Effect of Lipid Composition on the Atheroprotective Properties of HDL-Mimicking Micelles
Abstract
:1. Introduction
2. Materials and Methods
2.1. Material
2.2. Preparation of Micelle Library
2.3. Characterization of Micelles
2.4. Cholesterol Crystal Dissolution
2.5. Cholesterol Efflux
2.6. Anti-Inflammatory Effects of Micelles
2.7. Pharmacokinetic/Pharmacodynamic Evaluation in Rats
2.8. Quantification of Serum Phospholipids and Cholesterol
2.9. Pharmacokinetic/Pharmacodynamic Analysis
2.10. Statistical Analysis
3. Results
3.1. Preparation and Characterization of Micelles
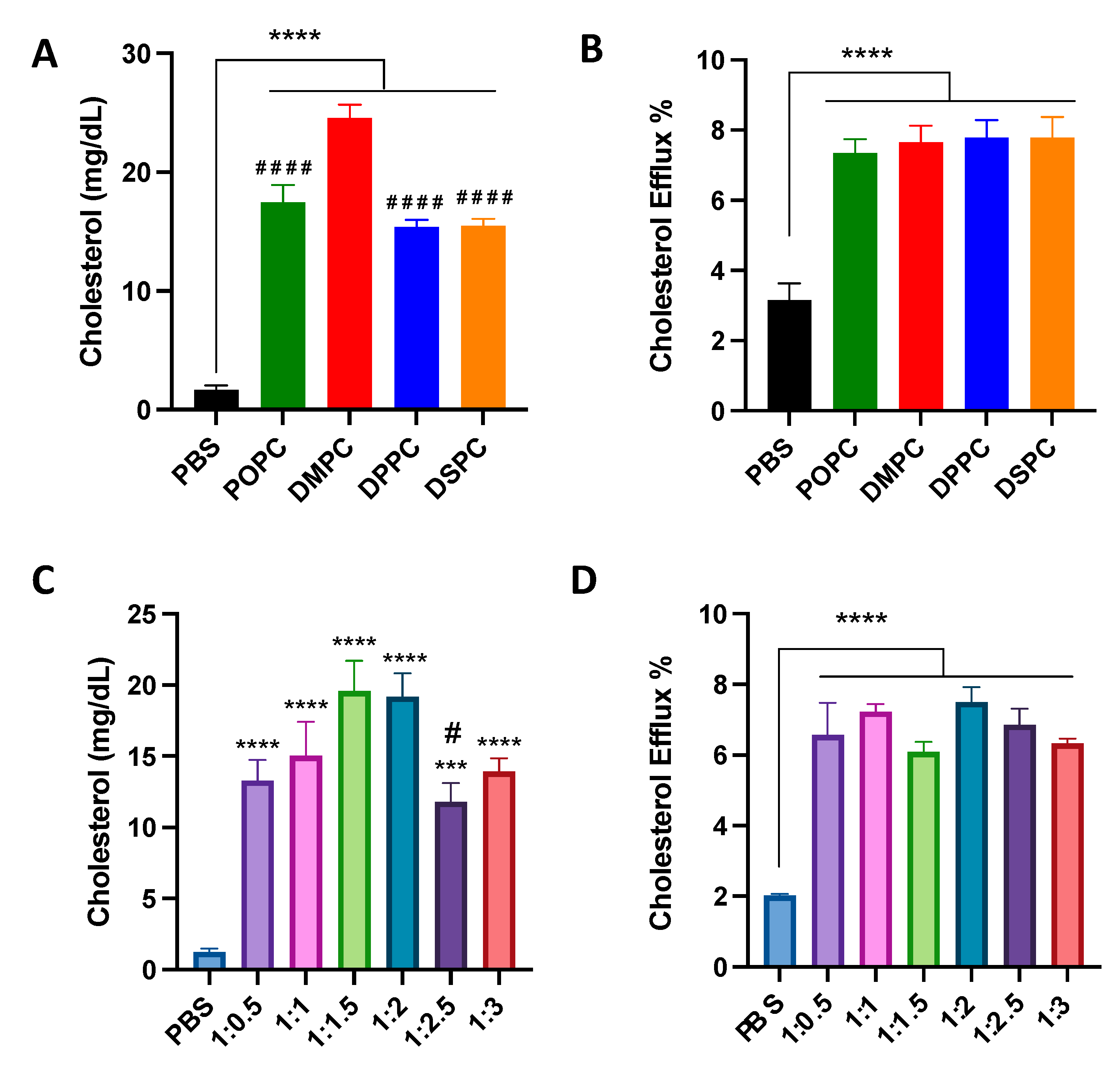
3.2. Cholesterol Crystal Dissolution and Cholesterol Efflux Capacity of Micelles
3.3. Anti-Inflammatory Effects of Micelles
3.4. Effects of PC Lipid Composition on the PK/PD Profiles
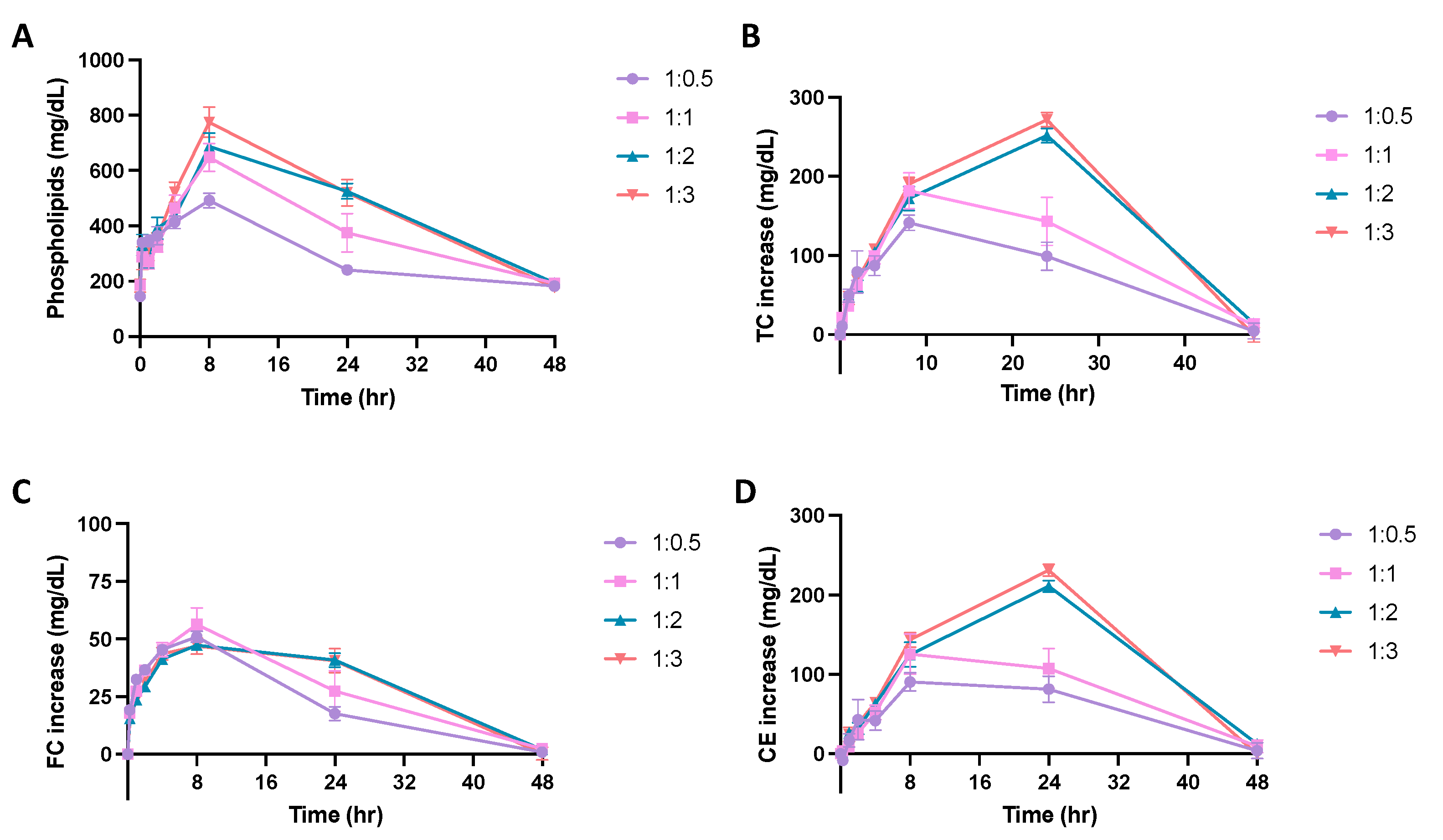
3.5. Effects of PEGylation on the PK/PD Profiles
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pahwa, R.; Jialal, I. Atherosclerosis—StatPearls—NCBI Bookshelf. StatPearls 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK507799/ (accessed on 21 April 2022).
