Improving Drug Delivery on Candida Albicans Using Geraniol Nanoemulsion
Abstract
:1. Introduction
2. Materials and Methods
2.1. Nanoemulsion (NE) Preparation
2.2. Nanoemulsion Characterization
Average Hydrodynamic Diameter, Polydispersity Index, and Zeta Potential
2.3. Transmission Electron Microscopy (TEM)
2.4. Microbial Strain and Antimicrobial Solutions
2.4.1. Solutions
2.4.2. Reactivation and Preparation of C. albicans Suspension
2.4.3. Minimum Inhibitory Concentration (MIC) and Minimum Fungicidal Concentration (MFC)
2.5. Antibiofilm Evaluation
2.5.1. Human Saliva Preparation
2.5.2. Biofilm Formation and Biofilm Analyses by Colony-Forming Units (CFU)
2.5.3. Confocal Scanning Laser Microscopy (CLSM)
2.5.4. Morphological Evaluation of the Biofilm by Scanning Electron Microscopy (SEM)
2.6. Cytotoxicity Assay
2.7. Statistical Analysis
3. Results
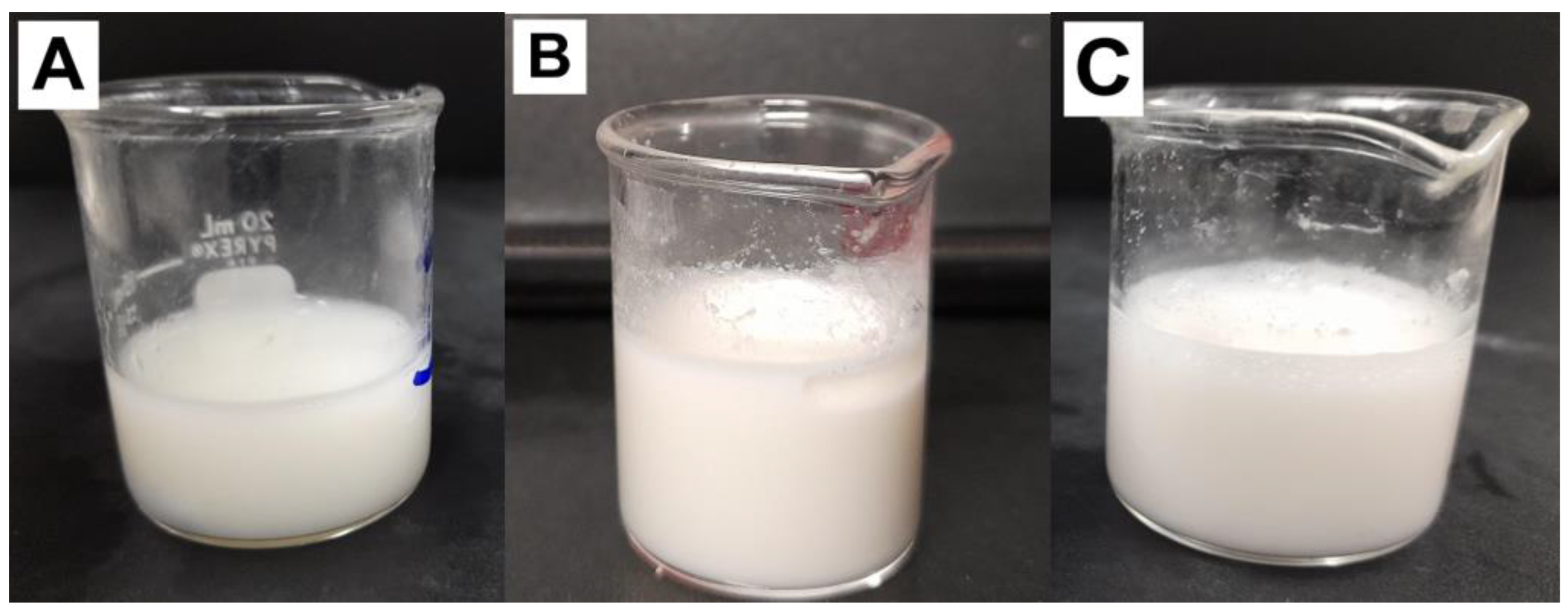
3.1. Characterization of Nanoemulsion
3.1.1. Stability of GE-NE over Six and Twelve Months after Formulation
3.1.2. Transmission Electron Microscopy (TEM)
3.2. MIC and MFC of GE and GE-NE under Planktonic Cultures of Candida albicans
3.3. Quantification of the Biofilm
3.4. Confocal Laser Scanning Microscopy (CLSM)
3.5. Scanning Electron Microscopy (SEM)
3.6. Cytotoxicity Assay
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lopes, J.P.; Lionakis, M.S. Pathogenesis and virulence of Candida albicans. Virulence 2022, 13, 89–121. [Google Scholar] [CrossRef] [PubMed]
- Armstrong-James, D.; Brown, G.D.; Netea, M.G.; Zelante, T.; Gresnigt, M.S.; van de Veerdonk, F.L.; Levitz, S.M. Immunotherapeutic approaches to treatment of fungal diseases. Lancet Infect. Dis. 2017, 17, e393–e402. [Google Scholar] [CrossRef] [PubMed]
- Nami, S.; Mohammadi, R.; Vakili, M.; Khezripour, K.; Mirzaei, H.; Morovati, H. Fungal vaccines, mechanism of actions and immunology: A comprehensive review. Biomed. Pharmacother. 2019, 109, 333–344. [Google Scholar] [CrossRef] [PubMed]
- Francisconi, R.S.; Maquera-Huacho, P.M.; Tonon, C.C.; Calixto, G.M.F.; de Cássia Orlandi Sardi, J.; Chorilli, M.; Spolidorio, D.M.P. Terpinen-4-ol and nystatin co-loaded precursor of liquid crystalline system for topical treatment of oral candidiasis. Sci. Rep. 2020, 10, 12984. [Google Scholar] [CrossRef] [PubMed]
- Ghannoum, M.; Roilides, E.; Katragkou, A.; Petraitis, V.; Walsh, T.J. The Role of Echinocandins in Candida Biofilm-Related Vascular Catheter Infections: In Vitro and In Vivo Model Systems. Clin. Infect. Dis. 2015, 61 (Suppl. S6), S618–S621. [Google Scholar] [CrossRef]
- Campoy, S.; Adrio, J.L. Antifungals. Biochem. Pharmacol. 2017, 133, 86–96. [Google Scholar] [CrossRef]
