The Complexity of Bariatric Patient’s Pharmacotherapy: Sildenafil Biopharmaceutics and Pharmacokinetics before vs. after Gastric Sleeve/Bypass
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. In Vitro Solubility
2.3. Ex Vivo Solubility
2.4. In Vitro Dissolution
2.5. Analytical Method
2.6. Physiologically Based Pharmacokinetic (PBPK) Modeling
| Value | Source/Ref | |
|---|---|---|
| Molecular weight (g/mol) | 474.59 | / |
| LogP/LogD | 2.7 (pH 7.4) | [46] |
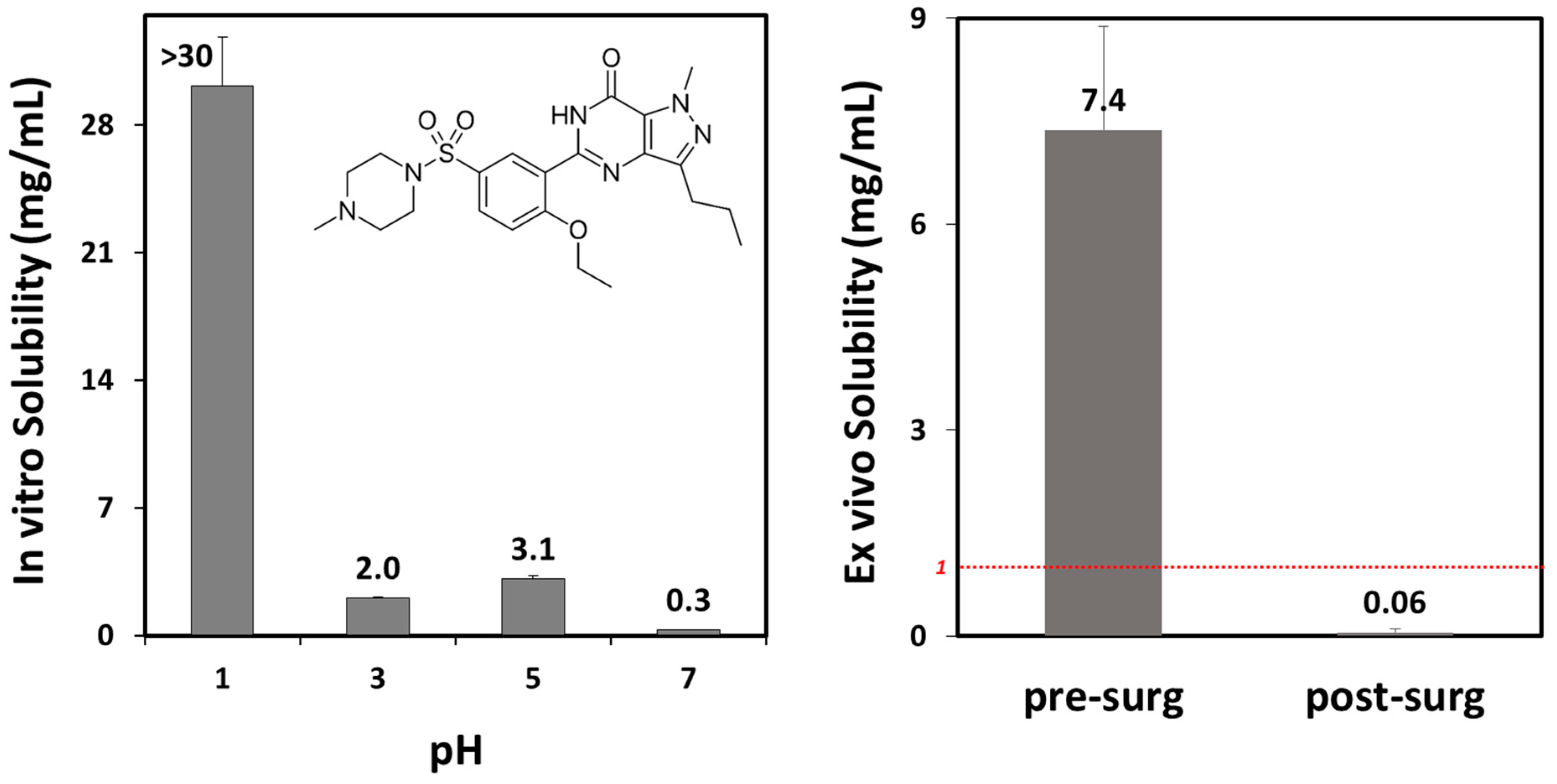
| Solubility at 37 °C (mg/mL) | 30 (pH 1); 2 (pH 3); 3.1 (pH 5); 0.3 (pH 7) | Experimental |
| pKa(s) | 1.72 (base); 6.03 (base); 8.74 (acid) | predicted using ADMET Predictor® module, then fitted (software integrated option) to the experimental pH solubility profile |
| Human effective permeability, Peff (cm/s) | 4.48 × 10−4 | [47] |
| Diffusion coefficient (cm2/s) | 0.6006 × 10−5 | software calculated (based on drug molecular weight) |
| Particle diameter (µm) | 100 | Approximated |
| Mean precipitation time (s) | 900 | software default |
| Drug dose (mg) (dosage form) | 20 a, 25, 100 (tablet); 50 (tablet, capsule a) | / |
| Volume of fluid taken with drug (mL) | 250 (presurgery); 50 (postsurgery) | software default or decreased by 80% to comply with the smaller gastric volume [35] and limited volume of fluid the bariatric patient can ingest |
| Blood/plasma concentration ratio | 0.81 | predicted using ADMET Predictor® module |
| Plasma fraction unbound (%) | 4 | [46,48] |
| First pass effect, FPE (%) | 60 | optimized to comply with the literature’s reported values [46,49,50] |
| Clearance, CL (L/h/kg) | 0.556 | estimated using PKPlusTM module, based on the in vivo data for i.v. drug dose [42]; comply with the reported data [41] |
| Volume of distribution, Vd (L/kg) | 1.112 | |
| Distribution constant k12 (1/h) | 0.049 | |
| Distribution constant k21 (1/h) | 0.292 | |
| Elimination half life, t1/2 (h) | 2.83 | software calculated; complies with the reported data [46,49] |
3. Results
3.1. Sildenafil Solubility
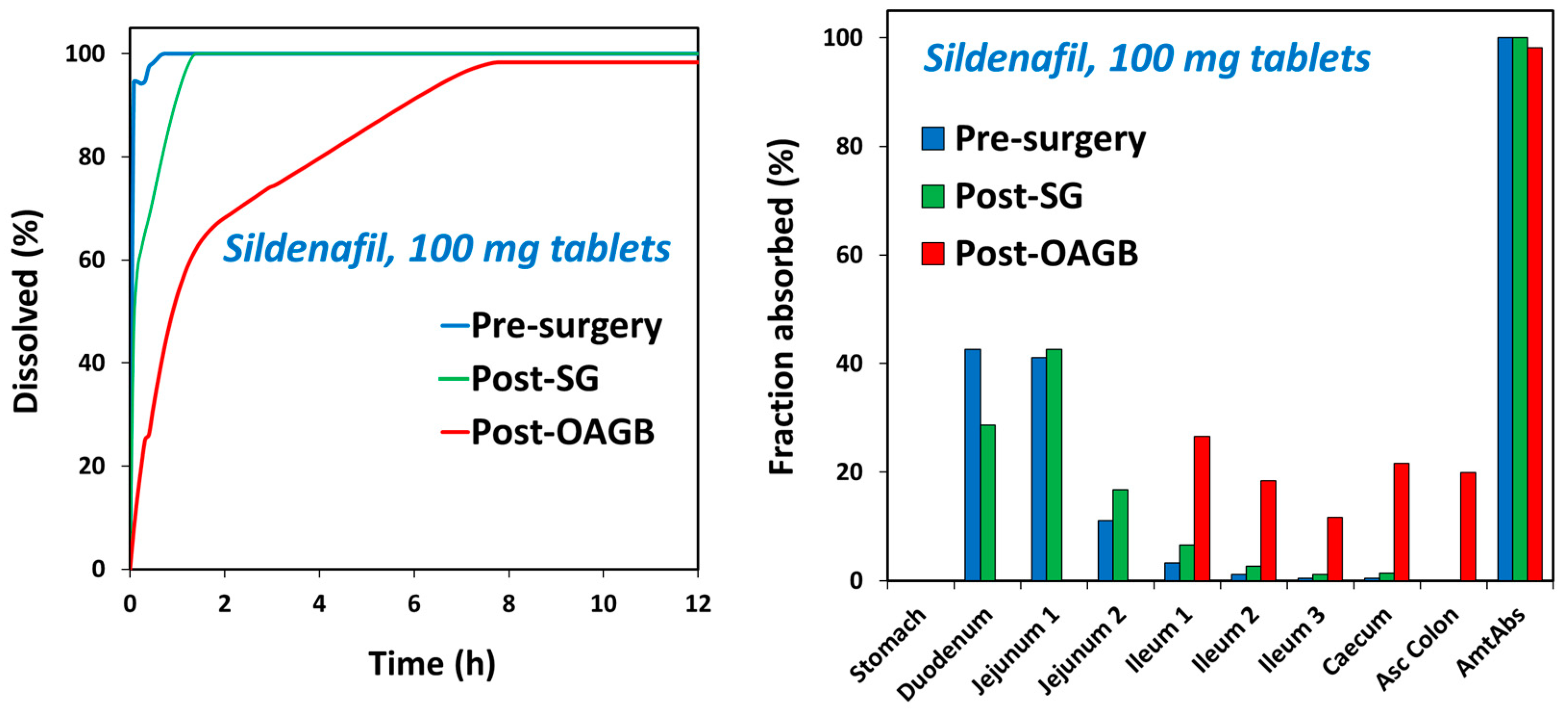
3.2. In Vitro Dissolution
3.3. Physiologically Based Pharmacokinetic (PBPK) Simulations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chitaley, K.; Kupelian, V.; Subak, L.; Wessells, H. Diabetes, obesity and erectile dysfunction: Field overview and research priorities. J. Urol. 2009, 182, S45–S50. [Google Scholar] [CrossRef] [PubMed]
- Akdemir, A.O.; Karabakan, M.; Aktas, B.K.; Bozkurt, A.; Ozgur, E.G.; Akdogan, N.; Yaris, M. Visceral adiposity index is useful for evaluating obesity effect on erectile dysfunction. Andrologia 2019, 51, e13282. [Google Scholar] [CrossRef] [PubMed]
