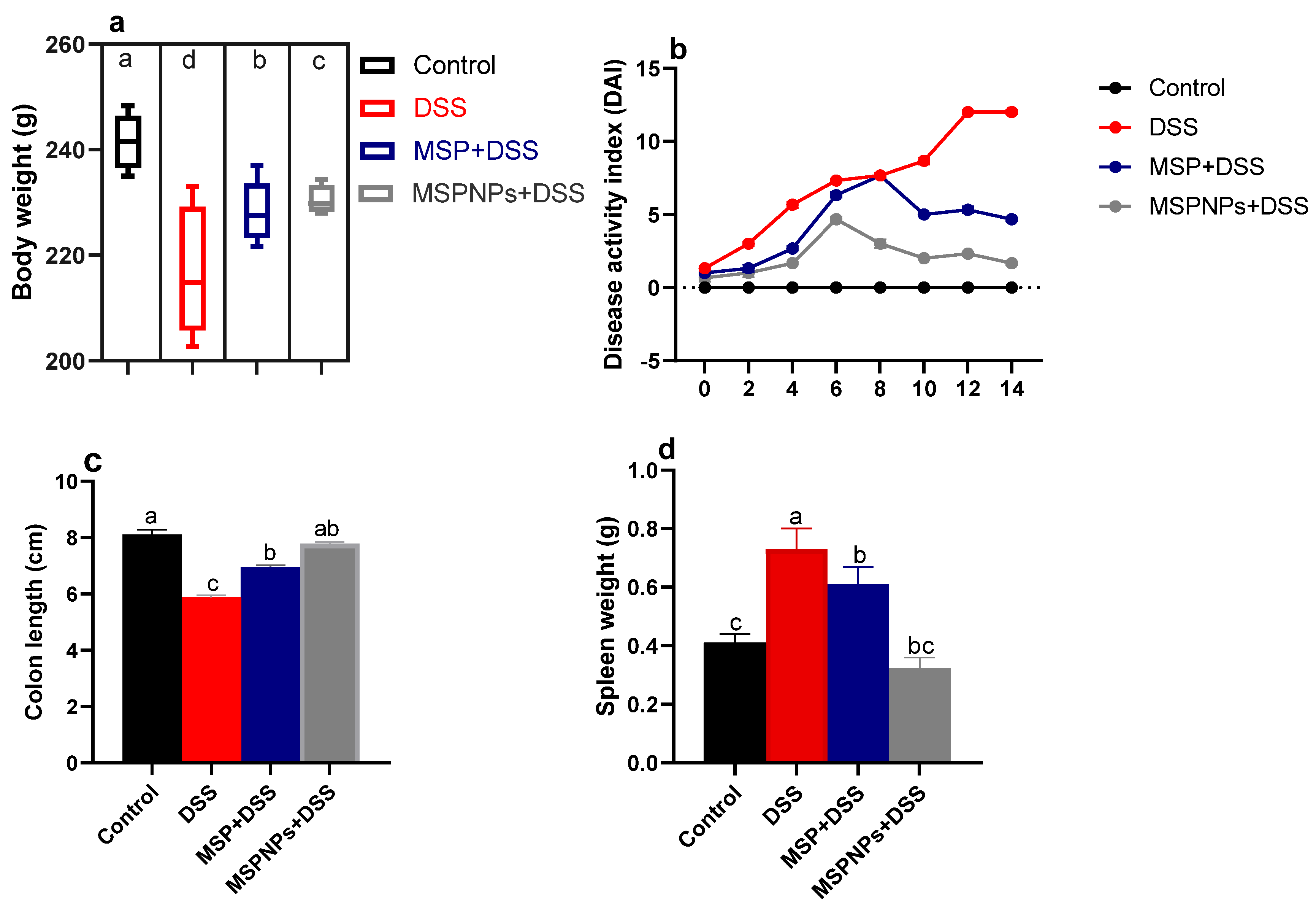
3.2. Effects of MSPNPs on Severity of Colon Injury
3.3. Hematological and Biochemical Estimation
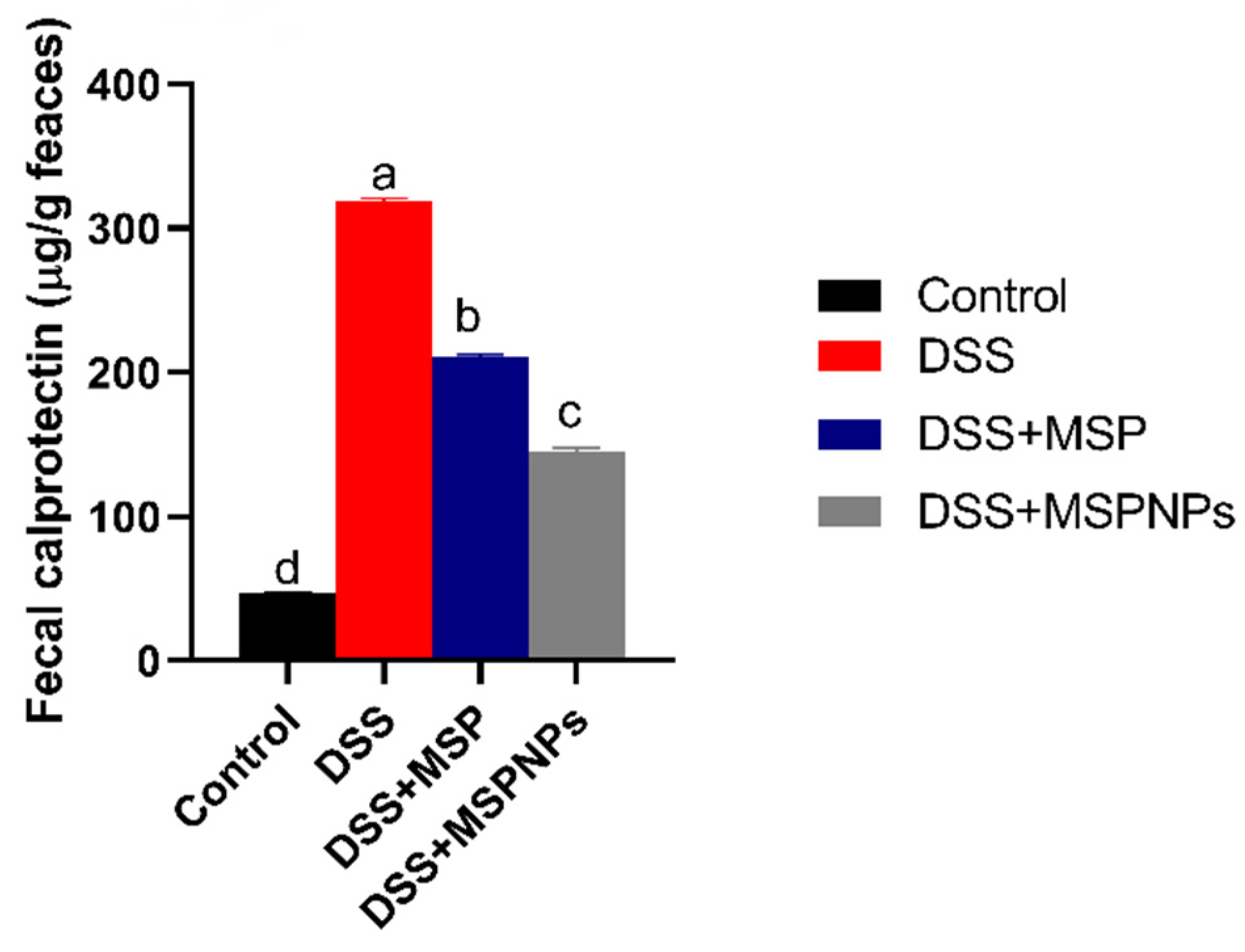
3.4. Assessment of Fecal Calprotectin Levels
3.5. Assessment of CRP Levels in Serum and of MPO and NO in Colonic Tissues
3.6. Quantification of Inflammatory Mediators in Colon by ELISA and Real-Time PCR
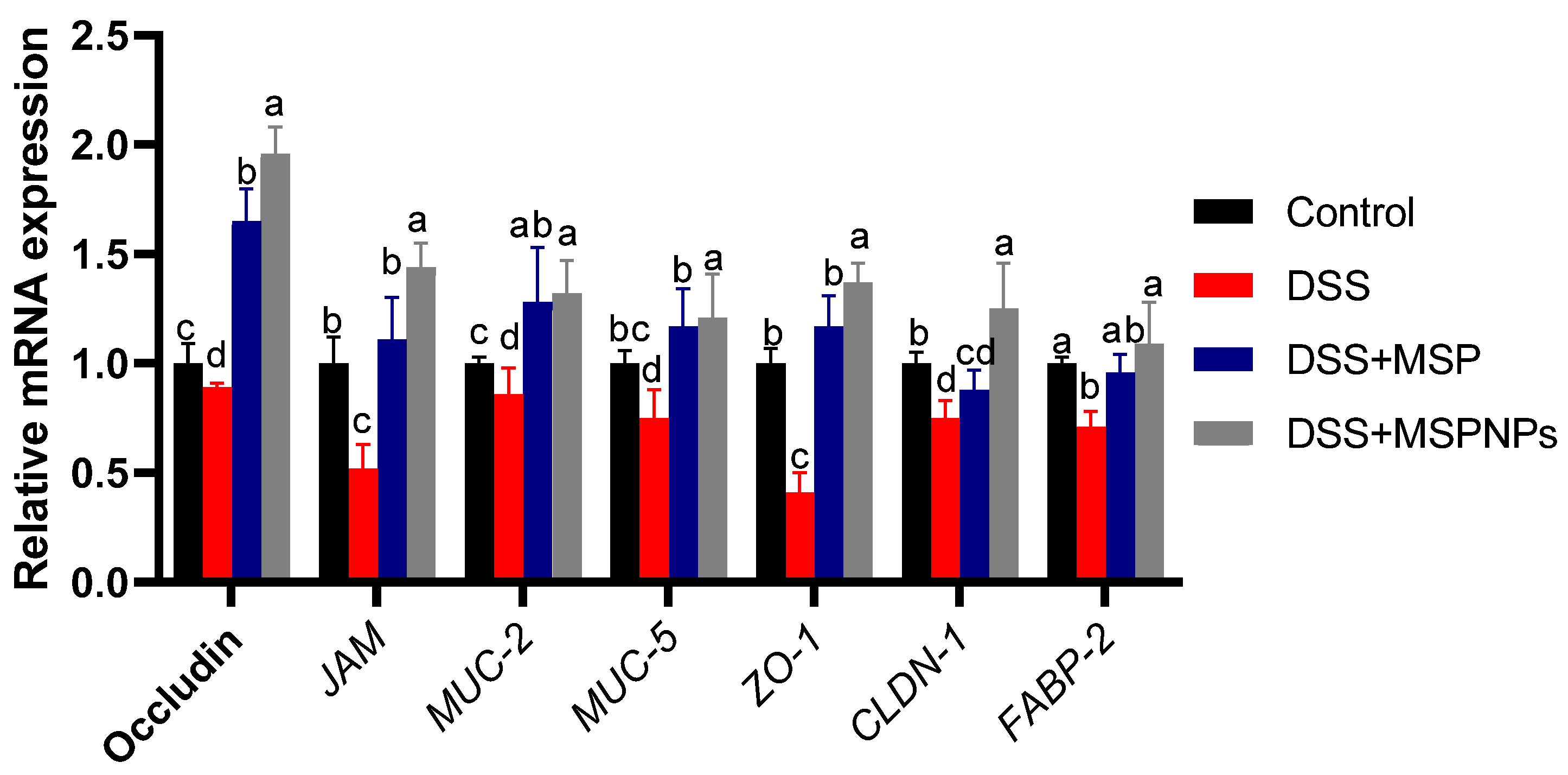
3.7. Tight Junction Protein Expression in Colitic Rats
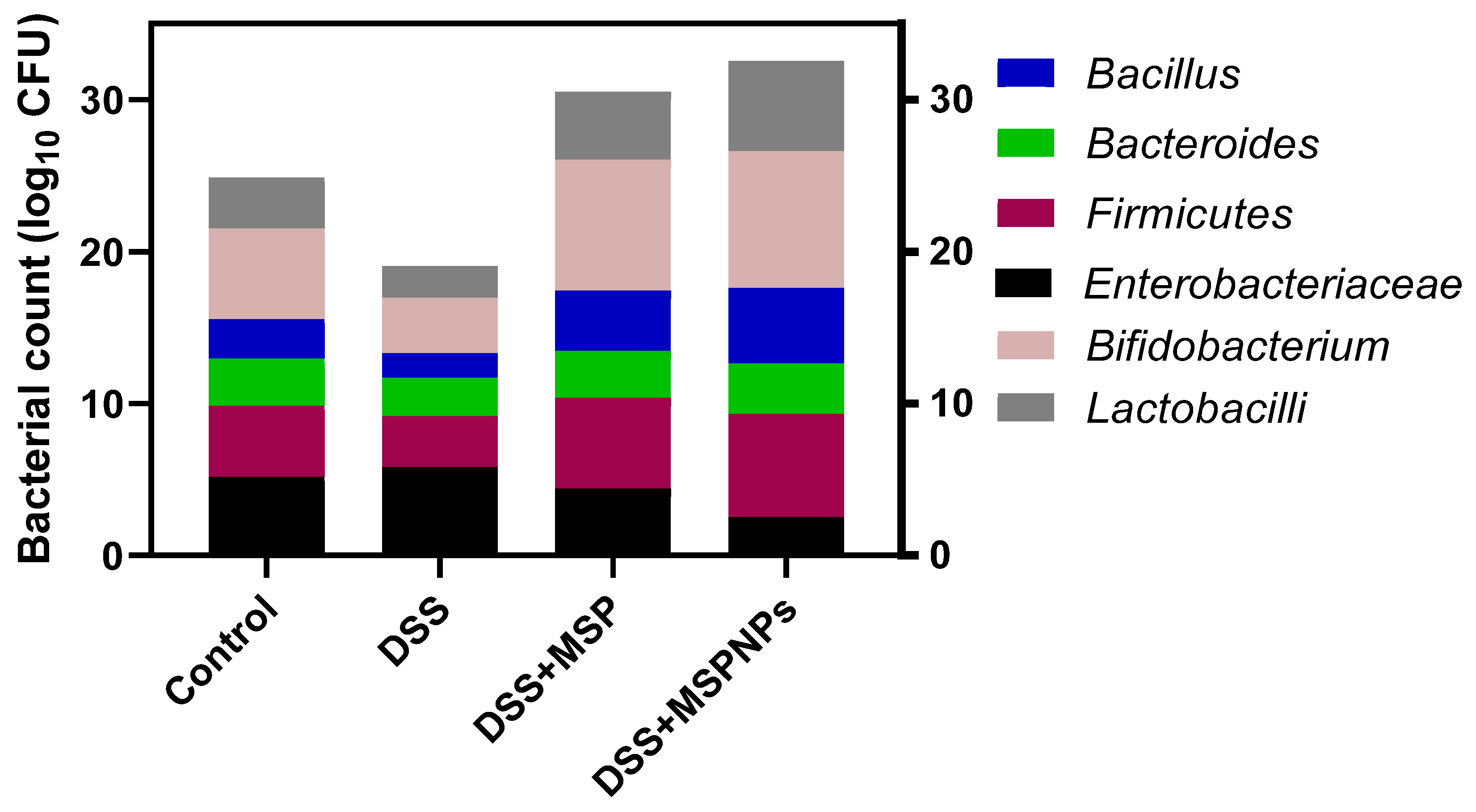
3.8. Analysis of Microbial Populations in Colon Contents
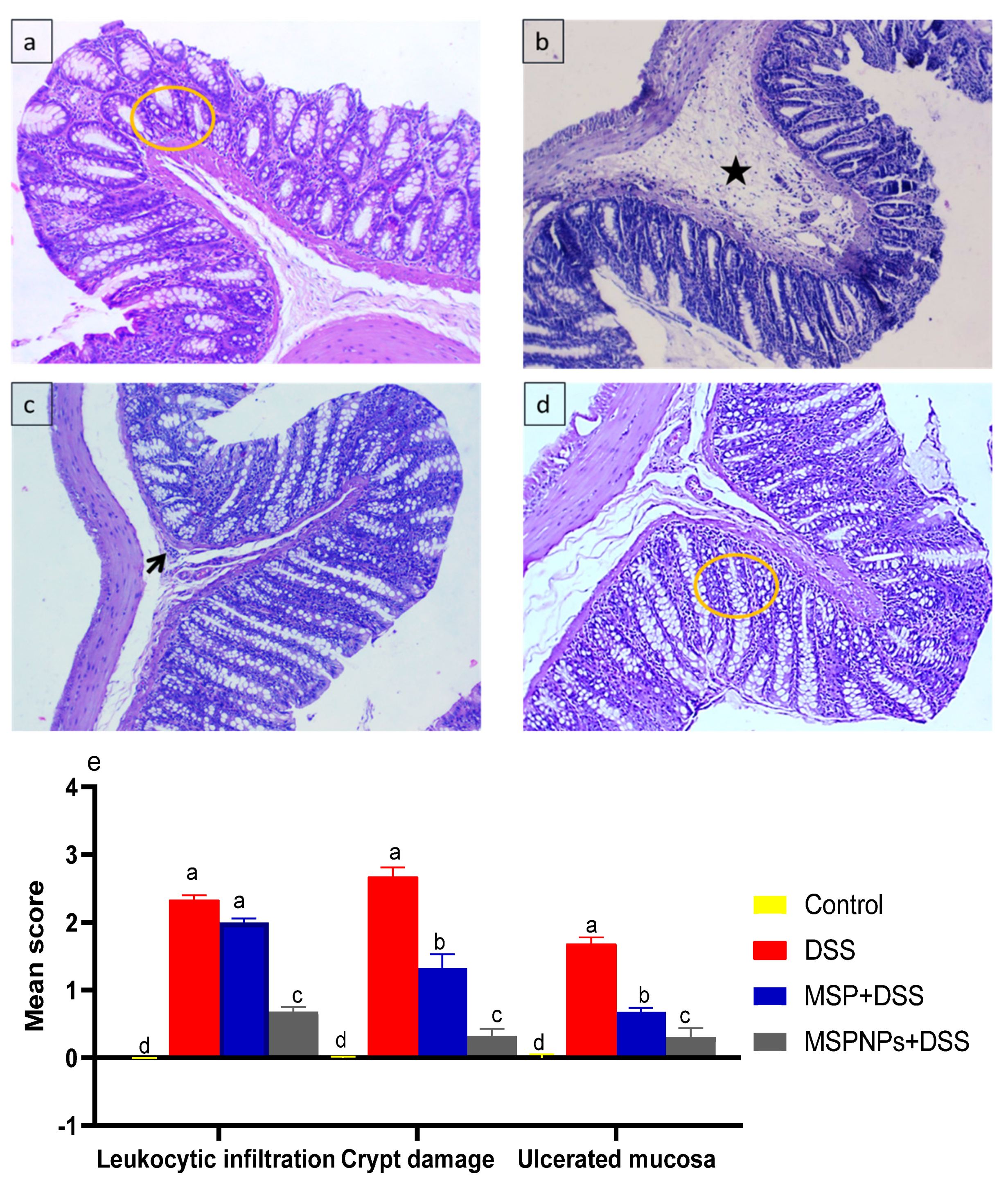
3.9. Histological Changes in the Colon
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cao, G.; Wang, K.; Li, Z.; Tao, F.; Xu, Y.; Lan, J.; Chen, G.; Yang, C. Bacillus amyloliquefaciens ameliorates dextran sulfate sodium-induced colitis by improving gut microbial dysbiosis in mice model. Front. Microbiol. 2019, 9, 3260. [Google Scholar] [CrossRef] [Green Version]
- Greten, F.R.; Grivennikov, S.I. Inflammation and cancer: Triggers, mechanisms, and consequences. Immunity 2019, 51, 27–41. [Google Scholar] [CrossRef]
- Kaplan, G.G.; Ng, S.C. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology 2017, 152, 313–321.e2. [Google Scholar] [CrossRef] [Green Version]
- Onizawa, M.; Nagaishi, T.; Kanai, T.; Nagano, K.-I.; Oshima, S.; Nemoto, Y.; Yoshioka, A.; Totsuka, T.; Okamoto, R.; Nakamura, T. Signaling pathway via TNF-α/NF-κB in intestinal epithelial cells may be directly involved in colitis-associated carcinogenesis. Am. J. Physiol.-Gastrointest. Liver Physiol. 2009, 296, G850–G859. [Google Scholar] [CrossRef]
- Sanchez-Muñoz, F.; Dominguez-Lopez, A.; Yamamoto-Furusho, J.K. Role of cytokines in inflammatory bowel disease. World J. Gastroenterol. WJG 2008, 14, 4280. [Google Scholar] [CrossRef]
- Chen, L.; Zhou, Z.; Yang, Y.; Chen, N.; Xiang, H. Therapeutic effect of imiquimod on dextran sulfate sodium-induced ulcerative colitis in mice. PLoS ONE 2017, 12, e0186138. [Google Scholar] [CrossRef] [Green Version]
- Zhen, Y.; Zhang, H. NLRP3 inflammasome and inflammatory bowel disease. Front. Immunol. 2019, 10, 276. [Google Scholar] [CrossRef] [Green Version]
- Kanneganti, T.-D. Inflammatory bowel disease and the NLRP3 inflammasome. N. Engl. J. Med. 2017, 377, 694–696. [Google Scholar] [CrossRef]
- Limdi, J.K. Dietary practices and inflammatory bowel disease. Indian J. Gastroenterol. 2018, 37, 284–292. [Google Scholar] [CrossRef] [Green Version]
- Abraham, C.; Cho, J. Interleukin-23/Th17 pathways and inflammatory bowel disease. Inflamm. Bowel Dis. 2009, 15, 1090–1100. [Google Scholar] [CrossRef]
- Shamoon, M.; Martin, N.M.; O’Brien, C.L. Recent advances in gut microbiota mediated therapeutic targets in inflammatory bowel diseases: Emerging modalities for future pharmacological implications. Pharmacol. Res. 2019, 148, 104344. [Google Scholar] [CrossRef]
- Boirivant, M.; Strober, W. The mechanism of action of probiotics. Curr. Opin. Gastroenterol. 2007, 23, 679–692. [Google Scholar] [CrossRef]
- Jampilek, J.; Kos, J.; Kralova, K. Potential of nanomaterial applications in dietary supplements and foods for special medical purposes. Nanomaterials 2019, 9, 296. [Google Scholar] [CrossRef] [Green Version]
- Krasaekoopt, W.; Bhandari, B.; Deeth, H. The influence of coating materials on some properties of alginate beads and survivability of microencapsulated probiotic bacteria. Int. Dairy J. 2004, 14, 737–743. [Google Scholar] [CrossRef]
- Wang, K.; Jin, X.; You, M.; Tian, W.; Leu, R.K.L.; Topping, D.L.; Conlon, M.A.; Wu, L.; Hu, F. Dietary propolis ameliorates dextran sulfate sodium-induced colitis and modulates the gut microbiota in rats fed a western diet. Nutrients 2017, 9, 875. [Google Scholar] [CrossRef]
