Chemopreventive and Anticancer Role of Resveratrol against Oral Squamous Cell Carcinoma
Abstract
:1. Introduction
2. Methodology
3. Oral Squamous Cell Carcinoma (OSCC)
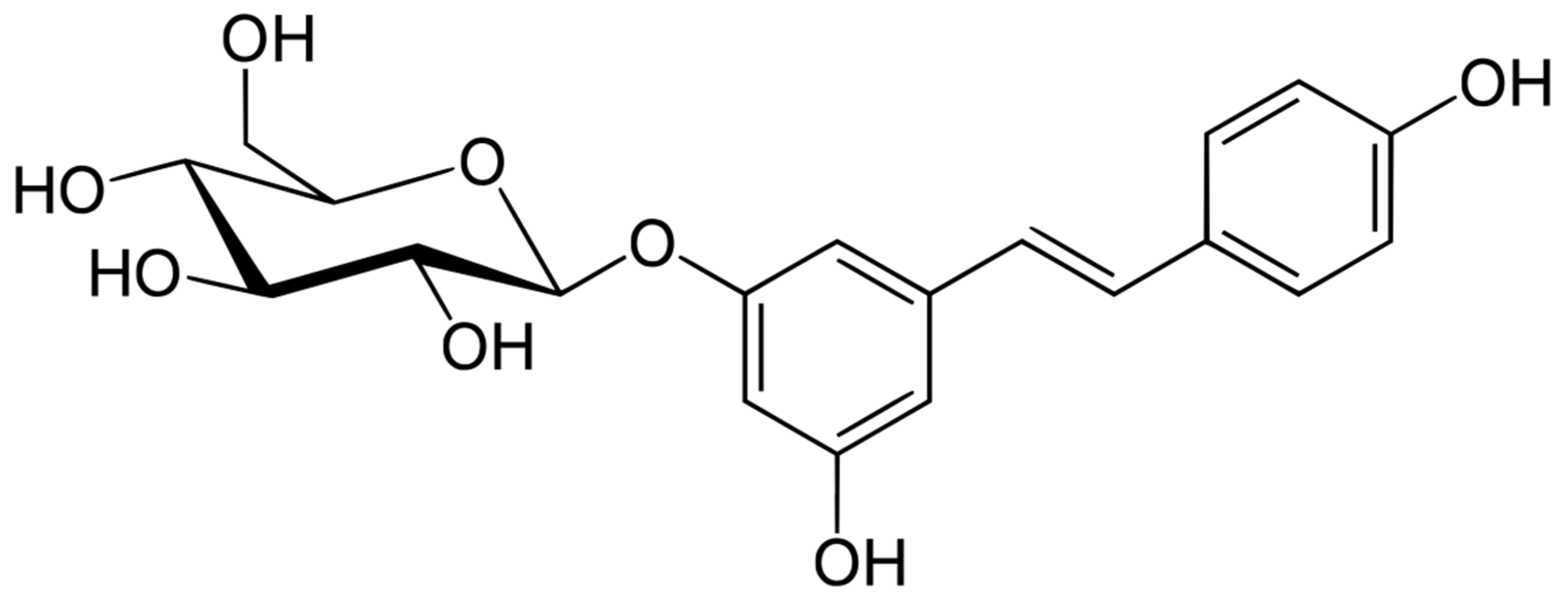
4. Resveratrol (RSV) and Polydatin (PD)
5. In Vitro and In Vivo Chemopreventive and Anticancer Activities of RSV and PD against OSCC
5.1. In Vitro Studies
5.2. Summary of the Employed Cell Lines, Considered Markers, and General Overview of the in Vitro Results
- Proapoptotic effect due to internucleosomal DNA fragmentation; the cleavage of procaspase-3, -7, and -9, as well as caspase-3; the downregulation of MMPs; the activation of Bax and Bak proteins; the reduction in bcl-2 and bcl-XL expression; the activation of caspase-3 and -9; and the release of cytochrome c from mitochondria [37,38,45].