- Minambres, I.; Sarda, H.; Urgell, E.; Genua, I.; Ramos, A.; Fernandez-Ananin, S.; Balague, C.; Sanchez-Quesada, J.L.; Bassas, L.; Perez, A. Obesity Surgery Improves Hypogonadism and Sexual Function in Men without Effects in Sperm Quality. J. Clin. Med. 2022, 11, 5126. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Sun, L.; Jiang, S.; Chen, X.; Zhu, J.; Zhao, X.; Yu, S.; Dong, Z.; Chen, Y.; Zhang, W.; et al. Effects of bariatric surgery on testosterone level and sexual function in men with obesity: A retrospective study. Front. Endocrinol. 2022, 13, 1036243. [Google Scholar] [CrossRef] [PubMed]
- El-Tholoth, H.S.; Bedaiwi, A.K.; Binjawhar, A.; Almulhem, A.A.; Bedaiwi, K.K.; Alshurafa, H.; Alzahrani, T.; Alhussein, R.K.; Alhussein, A.K.; Alnumi, M. Male sexual function after weight-loss surgeries in a group of Saudi population. Urol. Ann. 2021, 13, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Machado, F.P.; Rhoden, E.L.; Pioner, S.R.; Halmenschlager, G.; de Souza, L.V.B.; Lisot, B.C.; Drachler, I.P. Weight Loss Through Bariatric Surgery in Men Presents Beneficial Effects on Sexual Function, Symptoms of Testosterone Deficiency, and Hormonal Profile. Sex. Med. 2021, 9, 100400. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Xu, W.; Wang, T.; Wang, S.; Liu, J.; Jiang, H. Effect of weight loss on erectile function in men with overweight or obesity: A meta-analysis of randomised controlled trials. Andrologia 2022, 54, e14250. [Google Scholar] [CrossRef]
- Mora, M.; Aranda, G.B.; de Hollanda, A.; Flores, L.; Puig-Domingo, M.; Vidal, J. Weight loss is a major contributor to improved sexual function after bariatric surgery. Surg. Endosc. 2013, 27, 3197–3204. [Google Scholar] [CrossRef]
- Fahmy, A.; Abdeldaiem, H.; Abdelsattar, M.; Aboyoussif, T.; Assem, A.; Zahran, A.; Elgebaly, O. Impact of Bariatric Surgery on Sexual Dysfunction in Obese Men. Sex. Med. 2021, 9, 100322. [Google Scholar] [CrossRef]
- Nimbi, F.M.; Virginia, C.; Cinzia, D.M.; Michela, D.T.; Gianfranco, S.; Emanuela, P. The relation between sexuality and obesity: The role of psychological factors in a sample of obese men undergoing bariatric surgery. Int. J. Impot. Res. 2022, 34, 203–214. [Google Scholar] [CrossRef]
- Wang, C.M.; Wu, B.R.; Xiang, P.; Xiao, J.; Hu, X.C. Management of male erectile dysfunction: From the past to the future. Front. Endocrinol. 2023, 14, 1148834. [Google Scholar] [CrossRef] [PubMed]
