Development of L-Lysine-Loaded PLGA Microparticles as a Controlled Release System for Angiogenesis Enhancement
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. MS Synthesis
2.3. Yield
2.4. Morphological Analysis
2.5. Diameters Distribution
2.6. Encapsulation Efficiency
2.7. Release Kinetics
2.8. Degradation Resistance
2.9. In Vitro Biological Assays
2.9.1. Cell Culture and Treatments
2.9.2. Cell Viability
2.9.3. Cell Migration Assay
2.9.4. RNA Isolation and Real-Time Quantitative Polymerase Chain Reaction
2.10. Statistical Analysis
3. Results
3.1. Yields
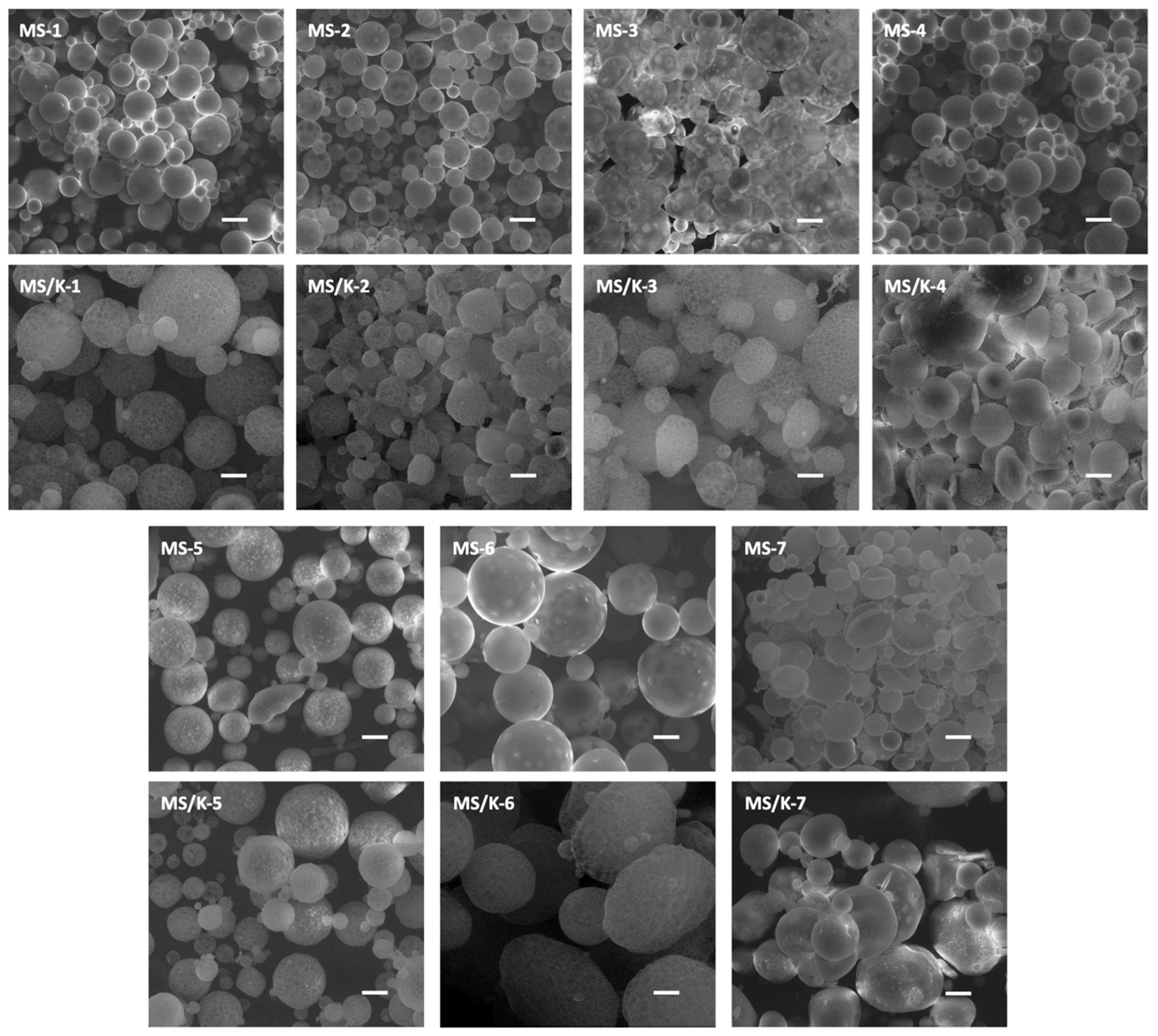
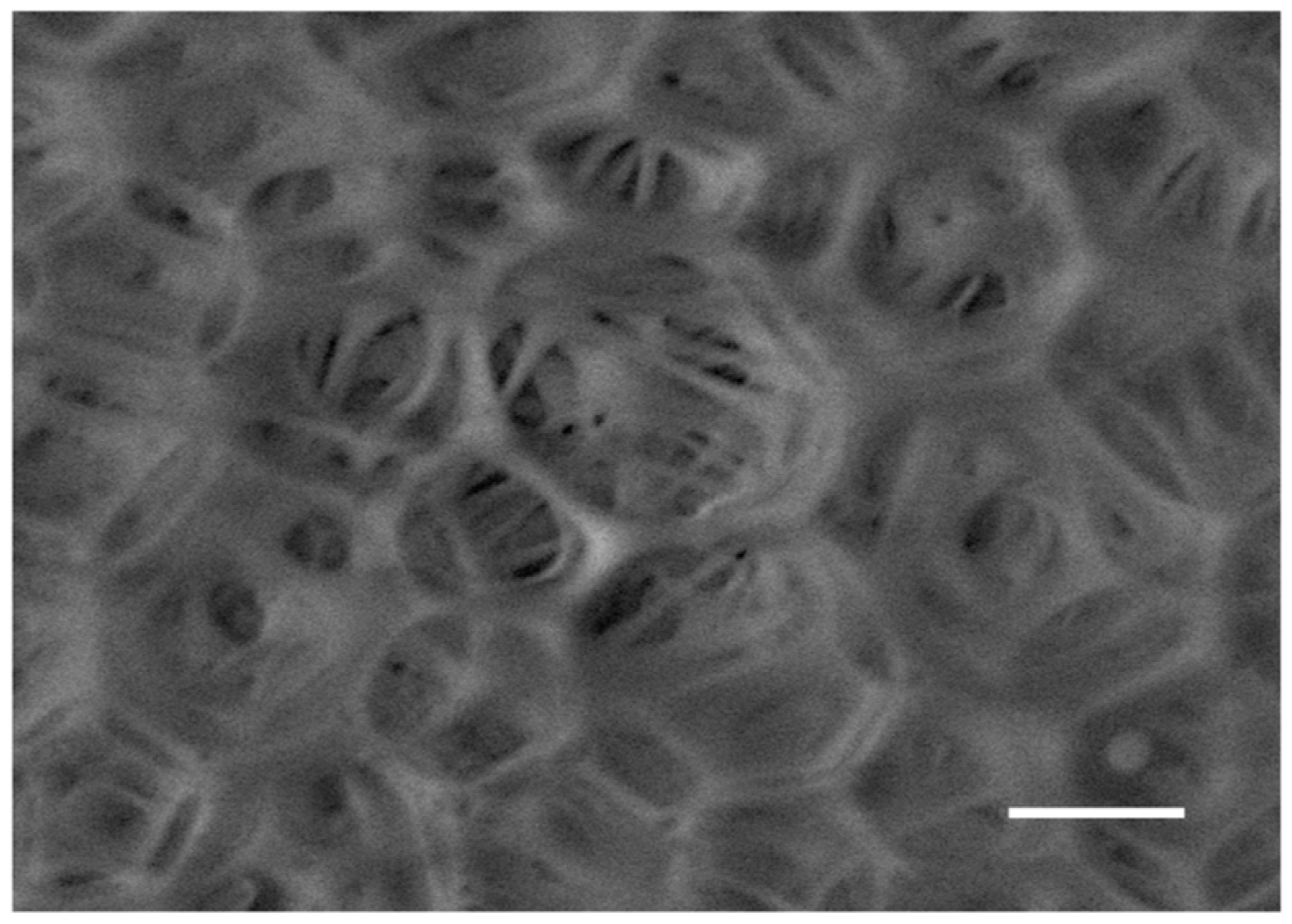
3.2. Morphological Analysis
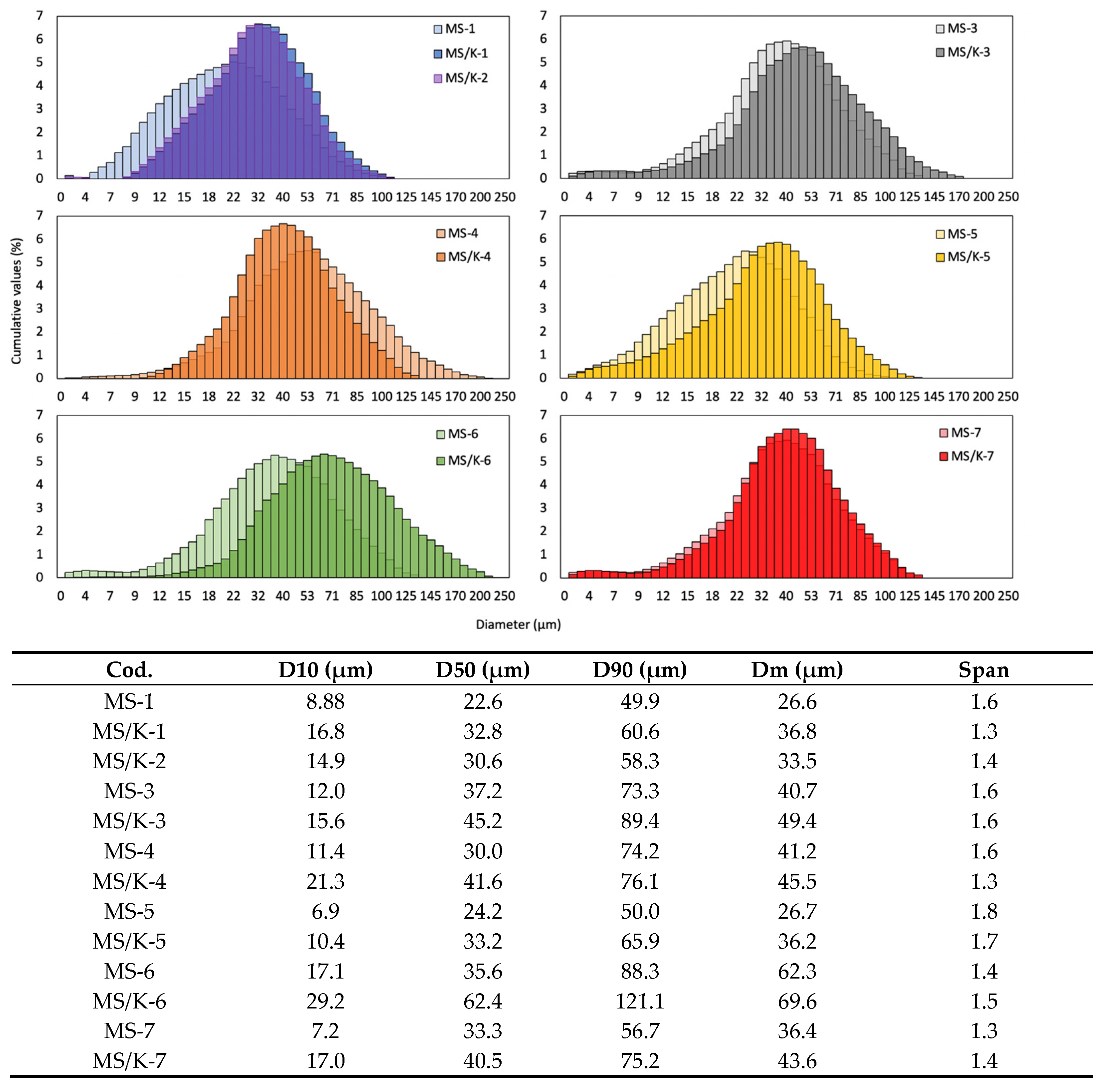
3.3. Diameter Distribution
3.4. Encapsulation Efficiency
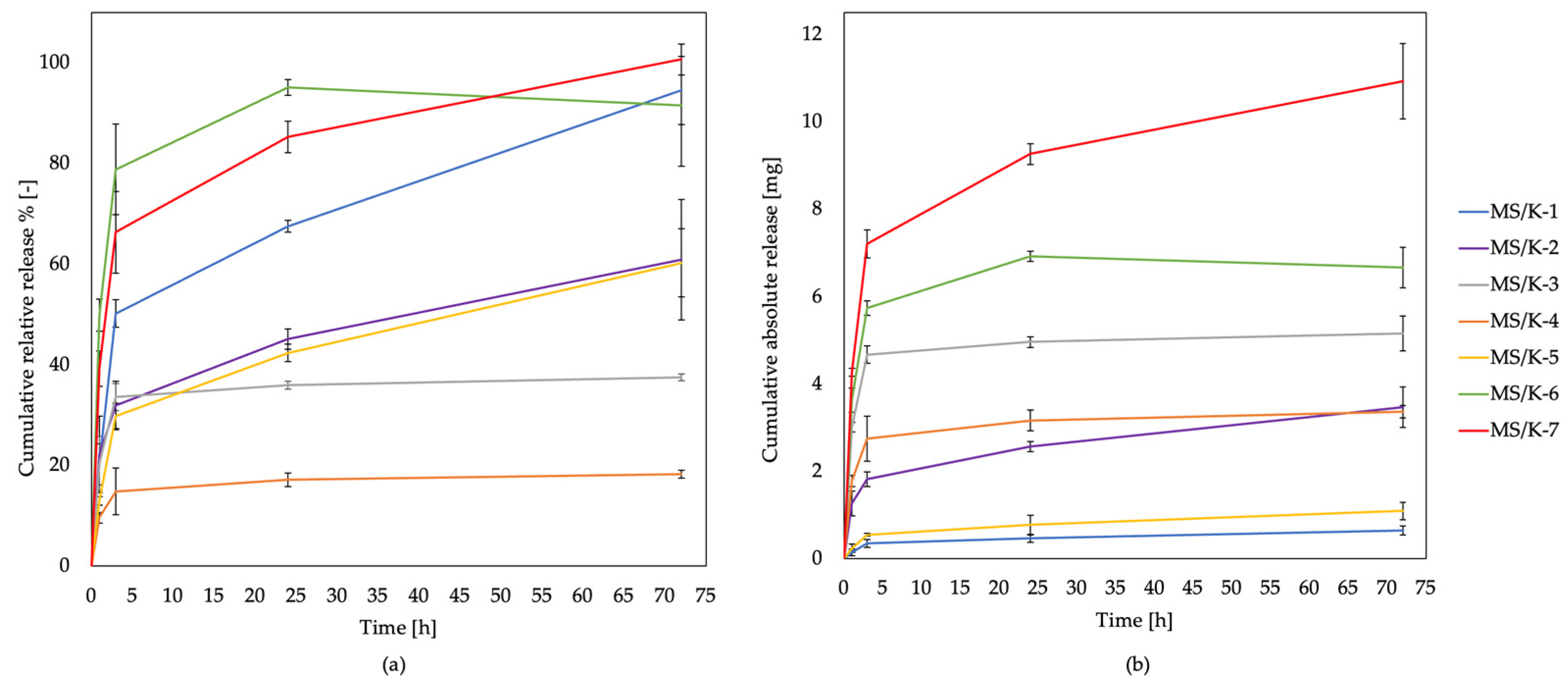
3.5. Release Kinetics
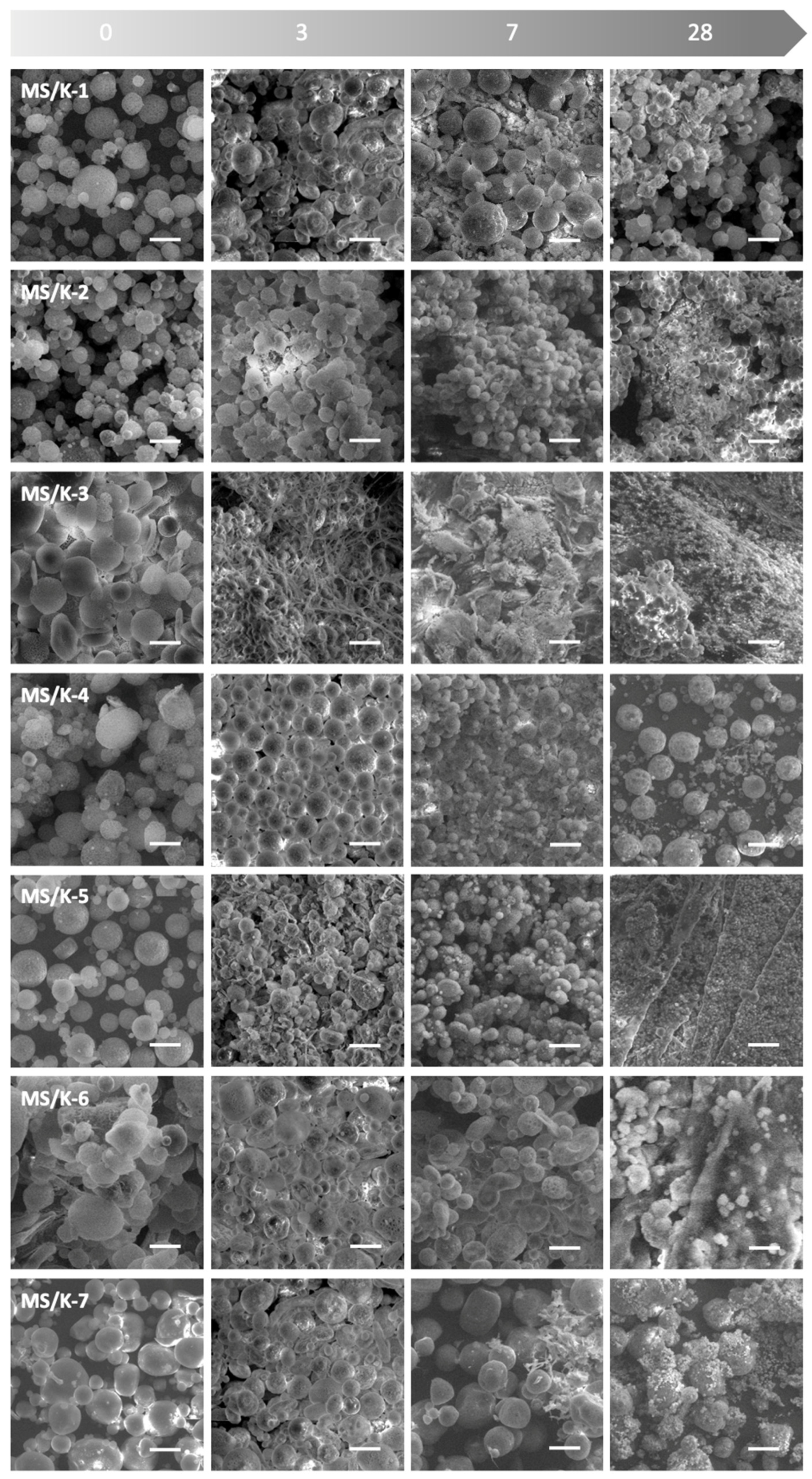
3.6. Degradation Resistance
3.7. In Vitro Response
3.7.1. MS/K-4 Biocompatibility Assessments with HMEC-1
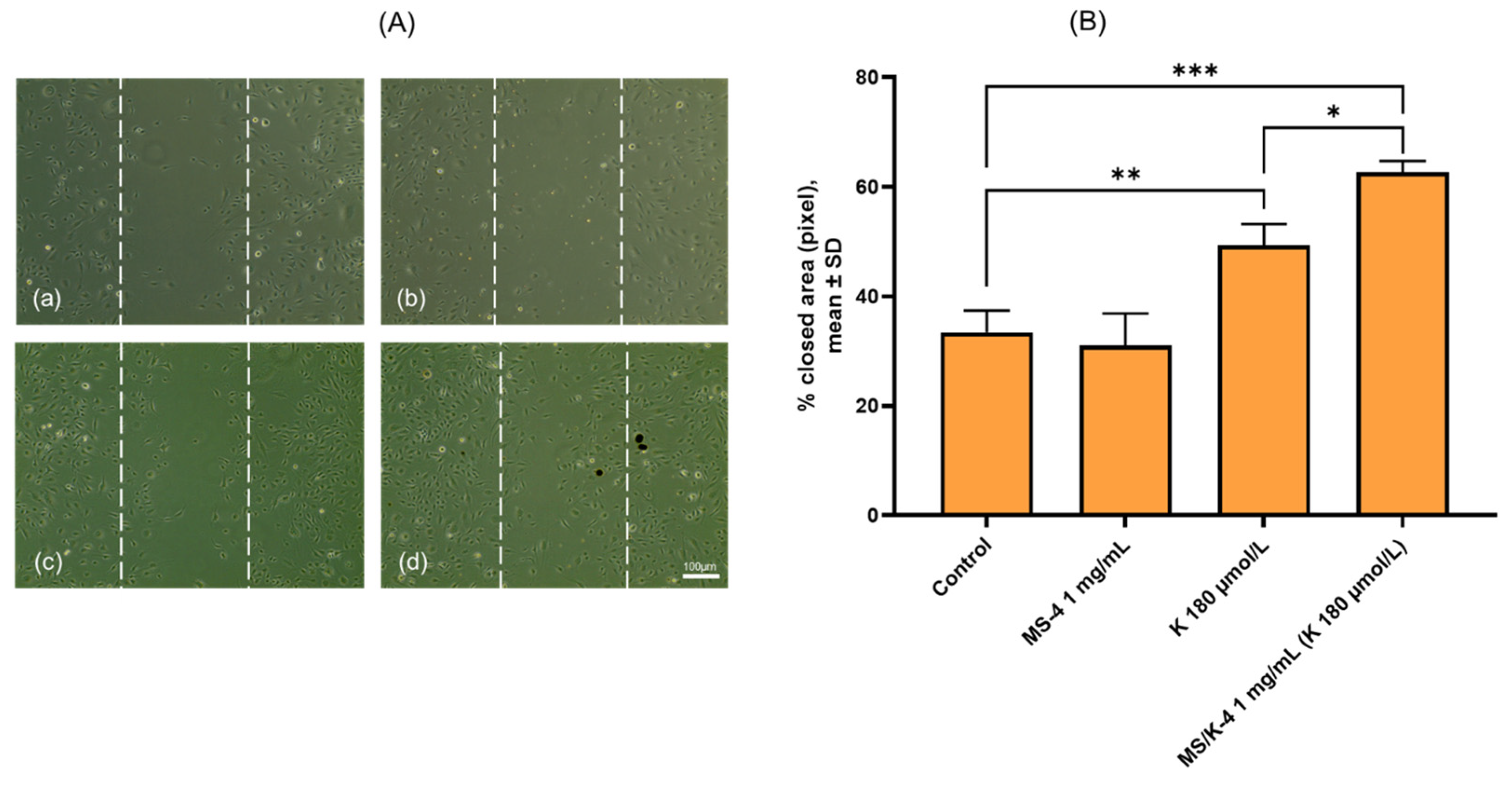
3.7.2. MS/K-4 Stimulated Angiogenesis: Effects on Cell Migration
3.7.3. MS/K-4 Stimulated the Expression of Pro-Angiogenic Genes in the Endothelium
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- van Hove, A.H.; Benoit, D.S.W. Depot-Based Delivery Systems for Pro-Angiogenic Peptides: A Review. Front. Bioeng. Biotechnol. 2015, 3, 102. [Google Scholar] [CrossRef] [PubMed]
- Vandekeere, S.; Dewerchin, M.; Carmeliet, P. Angiogenesis Revisited: An Overlooked Role of Endothelial Cell Metabolism in Vessel Sprouting. Microcirculation 2015, 22, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.Y.; Kwon, S.M. Angiogenesis and Its Therapeutic Opportunities. Mediat. Inflamm. 2013, 2013, 127170. [Google Scholar] [CrossRef] [PubMed]
- Chereddy, K.K.; Payen, V.L.; Préat, V. PLGA: From a Classic Drug Carrier to a Novel Therapeutic Activity Contributor. J. Control. Release 2018, 289, 10–13. [Google Scholar] [CrossRef]
- Chereddy, K.K.; Lopes, A.; Koussoroplis, S.; Payen, V.; Moia, C.; Zhu, H.; Sonveaux, P.; Carmeliet, P.; des Rieux, A.; Vandermeulen, G.; et al. Combined Effects of PLGA and Vascular Endothelial Growth Factor Promote the Healing of Non-Diabetic and Diabetic Wounds. Nanomedicine 2015, 11, 1975–1984. [Google Scholar] [CrossRef]
- Nagai, N.; Kumasaka, N.; Kawashima, T.; Kaji, H.; Nishizawa, M.; Abe, T. Preparation and Characterization of Collagen Microspheres for Sustained Release of VEGF. J. Mater. Sci. Mater. Med. 2010, 21, 1891–1898. [Google Scholar] [CrossRef]
