Design, Manufacturing, Characterization and Evaluation of Lipid Nanocapsules to Enhance the Biopharmaceutical Properties of Efavirenz
Abstract
:1. Introduction
2. Materials and Methods
2.1. Material
2.1.1. Chemical
2.1.2. Instrument
2.2. Methods
2.2.1. Quantitative Determination of Efavirenz
2.2.2. Solubility Assessment of Efavirenz
2.2.3. Design and Optimization of Lipid Nanocapsules
I-Optimal Mixture Design and Statistical Optimization
Model Optimization and Confirmation
2.2.4. Preparation of Lipid Nanocapsules
2.2.5. Characterization
Droplet Size, Polydispersity Index and Zeta Potential
Encapsulation Efficacy and Drug Loading Capacity
Differential Scanning Calorimetry
X-ray Diffraction
Fourier Transform Infrared Spectroscopy
Energy-Dispersive X-ray Spectroscopy
2.2.6. In Vitro Release
2.2.7. Statistical Analysis
3. Results and Discussion
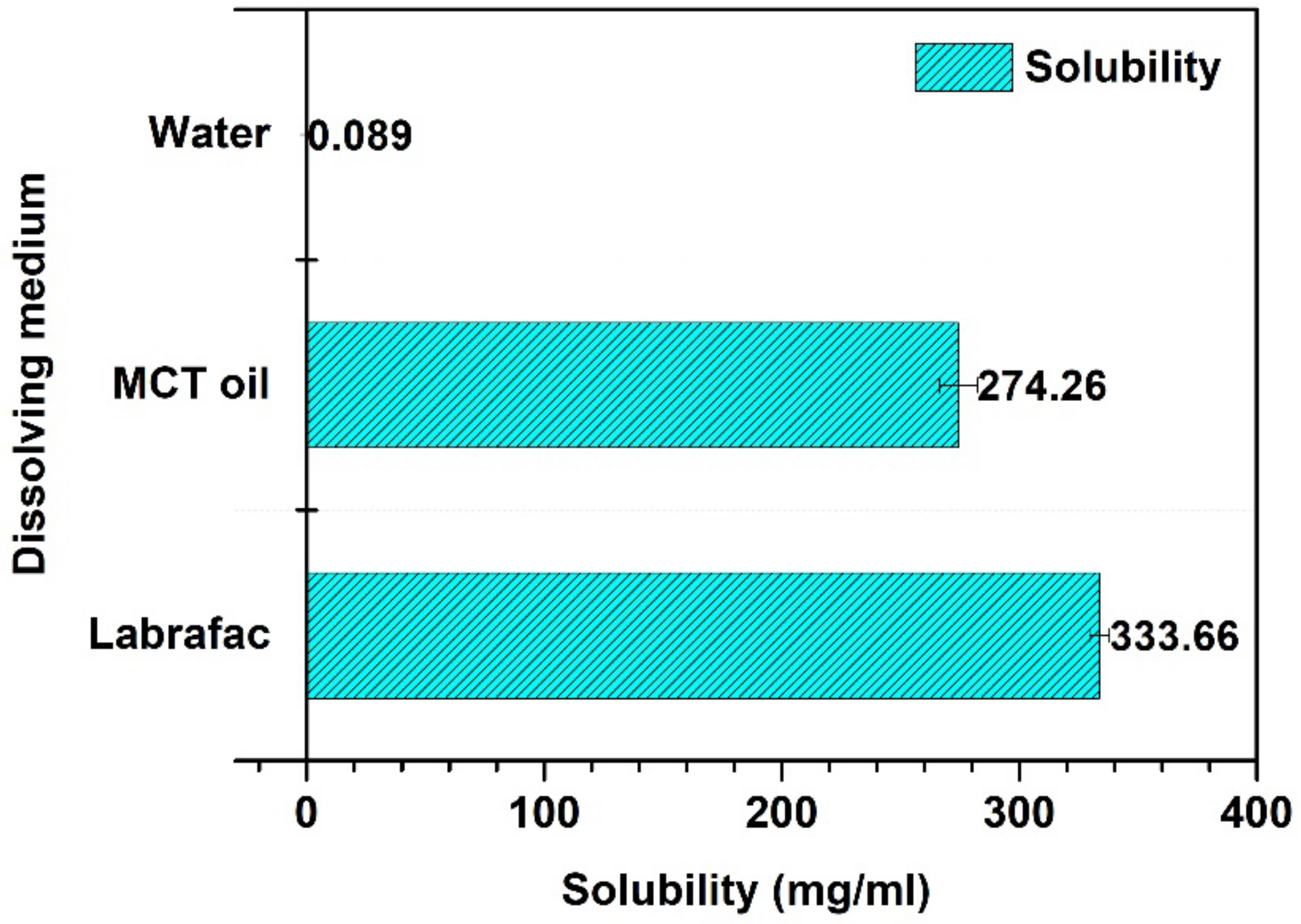
3.1. Solubility Assessment of Efavirenz
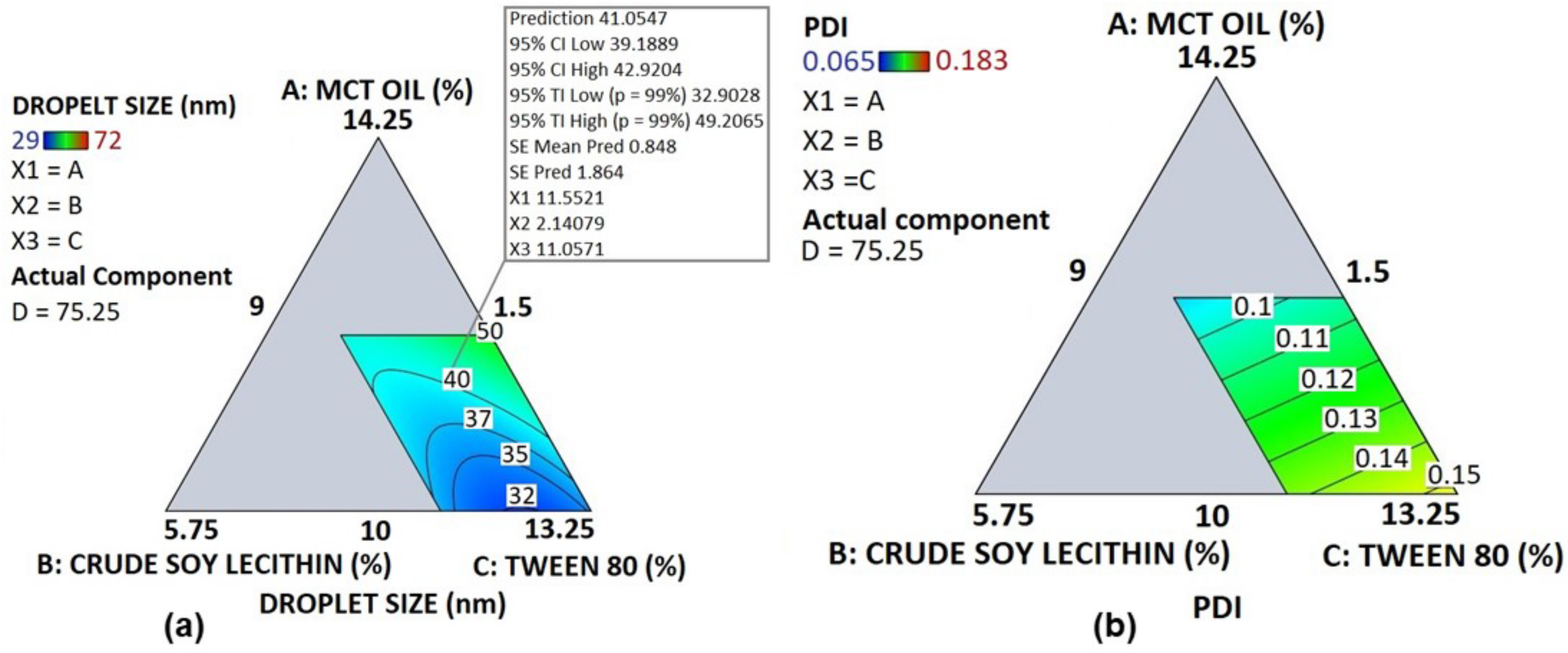
3.2. Statistical Analysis and Optimization of Lipid Nanocapsules
