Nanotechnology in the Diagnosis and Treatment of Osteomyelitis
Abstract
:1. Introduction
2. Osteomyelitis
3. Pathophysiology of Osteomyelitis
4. Diagnosis
- Clinical history and risk factors: Clinical history and risk factors for acute hematogenous osteomyelitis (AHO) include trauma, sepsis, bacteremia, chronic catheterization, immunodeficiency [17]. These same factors should be considered for other forms of osteomyelitis as well as including assessment of vascular disease. This criterion cannot be solely relied on for diagnosis as it requires self-reporting, which may compromise the validity.
- Clinical examination: Clinical exams often reveal diffuse or non-specific findings, making diagnosis on this basis alone virtually impossible. Nevertheless, AHO should be considered if a child presents with a fever and localized bone pain [17].
- Laboratory test results: The presence of elevated inflammatory markers are too non-specific to explain the differential diagnoses as osteomyelitis [18]; however, although it is not definitive for diagnosis, it is atypical for patients with acute osteomyelitis to have a normal erythrocyte sedimentation rate (ESR) or normal levels of C-reactive protein (CRP) [9].
- Imaging: X-ray, although not the gold standard, is one of the first diagnostic tools used to evaluate osteomyelitis. Unfortunately, radiographs may be unremarkable for 10–14 days following bone infection, with adults experiencing a longer delay [19]. Consequently, by the time that conventional radiographs effectively demonstrate lytic changes, 50–75% of the bone matrix has been destroyed [20]. This makes early detection of osteomyelitis unlikely. Nevertheless, X-ray radiographs are often initially performed to rule out alternative and more common diagnoses such as fracture or malignancy. Notably, several retrospective studies have revealed that X-ray imaging, once thought to be the gold standard, is of moderate diagnostic accuracy when detecting factures [21]. Alternatively, fluorodeoxyglucose-positron-emission-tomography/computed tomography (18F-FDG-PET/CT) may prove more specific, particularly when used as a hybrid technique with a radioisotope. 18F-FDG-PET/CT has proven useful specifically in patients with MRI contraindications and in the diagnosis of vertebral osteomyelitis as well as in the detection of other metastatic sites of infection [18]. However, PET scans also have limited specificity due to radionuclide uptake that can be present in many inflammatory and neoplastic processes [22]. Magnetic resonance imaging (MRI) has a specificity of 90% and may allow earlier diagnosis of infection due to its ability to image soft tissue prior to bone infiltration.
- Microbiology: Microbiological tests often result in false-negative outcomes due to the location of causative pathogens, the possibility of the patient starting antibiotic therapy prior to bone biopsy, and the culturability of the organism [23,24,25]. Thus, the recommendation is that isolation of causative microorganisms should be attempted using a minimum of three bone tissue cultures and the use of modern molecular testing should be employed [26].
- Histopathology: Bone biopsy (bone scintigraphy) at the site of necrosis is the gold standard of osteomyelitis diagnosis. Positive osteomyelitis bone biopsy results typically include elevated C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), with presence of causative organism (typically S. aureus). Bone scintigraphy in conjunction with a gallium scan can assist in the localization of the infected bone.
5. Vertebral Osteomyelitis—A Case Study to Demonstrate the Diagnostic Difficulties Associated with Osteomyelitis
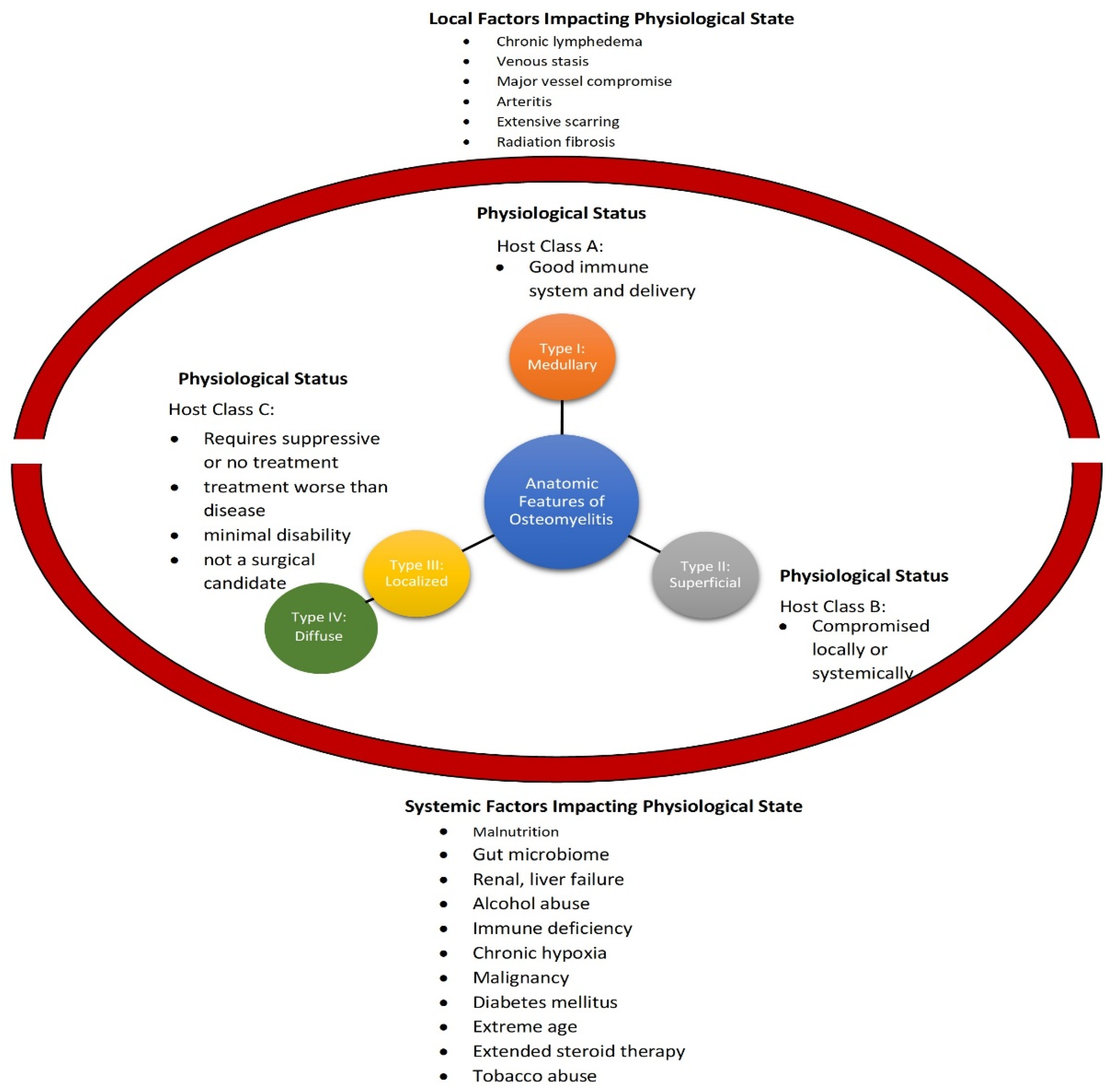
6. Osteomyelitis Classification and Staging
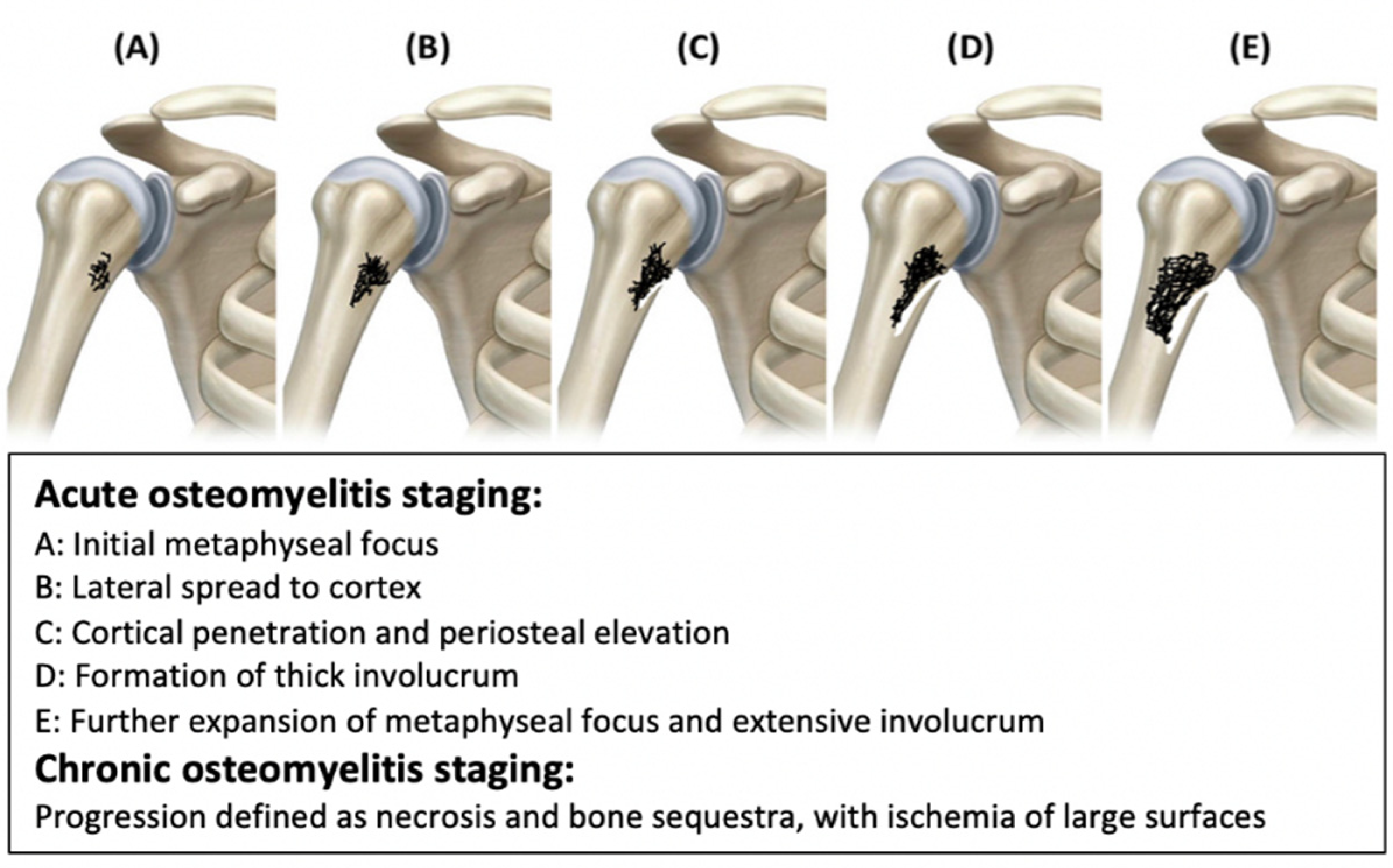
7. Acute Osteomyelitis
8. Chronic Osteomyelitis
9. Treatment
10. Nanotechnology
11. Nanotechnology in Diagnosis
12. Use of Nanotechnology in Diagnosis of Osteomyelitis
13. Nanotechnology in Treatment
14. Nanotechnology in Osteomyelitis Treatment
15. Nanotoxicity and Nanoparticle Safety in Treatment
16. Therapies for Osteomyelitis in Clinical Trials
17. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Owen-Woods, C.; Kusumbe, A. Fundamentals of Bone Vasculature: Specialization, Interactions and Functions. Semin. Cell Dev. Biol. 2022, 123, 36–47. [Google Scholar] [CrossRef] [PubMed]
- Desimpel, J.; Posadzy, M.; Vanhoenacker, F. The Many Faces of Osteomyelitis: A Pictorial Review. J. Belg. Soc. Radiol. 2017, 101, 24. [Google Scholar] [CrossRef]
- Hofstee, M.I.; Muthukrishnan, G.; Atkins, G.J.; Riool, M.; Thompson, K.; Morgenstern, M.; Stoddart, M.J.; Richards, R.G.; Zaat, S.A.J.; Moriarty, T.F. Current Concepts of Osteomyelitis: From Pathologic Mechanisms to Advanced Research Methods. Am. J. Pathol. 2020, 190, 1151–1163. [Google Scholar] [CrossRef] [PubMed]
- Hedrich, C.M.; Morbach, H.; Reiser, C.; Girschick, H.J. New Insights into Adult and Paediatric Chronic Non-Bacterial Osteomyelitis CNO. Curr. Rheumatol. Rep. 2020, 22, 52. [Google Scholar] [CrossRef] [PubMed]
- Taddio, A.; Ferrara, G.; Insalaco, A.; Pardeo, M.; Gregori, M.; Finetti, M.; Pastore, S.; Tommasini, A.; Ventura, A.; Gattorno, M. Dealing with Chronic Non-Bacterial Osteomyelitis: A Practical Approach. Pediatr. Rheumatol. Online J. 2017, 15, 87. [Google Scholar] [CrossRef]