- Bhise, N.S.; Shmueli, R.B.; Sunshine, J.C.; Tzeng, S.Y.; Green, J.J. Drug Delivery Strategies for Therapeutic Angiogenesis and Antiangiogenesis. Expert Opin. Drug Deliv. 2011, 8, 485–504. [Google Scholar] [CrossRef]
- Kim, D.-S.; Lee, J.-K.; Kim, J.H.; Lee, J.; Kim, D.S.; An, S.; Park, S.-B.; Kim, T.-H.; Rim, J.S.; Lee, S.; et al. Advanced PLGA Hybrid Scaffold with a Bioactive PDRN/BMP2 Nanocomplex for Angiogenesis and Bone Regeneration Using Human Fetal MSCs. Sci. Adv. 2021, 7, eabj1083. [Google Scholar] [CrossRef]
- de Negri Atanasio, G.; Ferrari, P.F.; Campardelli, R.; Firpo, G.; Perego, P.; Palombo, D. Bevacizumab-Controlled Delivery from Polymeric Microparticle Systems as Interesting Tools for Pathologic Angiogenesis Diseases. Polymers 2022, 14, 2593. [Google Scholar] [CrossRef]
- Simón-Yarza, T.; Formiga, F.R.; Tamayo, E.; Pelacho, B.; Prosper, F.; Blanco-Prieto, M.J. PEGylated-PLGA Microparticles Containing VEGF for Long Term Drug Delivery. Int. J. Pharm. 2013, 440, 13–18. [Google Scholar] [CrossRef]
- Tonello, S.; Moore, M.C.; Sharma, B.; Dobson, J.; McFetridge, P.S. Controlled Release of a Heterogeneous Human Placental Matrix from PLGA Microparticles to Modulate Angiogenesis. Drug Deliv. Transl. Res. 2016, 6, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Qiu, J.; Shu, C.; Li, X.; Ye, C.; Zhang, W.-C. Exosomes from Linc00511-Overexpressing ADSCs Accelerates Angiogenesis in Diabetic Foot Ulcers Healing by Suppressing PAQR3-Induced Twist1 Degradation. Diabetes Res. Clin. Pract. 2021, 180, 109032. [Google Scholar] [CrossRef] [PubMed]
- Sheehy, E.J.; Miller, G.J.; Amado, I.; Raftery, R.M.; Chen, G.; Cortright, K.; Vazquez, A.G.; O’Brien, F.J. Mechanobiology-Informed Regenerative Medicine: Dose-Controlled Release of Placental Growth Factor from a Functionalized Collagen-Based Scaffold Promotes Angiogenesis and Accelerates Bone Defect Healing. J. Control. Release 2021, 334, 96–105. [Google Scholar] [CrossRef]
- Kim, J.-H.; Kim, T.-H.; Kang, M.S.; Kim, H.-W. Angiogenic Effects of Collagen/Mesoporous Nanoparticle Composite Scaffold Delivering VEGF165. BioMed Res. Int. 2016, 2016, 9676934. [Google Scholar] [CrossRef]
- Dornelas, C.A.; Fechine-Jamacaru, F.V.; Albuquerque, I.L.; Magalhães, H.I.F.; Dias, T.A.; Faria, M.H.G.; Alves, M.K.S.; Rabenhorst, S.H.B.; de Almeida, P.R.C.; de Lemos, T.L.G.; et al. Angiogenesis Inhibition by Green Propolis and the Angiogenic Effect of L-Lysine on Bladder Cancer in Rats. Acta Cir. Bras. 2012, 27, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Datta, D.; Bhinge, A.; Chandran, V. Lysine: Is It Worth More? Cytotechnology 2001, 36, 3–32. [Google Scholar] [CrossRef]