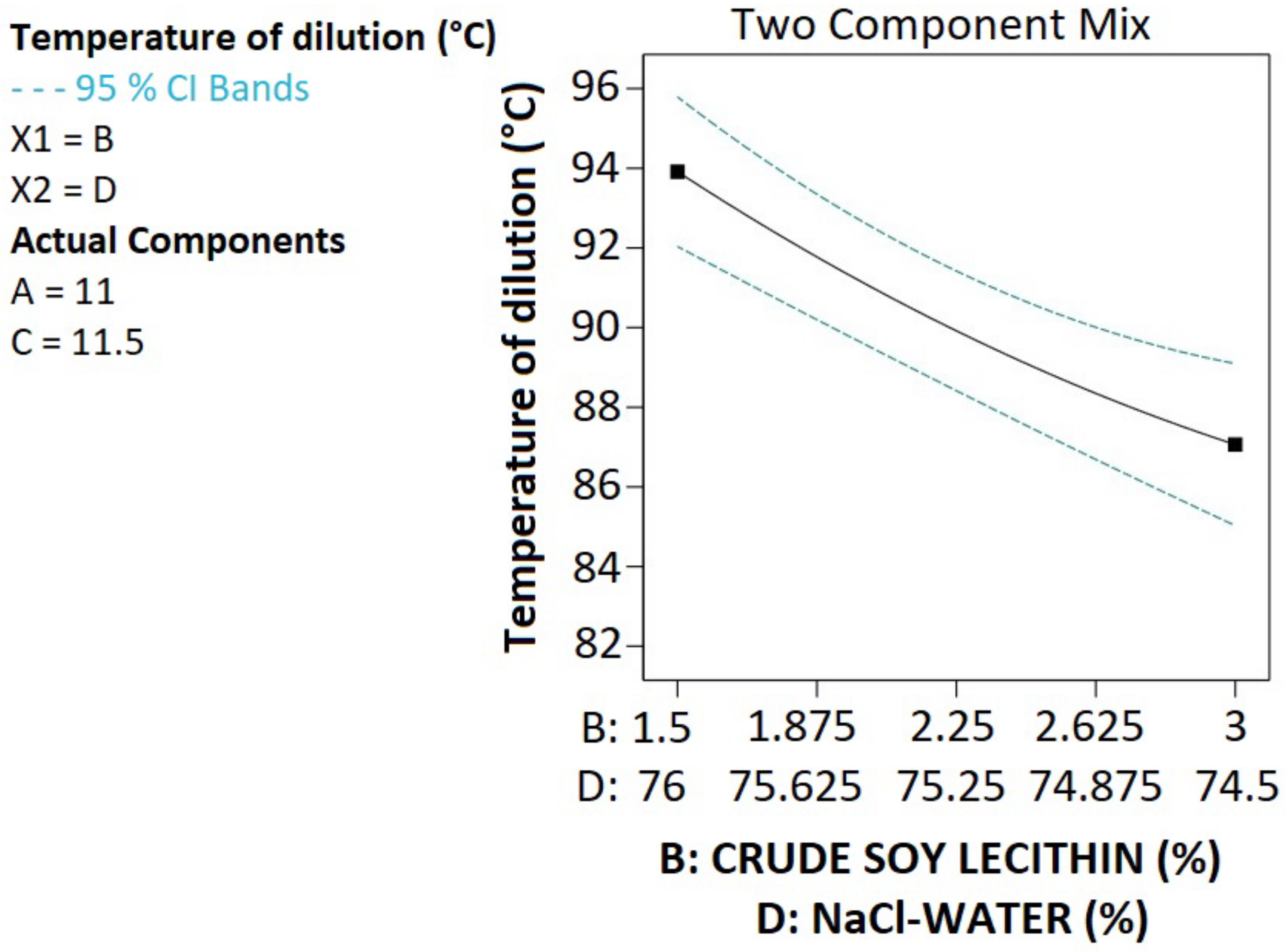
3.3. Droplet Size, Polydispersity Index, Zeta Potential and Temperature of Dilution
3.4. Model Optimization
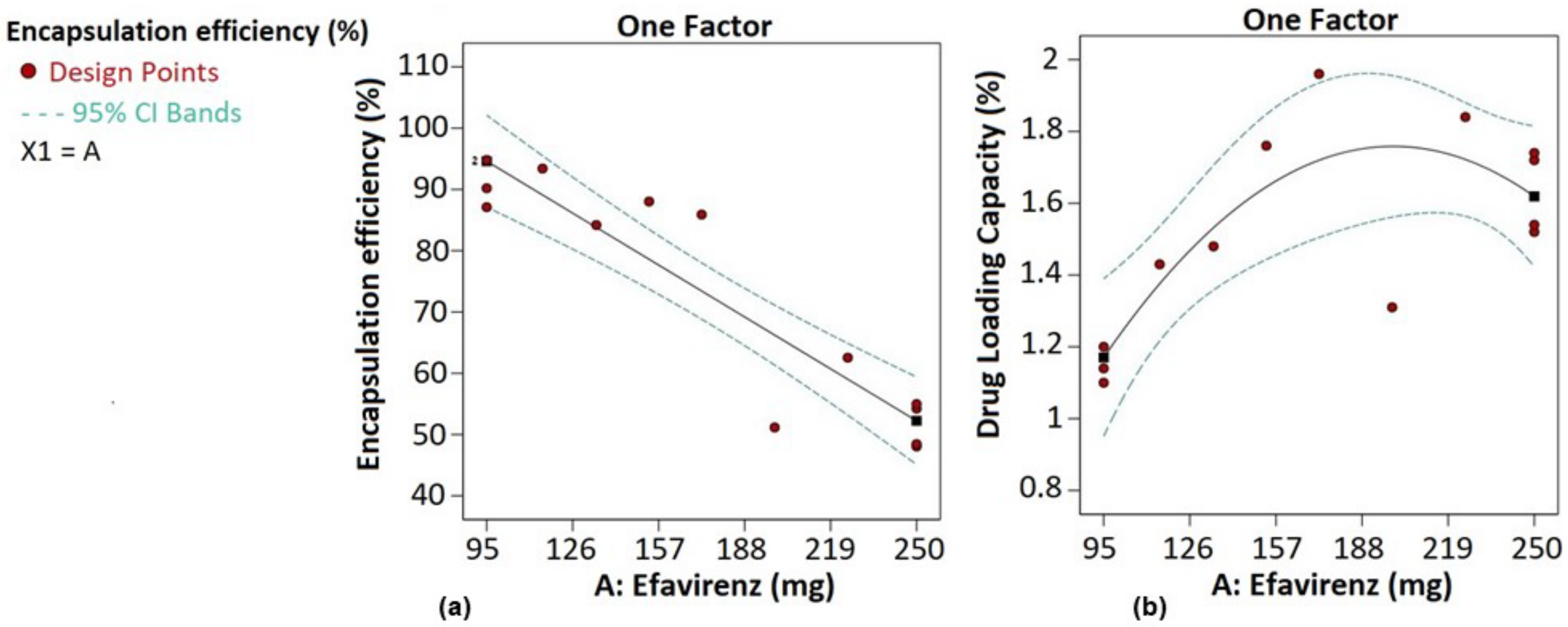
3.5. Encapsulation Efficacy and Drug Loading Capacity
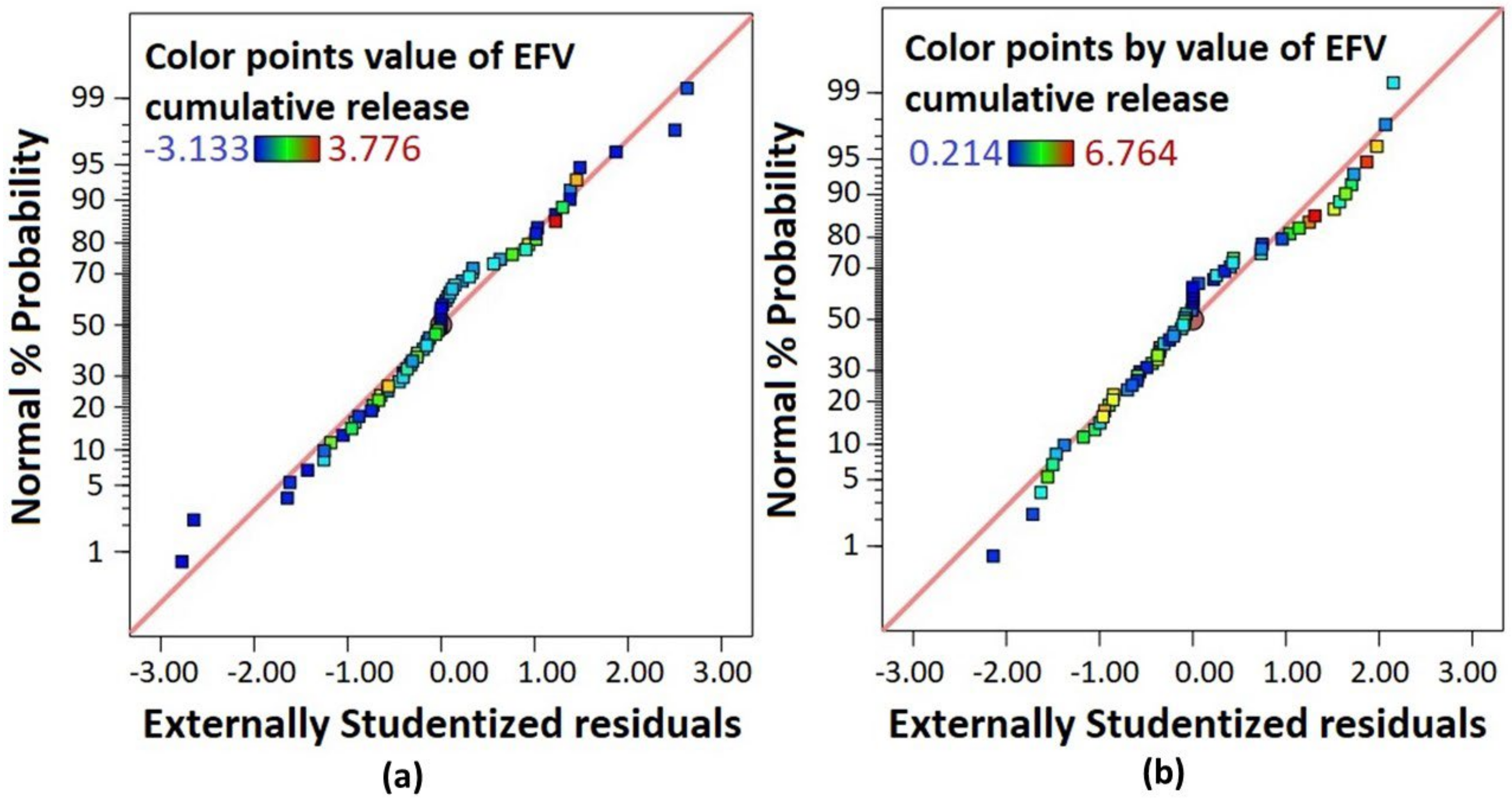
3.5.1. Statistical Analysis
3.5.2. Model Validation
3.6. Characterization of Blank-LNCs and EFV-LNCs
3.6.1. Droplet Size and Shape Analysis
3.6.2. Diffraction Scanning Calorimetry
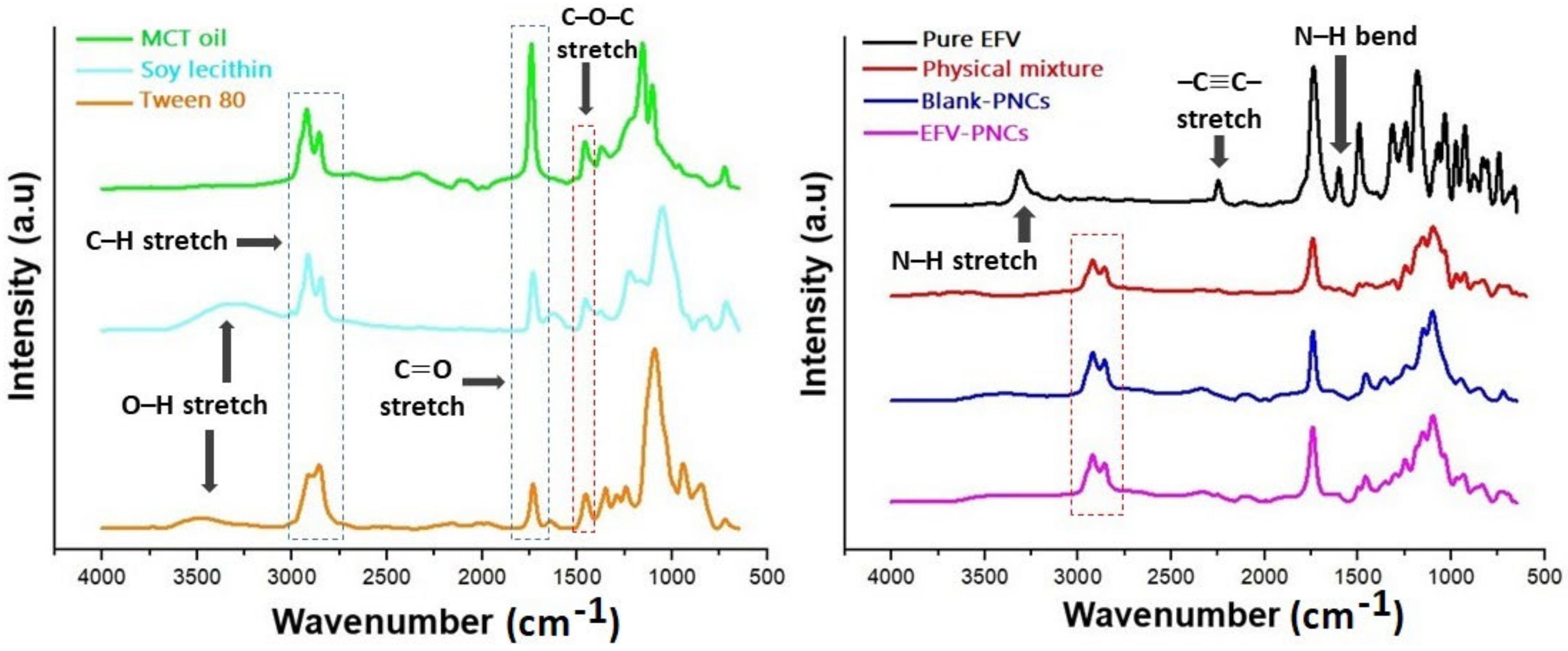
3.6.3. Fourier Transform Infrared Spectroscopy
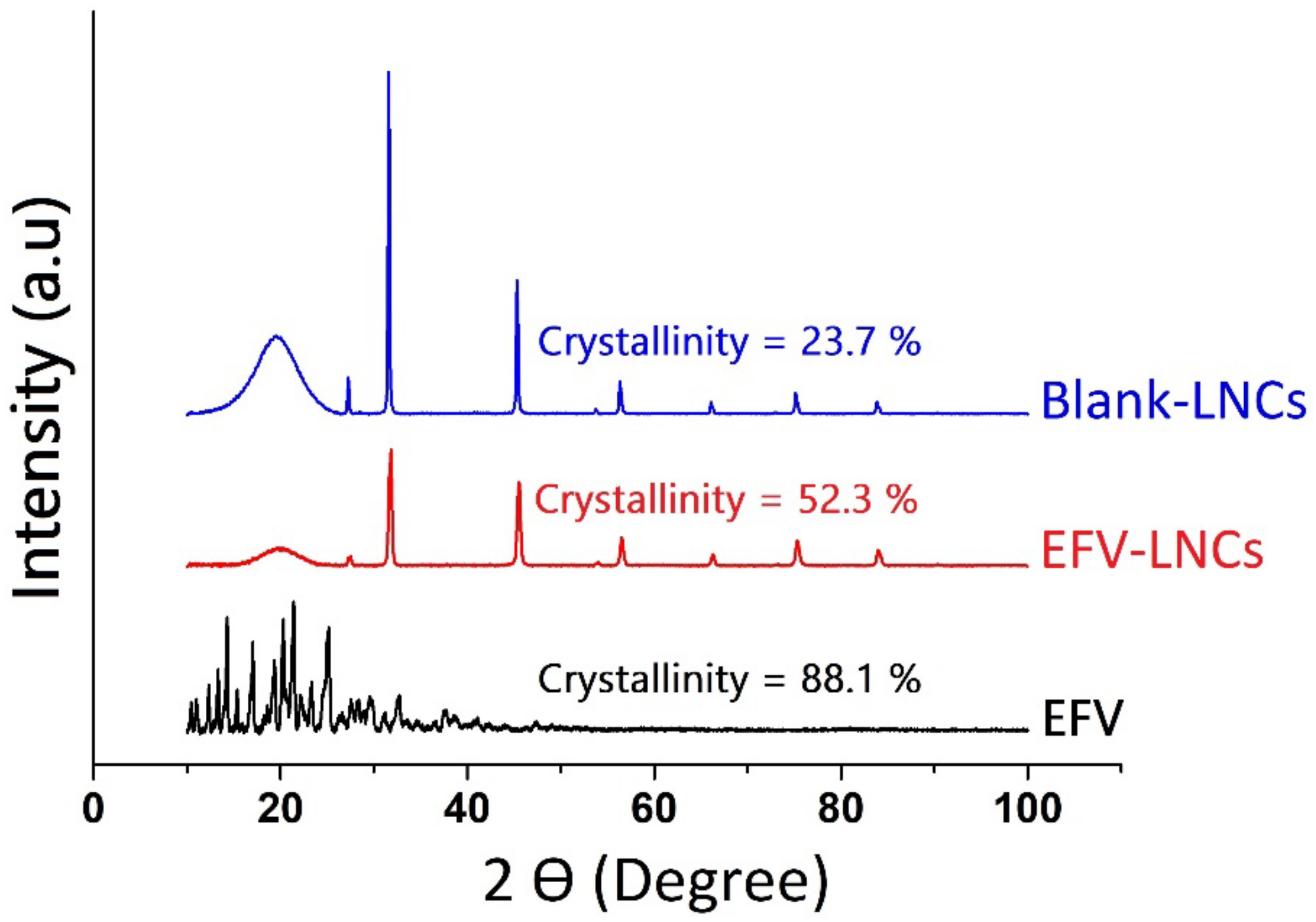
3.6.4. X-ray Diffraction
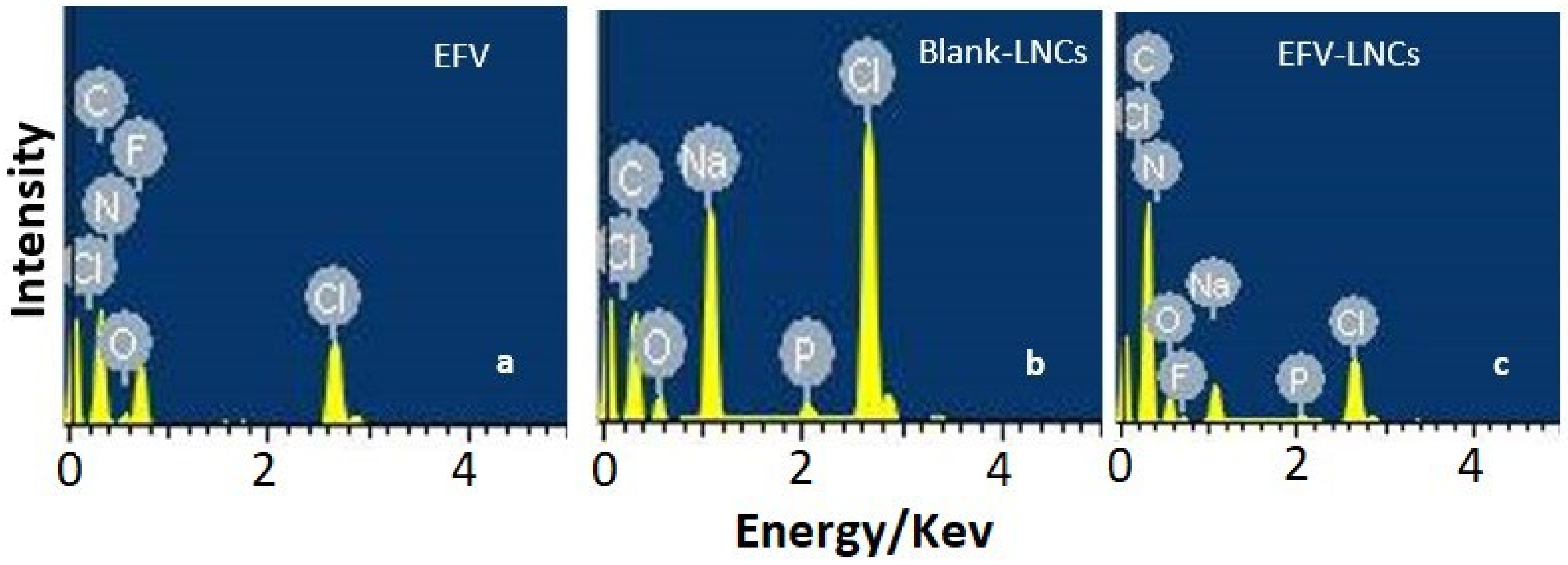
3.6.5. Energy-Dispersive X-ray Spectroscopy
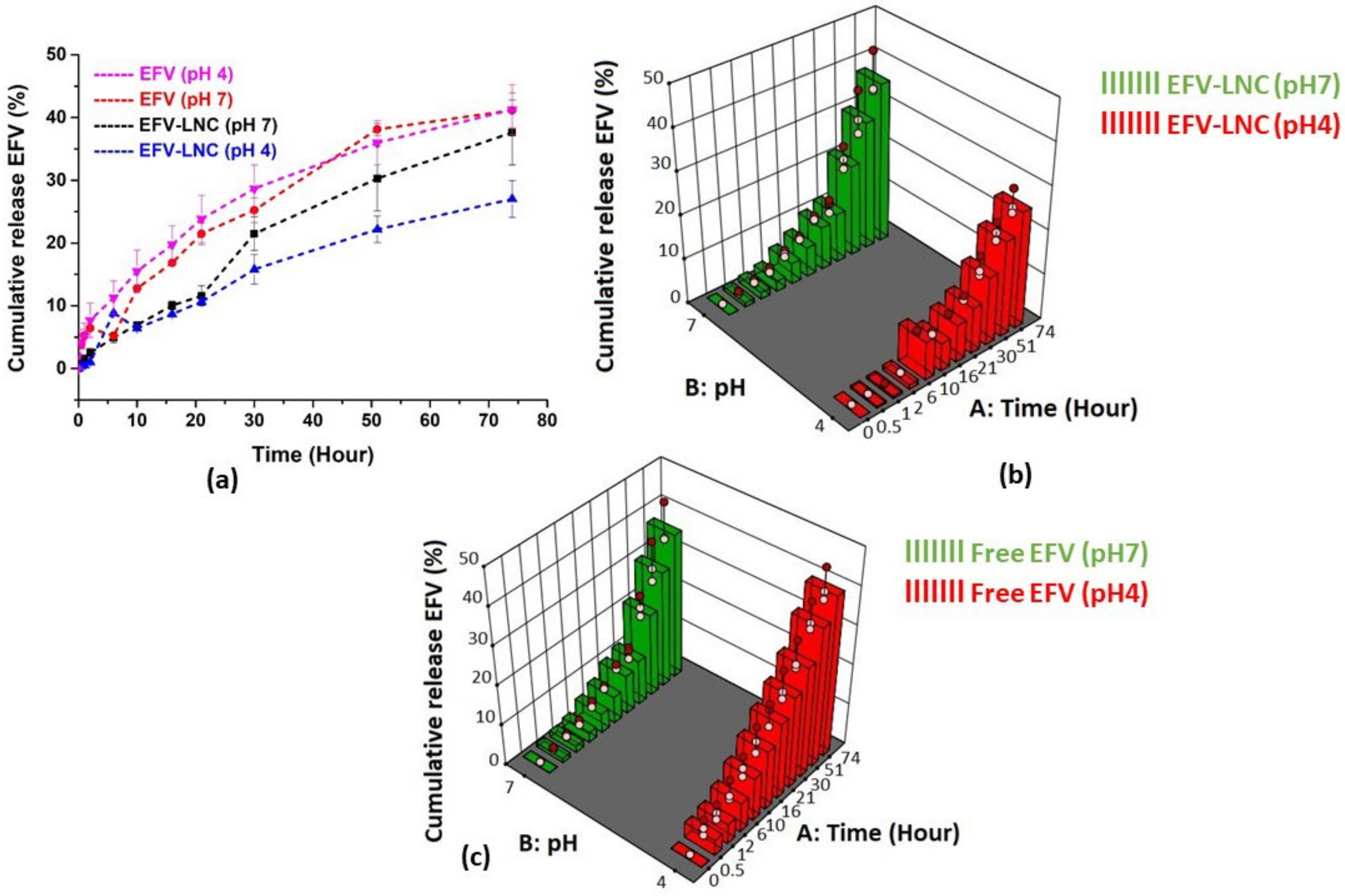
3.7. In Vitro Release
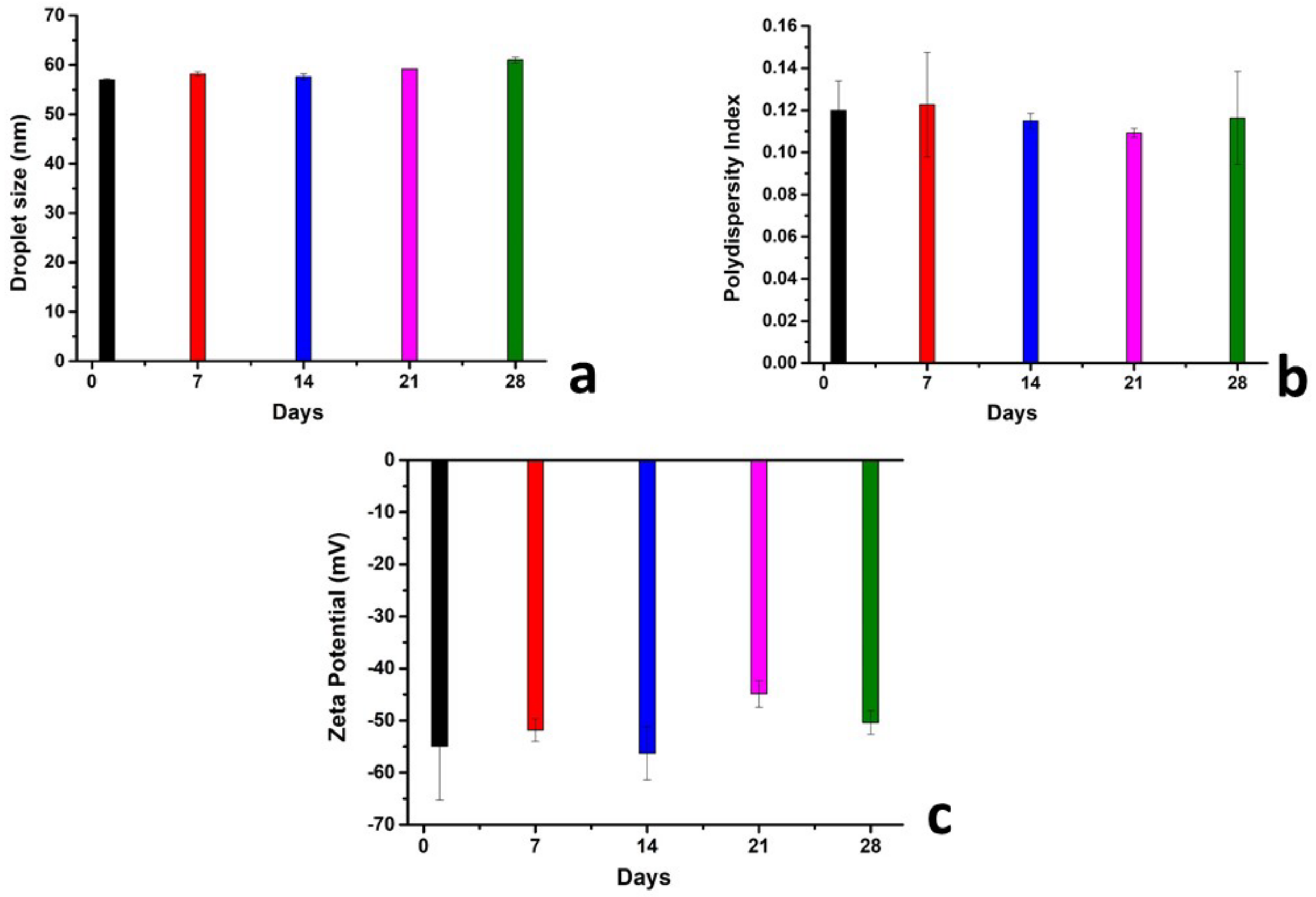
4. Stability Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tompa, D.R.; Immanuel, A.; Srikanth, S.; Kadhirvel, S. Trends and strategies to combat viral infections: A review on FDA approved antiviral drugs. Int. J. Biol. Macromol. 2021, 172, 524–541. [Google Scholar] [CrossRef]
