Therapeutic Potential of Naringenin Nanosuspension: In Vitro and In Vivo Anti-Osteoporotic Studies
Abstract
1. Introduction
2. Materials
2.1. Formulation of NS
2.2. Cell Culture
2.3. In Vitro Activity on MG-63 Cell Lines
2.3.1. Cell Viability Assay
2.3.2. Determination of Osteocalcin Levels
2.4. Animal Study
2.4.1. Anti-Osteoporotic Activity
2.4.2. Grouping of Animals and Assigning Treatment
2.4.3. Biochemical Estimation (Serum and Urine)
2.4.4. Bone Analysis
2.4.5. Body and Uterine Weights
2.4.6. Histopathology
2.4.7. Statistical Assessment
3. Results and Discussion
3.1. Cell Viability Assay
3.2. Effect of Formulation on Levels of Osteocalcin in Cell Lines
3.3. Effect of Formulation on Body Weight and Uterine Weight
3.4. Biochemical Parameters (Serum and Urine)
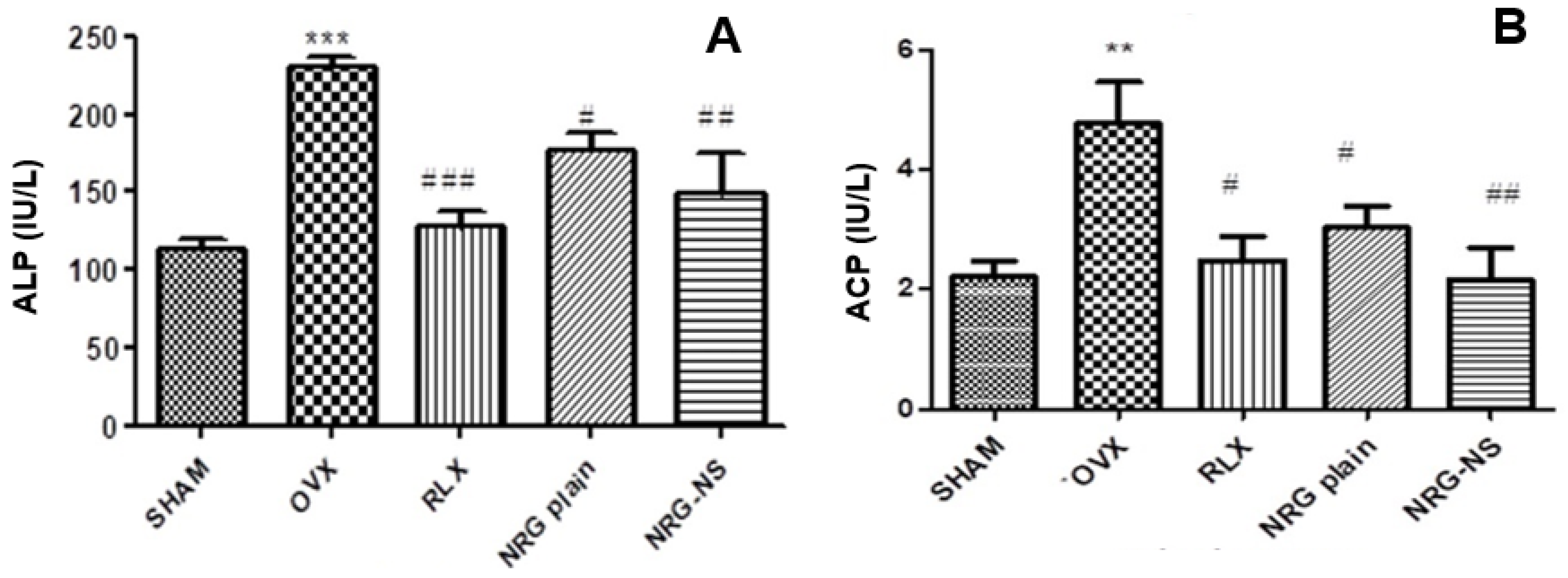
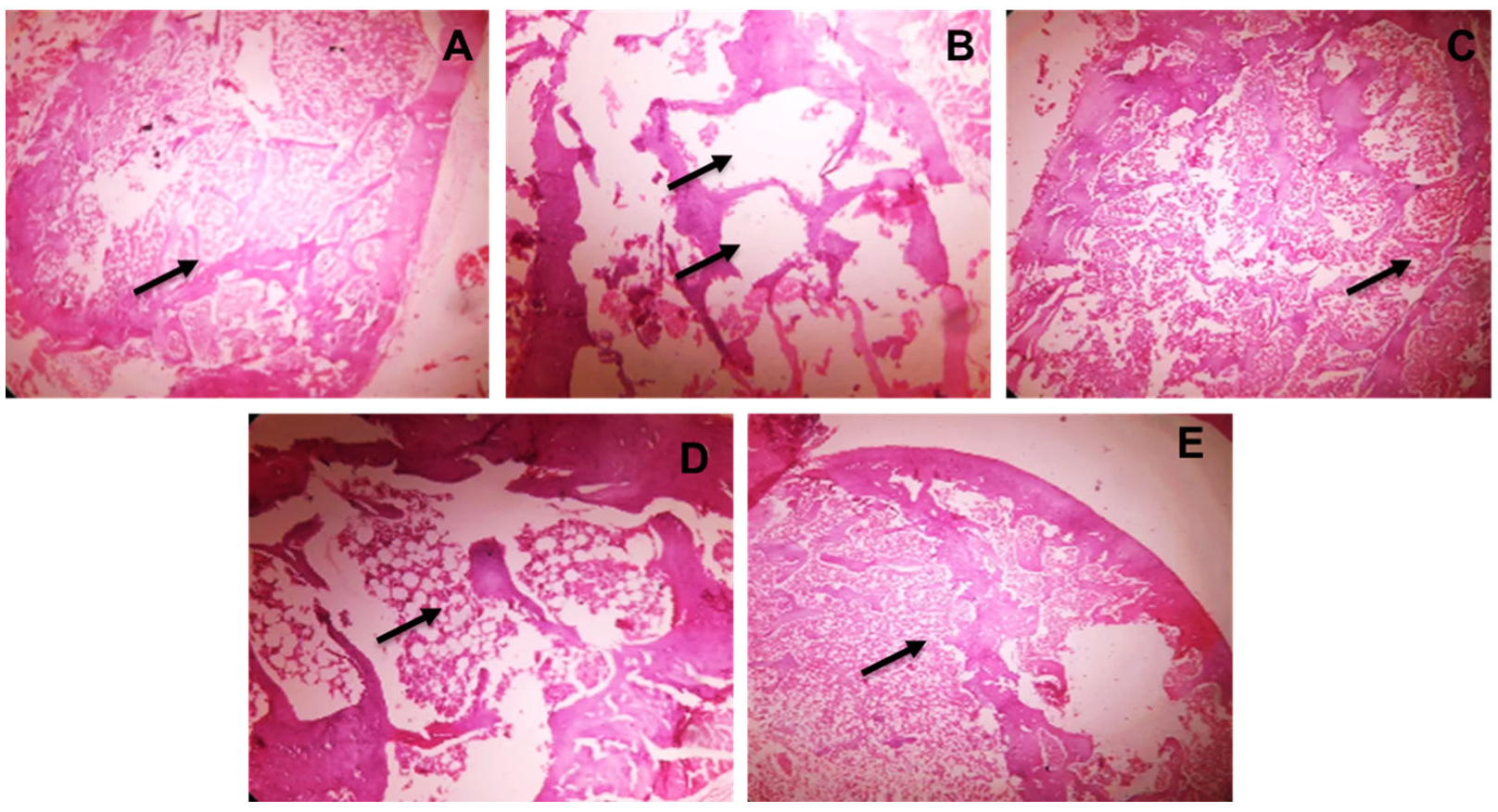
3.5. Histopathology
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rachner, T.D.; Khosla, S.; Hofbauer, L.C. Osteoporosis: Now and the future. Lancet 2011, 377, 1276–1287. [Google Scholar] [CrossRef]
- Unni, J.; Garg, R.; Pawar, R. Bone mineral density in women above 40 years. J. Mid-Life Health 2010, 1, 19–22. [Google Scholar] [CrossRef]
- Maximov, P.Y.; Lee, T.M.; Jordan, V.C. The Discovery and Development of Selective Estrogen Receptor Modulators (SERMs) for Clinical Practice. Curr. Clin. Pharmacol. 2013, 8, 135–155. [Google Scholar] [CrossRef]
- Johnell, O.; Kanis, J.A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos. Int. 2006, 17, 1726–1733. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, P. Antiresorptive therapy for the prevention of postmenopausal osteoporosis: When should treatment begin? Treat. Endocrinol. 2005, 4, 263–277. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, A.; Junnuthula, V.; Dyawanapelly, S. Ocular Therapeutics and Molecular Delivery Strategies for Neovascular Age-Related Macular Degeneration (nAMD). Int. J. Mol. Sci. 2021, 22, 10594. [Google Scholar] [CrossRef]
- Weitzmann, M.N.; Pacifici, R. Estrogen deficiency and bone loss: An inflammatory tale. J. Clin. Investig. 2006, 116, 1186–1194. [Google Scholar] [CrossRef]
- Chen, W.Y.; Manson, J.E.; Hankinson, S.E.; Rosner, B.; Holmes, M.D.; Willett, W.C.; Colditz, G.A. Unopposed Estrogen Therapy and the Risk of Invasive Breast Cancer. Arch. Intern. Med. 2006, 166, 1027–1032. [Google Scholar] [CrossRef]