- Datta, D.; Kundu, P.K.; Biswas, S.; Dasgupta, S.; Bhinge, A.; Chandran, V. Effect of Cationic Amino Acid, L-Lysine and Its Polymers on the Growth and Secretion of Hybridoma Cell Line OKT-3. Hybridoma 2000, 19, 339–346. [Google Scholar] [CrossRef]
- Datta, D.; Verma, P.; Banerjee, A.; Kar, S.; Sengupta, T.; Sengupta, N.; Samanta, S.K.; Khan, E.M. Lysine as a Potential Low Molecular Weight Angiogen: Its Clinical, Experimental and in-Silico Validation—A Brief Study. bioRxiv 2016, 080176. [Google Scholar] [CrossRef]
- Saravanan, P.; Chenthamarai, G. A Randomized, Open Label, Comparative Study of Lysine Cream with Standard Treatment in Patients with Second Degree Superficial Burns. Asian J. Pharm. Clin. Res. 2017, 10, 219. [Google Scholar] [CrossRef]
- Vani, J.; Kumara, S.; Prathima, C. A Randomized, Open-Label, Comparative Study of Lysine Cream 15% with Standard Therapy in the Management of Non-Diabetic Foot Ulcer Assessing by Bates-Jensen Wound Assessment Tool. Natl. J. Physiol. Pharm. Pharmacol. 2019, 9, 907–911. [Google Scholar] [CrossRef]
- Gupta, R.K.; Agarwal, A.; Agarwal, S.; Mohan, P.; Husain, M.; Alger, J.; Pandey, C.M.; Datta, D. Reversal of Acute Human Brain Ischemic Injury by Lysine Induced Therapeutic Angiogenesis: Preliminary Results of a Pilot Study. Internet J. Neurol. 2005, 4, 1–8. [Google Scholar] [CrossRef]
- Flodin, N.W. The Metabolic Roles, Pharmacology, and Toxicology of Lysine. J. Am. Coll. Nutr. 1997, 16, 7–21. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Skidmore, S.; Hadar, J.; Garner, J.; Park, H.; Otte, A.; Soh, B.K.; Yoon, G.; Yu, D.; Yun, Y.; et al. Injectable, Long-Acting PLGA Formulations: Analyzing PLGA and Understanding Microparticle Formation. J. Control. Release 2019, 304, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Maturavongsadit, P.; Paravyan, G.; Kovarova, M.; Garcia, J.V.; Benhabbour, S.R. A New Engineering Process of Biodegradable Polymeric Solid Implants for Ultra-Long-Acting Drug Delivery. Int. J. Pharm. X 2021, 3, 100068. [Google Scholar] [CrossRef]
- Benhabbour, S.R.; Kovarova, M.; Jones, C.; Copeland, D.J.; Shrivastava, R.; Swanson, M.D.; Sykes, C.; Ho, P.T.; Cottrell, M.L.; Sridharan, A.; et al. Ultra-Long-Acting Tunable Biodegradable and Removable Controlled Release Implants for Drug Delivery. Nat. Commun. 2019, 10, 4324. [Google Scholar] [CrossRef]
- Makadia, H.K.; Siegel, S.J. Poly Lactic-Co-Glycolic Acid (PLGA) as Biodegradable Controlled Drug Delivery Carrier. Polymers 2011, 3, 1377–1397. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Kunduru, K.R.; Basu, A.; Mizrahi, B.; Domb, A.J.; Khan, W. Injectable Formulations of Poly(Lactic Acid) and Its Copolymers in Clinical Use. Adv. Drug Deliv. Rev. 2016, 107, 213–227. [Google Scholar] [CrossRef]
