Approved Nanomedicine against Diseases
Abstract
:1. Introduction
2. Liposomes and Lipid Nanoparticles (LNPs)
2.1. Liposomes
2.1.1. Liposomes against Cancer
2.1.2. Liposomes against Infection
2.1.3. Liposomes for Pain Relief and Other Disease Therapy
2.2. LNPs against Hereditary Transthyretin Amyloidosis (hATTR) and COVID-19 Infection
| Trade Name | Approval Year | Drug Agent | Company | Clinical Applications | Agency | Administration Route | Ref. |
|---|---|---|---|---|---|---|---|
| Ambisome® | 1990 | Amphotericin B | Gilead Sciences (Foster, CA, USA) | Fungal infection/Anti-leishmanial | EMA | intravenous | [55,93,94] |
| Epaxal® | 1993 | Inactivated hepatitis A virus (strain RGSB) | Crucell Berna Biotech (Berne, Switzerland) | Hepatitis A | EMA | intramuscular | [95,96] |
| Abelcet® | 1995 | Amphotericin B | Sigma-Tau Pharmaceutical Inc. (Gaithersburg, MD, USA) | Invasive severe fungal infections | FDA | intravenous | [56] |
| Doxil®/Caelyx® | 1995/1996 | Doxorubicin | Sequus Pharmaceuticals (Santa Clara County, CA, USA) | Ovarian cancer and KS | FDA/EMA | intravenous | [33,34,97] |
| Amphotec® | 1996 | Amphotericin B | Ben Venue Laboratories (Bedford, OH, USA) | Severe fungal infections | FDA | intravenous | [98] |
| DaunoXome® | 1996 | Daunorubicin | NeXstar Pharmaceuticals (Foster, CA, USA) | KS infected with HIV | FDA | intravenous | [99] |
| Inflexal® V | 1997 | Inactivated hemagglutinin of Influenza virus strains A and B | Crucell Berna Biotech (Berne, Switzerland) | Influenza | EMA | intramuscular | [57] |
| Depocyt® | 1999 | Cytarabine | Skye Pharm Inc. (San Diego, CA, USA) | Neoplastic meningitis | FDA | spinal | [100,101] |
| Visudyne® | 2000 | Verteporfin | Novartis AG (Basel, Switzerland) | Choroidal neovascularization | FDA | intravenous | [75] |
| Myocet® | 2001 | Doxorubicin | IDM Pharma (Irvine, CA, USA) | Combination therapy with cyclophosphamide in metastatic breast cancer | EMA | intravenous | [102] |
| Lipusu® | 2003 | Paclitaxel | Luye Pharma (Nanjing, China) | Ovarian cancer | NMPA | intravenously guttae | [103] |
| DepoDur™ | 2004 | Morphine Sulfate | SkyPharm Inc. (San Diego, CA, USA) | Pain management | FDA | Epidural | [68] |
| Mepact® | 2009 | Mifamurtide | Elan Pharmaceuticals (San Diego, CA, USA) | Non-metastatic osteosarcoma | EMA | intravenous | [47,104] |
| Exparel® | 2011 | Bupivacaine | Pacira BioSciences (San Diego, CA, USA) | Pain management | FDA | intravenous | [105] |
| Marqibo® | 2012 | Vincristine | Talon Therapeutics (San Francisco, CA, USA) | ALL | FDA | intravenous | [44] |
| Onivyde™ | 2015 | Irinotecan | Merrimack Pharmaceuticals (Cambridge, UK) | Metastatic pancreatic cancer | FDA | intravenous | [46,106] |
| Vyxeos® | 2017 | Daunorubicin and Cytarabine | Jazz Pharmaceuticals (San Francisco, CA, USA) | AML-MRC and t-AML | FDA | intravenous | [41,42] |
| Shingrix® | 2017 | Recombinant VZV glycoprotein E | Glaxo Smith Kline (Middlesex, UK) | Against shingles and post-herpetic neuralgia | FDA | intramuscular | [107,108] |
| Onpattro™ | 2018 | siRNA | Alnylam (Cambridge, MA, USA) | Polyneuropathy caused by hATTR | FDA | intravenous | [82,109,110] |
| Arikayce® Kit | 2018 | Amikacin | Insmed (Glen Allen, VA, USA) | NTM lung disease caused by MAC | FDA | inhalation administration | [111,112] |
| Mosquirix® | 2021 | Recombinant CSP | Glaxo Smith Kline (Middlesex, UK) | Malaria | EMA | intramuscular | [59] |
| Comirnaty® | 2021 | BNT162b2 | Pfizer (New York, NY, USA) and BioNTech (Mainz, Germany) | COVID-19 | FDA | intramuscular | [113] |
| mRNA-1273 | 2021 | mRNA-1273 | Moderna (Cambridge, MA, USA) | COVID-19 | FDA | intramuscular | [114] |
3. Drug Nanocrystals (NCs)
3.1. NCs against CVDs
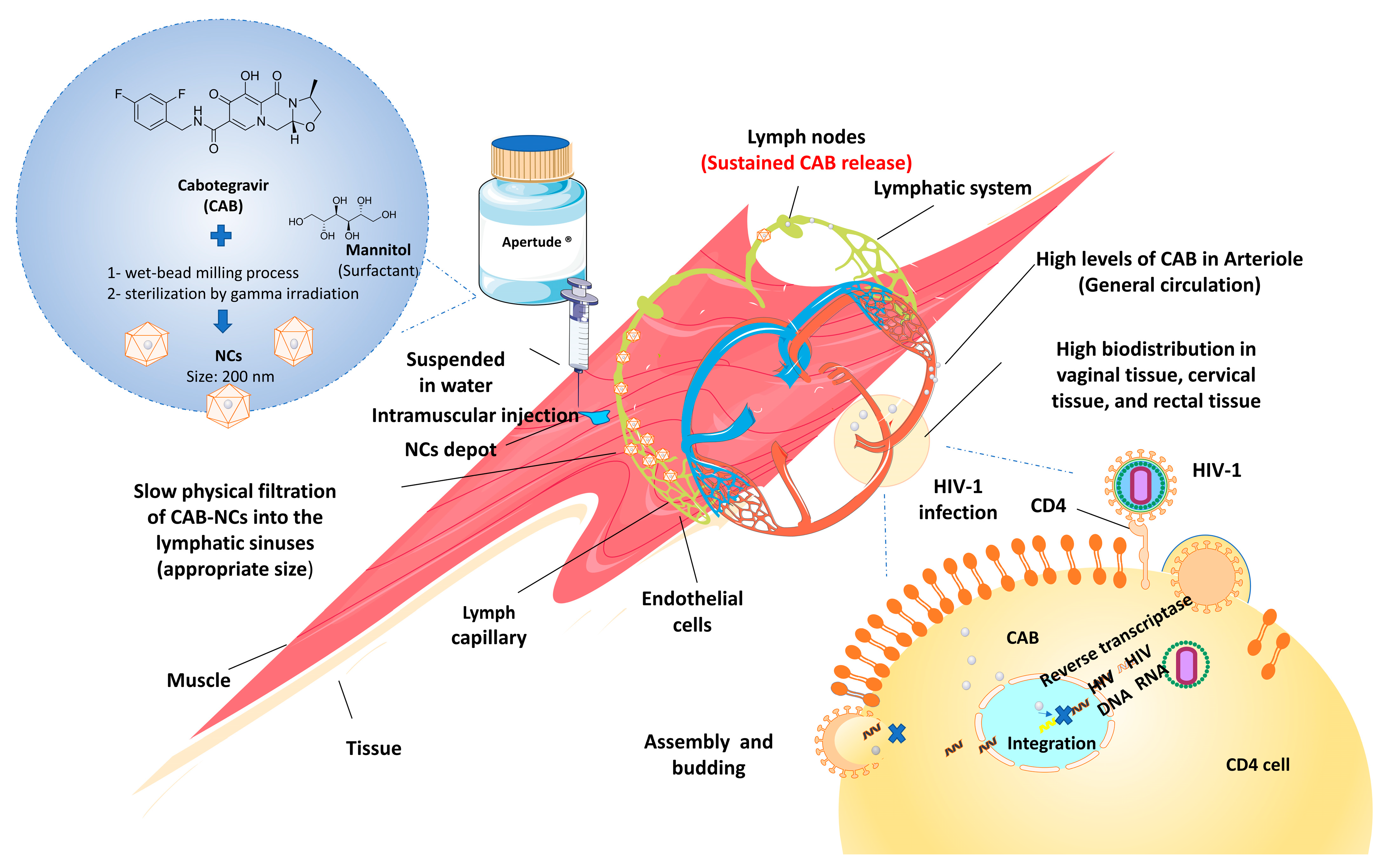
3.2. NCs against Infection
3.3. NCs for Psychosis and Other Disease Treatment
| Trade Name | Approval Year | Drug Agent | Company | Clinical Applications | Administration Route | Agency | Ref. |
|---|---|---|---|---|---|---|---|
| Gris-PEG® | 1998 | Griseofulvin | Recro Gainesville LLC (Gainesville, FL, USA) | Ringworm infections | Oral | FDA | [134] |
| Rapamune® | 2000 | Rapamycin/sirolimus | Wyeth (Philadelphia, PA, USA) | Immunosuppressive therapy in renal transplantation | Oral | FDA | [141] |
| Avinza® | 2002 | Morphine sulfate | King Pharma (Bristol, TN, USA) | Chronic pain | Oral | FDA | [145] |
| Ritalin LA® | 2002 | Methylphenidate hydrochloride | Novartis Novartis (Basel, Switzerland) | Attention-deficit-hyperactivity disorder | Oral | FDA | [146] |
| Emend® | 2003 | Aprepitant | Merck (Rahway, NJ, USA) | Chemotherapy-induced nausea and vomiting | Oral | FDA | [147] |