- Tang, C.; Kamiya, T.; Liu, Y.; Kadoki, M.; Kakuta, S.; Oshima, K.; Hattori, M.; Takeshita, K.; Kanai, T.; Saijo, S. Inhibition of dectin-1 signaling ameliorates colitis by inducing Lactobacillus-mediated regulatory T cell expansion in the intestine. Cell Host Microbe 2015, 18, 183–197. [Google Scholar] [CrossRef] [Green Version]
- Hewitt, S. Manual of Veterinary Investigation: Laboratory Techniques; Ministry of Agriculture, Fisheries and Food (MAFF): London, UK, 1984. [Google Scholar]
- Krawisz, J.; Sharon, P.; Stenson, W. Quantitative assay for acute intestinal inflammation based on myeloperoxidase activity: Assessment of inflammation in rat and hamster models. Gastroenterology 1984, 87, 1344–1350. [Google Scholar] [CrossRef]
- Miranda, K.M.; Espey, M.G.; Wink, D.A. A rapid, simple spectrophotometric method for simultaneous detection of nitrate and nitrite. Nitric Oxide 2001, 5, 62–71. [Google Scholar] [CrossRef]
- Tøn, H.; Brandsnes, Ø.; Dale, S.; Holtlund, J.; Skuibina, E.; Schjønsby, H.; Johne, B. Improved assay for fecal calprotectin. Clin. Chim. Acta 2000, 292, 41–54. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Layton, A.; McKay, L.; Williams, D.; Garrett, V.; Gentry, R.; Sayler, G. Development of Bacteroides 16S rRNA gene TaqMan-based real-time PCR assays for estimation of total, human, and bovine fecal pollution in water. Appl. Environ. Microbiol. 2006, 72, 4214–4224. [Google Scholar] [CrossRef] [Green Version]
- Walter, J.; Hertel, C.; Tannock, G.W.; Lis, C.M.; Munro, K.; Hammes, W.P. Detection of Lactobacillus, Pediococcus, Leuconostoc, and Weissella species in human feces by using group-specific PCR primers and denaturing gradient gel electrophoresis. Appl. Environ. Microbiol. 2001, 67, 2578–2585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, X.; Xia, X.; Tang, R.; Zhou, J.; Zhao, H.; Wang, K. Development of a real-time PCR method for Firmicutes and Bacteroidetes in faeces and its application to quantify intestinal population of obese and lean pigs. Lett. Appl. Microbiol. 2008, 47, 367–373. [Google Scholar] [CrossRef]
- Bartosch, S.; Fite, A.; Macfarlane, G.T.; McMurdo, M.E. Characterization of bacterial communities in feces from healthy elderly volunteers and hospitalized elderly patients by using real-time PCR and effects of antibiotic treatment on the fecal microbiota. Appl. Environ. Microbiol. 2004, 70, 3575–3581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Requena, T.; Burton, J.; Matsuki, T.; Munro, K.; Simon, M.A.; Tanaka, R.; Watanabe, K.; Tannock, G.W. Identification, detection, and enumeration of human Bifidobacterium species by PCR targeting the transaldolase gene. Appl. Environ. Microbiol. 2002, 68, 2420–2427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Chen, D.; Yu, B.; He, J.; Yu, J.; Mao, X.; Wang, J.; Luo, J.; Huang, Z.; Cheng, G. Spray-dried chicken plasma improves intestinal digestive function and regulates intestinal selected microflora in weaning piglets. J. Anim. Sci. 2015, 93, 2967–2976. [Google Scholar] [CrossRef]
- Alkushi, A.; Abdelfattah-Hassan, A.; Eldoumani, H.; Elazab, S.T.; Mohamed, S.A.; Metwally, A.S.; S El-Shetry, E.; Saleh, A.A.; ElSawy, N.A.; Ibrahim, D. Probiotics-loaded nanoparticles attenuated colon inflammation, oxidative stress, and apoptosis in colitis. Sci. Rep. 2022, 12, 5116. [Google Scholar] [CrossRef]
- Ibrahim, D.; Abdelfattah-Hassan, A.; Arisha, A.H.; Abd El-Aziz, R.M.; Sherief, W.R.; Adil, S.H.; El Sayed, R.; Metwally, A.E. Impact of feeding anaerobically fermented feed supplemented with acidifiers on its quality and growth performance, intestinal villi and enteric pathogens of mulard ducks. Livest. Sci. 2020, 242, 104299. [Google Scholar] [CrossRef]
- Ibrahim, D.; Abdelfattah-Hassan, A.; Badawi, M.; Ismail, T.A.; Bendary, M.M.; Abdelaziz, A.M.; Mosbah, R.A.; Mohamed, D.I.; Arisha, A.H.; El-Hamid, M.I.A. Thymol nanoemulsion promoted broiler chicken’s growth, gastrointestinal barrier and bacterial community and conferred protection against Salmonella Typhimurium. Sci. Rep. 2021, 11, 7742. [Google Scholar] [CrossRef]