- Ajetunmobi, O.H.; Badali, H.; Romo, J.A.; Ramage, G.; Lopez-Ribot, J.L. Antifungal therapy of Candida biofilms: Past, present and future. Biofilm 2023, 23, 100126. [Google Scholar] [CrossRef]
- Lee, Y.; Puumala, E.; Robbins, N.; Cowen, L.E. Antifungal Drug Resistance: Molecular Mechanisms in Candida albicans and Beyond. Chem. Rev. 2021, 121, 3390–3411. [Google Scholar] [CrossRef]
- Gulati, M.; Nobile, C.J. Candida albicans biofilms: Development, regulation, and molecular mechanisms. Microbes. Infect. 2016, 18, 310–321. [Google Scholar] [CrossRef]
- Dimech, G.S.; Soares, L.A.; Ferreira, M.A.; de Oliveira, A.G.; Carvalho Mda, C.; Ximenes, E.A. Phytochemical and antibacterial investigations of the extracts and fractions from the stem bark of Hymenaea stigonocarpa Mart. ex Hayne and effect on ultrastructure of Staphylococcus aureus induced by hydroalcoholic extract. Sci. World J. 2013, 2013, 862763. [Google Scholar] [CrossRef]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos EV, R.; Rodriguez-Torres MD, P.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018, 16, 71. [Google Scholar] [CrossRef] [PubMed]
- Govindarajan, M.; Rajeswary, M.; Arivoli, S.; Tennyson, S.; Benelli, G. Larvicidal and repellent potential of Zingiber nimmonii (J. Graham) Dalzell (Zingiberaceae) essential oil: An eco-friendly tool against malaria, dengue, and lymphatic filariasis mosquito vectors? Parasitol. Res. 2016, 115, 1807–1816. [Google Scholar] [CrossRef] [PubMed]
- Baveloni, F.G.; Riccio, B.V.F.; Di Filippo, L.D.; Fernandes, M.A.; Meneguin, A.B.; Chorilli, M. Nanotechnology-based Drug Delivery Systems as Potential for Skin Application: A Review. Curr. Med. Chem. 2021, 28, 3216–3248. [Google Scholar] [CrossRef] [PubMed]
- Plaza-Oliver, M.; Santander-Ortega, M.J.; Lozano, M.V. Current approaches in lipid-based nanocarriers for oral drug delivery. Drug Deliv. Transl. Res. 2021, 11, 471–497. [Google Scholar] [CrossRef] [PubMed]
- Ceci, C.; Graziani, G.; Faraoni, I.; Cacciotti, I. Strategies to improve ellagic acid bioavailability: From natural or semisynthetic derivatives to nanotechnological approaches based on innovative carriers. Nanotechnology 2020, 31, 382001. [Google Scholar] [CrossRef]
- Rehman, A.; Tong, Q.; Jafari, S.M.; Korma, S.A.; Khan, I.M.; Mohsin, A.; Manzoor, M.F.; Ashraf, W.; Mushtaq, B.S.; Zainab, S.; et al. Spray dried nanoemulsions loaded with curcumin, resveratrol, and borage seed oil: The role of two different modified starches as encapsulating materials. Int. J. Biol. Macromol. 2021, 1, 820–828. [Google Scholar] [CrossRef]