- Mykoniatis, I.; Pyrgidis, N.; Sokolakis, I.; Ouranidis, A.; Sountoulides, P.; Haidich, A.B.; van Renterghem, K.; Hatzichristodoulou, G.; Hatzichristou, D. Assessment of Combination Therapies vs Monotherapy for Erectile Dysfunction: A Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2036337. [Google Scholar] [CrossRef] [PubMed]
- Moncada, I.; Martinez-Salamanca, J.; Ruiz-Castane, E.; Romero, J. Combination therapy for erectile dysfunction involving a PDE5 inhibitor and alprostadil. Int. J. Impot. Res. 2018, 30, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Dahan, A.; Beig, A.; Lindley, D.; Miller, J.M. The solubility-permeability interplay and oral drug formulation design: Two heads are better than one. Adv. Drug Deliv. Rev. 2016, 101, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Martinez, M.N.; Amidon, G.L. A mechanistic approach to understanding the factors affecting drug absorption: A review of fundamentals. J. Clin. Pharmacol. 2002, 42, 620–643. [Google Scholar] [CrossRef]
- Porat, D.; Vaynshtein, J.; Gibori, R.; Avramoff, O.; Shaked, G.; Dukhno, O.; Czeiger, D.; Sebbag, G.; Dahan, A. Stomach pH before vs. after different bariatric surgery procedures: Clinical implications for drug delivery. Eur. J. Pharm. Biopharm. 2021, 160, 152–157. [Google Scholar] [CrossRef]
- Steenackers, N.; Vanuytsel, T.; Augustijns, P.; Tack, J.; Mertens, A.; Lannoo, M.; Van der Schueren, B.; Matthys, C. Adaptations in gastrointestinal physiology after sleeve gastrectomy and Roux-en-Y gastric bypass. Lancet Gastroenterol. Hepatol. 2021, 6, 225–237. [Google Scholar] [CrossRef]
- Azran, C.; Wolk, O.; Zur, M.; Fine-Shamir, N.; Shaked, G.; Czeiger, D.; Sebbag, G.; Kister, O.; Langguth, P.; Dahan, A. Oral drug therapy following bariatric surgery: An overview of fundamentals, literature and clinical recommendations. Obes. Rev. 2016, 17, 1050–1066. [Google Scholar] [CrossRef]
- Porat, D.; Dahan, A. Medication Management after Bariatric Surgery: Providing Optimal Patient Care. J. Clin. Med. 2020, 9, 1511. [Google Scholar] [CrossRef]
- Porat, D.; Dukhno, O.; Vainer, E.; Cvijic, S.; Dahan, A. Antiallergic Treatment of Bariatric Patients: Potentially Hampered Solubility/Dissolution and Bioavailability of Loratadine, but Not Desloratadine, Post-Bariatric Surgery. Mol. Pharm. 2022, 19, 2922–2936. [Google Scholar] [CrossRef]
- Porat, D.; Azran, C.; Mualem, Y.; Vainer, E.; Gibori, R.; Vaynshtein, J.; Dukhno, O.; Dahan, A. Lamotrigine therapy in patients after bariatric surgery: Potentially hampered solubility and dissolution. Int. J. Pharm. 2022, 612, 121298. [Google Scholar] [CrossRef] [PubMed]
