Mesoporous Materials as Elements of Modern Drug Delivery Systems for Anti-Inflammatory Agents: A Review of Recent Achievements
Abstract
:1. Introduction
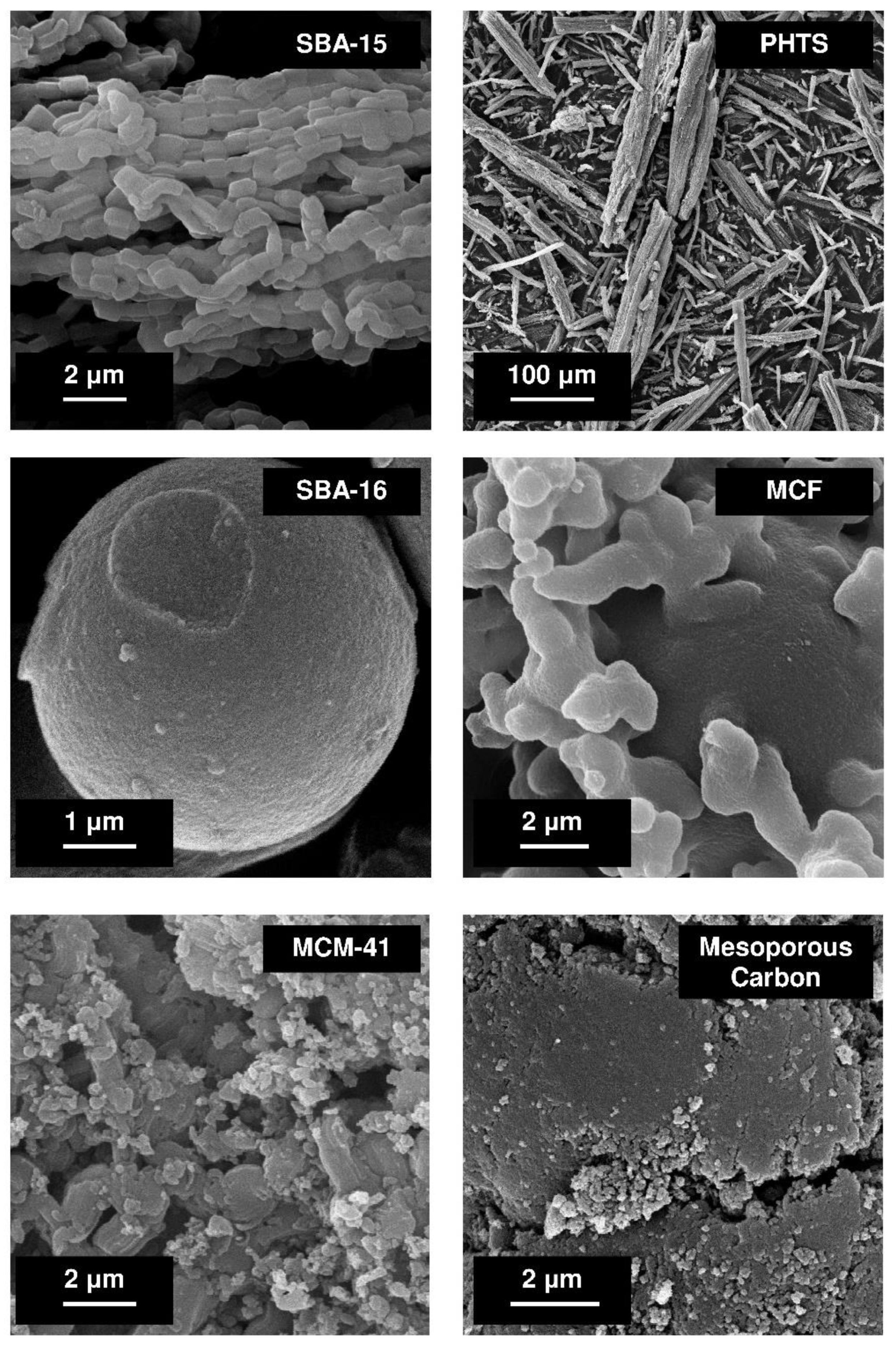
2. Anti-Inflammatory Agents
3. Physicochemical and Biological Characteristics of Mesoporous Material-Based Drug Delivery Systems (DDSs)
4. Mesoporous Material-Based Drug Delivery Systems for Anti-Inflammatory Agents
5. Conclusions and Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Sing, K.S.W.; Everett, D.H.; Haul, R.A.W.; Moscou, L.; Pierotti, R.A.; Rouquérol, J.; Siemieniewska, T. Reporting physisorption data for gas/solid systems with special references to the determination of surface area and porosity. Pure Appl. Chem. 1985, 57, 603–619. [Google Scholar] [CrossRef]
- Perego, A.; Millini, R. Porous materials in catalysis: Challenges for mesoporous materials. Chem. Soc. Rev. 2013, 42, 3956–3976. [Google Scholar] [CrossRef] [PubMed]
- Niu, B.; Wang, X.; Wu, K.; He, X.; Zhang, R. Mesoporous titanium dioxide: Synthesis and applications in photocatalysis, energy and biology. Materials 2018, 11, 1910. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Yu, T.; Fan, X.; Zhang, H.; Li, Z.; Ye, J.; Zou, Z. Enhanced activity of mesoporous Nb2O5 for photocatalytic hydrogen production. Appl. Surf. Sci. 2007, 253, 5800–8506. [Google Scholar] [CrossRef]
- Laskowski, Ł.; Laskowska, M.; Villa, N.; Schabikowski, M.; Walcarius, A. Mesoporous silica-based materials for electronics-oriented applications. Molecules 2019, 24, 2395. [Google Scholar] [CrossRef] [Green Version]
- Bach, U.; Lupo, D.; Comte, P.; Moser, J.E.; Weissörtel, F.; Salbeck, J.; Spreitzer, H.; Grätzel, M. Solid-state dye-sensitized mesoporous TiO2 solar cells with high photon-to-electron conversion efficiencies. Nature 1998, 395, 583–585. [Google Scholar] [CrossRef]
- Eftekhari, A. Ordered mesoporous materials for lithium-ion batteries. Mesoporous Microporous Mater. 2017, 243, 355–369. [Google Scholar] [CrossRef]
- Yang, P.; Gai, S.; Lin, J. Functionalized mesoporous silica materials for controlled drug delivery. Chem. Soc. Rev. 2012, 41, 3679–3698. [Google Scholar] [CrossRef]
- Ispas, C.; Sokolov, I.; Andreescu, S. Enzyme-functionalized mesoporous silica for bioanalytical applications. Anal. Bioanal. Chem. 2009, 393, 543–554. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Lu, Y.; Jiang, C.; Zhu, Y.; Yang, X.; Hu, X.; Lin, Z.; Zhang, Y.; Peng, M.; Xia, H.; et al. Actively targeted deep tissue imaging and photothermal-chemo therapy of breast cancer by antibody-functionalized drug-loaded X-ray-responsive bismuth sulfide@mesoporous silica core-shell nanoparticles. Adv. Funct. Mater. 2018, 28, 1704623. [Google Scholar] [CrossRef]
- Liu, Z.; Li, M.; Yang, X.; Yin, M.; Ren, J.; Qu, X. The use of multifunctional magnetic mesoporous core/shell heterostructures in a biomolecule separation system. Biomaterials 2011, 32, 4683–4690. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhou, X.; He, C. Mesoporous silica nanoparticles for tissue-engineering applications. WIREs Nanomed. Nanobiotechnol. 2019, 11, e1573. [Google Scholar] [CrossRef] [PubMed]
- Vallet-Regí, M.; Rámila, A.; del Real, R.P.; Pérez-Pariente, J. A new property of MCM-41: Drug delivery system. Chem. Mater. 2001, 13, 308–311. [Google Scholar] [CrossRef]
- Atkinson, I.; Seciu-Grama, A.M.; Petrescu, S.; Culita, D.; Mocioiu, O.C.; Voicescu, M.; Mitran, R.-A.; Lincu, D.; Prelipcean, A.-M.; Craciumescu, O. Cerium-containing mesoporous bioactive glasses (MBGs)-derived scaffolds with drug delivery capability for potential tissue engineering applications. Pharmaceutics 2022, 14, 1169. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.C.; Nguyen, C.T.H.; Strounina, E.; Davis-Poynter, N.; Ross, B.P. Structure-activity relationships of GAG mimetic-functionalized mesoporous silica nanoparticles and evaluation of acyclovir-loaded antiviral nanoparticles with dual mechanisms of action. ACS Omega 2018, 3, 1689–1699. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.-N.; Zhang, C.-Q.; Wang, W.; Wang, P.C.; Zhou, J.-P.; Liang, X.-J. pH-Responsive mesoporous silica nanoparticles employed un controlled drug delivery systems for cancer treatment. Cancer Biol. Med. 2014, 11, 34–43. [Google Scholar]
- Moritz, M. Solvent optimization for niacinamide adsorption on organo-functionalized SBA-15 mesoporous silica. Appl. Surf. Sci. 2013, 283, 537–545. [Google Scholar] [CrossRef]
- Moritz, M.; Łaniecki, M. Modified SBA-15 as the carrier for metoprolol and papaverine: Adsorption and release study. J. Solid State Chem. 2011, 184, 1761–1767. [Google Scholar] [CrossRef]
- Jadhav, N.V.; Vavia, P.R. Dodecylamine template-based hexagonal mesoporous silica (HMS) as a carrier for improved oral delivery of fenofibrate. AAPS PharmSciTech 2017, 18, 2764–2773. [Google Scholar] [CrossRef]
- Lengert, E.; Verkhovskii, R.; Yurasov, N.; Genina, E.; Svenskaya, Y. Mesoporous carriers for transdermal delivery of antifungal drug. Mater. Lett. 2019, 248, 211–213. [Google Scholar] [CrossRef]
- Moritz, M.; Geszke-Moritz, M. Mesoporous silica materials with different structures as the carriers for antimicrobial agent. Modeling of chlorhexidine adsorption and release. Appl. Surf. Sci. 2015, 356, 1327–1340. [Google Scholar] [CrossRef]
- Pajzderska, A.; Drużbicki, K.; Bilski, P.; Jenczyk, J.; Jarek, M.; Mielcarek, J.; Wąskicki, J. Environmental effects of the molecular mobility of ranitidine hydrochloride: Crystalline state versus drug loaded into the silica matrix. J. Phys. Chem. C 2019, 123, 18364–18375. [Google Scholar] [CrossRef]
- López-Noriega, A.; Arcos, D.; Vallet-Regí, M. Functionalizing mesoporous bioglasses for long-term anti-osteoporotic drug delivery. Chem. Eur. J. 2010, 16, 10879–10886. [Google Scholar] [CrossRef] [PubMed]
- Moritz, M.; Geszke-Moritz, M. Sulfonic acid derivative-modified SBA-15, PHTS and MCM-41 mesoporous silicas as carriers for a new antiplatelet drug: Ticagrelor adsorption and release studies. Materials 2020, 13, 2913. [Google Scholar] [CrossRef]
- Han, C.; Huang, H.; Dong, Y.; Sui, X.; Jian, B.; Zhu, W. A comparative study of the use of mesoporous carbon and mesoporous silica as drug carriers for oral delivery of the water-insoluble drug carvedilol. Molecules 2019, 24, 1770. [Google Scholar] [CrossRef] [Green Version]
- Geszke-Moritz, M.; Moritz, M. Modeling of boldine alkaloid adsorption onto pure and propyl-sulfonic acid-modified mesoporous silicas. A comparative study. Mater. Sci. Eng. C 2016, 69, 815–830. [Google Scholar] [CrossRef]
- Žid, L.; Zeleňák, V.; Almáši, M.; Zeleňáková, A.; Szücsová, J.; Bednarčik, J.; Šuleková, M.; Hudák, A.; Váhovská, L. Mesoporous silica as a drug delivery system for naproxen: Influence of surface functionalization. Molecules 2020, 25, 4722. [Google Scholar] [CrossRef]
- Gisbert-Garzarán, M.; Manzano, M.; Vallet-Regí, M. pH-Responsive mesoporous silica and carbon nanoparticles for drug delivery. Bioengineering 2017, 41, 3. [Google Scholar] [CrossRef] [Green Version]
- Yao, P.; Zou, A.; Tian, Z.; Meng, W.; Fang, X.; Wu, T.; Cheng, J. Construction and characterization of a temperature-responsive nanocarrier for imidacloprid based on mesoporous silica nanoparticles. Colloids Surf. B 2021, 198, 111464. [Google Scholar] [CrossRef]