- Rehman, A.; Tong, Q.; Korma, S.A.; Han, W.; Karim, A.; Sharif, H.R.; Ali, A.; Yaqoob, S.; Khalifa, S.A.; Cacciotti, I. Influence of diverse natural biopolymers on the physicochemical characteristics of borage seed oil-peppermint oil loaded W/O/W nanoemulsions entrapped with lycopene. Nanotechnology 2021, 32, 505302. [Google Scholar] [CrossRef]
- Majeed, U.; Shafi, A.; Shahbaz, M.; Khan, K.u.R.; Iqbal, K.J.; Akram, K.; Baboo, I.; Munawar, S.H.; Munir, M.M.; Sultan, R.; et al. Assessment of Growth Inhibition of Eugenol-Loaded Nano-Emulsions against Beneficial Bifidobacterium sp. along with Resistant Escherichia coli Using Flow Cytometry. Fermentation 2023, 9, 140. [Google Scholar] [CrossRef]
- Akombaetwa, N.; Ilangala, A.B.; Thom, L.; Memvanga, P.B.; Witika, B.A.; Buya, A.B. Current Advances in Lipid Nanosystems Intended for Topical and Transdermal Drug Delivery Applications. Pharmaceutics 2023, 15, 656. [Google Scholar] [CrossRef]
- Yukuyama, M.N.; Kato, E.T.; Lobenberg, R.; Bou-Chacra, N.A. Challenges and Future Prospects of Nanoemulsion as a Drug Delivery System. Curr. Pharm. Des. 2017, 23, 495–508. [Google Scholar] [CrossRef]
- Souto, E.B.; Cano, A.; Martins-Gomes, C.; Coutinho, T.E.; Zielińska, A.; Silva, A.M. Microemulsions and Nanoemulsions in Skin Drug Delivery. Bioengineering 2022, 9, 158. [Google Scholar] [CrossRef] [PubMed]
- Hagvall, L.; Backtorp, C.; Svensson, S.; Nyman, G.; Borje, A.; Karlberg, A.T. Fragrance compound geraniol forms contact allergens on air exposure. Identification and quantification of oxidation products and effect on skin sensitization. Chem. Res. Toxicol. 2007, 20, 807–814. [Google Scholar] [CrossRef] [PubMed]
- Queiroz, T.B.; Santos, G.F.; Ventura, S.C.; Hiruma-Lima, C.A.; Gaivao, I.O.M.; Maistro, E.L. Cytotoxic and genotoxic potential of geraniol in peripheral blood mononuclear cells and human hepatoma cell line (HepG2). Genet. Mol. Res. 2017, 16, gmr16039777. [Google Scholar] [CrossRef] [PubMed]
- Formariz, T.P.; Chiavacci, L.A.; Scarpa, M.V.; Silva-Júnior, A.D.; Egito ES, T.; Terrugi, C.H.; Franzini, C.M.; Sarmento, V.H.V.; Oliveira, A.G. Structure and viscoelastic behavior of pharmaceutical biocompatible anionic microemulsions containing the antitumoral drug compound doxorubicin. Colloids Surf. Biointerfaces 2010, 77, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Bonifácio, B.V.; Ramos, M.A.; da Silva, P.B.; Negri, K.M.; de Oliveira Lopes, É.; de Souza, L.P.; Vilegas, W.; Pavan, F.R.; Chorilli, M.; Bauab, T.M. Nanostructured lipid system as a strategy to improve the anti-Candida albicans activity of Astronium sp. Int. J. Nanomed. 2015, 10, 5081–5092. [Google Scholar] [CrossRef]