- Zucchi, A.; Costantini, E.; Scroppo, F.I.; Silvani, M.; Kopa, Z.; Illiano, E.; Petrillo, M.G.; Cari, L.; Nocentini, G. The first-generation phosphodiesterase 5 inhibitors and their pharmacokinetic issue. Andrology 2019, 7, 804–817. [Google Scholar] [CrossRef] [PubMed]
- Beig, A.; Miller, J.M.; Dahan, A. The interaction of nifedipine with selected cyclodextrins and the subsequent solubility-permeability trade-off. Eur. J. Pharm. Biopharm. 2013, 85, 1293–1299. [Google Scholar] [CrossRef] [PubMed]
- Beig, A.; Agbaria, R.; Dahan, A. The use of captisol (SBE7-beta-CD) in oral solubility-enabling formulations: Comparison to HPbetaCD and the solubility-permeability interplay. Eur. J. Pharm. Sci. 2015, 77, 73–78. [Google Scholar] [CrossRef]
- Fassihi, A.R.; Munday, D.L. Dissolution of theophylline from film-coated slow release mini-tablets in various dissolution media. J. Pharm. Pharmacol. 1989, 41, 369–372. [Google Scholar] [CrossRef]
- Silva, O.S.; Souza, C.R.; Oliveira, W.P.; Rocha, S.C. In vitro dissolution studies of sodium diclofenac granules coated with Eudragit L-30D-55 by fluidized-bed system. Drug Dev. Ind. Pharm. 2006, 32, 661–667. [Google Scholar] [CrossRef]
- Sugano, K. Biopharmaceutics Modeling and Simulations: Theory, Practice, Methods, and Applications; Wiley: Hoboken, NJ, USA, 2012. [Google Scholar]
- Beig, A.; Dahan, A. Quantification of carbamazepine and its 10,11-epoxide metabolite in rat plasma by UPLC-UV and application to pharmacokinetic study. Biomed. Chromatogr. 2014, 28, 934–938. [Google Scholar] [CrossRef]
- Agoram, B.; Woltosz, W.S.; Bolger, M.B. Predicting the impact of physiological and biochemical processes on oral drug bioavailability. Adv. Drug Deliv. Rev. 2001, 50 (Suppl. 1), S41–S67. [Google Scholar] [CrossRef]
- Lin, L.; Wong, H. Predicting Oral Drug Absorption: Mini Review on Physiologically-Based Pharmacokinetic Models. Pharmaceutics 2017, 9, 41. [Google Scholar] [CrossRef]
- Jereb, R.; Opara, J.; Bajc, A.; Petek, B. Evaluating the Impact of Physiological Properties of the Gastrointestinal Tract On Drug In Vivo Performance Using Physiologically Based Biopharmaceutics Modeling and Virtual Clinical Trials. J. Pharm. Sci. 2021, 110, 3069–3081. [Google Scholar] [CrossRef]
- Mudie, D.M.; Murray, K.; Hoad, C.L.; Pritchard, S.E.; Garnett, M.C.; Amidon, G.L.; Gowland, P.A.; Spiller, R.C.; Amidon, G.E.; Marciani, L. Quantification of gastrointestinal liquid volumes and distribution following a 240 mL dose of water in the fasted state. Mol. Pharm. 2014, 11, 3039–3047. [Google Scholar] [CrossRef] [PubMed]