- Wirtz, S.; Neufert, C.; Weigmann, B.; Neurath, M.F. Chemically induced mouse models of intestinal inflammation. Nat. Protoc. 2007, 2, 541–546. [Google Scholar] [CrossRef]
- Simrén, M.; Tack, J. New treatments and therapeutic targets for IBS and other functional bowel disorders. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 589–605. [Google Scholar] [CrossRef] [PubMed]
- Simren, M.; Barbara, G.; Flint, H.J.; Spiegel, B.M.; Spiller, R.C.; Vanner, S.; Verdu, E.F.; Whorwell, P.J.; Zoetendal, E.G. Intestinal microbiota in functional bowel disorders: A Rome foundation report. Gut 2013, 62, 159–176. [Google Scholar] [CrossRef] [PubMed]
- Isaacs, K.; Herfarth, H. Role of probiotic therapy in IBD. Inflamm. Bowel Dis. 2008, 14, 1597–1605. [Google Scholar] [CrossRef] [PubMed]
- Hong, L.; Kim, W.-S.; Lee, S.-M.; Kang, S.-K.; Choi, Y.-J.; Cho, C.-S. Pullulan nanoparticles as prebiotics enhance the antibacterial properties of Lactobacillus plantarum through the induction of mild stress in probiotics. Front. Microbiol. 2019, 10, 142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.J.; Shajib, M.S.; Manocha, M.M.; Khan, W.I. Investigating intestinal inflammation in DSS-induced model of IBD. JoVE J. Vis. Exp. 2012, 1, 3678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yao, M.; Lu, Y.; Zhang, T.; Xie, J.; Han, S.; Zhang, S.; Fei, Y.; Ling, Z.; Wu, J.; Hu, Y. Improved functionality of Ligilactobacillus salivarius Li01 in alleviating colonic inflammation by layer-by-layer microencapsulation. NPJ Biofilms Microbiomes 2021, 7, 58. [Google Scholar] [CrossRef]
- Pandurangan, A.K.; Saadatdoust, Z.; Mohd. Esa, N.; Hamzah, H.; Ismail, A. Dietary cocoa protects against colitis-associated cancer by activating the N rf2/K eap1 pathway. BioFactors 2015, 41, 1–14. [Google Scholar] [CrossRef]
- Ali, A.A.; Abd Al Haleem, E.N.; Khaleel, S.A.-H.; Sallam, A.S. Protective effect of cardamonin against acetic acid-induced ulcerative colitis in rats. Pharmacol. Rep. 2017, 69, 268–275. [Google Scholar] [CrossRef]
- Masoodi, I.; Kochhar, R.; Dutta, U.; Vaishnavi, C.; Prasad, K.K.; Vaiphei, K.; Kaur, S.; Singh, K. Fecal lactoferrin, myeloperoxidase and serum C-reactive are effective biomarkers in the assessment of disease activity and severity in patients with idiopathic ulcerative colitis. J. Gastroenterol. Hepatol. 2009, 24, 1768–1774. [Google Scholar] [CrossRef]
- Hegazy, S.K.; El-Bedewy, M.M. Effect of probiotics on pro-inflammatory cytokines and NF-κB activation in ulcerative colitis. World J. Gastroenterol. WJG 2010, 16, 4145. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, X.; Dong, X.; Samie, M.; Li, X.; Clapham, D.; Ren, D.; Xu, H. TPC proteins are phosphoinositide-activated sodium-selective ion channels in endosomes and lysosomes. Cell 2012, 151, 372–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Celiberto, L.S.; Bedani, R.; Dejani, N.N.; Ivo de Medeiros, A.; Sampaio Zuanon, J.A.; Spolidorio, L.C.; Tallarico Adorno, M.A.; Amancio Varesche, M.B.; Carrilho Galvão, F.; Valentini, S.R. Effect of a probiotic beverage consumption (Enterococcus faecium CRL 183 and Bifidobacterium longum ATCC 15707) in rats with chemically induced colitis. PLoS ONE 2017, 12, e0175935. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, M.J.; Lee, J.-K.; Choi, J.W.; Lee, C.-S.; Sim, J.H.; Cho, C.-H.; Lee, K.-H.; Cho, I.-H.; Chung, M.-H.; Kim, H.-R. Interleukin-6 induces S100A9 expression in colonic epithelial cells through STAT3 activation in experimental ulcerative colitis. PLoS ONE 2012, 7, e38801. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Özşeker, B.; Şahin, C.; Özşeker, H.S.; Efe, S.C.; Kav, T.; Bayraktar, Y. The role of fecal calprotectin in evaluating intestinal involvement of Behçet’s disease. Dis. Markers 2016, 2016, 5423043. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tibble, J.; Bjarnason, I. Non-invasive investigation of inflammatory bowel disease. World J. Gastroenterol. 2001, 7, 460. [Google Scholar] [CrossRef]