- Agnish, S.; Sharma, A.D.; Kaur, I. Nanoemulsions (O/W) containing Cymbopogon pendulus essential oil: Development, characterization, stability study, and evaluation of in vitro anti-bacterial, anti-inflammatory, anti-diabetic activities. Bionanoscience 2022, 1, 15. [Google Scholar] [CrossRef]
- de Carvalho Bernardo, W.L.; Boriollo, M.F.G.; Tonon, C.C.; da Silva, J.J.; Cruz, F.M.; Martins, A.L.; Höfling, J.F.; Spolidorio, D.M.P. Antimicrobial effects of silver nanoparticles and extracts of Syzygium cumini flowers and seeds: Periodontal, cariogenic and opportunistic pathogens. Arch. Oral. Biol. 2021, 125, 105101. [Google Scholar] [CrossRef]
- Carvalho, G.G.; Maquera-Huacho, P.M.; Pontes, C.S.; Annunzio, S.R.; Mendonça, C.R.F.; Rastelli, A.N.S.; de Oliveira, K.T.; Teughels, W.; Chorilli, M.; Leal, D.Z.; et al. Chlorin-e6 conjugated to the antimicrobial peptide LL-37 loaded nanoemulsion enhances photodynamic therapy against multi-species biofilms related to periodontitis. Photodiagnosis Photodyn. Ther. 2023, 43, 103725. [Google Scholar] [CrossRef]
- Leite, M.C.; de Brito Bezerra, A.P.; de Sousa, J.P.; de Oliveira Lima, E. Investigating the antifungal activity and mechanism(s) of geraniol against Candida albicans strains. Med. Mycol. 2015, 53, 275–284. [Google Scholar] [CrossRef]
- CLSI. Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts, 4th ed.; CLSI standard M27; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2017. [Google Scholar]
- Minhaco, V.M.T.R.; Maquera Huacho, P.M.; Mancim Imbriani, M.J.; Tonon, C.C.; Chorilli, M.; Rastelli, A.N.S.; Spolidorio, D.M.P. Improving antimicrobial activity against endodontic biofilm after exposure to blue light-activated novel curcumin nanoparticle. Photodiagnosis Photodyn. Ther. 2023, 42, 103322. [Google Scholar] [CrossRef]
- Thein, Z.M.; Samaranayake, Y.H.; Samaranayake, L.P. In vitro biofilm formation of Candida albicans and non-albicans Candida species under dynamic and anaerobic conditions. Arch. Oral. Biol. 2007, 52, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Sardi, J.C.; Freires, I.A.; Lazarini, J.G.; Infante, J.; de Alencar, S.M.; Rosalen, P.L. Unexplored endemic fruit species from Brazil: Antibiofilm properties, insights into mode of action, and systemic toxicity of four Eugenia spp. Microb. Pathog. 2017, 105, 280–287. [Google Scholar] [CrossRef] [PubMed]
- ISO 10993-5; Biological Evaluation of Medical Devices. Part 5: Tests for In Vitro Cytotoxicity. International Organization for Standardization: Geneva, Switzerland, 2009; ISO Store Order #: 10-1034100 (Date: 8 May 2009). Available online: http://www.iso.org/iso/home.html (accessed on 15 April 2023).