- Kaufmann, S.H.E.; Dorhoi, A.; Hotchkiss, R.S.; Bartenschlager, R. Host-directed therapies for bacterial and viral infections. Nat. Rev. Drug Discov. 2017, 17, 35–56. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.; Sengupta, M.; Prakash, J.; Tripathy, B.C. An Introduction to Biotechnology. In Basic Applied Aspects of Biotechnology; Springer: Berlin/Heidelberg, Germany, 2017; pp. 1–21. [Google Scholar] [CrossRef]
- Chen, R.; Wang, T.; Song, J.; Pu, D.; He, D.; Li, J.; Yang, J.; Li, K.; Zhong, C.; Zhang, J. Antiviral drug delivery system for enhanced bioactivity, better metabolism and pharmacokinetic characteristics. Int. J. Nanomedicine 2021, 16, 4959–4984. [Google Scholar] [CrossRef]
- De Clercq, E.; Li, G. Approved antiviral drugs over the past 50 years. Clin. Microbiol. Rev. 2016, 29, 695–747. [Google Scholar] [CrossRef] [Green Version]
- Arora, S.; Chawla, A.; Pawar, P.; Sharma, P. Novel drug delivery approaches on antiviral and antiretroviral agents. J. Adv. Pharm. Technol. Res. 2012, 3, 147–159. [Google Scholar] [CrossRef]