- Almáši, M.; Matiašová, A.A.; Šuleková, M.; Beňová, E.; Ševc, J.; Váhovská, L.; Lisnichuk, M.; Girman, V.; Zeleňáková, A.; Hudák, A.; et al. In vivo study of light-driven naproxen release from gated mesoporous silica drug delivery system. Sci. Rep. 2021, 11, 20191. [Google Scholar] [CrossRef]
- Paris, J.L.; Cabañas, V.; Manzano, M.; Vallet-Regí, M. Polymer-grafted mesoporous silica nanoparticles as ultrasound-responsive drug carriers. ACS Nano 2015, 9, 11023–11033. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, Z.; Wu, C.; Zhao, Y.; Hao, Y.; Liu, Y.; Zhao, W. Development of an oral push-pull osmotic pump of fenofibrate-loaded mesoporous silica nanoparticles. Int. J. Nanomed. 2015, 10, 1691–1701. [Google Scholar] [CrossRef] [PubMed]
- Wu, E.C.; Park, J.-H.; Park, J.; Segal, E.; Cunin, F.; Sailor, M.J. Oxidation-triggered release of fluorescent molecules or drugs from mesoporous Si microparticles. ACS Nano 2008, 11, 2401–2409. [Google Scholar] [CrossRef]
- Cheng, Y.-J.; Luo, G.-F.; Zhu, J.-Y.; Xu, X.-D.; Zeng, X.; Cheng, D.-B.; Li, Y.-M.; Wu, Y.; Zhang, X.-Z.; Zhuo, R.-X.; et al. Enzyme-induced and tumor-targeted drug delivery system based on multifunctional mesoporous silica nanoparticles. ACS Appl. Mater. Interfaces 2015, 7, 9078–9087. [Google Scholar] [CrossRef] [PubMed]
- Moritz, M.; Geszke-Moritz, M. Mesoporous materials as multifunctional tools in biosciences: Principles and applications. Mater. Sci. Eng. C 2015, 49, 114–151. [Google Scholar] [CrossRef]
- Wu, J.; Jiang, W.; Shen, Y.; Jiang, W.; Tian, R. Synthesis and characterization of mesoporous magnetic nanocomposites wrapped with chitosan gatekeepers for pH-sensitive controlled release of doxorubicin. Mater. Sci. Eng. C 2017, 70, 132–140. [Google Scholar] [CrossRef] [Green Version]
- Cho, Y.; Shi, R.; Ivanisevic, A.; Borgens, R.B. A mesoporous silica nanosphere-based drug delivery system using an electrically conducting polymer. Nanotechnology 2009, 20, 275102. [Google Scholar] [CrossRef] [PubMed]
- Palantavida, S.; Tang, R.; Sudlow, G.P.; Akers, W.J.; Schilefu, S.; Sokolov, I. Ultrabright NIR fluorescent mesoporous silica nanoparticles. J. Mater. Chem. B 2014, 2, 3107–3114. [Google Scholar] [CrossRef]
- Kresge, C.T.; Leonowicz, M.E.; Roth, W.J.; Vartuli, J.C.; Beck, J.S. Ordered mesoporous molecular sieves synthesized by a liquid-crystal template mechanism. Nature 1992, 359, 710–712. [Google Scholar] [CrossRef]
- Atiyah, N.A.; Albayati, T.M.; Atiya, M.A. Functionalization of mesoporous MCM-41 for the delivery of curcumin as an anti-inflammatory therapy. Adv. Powder Technol. 2022, 33, 103417. [Google Scholar] [CrossRef]
- Strømme, M.; Brohede, U.; Atluri, R.; Garcia-Bennett, A.E. Mesoporous silica-based nanomaterials for drug delivery: Evaluation of structuraal properties associated with release rate. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnology 2009, 1, 140–148. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, C.A.; Ahern, R.J.; Dontireddy, R.; Ryan, K.B.; Crean, A.M. Mesoporous silica formulation strategies for drug dissolution enhancement: A review. Expert Opin. Drug Deliv. 2016, 13, 93–108. [Google Scholar] [CrossRef] [PubMed]
- Bang, A.; Sadekar, A.G.; Buback, C.; Curtin, B.; Acar, S.; Kolasinac, D.; Yin, W.; Rubenstein, D.A.; Lu, H.; Leventis, N.; et al. Evaluation of dysprosia aerogels as drug delivery systems: A comparative study with random and ordered mesoporous silicas. ACS Appl. Mater. Interfaces 2014, 6, 4891–4902. [Google Scholar] [CrossRef]
- Maleki, A.; Hamidi, M. Dissolution enhancement of a model poorly water-soluble drug, atorvastatin, with ordered mesoporous silica: Comparison of MSF with SBA-15 as drug carriers. Expert Opin. Drug Deliv. 2016, 13, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Zhi, Z.; Zhao, Q.; Wu, C.; Zhao, P.; Jiang, H.; Jiang, T.; Wang, S. 3D cubic mesoporous silica microsphere as a carrier for poorly soluble drug carvedilol. Microporous Mesoporous Mater. 2012, 147, 94–101. [Google Scholar] [CrossRef]
- Ambrogi, V.; Perioli, L.; Pagano, C.; Latterini, L.; Marmottini, F.; Ricci, M.; Carlo, R. MCM-41 for furosemide dissolution improvement. Microporous Mesoporous Mater. 2012, 147, 343–349. [Google Scholar] [CrossRef]
- Ambrogi, V.; Perioli, L.; Pagano, C.; Marmottini, F.; Ricci, M.; Sagnella, A.; Rossi, C. Use of SBA-15 for furosemide oral delivery enhancement. Eur. J. Pharm. Sci. 2012, 46, 43–48. [Google Scholar] [CrossRef]
- Heikkilä, T.; Salonen, J.; Tuura, J.; Kumar, N.; Salmi, T.; Murzin, D.Y.; Hamdy, M.S.; Mul, G.; Laitinen, L.; Kaukonen, A.M.; et al. Evalauation of mesoporous TCPSi, MCM-41, SBA-15, and TUD-1 materials as API carriers for oral drug delivery. Drug Deliv. 2007, 14, 337–347. [Google Scholar] [CrossRef]
- Manzano, M.; Aina, V.; Arean, C.O.; Balas, F.; Cauda, V.; Colilla, M.; Delgado, M.R.; Vallet-Regí, M. Studies on MCM-41 mesoporous silica for drug delivery: Effect of particle morphology and amine functionalization. Chem. Eng. J. 2008, 137, 30–37. [Google Scholar] [CrossRef]
- Horcajada, P.; Ramilla, A.; Perez-Pariente, J.; Vallet-Regí, M. Influence of pore size of MCM-41 matrices on drug delivery rate. Microporous Mesoporous Mater. 2004, 68, 105–109. [Google Scholar] [CrossRef]
- Izquierdo-Barba, I.; Sousa, E.; Doadrio, J.C.; Doadrio, A.L.; Perez-Pariente, J.; Martínez, A.; Babonneau, F.; Vallet-Regí, M. Influence of mesoporous structure type on the controlled delivery of drugs: Release of ibuprofen from MCM-48, SBA-15 and functionalized SBA-15. J. Sol-Gel Sci. Technol. 2009, 50, 421–429. [Google Scholar] [CrossRef]
- Andersson, J.; Rosenholm, J.; Areva, S.; Linden, M. Influences of material characteristics on ibuprofen drug loading and release profiles from ordered micro- and mesoporous silica matrices. Chem. Mater. 2004, 16, 4160–4167. [Google Scholar] [CrossRef]
- Qu, F.; Zhu, G.; Lin, H.; Zhang, W.; Sun, J.; Li, S.; Qiu, S. A controlled release of ibuprofen by systematically tailoring the morphology of mesoporous silica materials. J. Solid State Chem. 2006, 179, 2027–2035. [Google Scholar] [CrossRef]
- Shen, S.-C.; Ng, W.K.; Chia, L.; Hu, J.; Tan, R.B.H. Physical state and dissolution of ibuprofen formulated by co-spray drying with mesoporous silica: Effect of pore and particle size. Int. J. Pharm. 2011, 410, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Mellaerts, L.; Aerts, C.A.; Van Humbeeck, J.; Augustijns, P.; Van den Mooter, G.; Martens, J.A. Enhanced release of itraconazole from ordered mesoporous SBA-15 silica materials. Chem. Commun. 2007, 13, 1375–1377. [Google Scholar] [CrossRef]
- Tao, Z. Mesoporous silica-based nanodevices for biological applications. RSC Adv. 2014, 4, 18961–18980. [Google Scholar] [CrossRef]
- Izquierdo-Barba, I.; Martínez, A.; Doadrio, A.L.; Perez-Pariente, J.; Vallet-Regí, M. Release evaluation of drugs from ordered three-dimensional silica structures. Eur. J. Pharm. Sci. 2005, 26, 365–373. [Google Scholar] [CrossRef]
- Xu, W.; Riikonen, J.; Lechto, V.-P. Mesoporous systems for poorly soluble drugs. Int. J. Pharm. 2013, 453, 181–197. [Google Scholar] [CrossRef]
- Shen, S.-C.; Ng, W.K.; Chia, L.; Dong, Y.-C.; Tan, R.B.H. Stabilized amorphous state of ibuprofen byco-spray drying with mesoporous SBA-15 to enhance dissolution properties. J. Pharm. Sci. 2010, 99, 1997–2007. [Google Scholar] [CrossRef]