- Sarker, D. Engineering of nanoemulsions for drug delivery. Curr. Drug Deliv. 2005, 2, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Eral, H.; Hatton, T.; Doyle, P. Nanoemulsions: Formation, properties and applications. Soft Matter. 2016, 12, 2826–2841. [Google Scholar] [CrossRef] [PubMed]
- Prasad, P.; Tippana, M. Morphogenic plasticity: The pathogenic attribute of Candida albicans. Curr. Genet. 2023, 69, 77–89. [Google Scholar] [CrossRef]
- Howe, A.M.; Pitt, A.R. Rheology and stability of oil-in-water nanoemulsions stabilised by anionic surfactant and gelatin 1) addition of nonionic, cationic and ethoxylated-cationic co-surfactants. Adv. Colloid. Interface Sci. 2008, 144, 24–29. [Google Scholar] [CrossRef]
- Páez-Hernández, G.; Mondragón-Cortez, P.; Espinosa-Andrews, H. Developing curcumin nanoemulsions by high-intensity methods: Impact of ultrasonication and microfluidization parameters. LWT 2019, 111, 291–300. [Google Scholar] [CrossRef]
- Strickley, R.G. Solubilizing excipients in oral and injectable formulations. Pharm. Res. 2004, 21, 201–230. [Google Scholar] [CrossRef]
- Yue, L.; Yan, Z.; Li, H.; Liu, X.; Sun, P. Brij-58, a potential injectable protein-stabilizer used in therapeutic protein formulation. Eur. J. Pharm. Biopharm. 2020, 146, 73–83. [Google Scholar] [CrossRef]
- Mitra, R.K.; Paul, B.K.; Moulik, S.P. Phase behavior, interfacial composition and thermodynamic properties of mixed surfactant (CTAB and Brij-58) derived w/o microemulsions with 1-butanol and 1-pentanol as cosurfactants and n-heptane and n-decane as oils. J. Colloid. Interface Sci. 2006, 300, 755–764. [Google Scholar] [CrossRef]
- Katz, J.S.; Chou, D.K.; Christian, T.R.; Das, T.K.; Patel, M.; Singh, S.N.; Wen, Y. Emerging Challenges and Innovations in Surfactant-mediated Stabilization of Biologic Formulations. J. Pharm. Sci. 2022, 111, 919–932. [Google Scholar] [CrossRef] [PubMed]
- Volkering, F.; Breure, A.M.; van Andel, J.G.; Rulkens, W.H. Influence of nonionic surfactants on bioavailability and biodegradation of polycyclic aromatic hydrocarbons. Appl. Environ. Microbiol. 1995, 61, 1699–1705. [Google Scholar] [CrossRef] [PubMed]
- Jantrawut, P.; Boonsermsukcharoen, K.; Thipnan, K.; Chaiwarit, T.; Hwang, K.-M.; Park, E.-S. Enhancement of Antibacterial Activity of Orange Oil in Pectin Thin Film by Microemulsion. Nanomaterials 2018, 8, 545. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Bishnoi, R.S.; Shukla, A.K.; Jain, C.P. Techniques for Formulation of Nanoemulsion Drug Delivery System: A Review. Prev. Nutr. Food Sci. 2019, 24, 225–234. [Google Scholar] [CrossRef]
- Zorzi, G.K.; Caregnato, F.; Moreira, J.C.; Teixeira, H.F.; Carvalho, E.L. Antioxidant Effect of Nanoemulsions Containing Extract of Achyrocline satureioides (Lam) D.C.-Asteraceae. AAPS Pharm. Sci. Technol. 2016, 17, 844–850. [Google Scholar] [CrossRef]