- Wen, Q.; Gu, F.; Sui, Z.; Su, Z.; Yu, T. The Process of Osteoblastic Infection by Staphylococcus aureus. Int. J. Med. Sci. 2020, 17, 1327–1332. [Google Scholar] [CrossRef] [PubMed]
- Gimza, B.D.; Cassat, J.E. Mechanisms of Antibiotic Failure during Staphylococcus aureus Osteomyelitis. Front. Immunol. 2021, 12, 638085. [Google Scholar] [CrossRef] [PubMed]
- Krauss, J.L.; Roper, P.M.; Ballard, A.; Shih, C.-C.; Fitzpatrick, J.A.J.; Cassat, J.E.; Ng, P.Y.; Pavlos, N.J.; Veis, D.J. Staphylococcus aureus Infects Osteoclasts and Replicates Intracellularly. MBio 2019, 10, 15. [Google Scholar] [CrossRef] [Green Version]
- Urish, K.L.; Cassat, J.E. Staphylococcus aureus Osteomyelitis: Bone, Bugs, and Surgery. Infect. Immun. 2020, 88, e00932-19. [Google Scholar] [CrossRef]
- Lima, A.L.L.; Oliveira, P.R.; Carvalho, V.C.; Cimerman, S.; Savio, E. Recommendations for the Treatment of Osteomyelitis. Braz. J. Infect. Dis. 2014, 18, 526–534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kusumbe, A.P.; Ramasamy, S.K.; Itkin, T.; Mäe, M.A.; Langen, U.H.; Betsholtz, C.; Lapidot, T.; Adams, R.H. Age-Dependent Modulation of Vascular Niches for Haematopoietic Stem Cells. Nature 2016, 532, 380–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.; Hendriks, M.; Chatzis, A.; Ramasamy, S.K.; Kusumbe, A.P. Bone Vasculature and Bone Marrow Vascular Niches in Health and Disease. J. Bone Miner. Res. 2020, 35, 2103–2120. [Google Scholar] [CrossRef]
- Ramasamy, S.K.; Kusumbe, A.P.; Schiller, M.; Zeuschner, D.; Bixel, M.G.; Milia, C.; Gamrekelashvili, J.; Limbourg, A.; Medvinsky, A.; Santoro, M.M.; et al. Blood Flow Controls Bone Vascular Function and Osteogenesis. Nat. Commun. 2016, 7, 13601. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papadakis, M.A.; McPhee, S.J.; Bernstein, J. Osteomyelitis, Staphylococcus aureus. In Quick Medical Diagnosis & Treatment 2022; McGraw-Hill Education: New York, NY, USA, 2022. [Google Scholar]
- Schmidt, H.G.K.; Tiemann, A.H.; Braunschweig, R.; Diefenbeck, M.; Bühler, M.; Abitzsch, D.; Haustedt, N.; Walter, G.; Schoop, R.; Heppert, V.; et al. Definition of the Diagnosis Osteomyelitis-Osteomyelitis Diagnosis Score (ODS). Z. Orthop. Unfall. 2011, 149, 449–460. [Google Scholar] [CrossRef] [PubMed]
- Tiemann, A.; Hofmann, G.O.; Krukemeyer, M.G.; Krenn, V.; Langwald, S. Histopathological Osteomyelitis Evaluation Score (HOES)—An Innovative Approach to Histopathological Diagnostics and Scoring of Osteomyelitis. GMS Interdiscip. Plast. Reconstr. Surg. DGPW 2014, 3, Doc08. [Google Scholar] [CrossRef]
- Popescu, B.; Tevanov, I.; Carp, M.; Ulici, A. Acute Hematogenous Osteomyelitis in Pediatric Patients: Epidemiology and Risk Factors of a Poor Outcome. J. Int. Med. Res. 2020, 48, 0300060520910889. [Google Scholar] [CrossRef]
- Hatzenbuehler, J.; Pulling, T.J. Diagnosis and Management of Osteomyelitis. AFP 2011, 84, 1027–1033. [Google Scholar]
- Schmitt, S.K. Osteomyelitis. Infect. Dis. Clin. N. Am. 2017, 31, 325–338. [Google Scholar] [CrossRef]
- Butt, W.P. The Radiology of Infection. Clin. Orthop. Relat. Res. 1973, 96, 20–30. [Google Scholar] [CrossRef]
- Lampart, A.; Arnold, I.; Mäder, N.; Niedermeier, S.; Escher, A.; Stahl, R.; Trumm, C.; Kammerlander, C.; Böcker, W.; Nickel, C.H.; et al. Prevalence of Fractures and Diagnostic Accuracy of Emergency X-Ray in Older Adults Sustaining a Low-Energy Fall: A Retrospective Study. J. Clin. Med. 2020, 9, 97. [Google Scholar] [CrossRef] [Green Version]
- Graeber, A.; Cecava, N.D. Vertebral Osteomyelitis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Vemu, L.; Sudhaharan, S.; Mamidi, N.; Chavali, P. Need for Appropriate Specimen for Microbiology Diagnosis of Chronic Osteomyelitis. J. Lab. Physicians 2018, 10, 21–25. [Google Scholar] [CrossRef]
- Parvizi, J.; Erkocak, O.F.; Della Valle, C.J. Culture-Negative Periprosthetic Joint Infection. JBJS 2014, 96, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Mendis, N.; Trigui, H.; Oliver, J.D.; Faucher, S.P. The Importance of the Viable but Non-Culturable State in Human Bacterial Pathogens. Front. Microbiol. 2014, 5, 258. [Google Scholar] [CrossRef] [Green Version]
- Tsang, S.-T.J.; Eyre, D.W.; Atkins, B.L.; Simpson, A.H.R.W. Should Modern Molecular Testing Be Routinely Available for the Diagnosis of Musculoskeletal Infection? Bone Jt. J. 2020, 102-B, 1274–1276. [Google Scholar] [CrossRef]
- Fragío Gil, J.J.; González Mazarío, R.; Salavert Lleti, M.; Román Ivorra, J.A. Vertebral Osteomyelitis: Clinical, Microbiological and Radiological Characteristics of 116 Patients. Med. Clínica 2020, 155, 335–339. [Google Scholar] [CrossRef]
- Marais, L.C.; Ferreira, N.; Aldous, C.; le Roux, T.L.B. The Classification of Chronic Osteomyelitis. SA Orthop. J. 2014, 13, 22–28. [Google Scholar]
- Cierny, G.I.; Mader, J.T.; Penninck, J.J. The Classic: A Clinical Staging System for Adult Osteomyelitis. Clin. Orthop. Relat. Res. 2003, 414, 7–24. [Google Scholar] [CrossRef] [Green Version]
- McPherson, E.J.; Woodson, C.; Holtom, P.; Roidis, N.; Shufelt, C.; Patzakis, M. Periprosthetic Total Hip Infection: Outcomes Using a Staging System. Clin. Orthop. Relat. Res. 2002, 403, 8–15. [Google Scholar] [CrossRef]
- Brady, R.A.; Leid, J.G.; Calhoun, J.H.; Costerton, J.W.; Shirtliff, M.E. Osteomyelitis and the Role of Biofilms in Chronic Infection. FEMS Immunol. Med. Microbiol. 2008, 52, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Snoddy, B.; Jayasuriya, A.C. The Use of Nanomaterials to Treat Bone Infections. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 67, 822–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wassif, R.K.; Elkayal, M.; Shamma, R.N.; Elkheshen, S.A. Recent Advances in the Local Antibiotics Delivery Systems for Management of Osteomyelitis. Drug Deliv. 2021, 28, 2392–2414. [Google Scholar] [CrossRef] [PubMed]