| Tricor® | 2004 | Fenofibrate | Abbott (North Chicago, IL, USA) | Hypercholesterolemia | Oral | FDA | [124] |
| Triglide® | 2005 | Fenofibrate | Skye Pharma (San Diego, CA, USA) | Hypercholesterolemia | Oral | FDA | [131] |
| Megace®ES | 2005 | Megestrol acetate | Par Pharma (Petaluma, CA, USA) | Anorexia | Oral | FDA | [142] |
| Naprelan® | 2006 | Naproxen sodium | Wyeth (Philadelphia, PA, USA) | Inflammation | Oral | FDA | [148] |
| Cesamet® | 2009 | Nabilone | Lilly (Indianapolis, IN, USA) | Nausea and vomiting | Oral | FDA | [149] |
| Invega Sustenna® | 2009 | Paliperidone palmitate | Janssen Pharmaceuticals Inc. (Titusville, NJ, USA) | Schizophrenia | Intramuscular | FDA | [150] |
| Invega Trinza® | 2015 | Paliperidone palmitate | Janssen Pharmaceuticals Inc. (Titusville, NJ, USA) | Schizophrenia | Intramuscular | FDA | [151] |
| Aristada Initio® | 2018 | Aripiprazole lauroxil | Alkermes Inc (Waltham, MA, USA) | Schizophrenia | Intramuscular | FDA | [152] |
| Invega Hafyera® | 2021 | Paliperidone palmitate | Janssen Pharmaceuticals Inc. (Titusville, NJ, USA) | Schizophrenia | Intramuscular | FDA | [144] |
| Cabenuva® | 2021 | Cabotegravir | Viiv Healthcare Co. (Brentford, London, UK) | HIV-1 infection | Gluteal intramuscular | FDA | [139] |
| Apretude® | 2021 | Cabotegravir | Viiv Healthcare Co. (Brentford, London, UK) | HIV-1 infection | Gluteal intramuscular | FDA | [140] |
4. Polymeric Nanoparticles
4.1. Polymeric Micelles for Cancer Treatment
4.2. Polymeric Nanoparticles for Cancer Treatment
4.3. Dendrimer-Based Nanoparticles against Infection
| Trade Name | Approval Year | Drug Agent | Company | Clinical Applications | Administration Route | Agency | Ref. |
|---|---|---|---|---|---|---|---|
| Genexol® PM | 2007 | PTX | Samyang Pharmaceuticals (Seoul, Republic of Korea) | MBC, NSCLC, and ovarian cancer | Intravenous | MFDS, PDH, CDSCO and DAV | [175] |
| Nanoxel® M | 2012 | Docetaxel | Samyang Pharmaceuticals (Seoul, Republic of Korea) | MBC, NSCLC, and ovarian cancer | Intravenous | MFDS | [178] |
| Paclical® | 2015 | PTX | Oasmia Pharmaceuticals (Uppsala, Sweden) | Ovarian cancer | Intravenous | RFMPH | [180] |
| Abraxane® | 2005 | PTX | Abraxis Bioscience, (Los Angeles, CA, USA) | Pancreatic cancer and MBC | Intravenous | FDA | [187] |
5. Other Nanomedicines for Disease Treatment
| Trade Name | Approval Year | Formulation Type | Drug Agent | Company | Clinical Applications | Administration Route | Agency | Ref. |
|---|---|---|---|---|---|---|---|---|
| Ontak® | 1999 | Protein-based formulation | Denileukin diftitox | Eisai (Norcross, GA, USA) | Cutaneous T-cell lymphoma therapy | Intravenous | FDA | [212] |
| Oncaspar® | 1994 | Pegylated enzyme | L-asparaginase | Enzon Pharmaceuticals (Cranford, NJ, USA); Baxter BioScience (Deerfield, IL, USA) | Acute lymphocytic leukemia | Intravenous | FDA | [217] |
| Restasis® | 2002 | Nanoemulsions | Cyclosporin | Allergan (Lansing, MI, USA) | Severe keratitis in dry eye patient | Topical | FDA | [216] |
| Feraheme™ | 2009 | Semi-synthetic iron oxide nanoparticles | Iron oxide particles | AMAG Pharmaceuticals (Waltham, MA, USA) | Anemia related to chronic kidney disease (CKD) | Intravenous | FDA | [218] |
| Injectafer® | 2013 | Iron nanoparticles | Polynuclear iron (III) oxyhydroxide iron particles | For Int. (Waltham, MA, USA) | Iron deficiency anemia | Oral | FDA | [219] |
| Monofer® | 2010 | Iron nanoparticles | Iron molecule with unbranched carbohydrate iron particles | Pharmacosmos (Rorvangsvej, Holbæk, Denmark) | Iron deficiency anemia | Oral | EMA/FDA | [220] |
| Mircera® | 2007 | Polymer-protein conjugate | Methoxy polyethylene glycol-epoetin beta | Hoffman-LaRoche (Basel, Switzerland) | CKD associated anemia | Intravenous | FDA | [221] |
| Adynovate® | 2015 | Polymer-protein conjugate | Recombinant anti-hemophilic factor VIII | Baxalta (Montgomery, AL, USA) | Hemophilia A | Intravenous | FDA | [222] |
| Neulasta® | 2002 | Polymer-protein conjugate | Recombinant human granulocyte-colony stimulating factor (G-CSF) | Amgen (Thousand Oaks, CA, USA) | Febrile neutropenia | Intravenous | FDA | [223] |
| Pegasys® | 2002 | Pegylated nanoparticles | Interferon alfa-2a | Genentech biotechnology (San Francisco, AL, USA) | Hepatitis B and C therapy | Intravenous | FDA | [224] |
| Pegintron® | 2001 | Pegylated nanoparticles | Interferon alfa-2b | Merck (Rahway, NJ, USA) | Hepatitis C | Intravenous | FDA | [225] |
| Copaxone® | 1996 | Polypeptide colloidal formulation | Glatiramer acetate | Teva Pharmaceuticals (Marietta, GA, USA) | Relapsing or remitting type of multiple sclerosis | Intravenous | FDA | [226] |