- Dos Santos Ramos, M.A.; da Silva, P.B.; de Toledo, L.G.; Oda, F.B.; da Silva, I.C.; Dos Santos, L.C.; Dos Santos, A.G.; de Almeida, M.T.G.; Pavan, F.R.; Chorilli, M.; et al. Intravaginal Delivery of Syngonanthus nitens (Bong.) Ruhland Fraction Based on a Nanoemulsion System Applied to Vulvovaginal Candidiasis Treatment. J. Biomedical. Nanotechnol. 2019, 15, 1072–1089. [Google Scholar] [CrossRef]
- Michels, L.R.; Maciel, T.R.; Nakama, K.A.; Teixeira, F.E.G.; de Carvalho, F.B.; Gundel, A.; de Araujo, B.V.; Haas, S.E. Effects of Surface Characteristics of Polymeric Nanocapsules on the Pharmacokinetics and Efficacy of Antimalarial Quinine. Int. J. Nanomed. 2019, 14, 10165–10178. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, L.; Liu, Y.; Zeng, Z.; Li, C.; Fang, Z.; Hu, B.; Chen, H.; Wang, C.; Chen, S.; et al. Effect of hydroxypropyl-β-cyclodextrin and lecithin co-stabilized nanoemulsions on the konjac glucomannan/pullulan film. Int. J. Biol. Macromol. 2023, 235, 123802. [Google Scholar] [CrossRef]
- Chavda, H. In-use stability studies: Guidelines and challenges. Drug Dev. Ind. Pharm. 2021, 47, 1373–1391. [Google Scholar] [CrossRef]
- Aligiannis, N.; Kalpoutzakis, E.; Mitaku, S.; Chinou, I. Composition and antimicrobial activity of the essential oils of two Origanum species. J. Agric. Food Chem. 2001, 49, 4168–4170. [Google Scholar] [CrossRef]
- Duarte, M.C.; Figueira, G.M.; Sartoratto, A.; Rehder, V.L.; Delarmelina, C. Anti-Candida activity of Brazilian medicinal plants. J. Ethnopharmacol. 2005, 97, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Sartoratto, A.; Machado, A.L.M.; Delarmelina, C.; Figueira, G.M.; Duarte, M.C.T.; Rehder, V.L.G. Composition and antimicrobial activity of essential oils from aromatic plants used in Brazil. Braz. J. Microbiol. 2004, 35, 275–280. [Google Scholar] [CrossRef]
- Marcos-Arias, C.; Eraso, E.; Madariaga, L.; Quindos, G. In vitro activities of natural products against oral Candida isolates from denture wearers. BMC Complement. Altern. Med. 2011, 11, 119. [Google Scholar] [CrossRef] [PubMed]
- Zore, G.B.; Thakre, A.D.; Rathod, V.; Karuppayil, S.M. Evaluation of anti-Candida potential of geranium oil constituents against clinical isolates of Candida albicans differentially sensitive to fluconazole: Inhibition of growth, dimorphism and sensitization. Mycoses 2011, 54, e99–e109. [Google Scholar] [CrossRef]
- Sharma, Y.; Khan, L.A.; Manzoor, N. Anti-Candida activity of geraniol involves disruption of cell membrane integrity and function. J. Mycol. Med. 2016, 26, 244–254. [Google Scholar] [CrossRef]
- Cunha Júnior, A.S.C.; Fialho, S.L.; Carneiro, L.B.; Orefice, F. Microemulsions as drug delivery systems for topical ocular administration. Arq. Bras. Oftalmol. 2003, 66, 385–391. [Google Scholar] [CrossRef]