- Carek, P.J.; Dickerson, L.M.; Sackier, J.M. Diagnosis and Management of Osteomyelitis. AFP 2001, 63, 2413. [Google Scholar]
- Kavanagh, N.; Ryan, E.J.; Widaa, A.; Sexton, G.; Fennell, J.; O’Rourke, S.; Cahill, K.C.; Kearney, C.J.; O’Brien, F.J.; Kerrigan, S.W. Staphylococcal Osteomyelitis: Disease Progression, Treatment Challenges, and Future Directions. Clin. Microbiol. Rev. 2018, 31, e00084-17. [Google Scholar] [CrossRef] [Green Version]
- Sanvicens, N.; Marco, M.P. Multifunctional Nanoparticles—Properties and Prospects for Their Use in Human Medicine. Trends Biotechnol. 2008, 26, 425–433. [Google Scholar] [CrossRef]
- Miziak, P.A.; Baran, M.; Bonio, K.; Piech, P. Nanoparticles in Medicine. J. Educ. Health Sport 2020, 10, 17–21. [Google Scholar] [CrossRef]
- Chatterjee, K.; Sarkar, S.; Jagajjanani Rao, K.; Paria, S. Core/Shell Nanoparticles in Biomedical Applications. Adv. Colloid Interface Sci. 2014, 209, 8–39. [Google Scholar] [CrossRef] [PubMed]
- Brun, E.; Sicard-Roselli, C. Actual Questions Raised by Nanoparticle Radiosensitization. Radiat. Phys. Chem. 2016, 128, 134–142. [Google Scholar] [CrossRef]
- Hamblin, M.R.; Chiang, L.Y.; Lakshmanan, S.; Huang, Y.-Y.; Garcia-Diaz, M.; Karimi, M.; Rastelli, A.N.d.S.; Chandran, R. Nanotechnology for Photodynamic Therapy: A Perspective from the Laboratory of Dr. Michael R. Hamblin in the Wellman Center for Photomedicine at Massachusetts General Hospital and Harvard Medical School. Nanotechnol. Rev. 2015, 4, 359–372. [Google Scholar] [CrossRef] [PubMed]
- Thunyaporn, R.; Doh, I.; Lee, D.W. Multi-Volume Hemacytometer. Sci. Rep. 2021, 11, 14106. [Google Scholar] [CrossRef]
- Taddie, W.; Dessie, D. The Role of Nanotechnology in Medicine. Int. J. Excell. Innov. Dev. 2019, 2, 8. [Google Scholar]
- Al-Mamoori, S.O.H.; Jabuk, S.I.A.; Mahdi, R.K.; Naji, N.M.; Almaamori, A.M.K. The use of nanotechnology in medicine. Eur. J. Res. Dev. Sustain. 2022, 3, 115–120. [Google Scholar]
- Alharbi, K.K.; Al-sheikh, Y.A. Role and Implications of Nanodiagnostics in the Changing Trends of Clinical Diagnosis. Saudi J. Biol. Sci. 2014, 21, 109–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tong, S.; Zhu, H.; Bao, G. Magnetic Iron Oxide Nanoparticles for Disease Detection and Therapy. Mater. Today 2019, 31, 86–99. [Google Scholar] [CrossRef]
- Chinen, A.B.; Guan, C.M.; Ferrer, J.R.; Barnaby, S.N.; Merkel, T.J.; Mirkin, C.A. Nanoparticle Probes for the Detection of Cancer Biomarkers, Cells, and Tissues by Fluorescence. Chem. Rev. 2015, 115, 10530–10574. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, L.; Wang, H.; Wang, J.; Chen, M.; Shang, L. Ofloxacin-Delivery System of a Polyanhydride and Polylactide Blend Used in the Treatment of Bone Infection. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 83, 589–595. [Google Scholar] [CrossRef]
- Masters, E.A.; Trombetta, R.P.; de Mesy Bentley, K.L.; Boyce, B.F.; Gill, A.L.; Gill, S.R.; Nishitani, K.; Ishikawa, M.; Morita, Y.; Ito, H.; et al. Evolving Concepts in Bone Infection: Redefining “Biofilm”, “Acute vs. Chronic Osteomyelitis”, “the Immune Proteome” and “Local Antibiotic Therapy”. Bone Res. 2019, 7, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Kyriacou, H.; Kamaraj, A.; Khan, W.S. Developments in Antibiotic-Eluting Scaffolds for the Treatment of Osteomyelitis. Appl. Sci. 2020, 10, 2244. [Google Scholar] [CrossRef] [Green Version]
- Cyphert, E.L.; Zhang, N.; Learn, G.D.; Hernandez, C.J.; von Recum, H.A. Recent Advances in the Evaluation of Antimicrobial Materials for Resolution of Orthopedic Implant-Associated Infections In Vivo. ACS Infect. Dis. 2021, 7, 3125–3160. [Google Scholar] [CrossRef]
- Billings, C.; Anderson, D.E. Role of Implantable Drug Delivery Devices with Dual Platform Capabilities in the Prevention and Treatment of Bacterial Osteomyelitis. Bioengineering 2022, 9, 65. [Google Scholar] [CrossRef] [PubMed]
- van de Belt, H.; Neut, D.; Uges, D.R.A.; Schenk, W.; van Horn, J.R.; van der Mei, H.C.; Busscher, H.J. Surface Roughness, Porosity and Wettability of Gentamicin-Loaded Bone Cements and Their Antibiotic Release. Biomaterials 2000, 21, 1981–1987. [Google Scholar] [CrossRef]
- Gálvez-López, R.; Peña-Monje, A.; Antelo-Lorenzo, R.; Guardia-Olmedo, J.; Moliz, J.; Hernández-Quero, J.; Parra-Ruiz, J. Elution Kinetics, Antimicrobial Activity, and Mechanical Properties of 11 Different Antibiotic Loaded Acrylic Bone Cement. Diagn. Microbiol. Infect. Dis. 2014, 78, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Alonge, T.O.; Fashina, A.N. Ceftriaxone-PMMA Beads—A Slow Release Preparation? Int. J. Clin. Pract. 2000, 54, 353–355. [Google Scholar] [PubMed]
- Patel, K.H.; Bhat, S.N.; Mamatha, H. Outcome Analysis of Antibiotic-Loaded Poly Methyl Methacrylate (PMMA) Beads in Musculoskeletal Infections. J. Taibah Univ. Med. Sci. 2021, 16, 177–183. [Google Scholar] [CrossRef]
- Greene, N.; Holtom, P.D.; Warren, C.A.; Ressler, R.L.; Shepherd, L.; McPherson, E.J.; Patzakis, M.J. In Vitro Elution of Tobramycin and Vancomycin Polymethylmethacrylate Beads and Spacers from Simplex and Palacos. Am. J. Orthop. 1998, 27, 201–205. [Google Scholar]