- Mellaerts, R.; Houthoofd, K.; Elen, K.; Chen, H.; Van Speybroeck, M.; Van Humbeeck, J.; Augustijns, P.; Mullens, J.; Van den Mooter, G.; Martens, J.A. Aging behavior of pharmaceutical formulations of itraconazole on SBA-15 ordered mesoporous silica carrier material. Microporous Mesoporous Mater. 2010, 130, 154–161. [Google Scholar] [CrossRef]
- Mellaerts, R.; Jammaer, A.A.G.; Speybroeck, M.V.; Chen, H.; Humbeeck, J.V.; Augustijns, P.; Van den Mooter, G.; Martens, J.A. Physical state of poorly water soluble therapeutic molecules loaded into SBA-15 ordered mesoporous silica carriers: A case study with itraconazole and ibuprofen. Langmuir 2008, 24, 8651–8659. [Google Scholar] [CrossRef] [PubMed]
- Miura, H.; Kanebako, M.; Shirai, H.; Nakao, H.; Inagi, T.; Terada, K. Stability of amorphous drug, 2-benzyl-5-(4-chlorophenyl)-6-[4-methylthio)phenyl]-2H-pyridazin-3-one, in silica mesopores and measurement of its molecular mobility by solid-state 13C NMR spectroscopy. Int. J. Pharm. 2011, 410, 61–67. [Google Scholar] [CrossRef]
- Sliwinska-Bartkowiak, M.; Dudziak, G.; Gras, R.; Sikorski, R.; Radhakrishnan, R.; Gubbins, K.E. Freezing behavior in porous glasses and MCM-41. Colloids Surf. A 2001, 187, 523–529. [Google Scholar] [CrossRef]
- Rengarajan, G.; Enke, D.; Steinhart, M.; Beiner, M. Stabilization of the amorphous state of pharmaceuticals in nanopores. J. Mater. Chem. 2008, 18, 2537–2539. [Google Scholar] [CrossRef]
- Qi, L.; Ma, J.; Cheng, H.; Zhao, Z. Micrometer-sized mesoporous silica spheres grown under static conditions. Chem. Mater. 1998, 10, 1623–1626. [Google Scholar] [CrossRef]
- Slowing, I.I.; Vivero-Escoto, J.L.; Wu, C.-W.; Lin, V.S.-Y. Mesoporous silica nanoparticles as controlled release drug delivery and gene transfection carriers. Adv. Drug Deliv. Rev. 2008, 60, 1278–1288. [Google Scholar] [CrossRef]
- Singh, A.; Worku, Z.A.; Van den Mooter, G. Oral formulation strategies to improve solubility of poorly water-soluble druga. Expert Opin. Drug Deliv. 2011, 8, 1361–1378. [Google Scholar] [CrossRef]
- Kumar, D.; Chirravuri, S.V.S.; Shastri, N.R. Impact of surface area of silica particles on dissolution rate and oral bioavailability of poorly water soluble drugs: A case study with aceclofenac. Int. J. Pharm. 2014, 461, 459–468. [Google Scholar] [CrossRef]
- Meynen, V.; Cool, P.; Vansant, E.F. Verified syntheses of mesoporous materials. Microporous Mesoporous Mater. 2009, 125, 170–223. [Google Scholar] [CrossRef]
- Schumacher, K.; Ravikovitch, P.I.; Chesne, A.D.; Neimark, A.V.; Unger, K.K. Characterization of MCM-48 materials. Langmuir 2000, 16, 4648–4654. [Google Scholar] [CrossRef]
- Zelenak, V.; Halamova, D.; Gaberova, L.; Bloch, E.; Llewellyn, P. Amine-modified SBA-12 mesoporous silica for carbon dioxide capture: Effect of amine basicity on sorption properties. Microporous Mesoporous Mater. 2008, 116, 358–364. [Google Scholar] [CrossRef]
- Moritz, M.; Łaniecki, M. SBA-15 mesoporous material modified with APTES as the carrier for 2-(3-benzoylphenyl)propionic acid. Appl. Surf. Sci. 2012, 258, 7523–7529. [Google Scholar] [CrossRef]
- Geszke-Moritz, M.; Moritz, M. APTES-modified mesoporous silicas as the carriers for poorly water-soluble drug. Modeling of diflunisal adsorption and release. Appl. Surf. Sci. 2016, 368, 348–359. [Google Scholar] [CrossRef]
- Moritz, M.; Geszke-Moritz, M. Amine-modified SBA-15 and MCF mesoporous molecular sieves as promising sorbents for natural antioxidant. Modeling of caffeic acid adsorption. Mater. Sci. Eng. C 2016, 61, 411–421. [Google Scholar] [CrossRef]
- Vallet-Regí, M.; Colilla, M.; Izquierdo-Barba, I.; Manzano, M. Mesoporous silica nanoparticles for drug delivery: Current insights. Molecules 2018, 23, 47. [Google Scholar] [CrossRef] [Green Version]
- Stephen, S.; Gorain, B.; Choudhury, H.; Chatterjee, B. Exploring the role of mesoporous silica nanoparticle in the development of novel drug delivery systems. Drug Deliv. Translat. Res. 2021, 12, 105–123. [Google Scholar] [CrossRef]
- Attia, M.S.; Hassaballah, M.Y.; Abdelqawy, M.A.; Emad-Eldin, M.; Farag, A.K.; Negida, A.; Ghaith, H.; Emam, S.E. An uptaded review of mesoporous carbon as a novel drug delivery system. Drug Dev. Ind. Pharm. 2021, 47, 1029–1037. [Google Scholar] [CrossRef]
- Iturrioz-Rodríguez, N.; Correa-Duarte, M.A.; Fanarraga, M.L. Controlled drug delivery systems for cancer based on mesoporous silica nanoparticles. Int. J. Nanomed. 2019, 14, 3389–3401. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Xhao, Q.; Han, N.; Bai, L.; Li, J.; Liu, J.; Che, E.; Hu, L.; Zhang, Q.; Jiang, T.; et al. Mesoporous silica nanoparticles in drug delivery and biomedical applications. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 313–327. [Google Scholar] [CrossRef]
- Wen, J.; Yang, K.; Liu, F.; Li, H.; Xu, Y.; Sun, S. Diverse gatekeepers for mesoporous silica nanoparticle based drug delivery systems. Chem. Soc. Rev. 2017, 46, 6024. [Google Scholar] [CrossRef]
- Rosenholm, J.M.; Sahlgren, C.; Lindén, M. Towards multifunctional, targeted drug delivery systems using mesoporous silica nanoparticles—Opportunities & challenges. Nanoscale 2010, 2, 1870–1883. [Google Scholar] [PubMed]
- Vallet-Regí, M.; Balas, F.; Arcos, D. Mesoporous materials for drug delivery. Angew. Chem. Int. Ed. 2007, 46, 7548–7558. [Google Scholar] [CrossRef] [PubMed]
- Bharti, C.; Nagaich, U.; Pal, A.K.; Gulati, N. Mesoporous silica nanoparticles in target drug delivery system: A review. Int. J. Pharm. Investig. 2015, 5, 124–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, Q.; Lin, Y.; Han, N.; Li, X.; Geng, H.; Wang, X.; Cui, Y.; Wang, S. Mesoporous carbon nanomaterials in drug delivery and biomedical applications. Drug Deliv. 2017, 24, 94–107. [Google Scholar] [CrossRef]
- Trzeciak, K.; Chotera-Ouda, A.; Bak-Sypien, I.I.; Potrzebowski, M.J. Mesoporous silica particles as drug delivery systems—The state of the art in loading methods and the recent progress in analytical techniques for monitoring these processes. Pharmaceutics 2021, 13, 950. [Google Scholar] [CrossRef]
- Hadisoewignyo, L.; Hartono, S.B.; Kresnamurti, A.; Soeliono, I.; Nataline, Y.; Prakoso, G.A.; Aulia, D.A.R.E. Evaluation of anti-inflammatory activity and biocompatibility of curcumin loaded mesoporous silica nanoparticles as an oral drug delivery system. Adv. Nat. Sci. Nanosci. Nanotechnol. 2018, 9, 035007. [Google Scholar] [CrossRef]
- Gou, K.; Wang, Y.; Guo, X.; Wang, Y.; Bian, Y.; Zhao, H.; Guo, Y.; Pang, Y.; Xie, L.; Li, S.; et al. Carboxyl-functionalized mesoporous silica nanoparticles for the controlled delivery of poorly water-soluble non-steroidal anti-inflammatory drugs. Acta Biomater. 2021, 134, 576–592. [Google Scholar] [CrossRef]
- Rai, S.K.; Shakambari, G.; Rajan, M.; Praphakar, R.A.; Ashokkumar, B.; Pugazhendhi, A.; Varalakshmi, P. Mesoporous nanoparticles for the delivery of (9S,E)-8-ethyl-9-methylnonadec-6-en-3-one (EME): A study of anti-inflammatory and tumor suppressing potential in RAW 264.7, HeLa and HepG2 cell lines. Process Biochem. 2021, 111, 1–11. [Google Scholar] [CrossRef]
- Crusz, S.M.; Balkwill, F.R. Inflammation and cancer: Advances and new agents. Nat. Rev. Clin. Oncol. 2015, 12, 584–596. [Google Scholar] [CrossRef]
- Świeboda, P.; Filip, R.; Prystupa, A.; Drozd, M. Assessment of pain: Types, mechanisms and treatment. Ann. Agric. Environ. Med. 2013, 1, 2–7. [Google Scholar]
- Honore, P.; Rogers, S.D.; Schwei, M.J.; Salak-Johnson, J.L.; Luger, N.M.; Sabino, M.C.; Clohisy, D.R.; Mantyh, P.W. Murine models of inflammatory, neuropathic and cancer pain each generates a unique set of neurochemical changes in the spinal cord and sensory neurons. Neuroscience 2000, 98, 585–598. [Google Scholar] [CrossRef]