- Lembo, D.; Cavalli, R. Nanoparticulate delivery systems for antiviral drugs. Antivir. Chem. Chemother. 2010, 21, 53–70. [Google Scholar] [CrossRef] [Green Version]
- Cojocaru, F.D.; Botezat, D.; Gardikiotis, I.; Uritu, C.M.; Dodi, G.; Trandafir, L.; Rezus, C.; Rezus, E.; Tamba, B.I.; Mihai, C.T. Nanomaterials designed for antiviral drug delivery transport across biological barriers. Pharmaceutics 2020, 12, 171. [Google Scholar] [CrossRef] [Green Version]
- Samimi, S.; Maghsoudnia, N.; Eftekhari, R.B.; Dorkoosh, F. Lipid-Based Nanoparticles for Drug Delivery Systems; Elsevier Inc.: Amsterdam, The Netherlands, 2018; ISBN 9780128140321. [Google Scholar]
- Kalepu, S.; Manthina, M.; Padavala, V. Oral lipid-based drug delivery systems—An overview. Acta Pharm. Sin. B 2013, 3, 361–372. [Google Scholar] [CrossRef] [Green Version]
- Jordaan, M.A.; Ebenezer, O.; Damoyi, N.; Shapi, M. Virtual screening, molecular docking studies and DFT calculations of FDA approved compounds similar to the non-nucleoside reverse transcriptase inhibitor (NNRTI) efavirenz. Heliyon 2020, 6, e04642. [Google Scholar] [CrossRef] [PubMed]
- Beck, B.R.; Shin, B.; Choi, Y.; Park, S.; Kang, K. Predicting commercially available antiviral drugs that may act on the novel coronavirus (SARS-CoV-2) through a drug-target interaction deep learning model. Comput. Struct. Biotechnol. J. 2020, 18, 784–790. [Google Scholar] [CrossRef]
- Heurtault, B.; Saulnier, P.; Pech, B.; Proust, J.E.; Benoit, J.P. A novel phase inversion-based process for the preparation of lipid nanocarriers. Pharm. Res. 2002, 19, 875–880. [Google Scholar] [CrossRef]
- Anton, N.; Gayet, P.; Benoit, J.P.; Saulnier, P. Nano-emulsions and nanocapsules by the PIT method: An investigation on the role of the temperature cycling on the emulsion phase inversion. Int. J. Pharm. 2007, 344, 44–52. [Google Scholar] [CrossRef]
- APA PubChem Compound Summary for CID 64139, Efavirenz. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Efavirenz (accessed on 24 November 2021).