- Rai, V.; Tan, H.S.; Michniak-Kohn, B. Effect of surfactants and pH on naltrexone (NTX) permeation across buccal mucosa. Int. J. Pharm. 2011, 411, 92–97. [Google Scholar] [CrossRef]
- Buyukozturk, F.; Benneyan, J.C.; Carrier, R.L. Impact of emulsion-based drug delivery systems on intestinal permeability and drug release kinetics. J. Control. Release 2010, 142, 22–30. [Google Scholar] [CrossRef]
- Hafidh, R.R.; Abdulamir, A.S.; Vern, L.S.; Abu Bakar, F.; Abas, F.; Jahanshiri, F.; Sekawi, Z. Inhibition of growth of highly resistant bacterial and fungal pathogens by a natural product. Open Microbiol. J. 2011, 5, 96–106. [Google Scholar] [CrossRef]
- Trindade, L.; de Araújo Oliveira, J.; de Castro, R.; de Oliveira Lima, E. Inhibition of adherence of C. albicans to dental implants and cover screws by Cymbopogon nardus essential oil and citronellal. Clin. Oral. Inv. 2015, 19, 2223–2231. [Google Scholar] [CrossRef]
- Monk, B.C.; Goffeau, A. Outwitting multidrug resistance to antifungals. Science 2008, 321, 367–369. [Google Scholar] [CrossRef]
- Brilhante, R.S.N.; de Lima, R.A.C.; Marques, F.J.F.; Silva, N.F.; Caetano, É.P.; Castelo-Branco, D.S.C.M.; Bandeira, T.J.P.G.; Moreira, J.L.B.; Cordeiro, R.A.; Monteiro, A.J.; et al. Histoplasma capsulatum in planktonic and biofilm forms: In vitro susceptibility to amphotericin B, itraconazole and farnesol. J. Med. Microbiol. 2015, 64 Pt 4, 394–399. [Google Scholar] [CrossRef] [PubMed]
- Sardi, C.J.; Pitangui, N.S.; Rodriguez-Arellanes, G.; Taylor, M.L.; Fusco-Almeida, A.M.; Mendes-Giannini, M.J. Highlights in pathogenic fungal biofilms. Rev. Iberoam. Micol. 2014, 31, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Rangel, M.L.; de Aquino, S.G.; de Lima, J.M.; Castellano, L.R.; de Castro, R.D. In Vitro Effect of Cinnamomum zeylanicum Blume Essential Oil on Candida spp. Involved in Oral Infections. Evid. Based Complement. Alternat. Med. 2018, 2018, 4045013. [Google Scholar] [CrossRef] [PubMed]
- Lopes, G.; Pinto, E.; Andrade, P.B.; Valentao, P. Antifungal activity of phlorotannins against dermatophytes and yeasts: Approaches to the mechanism of action and influence on Candida albicans virulence factor. PloS ONE 2013, 8, e72203. [Google Scholar] [CrossRef]
- Lei, Y.; Fu, P.; Jun, X.; Cheng, P. Pharmacological Properties of Geraniol—A Review. Planta Med. 2019, 85, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Fatima, Z.; Hameed, S. Insights into the mode of action of anticandidal herbal monoterpenoid geraniol reveal disruption of multiple MDR mechanisms and virulence attributes in Candida albicans. Arch. Microbiol. 2016, 198, 459–472. [Google Scholar] [CrossRef]