- NIH. Atherosclerosis |NHLBI, NIH. Natl. Heat Lung Blood Inst. 2020. Available online: https://www.nhlbi.nih.gov/health-topics/atherosclerosis (accessed on 21 April 2022).
- Spagnoli, L.G.; Mauriello, A.; Sangiorgi, G.; Bonanno, E.; Schwartz, R.S.; Piepgras, D.G.; Pistolese, R.; Ippoliti, A.; Homes, D.R. Extracranial thrombotically active carotid plaque as a risk factor for ischemic stroke. J. Am. Med. Assoc. 2004, 292, 1845–1852. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Formanowicz, D.; Krawczyk, J.B. Controlling the thickness of the atherosclerotic plaque by statin medication. PLoS ONE 2020, 15, e0239953. [Google Scholar] [CrossRef] [PubMed]
- LaRosa, J.C.; He, J.; Vupputuri, S. Effect of statins on risk of coronary disease. A meta-analysis of randomized controlled trials. J. Am. Med. Assoc. 1999, 282, 2340–2346. [Google Scholar] [CrossRef] [PubMed]
- Yurdagul, A., Jr.; Finney, A.; Woolard, M.D.; Orr, A.W. The Arterial Microenvironment: The Where and Why of Atherosclerosis. Biochem. J. 2016, 473, 1281–1295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chistiakov, D.A.; Melnichenko, A.A.; Myasoedova, V.A.; Grechko, A.V.; Orekhov, A.N. Mechanisms of foam cell formation in atherosclerosis. J. Mol. Med. 2017, 95, 1153–1165. [Google Scholar] [CrossRef] [PubMed]
- Janoudi, A.; Shamoun, F.E.; Kalavakunta, J.K.; Abela, G.S. Cholesterol crystal induced arterial inflammation and destabilization of atherosclerotic plaque. Eur. Heart J. 2016, 37, 1959–1967. [Google Scholar] [CrossRef] [Green Version]
- Abela, G.S. Cholesterol crystals piercing the arterial plaque and intima trigger local and systemic inflammation. J. Clin. Lipidol. 2010, 4, 156–164. [Google Scholar] [CrossRef]
- Samstad, E.O.; Niyonzima, N.; Nymo, S.; Aune, M.H.; Ryan, L.; Bakke, S.S.; Lappegård, K.T.; Brekke, O.-L.; Lambris, J.; Damås, J.K.; et al. Cholesterol crystals induce complement-dependent inflammasome activation and cytokine release. J. Immunol. 2014, 192, 2837–2845. [Google Scholar] [CrossRef] [Green Version]
- Kuai, R.; Li, D.; Chen, Y.E.; Moon, J.J.; Schwendeman, A. High-Density Lipoproteins: Nature’s Multifunctional Nanoparticles. ACS Nano 2016, 10, 3015–3041. [Google Scholar] [CrossRef] [Green Version]
- Tricoci, P.; D’Andrea, D.M.; Gurbel, P.A.; Yao, Z.; Cuchel, M.; Winston, B.; Schott, R.; Weiss, R.; Blazing, M.A.; Cannon, L.; et al. Infusion of Reconstituted High-Density Lipoprotein, CSL112, in Patients with Atherosclerosis: Safety and Pharmacokinetic Results from a Phase 2a Randomized Clinical Trial. J. Am. Heart Assoc. 2015, 4, e002171. [Google Scholar] [CrossRef] [Green Version]