- Caumo, W.; Deitos, A.; Carvahlo, S.; Leite, J.; Carvahlo, F.; Dussán-Sarria, J.A.; Tarrago, M.G.L.; Souza, A.; Torres, I.L.S.; Fregni, F. Motor cortex excitability and BDNF levels in chronic musculoskeletal pain according to structural pathology. Front. Hum. Neurosci. 2016, 10, 357. [Google Scholar] [CrossRef] [PubMed]
- Lerman, S.F.; Rudich, Z.; Brill, S.; Shalev, H.; Shahar, G. Longitudinal associations between depression, anxiety, pain, and pain-related disability in chronic pain patients. Psychosom. Med. 2015, 77, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Minami, K.; Uezono, Y. The recent progress in research on effects of anesthetics and analgesics on G protein-coupled receptors. J. Anesth. 2013, 27, 284–292. [Google Scholar] [CrossRef]
- Schug, S.A.; Garrett, W.R.; Gillespie, G. Opioid and non-opioid analgesics. Best Pract. Res. Clin. Anaesthesiol. 2003, 17, 91–110. [Google Scholar] [CrossRef]
- Berde, A.; Nurko, S. Opioid side effects—Mechanism-based therapy. N. Eng. J. Med. 2008, 358, 2400–2402. [Google Scholar] [CrossRef]
- Hser, Y.-I.; Evans, E.; Grella, C.; Ling, W.; Anglin, D. Long-term course of opioid addiction. Harv. Rev. Psychiatry 2015, 23, 76–89. [Google Scholar] [CrossRef]
- Hebbes, C.; Lambert, D. Non-opioid analgesics. Anaesth. Intensive Care Med. 2011, 12, 69–72. [Google Scholar] [CrossRef]
- Rainsford, K.D. Ibuprofen: Pharmacology, efficacy and safety. Inflammopharmacology 2009, 17, 275–342. [Google Scholar] [CrossRef]
- Fadeyi, O.O.; Obafemi, C.A.; Adewunmi, C.O.; Iwalewa, E.O. Antipyretic, analgesic, anti-inflammatory and cytotoxic effects of four derivatives of salicylic acid and anthranilic acid in mice and rats. Afr. J. Biotechnol. 2004, 3, 426–431. [Google Scholar]
- Xu, S.; Rouzer, C.A.; Marnett, L.J. Oxicams, a class of nonsteroidal anti-inflammatory drugs and beyond. IUBMB Life 2014, 66, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Grösch, S.; Niederberger, E.; Geisslinger, G. Investigational drugs targeting the prostaglandin E2 signaling pathway for the treaatment of inflammatory pain. Expert Opin. Investig. Drugs 2017, 26, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.-M.; An, J. Cytokines, inflammation and pain. Int. Anesthesiol. Clin. 2007, 45, 27–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, T.J.; Morley, J. Prostaglandins as potentiators of increased vascular permeability in inflammation. Nature 1973, 246, 215–217. [Google Scholar] [CrossRef]
- Hawkey, C.J. COX-2 inhibitors. Lancet 1999, 353, 307–314. [Google Scholar] [CrossRef]
- Rainsford, K.D. Profile and mechanisms of gastrointestinal and other side effects of nonsteroidal anti-inflammatory drugs (NSAIDs). Am. J. Med. 1999, 107, 27–35. [Google Scholar] [CrossRef]
- Lochs, H.; Mayer, M.; Fleig, W.E.; Mortensen, P.B.; Bauer, P.; Genser, D.; Petritsch, W.; Raithel, M.; Hoffmann, R.; Gross, V.; et al. Prophylaxis of postoperative relapse in Crohn’s disease with mesalamine: European Cooperative Crohn’s Disease Study VI. Gastroenterology 2000, 118, 264–273. [Google Scholar] [CrossRef]
- Amiry, F.; Sazegar, M.R.; Mahmoudi, A. Smart polymeric nanocomposite based on protonated aluminosilicate curcumin, and chitosan for mesalamine drug delivery as an anti-inflammatory nanocarrier. Microporous Mesoporous Mater. 2022, 330, 111533. [Google Scholar] [CrossRef]
- Chang, J.-H.; Gabison, E.E.; Kato, T.; Azar, D.T. Corneal neovascularization. Curr. Opin. Ophthalmol. 2001, 12, 242–249. [Google Scholar] [CrossRef] [Green Version]
- Lyu, N.; Zhao, Y.; Xiang, J.; Fan, X.; Huang, C.; Sun, X.; Xu, J.; Xu, Z.P.; Sun, J. Inhibiting corneal neovascularization by sustainably releasing anti-VEGF and anti-inflammation drugs from silica-thermogel nanohybrids. Mater. Sci. Eng. C 2021, 128, 112274. [Google Scholar] [CrossRef]
- Siemerink, M.J.; Augustin, A.J.; Schlingemann, R.O. Mechanisms of ocular angiogenesis and its molecular mediators. Anti-VEGF 2010, 46, 4–20. [Google Scholar]
- Suleyman, H.; Cadirci, E.; Albayrak, A.; Halici, Z. Nimesulide is a selective COX-2 inhibitory, atypical non-steroidal anti-inflammatory drug. Curr. Med. Chem. 2008, 15, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Yang, K.G.B.; Wang, Y.; Pu, X.; Li, S.; Li, H. Enlarged pore size chiral mesoporous silica nanoparticles loaded poorly water-soluble drug perform superior delivery effect. Molecules 2019, 24, 3552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huskisson, E.C. Nimesulide, a balanced drug for the treatment of osteoarthritis. Clin. Exp. Rheumatol. 2001, 19, S21–S25. [Google Scholar] [PubMed]
- Wu, L.; Gou, K.; Guo, X.; Guo, Y.; Chen, M.; Hou, J.; Li, S.; Li, H. Dual response to pH and chiral microenvironments for the release of a flurbiprofen-loaded chiral self-assembled mesoporous silica drug delivery system. Colloids Surf. B 2021, 199, 111501. [Google Scholar] [CrossRef]
- Tokunaga, M.; Ohuchi, K.; Yoshizawa, S.; Tsurufuji, S.; Rikimaru, A.; Wakamatsu, E. Change of prostaglandin E level in joint fluids after treatment with flurbiprofen in patients with rheumatoid arthritis and osteoarthritis. Ann. Rheum. Dis. 1981, 40, 462–465. [Google Scholar] [CrossRef] [Green Version]
- Brogden, R.N.; Heel, W.C.; Speight, T.M.; Avery, G.S. Flurbiprofen: A review of its pharmacological properties and therapeutic use in rheumatic diseases. Drugs 1979, 18, 417–438. [Google Scholar] [CrossRef]
- Fietta, P.; Fietta, P.; Delsante, G. Central nervous system effects of natural and synthetic glucocorticoids. Psychiatry Clin. Neurosci. 2009, 63, 613–622. [Google Scholar] [CrossRef]
- Stahn, C.; Buttgereit, F. Genomic and nongenomic effects of glucocorticosteroids. Nat. Clin. Pract. Rheumatol. 2008, 4, 525–533. [Google Scholar] [CrossRef]
- Vegiopoulos, A.; Herzig, S. Glucocorticosterids, metabolism and metabolic diseases. Mol. Cell. Endocrinol. 2007, 275, 43–61. [Google Scholar] [CrossRef] [Green Version]
- Cain, D.; Cidlowski, J. Immune regulation by glucocorticoids. Nat. Rev. Immunol. 2017, 17, 233–247. [Google Scholar] [CrossRef]
- Dygai, A.M.; Shakhov, V.P.; Goldberg, E.D. Role of glucocorticoids in the regulation of bone marrow hemopoiesis in stress reaction. Biomed. Pharmacother. 1991, 45, 9–14. [Google Scholar] [CrossRef]
- Stahn, C.; Löwenberg, M.; Hommes, D.W.; Buttgereit, F. Molecular mechanisms of glucocorticoid action and selective glucocorticoid receptor agonists. Mol. Cell. Endocrinol. 2007, 275, 71–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michels, A.; Michels, N. Addison Disease: Early detection and treatment principles. Am. Fam. Physician 2014, 89, 563–568. [Google Scholar]
- Paragliola, R.M.; Papi, G.; Pontecorvi, A.; Corsello, S.M. Treatment with synthetic glucocorticosteroids and the hypothalamus-pituitary-adrenal axis. Int. J. Mol. Sci. 2017, 18, 2201. [Google Scholar] [CrossRef]
- Broersen, L.H.A.; Pereira, A.M.; Jørgensen, J.O.L.; Dekkers, O.M. Adrenal insufficiency in corticosteroids use: Systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2015, 100, 2171–2180. [Google Scholar] [CrossRef] [PubMed]
- Amr, N.H.; Mahmoud, R.A.A.; Youssef, O.; Toaima, N.N.; Elsedfy, H. Effect of long-term glucocorticoid therapy on cardiac functions in children with congenital adrenal hyperplasia. Clin. Endocrinol. 2021, 94, 210–218. [Google Scholar] [CrossRef]