- Persson, L.C.; Porter, C.J.H.; Charman, W.N.; Bergström, C.A.S. Computational prediction of drug solubility in lipid based formulation excipients. Pharm. Res. 2013, 30, 3225–3237. [Google Scholar] [CrossRef]
- Rane, S.S.; Anderson, B.D. What determines drug solubility in lipid vehicles: Is it predictable? Adv. Drug Deliv. Rev. 2008, 60, 638–656. [Google Scholar] [CrossRef]
- Moura, R.P.; Pacheco, C.; Pêgo, A.P.; des Rieux, A.; Sarmento, B. Lipid nanocapsules to enhance drug bioavailability to the central nervous system. J. Control. Release 2020, 322, 390–400. [Google Scholar] [CrossRef]
- Heurtault, B.; Saulnier, P.; Proust, J.E.; Benoit, J.P. Lipid Nanocapsules, Preparation Process and Use As Medicine. U.S. Patent 8,057,823, 15 November 2011. [Google Scholar]
- Nasr, M.; Abdel-Hamid, S. Lipid based Nanocapsules: A Multitude of Biomedical Applications. Curr. Pharm. Biotechnol. 2015, 16, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Aydar, A.Y. Utilization of Response Surface Methodology in Optimization of Extraction of Plant Materials. In Statistical Approaches With Emphasis on Design of Experiments Applied to Chemical Processes; IntechOpen: London, UK, 2018. [Google Scholar] [CrossRef] [Green Version]
- Sarabia, L.A.; Ortiz, M.C. Response Surface Methodology. Compr. Chemom. 2009, 1, 345–390. [Google Scholar] [CrossRef]
- Bienvenu, E.; Hoffmann, K.J.; Ashton, M.; Kayumba, P.C. A rapid and selective HPLC-UV method for the quantitation of efavirenz in plasma from patients on concurrent HIV/AIDS and tuberculosis treatments. Biomed. Chromatogr. 2013, 27, 1554–1559. [Google Scholar] [CrossRef] [PubMed]
- Goos, P.; Jones, B.; Syafitri, U. I-Optimal Mixture Designs Faculty of Applied Economics; Working paper 2013033; University of Antwerp, Faculty of Business and Economics: Antwerp, Belgium, 2013; 32p, Available online: https://ideas.repec.org/g/ant/wpaper/2013033.html (accessed on 1 January 2022).
- Christofoletti, R.; Nair, A.; Abrahamsson, B.; Groot, D.W.; Kopp, S.; Langguth, P.; Polli, J.E.; Shah, V.P.; Dressman, J.B. Biowaiver Monographs for Immediate Release Solid Oral Dosage Forms: Efavirenz. J. Pharm. Sci. 2013, 102, 318–329. [Google Scholar] [CrossRef]
- Brinkmann, J.; Huxoll, F.; Luebbert, C.; Sadowski, G. Solubility of pharmaceutical ingredients in triglycerides. Eur. J. Pharm. Biopharm. 2019, 145, 113–120. [Google Scholar] [CrossRef]
- Mazonde, P.; Khamanga, S.M.M.; Walker, R.B. Design, optimization, manufacture and characterization of Efavirenz-loaded flaxseed oil nanoemulsions. Pharmaceutics 2020, 12, 797. [Google Scholar] [CrossRef]
- Brinkmann, J.; Rest, F.; Luebbert, C.; Sadowski, G. Solubility of Pharmaceutical Ingredients in Natural Edible Oils. Mol. Pharm. 2020, 17, 2499–2507. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Lu, D.; Gao, X. Optimization of mixture proportions by statistical experimental design using response surface method—A review. J. Build. Eng. 2021, 36, 102101. [Google Scholar] [CrossRef]
- Breig, S.J.M.; Luti, K.J.K. Response surface methodology: A review on its applications and challenges in microbial cultures. Mater. Today Proc. 2021, 42, 2277–2284. [Google Scholar] [CrossRef]
- Shabbiri, K.; Adnan, A.; Noor, B.; Jamil, S. Optimized production, purification and characterization of alpha amylase by Brevibacterium linens DSM 20158, using bio-statistical approach. Ann. Microbiol. 2012, 62, 523–532. [Google Scholar] [CrossRef]
- Singh, S.; Singla, Y.; Arora, S. Statistical, diagnostic and response surface analysis of nefopam hydrochloride nanospheres using 35 box-behnken design. Int. J. Pharm. Pharm. Sci. 2015, 7, 89–101. [Google Scholar]
- Christopher, A.M.L.S. Principles of nanoparticle design for overcoming biological. Physiol. Behav. 2016, 176, 100–106. [Google Scholar] [CrossRef]
- Xiao, K.; Li, Y.; Luo, J.; Lee, J.S.; Xiao, W.; Gonik, A.M.; Agarwal, R.G.; Lam, K.S. The effect of surface charge on in vivo biodistribution of PEG-oligocholic acid based micellar nanoparticles. Biomaterials 2011, 32, 3435–3446. [Google Scholar] [CrossRef] [Green Version]
- Gustafson, H.H.; Holt-Casper, D.; Grainger, D.W.; Ghandehari, H. Nanoparticle uptake: The phagocyte problem. Nano Today 2015, 10, 487–510. [Google Scholar] [CrossRef] [Green Version]
- Knoll, R.; Schultze, J.L.; Schulte-Schrepping, J. Monocytes and Macrophages in COVID-19. Front. Immunol. 2021, 12, 2952. [Google Scholar] [CrossRef]
- Byrne, A.J.; Mathie, S.A.; Gregory, L.G.; Lloyd, C.M. Pulmonary macrophages: Key players in the innate defence of the airways. Thorax 2015, 70, 1189–1196. [Google Scholar] [CrossRef] [Green Version]
- Thakur, R.K.; Villette, C.; Aubry, J.M.; Delaplace, G. Dynamic emulsification and catastrophic phase inversion of lecithin-based emulsions. Colloids Surfaces A Physicochem. Eng. Asp. 2008, 315, 285–293. [Google Scholar] [CrossRef]
- Shahrin, N. Solubility and Dissolution of Drug Product: A Review. Int. J. Pharm. Life Sci. 2013, 2, 33–41. [Google Scholar] [CrossRef] [Green Version]
- Ashour, A.A.; Ramadan, A.A.; Abdelmonsif, D.A.; El-Kamel, A.H. Enhanced oral bioavailability of Tanshinone IIA using lipid nanocapsules: Formulation, in-vitro appraisal and pharmacokinetics. Int. J. Pharm. 2020, 586, 119598. [Google Scholar] [CrossRef]
- Zaini, E.; Rachmaini, F.; Armin, F.; Fitriani, L. Preparation and characterization of binary mixture of efavirenz and nicotinamide. Orient. J. Chem. 2015, 31, 2271–2276. [Google Scholar] [CrossRef]