- Keyserling, C.H.; Barbaras, R.; Benghozi, R.; Dasseux, J.L. Development of CER-001: Preclinical Dose Selection Through to Phase I Clinical Findings. Clin. Drug Investig. 2017, 37, 483–491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanchez-Gaytan, B.L.; Fay, F.; Lobatto, M.E.; Tang, J.; Ouimet, M.; Kim, Y.; van der Staay, S.E.M.; van Rijs, S.M.; Priem, B.; Zhang, L.; et al. HDL-mimetic PLGA nanoparticle to target atherosclerosis plaque macrophages. Bioconjugate Chem. 2015, 26, 443–451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lai, C.T.; Sun, W.Q.; Palekar, R.U.; Thaxton, C.S.; Schatz, G.C. Molecular Dynamics Simulation and Experimental Studies of Gold Nanoparticle Templated HDL-like Nanoparticles for Cholesterol Metabolism Therapeutics. ACS Appl. Mater. Interfaces 2017, 9, 1247–1254. [Google Scholar] [CrossRef] [PubMed]
- Brace, R.J.; Sorrenson, B.; Sviridov, D.; McCormick, S.P. A gel-based method for purification of apolipoprotein A-I from small volumes of plasma. J. Lipid Res. 2010, 51, 3370–3376. [Google Scholar] [CrossRef] [Green Version]
- Feng, M.Q.; Cai, Q.S.; Song, D.X.; Dong, J.B.; Zhou, P. High yield and secretion of recombinant human apolipoprotein AI in Pichia pastoris. Protein Expr. Purif. 2006, 46, 337–342. [Google Scholar] [CrossRef]
- Pyle, L.E.; Fidge, N.H.; Barton, P.A.; Luong, A.; Sviridov, D. Production of mature human apolipoprotein A-I in a baculovirus-insect cell system: Propeptide is not essential for intracellular processing but may assist rapid secretion. Anal. Biochem. 1997, 253, 253–258. [Google Scholar] [CrossRef] [PubMed]
- McGuire, K.A.; Davidson, W.S.; Jonas, A. High yield overexpression and characterization of human recombinant proapolipoprotein A–I. J. Lipid Res. 1996, 37, 1519–1528. [Google Scholar] [CrossRef]
- Brissette, L.; Cahuzac-Bec, N.; Desforges, M.; Bec, J.L.; Marcel, Y.L.; Rassart, E. Expression of recombinant human apolipoprotein A–I in Chinese hamster ovary cells and Escherichia coli. Protein Expr. Purif. 1991, 2, 296–303. [Google Scholar] [CrossRef]
- Damen, J.; Regts, J.; Scherphof, G. Transfer and exchange of phospholipid between small unilamellar liposomes and rat plasma high density lipoproteins Dependence on cholesterol content and phospholipid composition. Biochim. Biophys. Acta (BBA)/Lipids Lipid Metab. 1981, 665, 538–545. [Google Scholar] [CrossRef]
- Dass, C.R.; Jessup, W. Apolipoprotein A–I, Cyclodextrins and Liposomes as Potential Drugs for the Reversal of Atherosclerosis. A Review. J. Pharm. Pharmacol. 2010, 52, 731–761. [Google Scholar] [CrossRef]
- Luo, Y.; Guo, Y.; Wang, H.; Yu, M.; Hong, K.; Li, D.; Li, R.; Wen, B.; Hu, D.; Chang, L.; et al. Phospholipid nanoparticles: Therapeutic potentials against atherosclerosis via reducing cholesterol crystals and inhibiting inflammation. EBioMedicine 2021, 74, 103725. [Google Scholar] [CrossRef] [PubMed]