- Loser, K.; Vogl, T.; Voskort, M.; Lueken, A.; Kupas, V.; Nacken, W.; Klenner, L.; Kuhn, A.; Foell, D.; Sorokin, L. The Toll-like receptor 4 ligands Mrp8 and Mrp14 are crucial in the development of autoreactive CD8+T cells. Nat. Med. 2010, 16, 713–717. [Google Scholar] [CrossRef]
- Gupta, R.C. Biomarkers in Toxicology; Academic Press: Cambridge, MA, USA, 2019. [Google Scholar]
- Aranda, C.J.; Ocón, B.; Arredondo-Amador, M.; Suárez, M.D.; Zarzuelo, A.; Chazin, W.J.; Martínez-Augustin, O.; Sanchez de Medina, F. Calprotectin protects against experimental colonic inflammation in mice. Br. J. Pharmacol. 2018, 175, 3797–3812. [Google Scholar] [CrossRef] [Green Version]
- McGuckin, M.A.; Eri, R.; Simms, L.A.; Florin, T.H.; Radford-Smith, G. Intestinal barrier dysfunction in inflammatory bowel diseases. Inflamm. Bowel Dis. 2009, 15, 100–113. [Google Scholar] [CrossRef] [Green Version]
- Guan, Q.; Zhang, J. Recent advances: The imbalance of cytokines in the pathogenesis of inflammatory bowel disease. Mediat. Inflamm. 2017, 2017, 4810258. [Google Scholar] [CrossRef] [Green Version]
- Nemeth, Z.H.; Bogdanovski, D.A.; Barratt-Stopper, P.; Paglinco, S.R.; Antonioli, L.; Rolandelli, R.H. Crohn’s disease and ulcerative colitis show unique cytokine profiles. Cureus 2017, 9, e1177. [Google Scholar] [CrossRef] [Green Version]
- Griet, M.; Zelaya, H.; Mateos, M.V.; Salva, S.; Juarez, G.E.; de Valdez, G.F.; Villena, J.; Salvador, G.A.; Rodriguez, A.V. Soluble factors from Lactobacillus reuteri CRL1098 have anti-inflammatory effects in acute lung injury induced by lipopolysaccharide in mice. PLoS ONE 2014, 9, e110027. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, K.-T.; Kim, J.-W.; Kim, S.-I.; Kim, S.; Nguyen, T.H.; Kang, C.-H. Antioxidant and Anti-Inflammatory Effect and Probiotic Properties of Lactic Acid Bacteria Isolated from Canine and Feline Feces. Microorganisms 2021, 9, 1971. [Google Scholar] [CrossRef] [PubMed]
- Niu, M.; Ying, Y.; Bartell, P.; Harvatine, K. The effects of feeding rations that differ in fiber and fermentable starch within a day on milk production and the daily rhythm of feed intake and plasma hormones and metabolites in dairy cows. J. Dairy Sci. 2017, 100, 187–198. [Google Scholar] [CrossRef] [PubMed]
- You, H.J.; Oh, D.-K.; Ji, G.E. Anticancerogenic effect of a novel chiroinositol-containing polysaccharide from Bifidobacterium bifidum BGN4. FEMS Microbiol. Lett. 2004, 240, 131–136. [Google Scholar] [CrossRef] [Green Version]
- Carroll, I.M.; Andrus, J.M.; Bruno-Bárcena, J.M.; Klaenhammer, T.R.; Hassan, H.M.; Threadgill, D.S. Anti-inflammatory properties of Lactobacillus gasseri expressing manganese superoxide dismutase using the interleukin 10-deficient mouse model of colitis. Am. J. Physiol.-Gastrointest. Liver Physiol. 2007, 293, G729–G738. [Google Scholar] [CrossRef] [Green Version]
- Chen, X.; Fu, Y.; Wang, L.; Qian, W.; Zheng, F.; Hou, X. Bifidobacterium longum and VSL# 3® amelioration of TNBS-induced colitis associated with reduced HMGB1 and epithelial barrier impairment. Dev. Comp. Immunol. 2019, 92, 77–86. [Google Scholar]
- Alard, J.; Peucelle, V.; Boutillier, D.; Breton, J.; Kuylle, S.; Pot, B.; Holowacz, S.; Grangette, C. New probiotic strains for inflammatory bowel disease management identified by combining in vitro and in vivo approaches. Benef. Microbes 2018, 9, 317–331. [Google Scholar] [CrossRef]