| Estrasorb® | 2003 | Emulsion | Estradiol | Novavax (Lutherville Timonium, MD, USA) | Estrogen therapy | Topical | FDA | [227] |
| Nanocoll® | 1995 | Albumin-based radiopharmaceutical nanocolloid | Albumin and stannous | GE Healthcare (Raleigh, NC, USA) | Breast cancer and also melanoma | Intravenous | FDA | [228] |
| Nanocis® | 2000 | Radiopharmaceutical colloid | Chloride dehydrates Radiopharmaceutical colloid | CIS Bio (Berlin, Germany) | As inflammation scintigraphy, bone marrow scintigraphy, and by cutaneous route for lymphatic scintigraphy | Intravenous | FDA | [229] |
6. Conclusions and Perspectives
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Shapiro, R.S. COVID-19 vaccines and nanomedicine. Int. J. Dermatol. 2021, 60, 1047–1052. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Mageed, H.M.; AbuelEzz, N.Z.; Radwan, R.A.; Mohamed, S.A. Nanoparticles in nanomedicine: A comprehensive updated review on current status, challenges and emerging opportunities. J. Microencapsul. 2021, 38, 414–436. [Google Scholar] [CrossRef] [PubMed]
- Dash, S.; Das, T.; Patel, P.; Panda, P.K.; Suar, M.; Verma, S.K. Emerging trends in the nanomedicine applications of functionalized magnetic nanoparticles as novel therapies for acute and chronic diseases. J. Nanobiotechnol. 2022, 20, 393. [Google Scholar] [CrossRef]
- Li, B.; Teng, C.; Yu, H.; Jiang, X.; Xing, X.; Jiang, Q.; Lin, C.; Zhao, Z.; Zhang, R.; He, W. Alleviating experimental pulmonary hypertension via co-delivering FoxO1 stimulus and apoptosis activator to hyperproliferating pulmonary arteries. Acta Pharm. Sin. B, 2022; in press. [Google Scholar] [CrossRef]
- Phung, C.D.; Nguyen, B.L.; Jeong, J.H.; Chang, J.H.; Jin, S.G.; Choi, H.G.; Ku, S.K.; Kim, J.O. Shaping the “hot” immunogenic tumor microenvironment by nanoparticles co-delivering oncolytic peptide and TGF-β1 siRNA for boosting checkpoint blockade therapy. Bioeng. Transl. Med. 2022, e10392. [Google Scholar] [CrossRef]
- He, W.; Xing, X.; Wang, X.; Wu, D.; Wu, W.; Guo, J.; Mitragotri, S. Nanocarrier-Mediated Cytosolic Delivery of Biopharmaceuticals. Adv. Funct. Mater. 2020, 30, 1910566. [Google Scholar] [CrossRef]
- Zoulikha, M.; He, W. Targeted Drug Delivery for Chronic Lymphocytic Leukemia. Pharm. Res. 2022, 39, 441–461. [Google Scholar] [CrossRef]
- Li, Z.; Shan, X.; Chen, Z.; Gao, N.; Zeng, W.; Zeng, X.; Mei, L. Applications of surface modification technologies in nanomedicine for deep tumor penetration. Adv. Sci. 2021, 8, 2002589. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, M.; Gao, X.; Chen, Y.; Liu, T. Nanotechnology in cancer diagnosis: Progress, challenges and opportunities. J. Hematol. Oncol. 2019, 12, 137. [Google Scholar] [CrossRef] [Green Version]
- Chandarana, M.; Curtis, A.; Hoskins, C. The use of nanotechnology in cardiovascular disease. Appl. Nanosci. 2018, 8, 1607–1619. [Google Scholar] [CrossRef] [Green Version]
- Poudel, K.; Nam, K.S.; Lim, J.; Ku, S.K.; Hwang, J.; Kim, J.O.; Byeon, J.H. Modified Aerotaxy for the Plug-in Manufacture of Cell-Penetrating Fenton Nanoagents for Reinforcing Chemodynamic Cancer Therapy. ACS Nano 2022, 16, 19423–19438. [Google Scholar] [CrossRef] [PubMed]
- Poudel, K.; Banstola, A.; Gautam, M.; Soe, Z.C.; Jeong, J.-H.; Choi, H.-G.; Ku, S.K.; Yong, C.S.; Tran, T.H.; Kim, J.O. Redox/photo dual-responsive, self-targeted, and photosensitizer-laden bismuth sulfide nanourchins for combination therapy in cancer. Nanoscale 2021, 13, 1231–1247. [Google Scholar] [CrossRef] [PubMed]
- Poudel, K.; Banstola, A.; Tran, T.H.; Thapa, R.K.; Gautam, M.; Ou, W.; Maharjan, S.; Jeong, J.-H.; Ku, S.K.; Choi, H.-G. Hyaluronic acid wreathed, trio-stimuli receptive and on-demand triggerable nanoconstruct for anchored combinatorial cancer therapy. Carbohydr. Polym. 2020, 249, 116815. [Google Scholar] [CrossRef]
- Anselmo, A.C.; Mitragotri, S. Nanoparticles in the clinic: An update. Bioeng. Transl. Med. 2019, 4, e10143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Germain, M.; Caputo, F.; Metcalfe, S.; Tosi, G.; Spring, K.; Åslund, A.K.; Pottier, A.; Schiffelers, R.; Ceccaldi, A.; Schmid, R. Delivering the power of nanomedicine to patients today. J. Control. Release 2020, 326, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Weissig, V.; Elbayoumi, T.; Flühmann, B.; Barton, A. The growing field of nanomedicine and its relevance to pharmacy curricula. Am. J. Pharm. Educ. 2021, 85, 8331. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Idris, R.A.M.; Wan Hanaffi, W.N.; Perumal, K.; Boer, J.C.; Plebanski, M.; Jaafar, J.; Lim, J.K.; Mohamud, R. Cancer nanomedicine and immune system—Interactions and challenges. Front. Nanotechnol. 2021, 3, 681305. [Google Scholar] [CrossRef]