- Clauss, M.; Trampuz, A.; Borens, O.; Bohner, M.; Ilchmann, T. Biofilm Formation on Bone Grafts and Bone Graft Substitutes: Comparison of Different Materials by a Standard in Vitro Test and Microcalorimetry. Acta Biomater. 2010, 6, 3791–3797. [Google Scholar] [CrossRef]
- Uskoković, V. Nanostructured Platforms for the Sustained and Local Delivery of Antibiotics in the Treatment of Osteomyelitis. Crit. Rev. Ther. Drug Carrier Syst. 2015, 32, 1–59. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, N.; Hyeon, T. Recent Development of Nanoparticles for Molecular Imaging. Philos. Trans. R. Soc. A Math. Phys. Eng. Sci. 2017, 375, 20170022. [Google Scholar] [CrossRef]
- Luo, D.; Wang, X.; Burda, C.; Basilion, J.P. Recent Development of Gold Nanoparticles as Contrast Agents for Cancer Diagnosis. Cancers 2021, 13, 1825. [Google Scholar] [CrossRef]
- Zhang, Z.; Ross, R.D.; Roeder, R.K. Preparation of Functionalized Gold Nanoparticles as a Targeted X-Ray Contrast Agent for Damaged Bone Tissue. Nanoscale 2010, 2, 582–586. [Google Scholar] [CrossRef]
- Erdman, W.A.; Tamburro, F.; Jayson, H.T.; Weatherall, P.T.; Ferry, K.B.; Peshock, R.M. Osteomyelitis: Characteristics and Pitfalls of Diagnosis with MR Imaging. Radiology 1991, 180, 533–539. [Google Scholar] [CrossRef]
- Durham, J.R.; Lukens, M.L.; Campanini, D.S.; Wright, J.G.; Smead, W.L. Impact of Magnetic Resonance Imaging on the Management of Diabetic Foot Infections. Am. J. Surg. 1991, 162, 150–153, discussion 153–154. [Google Scholar] [CrossRef]
- Lee, N.; Yoo, D.; Ling, D.; Cho, M.H.; Hyeon, T.; Cheon, J. Iron Oxide Based Nanoparticles for Multimodal Imaging and Magnetoresponsive Therapy. Chem. Rev. 2015, 115, 10637–10689. [Google Scholar] [CrossRef]
- Feliu, N.; Docter, D.; Heine, M.; Del Pino, P.; Ashraf, S.; Kolosnjaj-Tabi, J.; Macchiarini, P.; Nielsen, P.; Alloyeau, D.; Gazeau, F.; et al. In Vivo Degeneration and the Fate of Inorganic Nanoparticles. Chem. Soc. Rev. 2016, 45, 2440–2457. [Google Scholar] [CrossRef] [Green Version]
- Tenover, F.C.; Tickler, I.A.; Le, V.M.; Dewell, S.; Mendes, R.E.; Goering, R.V. Updating Molecular Diagnostics for Detecting Methicillin-Susceptible and Methicillin-Resistant Staphylococcus aureus Isolates in Blood Culture Bottles. J. Clin. Microbiol. 2019, 57, e01195-19. [Google Scholar] [CrossRef] [Green Version]
- Stürenburg, E. Rapid Detection of Methicillin-Resistant Staphylococcus aureus Directly from Clinical Samples: Methods, Effectiveness and Cost Considerations. GMS Ger. Med. Sci. 2009, 7, Doc06. [Google Scholar] [CrossRef]
- Jain, K.K. Nanomicrobiology. In The Handbook of Nanomedicine; Humana Press: New York, NY, USA, 2017; pp. 511–537. [Google Scholar] [CrossRef]
- Cui, J.; Zhou, M.; Li, Y.; Liang, Z.; Li, Y.; Yu, L.; Liu, Y.; Liang, Y.; Chen, L.; Yang, C. A New Optical Fiber Probe-Based Quantum Dots Immunofluorescence Biosensors in the Detection of Staphylococcus aureus. Front. Cell. Infect. Microbiol. 2021, 11, 665241. [Google Scholar] [CrossRef]
- Funao, H.; Ishii, K.; Nagai, S.; Sasaki, A.; Hoshikawa, T.; Aizawa, M.; Okada, Y.; Chiba, K.; Koyasu, S.; Toyama, Y.; et al. Establishment of a Real-Time, Quantitative, and Reproducible Mouse Model of Staphylococcus Osteomyelitis Using Bioluminescence Imaging. Infect. Immun. 2012, 80, 733–741. [Google Scholar] [CrossRef] [Green Version]
- del Pozo, E.G.; Collazos, J.; Cartón, J.A.; Camporro, D.; Asensi, V. Bacterial Osteomyelitis: Microbiological, Clinical, Therapeutic, and Evolutive Characteristics of 344 Episodes. Rev. Esp. Quimioter. 2018, 31, 217–225. [Google Scholar]
- Ghasemi, R.; Mirahmadi-Zare, S.Z.; Nasr-Esfahani, M.H.; Allafchian, A.; Behmanesh, M. Optical Biosensing of Streptococcus Agalactiae Based on Core/Shell Magnetic Nanoparticle-Quantum Dot. Anal. Bioanal. Chem. 2019, 411, 6733–6743. [Google Scholar] [CrossRef]
- Ye, W.; Guo, J.; Bao, X.; Chen, T.; Weng, W.; Chen, S.; Yang, M. Rapid and Sensitive Detection of Bacteria Response to Antibiotics Using Nanoporous Membrane and Graphene Quantum Dot (GQDs)-Based Electrochemical Biosensors. Materials 2017, 10, 603. [Google Scholar] [CrossRef] [Green Version]
- Yang, H.; Jie, X.; Wang, L.; Zhang, Y.; Wang, M.; Wei, W. An Array Consisting of Glycosylated Quantum Dots Conjugated to MoS2 Nanosheets for Fluorometric Identification and Quantitation of Lectins and Bacteria. Mikrochim. Acta 2018, 185, 512. [Google Scholar] [CrossRef]
- Zhang, C.; Zheng, X.; Bai, Y.; Luo, Q.; Shang, J.; Xie, L.; Wei, Y. Novel Carbon Dots Based on Pseudomonas Aeruginosa for High Selectivity Detection of Cr6+ and Bioimaging Both in Vitro and in Vivo. NANO 2022, 17, 2250003. [Google Scholar] [CrossRef]
- Tomas, M.B.; Patel, M.; Marwin, S.E.; Palestro, C.J. The Diabetic Foot. Br. J. Radiol. 2000, 73, 443–450. [Google Scholar] [CrossRef]
- Bierry, G.; Jehl, F.; Boehm, N.; Robert, P.; Dietemann, J.-L.; Kremer, S. Macrophage Imaging by USPIO-Enhanced MR for the Differentiation of Infectious Osteomyelitis and Aseptic Vertebral Inflammation. Eur. Radiol. 2009, 19, 1604–1611. [Google Scholar] [CrossRef]
- Erlemann, R.; Sciuk, J.; Wuisman, P.; Bene, D.; Edel, G.; Ritter, J.; Peters, P.E. Dynamic MR tomography in the diagnosis of inflammatory and tumorous space-occupying lesions of the musculoskeletal system. Rofo 1992, 156, 353–359. [Google Scholar] [CrossRef]
- Fukuda, Y.; Ando, K.; Ishikura, R.; Kotoura, N.; Tsuda, N.; Kato, N.; Yoshiya, S.; Nakao, N. Superparamagnetic Iron Oxide (SPIO) MRI Contrast Agent for Bone Marrow Imaging: DiŠerentiating Bone Metastasis and Osteomyelitis. Magn. Reson. Med. Sci. 2006, 5, 6. [Google Scholar] [CrossRef] [Green Version]