- Park, J.-S.; Choi, J.W.; Jhun, J.; Kwon, J.Y.; Lee, B.-I.; Yang, C.W.; Park, S.-H.; Cho, M.-L. Lactobacillus acidophilus improves intestinal inflammation in an acute colitis mouse model by regulation of Th17 and Treg cell balance and fibrosis development. J. Med. Food 2018, 21, 215–224. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Zhao, X.; Zhu, Y.; Ma, J.; Ma, H.; Zhang, H. Probiotic mixture protects dextran sulfate sodium-induced colitis by altering tight junction protein expressions and increasing Tregs. Mediat. Inflamm. 2018, 2018, 9416391. [Google Scholar] [CrossRef] [Green Version]
- Otte, J.-M.; Mahjurian-Namari, R.; Brand, S.; Werner, I.; Schmidt, W.E.; Schmitz, F. Probiotics regulate the expression of COX-2 in intestinal epithelial cells. Nutr. Cancer 2008, 61, 103–113. [Google Scholar] [CrossRef]
- Chávarri, M.; Marañón, I.; Ares, R.; Ibáñez, F.C.; Marzo, F.; del Carmen Villarán, M. Microencapsulation of a probiotic and prebiotic in alginate-chitosan capsules improves survival in simulated gastro-intestinal conditions. Int. J. Food Microbiol. 2010, 142, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Madsen, K.; Cornish, A.; Soper, P.; McKaigney, C.; Jijon, H.; Yachimec, C.; Doyle, J.; Jewell, L.; De Simone, C. Probiotic bacteria enhance murine and human intestinal epithelial barrier function. Gastroenterology 2001, 121, 580–591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maloy, K.J.; Powrie, F. Intestinal homeostasis and its breakdown in inflammatory bowel disease. Nature 2011, 474, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Edelblum, K.L.; Turner, J.R. The tight junction in inflammatory disease: Communication breakdown. Curr. Opin. Pharmacol. 2009, 9, 715–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsieh, C.Y.; Osaka, T.; Moriyama, E.; Date, Y.; Kikuchi, J.; Tsuneda, S. Strengthening of the intestinal epithelial tight junction by Bifidobacterium bifidum. Physiol. Rep. 2015, 3, e12327. [Google Scholar] [CrossRef] [Green Version]
- Sultana, R.; McBain, A.J.; O’Neill, C.A. Strain-dependent augmentation of tight-junction barrier function in human primary epidermal keratinocytes by Lactobacillus and Bifidobacterium lysates. Appl. Environ. Microbiol. 2013, 79, 4887–4894. [Google Scholar] [CrossRef] [Green Version]
- Miyauchi, E.; O’Callaghan, J.; Buttó, L.F.; Hurley, G.; Melgar, S.; Tanabe, S.; Shanahan, F.; Nally, K.; O’Toole, P.W. Mechanism of protection of transepithelial barrier function by Lactobacillus salivarius: Strain dependence and attenuation by bacteriocin production. Am. J. Physiol.-Gastrointest. Liver Physiol. 2012, 303, G1029–G1041. [Google Scholar] [CrossRef] [Green Version]
- Ohland, C.L.; MacNaughton, W.K. Probiotic bacteria and intestinal epithelial barrier function. Am. J. Physiol.-Gastrointest. Liver Physiol. 2010, 298, G807–G819. [Google Scholar] [CrossRef] [Green Version]
- Mennigen, R.; Nolte, K.; Rijcken, E.; Utech, M.; Loeffler, B.; Senninger, N.; Bruewer, M. Probiotic mixture VSL# 3 protects the epithelial barrier by maintaining tight junction protein expression and preventing apoptosis in a murine model of colitis. Am. J. Physiol.-Gastrointest. Liver Physiol. 2009, 296, G1140–G1149. [Google Scholar]
- Mao, L.; Kitani, A.; Strober, W.; Fuss, I.J. The role of NLRP3 and IL-1β in the pathogenesis of inflammatory bowel disease. Front. Immunol. 2018, 9, 2566. [Google Scholar] [CrossRef] [Green Version]
- Itani, S.; Watanabe, T.; Nadatani, Y.; Sugimura, N.; Shimada, S.; Takeda, S.; Otani, K.; Hosomi, S.; Nagami, Y.; Tanaka, F. NLRP3 inflammasome has a protective effect against oxazolone-induced colitis: A possible role in ulcerative colitis. Sci. Rep. 2016, 6, 39075. [Google Scholar] [CrossRef] [PubMed]