- Fitriani, L.; Haqi, A.; Zaini, E. Preparation and characterization of solid dispersion freeze-dried efavirenz–polyvinylpyrrolidone K-30. J. Adv. Pharm. Technol. Res. 2016, 7, 105. [Google Scholar] [CrossRef] [PubMed]
- Chadha, R.; Arora, P.; Saini, A.; Jain, D.S. An insight into thermodynamic relationship between polymorphic forms of efavirenz. J. Pharm. Pharm. Sci. 2012, 15, 234–251. [Google Scholar] [CrossRef] [Green Version]
- Liao, H.Y.; Chu, S.Y. Hydrogen bond acceptor capability of carbonyl π-electrons—case study of the hydrogen-bonded urea dimer. New J. Chem. 2003, 27, 421–424. [Google Scholar] [CrossRef] [Green Version]
- Koh, P.; Chuah, J.; Talekar, M.; Gorajana, A.; Garg, S. Formulation development and dissolution rate enhancement of efavirenz by solid dispersion systems. Indian J. Pharm. Sci. 2013, 75, 291–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lavra, Z.M.M.; Pereira de Santana, D.; Ré, M.I. Solubility and dissolution performances of spray-dried solid dispersion of Efavirenz in Soluplus. Drug Dev. Ind. Pharm. 2017, 43, 42–54. [Google Scholar] [CrossRef]
- Reddy, N.P.; Padmavathi, Y.; Mounika, P.; Anjali, A. FTIR spectroscopy for estimation of efavirenz in raw material and tablet dosage form. Int. Curr. Pharm. J. 2015, 4, 390–395. [Google Scholar] [CrossRef] [Green Version]
- Sathigari, S.K.; Radhakrishnan, V.K.; Davis, V.A.; Parsons, D.L.; Babu, R.J. Amorphous-state characterization of efavirenz-polymer hot-melt extrusion systems for dissolution enhancement. J. Pharm. Sci. 2012, 101, 3456–3464. [Google Scholar] [CrossRef]
- Li, J.; Wang, X.; Zhang, T.; Wang, C.; Huang, Z.; Luo, X.; Deng, Y. A review on phospholipids and their main applications in drug delivery systems. Asian J. Pharm. Sci. 2015, 10, 81–98. [Google Scholar] [CrossRef]
- Omari, D.; Akkam, Y.; Sallam, A. Drug-Excipient Interactions: An Overview on Mechanisms and Effects on Drug Stability and Bioavailability. Ann. Rom. Soc. Cell Biol. 2021, 25, 8402–8429. [Google Scholar]
- Matusiak, J.; Grządka, E. Stability of colloidal systems—A review of the stability measurements methods. Ann. Univ. Mariae Curie-Sklodowska, Sect. AA–Chem. 2017, 72, 33. [Google Scholar] [CrossRef]
- Van Der Hoeven, P.C.; Lyklema, J. Electrostatic stabilization in non-aqueous media. Adv. Colloid Interface Sci. 1992, 42, 205–277. [Google Scholar] [CrossRef]
- Weiner, B.B.; Tscharnuter, W.W.; Fairhurst, D. Zeta Potential: A new approach. In Canadian Mineral Analysts Meeting; Brookhaven Instruments Corporation: Winnipeg, MA, Canada, 1993; pp. 1–12. [Google Scholar]
- Clogston, J.D.; Patri, A.K. Zeta Potential Measurement. Methods Mol. Biol. 2011, 697, 63–70. [Google Scholar] [CrossRef]




| Low Limit | Constraint | High Limit | ||
|---|---|---|---|---|
| 10,000 | ≤ | A: PURE MCT OIL | ≤ | 12,000 |
| 1500 | ≤ | B: CRUDE SOY LECITHIN | ≤ | 3000 |
| 9000 | ≤ | C: TWEEN 80 | ≤ | 14,000 |
| 71,000 | ≤ | D: NaCl-WATER | ≤ | 79,500 |
| A + B + C + D | = | 100,000 |
| Components (%) | Blend 1 | Blend 2 | Blend 3 | Blend 4 |
|---|---|---|---|---|
| Criteria | A maximized and C minimized | A minimized and C maximized | ||
| Unit | % | % | ||
| MCT oil (A) | 12.00 | 12.00 | 10.00 | 10.00 |
| Crude soy lecithin (B) | 3.00 | 1.50 | 3.00 | 1.50 |
| Tween 80 (C) | 9.00 | 11.70 | 13.10 | 12.94 |
| NaCl-water (D) | 76.00 | 74.80 | 73.90 | 75.56 |
| Input Variables (% m/m) | Responses | |||||||
|---|---|---|---|---|---|---|---|---|
| MCT Oil A | Crude Soy Lecithin B | Tween 80 C | Salt Water D | Droplet Size (nm) | PDI | Zeta Potential (mV) | Temperature of Dilution (°C) | |
| 1 | 12.00 | 2.16 | 11.50 | 74.34 | 40 | 0.093 | −49 | 93 |
| 2 | 10.00 | 2.42 | 11.49 | 76.09 | 33 | 0.127 | −73 | 83 |
| 3 | 11.16 | 1.50 | 11.38 | 75.95 | 46 | 0.152 | −56 | 95 |
| 4 | 11.83 | 2.87 | 13.89 | 71.41 | 31 | 0110 | −50 | 86 |
| 5 | 10.00 | 3.00 | 9.00 | 78.00 | 34 | 0.097 | −37 | 85 |
| 6 | 10.68 | 1.99 | 14.00 | 73.33 | 33 | 0.128 | −46 | 87 |
| 7 | 10.00 | 1.50 | 13.07 | 75.44 | 35 | 0.161 | −48 | 90 |
| 8 | 10.00 | 3.00 | 14.00 | 73.00 | 29 | 0.183 | −56 | 85 |
| 9 | 11.16 | 1.50 | 11.38 | 75.95 | 46 | 0.149 | −57 | 95 |
| 10 | 12.00 | 1.50 | 9.00 | 77.50 | 72 | 0.065 | −54 | 95 |
| 11 | 10.21 | 1.64 | 9.03 | 79.13 | 46 | 0.090 | −35 | 95 |
| 12 | 12.00 | 2.16 | 11.50 | 74.34 | 40 | 0.136 | −55 | 91 |
| 13 | 12.00 | 3.00 | 9.55 | 75.45 | 42 | 0.073 | −53 | 89 |
| 14 | 11.79 | 1.50 | 12.92 | 73.79 | 43 | 0.101 | −39 | 92 |
| 15 | 10.00 | 2.96 | 12.83 | 74.22 | 35 | 0.137 | −56 | 86 |
| 16 | 10.97 | 3.00 | 11.45 | 74.58 | 39 | 0.113 | −49 | 86 |
| 17 | 11.27 | 2.42 | 9.00 | 77.31 | 41 | 0.147 | −64 | 87 |
| 18 | 10.25 | 1.50 | 10.53 | 77.72 | 40 | 0.089 | −36 | 93 |
| 19 | 12.00 | 1.50 | 14.00 | 72.50 | 42 | 0.129 | −41 | 89 |
| 20 | 10.67 | 3.00 | 10.10 | 76.22 | 37 | 0.099 | −52 | 89 |
| 21 | 10.68 | 1.99 | 14.00 | 73.33 | 35 | 0.141 | −44 | 87 |
| 22 | 10.00 | 2.42 | 11.49 | 76.09 | 33 | 0.177 | −70 | 85 |
| 23 | 12.00 | 3.00 | 12.32 | 72.68 | 35 | 0.108 | −52 | 85 |
| 24 | 11.27 | 2.42 | 9.00 | 77.31 | 47 | 0.113 | −68 | 87 |
| Response | Suggested Model | f-Value | Degrees of Freedom | p-Value | R2 | Adjusted R2 | Predicted R2 | Adequate Precision |
|---|---|---|---|---|---|---|---|---|
| Droplet size (nm) | Special cubic | 45.80 | 13 | <0.0001 | 0.9835 | 0.9620 | 0.8718 | 33.2536 |
| PDI | Linear | 4.69 | 3 | 0.0123 | 0.4128 | 0.3247 | 0.1771 | 6.7749 |
| Zeta potential (mV) | Special cubic | 5.09 | 13 | 0.0072 | 0.687 | 0.6980 | −2.3389 | 8.9294 |
| Temperature of dilution (°C) | Linear | 7.22 | 13 | 0.0018 | 0.9037 | 0.7785 | −0.1615 | 7.8467 |