- Shibli-Rahhal, A.; Beek, M.V.; Schlechte, J.A. Cushing’s syndrome. Clin. Dermatol. 2006, 24, 260–265. [Google Scholar] [CrossRef]
- Barnes, P.J. Glucocorticosteroids: Current and future directions. Brit. J. Pharmacol. 2011, 163, 29–43. [Google Scholar] [CrossRef] [Green Version]
- Gold, R.; Buttgereit, F.; Toyka, K.V. Mechanism of action of glucocorticosteoid hormones: Possible implications for therapy of neuroimmunological disorders. J. Neuroimmunol. 2001, 117, 1–8. [Google Scholar] [CrossRef]
- Shimada, T.; Hiwatashi, N.; Yamazaki, H. Relationship between glucocorticoid receptor and response to glucocorticoid therapy in ulcerative colitis. Dis. Colon Rectum 1997, 40, S54–S58. [Google Scholar] [CrossRef]
- Gao, R.; Li, Y.; Cao, Y.; Zheng, R.; Tang, L.; Yang, J.; Lu, X. Glucocorticoid versus traditional therapy for hepatitis B virus-related acute-on-chronic liver failure. A systematic review and meta-analysis. Medicine 2020, 99, e20604. [Google Scholar] [CrossRef]
- Niewoehner, D.E.; Erbland, M.L.; Deupree, R.H.; Collins, D.; Gross, N.J.; Light, R.W.; Anderson, P.; Morgan, N.A. Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. N. Eng. J. Med. 1999, 340, 1941–1947. [Google Scholar] [CrossRef]
- Kaneda, T.; Iwai, S.; Suematsu, T.; Yamamoto, R.; Takata, M.; Higashikata, T.; Ino, H.; Tsujibata, A. Acute necrotizing eosinophilic myocarditis complicated by complete atriventricular block promptly responded to glucocorticoid therapy. J. Cardiol. Cases 2017, 16, 5–8. [Google Scholar] [CrossRef] [Green Version]
- Ahluwalia, A. Topical glucocorticoids and the skin-mechanisms of action: An uptade. Mediat. Inflamm. 1998, 7, 183–193. [Google Scholar] [CrossRef]
- Hua, C.; Buttgereit, F.; Combe, B. Glucocorticosteroids in rheumatoid arthritis: Current status and future studies. RMD Open 2020, 6, e000536. [Google Scholar] [CrossRef] [Green Version]
- Sadowska, A.M.; Klebe, B.; Germonpré, P.; De Backer, W.A. Glucocorticosteroids as antioxidants in treatment of asthma and COPD: New application for an old medication? Steroids 2007, 72, 1–6. [Google Scholar] [CrossRef]
- Shapiro, A.G. Corticosteroids in the treatment of allergic disease: Principles and practise. Pediatric Clin. North Am. 1983, 30, 955–971. [Google Scholar] [CrossRef]
- Gaynon, P.S.; Lustig, R.H. The use of glucocorticoids in accute lymphoblastic leukemia of childhood. Molecular, cellular, and clinical considerations. J. Pediatric Hematol. Oncol. 1995, 17, 1–12. [Google Scholar] [CrossRef]
- Weller, M. Glucocorticoid treatment of primary CNS lymphoma. J. Neuro-Oncol. 1999, 43, 237–239. [Google Scholar] [CrossRef]
- Fricke, L.; Klüter, H.; Feddersen, A.; Doehn, C.; Steinhoff, J.; Hoyer, J.; Sack, K. Preoperative application of glucocorticosteroids efficaciously reduces the primary immunological response in kidney transplantation. Clin. Transplant. 1996, 10, 432–436. [Google Scholar] [PubMed]
- Choo, K.J.L.; Simons, F.E.R.; Sheikh, A. Glucocorticoids for the treatment of anaphylaxis (Review). Evid.-Based Child Health 2013, 8, 1276–1294. [Google Scholar] [CrossRef] [PubMed]
- Kaal, E.C.A.; Vecht, C.J. The management of brain endema in brain tumors. Curr. Opin. Oncol. 2004, 16, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Gulin-Sarfraz, T.; Jonasson, S.; Wigenstam, E.; Haartman, E.v.; Bucht, A.; Rosenholm, J.M. Feasibility study of mesoporous silica particles for pulmonary drug delivery: Therapeutic treatment with dexamethasone in a mouse model of airway inflammation. Pharmaceutics 2019, 11, 149. [Google Scholar] [CrossRef] [Green Version]
- García-Fernández, A.; Sancho, M.; Bisbal, V.; Amorós, P.; Marcos, M.D.; Orzáez, M.; Sancenón, F.; Martínez-Máñez, R. Targeted-lung delivery of dexamethasone using gated mesoporous silica nanoparticles. A new therapeutic approach for acute lung injury treatment. J. Control. Release 2021, 337, 14–26. [Google Scholar] [CrossRef]
- Hashemikia, S.; Hemmatinejad, N.; Ahmadi, E.; Montazer, M. Antibacterial and anti-inflammatory drug delivery properties on cotton fabric using betamethasone-loaded mesoporous silica particles stabilized with chitosan and silicone softener. Drug Deliv. 2015, 23, 2946–2955. [Google Scholar] [CrossRef] [Green Version]
- Dibas, A.; Yorio, T. Glucocorticoid therapy and ocular hypertension. Eur. J. Pharmacol. 2016, 787, 57–71. [Google Scholar] [CrossRef] [Green Version]
- Vandewalle, J.; Luypaert, A.; De Bosscher, K.; Libert, C. Therapeutic mechanisms of glucocorticoids. Trends Endocrinol. Metab. 2018, 29, 42–54. [Google Scholar] [CrossRef]
- Leung, K.W.; Wong, A.S.-T. Pharmacology of ginsenosides: A literature review. Chin. Med. 2010, 5, 20. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.-Y.; Shie, M.-Y.; Lee, A.-X.; Chou, Y.-T.; Chiang, C.; Lin, C.-P. 3D-Printed ginsenoside Rb1-loaded mesoporous calcium silicate/calcium sulfate scaffolds for inflammation inhibition and bone regeneration. Biomedicines 2021, 9, 907. [Google Scholar] [CrossRef]
- He, M.; Qin, Z.; Liang, X.; He, X.; Zhu, B.; Lu, Z.; Wei, Q.; Zheng, L. A pH-responsive mesoporous silica nanoparticles-based drug delivery system with controlled release of andrographolide for OA treatment. Regener. Biomater. 2021, 8, rbab020. [Google Scholar] [CrossRef] [PubMed]
- Mussard, E.; Cesaro, A.; Lespessailles, E.; Legrain, B.; Berteina-Raboin, S.; Toumi, H. Andrographolide, a natural antioxidant: An uptade. Antioxidants 2019, 8, 571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dadej, A.; Woźniak-Braszak, A.; Bilski, P.; Piotrowska-Kempisty, H.; Józkowiak, M.; Geszke-Moritz, M.; Moritz, M.; Dadej, D.; Jelińska, A. Modification of the release of poorly soluble sulindac with the APTES-modified SBA-15 mesoporous silica. Pharmaceutics 2021, 13, 1693. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhang, S.; Zhang, X.; Hou, Y.; Meng, X.; Li, G.; Xu, F.; Teng, L.; Qi, Y.; Sun, F.; et al. Folate receptor-targeting semiconducting polymer dots hybrid mesoporous silica nanoparticles against rheumatoid arthritis through synergistic photothermal therapy, photodynamic therapy, and chemotherapy. Int. J. Pharm. 2021, 607, 120947. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Zheng, N.; Chen, L.; Xie, L.; Cui, M.; Li, S.; Xu, L. Effect of shape on mesoporous silica nanoparticles for oral delivery of indomethacin. Pharmaceutics 2019, 11, 4. [Google Scholar] [CrossRef] [Green Version]
- Kurtuldu, F.; Kaňková, H.; Beltrán, A.M.; Liverani, L.; Galusek, D.; Boccaccini, A. Anti-inflammatory and antibacterial activities of cerium-containing mesoporous bioactive glass nanoparticles for drug-free biomedical applications. Mater. Today Bio 2021, 12, 100150. [Google Scholar] [CrossRef]
- Eleftheriadis, G.K.; Filippousi, M.; Tsachouridou, V.; Darda, M.-A.; Sygellou, L.; Kontopoulou, I.; Bouropoulos, N.; Steriotis, T.; Charalambopoulou, G.; Vizirianakis, I.S.; et al. Evaluation of mesoporous carbon aerogels as carriers of the non-steroidal anti-inflammatory drug ibuprofen. Int. J. Pharm. 2016, 515, 262–270. [Google Scholar] [CrossRef]
- Du, X.; Kleitz, F.; Li, X.; Huang, H.; Zhang, X.; Qiao, S.-Z. Disulfide-bridged organosilica frameworks: Designed, synthesis, redox-triggered biodegradation, and nanobiomedical applications. Adv. Funct. Mater. 2018, 28, 1707325. [Google Scholar] [CrossRef] [Green Version]