- Lackington, W.A.; Kočí, Z.; Alekseeva, T.; Hibbitts, A.J.; Kneafsey, S.L.; Chen, G.; O’Brien, F.J. Controlling the Dose-Dependent, Synergistic and Temporal Effects of NGF and GDNF by Encapsulation in PLGA Microparticles for Use in Nerve Guidance Conduits for the Repair of Large Peripheral Nerve Defects. J. Control. Release 2019, 304, 51–64. [Google Scholar] [CrossRef]
- Porporato, P.E.; Payen, V.L.; de Saedeleer, C.J.; Préat, V.; Thissen, J.-P.; Feron, O.; Sonveaux, P. Lactate Stimulates Angiogenesis and Accelerates the Healing of Superficial and Ischemic Wounds in Mice. Angiogenesis 2012, 15, 581–592. [Google Scholar] [CrossRef]
- Chereddy, K.K.; Coco, R.; Memvanga, P.B.; Ucakar, B.; des Rieux, A.; Vandermeulen, G.; Préat, V. Combined Effect of PLGA and Curcumin on Wound Healing Activity. J. Control. Release 2013, 171, 208–215. [Google Scholar] [CrossRef]
- Swider, E.; Koshkina, O.; Tel, J.; Cruz, L.J.; de Vries, I.J.M.; Srinivas, M. Customizing Poly(Lactic-Co-Glycolic Acid) Particles for Biomedical Applications. Acta Biomater. 2018, 73, 38–51. [Google Scholar] [CrossRef]
- Chaisri, W.; Ghassemi, A.H.; Hennink, W.E.; Okonogi, S. Enhanced Gentamicin Loading and Release of PLGA and PLHMGA Microspheres by Varying the Formulation Parameters. Colloids Surf. B Biointerfaces 2011, 84, 508–514. [Google Scholar] [CrossRef] [PubMed]
- Ravi, S.; Peh, K.K.; Darwis, Y.; Murthy, B.K.; Sing, T.R.R.; Mallikarjun, C. Development and Characterization of Polymeric Microspheres for Controlled Release Protein Loaded Drug Delivery System. Indian J. Pharm. Sci. 2008, 70, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Essa, D.; Kondiah, P.P.D.; Choonara, Y.E.; Pillay, V. The Design of Poly(Lactide-Co-Glycolide) Nanocarriers for Medical Applications. Front. Bioeng. Biotechnol. 2020, 8, 48. [Google Scholar] [CrossRef] [PubMed]
- Rosca, I.D.; Watari, F.; Uo, M. Microparticle Formation and Its Mechanism in Single and Double Emulsion Solvent Evaporation. J. Control. Release 2004, 99, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Yeo, Y.; Park, K. Control of Encapsulation Efficiency and Initial Burst in Polymeric Microparticle Systems. Arch. Pharm. Res. 2004, 27, 1–12. [Google Scholar] [CrossRef]
- Si, W.; Yang, Q.; Zong, Y.; Ren, G.; Zhao, L.; Hong, M.; Xin, Z. Toward Understanding the Effect of Solvent Evaporation on the Morphology of PLGA Microspheres by Double Emulsion Method. Ind. Eng. Chem. Res. 2021, 60, 9196–9205. [Google Scholar] [CrossRef]