- Neuwelt, A.; Sidhu, N.; Hu, C.-A.A.; Mlady, G.; Eberhardt, S.C.; Sillerud, L.O. Iron-Based Superparamagnetic Nanoparticle Contrast Agents for MRI of Infection and Inflammation. AJR Am. J. Roentgenol. 2015, 204, W302–W313. [Google Scholar] [CrossRef] [Green Version]
- Hafner, A.; Lovrić, J.; Lakoš, G.P.; Pepić, I. Nanotherapeutics in the EU: An Overview on Current State and Future Directions. Int. J. Nanomed. 2014, 9, 1005–1023. [Google Scholar] [CrossRef] [Green Version]
- Petros, R.A.; DeSimone, J.M. Strategies in the Design of Nanoparticles for Therapeutic Applications. Nat. Rev. Drug Discov. 2010, 9, 615–627. [Google Scholar] [CrossRef]
- Szlachcic, A.; Pala, K.; Zakrzewska, M.; Jakimowicz, P.; Wiedlocha, A.; Otlewski, J. FGF1-Gold Nanoparticle Conjugates Targeting FGFR Efficiently Decrease Cell Viability upon NIR Irradiation. IJN 2012, 7, 5915–5927. [Google Scholar] [CrossRef] [Green Version]
- Guo, H.; Qian, H.; Idris, N.M.; Zhang, Y. Singlet Oxygen-Induced Apoptosis of Cancer Cells Using Upconversion Fluorescent Nanoparticles as a Carrier of Photosensitizer. Nanomed. Nanotechnol. Biol. Med. 2010, 6, 486–495. [Google Scholar] [CrossRef]
- Yan, X.; Al-Hayek, S.; Huang, H.; Zhu, Z.; Zhu, W.; Guo, H. Photodynamic Effect of 5-Aminolevulinic Acid-Loaded Nanoparticles on Bladder Cancer Cells: A Preliminary Investigation. Scand. J. Urol. 2013, 47, 145–151. [Google Scholar] [CrossRef]
- Ni, W.; Li, M.; Cui, J.; Xing, Z.; Li, Z.; Wu, X.; Song, E.; Gong, M.; Zhou, W. 808nm Light Triggered Black TiO2 Nanoparticles for Killing of Bladder Cancer Cells. Mater. Sci. Eng. C 2017, 81, 252–260. [Google Scholar] [CrossRef]
- Alifu, N.; Zebibula, A.; Qi, J.; Zhang, H.; Sun, C.; Yu, X.; Xue, D.; Lam, J.W.Y.; Li, G.; Qian, J.; et al. Single-Molecular Near-Infrared-II Theranostic Systems: Ultrastable Aggregation-Induced Emission Nanoparticles for Long-Term Tracing and Efficient Photothermal Therapy. ACS Nano 2018, 12, 11282–11293. [Google Scholar] [CrossRef]
- Prasad, M.; Lambe, U.P.; Brar, B.; Shah, I.; Manimegalai, J.; Ranjan, K.; Rao, R.; Kumar, S.; Mahant, S.; Khurana, S.K.; et al. Nanotherapeutics: An Insight into Healthcare and Multi-Dimensional Applications in Medical Sector of the Modern World. Biomed. Pharmacother. 2018, 97, 1521–1537. [Google Scholar] [CrossRef]
- Anju, S.; Prajitha, N.; Sukanya, V.S.; Mohanan, P.V. Complicity of Degradable Polymers in Health-Care Applications. Mater. Today Chem. 2020, 16, 100236. [Google Scholar] [CrossRef]
- Samavedi, S.; Poindexter, L.K.; Van Dyke, M.; Goldstein, A.S. Chapter 7—Synthetic Biomaterials for Regenerative Medicine Applications. In Regenerative Medicine Applications in Organ Transplantation; Orlando, G., Lerut, J., Soker, S., Stratta, R.J., Eds.; Academic Press: Cambridge, MA, USA, 2014; pp. 81–99. ISBN 978-0-12-398523-1. [Google Scholar]
- Senra, M.R.; Marques, M.d.F.V. Synthetic Polymeric Materials for Bone Replacement. J. Compos. Sci. 2020, 4, 191. [Google Scholar] [CrossRef]
- Xu, X.; Song, J. Segmental Long Bone Regeneration Guided by Degradable Synthetic Polymeric Scaffolds. Biomater. Transl. 2020, 1, 33. [Google Scholar] [CrossRef]
- Gentile, P.; Chiono, V.; Carmagnola, I.; Hatton, P.V. An Overview of Poly(Lactic-Co-Glycolic) Acid (PLGA)-Based Biomaterials for Bone Tissue Engineering. Int. J. Mol. Sci. 2014, 15, 3640–3659. [Google Scholar] [CrossRef]
- Posadowska, U.; Brzychczy-Włoch, M.; Pamuła, E. Gentamicin Loaded PLGA Nanoparticles as Local Drug Delivery System for the Osteomyelitis Treatment. Acta Bioeng. Biomech. 2015, 17, 41–48. [Google Scholar]
- Pillai, R.R.; Somayaji, S.N.; Rabinovich, M.; Hudson, M.C.; Gonsalves, K.E. Nafcillin-Loaded PLGA Nanoparticles for Treatment of Osteomyelitis. Biomed. Mater. 2008, 3, 034114. [Google Scholar] [CrossRef]
- Basu, A.; Domb, A.J. Recent Advances in Polyanhydride Based Biomaterials. Adv. Mater. 2018, 30, 1706815. [Google Scholar] [CrossRef]
- Li, L.C.; Deng, J.; Stephens, D. Polyanhydride Implant for Antibiotic Delivery—From the Bench to the Clinic. Adv. Drug Deliv. Rev. 2002, 54, 963–986. [Google Scholar] [CrossRef]
- Barros, J.; Grenho, L.; Manuel, C.; Ferreira, C.; Melo, L.; Nunes, O.; Monteiro, F.; Ferraz, M. Influence of Nanohydroxyapatite Surface Properties on Staphylococcus Epidermidis Biofilm Formation. J. Biomater. Appl. 2014, 28, 1325–1335. [Google Scholar] [CrossRef] [Green Version]
- Rau, J.V.; Cacciotti, I.; Laureti, S.; Fosca, M.; Varvaro, G.; Latini, A. Bioactive, Nanostructured Si-Substituted Hydroxyapatite Coatings on Titanium Prepared by Pulsed Laser Deposition. J. Biomed. Mater. Res. Part B Appl. Biomater. 2015, 103, 1621–1631. [Google Scholar] [CrossRef]
- Wang, Q.; Chen, C.; Liu, W.; He, X.; Zhou, N.; Zhang, D.; Gu, H.; Li, J.; Jiang, J.; Huang, W. Levofloxacin Loaded Mesoporous Silica Microspheres/Nano-Hydroxyapatite/Polyurethane Composite Scaffold for the Treatment of Chronic Osteomyelitis with Bone Defects. Sci. Rep. 2017, 7, 41808. [Google Scholar] [CrossRef] [Green Version]
- Qiao, K.; Xu, L.; Tang, J.; Wang, Q.; Lim, K.S.; Hooper, G.; Woodfield, T.B.F.; Liu, G.; Tian, K.; Zhang, W.; et al. The Advances in Nanomedicine for Bone and Cartilage Repair. J. Nanobiotechnol. 2022, 20, 141. [Google Scholar] [CrossRef]
- Li, P.; Li, Y.; Kwok, T.; Yang, T.; Liu, C.; Li, W.; Zhang, X. A Bi-Layered Membrane with Micro-Nano Bioactive Glass for Guided Bone Regeneration. Colloids Surf. B Biointerfaces 2021, 205, 111886. [Google Scholar] [CrossRef]