- Antimetastatic effects due to reduced cell adhesion (even after short, 1–5 h, treatments) and migration. Particularly, after LPA (proinvasion agent) pretreatment, the antimetastatic effect emerged as being related to the promotion of EMT transcription factors (e.g., TWIST and SLUG) [36,38,39,40,43,44].
5.3. Safety of RSV Administration
5.4. In Vivo Studies
6. Innovative RSV-Loaded Formulations to Treat OSCC
7. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Markopoulos, A.K. Current Aspects on Oral Squamous Cell Carcinoma. Open Dent. J. 2012, 6, 126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, H.B.d.P.; dos Santos, T.K.G.; Paz, A.R.; Cavalcanti, Y.W.; Nonaka, C.F.W.; Godoy, G.P.; Alves, P.M. Clinical findings and risk factors to oral squamous cell carcinoma in young patients: A 12-year retrospective analysis. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e151–e156. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.E.; Burtness, B.; Leemans, C.R.; Lui, V.W.Y.; Bauman, J.E.; Grandis, J.R. Head and neck squamous cell carcinoma. Nat. Rev. Dis. Prim. 2020, 6, 92. [Google Scholar] [CrossRef] [PubMed]
- Haque, A.; Brazeau, D.; Amin, A.R. Perspectives on natural compounds in chemoprevention and treatment of cancer: An update with new promising compounds. Eur. J. Cancer 2021, 149, 165–183. [Google Scholar] [CrossRef]
- Chinembiri, T.N.; Du Plessis, L.H.; Gerber, M.; Hamman, J.H.; Du Plessis, J. Review of Natural Compounds for Potential Skin Cancer Treatment. Molecules 2014, 19, 11679–11721. [Google Scholar] [CrossRef] [Green Version]
- Rejhová, A.; Opattová, A.; Čumová, A.; Slíva, D.; Vodička, P. Natural compounds and combination therapy in colorectal cancer treatment. Eur. J. Med. Chem. 2018, 144, 582–594. [Google Scholar] [CrossRef]
- Cardona-Mendoza, A.; Olivares-Niño, G.; Díaz-Báez, D.; Lafaurie, G.I.; Perdomo, S.J. Chemopreventive and Anti-tumor Potential of Natural Products in Oral Cancer. Nutr. Cancer 2021, 74, 779–795. [Google Scholar] [CrossRef]
- Prakash, S.; Radha; Kumar, M.; Kumari, N.; Thakur, M.; Rathour, S.; Pundir, A.; Sharma, A.K.; Bangar, S.P.; Dhumal, S.; et al. Plant-Based Antioxidant Extracts and Compounds in the Management of Oral Cancer. Antioxidants 2021, 10, 1358. [Google Scholar] [CrossRef] [PubMed]
- Cháirez-Ramírez, M.H.; de la Cruz-López, K.G.; García-Carrancá, A. polyphenols as antitumor agents targeting key players in cancer-driving signaling pathways. Front. Pharmacol. 2021, 12, 2672. [Google Scholar] [CrossRef] [PubMed]
- Coimbra, M.; Isacchi, B.; Van Bloois, L.; Torano, J.S.; Ket, A.; Wu, X.; Broere, F.; Metselaar, J.M.; Rijcken, C.J.F.; Storm, G.; et al. Improving solubility and chemical stability of natural compounds for medicinal use by incorporation into liposomes. Int. J. Pharm. 2011, 416, 433–442. [Google Scholar] [CrossRef]
- Rauf, A.; Imran, M.; Butt, M.S.; Nadeem, M.; Peters, D.G.; Mubarak, M.S. Resveratrol as an anti-cancer agent: A review. Crit. Rev. Food Sci. Nutr. 2018, 58, 1428–1447. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Zhao, X.; Zeng, X.; Dan, H.; Chen, Q. Non-Invasive Techniques for Detection and Diagnosis of Oral Potentially Malignant Disorders. Tohoku J. Exp. Med. 2016, 238, 165–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Givony, S. Oral squamous cell carcinoma (OSCC) an overview. J. Med. Sci. 2020, 8, 67–74. [Google Scholar]