- van der Meel, R.; Sulheim, E.; Shi, Y.; Kiessling, F.; Mulder, W.J.; Lammers, T. Smart cancer nanomedicine. Nat. Nanotechnol. 2019, 14, 1007–1017. [Google Scholar] [CrossRef]
- Zhang, C.; Yan, L.; Wang, X.; Zhu, S.; Chen, C.; Gu, Z.; Zhao, Y. Progress, challenges, and future of nanomedicine. Nano Today 2020, 35, 101008. [Google Scholar] [CrossRef]
- Xiang, H.; Xu, S.; Li, J.; Li, Y.; Xue, X.; Liu, Y.; Li, J.; Miao, X. Functional drug nanocrystals for cancer-target delivery. J. Drug Deliv. Sci. Technol. 2022, 76, 103807. [Google Scholar] [CrossRef]
- Desai, P.P.; Rustomjee, M.T. Business potential of advanced drug delivery systems. Confocal Microsc. 2018, 23, 29. [Google Scholar]
- Wang, L.; Xu, H.; Weng, L.; Sun, J.; Jin, Y.; Xiao, C. Activation of cancer immunotherapy by nanomedicine. Front. Pharmcol. 2022, 13, 1041073. [Google Scholar] [CrossRef] [PubMed]
- Al-Zoubi, M.S.; Al-Zoubi, R.M. Nanomedicine tactics in cancer treatment: Challenge and hope. Crit. Rev. Oncol. Hematol. 2022, 174, 103677. [Google Scholar] [CrossRef] [PubMed]
- Zhao, B.; Chen, S.; Hong, Y.; Jia, L.; Zhou, Y.; He, X.; Wang, Y.; Tian, Z.; Yang, Z.; Gao, D. Research Progress of Conjugated Nanomedicine for Cancer Treatment. Pharmaceutics 2022, 14, 1522. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Du, C.; Guo, N.; Teng, Y.; Meng, X.; Sun, H.; Li, S.; Yu, P.; Galons, H. Composition design and medical application of liposomes. Eur. J. Med. Chem. 2019, 164, 640–653. [Google Scholar] [CrossRef]
- Kurano, T.; Kanazawa, T.; Ooba, A.; Masuyama, Y.; Maruhana, N.; Yamada, M.; Iioka, S.; Ibaraki, H.; Kosuge, Y.; Kondo, H. Nose-to-brain/spinal cord delivery kinetics of liposomes with different surface properties. J. Control. Release 2022, 344, 225–234. [Google Scholar] [CrossRef]
- Barros, C.d.; Aranha, N.; Severino, P.; Souto, E.B.; Zielińska, A.; Lopes, A.; Rios, A.; Batain, F.; Crescencio, K.; Chaud, M. Quality by design approach for the development of liposome carrying ghrelin for intranasal administration. Pharmaceutics 2021, 13, 686. [Google Scholar] [CrossRef]
- Barenholz, Y. Doxil(R)—the first FDA-approved nano-drug: Lessons learned. J. Control. Release 2012, 160, 117–134. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Xiao, Q.; Li, X.; Liu, C.; Yang, Y.; Hou, Y.; Wang, Y.; Su, M.; He, W. Liposome-based anchoring and core-encapsulation for combinatorial cancer therapy. Chin. Chem. Lett. 2022, 33, 4191–4196. [Google Scholar] [CrossRef]
- Du, X.; Hou, Y.; Huang, J.; Pang, Y.; Ruan, C.; Wu, W.; Xu, C.; Zhang, H.; Yin, L.; He, W. Cytosolic delivery of the immunological adjuvant Poly I: C and cytotoxic drug crystals via a carrier-free strategy significantly amplifies immune response. Acta Pharm. Sin. B 2021, 11, 3272–3285. [Google Scholar] [CrossRef] [PubMed]
- Ashrafizadeh, M.; Saebfar, H.; Gholami, M.H.; Hushmandi, K.; Zabolian, A.; Bikarannejad, P.; Hashemi, M.; Daneshi, S.; Mirzaei, S.; Sharifi, E. Doxorubicin-loaded graphene oxide nanocomposites in cancer medicine: Stimuli-responsive carriers, co-delivery and suppressing resistance. Expert Opin. Drug Deliv. 2022, 19, 355–382. [Google Scholar] [CrossRef] [PubMed]
- Rizzardini, G.; Pastecchia, C.; Vigevani, G.M.; Milella, A.M.; Cremoni, L.; Milazzo, F. Stealth liposomal doxorubicin or bleomycin/vincristine for the treatment of AIDS-related Kaposi’s sarcoma. J. Acquir. Immune Defic. Syndr. 1997, 14, 17. [Google Scholar]
- Neale, M.H.; Lamont, A.; Hindley, A.; Kurbacher, C.M.; Cree, I.A. The ex vivo effect of high concentrations of doxorubicin on recurrent ovarian carcinoma. Anticancer Drugs 2000, 11, 865–871. [Google Scholar] [CrossRef]
- Working, P.K.; Dayan, A.D. Pharmacological-toxicological expert report—Caelyx(TM)—(Stealth(R) liposomal doxorubicin HCl)—Foreword. Hum. Exp. Toxicol. 1996, 15, 751–785. [Google Scholar]
- Minamisakamoto, T.; Nishiguchi, S.; Hashimoto, K.; Og.gawara, K.-i.; Maruyama, M.; Higaki, K. Sequential administration of PEG-Span 80 niosome enhances anti-tumor effect of doxorubicin-containing PEG liposome. Eur. J. Pharm. Biopharm. 2021, 169, 20–28. [Google Scholar] [CrossRef]
- Gabizon, A.; Isacson, R.; Libson, E.; Kaufman, B.; Uziely, B.; Catane, R.; Ben-Dor, C.G.; Rabello, E.; Cass, Y.; Peretz, T.; et al. Clinical studies of liposome-encapsulated doxorubicin. Acta Oncol. 1994, 33, 779–786. [Google Scholar] [CrossRef]
- Hu, X.; Dong, M.; Liang, X.; Liu, Z.; Li, Q. Reactive oxygen species-mediated inflammation and apoptosis in hand-foot syndrome induced by PEGylated liposomal doxorubicin. Int. J. Nanomed. 2021, 16, 471. [Google Scholar] [CrossRef]