- Zhang, J.; Chen, Y.; Xu, J.; Wang, J.; Li, C.; Wang, L. Tissue Engineering Using 3D Printed Nano-Bioactive Glass Loaded with NELL1 Gene for Repairing Alveolar Bone Defects. Regen. Biomater. 2018, 5, 213–220. [Google Scholar] [CrossRef] [Green Version]
- Tian, T.; Xie, W.; Gao, W.; Wang, G.; Zeng, L.; Miao, G.; Lei, B.; Lin, Z.; Chen, X. Micro-Nano Bioactive Glass Particles Incorporated Porous Scaffold for Promoting Osteogenesis and Angiogenesis in Vitro. Front. Chem. 2019, 7, 186. [Google Scholar] [CrossRef]
- Christy, P.N.; Basha, S.K.; Kumari, V.S. Nano Zinc Oxide and Nano Bioactive Glass Reinforced Chitosan/Poly(Vinyl Alcohol) Scaffolds for Bone Tissue Engineering Application. Mater. Today Commun. 2022, 31, 103429. [Google Scholar] [CrossRef]
- Mondal, S.; Hoang, G.; Manivasagan, P.; Moorthy, M.S.; Nguyen, T.P.; Vy Phan, T.T.; Kim, H.H.; Kim, M.H.; Nam, S.Y.; Oh, J. Nano-Hydroxyapatite Bioactive Glass Composite Scaffold with Enhanced Mechanical and Biological Performance for Tissue Engineering Application. Ceram. Int. 2018, 44, 15735–15746. [Google Scholar] [CrossRef]
- Alizadeh-Osgouei, M.; Li, Y.; Wen, C. A Comprehensive Review of Biodegradable Synthetic Polymer-Ceramic Composites and Their Manufacture for Biomedical Applications. Bioact. Mater. 2019, 4, 22–36. [Google Scholar] [CrossRef]
- Drago, L.; Romanò, D.; De Vecchi, E.; Vassena, C.; Logoluso, N.; Mattina, R.; Romanò, C.L. Bioactive Glass BAG-S53P4 for the Adjunctive Treatment of Chronic Osteomyelitis of the Long Bones: An in Vitro and Prospective Clinical Study. BMC Infect. Dis. 2013, 13, 584. [Google Scholar] [CrossRef] [Green Version]
- Jia, W.-T.; Fu, Q.; Huang, W.-H.; Zhang, C.-Q.; Rahaman, M.N. Comparison of Borate Bioactive Glass and Calcium Sulfate as Implants for the Local Delivery of Teicoplanin in the Treatment of Methicillin-Resistant Staphylococcus Aureus-Induced Osteomyelitis in a Rabbit Model. Antimicrob. Agents Chemother. 2015, 59, 7571–7580. [Google Scholar] [CrossRef] [Green Version]
- Hasan, R.; Schaner, K.; Mulinti, P.; Brooks, A. A Bioglass-Based Antibiotic (Vancomycin) Releasing Bone Void Filling Putty to Treat Osteomyelitis and Aid Bone Healing. Int. J. Mol. Sci. 2021, 22, 7736. [Google Scholar] [CrossRef]
- Daramola, O.O.; Olajide, J.L.; Agwuncha, S.C.; Mochane, M.J.; Sadiku, E.R. Nanostructured Green Biopolymer Composites for Orthopedic Application. In Green Biopolymers and Their Nanocomposites; Gnanasekaran, D., Ed.; Materials Horizons: From Nature to Nanomaterials; Springer: Berlin/Heidelberg, Germany, 2019; pp. 159–190. ISBN 9789811380631. [Google Scholar]
- Filippi, M.; Born, G.; Chaaban, M.; Scherberich, A. Natural Polymeric Scaffolds in Bone Regeneration. Front. Bioeng. Biotechnol. 2020, 8, 474. [Google Scholar] [CrossRef]
- Mendel, V.; Simanowski, H.-J.; Scholz, H.C.; Heymann, H. Therapy with Gentamicin-PMMA Beads, Gentamicin-Collagen Sponge, and Cefazolin for Experimental Osteomyelitis Due to Staphylococcus aureus in Rats. Arch. Orthop. Trauma. Surg. 2005, 125, 363–368. [Google Scholar] [CrossRef]
- Padrão, T.; Coelho, C.C.; Costa, P.; Alegrete, N.; Monteiro, F.J.; Sousa, S.R. Combining Local Antibiotic Delivery with Heparinized Nanohydroxyapatite/Collagen Bone Substitute: A Novel Strategy for Osteomyelitis Treatment. Mater. Sci. Eng. C 2021, 119, 111329. [Google Scholar] [CrossRef]
- Aimin, C.; Chunlin, H.; Juliang, B.; Tinyin, Z.; Zhichao, D. Antibiotic Loaded Chitosan Bar. An in Vitro, in Vivo Study of a Possible Treatment for Osteomyelitis. Clin. Orthop. Relat. Res. 1999, 366, 239–247. [Google Scholar] [CrossRef]
- Shi, P.; Zuo, Y.; Li, X.; Zou, Q.; Liu, H.; Zhang, L.; Li, Y.; Morsi, Y.S. Gentamicin-Impregnated Chitosan/Nanohydroxyapatite/Ethyl Cellulose Microspheres Granules for Chronic Osteomyelitis Therapy. J. Biomed. Mater. Res. Part A 2010, 93A, 1020–1031. [Google Scholar] [CrossRef]
- Tao, J.; Zhang, Y.; Shen, A.; Yang, Y.; Diao, L.; Wang, L.; Cai, D.; Hu, Y. Injectable Chitosan-Based Thermosensitive Hydrogel/Nanoparticle-Loaded System for Local Delivery of Vancomycin in the Treatment of Osteomyelitis. Int. J. Nanomed. 2020, 15, 5855–5871. [Google Scholar] [CrossRef]
- Koh, L.-D.; Cheng, Y.; Teng, C.-P.; Khin, Y.-W.; Loh, X.-J.; Tee, S.-Y.; Low, M.; Ye, E.; Yu, H.-D.; Zhang, Y.-W.; et al. Structures, Mechanical Properties and Applications of Silk Fibroin Materials. Prog. Polym. Sci. 2015, 46, 86–110. [Google Scholar] [CrossRef]
- Altman, G.H.; Diaz, F.; Jakuba, C.; Calabro, T.; Horan, R.L.; Chen, J.; Lu, H.; Richmond, J.; Kaplan, D.L. Silk-Based Biomaterials. Biomaterials 2003, 24, 401–416. [Google Scholar] [CrossRef] [Green Version]
- Mottaghitalab, F.; Hosseinkhani, H.; Shokrgozar, M.A.; Mao, C.; Yang, M.; Farokhi, M. Silk as a Potential Candidate for Bone Tissue Engineering. J. Control. Release 2015, 215, 112–128. [Google Scholar] [CrossRef]
- Saleem, M.; Rasheed, S.; Yougen, C. Silk Fibroin/Hydroxyapatite Scaffold: A Highly Compatible Material for Bone Regeneration. Sci. Technol. Adv. Mater. 2020, 21, 242–266. [Google Scholar] [CrossRef] [Green Version]
- Besheli, N.H.; Mottaghitalab, F.; Eslami, M.; Gholami, M.; Kundu, S.C.; Kaplan, D.L.; Farokhi, M. Sustainable Release of Vancomycin from Silk Fibroin Nanoparticles for Treating Severe Bone Infection in Rat Tibia Osteomyelitis Model. Available online: https://pubs.acs.org/doi/pdf/10.1021/acsami.6b14912 (accessed on 9 April 2022).