- Jerjes, W.; Upile, T.; Petrie, A.; Riskalla, A.; Hamdoon, Z.; Vourvachis, M.; Karavidas, K.; Jay, A.; Sandison, A.; Thomas, G.J.; et al. Clinicopathological parameters, recurrence, locoregional and distant metastasis in 115 T1-T2 oral squamous cell carcinoma patients. Head Neck Oncol. 2010, 2, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rivera, C. Essentials of oral cancer. Int. J. Clin. Exp. Pathol. 2015, 8, 11884. [Google Scholar]
- Schoop, R.A.L.; Noteborn, M.H.M.; Baatenburg De Jong, R.J. A mouse model for oral squamous cell carcinoma. J. Mol. Histol. 2009, 40, 177–181. [Google Scholar] [CrossRef] [Green Version]
- Varela, P.; Manuel, J.; Gmez, I.; Diz-Dios, P.; de Melo, N.S.; Seoane, J. Timing of Oral Cancer Diagnosis: Implications for Prognosis and Survival. In Oral Cancer; InTechOpen: London, UK, 2012. [Google Scholar]
- Dumache, R. Early Diagnosis of Oral Squamous Cell Carcinoma by Salivary microRNAs. Clin. Lab. 2017, 63, 1771–1776. [Google Scholar] [CrossRef]
- Deshmukh, V.; Shekar, K. Oral Squamous Cell Carcinoma: Diagnosis and Treatment Planning. In Oral and Maxillofacial Surgery for the Clinician; Springer: Singapore, 2021; pp. 1853–1867. [Google Scholar]
- Benetou, V.; Lagiou, A.; Lagiou, P. Chemoprevention of cancer: Current evidence and future prospects. F1000Research 2015, 4, 916. [Google Scholar] [CrossRef] [Green Version]
- Mohan Shankar, G.; Swetha, M.; Keerthana, C.K.; Rayginia, T.P.; Anto, R.J. Cancer Chemoprevention: A Strategic Approach Using Phytochemicals. Front. Pharmacol. 2022, 12, 4044. [Google Scholar]
- Koh, Y.C.; Ho, C.T.; Pan, M.H. Recent advances in cancer chemoprevention with phytochemicals. J. Food Drug Anal. 2020, 28, 14–37. [Google Scholar] [CrossRef] [Green Version]
- Ding, Y.; Yao, H.; Yao, Y.; Fai, L.; Zhang, Z. Protection of Dietary Polyphenols against Oral Cancer. Nutrients 2013, 5, 2173–2191. [Google Scholar] [CrossRef] [Green Version]
- De La Lastra, C.A.; Villegas, I. Resveratrol as an anti-inflammatory and anti-aging agent: Mechanisms and clinical implications. Mol. Nutr. Food Res. 2005, 49, 405–430. [Google Scholar] [CrossRef] [PubMed]
- Du, Q.-H.; Peng, C.; Zhang, H. Polydatin: A review of pharmacology and pharmacokinetics. Pharm. Biol. 2013, 51, 1347–1354. [Google Scholar] [CrossRef] [PubMed]
- Colica, C.; Milanović, M.; Milić, N.; Aiello, V.; De Lorenzo, A.; Abenavoli, L. A systematic review on natural antioxidant properties of resveratrol. Nat. Prod. Commun. 2018, 13, 1934578X1801300923. [Google Scholar] [CrossRef] [Green Version]
- de Sá Coutinho, D.; Pacheco, M.T.; Frozza, R.L.; Bernardi, A. Anti-inflammatory effects of resveratrol: Mechanistic insights. Int. J. Mol. Sci. 2018, 19, 1812. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Zhang, C.X.; Liu, Y.M.; Chen, K.L.; Chen, G. A comparative study of anti-aging properties and mechanism: Resveratrol and caloric restriction. Oncotarget 2017, 8, 65717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xia, N.; Daiber, A.; Förstermann, U.; Li, H. Antioxidant effects of resveratrol in the cardiovascular system. Br. J. Pharmacol. 2017, 174, 1633–1646. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murgia, D.; Mauceri, R.; Campisi, G.; De Caro, V. Advance on resveratrol application in bone regeneration: Progress and perspectives for use in oral and maxillofacial surgery. Biomolecules 2019, 9, 94. [Google Scholar] [CrossRef] [Green Version]