- Strowig, T.; Henao-Mejia, J.; Elinav, E.; Flavell, R. Inflammasomes in health and disease. Nature 2012, 481, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Cerretti, D.P.; Kozlosky, C.J.; Mosley, B.; Nelson, N.; Van Ness, K.; Greenstreet, T.A.; March, C.J.; Kronheim, S.R.; Druck, T.; Cannizzaro, L.A. Molecular cloning of the interleukin-1β converting enzyme. Science 1992, 256, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Bergsbaken, T.; Fink, S.L.; Cookson, B.T. Pyroptosis: Host cell death and inflammation. Nat. Rev. Microbiol. 2009, 7, 99–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kerur, N.; Veettil, M.V.; Sharma-Walia, N.; Bottero, V.; Sadagopan, S.; Otageri, P.; Chandran, B. IFI16 acts as a nuclear pathogen sensor to induce the inflammasome in response to Kaposi Sarcoma-associated herpesvirus infection. Cell Host Microbe 2011, 9, 363–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Llewellyn, A.; Foey, A. Probiotic modulation of innate cell pathogen sensing and signaling events. Nutrients 2017, 9, 1156. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Dong, Y.; Ye, M.; Jin, S.; Yang, J.; Joosse, M.E.; Sun, Y.; Zhang, J.; Lazarev, M.; Brant, S.R. The pathogenic role of NLRP3 inflammasome activation in inflammatory bowel diseases of both mice and humans. J. Crohn’s Colitis 2017, 11, 737–750. [Google Scholar] [CrossRef]
- Yin, H.; Guo, Q.; Li, X.; Tang, T.; Li, C.; Wang, H.; Sun, Y.; Feng, Q.; Ma, C.; Gao, C. Curcumin suppresses IL-1β secretion and prevents inflammation through inhibition of the NLRP3 inflammasome. J. Immunol. 2018, 200, 2835–2846. [Google Scholar] [CrossRef] [Green Version]
- Teixeira, L.; Kling, D.; Lorca, G.; Gonzalez, C. Lactobacillus johnsonii N6. 2 diminishes caspase-1 maturation in the gastrointestinal system of diabetes prone rats. Benef. Microbes 2018, 9, 527–539. [Google Scholar] [CrossRef]
- Luo, Z.; Xu, X.; Zhao, S.; Sho, T.; Luo, W.; Zhang, J.; Xu, W.; Hon, K.; Xu, J. Inclusion of microbe-derived antioxidant during pregnancy and lactation attenuates high-fat diet-induced hepatic oxidative stress, lipid disorders, and NLRP3 inflammasome in mother rats and offspring. Food Nutr. Res. 2019, 63. [Google Scholar] [CrossRef] [Green Version]
- Moroeanu, V.I.; Vamanu, E.; Paun, G.; Neagu, E.; Ungureanu, O.R.; Eremia, S.A.; Radu, G.-L.; Ionescu, R.; Pelinescu, D.R. Probiotic strains influence on infant microbiota in the in vitro colonic fermentation model GIS1. Indian J. Microbiol. 2015, 55, 423–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, S.; Zhao, D.; Cai, C.; Song, D.; Shen, J.; Xu, A.; Qiao, Y.; Ran, Z.; Zheng, Q. Low-dose penicillin exposure in early life decreases Th17 and the susceptibility to DSS colitis in mice through gut microbiota modification. Sci. Rep. 2017, 7, 43662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaura, E.; Nicu, E.A.; Krom, B.P.; Keijser, B.J. Acquiring and maintaining a normal oral microbiome: Current perspective. Front. Cell. Infect. Microbiol. 2014, 4, 85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, Z.-H.; Zhu, C.-X.; Quan, Y.-S.; Yang, Z.-Y.; Wu, S.; Luo, W.-W.; Tan, B.; Wang, X.-Y. Relationship between intestinal microbiota and ulcerative colitis: Mechanisms and clinical application of probiotics and fecal microbiota transplantation. World J. Gastroenterol. 2018, 24, 5. [Google Scholar] [CrossRef] [PubMed]
- Leccese, G.; Bibi, A.; Mazza, S.; Facciotti, F.; Caprioli, F.; Landini, P.; Paroni, M. Probiotic Lactobacillus and Bifidobacterium strains counteract adherent-invasive Escherichia coli (AIEC) virulence and hamper IL-23/Th17 axis in ulcerative colitis, but not in crohn’s disease. Cells 2020, 9, 1824. [Google Scholar] [CrossRef] [PubMed]
- Schierová, D.; Březina, J.; Mrázek, J.; Fliegerová, K.O.; Kvasnová, S.; Bajer, L.; Drastich, P. Gut microbiome changes in patients with active left-sided ulcerative colitis after fecal microbiome transplantation and topical 5-aminosalicylic acid therapy. Cells 2020, 9, 2283. [Google Scholar] [CrossRef]