- Satapathy, S.R.; Sahoo, R.N. Conventional treatments and non-PEGylated liposome encapsulated doxorubicin for visceral leishmaniasis: A scoping review. Asian Pac. J. Trop. Med. 2022, 15, 293. [Google Scholar]
- Boafo, G.F.; Shi, Y.; Xiao, Q.; Magar, K.T.; Zoulikha, M.; Xing, X.; Teng, C.; Brobbey, E.; Li, X.; Jiang, X. Targeted co-delivery of daunorubicin and cytarabine based on the hyaluronic acid prodrug modified liposomes. Chin. Chem. Lett. 2022, 33, 4600–4604. [Google Scholar] [CrossRef]
- Krauss, A.C.; Gao, X.; Li, L.; Manning, M.L.; Patel, P.; Fu, W.; Janoria, K.G.; Gieser, G.; Bateman, D.A.; Przepiorka, D.; et al. FDA Approval Summary: (Daunorubicin and Cytarabine) Liposome for Injection for the Treatment of Adults with High-Risk Acute Myeloid Leukemia. Clin. Cancer Res. 2019, 25, 2685–2690. [Google Scholar] [CrossRef] [PubMed]
- Alfayez, M.; Kantarjian, H.; Kadia, T.; Ravandi-Kashani, F.; Daver, N. CPX-351 (vyxeos) in AML. Leuk. Lymphoma 2020, 61, 288–297. [Google Scholar] [CrossRef] [PubMed]
- Crommelin, D.J.A.; van Hoogevest, P.; Storm, G. The role of liposomes in clinical nanomedicine development. What now? Now what? J. Control. Release 2020, 318, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Schiller, G.J.; Damon, L.E.; Stock, W.; Coutre, S.E.; Hsu, P.; Prasad, L.; Douer, D. Marqibo (R), Vincristine Sulfate Liposome Injection, for the Treatment of Advanced, Relapsed or Refractory Philadelphia Chromosome-Negative (Ph-) Acute Lymphoblastic Leukemia (ALL) in an Adolescent Young Adult (AYA) Population. Blood 2015, 126, 1291. [Google Scholar] [CrossRef]
- Murry, D.J.; Blaney, S.M. Clinical pharmacology of encapsulated sustained-release cytarabine. Ann. Pharmacother. 2000, 34, 1173–1178. [Google Scholar] [CrossRef] [PubMed]
- Drummond, D.C.; Noble, C.O.; Guo, Z.; Hong, K.; Park, J.W.; Kirpotin, D.B. Development of a highly active nanoliposomal irinotecan using a novel intraliposomal stabilization strategy. Cancer Res. 2006, 66, 3271–3277. [Google Scholar] [CrossRef] [Green Version]
- Zarkovic, M.; Qin, X.; Nakatsuru, Y.; Zhang, S.; Yamazaki, Y.; Oda, H.; Ishikawa, T.; Ishikawa, T. Inhibitory effect of probucol on benzo [a]pyrene induced lung tumorigenesis. Carcinogenesis 1995, 16, 2599–2601. [Google Scholar] [CrossRef]
- Xiaohui, L. New progress and clinical application of anti-infective drugs. Prog. Pharm. Sci. 2021, 45, 401–402. [Google Scholar]
- Wang, X.; Mohammad, I.S.; Fan, L.; Zhao, Z.; Nurunnabi, M.; Sallam, M.A.; Wu, J.; Chen, Z.; Yin, L.; He, W. Delivery strategies of amphotericin B for invasive fungal infections. Acta Pharm. Sin. B 2021, 11, 2585–2604. [Google Scholar] [CrossRef]
- Desjeux, P.; Piot, B.; O’Neill, K.; Meert, J.P. Co-infections of leishmania/HIV in south Europe. Med. Trop. (Mars) 2001, 61, 187–193. [Google Scholar]
- Minodier, P.; Piarroux, R.; Garnier, J.M.; Unal, D.; Perrimond, H.; Dumon, H. Pediatric visceral leishmaniasis in southern France. Pediatr. Infect. Dis. J. 1998, 17, 701–704. [Google Scholar] [CrossRef]
- Silva-Carvalho, R.; Leão, T.; Gama, F.M.; Tomás, A.M. Covalent Conjugation of Amphotericin B to Hyaluronic Acid: An Injectable Water-Soluble Conjugate with Reduced Toxicity and Anti-Leishmanial Potential. Biomacromolecules 2022, 23, 1169–1182. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, S.M.; Khafagy, E.-S.; Riadi, Y.; Al Saqr, A.; Alfadhel, M.M.; Hegazy, W.A. Amphotericin B-PEG Conjugates of ZnO Nanoparticles: Enhancement Antifungal Activity with Minimal Toxicity. Pharmaceutics 2022, 14, 1646. [Google Scholar] [CrossRef] [PubMed]
- Janoff, A.S.; Boni, L.T.; Popescu, M.C.; Minchey, S.R.; Cullis, P.R.; Madden, T.D.; Taraschi, T.; Gruner, S.M.; Shyamsunder, E.; Tate, M.W.; et al. Unusual lipid structures selectively reduce the toxicity of amphotericin B. Proc. Natl. Acad. Sci. USA 1988, 85, 6122–6126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adler-Moore, J.; Proffitt, R.T. AmBisome: Liposomal formulation, structure, mechanism of action and pre-clinical experience. J. Antimicrob. Chemother. 2002, 49, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Lister, J. Amphotericin B Lipid Complex (Abelcet) in the treatment of invasive mycoses: The North American experience. Eur. J. Haematol. 1996, 57, 18–23. [Google Scholar] [CrossRef]
- Kunzi, V.; Dornseiff, M.; Horwath, J.; Hartmann, K. Safe vaccination of children with a virosomal adjuvanted influenza vaccine. Vaccine 2009, 27, 1261–1265. [Google Scholar] [CrossRef] [PubMed]
- Kanra, G.; Marchisio, P.; Feiterna-Sperling, C.; Gaedicke, G.; Lazar, H.; Durrer, P.; Kürsteiner, O.; Herzog, C.; Kara, A.; Principi, N. Comparison of immunogenicity and tolerability of a virosome-adjuvanted and a split influenza vaccine in children. Pediatr. Infect. Dis. J. 2004, 23, 300–306. [Google Scholar] [CrossRef]