- Murray, K.; Hoad, C.L.; Mudie, D.M.; Wright, J.; Heissam, K.; Abrehart, N.; Pritchard, S.E.; Al Atwah, S.; Gowland, P.A.; Garnett, M.C.; et al. Magnetic Resonance Imaging Quantification of Fasted State Colonic Liquid Pockets in Healthy Humans. Mol. Pharm. 2017, 14, 2629–2638. [Google Scholar] [CrossRef] [PubMed]
- Schiller, C.; Frohlich, C.P.; Giessmann, T.; Siegmund, W.; Monnikes, H.; Hosten, N.; Weitschies, W. Intestinal fluid volumes and transit of dosage forms as assessed by magnetic resonance imaging. Aliment. Pharmacol. Ther. 2005, 22, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Elbanna, H.; Emile, S.; El-Hawary, G.E.; Abdelsalam, N.; Zaytoun, H.A.; Elkaffas, H.; Ghanem, A. Assessment of the Correlation Between Preoperative and Immediate Postoperative Gastric Volume and Weight Loss After Sleeve Gastrectomy Using Computed Tomography Volumetry. World J. Surg. 2019, 43, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Almukainzi, M.; Lukacova, V.; Löbenberg, R. Modelling the Absorption of Metformin with Patients Post Gastric Bypass Surgery. J. Diabetes Metab. 2014, 5, 1000353. [Google Scholar] [CrossRef]
- Dahan, A.; Porat, D.; Markovic, M.; Zur, M.; Kister, O.; Langguth, P. Optimized In Silico Modeling of Drug Absorption after Gastric Bypass: The Case of Metformin. Pharmaceutics 2021, 13, 1873. [Google Scholar] [CrossRef]
- Darwich, A.S.; Pade, D.; Rowland-Yeo, K.; Jamei, M.; Asberg, A.; Christensen, H.; Ashcroft, D.M.; Rostami-Hodjegan, A. Evaluation of an In Silico PBPK Post-Bariatric Surgery Model through Simulating Oral Drug Bioavailability of Atorvastatin and Cyclosporine. CPT Pharmacomet. Syst. Pharmacol. 2013, 2, e47. [Google Scholar] [CrossRef]
- Steenackers, N.; Vanuytsel, T.; Augustijns, P.; Deleus, E.; Deckers, W.; Deroose, C.M.; Falony, G.; Lannoo, M.; Mertens, A.; Mols, R.; et al. Effect of sleeve gastrectomy and Roux-en-Y gastric bypass on gastrointestinal physiology. Eur. J. Pharm. Biopharm. 2023, 183, 92–101. [Google Scholar] [CrossRef]
- Lu, A.T.; Frisella, M.E.; Johnson, K.C. Dissolution modeling: Factors affecting the dissolution rates of polydisperse powders. Pharm. Res. 1993, 10, 1308–1314. [Google Scholar] [CrossRef]
- Alwhaibi, A.; Alsanea, S.; Alrabiah, Z.; Alanazi, F.K.; Al-Hadiya, B.M.; Abou-Auda, H.S. Pharmacokinetic profile of sildenafil citrate in healthy Middle Eastern Males: Comparison with other ethnicities. Saudi Pharm. J. 2021, 29, 1498–1505. [Google Scholar] [CrossRef]
- Food and Drug Administration, Center for Drug Evaluation and Research. Viagra (Sildenafil) “Joint Clinical Review” for NDA-20-895. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/NDA/98/viagra/sect7.PDF (accessed on 15 December 2023).