- Ratz-Łyko, A.; Arct, J. Resveratrol as an active ingredient for cosmetic and dermatological applications: A review. J. Cosmet. Laser Ther. 2019, 21, 84–90. [Google Scholar] [CrossRef]
- Udenigwe, C.C.; Ramprasath, V.R.; Aluko, R.E.; Jones, P.J.H. Potential of resveratrol in anticancer and anti-inflammatory therapy. Nutr. Rev. 2008, 66, 445–454. [Google Scholar] [CrossRef]
- Da Costa, D.C.F.; Fialho, E.; Silva, J.L. Cancer chemoprevention by resveratrol: The P53 tumor suppressor protein as a promising molecular target. Molecules 2017, 22, 1014. [Google Scholar] [CrossRef] [Green Version]
- Atienzar, A.N.; Camacho-Alonso, F.; Lopez-Jornet, P. Effects of resveratrol and irradiation upon oral squamous cell carcinoma cells. Acta Odontol. Scand. 2014, 72, 481–488. [Google Scholar] [CrossRef]
- Yu, X.D.; Yang, J.L.; Zhang, W.L.; Liu, D.X. Resveratrol inhibits oral squamous cell carcinoma through induction of apoptosis and G2/M phase cell cycle arrest. Tumor Biol. 2016, 37, 2871–2877. [Google Scholar] [CrossRef] [PubMed]
- Shan, Z.; Yang, G.; Xiang, W.; Pei-jun, W.; Bin, Z. Effects of resveratrol on oral squamous cell carcinoma (OSCC) cells in vitro. J. Cancer Res. Clin. Oncol. 2014, 140, 371–374. [Google Scholar] [CrossRef]
- Kim, S.-H.; Kim, H.-J.; Lee, M.-H.; Yu, S.-K.; Kim, C.S.; Kook, J.-K.; Chun, H.S.; Park, E.; Lee, S.-Y.; Kim, S.G.; et al. Resveratrol induces apoptosis of KB human oral cancer cells. J. Korean Soc. Appl. Biol. Chem. 2011, 54, 966–971. [Google Scholar] [CrossRef]
- Kim, S.-E.; Shin, S.-H.; Lee, J.-Y.; Kim, C.-H.; Chung, I.-K.; Kang, H.-M.; Park, H.-R.; Park, B.-S.; Kim, I.-R. Resveratrol Induces Mitochondrial Apoptosis and Inhibits Epithelial-Mesenchymal Transition in Oral Squamous Cell Carcinoma Cells. Nutr. Cancer 2018, 70, 125–135. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.Y.; Cho, K.H.; Lee, H.Y. Effect of Resveratrol on Oral Cancer Cell Invasion Induced by Lysophosphatidic Acid. J. Dent. Hyg. Sci. 2018, 18, 188–193. [Google Scholar] [CrossRef]
- Kim, J.Y.; Cho, K.H.; Jeong, B.Y.; Park, C.G.; Lee, H.Y. Zeb1 for RCP-induced oral cancer cell invasion and its suppression by resveratrol. Exp. Mol. Med. 2020, 52, 1152–1163. [Google Scholar] [CrossRef]
- Shang, Y.; Jiang, Y.-L.; Ye, L.-J.; Chen, L.-N.; Ke, Y. Resveratrol acts via melanoma-associated antigen A12 (MAGEA12)/protein kinase B (Akt) signaling to inhibit the proliferation of oral squamous cell carcinoma cells. Bioengineered 2021, 12, 2253–2262. [Google Scholar] [CrossRef] [PubMed]
- Masuelli, L.; Stefano, E.D.; Fantini, M.; Mattera, R.; Benvenuto, M.; Marzocchella, L.; Sacchetti, P.; Focaccetti, C.; Bernardini, R.; Tresoldi, I.; et al. Resveratrol potentiates the in vitro and in vivo anti-tumoral effects of curcumin in head and neck carcinomas. Oncotarget 2014, 5, 10745–10762. [Google Scholar] [CrossRef] [Green Version]