- Nadeem, A.Y.; Shehzad, A.; Islam, S.U.; Al-Suhaimi, E.A.; Lee, Y.S. Mosquirix RTS, S/AS01 Vaccine Development, Immunogenicity, and Efficacy. Vaccines 2022, 10, 713. [Google Scholar] [CrossRef]
- Li, Z.; Perkins, W.; Cipolla, D. Robustness of aerosol delivery of amikacin liposome inhalation suspension using the eFlow® Technology. Eur. J. Pharm. Biopharm. 2021, 166, 10–18. [Google Scholar] [CrossRef]
- Wendt, S.; Ranft, D.; de With, K.; Kern, W.V.; Salzberger, B.; Lubbert, C. Antibiotic stewardship (ABS). Part 2: Application. Internist 2020, 61, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Aplin, C.; Milano, S.K.; Zielinski, K.A.; Pollack, L.; Cerione, R.A. Evolving Experimental Techniques for Structure-Based Drug Design. J. Phys. Chem. B 2022, 126, 6599–6607. [Google Scholar] [CrossRef] [PubMed]
- Kothari, V. Discovery and Development of New Anti-infectives: Perspectives and Prospective. Curr. Drug Discov. Technol. 2020, 17, 414. [Google Scholar] [CrossRef] [PubMed]
- Waddimba, A.C.; Newman, P.; Shelley, J.K.; McShan, E.E.; Cheung, Z.-O.; Gibson, J.N.; Bennett, M.M.; Petrey, L.B. Pain management after laparoscopic appendectomy: Comparative effectiveness of innovative pre-emptive analgesia using liposomal bupivacaine. Am. J. Surg. 2022, 223, 832–838. [Google Scholar] [CrossRef] [PubMed]
- Ke, P.; Qin, Y.; Shao, Y.; Han, M.; Jin, Z.; Zhou, Y.; Zhong, H.; Lu, Y.; Wu, X.; Zeng, K. Preparation and evaluation of liposome with ropivacaine ion-pairing in local pain management. Drug Dev. Ind. Pharm. 2022, 48, 255–264. [Google Scholar] [CrossRef]
- Cheng, X.; Gao, J.; Ding, Y.; Lu, Y.; Wei, Q.; Cui, D.; Fan, J.; Li, X.; Zhu, E.; Lu, Y. Multi-Functional Liposome: A Powerful Theranostic Nano-Platform Enhancing Photodynamic Therapy. Adv. Sci. 2021, 8, 2100876. [Google Scholar] [CrossRef]
- Horlocker, T.T.; Wedel, D.J.; Benzon, H.; Brown, D.L.; Enneking, F.K.; Heit, J.A.; Mulroy, M.F.; Rosenquist, R.W.; Rowlingson, J.; Tryba, M.; et al. Regional anesthesia in the anticoagulated patient: Defining the risks (the second ASRA Consensus Conference on Neuraxial Anesthesia and Anticoagulation). Reg. Anesth. Pain Med. 2003, 28, 172–197. [Google Scholar] [CrossRef]
- Pasero, C.; McCaffery, M. Extended-release epidural morphine (DepoDur). J. Perianesth. Nurs. 2005, 20, 345–350. [Google Scholar] [CrossRef]
- Malik, O.; Kaye, A.D.; Kaye, A.; Belani, K.; Urman, R.D. Emerging roles of liposomal bupivacaine in anesthesia practice. J. Anaesthesiol. Clin. Pharmcol. 2017, 33, 151–156. [Google Scholar]
- Tong, Y.C.; Kaye, A.D.; Urman, R.D. Liposomal bupivacaine and clinical outcomes. Best Pract. Res. Clin. Anaesthesiol. 2014, 28, 15–27. [Google Scholar] [CrossRef]
- Xiao, Q.; Li, X.; Liu, C.; Jiang, Y.; He, Y.; Zhang, W.; Azevedo, H.S.; Wu, W.; Xia, Y.; He, W. Improving cancer immunotherapy via co-delivering checkpoint blockade and thrombospondin-1 downregulator. Acta Pharm. Sin. B, 2022; in press. [Google Scholar] [CrossRef]
- Li, X.; Gu, J.; Xiao, Q.; Liu, Y.; Zhou, P.; Fan, L.; Zhang, X.; Lu, X.; Wu, J.; Liu, Z. Liposomal codelivery of inflammation inhibitor and collagen protector to the plaque for effective anti-atherosclerosis. Chin. Chem. Lett. 2023, 34, 107483. [Google Scholar] [CrossRef]
- Magar, K.T.; Boafo, G.F.; Li, X.; Chen, Z.; He, W. Liposome-based delivery of biological drugs. Chin. Chem. Lett. 2022, 33, 587–596. [Google Scholar] [CrossRef]
- Sirks, M.J.; van Dijk, E.H.; Rosenberg, N.; Hollak, C.E.; Aslanis, S.; Cheung, C.M.G.; Chowers, I.; Eandi, C.M.; Freund, K.B.; Holz, F.G. Clinical impact of the worldwide shortage of verteporfin (Visudyne®) on ophthalmic care. Acta Ophthalmol. 2022, 100, e1522–e1532. [Google Scholar] [CrossRef] [PubMed]
- Bakri, S.J.; Kaiser, P.K. Verteporfin ocular photodynamic therapy. Expert Opin. Pharmcother. 2004, 5, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Kiaie, S.H.; Majidi Zolbanin, N.; Ahmadi, A.; Bagherifar, R.; Valizadeh, H.; Kashanchi, F.; Jafari, R. Recent advances in mRNA-LNP therapeutics: Immunological and pharmacological aspects. J. Nanobiotechnol. 2022, 20, 276. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Jiang, Y.; He, Y.; Boucetta, H.; Wu, J.; Chen, Z.; He, W. Lipid carriers for mRNA delivery. Acta Pharm. Sin. B, 2022; in press. [Google Scholar] [CrossRef]
- He, Y.; Zhang, W.; Xiao, Q.; Fan, L.; Huang, D.; Chen, W.; He, W. Liposomes and liposome-like nanoparticles: From anti-fungal infection to the COVID-19 pandemic treatment. Asian J. Pharm. Sci. 2022, 17, 817–837. [Google Scholar] [CrossRef]