- Mulinti, P.; Shreffler, J.; Hasan, R.; Dea, M.; Brooks, A.E. Infection Responsive Smart Delivery of Antibiotics Using Recombinant Spider Silk Nanospheres. Pharmaceutics 2021, 13, 1358. [Google Scholar] [CrossRef]
- Lu, M.; Liao, J.; Dong, J.; Wu, J.; Qiu, H.; Zhou, X.; Li, J.; Jiang, D.; He, T.-C.; Quan, Z. An Effective Treatment of Experimental Osteomyelitis Using the Antimicrobial Titanium/Silver-Containing NHP66 (Nano-Hydroxyapatite/Polyamide-66) Nanoscaffold Biomaterials. Sci. Rep. 2016, 6, 39174. [Google Scholar] [CrossRef] [Green Version]
- Feng, Q.L.; Wu, J.; Chen, G.Q.; Cui, F.Z.; Kim, T.N.; Kim, J.O. A Mechanistic Study of the Antibacterial Effect of Silver Ions on Escherichia coli and Staphylococcus aureus. J. Biomed. Mater. Res. 2000, 52, 662–668. [Google Scholar] [CrossRef]
- Akiyama, T.; Miyamoto, H.; Yonekura, Y.; Tsukamoto, M.; Ando, Y.; Noda, I.; Sonohata, M.; Mawatari, M. Silver Oxide-Containing Hydroxyapatite Coating Has in Vivo Antibacterial Activity in the Rat Tibia. J. Orthop. Res. 2013, 31, 1195–1200. [Google Scholar] [CrossRef]
- Drewa, T.; Szmytkowska, K.; Chaberski, M. The Short Term Exposition of AgNO3 on 3T3 Mouse Fibroblasts Cell Line. Acta Pol. Pharm. 2007, 64, 175–178. [Google Scholar]
- Roy, M.; Fielding, G.A.; Beyenal, H.; Bandyopadhyay, A.; Bose, S. Mechanical, in Vitro Antimicrobial, and Biological Properties of Plasma-Sprayed Silver-Doped Hydroxyapatite Coating. ACS Appl. Mater. Interfaces 2012, 4, 1341–1349. [Google Scholar] [CrossRef] [Green Version]
- Geng, Z.; Cui, Z.; Li, Z.; Zhu, S.; Liang, Y.; Liu, Y.; Li, X.; He, X.; Yu, X.; Wang, R.; et al. Strontium Incorporation to Optimize the Antibacterial and Biological Characteristics of Silver-Substituted Hydroxyapatite Coating. Mater. Sci. Eng. C 2016, 58, 467–477. [Google Scholar] [CrossRef]
- Jin, G.; Qin, H.; Cao, H.; Qian, S.; Zhao, Y.; Peng, X.; Zhang, X.; Liu, X.; Chu, P.K. Synergistic Effects of Dual Zn/Ag Ion Implantation in Osteogenic Activity and Antibacterial Ability of Titanium. Biomaterials 2014, 35, 7699–7713. [Google Scholar] [CrossRef] [PubMed]
- Yonekura, Y.; Miyamoto, H.; Shimazaki, T.; Ando, Y.; Noda, I.; Mawatari, M.; Hotokebuchi, T. Osteoconductivity of Thermal-Sprayed Silver-Containing Hydroxyapatite Coating in the Rat Tibia. J. Bone Jt. Surg. Br. 2011, 93, 644–649. [Google Scholar] [CrossRef]
- Gopi, D.; Shinyjoy, E.; Kavitha, L. Synthesis and Spectral Characterization of Silver/Magnesium Co-Substituted Hydroxyapatite for Biomedical Applications. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2014, 127, 286–291. [Google Scholar] [CrossRef]
- Landi, E.; Sprio, S.; Sandri, M.; Celotti, G.; Tampieri, A. Development of Sr and CO3 Co-Substituted Hydroxyapatites for Biomedical Applications. Acta Biomater. 2008, 4, 656–663. [Google Scholar] [CrossRef]
- Qadri, S.; Haik, Y.; Mensah-Brown, E.; Bashir, G.; Fernandez-Cabezudo, M.J.; Al-Ramadi, B.K. Metallic Nanoparticles to Eradicate Bacterial Bone Infection. Nanomedicine 2017, 13, 2241–2250. [Google Scholar] [CrossRef]
- Ulbrich, K.; Holá, K.; Šubr, V.; Bakandritsos, A.; Tuček, J.; Zbořil, R. Targeted Drug Delivery with Polymers and Magnetic Nanoparticles: Covalent and Noncovalent Approaches, Release Control, and Clinical Studies. Chem. Rev. 2016, 116, 5338–5431. [Google Scholar] [CrossRef]
- Fang, C.-H.; Tsai, P.-I.; Huang, S.-W.; Sun, J.-S.; Chang, J.Z.-C.; Shen, H.-H.; Chen, S.-Y.; Lin, F.H.; Hsu, L.-T.; Chen, Y.-C. Magnetic Hyperthermia Enhance the Treatment Efficacy of Peri-Implant Osteomyelitis. BMC Infect. Dis. 2017, 17, 516. [Google Scholar] [CrossRef] [Green Version]
- Ferreira-Ermita, D.A.C.; Valente, F.L.; Carlo-Reis, E.C.; Araújo, F.R.; Ribeiro, I.M.; Cintra, C.C.V.; Borges, A.P.B. Characterization and in Vivo Biocompatibility Analysis of Synthetic Hydroxyapatite Compounds Associated with Magnetite Nanoparticles for a Drug Delivery System in Osteomyelitis Treatment. Results Mater. 2020, 5, 100063. [Google Scholar] [CrossRef]
- Ak, G.; Bozkaya, Ü.F.; Yılmaz, H.; Sarı Turgut, Ö.; Bilgin, İ.; Tomruk, C.; Uyanıkgil, Y.; Hamarat Şanlıer, Ş. An Intravenous Application of Magnetic Nanoparticles for Osteomyelitis Treatment: An Efficient Alternative. Int. J. Pharm. 2021, 592, 119999. [Google Scholar] [CrossRef]
- Ai, J.; Biazar, E.; Jafarpour, M.; Montazeri, M.; Majdi, A.; Aminifard, S.; Zafari, M.; Akbari, H.R.; Rad, H.G. Nanotoxicology and Nanoparticle Safety in Biomedical Designs. Int. J. Nanomed. 2011, 6, 1117–1127. [Google Scholar] [CrossRef] [Green Version]
- Vimbela, G.V.; Ngo, S.M.; Fraze, C.; Yang, L.; Stout, D.A. Antibacterial Properties and Toxicity from Metallic Nanomaterials. Int. J. Nanomed. 2017, 12, 3941–3965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albers, C.E.; Hofstetter, W.; Siebenrock, K.A.; Landmann, R.; Klenke, F.M. In Vitro Cytotoxicity of Silver Nanoparticles on Osteoblasts and Osteoclasts at Antibacterial Concentrations. Nanotoxicology 2013, 7, 30–36. [Google Scholar] [CrossRef]
- Pauksch, L.; Hartmann, S.; Rohnke, M.; Szalay, G.; Alt, V.; Schnettler, R.; Lips, K.S. Biocompatibility of Silver Nanoparticles and Silver Ions in Primary Human Mesenchymal Stem Cells and Osteoblasts. Acta Biomater. 2014, 10, 439–449. [Google Scholar] [CrossRef]
- Shen, Y.; Huang, Z.; Liu, X.; Qian, J.; Xu, J.; Yang, X.; Sun, A.; Ge, J. Iron-Induced Myocardial Injury: An Alarming Side Effect of Superparamagnetic Iron Oxide Nanoparticles. J. Cell Mol. Med. 2015, 19, 2032–2035. [Google Scholar] [CrossRef] [PubMed]
- Lyons, J.G.; Plantz, M.A.; Hsu, W.K.; Hsu, E.L.; Minardi, S. Nanostructured Biomaterials for Bone Regeneration. Front. Bioeng. Biotechnol. 2020, 8, 922. [Google Scholar] [CrossRef] [PubMed]
- Connelly, P. Rate of Bony Fusion Using NanoBone® Synthetic Bone Graft Versus Local Autologous Bone Graft. (BONE). Available online: https://clinicaltrials.gov/ct2/show/NCT04615260?term=Rate+of+Bony+Fusion+Using+NanoBone%C2%AE+Synthetic+Bone+Graft+Versus&draw=2&rank=1 (accessed on 4 November 2020).