- Chang, W.; Tsai, C.; Yang, J.; Hsu, Y.; Shih, L.; Chiu, H.; Bau, D.; Tsai, F. Resveratrol inhibited the metastatic behaviors of cisplatin-resistant human oral cancer cells via phosphorylation of ERK/p-38 and suppression of MMP-2/9. J. Food Biochem. 2021, 45, e13666. [Google Scholar] [CrossRef] [PubMed]
- Uzawa, K.; Amelio, A.L.; Kasamatsu, A.; Saito, T.; Kita, A.; Fukamachi, M.; Sawai, Y.; Toeda, Y.; Eizuka, K.; Hayashi, F.; et al. Resveratrol Targets Urokinase-Type Plasminogen Activator Receptor Expression to Overcome Cetuximab-Resistance in Oral Squamous Cell Carcinoma. Sci. Rep. 2019, 9, 12179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bang, T.-H.; Park, B.-S.; Kang, H.-M.; Kim, J.-H.; Kim, I.-R. Polydatin, a Glycoside of Resveratrol, Induces Apoptosis and Inhibits Metastasis Oral Squamous Cell Carcinoma Cells In Vitro. Pharmaceuticals 2021, 14, 902. [Google Scholar] [CrossRef] [PubMed]
- Campisi, G.; Italo Giannola, L.; Fucarino, A.; Marino Gammazza, A.; Pitruzzella, A.; Marciano, V.; De Caro, V.; Gabriella Siragusa, M.; Giandalia, G.; Compilato, D.; et al. Medium-term culture of primary oral squamous cell carcinoma in a three- dimensional model: Effects on cell survival following topical 5-fluororacile delivery by drug-loaded matrix tablets. Curr. Pharm. Des. 2012, 18, 5411–5420. [Google Scholar] [CrossRef]
- Bucchieri, F.; Fucarino, A.; Marino Gammazza, A.; Pitruzzella, A.; Marciano, V.; Paderni, C.; De Caro, V.; Gabriella Siragusa, M.; Lo Muzio, L.; Holgate, T.S.; et al. Medium-term culture of normal human oral mucosa: A novel three-dimensional model to study the effectiveness of drugs administration. Curr. Pharm. Des. 2012, 18, 5421–5430. [Google Scholar] [CrossRef] [PubMed]
- Jia, Y.; Shao, J.-H.; Zhang, K.-W.; Zou, M.-L.; Teng, Y.-Y.; Tian, F.; Chen, M.-N.; Chen, W.-W.; Yuan, Z.-D.; Wu, J.-J.; et al. Emerging Effects of Resveratrol on Wound Healing: A Comprehensive Review. Molecules 2022, 27, 6736. [Google Scholar] [CrossRef] [PubMed]
- Salehi, B.; Mishra, A.; Nigam, M.; Sener, B.; Kilic, M.; Sharifi-Rad, M.; Fokou, P.; Martins, N.; Sharifi-Rad, J. Resveratrol: A Double-Edged Sword in Health Benefits. Biomedicines 2018, 6, 91. [Google Scholar] [CrossRef] [Green Version]
- Rocha, V.; Marques, C.; Figueiredo, J.L.; Gaio, A.R.; Costa, P.C.; Sousa Lobo, J.M.; Almeida, I.F. In vitro cytotoxicity evaluation of resveratrol-loaded nanoparticles: Focus on the challenges of in vitro methodologies. Food Chem. Toxicol. 2017, 103, 214–222. [Google Scholar] [CrossRef]
- Ivanova, D.; Zhelev, Z.; Semkova, S.; Aoki, I.; Bakalova, R. Resveratrol Modulates the Redox-status and Cytotoxicity of Anticancer Drugs by Sensitizing Leukemic Lymphocytes and Protecting Normal Lymphocytes. Anticancer Res. 2019, 39, 3745–3755. [Google Scholar] [CrossRef]
- Rita, C.O.C.; Tamaki, N.; Mukai, R.; Fukui, M.; Miki, K.; Terao, J.; Ito, H.O. Biological impacts of resveratrol, quercetin, and N-acetylcysteine on oxidative stress in human gingival fibroblasts. J. Clin. Biochem. Nutr. 2015, 56, 220. [Google Scholar]