- Huang, H.-Y. mRNA vaccine delivery system based on liposome:research advances. J. Int. Pharm. Res. 2019, 46, 339–346. [Google Scholar]
- Zuo, Q.; Xiong, W. Progress of mRNA vaccine delivery system based on non-viral vector. Sichuan J. Physiol. Sci. 2020, 42, 370–374. [Google Scholar]
- Sahay, G.; Querbes, W.; Alabi, C.; Eltoukhy, A.; Sarkar, S.; Zurenko, C.; Karagiannis, E.; Love, K.; Chen, D.; Zoncu, R.; et al. Efficiency of siRNA delivery by lipid nanoparticles is limited by endocytic recycling. Nat. Biotechnol. 2013, 31, 653–658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Urits, I.; Swanson, D.; Swett, M.C.; Patel, A.; Berardino, K.; Amgalan, A.; Berger, A.A.; Kassem, H.; Kaye, A.D.; Viswanath, O. Correction to: A Review of Patisiran (ONPATTRO(R)) for the Treatment of Polyneuropathy in People with Hereditary Transthyretin Amyloidosis. Neurol. Ther. 2021, 10, 407. [Google Scholar] [CrossRef]
- Setten, R.L.; Rossi, J.J.; Han, S.P. The current state and future directions of RNAi-based therapeutics. Nat. Rev. Drug Discov. 2019, 18, 421–446. [Google Scholar] [CrossRef] [PubMed]
- Piperno, A.; Sciortino, M.T.; Giusto, E.; Montesi, M.; Panseri, S.; Scala, A. Recent advances and challenges in gene delivery mediated by polyester-based nanoparticles. Int. J. Nanomed. 2021, 16, 5981. [Google Scholar] [CrossRef] [PubMed]
- Rahmati, Z.; Roushani, M.; Hosseini, H.; Choobin, H. An electrochemical immunosensor using SARS-CoV-2 spike protein-nickel hydroxide nanoparticles bio-conjugate modified SPCE for ultrasensitive detection of SARS-CoV-2 antibodies. Microchem. J. 2021, 170, 106718. [Google Scholar] [CrossRef]
- Choi, J.; Poudel, K.; Nam, K.S.; Piri, A.; Rivera–Piza, A.; Ku, S.K.; Hwang, J.; Kim, J.O.; Byeon, J.H. Aero-manufacture of nanobulges for an in-place anticoronaviral on air filters. J. Hazard. Mater. 2023, 445, 130458. [Google Scholar] [CrossRef]
- Tenchov, R.; Bird, R.; Curtze, A.E.; Zhou, Q. Lipid Nanoparticles-From Liposomes to mRNA Vaccine Delivery, a Landscape of Research Diversity and Advancement. ACS Nano 2021, 15, 16982–17015. [Google Scholar] [CrossRef]
- Paramasivam, P.; Franke, C.; Stöter, M.; Höijer, A.; Bartesaghi, S.; Sabirsh, A.; Lindfors, L.; Arteta, M.Y.; Dahlén, A.; Bak, A.; et al. Endosomal escape of delivered mRNA from endosomal recycling tubules visualized at the nanoscale. J. Cell Biol. 2022, 221, e202110137. [Google Scholar] [CrossRef]
- Shang, H.; Feng, X.; Xu, P.; Wang, Y.; Fu, H.; Li, Y. Research development of mRNA vaccine delivery based on lipid carrier. Drug Eval. Res. 2021, 44, 869–875. [Google Scholar]
- Corbett, K.S.; Flynn, B.; Foulds, K.E.; Francica, J.R.; Boyoglu-Barnum, S.; Werner, A.P.; Flach, B.; O’Connell, S.; Bock, K.W.; Minai, M.; et al. Evaluation of the mRNA-1273 Vaccine against SARS-CoV-2 in Nonhuman Primates. N. Engl. J. Med. 2020, 383, 1544–1555. [Google Scholar] [CrossRef]
- Mulligan, M.J.; Lyke, K.E.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Neuzil, K.; Raabe, V.; Bailey, R.; Swanson, K.A.; et al. Phase I/II study of COVID-19 RNA vaccine BNT162b1 in adults. Nature 2020, 586, 589–593. [Google Scholar] [CrossRef] [PubMed]
- Allen, T.M.; Cullis, P.R. Liposomal drug delivery systems: From concept to clinical applications. Adv. Drug Deliv. Rev. 2013, 65, 36–48. [Google Scholar] [CrossRef] [PubMed]
- Stone, N.R.; Bicanic, T.; Salim, R.; Hope, W. Liposomal Amphotericin B (AmBisome((R))): A Review of the Pharmacokinetics, Pharmacodynamics, Clinical Experience and Future Directions. Drugs 2016, 76, 485–500. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lanza, J.S.; Pomel, S.; Loiseau, P.M.; Frézard, F. Recent advances in amphotericin B delivery strategies for the treatment of leishmaniases. Expert Opin. Drug Deliv. 2019, 16, 1063–1079. [Google Scholar] [CrossRef] [PubMed]
- Zylberberg, C.; Matosevic, S. Pharmaceutical liposomal drug delivery: A review of new delivery systems and a look at the regulatory landscape. Drug Deliv. 2016, 23, 3319–3329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bovier, P.A. Epaxal: A virosomal vaccine to prevent hepatitis A infection. Expert Rev. Vaccines 2008, 7, 1141–1150. [Google Scholar] [CrossRef] [PubMed]
- Rivankar, S. An overview of doxorubicin formulations in cancer therapy. J. Cancer Res. Ther. 2014, 10, 853–858. [Google Scholar] [CrossRef]
- Minodier, P.; Retornaz, K.; Horelt, A.; Garnier, J.M. Liposomal amphotericin B in the treatment of visceral leishmaniasis in immunocompetent patients. Fundam. Clin. Pharmcol. 2003, 17, 183–188. [Google Scholar] [CrossRef]
- Kaposi’s sarcoma: DaunoXome approved. AIDS Treat. News 1996, 246, 3–4.