- Ahmad, A.; Khan, A.; Yousuf, S.; Khan, L.A.; Manzoor, N. Proton translocating ATPase mediated fungicidal activity of eugenol and thymol. Fitoterapia 2010, 81, 1157–1162. [Google Scholar] [CrossRef]
- Cimino, C.; Maurel, O.M.; Musumeci, T.; Bonaccorso, A.; Drago, F.; Souto, E.M.B.; Pignatello, R.; Carbone, C. Essential Oils: Pharmaceutical Applications and Encapsulation Strategies into Lipid-Based Delivery Systems. Pharmaceutics 2021, 13, 327. [Google Scholar] [CrossRef]
- Nee, T.W.; Ring, L.C.; Arumugam, V.; Yee, J.L.C.; Hin, L.W.; Yusof, F.A.M.; MAM Noor, M.A.; Yenn, T.W. Sustained Release Geraniol Nanoparticles Inhibit Human Axillary Odor-Causing Bacteria. Arab. J. Sci. Eng. 2018, 44, 103–109. [Google Scholar] [CrossRef]
- Donsì, F.; Ferrari, G. Essential oil nanoemulsions as antimicrobial agents in food. J. Biotechnol. 2016, 233, 106–120. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, V.G.; Thuy, V.N.; Van, T.V.; Dao, A.H.; Lee, B. Nanostructured lipid carriers and their potential applications for versatile drug delivery via oral administration. OpenNano 2022, 8, 100064. [Google Scholar] [CrossRef]
- Pinilla, C.M.B.; Lopes, N.A.; Brandelli, A. Lipid-Based Nanostructures for the Delivery of Natural Antimicrobials. Molecules 2021, 26, 3587. [Google Scholar] [CrossRef] [PubMed]







| Formulation | Particle Size (nm) | Polydispersity Index (PDI) | Zeta Potential (mV) |
|---|---|---|---|
| NE | 150.8 ± 70.4 | 0.450 | −6.35 |
| GE-NE | 232.3 ± 122.5 | 0.155 | −4.60 |
| C. albicans | |||
|---|---|---|---|
| MIC | MFC | Nature | |
| GE | 300 μg/mL | 600 μg/mL | Fungicide * |
| GE-NE | 18.75 μg/mL | 37.5 μg/mL | Fungicide * |
| Nistatina | 4 μg/mL | 8 μg/mL | Fungicide * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva Pontes, C.; Garcia de Carvalho, G.; Rosa Perin Leite, A.; Chorilli, M.; Palomari Spolidorio, D.M. Improving Drug Delivery on Candida Albicans Using Geraniol Nanoemulsion. Pharmaceutics 2023, 15, 2475. https://doi.org/10.3390/pharmaceutics15102475
Silva Pontes C, Garcia de Carvalho G, Rosa Perin Leite A, Chorilli M, Palomari Spolidorio DM. Improving Drug Delivery on Candida Albicans Using Geraniol Nanoemulsion. Pharmaceutics. 2023; 15(10):2475. https://doi.org/10.3390/pharmaceutics15102475
Chicago/Turabian StyleSilva Pontes, Cristiano, Gabriel Garcia de Carvalho, Andressa Rosa Perin Leite, Marlus Chorilli, and Denise Madalena Palomari Spolidorio. 2023. "Improving Drug Delivery on Candida Albicans Using Geraniol Nanoemulsion" Pharmaceutics 15, no. 10: 2475. https://doi.org/10.3390/pharmaceutics15102475
APA StyleSilva Pontes, C., Garcia de Carvalho, G., Rosa Perin Leite, A., Chorilli, M., & Palomari Spolidorio, D. M. (2023). Improving Drug Delivery on Candida Albicans Using Geraniol Nanoemulsion. Pharmaceutics, 15(10), 2475. https://doi.org/10.3390/pharmaceutics15102475