- Putnam, S.E.; Scutt, A.M.; Bicknell, K.; Priestley, C.M.; Williamson, E.M. Natural products as alternative treatments for metabolic bone disorders and for maintenance of bone health. Phytother. Res. 2007, 21, 99–112. [Google Scholar] [CrossRef]
- Welch, A.A.; Hardcastle, A.C. The effects of flavonoids on bone. Curr. Osteoporos. Rep. 2014, 12, 205–210. [Google Scholar] [CrossRef]
- Horcajada-Molteni, M.N.; Crespy, V.; Coxam, V.; Davicco, M.J.; Remesy, C.; Barlet, J.P. Rutin inhibits ovariectomy-induced osteopenia in rats. J. Bone Miner. Res. 2000, 15, 2251–2258. [Google Scholar] [CrossRef] [PubMed]
- Chiba, H.; Uehara, M.; Wu, J.; Wang, X.; Masuyama, R.; Suzuki, K.; Kanazawa, K.; Ishimi, Y. Hesperidin, a citrus flavonoid, inhibits bone loss and decreases serum and hepatic lipids in ovariectomized mice. J. Nutr. 2003, 133, 1892–1897. [Google Scholar] [CrossRef] [PubMed]
- Thilakarathna, S.H.; Rupasinghe, H.P.V. Flavonoid Bioavailability and Attempts for Bioavailability Enhancement. Nutrients 2013, 5, 3367–3387. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, A.; Dyawanapelly, S. Nanodiagnostics and Nanotherapeutics for age-related macular degeneration. J. Control. Release 2021, 329, 1262–1282. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, A.; Sodha, S.J.; Junnuthula, V.; Kolimi, P.; Dyawanapelly, S. Novel and investigational therapies for wet and dry age-related macular degeneration. Drug Discov. Today 2022, 27, 2322–2332. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.S.; Pawar, P.S.; Sarkar, A.; Junnuthula, V.; Dyawanapelly, S. Bionanofactories for green synthesis of silver nanoparticles: Toward antimicrobial applications. Int. J. Mol. Sci. 2021, 22, 11993. [Google Scholar] [CrossRef]
- Ramachandran, R.; Junnuthula, V.R.; Gowd, G.S.; Ashokan, A.; Thomas, J.; Peethambaran, R.; Thomas, A.; Unni, A.K.K.; Panikar, D.; Nair, S.V.; et al. Theranostic 3-Dimensional nano brain-implant for prolonged and localized treatment of recurrent glioma. Sci. Rep. 2017, 7, 43271. [Google Scholar] [CrossRef]
- Ridolfo, R.; Tavakoli, S.; Junnuthula, V.; Williams, D.S.; Urtti, A.; van Hest, J.C.M. Exploring the Impact of Morphology on the Properties of Biodegradable Nanoparticles and Their Di ff usion in Complex Biological Medium. Biomacromolecules 2020, 22, 126–133. [Google Scholar] [CrossRef]