- Martarelli, D.; Verdenelli, M.C.; Scuri, S.; Cocchioni, M.; Silvi, S.; Cecchini, C.; Pompei, P. Effect of a probiotic intake on oxidant and antioxidant parameters in plasma of athletes during intense exercise training. Curr. Microbiol. 2011, 62, 1689–1696. [Google Scholar] [CrossRef]
- Zhu, Y.; Wang, C.; Li, F. Impact of dietary fiber/starch ratio in shaping caecal microbiota in rabbits. Can. J. Microbiol. 2015, 61, 771–784. [Google Scholar] [CrossRef] [Green Version]
- Magrone, T.; Jirillo, E. The interplay between the gut immune system and microbiota in health and disease: Nutraceutical intervention for restoring intestinal homeostasis. Curr. Pharm. Des. 2013, 19, 1329–1342. [Google Scholar]
- Dzik, S. COVID-19 convalescent plasma: Now is the time for better science. Transfus. Med. Rev. 2020, 34, 141. [Google Scholar] [CrossRef]
- Cho, I.; Blaser, M.J. The human microbiome: At the interface of health and disease. Nat. Rev. Genet. 2012, 13, 260–270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, Y.; Liu, L.; Sun, Z.; Ji, Y.; Wang, D.; Mei, L.; Shen, P.; Li, Z.; Tang, S.; Zhang, H. Fucoidan as a marine-origin prebiotic modulates the growth and antibacterial ability of Lactobacillus rhamnosus. Int. J. Biol. Macromol. 2021, 180, 599–607. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.-C.; Tsai, S.-S.; Liu, L.-F.; Liu, Y.L.; Liu, H.-J.; Chuang, K.P. Effect of Arctium lappa L. in the dextran sulfate sodium colitis mouse model. World J. Gastroenterol. WJG 2010, 16, 4193. [Google Scholar] [CrossRef] [PubMed]
- Kiesler, P.; Fuss, I.J.; Strober, W. Experimental models of inflammatory bowel diseases. Cell. Mol. Gastroenterol. Hepatol. 2015, 1, 154–170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, S.; Ahmadi, S.; Nagpal, R.; Jain, S.; Mishra, S.P.; Kavanagh, K.; Zhu, X.; Wang, Z.; McClain, D.A.; Kritchevsky, S.B. Lipoteichoic acid from the cell wall of a heat killed Lactobacillus paracasei D3-5 ameliorates aging-related leaky gut, inflammation and improves physical and cognitive functions: From C. elegans to mice. Geroscience 2020, 42, 333–352. [Google Scholar] [CrossRef] [PubMed]

| Weight Loss (%) | Stool Consistency | Gross Bleeding | |
|---|---|---|---|
| Scores | 0 = None | 0 = Normal | 0 = Negative |
| 1 = 0.1–5% | |||
| 2 = 5–10% | 2 = Loose stool | 2 = Hemoccult | |
| 3 = 10–20% | |||
| 4 = >20% | 4 = Diarrhea | 4 = Gross bleeding |
| Target Gene | Primer Sequence (5′–3′) | Accession No./Reference |
|---|---|---|
| OCCLUDIN | F-CTGTCTATGCTCGTCATCG R-CATTCCCGATCTAATGACGC | NM-031329 |
| JAM | F-GCTCAGCC ATACAGCAAATCC R-GGGAGTCGGGCAAT CATCAG | NM_017232 |
| MUC-2 | F-CAGAGTGCATCAGTGGCTGT R-CCCGTCGAAGGTGATGTAGT | XM_039101270.1 |
| MUC-5 | F-AACTCTGCCCACCACAAG R-TGCCATCTATCCAATCAGTCCAAT | XM_039101269.1 |
| ZO-1 | F-AGCGAAGCCACCTGAAGATA R-GATGGCCAGCAGGAATATGT | NM-001106266 |
| CLDN-2 | F-TCTGGATGGAGTGTGCGAC R-AGTGGCAAGAGGCTGGGC | NM-001106846 |
| FABP-2 | TGACGATCACACAGGAAGGA CCAGAAATCTCTCGGACAGC | XM_032897378.1 |
| IL-1β | F-TGACAGACCCCAAAAGATTAAGG R-CTCATCTGGACAGCCCAAGTC | NM_031512.2 |
| IL-6 | F-CCACCAGGAACGAAAGTCAAC R-TTGCGGAGAGAAACTTCATAGCT | NM_012589.2 |
| IL-18 | F- ATGGCTGCCATGTCAGAAGA R-TTGTTAAGCTTATAAATCATGCGGCCTCAGG | XM_039080945.1 |
| IL-10 | F-GCCCAGAAATCAAGGAGCATT R-CAGCTGTATCCAGAGGGTCTTCA | L02926.1 |
| TNFα | F-CAGCCGATTTGCCATTTCA R-AGGGCTCTTGATGGCAGAGA | L19123.1 |
| TLR2 | F-CGCTTCCTGAACTTGTCC R-GGTTGTCACCTGCTTCCA | XM_008761102.3 |
| TLR9 | F-CCGAAGACCTAGCCAACCT R-TGATCACAGCGACGGCAATT | XM_032911318.1 |
| Caspase-1 | F-GTGTTGCAGATAATGAGGGC R-AAGGTCCTGAGGGCAAAGAG | NM_012762.3 |
| NLRP3 inflammasome | F-CCAGGGCTCTGTTCATTG R-CCTTGGCTTTCACTTCG | XM_039085397.1 |
| β-actin | F-CGCAGTTGGTTGGAGCAAA R-ACAATCAAAGTCCTCAGCCACAT | V01217.1 |
| GAPDH | F-TGCTGGTGCTGAGTATGTCG-3′ R-TTGAGAGCAATGCCAGCC-3′ | NM_017008 |
| Bacteroides spp. | F-GAG AGG AAG GTC CCC CAC R-CGC TAC TTG GCT GGT TCA G | Layton, McKay, Williams, Garrett, Gentry and Sayler [22] |