- Mensah, R.A.; Kirton, S.B.; Cook, M.T.; Styliari, I.D.; Hutter, V.; Chau, D.Y.S. Optimising Poly(Lactic-Co-Glycolic Acid) Microparticle Fabrication Using a Taguchi Orthogonal Array Design-of-Experiment Approach. PLoS ONE 2019, 14, e0222858. [Google Scholar] [CrossRef]
- Gallo, L.C.; Madaghiele, M.; Salvatore, L.; Barca, A.; Scialla, S.; Bettini, S.; Valli, L.; Verri, T.; Bucalá, V.; Sannino, A. Integration of PLGA Microparticles in Collagen-Based Matrices: Tunable Scaffold Properties and Interaction Between Microparticles and Human Epithelial-Like Cells. Int. J. Polym. Mater. Polym. Biomater. 2020, 69, 137–147. [Google Scholar] [CrossRef]
- Vysloužil, J.; Doležel, P.; Kejdušová, M.; Mašková, E.; Mašek, J.; Lukáč, R.; KošѤál, V.; Vetchý, D.; Dvorackova, K. Influence of Different Formulations and Process Parameters during the Preparation of Drug-Loaded PLGA Microspheres Evaluated by Multivariate Data Analysis. Acta Pharm. 2014, 64, 403–417. [Google Scholar] [CrossRef] [Green Version]
- Kim, D.; Han, T.H.; Hong, S.C.; Park, S.J.; Lee, Y.H.; Kim, H.; Park, M.; Lee, J. PLGA Microspheres with Alginate-Coated Large Pores for the Formulation of an Injectable Depot of Donepezil Hydrochloride. Pharmaceutics 2020, 12, 311. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, L.; Calò, E.; Bonfrate, V.; Pedone, D.; Gallo, N.; Natali, M.L.; Sannino, A.; Madaghiele, M. Exploring the Effects of the Crosslink Density on the Physicochemical Properties of Collagen-Based Scaffolds. Polym. Test. 2021, 93, 106966. [Google Scholar] [CrossRef]
- Gallo, N.; Natali, M.L.; Curci, C.; Picerno, A.; Gallone, A.; Vulpi, M.; Vitarelli, A.; Ditonno, P.; Cascione, M.; Sallustio, F.; et al. Analysis of the Physico-Chemical, Mechanical and Biological Properties of Crosslinked Type-I Collagen from Horse Tendon: Towards the Development of Ideal Scaffolding Material for Urethral Regeneration. Materials 2021, 14, 7648. [Google Scholar] [CrossRef] [PubMed]
- Giampetruzzi, L.; Laura Blasi, L.; Alessandra Quarta, A.; Simona Argentiere, S.; Claudia Cella, C.; Luca Salvatore, L.; Marta Madaghiele, M.; Giuseppe Gigli, G.; Alessandro Sannino, A. Poly(Lactide-Co-Glycolide) Nanoparticles Embeddedin a Micropatterned Collagen Scaffold for Neuronaltissue Regeneration. Int. J. Polym. Mater. Polym. Biomater. 2017, 66, 359–368. [Google Scholar] [CrossRef]
- Masaeli, R.; Kashi, T.S.J.; Dinarvand, R.; Tahriri, M.; Rakhshan, V.; Esfandyari-Manesh, M. Preparation, Characterization and Evaluation of Drug Release Properties of Simvastatin-Loaded PLGA Microspheres. Iran. J. Pharm. Res. 2016, 15, 205–211. [Google Scholar]