- Berta, G.N.; Salamone, P.; Sprio, A.E.; Di Scipio, F.; Marinos, L.M.; Sapino, S.; Carlotti, M.E.; Cavalli, R.; Di Carlo, F. Chemoprevention of 7,12-dimethylbenz[a]anthracene (DMBA)-induced oral carcinogenesis in hamster cheek pouch by topical application of resveratrol complexed with 2-hydroxypropyl-β-cyclodextrin. Oral Oncol. 2010, 46, 42–48. [Google Scholar] [CrossRef]
- Zheng, T.; Feng, H.; Liu, L.; Peng, J.; Xiao, H.; Yu, T.; Zhou, Z.; Li, Y.; Zhang, Y.; Bai, X.; et al. Enhanced antiproliferative effect of resveratrol in head and neck squamous cell carcinoma using GE11 peptide conjugated liposome. Int. J. Mol. Med. 2019, 43, 1635–1642. [Google Scholar] [CrossRef] [Green Version]
- Lee, T.H.; Kang, J.H.; Seo, J.O.; Baek, S.-H.; Moh, S.H.; Chae, J.K.; Park, Y.U.; Ko, Y.T.; Kim, S.Y. Anti-Melanogenic Potentials of Nanoparticles from Calli of Resveratrol-Enriched Rice against UVB-Induced Hyperpigmentation in Guinea Pig Skin. Biomol. Ther. 2016, 24, 85–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ravikumar, P.; Katariya, M.; Patil, S.; Tatke, P.; Pillai, R. Skin delivery of resveratrol encapsulated lipidic formulation for melanoma chemoprevention. J. Microencapsul. 2019, 36, 535–551. [Google Scholar] [CrossRef]
- Angellotti, G.; Murgia, D.; Presentato, A.; D’Oca, M.C.; Scarpaci, A.G.; Alduina, R.; Raimondi, M.V.; De Caro, V. Antibacterial PEGylated Solid Lipid Microparticles for Cosmeceutical Purpose: Formulation, Characterization, and Efficacy Evaluation. Materials 2020, 13, 2073. [Google Scholar] [CrossRef] [PubMed]
- Paczkowska-Walendowska, M.; Dvořák, J.; Rosiak, N.; Tykarska, E.; Szymańska, E.; Winnicka, K.; Ruchała, M.A.; Cielecka-Piontek, J. Buccal resveratrol delivery system as a potential new concept for the periodontitis treatment. Pharmaceutics 2021, 13, 417. [Google Scholar] [CrossRef]
- Martins, I.C.F.; Raposo, N.R.B.; Mockdeci, H.R.; Polonini, H.C.; de Oliveira Ferreira, A.; Fabri, G.M.C.; das Gracas Afonso Miranda Chaves, M. Delivering Resveratrol on the Buccal Mucosa Using Mucoadhesive Tablets: A Potential Treatment Strategy for Inflammatory Oral Lesions. Curr. Drug Deliv. 2018, 15, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Di Prima, G.; Angellotti, G.; Scarpaci, A.G.; Murgia, D.; D’agostino, F.; Campisi, G.; De Caro, V. Improvement of resveratrol permeation through sublingual mucosa: Chemical permeation enhancers versus spray drying technique to obtain fast-disintegrating sublingual mini-tablets. Pharmaceutics 2021, 13, 1370. [Google Scholar] [CrossRef]
- Di Prima, G.; Conigliaro, A.; De Caro, V. Mucoadhesive Polymeric Films to Enhance Barbaloin Penetration Into Buccal Mucosa: A Novel Approach to Chemoprevention. AAPS PharmSciTech 2019, 20, 18. [Google Scholar] [CrossRef]
- Popovici, V.; Matei, E.; Cozaru, G.C.; Bucur, L.; Gîrd, C.E.; Schröder, V.; Ozon, E.A.; Musuc, A.M.; Mitu, M.A.; Atkinson, I.; et al. In Vitro Anticancer Activity of Mucoadhesive Oral Films Loaded with Usnea barbata (L.) F. H. Wigg Dry Acetone Extract, with Potential Applications in Oral Squamous Cell Carcinoma Complementary Therapy. Antioxidants 2022, 11, 1934. [Google Scholar] [CrossRef]
- De Caro, V.; Scaturro, A.L.; Di Prima, G.; Avellone, G.; Sutera, F.M.; Di Fede, O.; Campisi, G.; Giannola, L.I. Aloin delivery on buccal mucosa: Ex vivo studies and design of a new locoregional dosing system. Drug Dev. Ind. Pharm. 2015, 41, 1541–1547. [Google Scholar] [CrossRef] [PubMed]