- Fawaz, M.V.; Kim, S.Y.; Li, D.; Ming, R.; Xia, Z.; Olsen, K.; Pogozheva, I.D.; Tesmer, J.J.G.; Schwendeman, A. Phospholipid component defines pharmacokinetic and pharmacodynamic properties of synthetic high-density lipoproteins. J. Pharmacol. Exp. Ther. 2020, 372, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Schwendeman, A.; Sviridov, D.O.; Yuan, W.; Guo, Y.; Morin, E.E.; Yuan, Y.; Stonik, J.; Freeman, L.; Ossoli, A.; Thacker, S.; et al. The effect of phospholipid composition of reconstituted HDL on its cholesterol efflux and anti-inflammatory properties. J. Lipid Res. 2015, 56, 1727–1737. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, D.; Fawas, M.; Morin, E.; Ming, R.; Sviridov, D.; Tang, J.; Ackermann, R.; Olsen, K.; Remaley, A.T.; Schwendeman, A. The effect of synthetic high density lipoproteins modification with polyethylene glycol on pharmacokinetics and pharmacodynamics. Mol. Pharm. 2018, 15, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Prilepskii, A.Y.; Serov, N.S.; Kladko, D.V.; Vinogradov, V.V. Nanoparticle-based approaches towards the treatment of atherosclerosis. Pharmaceutics 2020, 12, 1056. [Google Scholar] [CrossRef] [PubMed]
- Thewalt, J.L.; Bloom, M. Phosphatidylcholine: Cholesterol phase diagrams. Biophys. J. 1992, 63, 1176–1181. [Google Scholar] [CrossRef] [Green Version]
- Koynova, R.; Caffrey, M. Phases and phase transitions of the phosphatidylcholines. Biochim. Biophys. Acta Rev. Biomembr. 1998, 1376, 91–145. [Google Scholar] [CrossRef]
- Wang, M.; Zander, T.; Liu, X.; Liu, C.; Raj, A.; Wieland, D.C.F.; Garamus, V.M.; Willumeit-Römer, R.; Claesson, P.M.; Dėdinaitė, A. The effect of temperature on supported dipalmitoylphosphatidylcholine (DPPC) bilayers: Structure and lubrication performance. J. Colloid Interface Sci. 2015, 445, 84–92. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.; Cheng, D.; Li, J.; Wang, Y.; Guo, J.X.; Chen, Z.P.; Cai, B.C.; Yang, T. Influence of lipid composition on the phase transition temperature of liposomes composed of both DPPC and HSPC. Drug Dev. Ind. Pharm. 2013, 39, 197–204. [Google Scholar] [CrossRef]
- Abumanhal-Masarweh, H.; da Silva, D.; Poley, M.; Zinger, A.; Goldman, E.; Krinsky, N.; Kleiner, R.; Shenbach, G.; Schroeder, J.E.; Shklover, J.; et al. Tailoring the lipid composition of nanoparticles modulates their cellular uptake and affects the viability of triple negative breast cancer cells. J. Control. Release 2019, 307, 331–341. [Google Scholar] [CrossRef]