- Khatik, R.; Dwivedi, P.; Junnuthula, V.R.; Sharma, K.; Chuttani, K.; Mishra, A.K.; Dwivedi, A.K. Potential in vitro and in vivo colon specific anticancer activity in a HCT-116 xenograft nude mice model: Targeted delivery using enteric coated folate modified nanoparticles. RSC Adv. 2015, 5, 16507–16520. [Google Scholar] [CrossRef]
- Junnuthula, V.; Sadeghi Boroujeni, A.; Cao, S.; Tavakoli, S.; Ridolfo, R.; Toropainen, E.; Ruponen, M.; van Hest, J.C.; Urtti, A. Intravitreal Polymeric Nanocarriers with Long Ocular Retention and Targeted Delivery to the Retina and Optic Nerve Head Region. Pharmaceutics 2021, 13, 445. [Google Scholar] [CrossRef]
- Devassy, G.; Ramachandran, R.; Jeena, K.; Junnuthula, V.R.; Gopinatha, V.K.; Manju, C.A.; Manohar, M.; Nair, S.V.; Raghavan, S.C.; Koyakutty, M. Simultaneous release of two drugs from polymer nano-implant inhibits recurrence in glioblastoma spheroids. Precis. Nanomed. 2018, 2, 218–229. [Google Scholar] [CrossRef]
- Sharma, A.; Bhardwaj, P.; Arya, S.K. Naringin: A potential natural product in the field of biomedical applications. Carbohydr. Polym. Technol. Appl. 2021, 2, 100068. [Google Scholar] [CrossRef]
- Li, N.; Jiang, Y.; Wooley, P.H.; Xu, Z.; Yang, S.Y. Naringin promotes osteoblast differentiation and effectively reverses ovariectomy-associated osteoporosis. J. Orthop. Sci. 2013, 18, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Hirata, M.; Matsumoto, C.; Takita, M.; Miyaura, C.; Inada, M. Naringin suppresses osteoclast formation and enhances bone mass in mice. J. Health Sci. 2009, 55, 463–467. [Google Scholar] [CrossRef][Green Version]
- Pang, W.Y.; Wang, X.L.; Mok, S.K.; Lai, W.P.; Chow, H.K.; Leung, P.C.; Yao, X.S.; Wong, M.S. Naringin improves bone properties in ovariectomized mice and exerts oestrogen-like activities in rat osteoblast-like (UMR-106) cells. Br. J. Pharmacol. 2010, 159, 1693–1703. [Google Scholar] [CrossRef]
- Wei, X.; Xu, A.; Shen, H.; Xie, Y. Qianggu capsule for the treatment of primary osteoporosis: Evidence from a Chinese patent medicine. BMC Complement. Altern. Med. 2017, 17, 108. [Google Scholar] [CrossRef]
- Shulman, M.; Cohen, M.; Soto-Gutierrez, A.; Yagi, H.; Wang, H.; Goldwasser, J.; Lee-Parsons, C.W.; Benny-Ratsaby, O.; Yarmush, M.L.; Nahmias, Y. Enhancement of naringenin bioavailability by complexation with hydroxypropoyl-β-cyclodextrin. PLoS ONE 2011, 6, e18033. [Google Scholar] [CrossRef]
- Patel, V.R.; Agrawal, Y.K. Nanosuspension: An approach to enhance solubility of drugs. J. Adv. Pharm. Technol. Res. 2011, 2, 81–87. [Google Scholar] [CrossRef]