- Bithi, K.A.; Minami, H.; Hossain, M.K.; Rahman, M.M.; Rahman, M.A.; Gafur, M.A.; Ahmad, H. Cationic polyelectrolyte grafted mesoporous magnetic silica composite particles for targeted drug delivery and thrombolysis. Materialia 2020, 11, 100676. [Google Scholar] [CrossRef]
- Beñová, E.; Hornebecq, V.; Zeleňák, V.; Huntošová, V.; Almáši, M.; Máčajová, M.; Bergé-Lefranc, D. pH-responsive mesoporous silica drug delivery system, its biocompatibility and co-adsorption/co-release of 5-fluorouracil and naproxen. Appl. Surf. Sci. 2021, 561, 150011. [Google Scholar] [CrossRef]
- Zhou, J.; Zhu, F.; Li, J.; Wang, Y. Concealed body mesoporous silica nanoparticles for orally delivering indometacin with chiral recognition function. Mater. Sci. Eng. C 2018, 90, 314–324. [Google Scholar] [CrossRef] [PubMed]
- Gou, K.; Guo, X.; Wang, Y.; Wang, Y.; Sang, Z.; Ma, S.; Guo, Y.; Xie, L.; Li, S.; Li, H. Chiral microenvironment-responsive mesoporous silica nanoparticles for delivering indometacin with chiral recognition function. Mater. Des. 2022, 214, 110359. [Google Scholar] [CrossRef]
- Zeleňáková, A.; Szűcsová, J.; Nagy, L.; Girman, V.; Zeleňák, V.; Huntošová, V. Magnetic characterization and moderate cytotoxicity of magnetic mesoporous silica nanocomposite for drug delivery of naproxen. Nanomaterials 2021, 11, 901. [Google Scholar] [CrossRef] [PubMed]
- Lau, M.; Sealy, B.; Combes, V.; Morsch, M.; Garcia-Bennett, A.E. Enhanced antioxidant effects of the anti-inflammatory compound probucol when released from mesoporous silica particles. Pharmaceutics 2022, 14, 502. [Google Scholar] [CrossRef]
- Yan, X.; Zhang, L.; Zhang, Y.; Qiao, K.; Yan, Z.; Komarneni, S. Amine-modified mesocellular silica foams for CO2 capture. Chem. Eng. J. 2011, 193, 918–924. [Google Scholar] [CrossRef]
- Lin, Y.-S.; Hurley, K.R.; Haynes, C.L. Critical considerations in the biomedical use of mesoporous silica nanoparticles. J. Phys. Chem. Lett. 2012, 3, 364–374. [Google Scholar] [CrossRef]
- Chen, W.; Wang, J.; Cheng, L.; Du, W.; Wang, J.; Pan, W.; Qiu, S.; Song, L.; Ma, X.; Hu, Y. Polypyrrole-coated mesoporous TiO2 nanocomposites simultaneously loading DOX and aspirin prodrugs for a synergistic theranostic and anti-inflammatory effect. ACS Appl. Bio Mater. 2021, 4, 1483–1492. [Google Scholar] [CrossRef]
- De Almeida Junior, S.; Pereira, P.M.; de Sousa Tótoli, V.; Neves, E.S.; Monochio, M.; Alvarenga, A.W.O.; Hori, J.I.; Braz, W.R.; Rocha, L.A.; Nassar, E.J.; et al. Incorporation of indomethacin into a mesoporous silica nanoparticle enhances the anti-inflammatory effect indomethacin into a mesoporous silica. Eur. J. Pharm. Sci. 2021, 157, 105601. [Google Scholar] [CrossRef]


| Parameter | Drug | Mesoporous Silica | Effect on Drug Loading/Release | Ref. |
|---|---|---|---|---|
| Pore size, pore geometry | Atorvastatin | Hexagonal SBA-15 silica, MSF with continuous pore system | Significant enhancement in the rapid burst release of drug from both silica (MSF showed a higher degree of burst release) The faster drug release from MSF resulted from bigger pore size of this carrier in comparison to SBA-15 material The 3D spherical pore system and the particular geometry of MSF made the molecular diffusion easier from the inner pores into the release fluid thus avoiding pore blocking | [44] |
| Pore geometry | Carvedilol | Hexagonal MCM-41 SBA-16 cage-like mesoporous silica | Improved drug dissolution rate for both carriers compared with crystalline form SBA-16 displayed a faster release kinetics which may be attributed to the 3D interconnected pore networks in comparison to 2D cylindrical pores of MCM-41 | [45] |
| Pore size | Furosemide | MCM-41, SBA-15 | Fast drug release for both silicas was observed with respect to the crystalline drug (faster for SBA-15) When pores were larger, the diffusion of the drug molecule into the dissolution medium was improved | [46,47] |
| Pore volume and pore morphology | Ibuprofen | SBA-15 MCM-41 TUD-1 | Total pore volume has a significant influence on the degree of drug loading TUD-1 exhibited the fastest drug release due to its highly accessible pore network compared to the undirectional, uniform hexagonal mesopores of SBA-15 and MCM-41 | [48] |
| Particle morphology | Ibuprofen | Irregular and spherical MCM-41 particles | With nearly the same loading of ibuprofen irregularly-shaped particles (with the largest pores) released the drug fastest than spherical particles | [49] |
| Pore size | Ibuprofen | MSNs (hexagonal MCM-41 and SBA-15, and cubic MCM-48) | Loading capacity in the presence of sufficient ibuprofen was found to be proportional to the pore dimensions (mesopore size SBA-15 > MCM-48 > MCM-41) | [13,50,51] |
| Pore size and pore geometry | Ibuprofen | MSNs (MCM-41, SBA particles with different pore sizes: cubic SBA-1 with interconnected porosity and micro-/meso-porous hexagonal SBA-3) | Drug loading degree and the release rate was consistent with the decrease in their pore size Interconnected small opening between pore channels in SBA-1 increased the diffusion of encapsulated molecules | [52] |
| Pore geometry, particle morphology | Ibuprofen | Hexagonal MCM-41 Cubic MCM-48 | With the same spherical morphology and particle size but different pore geometry MCM-48 possessing higher surface area and pore volume exhibited significantly larger loading capacity and much quicker drug release than MCM-41 | [53] |
| Pore size | Ibuprofen | MCM-41, SBA-15, SBA-15-LP | The pore size effected the physical state of the drug: drug loaded inside SBA-15-LP (pore size 20 nm) was organized in nanocrystals, drug loaded in MCM-41 and SBA-15 (pore size smaller than 10 nm) was in amorphous state Amorphous drug showed a rapid dissolution while nanocrystalline drug showed a slower dissolution rate | [54] |
| Pore size | Itraconazole | SBA-15 with pore diameters ranging from 4.5 to 9.0 nm | Broadening the pore size from 4.5 to 6.4 nm greatly improved drug release The supplementary increase in the pore size up to 7.9 and 9.0 nm showed only a minor additional increase | [55] |
| Class of Anti-Inflammatory Agents | Drug | Administration Route | Drug Form |
|---|---|---|---|
| NSAIDs | Aceclofenac | Oral | Film-coated tablets |
| Acidum salicylicum | Topical | Cream Ointment | |
| Aspirin | Oral | Effervescent tablets Enteric tablets Granules Modified release tablets Powder Tablets Tablets for the socket | |
| Bromfenac | Intraocular | Eye drops | |
| Dexibuprofen | Oral | Film-coated tablets | |
| Diclofenac | Oral | Enteric tablets Film-coated enteric tablets Film-coated tablets Modified-release and prolonged-release capsules Modified-release and prolonged-release tablets | |
| Topical | Adhesive bandage Aerosol Gel | ||
| Diethylamine salicylate | Topical | Cream Gel | |
| Etofenamate | Topical | Aerosol Cream Gel Solution | |
| Flurbiprofen | Oral | Lozenges Prolonged-release capsules | |
| Ibuprofen | Intravenous | Solution for injection | |
| Oral | Capsules Effervescent granules Film-coated tablets Suspension Syrup Tablets | ||
| Rectal | Rectal suppositories | ||
| Topical | Cream Gel | ||
| Indomethacin | Intravenous | Solution for injection | |
| Oral | Prolonged-release tablets | ||
| Rectal | Rectal capsules Rectal suppositories | ||
| Topical | Ointment | ||
| Ketoprofen | Intravenous | Solution for injection | |
| Oral | Film-coated tablets Modified-release capsules Modified-release tablets Suspension | ||