- Li, L.; Wang, Q.; Li, H.; Yuan, M.; Yuan, M. Preparation, Characterization, In Vitro Release and Degradation of Cathelicidin-BF-30-PLGA Microspheres. PLoS ONE 2014, 9, e100809. [Google Scholar] [CrossRef]
- Ades, E.W.; Candal, F.J.; Swerlick, R.A.; George, V.G.; Summers, S.; Bosse, D.C.; Lawley, T.J. HMEC-1: Establishment of an Immortalized Human Microvascular Endothelial Cell Line. J. Investig. Dermatol. 1992, 99, 683–690. [Google Scholar] [CrossRef]
- Quarta, S.; Santarpino, G.; Carluccio, M.A.; Calabriso, N.; Scoditti, E.; Siculella, L.; Damiano, F.; Maffia, M.; Verri, T.; de Caterina, R.; et al. Analysis of the Anti-Inflammatory and Anti-Osteoarthritic Potential of Flonat Fast®, a Combination of Harpagophytum Procumbens DC. Ex Meisn., Boswellia Serrata Roxb., Curcuma longa L., Bromelain and Escin (Aesculus hippocastanum), Evaluated in In Vitro Models of Inflammation Relevant to Osteoarthritis. Pharmaceuticals 2022, 15, 1263. [Google Scholar] [CrossRef]
- Suarez-Arnedo, A.; Torres Figueroa, F.; Clavijo, C.; Arbeláez, P.; Cruz, J.C.; Muñoz-Camargo, C. An Image J Plugin for the High Throughput Image Analysis of In Vitro Scratch Wound Healing Assays. PLoS ONE 2020, 15, e0232565. [Google Scholar] [CrossRef]
- Adebileje, T.; Amani, A. Modelling Particle Size, Drug Loading and Release of BSA Encapsulated into PLGA Nanoparticles. J. Mater. Sci. Eng. 2018, 7, 1000496. [Google Scholar] [CrossRef]
- Han, F.Y.; Thurecht, K.J.; Whittaker, A.K.; Smith, M.T. Bioerodable PLGA-Based Microparticles for Producing Sustained-Release Drug Formulations and Strategies for Improving Drug Loading. Front. Pharmacol. 2016, 7, 185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Engineer, C.; Parikh, J.; Raval, A. Hydrolytic Degradation Behavior of 50/50 Poly Lactide-Co-Glycolide from Drug Eluting Stents. Trends Biomater. Artif. Organs 2010, 24, 131–138. [Google Scholar]
- Lamalice, L.; le Boeuf, F.; Huot, J. Endothelial Cell Migration During Angiogenesis. Circ. Res. 2007, 100, 782–794. [Google Scholar] [CrossRef] [PubMed]
- Jadhav, U.; Chigurupati, S.; Lakka, S.S.; Mohanam, S. Inhibition of Matrix Metalloproteinase-9 Reduces In Vitro Invasion and Angiogenesis in Human Microvascular Endothelial Cells. Int. J. Oncol. 2004, 25, 1407–1414. [Google Scholar] [CrossRef] [PubMed]
- Cox, B.D.; Natarajan, M.; Stettner, M.R.; Gladson, C.L. New Concepts Regarding Focal Adhesion Kinase Promotion of Cell Migration and Proliferation. J. Cell. Biochem. 2006, 99, 35–52. [Google Scholar] [CrossRef] [PubMed]
- Ucuzian, A.A.; Gassman, A.A.; East, A.T.; Greisler, H.P. Molecular Mediators of Angiogenesis. J. Burn Care Res. 2010, 31, 158–175. [Google Scholar] [CrossRef] [PubMed]