- Müller, R.H.; Jacobs, C.; Kayser, O. Nanosuspensions as particulate drug formulations in therapy: Rationale for development and what we can expect for the future. Adv. Drug Deliv. Rev. 2001, 47, 3–19. [Google Scholar] [CrossRef]
- Lu, L.; Xu, Q.; Wang, J.; Wu, S.; Luo, Z.; Lu, W. Drug Nanocrystals for Active Tumor-Targeted Drug Delivery. Pharmaceutics 2022, 14, 797. [Google Scholar] [CrossRef]
- Junghanns, J.U.A.; Müller, R.H. Nanocrystal technology, drug delivery and clinical applications. Int. J. Nanomed. 2008, 3, 295. [Google Scholar] [CrossRef]
- Singh, M.K.; Pooja, D.; Ravuri, H.G.; Gunukula, A.; Kulhari, H.; Sistla, R. Fabrication of surfactant-stabilized nanosuspension of naringenin to surpass its poor physiochemical properties and low oral bioavailability. Phytomedicine 2018, 40, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Gera, S.; Talluri, S.; Rangaraj, N.; Sampathi, S. Formulation and Evaluation of Naringenin Nanosuspensions for Bioavailability Enhancement. AAPS PharmSciTech 2017, 18, 3151–3162. [Google Scholar] [CrossRef] [PubMed]
- Gera, S.; Pooladanda, V.; Godugu, C.; Swamy Challa, V.; Wankar, J.; Dodoala, S.; Sampathi, S. Rutin nanosuspension for potential management of osteoporosis: Effect of particle size reduction on oral bioavailability, in vitro and in vivo activity. Pharm. Dev. Technol. 2020, 25, 971–988. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Pooladanda, V.; Bulbake, U.; Doppalapudi, S.; Rafeeqi, T.A.; Godugu, C.; Khan, W. Liposphere mediated topical delivery of thymoquinone in the treatment of psoriasis. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 2251–2262. [Google Scholar] [CrossRef]
- Potu, B.K.; Rao, M.S.; Nampurath, G.K.; Chamallamudi, M.R.; Prasad, K.; Nayak, S.R.; Dharmavarapu, P.K.; Kedage, V.; Bhat, K.M. Evidence-based assessment of antiosteoporotic activity of petroleum-ether extract of Cissus quadrangularis Linn. on ovariectomy-induced osteoporosis. Ups J. Med. Sci. 2009, 114, 140–148. [Google Scholar] [CrossRef]
- Anderson, J.J.B.; Ambrose, W.W.; Garner, S.C. Biphasic effects of genistein on bone tissue in the ovariectomized, lactating rat model. Proc. Soc. Exp. Biol. Med. 1998, 217, 345–350. [Google Scholar] [CrossRef]
- Muhammad, S.I.; Maznah, I.; Mahmud, R.B.; Esmaile, M.F.; Zuki, A.B.Z. Bone mass density estimation: Archimede’s principle versus automatic X-ray histogram and edge detection technique in ovariectomized rats treated with germinated brown rice bioactives. Clin. Interv. Aging 2013, 8, 1421–1431. [Google Scholar] [CrossRef]