| Topical | Gel Spray | ||
| Rectal | Rectal suppositories | ||
| Ketorolac | Intraocular | Eye drops | |
| Meloxicam | Intravenous | Solution for injection | |
| Oral | Tablets | ||
| Mefenamic acid | Oral | Tablets | |
| Metamizole | Intravenous | Solution for injection | |
| Oral | Granules for oral solution Tablets | ||
| Rectal | Rectal suppositories | ||
| Methyl salicylate | Topical | Cream Ointment | |
| Naproxen | Oral | Film-coated tablets Enteric tablets Suspension Tablets | |
| Rectal | Rectal suppositories | ||
| Topical | Gel | ||
| Nepafenac | Intraocular | Eye suspension | |
| Nimesulide | Oral | Granules/powder for suspension preparation Tablets | |
| Phenazone | In-ear | Ear drops | |
| Phenylbutazone | Topical | Ointment | |
| Rectal | Rectal suppositories | ||
| Piroxicam | Oral | Film-coated tablets Powder for oral solution Tablets | |
| Tolfenamic acid | Oral | Tablets | |
| Steroids | Beclometasone | Intranasal | Aerosol Suspension |
| Pulmonary | Aerosol Solution | ||
| Betamethasone dipropionate | Topical | Cream Ointment Solution | |
| Betamethasone sodium phosphate | Intramuscular | Suspension for injection | |
| Intravenous | Solution for injection | ||
| Topical | Cream Ointment | ||
| Budesonide | Intranasal | Aerosol | |
| Oral | Enteric capsules Prolonged-release capsules | ||
| Pulmonary | Aerosol Powder in capsules for inhalation Powder for inhalation | ||
| Clobetasol propionate | Topical | Cream Ointment Shampoo Solution | |
| Dexamethasone | Intraocular | Eye drops Eye suspension Ointment | |
| Oral | Tablets | ||
| Topical | Aerosol | ||
| Fludricortisone acetate | Intraocular/in-ear | Ointment Suspension | |
| Oral | Tablets | ||
| Hydrocortisone | Intravenous | Powder and solvent for intravenous solution | |
| Oral | Tablets | ||
| Rectal | Rectal ointment Rectal suppositories | ||
| Topical | Aerosol Cream Ointment | ||
| Mometasone furoate | Oral | Tablets | |
| Pulmonary | Powder for inhalation | ||
| Topical | Cream Ointment Solution | ||
| Prednisolone | Oral | Tablets | |
| Topical | Solution |
| Drug Delivery System (Drug/Carrier) | Physicochemical Characterization Methods | Size/Morphology of Mesoporous Structure | In Vitro Studies | In Vivo Studies | Ref. |
|---|---|---|---|---|---|
| Andrographolide/Mesoporous silica nanoparticles modified with pH-responsive polyacrylic acid | TEM DLS FT-IR | 100 nm/nanoparticles | Drug release Cytotoxicity test Live/dead cells assay | Histological evaluation Changes in articular cartilage examination | [151] |
| Aspirin/Cationic polyelectrolyte grafted mesoporous magnetic silica composite particles (magnetic iron oxide Fe3O4 microparticles modified with SiO2 layer and functionalized with vinyl groups) grafted with polyelectrolyte layer composed of isobornyl methacrylate and APTMACl | SEM TEM XRD N2 sorption DLS FT-IR XPS TGA | 430 nm/spherical particles | Anti-inflammatory activity Thrombolytic activity | --- | [159] |
| Betamethasone sodium phosphate /Cotton fabric with grafted SBA-15 mesoporous silica modified with (3-aminopropyl)triethoxysilane particles) stabilized with chitosan and polysiloxane softener | SEM Stiffness test (bending length) Warp direction (tensile strength) Shirley instrument (air permeability) | 1 µm/rope-like morphology | Cytometry Drug release Antibacterial activity | --- | [146] |
| Bevacizumab and cyclosporine A/Silica thermogel nanohybrids (PLGA-PEG-PLGA copolymer and mesoporous silica nanoparticles) | NMR Gel permeation chromatography TEM N2 sorption Zeta potential FT-IR | 40 nm/nanoparticles | Drug release Cytotoxicity Inhibition effect on corneal neovascularization | Corneal neovascularization effectiveness (biosafety) | [110] |
| Cerium/Mesoporous bioactive glass nanoparticles | SEM TEM XRD FT-IR N2 sorption ICP-OES | 100–200 nm/spherical nanoparticles | Anti-inflammatory effect Cytotoxicity Antibacterial activity Biocompatibility | --- | [156] |
| Dexamethasone/Gated mesoporous silica nanoparticles | XRD TEM N2 sorption DLS Zeta potential | 100 nm/nanoparticles | Biocompatibility (cell viability studies) Inflammatory response | Testing of anti-inflammatory effect Histopathological studies | [145] |
| Dexamethasone/Mesoporous silica nanoparticles modified with PEG-PEI copolymer (size 1 μm, 200 nm) | N2 sorption SEM TEM | 200 nm–1 µm/spherical particles | --- | Examination of anti-inflammatory response | [144] |
| 5-Fluorouracil and naproxen/System composed of N-(propyl)aniline modified mesoporous silica nanoparticles (SBA-15) and β-cyclodextrin | N2 sorption TEM TGA Small-angle XRD microcalorimetry | --- | MTT (cell viability) Apoptotic assay | Biocompatibility study (CAM assay, histology) | [160] |
| Ginsenoside Rb1/Mesoporous calcium silicate and calcium sulfate scaffolds | XRD FT-IR SEM | --- | Soaking Cell adhesion and proliferation Fluorescent staining ELISA | Implantation of drug-containing scaffold Histological staining | [150] |
| Ibuprofen/Mesoporous carbon aerogels with different pore sizes (10 nm and 20 nm) | HRTEM N2 sorption XRD DSC XPS Zeta potential | --- | Release studies (HPLC) Cytotoxicity studies Stability tests | --- | [157] |
| Indomethacin/Mesoporous silica nanoparticles modified with D-tartaric acid and L-tartaric acid | N2 sorption FT-IR TEM Zeta potential DSC | 200 nm/nanoparticles | Drug release | Anti-inflammation pharmacodynamics Pharmacokinetics study | [161] |
| Indomethacin/Mesoporous silica nanoparticles modified with TESPSA-L-proline and TESPSA-D-proline | TEM N2 sorption FT-IR Circular dichroism XRD TGA DSC Zeta potential | 135–252 nm/nanoparticles | Drug release Contact angle measurement Hemolysis assay Cytotoxicity Biodegradability | Bio-adhesion study Gastrointestinal tract retention Distribution pharmacokinetics Anti-inflammatory pharmacodynamics | [162] |
| Indomethacin/Mesoporous silica nanorods | TEM N2 sorption FT-IR Small-angle XRD | ---/nanorods, nanoparticles | Cytotoxicity Drug release | Pharmacokinetic studies | [155] |
| Tirapazamine/Folate acid-decorated semiconducting polymer (PCPDTBT) dots hybrid mesoporous silica nanoparticles | Zeta sizer TEM N2 sorption | ---/nanoparticles | Photothermal and photodynamic properties Drug loading and NIR-induced release Cytotoxicity Cellular uptake NIR-induced intracellular hypoxia/singlet oxygen detection | Therapeutic efficacy Histological analysis Serum cytotoxicity assay | [154] |
| Naproxen/Magnetic mesoporous silica nanocomposite (hexagonally ordered mesoporous silica MCM-41 and iron oxide magnetic nanoparticles) | TEM DLS N2 sorption FT-IR Magnetic measurements | 350 nm × 150 nm/rod-like shape | Cytotoxicity studies (MTT, fluorescence microscopy) | --- | [163] |
| Naproxen sodium salt/MCM-41 mesoporous particles modified with photo-sensitive ligand (cinnamic acid derivative) | IR N2 sorption TGA STEM EDX | 1 µm/rod-like shape | Drug release | Drug release | [30] |
| Nimesulide and indomethacin/Carboxyl-functionalized mesoporous silica nanoparticles | FT-IR TEM Small angle XRD N2 sorption Zeta potential TGA | 100–300 nm/spherical nanoparticles | Drug release | Pharmacokinetic studies (determination of drug concentration in blood) Anti-inflammation pharmacodynamics (evaluation of ankle swelling, measurement of serum TNF-α and IL-1β concentrations histopathological examination) | [87] |