| Response | Reduced Model | f-Value | Degrees of Freedom | p-Value | R2 | Adjusted R2 | Predicted R2 | Adequate Precision |
|---|---|---|---|---|---|---|---|---|
| Droplet size (nm) | Reduced special cubic | 50.28 | 12 | <0.0001 | 0.9821 | 0.9626 | 0.8876 | 34.5526 |
| PDI | Linear | NM | NM | NM | NM | NM | NM | NM |
| Zeta potential (mV) | Reduced special cubic | 4.79 | 12 | 0.0072 | 0.8393 | 0.6641 | −1.0050 | 8.3624 |
| Temperature of dilution (°C) | Reduced special cubic | 10.79 | 8 | <0.0001 | 0.8520 | 0.7730 | 0.6025 | 9.3516 |
| PRESS Values | ||
|---|---|---|
| Suggested Models | Modified Models | |
| Droplet size (nm) | 217.02 | 190.28 |
| Polydispersity index | 0.0182 | NM |
| Zeta potential (mV) | 8171.50 | 4906.83 |
| Temperature of dilution (°C) | 386.72 | 132.34 |
| Response | Name | Units | Observations | Minimum | Maximum | Mean | Std. Dev. | Ratio |
|---|---|---|---|---|---|---|---|---|
| R1 | Droplet size | nm | 24.00 | 29 | 72 | 39.75 | 8.58 | 2.48 |
| R2 | PDI | 24.00 | 0.065 | 0.183 | 0.1216 | 0.031 | 2.82 | |
| R3 | Zeta potential | mV | 24.00 | −73 | −35 | −51.67 | 10.32 | 2.09 |
| R4 | Temperature of dilution | °C | 24.00 | 83 | 95 | 88.96 | 3.80 | 1.14 |
| Response | Mean | 95% Prediction | |||
|---|---|---|---|---|---|
| Predicted | Observed | 95% PI Low | 95% PI High | ||
| Blend 1 | |||||
| MCT oil: 12% | Droplet size (nm) | 41.5892 | 41.3333 | 37.0875 | 46.0908 |
| Lecithin: 3% | PDI | 0.0835994 | 0.12 | 0.0426535 | 0.124545 |
| Tween 80: 9% | Zeta potential (mV) | −59.8024 | −58.6333 | −76.1047 | −43.5001 |
| NaCl-Water: 71% | Temperature of dilution (°C) | 86.272 | 86 | 82.2926 | 90.2514 |
| Blend 2 | |||||
| MCT oil: 12% | Droplet size (nm) | 48.3797 | 49.7633 | 44.9551 | 51.8043 |
| Lecithin: 1.5% | PDI | 0.108375 | 0.141 | 0.0710762 | 0.145674 |
| Tween 80: 11.7% | Zeta potential (mV) | −41.9609 | −53.5333 | −53.8046 | −30.1172 |
| NaCl-Water: 74.8% | Temperature of dilution (°C) | 94.9996 | 95 | 91.9209 | 98.0782 |
| Blend 3 | |||||
| MCT oil: 10% | Droplet size (nm) | 33.5363 | 30.52 | 30.3943 | 36.6782 |
| Lecithin: 3% | PDI | 0.149043 | 0.179667 | 0.110426 | 0.187661 |
| Tween 80: 13.1% | Zeta potential (mV) | −58.7789 | −51.8667 | −70.0912 | −47.4666 |
| NaCl-Water: 73.9% | Temperature of dilution (°C) | 84.3132 | 84 | 81.3159 | 87.3105 |
| Blend 4 | |||||
| MCT oil: 10% | Droplet size (nm) | 35.1093 | 38.5033 | 31.3772 | 38.8414 |
| Lecithin: 1.5% | PDI | 0.150377 | 0.177667 | 0.111305 | 0.189449 |
| Tween 80: 12.9% | Zeta potential (mV) | −42.8831 | −41.2667 | −57.0207 | −28.7456 |
| NaCl-Water: 75.6% | Temperature of dilution (°C) | 88.6115 | 88 | 84.9719 | 92.2511 |
| Input Variables (% m/m) | Response (%) | ||||||
|---|---|---|---|---|---|---|---|
| MCT Oil A | Crude Soy Lecithin B | Tween 80 C | Salted Water D | Efavirenz | Encapsulation Efficiency | Drug Loading Capacity | |
| 1 | 12.00 | 3.00 | 9.00 | 76.00 | 115.15 | 93.4 | 1.43 |
| 2 | 12.00 | 3.00 | 9.00 | 76.09 | 95 | 90.19 | 1.14 |
| 3 | 12.00 | 3.00 | 9.00 | 75.95 | 134.525 | 84.19 | 1.48 |
| 4 | 12.00 | 3.00 | 9.00 | 71.41 | 250 | 48.44 | 1.54 |
| 5 | 12.00 | 3.00 | 9.00 | 78.00 | 172.5 | 85.89 | 1.96 |
| 6 | 12.00 | 3.00 | 9.00 | 73.33 | 198.85 | 51.15 | 1.31 |
| 7 | 12.00 | 3.00 | 9.00 | 75.44 | 153.545 | 88.03 | 1.76 |
| 8 | 12.00 | 3.00 | 9.00 | 73.00 | 250 | 48.05 | 1.52 |
| 9 | 12.00 | 3.00 | 9.00 | 75.95 | 250 | 54.97 | 1.74 |
| 10 | 12.00 | 3.00 | 9.00 | 77.50 | 95 | 87.1 | 1.1 |
| 11 | 12.00 | 3.00 | 9.00 | 79.13 | 95 | 94.8 | 1.2 |
| 12 | 12.00 | 3.00 | 9.00 | 74.34 | 225.2 | 62.54 | 1.84 |
| 13 | 12.00 | 3.00 | 9.00 | 75.45 | 250 | 54.23 | 1.72 |
| Encapsulation Efficiency | Drug Loading Capacity | |||
|---|---|---|---|---|
| Sixth Order Model | Linear Model | Sixth Order Model | Quadratic Model | |
| PRESS values | 2408.35 | 789.70 | 4.43 | 0.5820 |
| R squared | 0.9826 | 0.8584 | 0.9393 | 0.6311 |
| Adjusted R squared | 0.9653 | 0.8455 | 0.8783 | 0.5573 |
| Predicted R squared | 0.4514 | 0.8201 | −3.8134 | 0.3669 |
| Adeq Precision | 16.1970 | 14.3630 | 10.7785 | 6.6481 |
| Response | Mean | 95% Prediction | |||
|---|---|---|---|---|---|
| Predicted | Observed | 95% PI Low | 95% PI High | ||
| Blend 1-EFV 135 | EE% | 83.7808 | 87.4 | 72.7572 | 94.8044 |
| DLC% | 1.53233 | 1.5 | 1.2386 | 1.82605 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mukubwa, G.K.; Safari, J.B.; Walker, R.B.; Krause, R.W.M. Design, Manufacturing, Characterization and Evaluation of Lipid Nanocapsules to Enhance the Biopharmaceutical Properties of Efavirenz. Pharmaceutics 2022, 14, 1318. https://doi.org/10.3390/pharmaceutics14071318
Mukubwa GK, Safari JB, Walker RB, Krause RWM. Design, Manufacturing, Characterization and Evaluation of Lipid Nanocapsules to Enhance the Biopharmaceutical Properties of Efavirenz. Pharmaceutics. 2022; 14(7):1318. https://doi.org/10.3390/pharmaceutics14071318
Chicago/Turabian StyleMukubwa, Grady K., Justin B. Safari, Roderick B. Walker, and Rui W. M. Krause. 2022. "Design, Manufacturing, Characterization and Evaluation of Lipid Nanocapsules to Enhance the Biopharmaceutical Properties of Efavirenz" Pharmaceutics 14, no. 7: 1318. https://doi.org/10.3390/pharmaceutics14071318
APA StyleMukubwa, G. K., Safari, J. B., Walker, R. B., & Krause, R. W. M. (2022). Design, Manufacturing, Characterization and Evaluation of Lipid Nanocapsules to Enhance the Biopharmaceutical Properties of Efavirenz. Pharmaceutics, 14(7), 1318. https://doi.org/10.3390/pharmaceutics14071318