- Chaplin, A.J. Manual of histological techniques. J. D. Bancroft and H. C. Cook. Churchill Livingstone, Edinburgh, London, Melbourne, New York, 1984. No. of pages: Ii + 274. Price: £12.50. ISBN: 0 443 02870 2. J. Pathol. 1985, 145, 355–356. [Google Scholar] [CrossRef]
- Barry, M.; Pearce, H.; Cross, L.; Tatullo, M.; Gaharwar, A.K. Advances in Nanotechnology for the Treatment of Osteoporosis. Curr. Osteoporos. Rep. 2016, 14, 87–94. [Google Scholar] [CrossRef]
- Czekanska, E.M.; Stoddart, M.J.; Richards, R.G.; Hayes, J.S. In search of an osteoblast cell model for in vitro research. Eur. Cells Mater. 2012, 24, 1–17. [Google Scholar] [CrossRef]
- Yin, L.; Cheng, W.; Qin, Z.; Yu, H.; Yu, Z.; Zhong, M.; Sun, K.; Zhang, W. Effects of naringin on proliferation and osteogenic differentiation of human periodontal ligament stem cells in vitro and in vivo. Stem Cells Int. 2015, 2015, 758706. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, Y.; Kode, A.; Xu, L.; Mosialou, I.; Silva, B.C.; Ferron, M.; Clemens, T.L.; Economides, A.N.; Kousteni, S. Genetic evidence points to an osteocalcin-independent influence of osteoblasts on energy metabolism. J. Bone Miner. Res. 2011, 26, 2012–2025. [Google Scholar] [CrossRef] [PubMed]
- Toth, M.J.; Poehlman, E.T.; Matthews, D.E.; Tchernof, A.; MacCoss, M.J. Effects of estradiol and progesterone on body composition, protein synthesis, and lipoprotein lipase in rats. Am. J. Physiol. Endocrinol. Metab. 2001, 280, E496–E501. [Google Scholar] [CrossRef]
- Li, F.; Yang, X.; Yang, Y.; Guo, C.; Zhang, C.; Yang, Z.; Li, P. Antiosteoporotic activity of echinacoside in ovariectomized rats. Phytomedicine 2013, 20, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Guo, D.; Wang, J.; Wang, X.; Luo, H.; Zhang, H.; Cao, D.; Chen, L.; Huang, N. Double directional adjusting estrogenic effect of naringin from Rhizoma drynariae (Gusuibu). J. Ethnopharmacol. 2011, 138, 451–457. [Google Scholar] [CrossRef]
- Breinholt, V.M.; Svendsen, G.W.; Dragsted, L.O.; Hossaini, A. The Citrus-Derived Flavonoid Naringenin Exerts Uterotrophic Effects in Female Mice at Human Relevant Doses. Basic Clin. Pharmacol. Toxicol. 2004, 94, 30–36. [Google Scholar] [CrossRef]
- Siffert, R.S. The role of alkaline phosphatase in osteogenesis. J. Exp. Med. 1951, 93, 415–426. [Google Scholar] [CrossRef]