- Kim, S.Y. Optimization of Syntheic High-Density Lipoprotein Nanostructures for Treatment of Inflammatory Diseases; University of Michigan Library: Ann Arbor, MI, USA, 2019. [Google Scholar]
- Matthew, T.H.; Huang, L. Maximizing the Supported Bilayer Phenomenon: Liposomes Comprised Exclusively of PEGylated Phospholipids for Enhanced Systemic and Lymphatic Delivery. Physiol. Behav. 2017, 176, 139–148. [Google Scholar] [CrossRef]
- Yang, C.; Gao, S.; Dagnæs-Hansen, F.; Jakobsen, M.; Kjems, J. Impact of PEG Chain Length on the Physical Properties and Bioactivity of PEGylated Chitosan/siRNA Nanoparticles in Vitro and in Vivo. ACS Appl. Mater. Interfaces 2017, 9, 12203–12216. [Google Scholar] [CrossRef] [PubMed]
- Parveen, S.; Sahoo, S.K. Long circulating chitosan/PEG blended PLGA nanoparticle for tumor drug delivery. Eur. J. Pharmacol. 2011, 670, 372–383. [Google Scholar] [CrossRef] [PubMed]



| Formulation (Molar Ratio) | Size (nm) | PDI |
|---|---|---|
| POPC:DSPE-PEG2k (1:2.09). | 15.97 ± 0.20 | 0.162 ± 0.047 |
| DMPC:DSPE-PEG2k (1:2.09) | 17.12 ± 1.09 | 0.298 ± 0.030 |
| DPPC:DSPE-PEG2k (1:2.09) | 18.29 ± 1.39 | 0.196 ± 0.028 |
| DSPC:DSPE-PEG2k (1:2.09) | 17.32 ± 0.30 | 0.061 ± 0.016 |
| DMPC:DSPE-PEG2k (1:0.5) | 29.74 ± 2.02 | 0.306 ± 0.002 |
| DMPC:DSPE-PEG2k (1:1) | 17.14 ± 0.51 | 0.190 ± 0.048 |
| DMPC:DSPE-PEG2k (1:1.5) | 18.88 ± 1.45 | 0.333 ± 0.033 |
| DMPC:DSPE-PEG2k (1:2) | 15.51 ± 0.41 | 0.260 ± 0.030 |
| DMPC:DSPE-PEG2k (1:2.5) | 17.69 ± 0.69 | 0.559 ± 0.028 |
| DMPC:DSPE-PEG2k (1:3) | 15.86 ± 0.88 | 0.344 ± 0.050 |
| Parameters | POPC | DMPC | DPPC | DSPC |
|---|---|---|---|---|
| Cmax (mg/dL) | 507.4 (20.1) | 723.7 (24.1) | 613.5 (25.1) | 678.1 (48.5) |
| Tmax (h) | 7.0 (28.6) | 7.0 (28.6) | 6.7 (34.6) | 7.0 (28.6) |
| AUC (mg·h/dL) | 16,732.8 (21.4) | 17,654.4 (18.2) | 188,482.0 (32.2) | 20,607.5 (37.4) |
| K10 (h−1) | 0.022 (33.6) | 0.027 (17.1) | 0.025 (36.0) | 0.026 (44.9) |
| T1/2 (h) | 35.0 (46.5) | 31.0 (41.8) | 29.9 (34.5) | 33.5 (81.7) |
| CL (dL/h) | 0.001 (32.9) | 0.001(5.4) | 0.001(56.7) | 0.001 (57.1) |
| VSS (dL) | 0.051 (20.2) | 0.047 (37.9) | 0.044 (20.7) | 0.043 (49.4) |
| Parameters | POPC | DMPC | DPPC | DSPC | |
|---|---|---|---|---|---|
| TC | Tmax (h) | 20.0 (40.0) | 12.0 (66.7) | 18.6 (49.5) | 8.0 (0.0) |
| Emax (mg/dL) | 201.9 (16.8) | 234.7 (33.6) | 251.4 (20.6) | 226.2 (11.0) | |
| AUEC (mg·h/dL) | 6043.8 (23.9) | 5925.7 (28.4) | 7266.0 (16.5) | 6472.5 (12.4) | |
| FC | Tmax (h) | 8.0 (0.0) | 8.0 (0.0) | 8.0 (0.0) | 8.0 (0.0) |
| Emax (mg/dL) | 72.0 (9.4) | 64.5 (24.7) | 76.5 (9.5) | 77.9 (1.5) | |
| AUEC (mg·h/dL) | 1600.0 (8.1) | 1488.0 (32.1) | 1923.6 (11.6) | 1868.6 (9.5) | |
| CE | Tmax (h) | 24.0 (0.0) | 20.0 (4.0) | 24.0 (0.0) | 20.0 (4.0) |