- Bir, S.C.; Xiong, Y.; Kevil, C.G.; Luo, J. Emerging Role of PKA/ENOS Pathway in Therapeutic Angiogenesis for Ischaemic Tissue Diseases. Cardiovasc. Res. 2012, 95, 7–18. [Google Scholar] [CrossRef]
- Sun, S.; Wu, H.-J.; Guan, J.-L. Nuclear FAK and Its Kinase Activity Regulate VEGFR2 Transcription in Angiogenesis of Adult Mice. Sci. Rep. 2018, 8, 2550. [Google Scholar] [CrossRef]
- Lu, H.; Xu, X.; Zhang, M.; Cao, R.; Bråkenhielm, E.; Li, C.; Lin, H.; Yao, G.; Sun, H.; Qi, L.; et al. Combinatorial Protein Therapy of Angiogenic and Arteriogenic Factors Remarkably Improves Collaterogenesis and Cardiac Function in Pigs. Proc. Natl. Acad. Sci. USA 2007, 104, 12140–12145. [Google Scholar] [CrossRef]
- Anderson, J.M.; Shive, M.S. Biodegradation and Biocompatibility of PLA and PLGA Microspheres. Adv. Drug Deliv. Rev. 2012, 64, 72–82. [Google Scholar] [CrossRef]
- Dawes, G.J.S.; Fratila-Apachitei, L.E.; Mulia, K.; Apachitei, I.; Witkamp, G.J.; Duszczyk, J. Size Effect of PLGA Spheres on Drug Loading Efficiency and Release Profiles. J. Mater. Sci. Mater. Med. 2009, 20, 1089–1094. [Google Scholar] [CrossRef] [PubMed]
- Danhier, F.; Ansorena, E.; Silva, J.M.; Coco, R.; le Breton, A.; Préat, V. PLGA-Based Nanoparticles: An Overview of Biomedical Applications. J. Control. Release 2012, 161, 505–522. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, S.M.; Gajdusek, C.M. Contact Inhibition in the Endothelium. In Biology of Endothelial Cells; Springer: Berlin/Heidelberg, Germany, 1984; pp. 66–73. [Google Scholar]
- Zecchin, A.; Kalucka, J.; Dubois, C.; Carmeliet, P. How Endothelial Cells Adapt Their Metabolism to Form Vessels in Tumors. Front. Immunol. 2017, 8, 1750. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Cod. | W1 | O | W2 | |||
|---|---|---|---|---|---|---|
| LYS (%) | VW1 (mL) | VO (mL) | PLGA (%) | VW2 (mL) | PVA (%) | |
| MS-1 | 2 | 0.5 | 5 | 10 | 50 | 0.5 |
| MS-2 | 10 | 0.5 | 5 | 10 | 50 | 0.5 |
| MS-3 | 10 | 0.5 | 5 | 15 | 50 | 1 |
| MS-4 | 10 | 0.5 | 5 | 15 | 50 | 2 |
| MS-5 | 10 | 0.5 | 5 | 15 | 500 | 1 |
| MS-6 | 10 | 0.5 | 5 | 15 | 50 | 1, PBS 0.01 M |
| MS-7 | 10 | 0.5 | 5 | 15 | 50 | 1, PBS 0.07 M |
| Gene Symbol | Full Name | Forward Primer (5′-3′) | Revers Primer (3′-5′) | Accession Number |
|---|---|---|---|---|
| VEGF | Vascular endothelial growth factor | GACACACCCACCCACATACA | TCTCCTCCTCTTCCCTGTCA | NM_001171626.1 |
| KDR/VEGFR-2 | Kinase insert domain receptor/vascular endothelial growth factor receptor 2 | AGCGATGGCCTCTTCTGTAA | ACACGACTCCATGTTGGTCA | NM_002253.2 |
| MMP-9 | Matrix metalloproteinase-9 | TTGACAGCGACAAGAAGTGG | GCCATTCACGTCGTCCTTAT | NM_004994.2 |