- Bull, H.; Murray, P.G.; Thomas, D.; Fraser, A.M.; Nelson, P.N. Acid phosphatases. Mol. Pathol. 2002, 55, 65–72. [Google Scholar] [CrossRef]
- Ivaska, K.K.; Hentunen, T.A.; Vääräniemi, J.; Ylipahkala, H.; Pettersson, K.; Väänänen, H.K. Release of Intact and Fragmented Osteocalcin Molecules from Bone Matrix during Bone Resorption in Vitro. J. Biol. Chem. 2004, 279, 18361–18369. [Google Scholar] [CrossRef]
- Uebelhart, B.; Herrmann, F.; Rizzoli, R. Effects of the SERM raloxifene on calcium and phosphate metabolism in healthy middle-aged men. Clin. Cases Miner. Bone Metab. 2009, 6, 163–168. [Google Scholar] [PubMed]
- Habauzit, V.; Sacco, S.M.; Gil-Izquierdo, A.; Trzeciakiewicz, A.; Morand, C.; Barron, D.; Pinaud, S.; Offord, E.; Horcajada, M.N. Differential effects of two citrus flavanones on bone quality in senescent male rats in relation to their bioavailability and metabolism. Bone 2011, 49, 1108–1116. [Google Scholar] [CrossRef]
- Moser, S.C.; van der Eerden, B.C.J. Osteocalcin—A Versatile Bone-Derived Hormone. Front. Endocrinol. 2018, 9, 794. [Google Scholar] [CrossRef] [PubMed]
- Wronski, T.J.; Cintrón, M.; Dann, L.M. Temporal relationship between bone loss and increased bone turnover in ovariectomized rats. Calcif. Tissue Int. 1988, 43, 179–183. [Google Scholar] [CrossRef] [PubMed]


| S. No. | Parameters | Initial Weight (g) | Final Weight (g) | Weight Variation (g) | Uterine Weight (g) |
|---|---|---|---|---|---|
| 1 | Sham | 189.12 ± 8.22 | 205.32 ± 12.54 | 16.2 ± 4.32 | 0.56 ± 0.15 |
| 2 | OVX (Control) | 190.45 ± 9.65 | 284.19 ± 23.32 *** | 93.74 ± 3.67 | 0.09 ± 0.02 *** |
| 3 | RLX | 205.12 ± 5.43 | 257.86 ± 18.98 | 52.74 ± 3.55 | 0.16 ± 0.02 ### |
| 4 | NRG | 216.23 ± 2.13 | 240.74 ± 28.90 | 24.51 ± 6.77 | 0.13 ± 0.07 # |
| 5 | NRG-NS | 209.15 ± 1.98 | 225.52 ± 17.87 | 16.37 ± 5.89 | 0.15 ± 0.06 ## |
| 6 | Blank-NS | 192.64 ± 5.87 | 228.81 ± 18.76 | 36.17 ± 2.89 | 0.10 ± 0.03 |
| S. No. | Treatment | Calcium Estimation in Urine (mg/dL) | Serum Calcium Estimation (mg/dL) | Serum Phosphorus Estimation (mg/dL) | Total Protein (g%) | Phosphorus Estimation in Urine (mg/dL) | Serum OCN (ng/mL) |
|---|---|---|---|---|---|---|---|
| 1 | Sham | 5.02 ± 2.78 | 10.05 ± 1.06 | 25.53 ± 0.52 | 10.05 ± 1.40 | 4.75 ± 1.98 * | 2.20 ± 1.7 |
| 2 | OVX untreated | 4.45 ± 0.38 | 5.90 ± 0.47 ### | 22.31 ± 0.09 | 9.98 ± 0.87 | 2.29 ± 0.95 | 2.53 ± 1.90 ** |