- Giannola, L.I.; De Caro, V.; Giandalia, G.; Gabriella Siragusa, M.; Paderni, C.; Campisi, G.; Maria Florena, A. 5-Fluorouracil buccal tablets for locoregional chemotherapy of oral squamous cell carcinoma: Formulation, drug release and histological effects on reconstituted human oral epithelium and porcine buccal mucosa. Curr. Drug Deliv. 2010, 7, 109–117. [Google Scholar] [PubMed]
- Li, W.; Tao, C.; Wang, J.; Le, Y.; Zhang, J. MMP-responsive in situ forming hydrogel loaded with doxorubicin-encapsulated biodegradable micelles for local chemotherapy of oral squamous cell carcinoma. RSC Adv. 2019, 9, 31264–31273. [Google Scholar] [CrossRef] [PubMed]

| In Vitro Concentrationsand Times | Cell Lines | Markers | Results | Reference |
|---|---|---|---|---|
| 5, 10, 25, 50, and 100 µM, for 24, 48, and 72 h | PE/CA-PJ15 | Dose-dependent cytotoxicity. Prolongation of the S phase of the cell cycle (50–100 µM). Reduction in cell migration ability (25–100 µM). | Atienzar et al. [34] | |
| From 0.1 to 1.5 μg/mL, for 48 h | SCC-VII SCC-25 YD-38 | Myt1,cdc2 proteins | Dose-dependent cytotoxicity. IC50 values: 0.5–1 μg/mL. Cell cycle interruption (48 h treatment) by the upregulation of Myt1 and the phosphorylation of cdc2. Promotion of cell apoptosis. | Yu et al. [35] |
| 25, 50, and 100 μM, for 5 h | KB | An RSV concentration of 100 μM significantly reduced cell adhesion and migration. | Shan et al. [36] | |
| 30–300 µM, for a maximum of 72 h | KB | Procaspase-3, -7, and -9, caspase-3 | IC50 values: 197.4 and 63.3 µM after 12 and 72 h treatments, respectively. Pro-apoptotic activity by internucleosomal DNA fragmentation as well as the cleavage of procaspase-3, -7, and -9, and caspase-3. | Kim et al. [37] |
| 10–500 µM, for 24, 48, and 72 h | Cal27 SCC25 SCC15 | MPP, Bax, Bak, bcl-2, bcl-XL, cytochrome c, caspase-3, caspase-9, and EMT transcription factor | IC50 values: 100 µM against Cal27 (24 h treatment), 200 µM against SCC15 (72 h treatment), and 300 µM against SCC25 (72 h treatment). Proapoptotic effect by the modulation of several factors: MMP, Bax, Bak, bcl-2 and bcl-XL, cytochrome c, and caspases. Reduction in cell migration by the inhibition of the EMT transcription factor. | Kim et al. [38] |
| 25 µM, for 1 h | YD-10B | TWIST, SLUG | Downregulation of EMT transcription factors, resulting in the reduction in the number of invading cells when compared with the positive control (LPA). | Kim et al. [39] |
| Up to 25 µM | YD-9YD-10B YD-38 | MT1-MMP, Zeb1 | Dose-dependent reduction in cell invasion. Suppression of MT1-MMP and Zeb1 expression. | Kim et al. [40] |
| 10, 20, 50, and 100 µM, for 48 h | Cal-27 | MAGEA12/Akt pathway | Dose-dependent reduction in cell viability and the MAGEA12/Akt cascade. IC50 value: 50 µM. Slightly decreased effect against cells overexpressing MAGEA12. | Shang et al. [41] |
| Coadministration with CUR at 6.2, 12.5, 25, and 50 μM, for 48 h | Cal-27 SCC-15 FaDU | Dose-dependent cytotoxicity, which was enhanced with the coadministration of the two polyphenols. | Masuelli et al. [42] | |