- Gao, X.; O’Gorman, M.; Cook, J.; Shi, H.; LaBadie, R.R. A Randomized, Open-Label, 3-Way Crossover Study to Demonstrate Bioequivalence of Sildenafil Powder for Oral Suspension With Tablets Used Commercially and in Clinical Studies for the Treatment of Pulmonary Arterial Hypertension. Clin. Pharmacol. Drug Dev. 2012, 1, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Abduljalil, K.; Cain, T.; Humphries, H.; Rostami-Hodjegan, A. Deciding on success criteria for predictability of pharmacokinetic parameters from in vitro studies: An analysis based on in vivo observations. Drug Metab. Dispos. 2014, 42, 1478–1484. [Google Scholar] [CrossRef] [PubMed]
- Puttrevu, S.K.; Arora, S.; Polak, S.; Patel, N.K. Physiologically Based Pharmacokinetic Modeling of Transdermal Selegiline and Its Metabolites for the Evaluation of Disposition Differences between Healthy and Special Populations. Pharmaceutics 2020, 12, 942. [Google Scholar] [CrossRef] [PubMed]
- Walker, D.K.; Ackland, M.J.; James, G.C.; Muirhead, G.J.; Rance, D.J.; Wastall, P.; Wright, P.A. Pharmacokinetics and metabolism of sildenafil in mouse, rat, rabbit, dog and man. Xenobiotica 1999, 29, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Macente, J.; Nauwelaerts, N.; Russo, F.M.; Deprest, J.; Allegaert, K.; Lammens, B.; Hernandes Bonan, R.; Turner, J.M.; Kumar, S.; Diniz, A.; et al. PBPK-based dose finding for sildenafil in pregnant women for antenatal treatment of congenital diaphragmatic hernia. Front. Pharmacol. 2023, 14, 1068153. [Google Scholar] [CrossRef] [PubMed]
- Salerno, S.N.; Edginton, A.; Gerhart, J.G.; Laughon, M.M.; Ambalavanan, N.; Sokol, G.M.; Hornik, C.D.; Stewart, D.; Mills, M.; Martz, K.; et al. Physiologically-Based Pharmacokinetic Modeling Characterizes the CYP3A-Mediated Drug-Drug Interaction Between Fluconazole and Sildenafil in Infants. Clin. Pharmacol. Ther. 2021, 109, 253–262. [Google Scholar] [CrossRef]
- Nichols, D.J.; Muirhead, G.J.; Harness, J.A. Pharmacokinetics of sildenafil after single oral doses in healthy male subjects: Absolute bioavailability, food effects and dose proportionality. Br. J. Clin. Pharmacol. 2002, 53 (Suppl. 1), 5S–12S. [Google Scholar] [CrossRef]
- Jetter, A.; Kinzig-Schippers, M.; Walchner-Bonjean, M.; Hering, U.; Bulitta, J.; Schreiner, P.; Sorgel, F.; Fuhr, U. Effects of grapefruit juice on the pharmacokinetics of sildenafil. Clin. Pharmacol. Ther. 2002, 71, 21–29. [Google Scholar] [CrossRef]
- Gupta, M.; Kovar, A.; Meibohm, B. The clinical pharmacokinetics of phosphodiesterase-5 inhibitors for erectile dysfunction. J. Clin. Pharmacol. 2005, 45, 987–1003. [Google Scholar] [CrossRef]
- Barbas, R.; Llinas, A.; Prohens, R. The Solid State Landscape of the Sildenafil Drug. J. Pharm. Sci. 2022, 111, 1104–1109. [Google Scholar] [CrossRef]
- Mitra, A.; Kesisoglou, F. Impaired drug absorption due to high stomach pH: A review of strategies for mitigation of such effect to enable pharmaceutical product development. Mol. Pharm. 2013, 10, 3970–3979. [Google Scholar] [CrossRef] [PubMed]
- Masaoka, Y.; Tanaka, Y.; Kataoka, M.; Sakuma, S.; Yamashita, S. Site of drug absorption after oral administration: Assessment of membrane permeability and luminal concentration of drugs in each segment of gastrointestinal tract. Eur. J. Pharm. Sci. 2006, 29, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Abuhelwa, A.Y.; Foster, D.J.R.; Upton, R.N. A Quantitative Review and Meta-models of the Variability and Factors Affecting Oral Drug Absorption-Part II: Gastrointestinal Transit Time. AAPS J. 2016, 18, 1322–1333. [Google Scholar] [CrossRef] [PubMed]
- Porat, D.; Dukhno, O.; Partook-Maccabi, M.; Vainer, E.; Cvijic, S.; Dahan, A. Selective COX-2 inhibitors after bariatric surgery: Celecoxib, etoricoxib and etodolac post-bariatric solubility/dissolution and pharmacokinetics. Int. J. Pharm. 2023, 645, 123347. [Google Scholar] [CrossRef] [PubMed]
- ClinCalc.com. The Top 300 Drugs of 2020. Available online: https://clincalc.com/DrugStats/Top300Drugs.aspx (accessed on 15 December 2023).