| 3 | RLX | 4.55 ± 0.82 | 9.10 ± 0.25 ** | 27.95 ± 1.42 | 10.13 ± 1.12 | 6.38 ± 2.77 * | 2.19 ± 1.25 * |
| 4 | NRG | 4.91 ± 0.72 | 7.63 ± 1.19 * | 25.89 ± 0.23 | 9.57 ± 1.20 | 3.96 ± 0.81 | 2.47± 1.98 ** |
| 5 | NRG-NS | 3.81 ± 0.99 | 9.83 ± 0.87 ** | 26.31 ± 0.48 | 9.56 ± 2.76 | 4.18 ± 0.70 | 3.89 ± 1.5 ## |
| 6 | Blank-NS | 4.23 ± 0.34 | 6.34 ± 0.04 | 21.76 ± 0.34 | 9.06 ± 1.43 | 2.65 ± 0.23 | 2.32 ± 1.54 |
| S. No. | Group | Weight (g) | Ash Weight (g) | Length (mm) | Diameter (mm) | Bone Density (g/cm3) | Bone Inorganic Content (mg%) | |
|---|---|---|---|---|---|---|---|---|
| Ca | P | |||||||
| 1 | SHAM | 0.88 ± 0.18 | 0.07 ± 0.02 | 28.46 ± 1.28 | 2.48 ± 0.32 | 1.79 ± 0.008 | 10.27 ± 0.40 | 4.19 ± 0.08 |
| 2 | OVX Control | 0.58 ± 0.07 # | 0.03 ± 0.01 # | 27.76 ± 0.30 | 2.09 ± 0.05 | 0.54 ± 0.09 ## | 5.25 ± 0.65 ## | 3.76 ± 0.05 # |
| 3 | RLX | 0.80 ± 0.08 | 0.08 ± 0.02 | 28.01 ± 0.49 | 2.17 ± 0.01 | 1.80 ± 0.07 ** | 11.57 ± 2.19 | 4.64 ± 0.01 |
| 4 | NRG | 0.70 ± 0.07 | 0.08 ± 0.01 | 26.66 ± 1.24 | 2.54 ± 0.34 | 0.69 ± 0.07 | 11.48 ± 1.45 | 4.20 ± 0.04 |
| 5 | NRG-NS | 0.85 ± 0.12 | 0.08 ± 0.01 | 27.86 ± 1.13 | 2.56 ± 0.76 | 1.40 ± 0.29 * | 11.09 ± 0.05 | 4.06 ± 0.03 |
| 6 | Blank-NS | 0.61 ± 0.11 | 0.02 ± 0.01 | 26.43 ± 1.43 | 2.23 ± 1.52 | 0.66 ± 0.12 | 6.32 ± 0.32 | 4.12 ± 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gera, S.; Sampathi, S.; Maddukuri, S.; Dodoala, S.; Junnuthula, V.; Dyawanapelly, S. Therapeutic Potential of Naringenin Nanosuspension: In Vitro and In Vivo Anti-Osteoporotic Studies. Pharmaceutics 2022, 14, 1449. https://doi.org/10.3390/pharmaceutics14071449
Gera S, Sampathi S, Maddukuri S, Dodoala S, Junnuthula V, Dyawanapelly S. Therapeutic Potential of Naringenin Nanosuspension: In Vitro and In Vivo Anti-Osteoporotic Studies. Pharmaceutics. 2022; 14(7):1449. https://doi.org/10.3390/pharmaceutics14071449
Chicago/Turabian StyleGera, Sonia, Sunitha Sampathi, Sravya Maddukuri, Sujatha Dodoala, Vijayabhaskarreddy Junnuthula, and Sathish Dyawanapelly. 2022. "Therapeutic Potential of Naringenin Nanosuspension: In Vitro and In Vivo Anti-Osteoporotic Studies" Pharmaceutics 14, no. 7: 1449. https://doi.org/10.3390/pharmaceutics14071449
APA StyleGera, S., Sampathi, S., Maddukuri, S., Dodoala, S., Junnuthula, V., & Dyawanapelly, S. (2022). Therapeutic Potential of Naringenin Nanosuspension: In Vitro and In Vivo Anti-Osteoporotic Studies. Pharmaceutics, 14(7), 1449. https://doi.org/10.3390/pharmaceutics14071449