| FAK | Focal adhesion kinase | ATTAAATGGATGGCTCCA | CTCCCACATACACACACC | MN_001352694.2 |
| PDGF | Platelet-derived growth factor | TTGTGCGGAAGAAGCCAATC | CTCCTTCAGTGCCGTCTTGT | NM_033016.3 |
| FGF-2 | Basic fibroblast growth factor-2 | AGAGCGACCCTCACATCAAG | TCGTTTCAGTGCCACATACC | NM_002006.5 |
| eNOS | Endothelial nitric oxide synthase | ACCCTCACCGCTACAACATC | GCTCATTCTCCAGGTGCTTC | NM_000603.4 |
| GAPDH | Glyceraldehyde-3-phosphate dehydrogenase | ATGGCCTTCCGTGTCCCCAC | ACGCCTGCTTCACCACCTTC | NM_002046.3 |
| Cod. | Yield (%) |
|---|---|
| MS-1 | 71.8 ± 1.7 |
| MS/K-1 | 70.6 ± 1.2 |
| MS/K-2 | 74.2 ± 0.9 |
| MS-3 | 69.3 ± 1.8 |
| MS/K-3 | 90.1 ± 0.6 |
| MS-4 | 98.4 ± 1.1 |
| MS/K-4 | 88.3 ± 1.3 |
| MS-5 | 80.6 ± 0.8 |
| MS/K-5 | 84.0 ± 1.0 |
| MS-6 | 78.6 ± 0.7 |
| MS/K-6 | 84.0 ± 0.9 |
| MS-7 | 85.3 ± 1.5 |
| MS/K-7 | 86.5 ± 1.4 |
| Sample | LYSi (mg) | LYSf (mg) | EE (%) |
|---|---|---|---|
| MS/K-1 | 10 | 0.9 ± 0.3 | 8.9 ± 1.8 |
| MS/K-2 | 50 | 6.2 ± 1.0 | 12.4 ± 2.0 |
| MS/K-3 | 50 | 13.2 ± 1.4 | 25.9 ± 3.2 |
| MS/K-4 | 50 | 18.0 ± 1.6 | 36.0 ± 2.3 |
| MS/K-5 | 50 | 1.8 ± 0.8 | 3.6 ± 2.2 |
| MS/K-6 | 50 | 8.2 ± 1.4 | 16.4 ± 3.4 |
| MS/K-7 | 50 | 11.9 ± 2.1 | 23.7 ± 2.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gallo, N.; Quarta, S.; Massaro, M.; Carluccio, M.A.; Barca, A.; Cannoletta, D.; Siculella, L.; Salvatore, L.; Sannino, A. Development of L-Lysine-Loaded PLGA Microparticles as a Controlled Release System for Angiogenesis Enhancement. Pharmaceutics 2023, 15, 479. https://doi.org/10.3390/pharmaceutics15020479
Gallo N, Quarta S, Massaro M, Carluccio MA, Barca A, Cannoletta D, Siculella L, Salvatore L, Sannino A. Development of L-Lysine-Loaded PLGA Microparticles as a Controlled Release System for Angiogenesis Enhancement. Pharmaceutics. 2023; 15(2):479. https://doi.org/10.3390/pharmaceutics15020479
Chicago/Turabian StyleGallo, Nunzia, Stefano Quarta, Marika Massaro, Maria Annunziata Carluccio, Amilcare Barca, Donato Cannoletta, Luisa Siculella, Luca Salvatore, and Alessandro Sannino. 2023. "Development of L-Lysine-Loaded PLGA Microparticles as a Controlled Release System for Angiogenesis Enhancement" Pharmaceutics 15, no. 2: 479. https://doi.org/10.3390/pharmaceutics15020479
APA StyleGallo, N., Quarta, S., Massaro, M., Carluccio, M. A., Barca, A., Cannoletta, D., Siculella, L., Salvatore, L., & Sannino, A. (2023). Development of L-Lysine-Loaded PLGA Microparticles as a Controlled Release System for Angiogenesis Enhancement. Pharmaceutics, 15(2), 479. https://doi.org/10.3390/pharmaceutics15020479