- Liu, S.; Cao, D.; Ren, Z.; Li, J.; Peng, L.; Zhang, Q.; Cheng, B.; Cheng, Z.; Ai, J.; Zheng, X.; et al. The relationships between bariatric surgery and sexual function: Current evidence based medicine. BMC Urol. 2020, 20, 150. [Google Scholar] [CrossRef] [PubMed]
- Tenhagen, M.; van Ramshorst, G.H.; Demirkiran, A.; Hunfeld, M.A.; Cense, H.A. Perioperative Online Weight Monitoring in Bariatric Surgery with a Digital Internet-Connected Scale. Obes. Surg. 2016, 26, 1120–1126. [Google Scholar] [CrossRef] [PubMed]
- Sockalingam, S.; Leung, S.E.; Wnuk, S.; Cassin, S.E.; Yanofsky, R.; Hawa, R. Psychiatric Management of Bariatric Surgery Patients: A Review of Psychopharmacological and Psychological Treatments and Their Impact on Postoperative Mental Health and Weight Outcomes. Psychosomatics 2020, 61, 498–507. [Google Scholar] [CrossRef] [PubMed]
- Becerra, A.Z.; Khalid, S.I.; Morgenstern, A.S.; Rembert, E.A.; Carroll, M.M.; Omotosho, P.A.; Torquati, A. The Association Between Bariatric Surgery and Psychiatric Disorders: A National Cohort Study. Obes. Surg. 2022, 32, 1110–1118. [Google Scholar] [CrossRef]
- Trinchieri, M.; Trinchieri, M.; Perletti, G.; Magri, V.; Stamatiou, K.; Cai, T.; Montanari, E.; Trinchieri, A. Erectile and Ejaculatory Dysfunction Associated with Use of Psychotropic Drugs: A Systematic Review. J. Sex. Med. 2021, 18, 1354–1363. [Google Scholar] [CrossRef]
- El Ansari, W.; Elhag, W. Weight Regain and Insufficient Weight Loss After Bariatric Surgery: Definitions, Prevalence, Mechanisms, Predictors, Prevention and Management Strategies, and Knowledge Gaps-a Scoping Review. Obes. Surg. 2021, 31, 1755–1766. [Google Scholar] [CrossRef]
- Porat, D.; Markovic, M.; Zur, M.; Fine-Shamir, N.; Azran, C.; Shaked, G.; Czeiger, D.; Vaynshtein, J.; Replyanski, I.; Sebbag, G.; et al. Increased Paracetamol Bioavailability after Sleeve Gastrectomy: A Crossover Pre- vs. Post-Operative Clinical Trial. J. Clin. Med. 2019, 8, 1949. [Google Scholar] [CrossRef] [PubMed]
- Dahan, A.; Porat, D.; Azran, C.; Mualem, Y.; Sakran, N.; Abu-Abeid, S. Lithium Toxicity with Severe Bradycardia Post Sleeve Gastrectomy: A Case Report and Review of the Literature. Obes. Surg. 2019, 29, 735–738. [Google Scholar] [CrossRef] [PubMed]
- Margolin, N.; Porat, D.; Dahan, A.; Lavon, O. Influence of Bariatric Surgery on Levetiracetam Clinical Effectiveness: Case Series. Obes. Surg. 2022, 32, 2795–2796. [Google Scholar] [CrossRef] [PubMed]
- Azran, C.; Porat, D.; Fine-Shamir, N.; Hanhan, N.; Dahan, A. Oral levothyroxine therapy postbariatric surgery: Biopharmaceutical aspects and clinical effects. Surg. Obes. Relat. Dis. 2019, 15, 333–341. [Google Scholar] [CrossRef]
- Porat, D.; Azran, C.; Kais, H.; Dahan, A. Managing the Unpredictable: Mechanistic Analysis and Clinical Recommendations for Lamotrigine Treatment after Bariatric Surgery. J. Clin. Med. 2021, 10, 5627. [Google Scholar] [CrossRef]