| 10, 20, 50, and 75 µM, for 24 h | Cisplatin-resistant Cal-27 | ERK, p-38, MMP-2, and MMP-9 | Reduced cytotoxicity in cisplatin-resistant cells. Dose-dependent antimetastatic effects. Inhibition of ERK and p-38 phosphorylation, as well as the downregulation of MMP-2 and -9 expression. | Chang et al. [43] |
| 20 μM, or 24 h | SAS Sa3 HSC-3 | EGFR ERK1/2 uPAR | Increased level of phosphorylated ERK1/2. Downregulation of integrin β1 and uPAR expression. | Uzawa et al. [44] |
| PD up to 2 mM, for 24 and 72 h | Ca9-22 Cal-27 Keratinocites | Cytochrome c, bcl-2, bax, ATG5, LC3, E-cadherin, N-cadherin, SLUG, and Snail | Dose-dependent cytotoxicity against cancer cells. Cytocompatibility against healthy cells (keratinocites) at the tested concentrations.IC50 values: 1.15 and 0.95 mM for Cal-27 and Ca9-22 cells, respectively. Proapoptotic effect via the release of cytochrome c, decrease in bcl-2 synthesis, and increase in bax expression. Autophagy induction by the stimulation of ATG5 and LC3 expression. Antimetastatic effect by increasing E-cadherin expression and the suppression of Snail and Slug proteins. | Bang et al. [45] |
| In Vivo Dose and Timing | Animal Models | Results | Reference |
|---|---|---|---|
| 2 mg of RSV, 2 mg of CUR, or 4 mg of an RSV+CUR combination per os two weeks before or simultaneously with SALTO treatment | BALB/c treated with SALTO cancer cell line | The 33% of the cases treated by the combination of RSV+CUR displayed complete cancer regression, synergic effects, and safety. | Masuelli et al. [42] |
| Intraperitoneal administration of RSV 100 mg/kg daily alone or in combination with cetuximab (10 mg/kg three times weekly) | Xenografted nude BALB/cAnNCrj-nu/nu mice | Suppression of tumor growth and downregulation of uPAR expression. Synergic effect with cetuximab due to overcoming the drug resistance phenomenon. | Uzawa et al. [44] |
| Buccal administration of 74.5 mM of RSV (ethanol solution) or cream and mouthwash containing the RSV–HPCD complex two times a week | Syrian golden hamsters treated with neoplastic agent | Chemopreventive effects leading to a reduction in OPLs. The RSV–HPCD complex mouthwash highlighted the best efficacy. | Berta et al. [53] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angellotti, G.; Di Prima, G.; Belfiore, E.; Campisi, G.; De Caro, V. Chemopreventive and Anticancer Role of Resveratrol against Oral Squamous Cell Carcinoma. Pharmaceutics 2023, 15, 275. https://doi.org/10.3390/pharmaceutics15010275
Angellotti G, Di Prima G, Belfiore E, Campisi G, De Caro V. Chemopreventive and Anticancer Role of Resveratrol against Oral Squamous Cell Carcinoma. Pharmaceutics. 2023; 15(1):275. https://doi.org/10.3390/pharmaceutics15010275
Chicago/Turabian StyleAngellotti, Giuseppe, Giulia Di Prima, Elena Belfiore, Giuseppina Campisi, and Viviana De Caro. 2023. "Chemopreventive and Anticancer Role of Resveratrol against Oral Squamous Cell Carcinoma" Pharmaceutics 15, no. 1: 275. https://doi.org/10.3390/pharmaceutics15010275
APA StyleAngellotti, G., Di Prima, G., Belfiore, E., Campisi, G., & De Caro, V. (2023). Chemopreventive and Anticancer Role of Resveratrol against Oral Squamous Cell Carcinoma. Pharmaceutics, 15(1), 275. https://doi.org/10.3390/pharmaceutics15010275