| Lactobacillus | F-AGCAGTAGGGAATCTTCCA R-CACCGCTACACATGGAG | [23] |
| Firmicutes spp. | F-GGAGYATGTGGTTTAATTCGAAGCA R-AGCTGACGACAACCATGCAC | Guo, Xia, Tang, Zhou, Zhao and Wang [24] |
| Enterobacteriaceae | F-CATTGACGTTACCCGCAGAAGAAGC R-CTCTACGAGACTCAAGCTTGC | Bartosch, Fite, Macfarlane and McMurdo [25] |
| Bifidobacterium spp. | F-GCG TCC GCT GTG GGC R-CTT CTC CGG CATGGT GTTG | Requena, Burton, Matsuki, Munro, Simon, Tanaka, Watanabe and Tannock [26] |
| Bacillus spp. | F-GCA ACG AGC GCA ACC CTT GA R-TCA TCC CCA CCT TCC GGT | Zhang, Chen, Yu, He, Yu, Mao, Wang, Luo, Huang and Cheng [27] |
| No. of Survival Cells (CFU/mL)/min | ||||
|---|---|---|---|---|
| 30 | 60 | 90 | 120 | |
| Free Lactobacillus acidophilus | 9.2 ± 0.21 × 109 a | 8.8 ± 0.21 × 109 ab | 8.3 ± 0.15 × 108 b | 6.1 ± 0.22 × 105 c |
| Lactobacillus acidophilus double-coated with nanoparticles | 9.8 ± 0.20 × 109 a | 9.1 ± 0.11 × 109 b | 8.4 ± 0.17 × 108 c | 5.8 ± 0.20 × 107 d |
| Free Bifidobacterium bifidum | 8.3 ± 0.10 × 108 a | 8.1 ± 0.25 × 107 b | 6.9 ± 0.3 × 106 c | 5.1 ± 0.21 × 106 d |
| Bifidobacterium bifidum double-coated with nanoparticles | 8.9 ± 0.17 × 109 a | 8.1 ± 0.13 × 109 ab | 8.9 ± 0.19 × 108 b | 7.5 ± 0.29 × 107 c |
| Free Bacillus amyloliquefaciens | 7.5 ± 0.22 × 109 a | 7.1 ± 0.3 × 108 b | 6.7 ± 0.24 × 108 bc | 6.1 ± 0.11 × 107 c |
| Bacillus amyloliquefaciens double-coated with nanoparticles | 8.6 ± 0.22 × 109 a | 7.9 ± 0.24 × 109 a | 7.1 ± 0.19 × 108 ab | 6.8 ± 0.22 × 108 b |
| Parameter | Control | DSS | DSS + MSPs | DSS + MSPNPs | p-Value | SEM |
|---|---|---|---|---|---|---|
| ALT (U/L) | 46.23 c | 90.14 a | 50.33 b | 48.22 c | 0.02 | 0.23 |
| AST(U/L) | 23.29 d | 49.44 a | 29.86 b | 24.22 cd | 0.03 | 0.28 |
| Urea | 32.69 d | 50.25 a | 44.47 b | 35.51 c | 0.04 | 0.34 |
| Creatinine | 1.05 d | 3.3 a | 1.90 b | 1.63 c | 0.02 | 0.08 |
| RBCs (×106/μL) | 11.33 a | 7.23 c | 9.25 b | 10.49 ab | <0.001 | 0.13 |
| Hb (g/dL) | 12.93 a | 8.20 c | 8.75 c | 11.53 b | <0.001 | 0.17 |
| MPO (u/g tissue) | 2.10 d | 14.36 a | 7.63 b | 4.27 c | <0.001 | 0.29 |
| CRP (mg/L) | 0.85 d | 18.39 a | 10.36 b | 4.33 c | <0.001 | 0.30 |
| NO (nmol/g tissue) | 178.36 c | 698.25 a | 386.32 b | 365.14 b | 0.03 | 0.39 |
| TNF-α | 25.36 d | 77.39 a | 32.36 b | 29.36 cd | 0.02 | 0.24 |
| IFNγ | 40.23 d | 83.39 a | 69.32 b | 46.31 c | <0.001 | 0.34 |
| IL-6 | 12.37 d | 36.98 a | 25.47 b | 20.36 c | <0.01 | 0.09 |
| IL-10 | 280.36 c | 789.36 a | 546.32 b | 569.36 b | <0.01 | 0.43 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkushi, A.G.; Elazab, S.T.; Abdelfattah-Hassan, A.; Mahfouz, H.; Salem, G.A.; Sheraiba, N.I.; Mohamed, E.A.A.; Attia, M.S.; El-Shetry, E.S.; Saleh, A.A.; et al. Multi-Strain-Probiotic-Loaded Nanoparticles Reduced Colon Inflammation and Orchestrated the Expressions of Tight Junction, NLRP3 Inflammasome and Caspase-1 Genes in DSS-Induced Colitis Model. Pharmaceutics 2022, 14, 1183. https://doi.org/10.3390/pharmaceutics14061183
Alkushi AG, Elazab ST, Abdelfattah-Hassan A, Mahfouz H, Salem GA, Sheraiba NI, Mohamed EAA, Attia MS, El-Shetry ES, Saleh AA, et al. Multi-Strain-Probiotic-Loaded Nanoparticles Reduced Colon Inflammation and Orchestrated the Expressions of Tight Junction, NLRP3 Inflammasome and Caspase-1 Genes in DSS-Induced Colitis Model. Pharmaceutics. 2022; 14(6):1183. https://doi.org/10.3390/pharmaceutics14061183
Chicago/Turabian StyleAlkushi, Abdullah Glil, Sara T. Elazab, Ahmed Abdelfattah-Hassan, Hala Mahfouz, Gamal A. Salem, Nagwa I. Sheraiba, Eman A. A. Mohamed, Mai S. Attia, Eman S. El-Shetry, Ayman A. Saleh, and et al. 2022. "Multi-Strain-Probiotic-Loaded Nanoparticles Reduced Colon Inflammation and Orchestrated the Expressions of Tight Junction, NLRP3 Inflammasome and Caspase-1 Genes in DSS-Induced Colitis Model" Pharmaceutics 14, no. 6: 1183. https://doi.org/10.3390/pharmaceutics14061183