| Emax (mg/dL) | 164.1 (15.9) | 180.1 (37.9) | 197.0 (25.9) | 159.0 (18.8) | |
| AUEC (mg·h/dL) | 4382.4 (30.7) | 4437.7 (27.2) | 5189.1 (25.3) | 4492.7 (16.0) |
| Parameters | 1:0.5 | 1:1 | 1:2 | 1:3 |
|---|---|---|---|---|
| Cmax (mg/dL) | 523.2 (18.0) | 648.0 (15.6) | 686.7 (14.2) | 775.0 (14.1) |
| Tmax (h) | 6.0 (63.9) | 8.0 (0.0) | 8.0 (0.0) | 8.0 (0.0) |
| AUC (mg·h/dL) | 14,266.1 (7.0) | 18,595.4 (19.7) | 22,019.4 (10.1) | 22,815.2 (13.5) |
| K10 (h−1) | 0.023 (23.3) | 0.030 (20.2) | 0.032 (10.8) | 0.038 (9.6) |
| T1/2 (h) | 31.2 (20.3) | 24.0 (21.3) | 21.6 (10.8) | 18.58 (9.3) |
| CL (dL/h) | 0.006 (11.6) | 0.005 (18.3) | 0.005 (9.2) | 0.005 (13.0) |
| VSS (dL) | 0.277 (12.8) | 0.196 (22.7) | 0.158 (13.0) | 0.142 (17.4) |
| Parameters | 1:0.5 | 1:1 | 1:2 | 1:3 | |
|---|---|---|---|---|---|
| TC | Tmax,E (h) | 8.0 (0.0) | 8.0 (0.0) | 24.0 (0.0) | 24.0 (0.0) |
| Emax (mg/dL) | 141.5 (13.7) | 181.9 (25.2) | 251.7 (7.2) | 271.7 (6.7) | |
| AUEC (mg·h/dL) | 3883.3 (17.9) | 5252.1 (33.8) | 7383.8 (8.7) | 7813.3 (8.0) | |
| FC | Tmax,E (h) | 8.0 (0.0) | 12.0 (66.7) | 8.0 (0.0) | 6.0 (38.5) |
| Emax (mg/dL) | 50.9 (9.5) | 58.4 (24.5) | 47.3 (4.7) | 47.3 (14.8) | |
| AUEC (mg·h/dL) | 1102.7 (14.6) | 1529.6 (30.0) | 1511.5 (10.0) | 1492.6 (23.3) | |
| CE | Tmax,E (h) | 15.0 (70.10) | 12.0 (66.7) | 24.0 (0.0) | 24.0 (0.0) |
| Emax (mg/dL) | 96.9 (19.6) | 129.6 (38.1) | 210.8 (6.8) | 231.0 (6.6) | |
| AUEC (mg·h/dL) | 2780.5 (24.9) | 3722.5 (44.0) | 5872.2 (10.1) | 6320.7 (6.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, K.; Yu, M.; Crowther, J.; Mei, L.; Olsen, K.; Luo, Y.; Chen, Y.E.; Guo, Y.; Schwendeman, A. Effect of Lipid Composition on the Atheroprotective Properties of HDL-Mimicking Micelles. Pharmaceutics 2022, 14, 1570. https://doi.org/10.3390/pharmaceutics14081570
Hong K, Yu M, Crowther J, Mei L, Olsen K, Luo Y, Chen YE, Guo Y, Schwendeman A. Effect of Lipid Composition on the Atheroprotective Properties of HDL-Mimicking Micelles. Pharmaceutics. 2022; 14(8):1570. https://doi.org/10.3390/pharmaceutics14081570
Chicago/Turabian StyleHong, Kristen, Minzhi Yu, Julia Crowther, Ling Mei, Karl Olsen, Yonghong Luo, Yuqing Eugene Chen, Yanhong Guo, and Anna Schwendeman. 2022. "Effect of Lipid Composition on the Atheroprotective Properties of HDL-Mimicking Micelles" Pharmaceutics 14, no. 8: 1570. https://doi.org/10.3390/pharmaceutics14081570
APA StyleHong, K., Yu, M., Crowther, J., Mei, L., Olsen, K., Luo, Y., Chen, Y. E., Guo, Y., & Schwendeman, A. (2022). Effect of Lipid Composition on the Atheroprotective Properties of HDL-Mimicking Micelles. Pharmaceutics, 14(8), 1570. https://doi.org/10.3390/pharmaceutics14081570