| Nimesulide/Chiral mesoporous silica nanoparticles with enlarged mesopores | FT-IR Circular dichroism TEM SEM N2 sorption | 200–300 nm/nanoparticles | Drug dissolution | Pharmacokinetics Anti-inflammatory pharmacodynamics Mucous membrane adhesion | [113] |
| Probucol/Mesoporous silica particles (AMS-6) | SEM DLS Powder XRD FT-IR N2 sorption TGA DSC | 4.7 nm/particles | Oxidative stress and cell viability assays DCFDA cellular reactive oxygen stress measurement Mitochondria hydroxyl assay Nitric oxide assay Peroxynitrite assay COX enzyme activity PGE2 measurement TNF-α assay Flow cytometry | Measurement of ROS concentration in Zebrafish | [164] |
| Sulindac/SBA-15 mesoporous silica modified with (3-aminopropyl)triethoxysilane | XRD DSC TEM SEM FT-IR 1H-NMR Spectrophotometry | 1 µm/rod-like shape | Drug release Cytotoxicity studies | --- | [153] |
| Characterization Method of Loaded API | Information Obtained |
|---|---|
| DSC | Confirmation of drug amorphous/crystalline state |
| Elemental analysis | Assessment of drug content in mesoporous carrier |
| FT-IR | Confirmation of drug presence in the mesoporous carrier/drug-mesoporous carrier interactions |
| Low temperature N2 sorption | Examination of changes in textural properties of mesoporous carrier after drug loading |
| NMR | Confirmation of drug-mesoporous carrier interactions |
| Release profile | Assessment of drug pharmaceutical bioavailability |
| TGA | Evaluation of drug thermal stability/drug amount in carrier |
| XRD | Confirmation of drug amorphous/crystalline state |
| Drug | Carrier | Therapeutic Achievement | Ref. |
|---|---|---|---|
| Aspirin | Cationic polyelectrolyte grafted mesoporous magnetic silica composite particles (magnetic Fe3O4 microparticles modified with SiO2 layer and vinyl groups) grafted with polyelectrolyte layer composed of iBMA and APTMACl | pH-Dependent adsorption and release of anionic drug (through off- and on-capping of polyelectrolyte valve/gate)–controlled drug release in response to specific physiological change Significant thrombolytic activity | [159] |
| EME | Mesoporous silica nanoparticles modified with amine (-NH2) functions | Significant reduction in COX-2 expression EME combined with MSNs showed the therapeutic potential of an anti-inflammatory agent | [88] |
| Flurbiprofen | Chiral self-assembled mesoporous silica nanoparticles functionalized using L/D-tartaric acid | Enhanced pH-response (carboxyl groups induced stronger electrostatic repulsions between drug and the system) Drug release was inhibited in the chiral environment | [115] |
| Indomethacin | APTES-functionalized hexagonal mesoporous silica | Increment of drug activity Prevention of the harmful potential of indomethacin on the gastric and hepatic tissues | [168] |
| Indomethacin | Mesoporous silica nanorods | Excellent dissolution-enhancing effect Better oral bioavailability of drug resulting from ordered helical channels and larger surface area-to-volume ratio of mesoporous silica nanorods | [155] |
| Indomethacin | MSNs modified with TESPSA-L-proline and TESPSA-D-proline | Both kinds of MSNs significantly improved drug dissolution compared with naked MSNs and exhibited different chiral recognition functions for drug release in the simulated chiral environment in vitro D-MSN could facilitate the drug retention, enhance the in vivo distribution and bioavailability due to the chiral recognition function at the molecular level | [162] |
| Naproxen | MCM-41 mesoporous silica modified with magnetic Fe3O4 nanoparticles | After encapsulation of the magnetic nanoparticles into the mesoporous silica the particles keep their superparamagnetic behavior and could be used for vectored drug delivery using magnetic fields and preparation of smart drug delivery systems | [163] |
| Naproxen | SBA-15 mesoporous silica modified with 3-aminopropyl, phenyl and cyclohexyl groups | Functionalization of the surface with more bulky and more hydrophobic ligands (cyclohexyl, phenyl) led to lower drug loading and release More drug was released in neutral pH in comparison with the acidic pH | [27] |
| Naproxen sodium salt | MCM-41 mesoporous particles modified with photo-sensitive ligand cinnamic acid derivative | Cinnamic acid derivative molecules located on the surface of MCM-41 served as gatekeepers through which the drug is blocked/released by UV irradiation Cinnamic acid derivative molecules undergo a photo-dimerization reaction by radiation with a wavelength higher than 365 nm, through which the drug molecules were encapsulated in the pores | [30] |
| Nimesulide | Chiral mesoporous silica nanoparticles with enlarged mesopores | Superior delivery effect (most crystalline drug converted to amorphous phase) Higher oral relative bioavailability and anti-inflammatory effect because enlarge mesopores contributed to load and release more amorphous drug | [113] |
| Nimesulide Indomethacin | Carboxyl group-functionalized mesoporous silica nanoparticles | Significant improvement of dissolution of drugs due to the beneficial pore structure and pore chemistry Good biocompatibility and bio-adsorption capacity Higher bioavailability of drugs Strong anti-inflammatory effect by delivering more drugs in vivo | [87] |
| Sulindac | APTES-modified SBA-15 | Increase of drug dissolution rate Non-toxicity of the system | [153] |
| Level | Challenge | Details |
|---|---|---|
| Manufacture | Large-scale manufacturing | Protocols for reproducible synthesis and functionalization should be standardized Particles should be stable and dispersible |
| Bioapplication | Toxicity (acute, chronic) | In vitro In vivo (different animal models, human body) |
| Biocompatibility | Animal models | |
| Biodegradability | Animal models | |
| Biodistribution | Understanding the interactions between DDS and living organism Accumulation in vital organs causing toxicity (unspecific interactions with non-targeted cells) | |
| Targeting efficacy | Influence of particle size, surface functionalization, porosity, charge | |
| Drug delivery | Inertness of DDS during the time needed to reach the target Long-term stability | |
| Introduction to the market | Sophisticated surface modification | Increased cost of the final product |
| Commercialization | Safety (short term and long term) of the product must be proven for the human body which is time consuming and laborious |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moritz, M.; Geszke-Moritz, M. Mesoporous Materials as Elements of Modern Drug Delivery Systems for Anti-Inflammatory Agents: A Review of Recent Achievements. Pharmaceutics 2022, 14, 1542. https://doi.org/10.3390/pharmaceutics14081542
Moritz M, Geszke-Moritz M. Mesoporous Materials as Elements of Modern Drug Delivery Systems for Anti-Inflammatory Agents: A Review of Recent Achievements. Pharmaceutics. 2022; 14(8):1542. https://doi.org/10.3390/pharmaceutics14081542
Chicago/Turabian StyleMoritz, Michał, and Małgorzata Geszke-Moritz. 2022. "Mesoporous Materials as Elements of Modern Drug Delivery Systems for Anti-Inflammatory Agents: A Review of Recent Achievements" Pharmaceutics 14, no. 8: 1542. https://doi.org/10.3390/pharmaceutics14081542
APA StyleMoritz, M., & Geszke-Moritz, M. (2022). Mesoporous Materials as Elements of Modern Drug Delivery Systems for Anti-Inflammatory Agents: A Review of Recent Achievements. Pharmaceutics, 14(8), 1542. https://doi.org/10.3390/pharmaceutics14081542