- Tzur, E. Filling Bone Defects/Voids with Autologous BonoFill-II for Maxillofacial Bone Regeneration. Available online: https://www.centerwatch.com/clinical-trials/listings/97777/filling-bone-defectsvoids-with-autologous-bonofill-ii-for-maxillofacial-bone-regeneration/?sort_by=last_updated&page=2&query=osteomyelitis&rnk=20 (accessed on 25 July 2015).
- Borens, O. CERAMENTTM|G-Bone Healing and Re-Infection Prophylaxis. Available online: https://clinicaltrials.gov/ct2/show/NCT02128256?type=Intr&cond=osteomyelitis&draw=3&rank=19 (accessed on 1 May 2014).
- Gambaro, F.M.; Ummarino, A.; Andón, F.T.; Ronzoni, F.; Di Matteo, B.; Kon, E. Drug Delivery Systems for the Treatment of Knee Osteoarthritis: A Systematic Review of In Vivo Studies. Int. J. Mol. Sci. 2021, 22, 9137. [Google Scholar] [CrossRef] [PubMed]
- Hegazi, M.S.; Hassan, R. Post-Operative Pain Reduction after Application of Three Intracanal Medicament within Necrotic Root Canals and Pulp. Available online: https://clinicaltrials.gov/ct2/show/NCT04338633?term=nanotechnology&recrs=abdf&draw=3&rank=15 (accessed on 8 November 2018).
- Ferry, T. Evaluation of the Efficiency of the Bone Substitute Cerament-G Locally Delivering Gentamicin in the Treatment of Chronic Osteomyelitis of Long Bones (CONVICTION). Available online: https://clinicaltrials.gov/ct2/show/NCT04805164?type=Intr&cond=osteomyelitis&draw=2&rank=1 (accessed on 18 March 2021).
- Hofmann, A.; Gorbulev, S.; Guehring, T.; Schulz, A.P.; Schupfner, R.; Raschke, M.; Huber-Wagner, S.; Rommens, P.M. Autologous Iliac Bone Graft Compared with Biphasic Hydroxyapatite and Calcium Sulfate Cement for the Treatment of Bone Defects in Tibial Plateau Fractures. J. Bone Jt. Surg. 2020, 102, 179–193. [Google Scholar] [CrossRef] [Green Version]
- Haider, S. Nanoparticles: The Future of Drug Delivery. J. Young Investig. 2020, 38. [Google Scholar]
- Tang, B.; Zhu, W. Progress in Diagnosis and Treatment of Post-Traumatic Osteomyelitis. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2021, 46, 1290–1297. [Google Scholar] [CrossRef]



| Diagnostic Procedure | Scoring | Diagnosis | Score (Add the Score for Each Procedure) | |
| Clinical History and Risk Factors | Can score up to 6 points/procedure | |||
| Clinical examination and laboratory test results (e.g., leukocyte counts, inflammatory markers, ESR, and CRP) | ||||
| Class A—Safe | ≥18 points | |||
| Class B—Probable | 8–17 points | |||
| Diagnostic imaging (e.g., ultrasounds, radiology, CT, MRI, nuclear medicine, etc.) | ||||
| Class C—Possible but unlikely | ≤8 points | |||
| Microbiology analysis | ||||
| Histopathology | ||||
| A reliable diagnosis can only be made if at least 3 procedures are scored with 6 points. | ||||
| Grade | Characteristics | |
|---|---|---|
| Clinical | Acute | |
| Grade 1 | Acute fulminating | |
| Grade 2 | Sub-acute | |
| Grade 3a | Acute with insidious onset | |
| Grade 3b | Acute exacerbation of chronic | |
| Chronic | ||
| Grade 4 | Chronic overwhelming | |
| Grade 5 | Chronic diffuse with inflammation | |
| Grade 6 | Chronic low grade extensive without inflammation | |
| Grade 7 | Chronic localized lesion | |
| Grade 8 | Non-infective pathology | |
| Laboratory Results | Chronic | |
| Grade 4 | Increased WBC, neutrophilia, left shift and toxic granulation, decreased transferrin, procalcitonin > 2, increased platelets, abnormal RBC corpuscles | |
| Grade 5 | Decreased Hb MCV and MCH, rouleaux formation | |
| Grade 6 | Increased ferritin, decreased iron, decreased iron saturation, increased ESR | |
| Grade 7 | Ferritin iron ratio > 7 | |
| Grade 8 | Normal | |
| Radiological Findings |
|
| Antibiotic: | Dosage: | Notes: |
|---|---|---|
| Nafcillin | 9–12 g/day (6 individual doses) (IV administration) | Empiric antibiotic of choice Causative bacteria: Staphylococcus aureus |
| Penicillin G | 4 million units every 6 h (IV administration) | Causative bacteria: Streptococcus pneumoniae |
| Vancomycin | 30 mg/kg/day (2–3 doses) (IV administration) | Used for patients with penicillin-allergic reactions due to methicillin resistant S. aureus (MRSA) Causative bacteria: MRSA |
| Ceftazidime | 2g every 8 h (IV administration) | Administered with an aminoglycoside IV for the first two weeks Causative bacteria: Pseudomonas aeruginosa |
| Ciprofloxacin | 750 mg every 12 h (Oral administration) | Causative bacteria: Enteric gram-negative rods |
| Augmentin | 875 mg every 12 h (Oral administration) | Causative bacteria: Mixed aerobic organisms |
| Clindamycin | 600 mg every 6 h (Oral administration) | Causative bacteria: Anaerobes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zapata, D.; Higgs, J.; Wittholt, H.; Chittimalli, K.; Brooks, A.E.; Mulinti, P. Nanotechnology in the Diagnosis and Treatment of Osteomyelitis. Pharmaceutics 2022, 14, 1563. https://doi.org/10.3390/pharmaceutics14081563
Zapata D, Higgs J, Wittholt H, Chittimalli K, Brooks AE, Mulinti P. Nanotechnology in the Diagnosis and Treatment of Osteomyelitis. Pharmaceutics. 2022; 14(8):1563. https://doi.org/10.3390/pharmaceutics14081563
Chicago/Turabian StyleZapata, Demi, Jordan Higgs, Hunter Wittholt, Kishore Chittimalli, Amanda E. Brooks, and Pranothi Mulinti. 2022. "Nanotechnology in the Diagnosis and Treatment of Osteomyelitis" Pharmaceutics 14, no. 8: 1563. https://doi.org/10.3390/pharmaceutics14081563
APA StyleZapata, D., Higgs, J., Wittholt, H., Chittimalli, K., Brooks, A. E., & Mulinti, P. (2022). Nanotechnology in the Diagnosis and Treatment of Osteomyelitis. Pharmaceutics, 14(8), 1563. https://doi.org/10.3390/pharmaceutics14081563