- Kvitne, K.E.; Robertsen, I.; Skovlund, E.; Christensen, H.; Krogstad, V.; Wegler, C.; Angeles, P.C.; Wollmann, B.M.; Hole, K.; Johnson, L.K.; et al. Short- and long-term effects of body weight loss following calorie restriction and gastric bypass on CYP3A-activity—A non-randomized three-armed controlled trial. Clin. Transl. Sci. 2022, 15, 221–233. [Google Scholar] [CrossRef]
- Zarezadeh, M.; Saedisomeolia, A.; Shekarabi, M.; Khorshidi, M.; Emami, M.R.; Muller, D.J. The effect of obesity, macronutrients, fasting and nutritional status on drug-metabolizing cytochrome P450s: A systematic review of current evidence on human studies. Eur. J. Nutr. 2021, 60, 2905–2921. [Google Scholar] [CrossRef]
- Porat, D.; Margolin, N.; Lavon, O.; Dahan, A. Carbamazepine Therapy After Bariatric Surgery: Eight Sleeve Gastrectomy Cases and Review of the Literature. Obes. Surg. 2022, 32, 3481–3486. [Google Scholar] [CrossRef]
- Ryu, S.Y.; Choi, Y.J.; Park, S.Y.; Kim, J.Y.; Kim, Y.D.; Kim, Y.W. Udenafil, a Phosphodiesterase 5 Inhibitor, Reduces Body Weight in High-Fat-Fed Mice. World J. Mens. Health 2018, 36, 41–49. [Google Scholar] [CrossRef]


| Drug | Column | Mobile Phase | Flow Rate (mL/min) | Injection Volume (µL) | Total Run Time (min) | Retention Time (min) | Detection Wavelength (nm) |
|---|---|---|---|---|---|---|---|
| Sildenafil | Waters XBridge C8, 3.5 µm, 4.6 × 150 mm | Water:Acetonitrile (+0.1% trifluoroacetic acid), 90:10 to 15:85 (v/v), gradient | 1.0 | 5 | 5.0 | 4.0 | 294 |
| Patient | Age | Gender | BMI | Procedure | Presurg pH | Postsurg pH |
|---|---|---|---|---|---|---|
| 1 | 49 | male | 43 | RYGB | 2.7 | 6.8 |
| 2 | 51 | female | 39 | OAGB | 1.5 | 7.2 |
| 3 | 25 | male | 71 | SG | 2.0 | 7.0 |
| In Vitro | Ex Vivo | ||||||
|---|---|---|---|---|---|---|---|
| Conditions | Medium | Maleate Buffer | Maleate Buffer | Acetate Buffer | Phosphate Buffer | Presurgery Stomach Content | Postsurgery Stomach Content |
| pH | 1 | 3 | 5 | 7 | 2.1 (0.6) | 7.0 (0.2) | |
| Solubility (mg/mL) | >30 | 2.0 (0.09) | 3.1 (0.2) | 0.3 (0.03) | 7.4 (1.5) | 0.06 (0.05) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Porat, D.; Dukhno, O.; Cvijić, S.; Dahan, A. The Complexity of Bariatric Patient’s Pharmacotherapy: Sildenafil Biopharmaceutics and Pharmacokinetics before vs. after Gastric Sleeve/Bypass. Pharmaceutics 2023, 15, 2795. https://doi.org/10.3390/pharmaceutics15122795
Porat D, Dukhno O, Cvijić S, Dahan A. The Complexity of Bariatric Patient’s Pharmacotherapy: Sildenafil Biopharmaceutics and Pharmacokinetics before vs. after Gastric Sleeve/Bypass. Pharmaceutics. 2023; 15(12):2795. https://doi.org/10.3390/pharmaceutics15122795
Chicago/Turabian StylePorat, Daniel, Oleg Dukhno, Sandra Cvijić, and Arik Dahan. 2023. "The Complexity of Bariatric Patient’s Pharmacotherapy: Sildenafil Biopharmaceutics and Pharmacokinetics before vs. after Gastric Sleeve/Bypass" Pharmaceutics 15, no. 12: 2795. https://doi.org/10.3390/pharmaceutics15122795
APA StylePorat, D., Dukhno, O., Cvijić, S., & Dahan, A. (2023). The Complexity of Bariatric Patient’s Pharmacotherapy: Sildenafil Biopharmaceutics and Pharmacokinetics before vs. after Gastric Sleeve/Bypass. Pharmaceutics, 15(12), 2795. https://doi.org/10.3390/pharmaceutics15122795