- Salehi, B.; Selamoglu, Z.; Mileski, K.S.; Pezzani, R.; Redaelli, M.; Cho, W.C.; Kobarfard, F.; Rajabi, S.; Martorell, M.; Kumar, P.; et al. Liposomal Cytarabine as Cancer Therapy: From Chemistry to Medicine. Biomolecules 2019, 9, 773. [Google Scholar] [CrossRef] [Green Version]
- Chhikara, B.S.; Parang, K. Development of cytarabine prodrugs and delivery systems for leukemia treatment. Expert Opin. Drug Deliv. 2010, 7, 1399–1414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leonard, R.C.F.; Williams, S.; Tulpule, A.; Levine, A.M.; Oliveros, S. Improving the therapeutic index of anthracycline chemotherapy: Focus on liposomal doxorubicin (Myocet (TM)). Breast 2009, 18, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Koudelka, S.; Turanek, J. Liposomal paclitaxel formulations. J. Control. Release 2012, 163, 322–334. [Google Scholar] [CrossRef] [PubMed]
- Alphandery, E.; Grand-Dewyse, P.; Lefevre, R.; Mandawala, C.; Durand-Dubief, M. Cancer therapy using nanoformulated substances: Scientific, regulatory and financial aspects. Expert Rev. Anticancer Ther. 2015, 15, 1233–1255. [Google Scholar] [CrossRef] [PubMed]
- Kaye, A.D.; Armstead-Williams, C.; Hyatali, F.; Cox, K.S.; Kaye, R.J.; Eng, L.K.; Farooq Anwar, M.A.; Patel, P.V.; Patil, S.; Cornett, E.M. Exparel for Postoperative Pain Management: A Comprehensive Review. Curr. Pain Headache Rep. 2020, 24, 73. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H. Onivyde for the therapy of multiple solid tumors. Onco Targets Ther. 2016, 9, 3001–3007. [Google Scholar] [CrossRef] [Green Version]
- Alving, C.R.; Beck, Z.; Matyas, G.R.; Rao, M. Liposomal adjuvants for human vaccines. Expert Opin. Drug Deliv. 2016, 13, 807–816. [Google Scholar] [CrossRef] [PubMed]
- Beck, Z.; Matyas, G.R.; Alving, C.R. Detection of liposomal cholesterol and monophosphoryl lipid A by QS-21 saponin and Limulus polyphemus amebocyte lysate. Biochim. Biophys. Acta 2015, 1848, 775–780. [Google Scholar] [CrossRef] [Green Version]
- Viana, I.M.O.; Roussel, S.; Defrêne, J.; Lima, E.M.; Barabé, F.; Bertrand, N. Innate and adaptive immune responses toward nanomedicines. Acta Pharm. Sin. B 2021, 11, 852–870. [Google Scholar] [CrossRef]
- Kristen, A.V.; Ajroud-Driss, S.; Conceicao, I.; Gorevic, P.; Kyriakides, T.; Obici, L. Patisiran, an RNAi therapeutic for the treatment of hereditary transthyretin-mediated amyloidosis. Neurodegener. Dis. Manag. 2019, 9, 5–23. [Google Scholar] [CrossRef] [Green Version]
- Khan, O.; Chaudary, N. The Use of Amikacin Liposome Inhalation Suspension (Arikayce) in the Treatment of Refractory Nontuberculous Mycobacterial Lung Disease in Adults. Drug Des. Dev. Ther. 2020, 14, 2287–2294. [Google Scholar] [CrossRef] [PubMed]
- Hoy, S.M. Amikacin Liposome Inhalation Suspension in Refractory Mycobacterium avium Complex Lung Disease: A Profile of Its Use. Clin. Drug Investig. 2021, 41, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Perez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA COVID-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Fathizadeh, H.; Afshar, S.; Masoudi, M.R.; Gholizadeh, P.; Asgharzadeh, M.; Ganbarov, K.; Kose, S.; Yousefi, M.; Kafil, H.S. SARS-CoV-2 (COVID-19) vaccines structure, mechanisms and effectiveness: A review. Int. J. Biol. Macromol. 2021, 188, 740–750. [Google Scholar] [CrossRef] [PubMed]
- McGuckin, M.B.; Wang, J.; Ghanma, R.; Qin, N.; Palma, S.D.; Donnelly, R.F.; Paredes, A.J. Nanocrystals as a master key to deliver hydrophobic drugs via multiple administration routes. J. Control. Release 2022, 345, 334–353. [Google Scholar] [CrossRef] [PubMed]
- Miao, X.; Yang, W.; Feng, T.; Lin, J.; Huang, P. Drug nanocrystals for cancer therapy. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2018, 10, e1499. [Google Scholar] [CrossRef] [PubMed]
- Magar, K.T.; Boafo, G.F.; Zoulikha, M.; Jiang, X.; Li, X.; Xiao, Q.; Xing, X.; Wang, X.; Fan, L.; Wu, Z. Metal phenolic network-stabilized nanocrystals of andrographolide to alleviate macrophage-mediated inflammation in-vitro. Chin. Chem. Lett. 2022, 34, 107453. [Google Scholar] [CrossRef]
- Teng, C.; Li, B.; Lin, C.; Xing, X.; Huang, F.; Yang, Y.; Li, Y.; Azevedo, H.S.; He, W. Targeted delivery of baicalein-p53 complex to smooth muscle cells reverses pulmonary hypertension. J. Control. Release 2022, 341, 591–604. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Xie, H.; Liu, Y.; Gao, P.; Yang, X.; Shen, Z. Effect of metformin on all-cause and cardiovascular mortality in patients with coronary artery diseases: A systematic review and an updated meta-analysis. Cardiovas. Diabetol. 2019, 18, 96. [Google Scholar] [CrossRef] [Green Version]
- He, W.; Kapate, N.; Shields, C.W.t.; Mitragotri, S. Drug delivery to macrophages: A review of targeting drugs and drug carriers to macrophages for inflammatory diseases. Adv. Drug Deliv. Rev. 2019, 165–166, 15–40. [Google Scholar] [CrossRef]
- Teng, C.; Lin, C.; Huang, F.; Xing, X.; Chen, S.; Ye, L.; Azevedo, H.S.; Xu, C.; Wu, Z.; Chen, Z.; et al. Intracellular codelivery of anti-inflammatory drug and anti-miR 155 to treat inflammatory disease. Acta Pharm. Sin. B 2020, 10, 1521–1533. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Q.; Li, X.; Li, Y.; Wu, Z.; Xu, C.; Chen, Z.; He, W. Biological drug and drug delivery-mediated immunotherapy. Acta Pharm. Sin. B 2021, 11, 941–960. [Google Scholar] [CrossRef] [PubMed]
- Jia, B.; Zou, Y.; Han, X.; Bae, J.-W.; Jeon, C.O. Gut microbiome-mediated mechanisms for reducing cholesterol levels: Implications for ameliorating cardiovascular disease. Trends Microbiol. 2023, 31, 76–91. [Google Scholar] [CrossRef] [PubMed]
- Shegokar, R.; Müller, R.H. Nanocrystals: Industrially feasible multifunctional formulation technology for poorly soluble actives. Int. J. Pharm. 2010, 399, 129–139. [Google Scholar] [CrossRef]
- Yousaf, A.M.; Kim, D.W.; Oh, Y.-K.; Yong, C.S.; Kim, J.O.; Choi, H.-G. Enhanced oral bioavailability of fenofibrate using polymeric nanoparticulated systems: Physicochemical characterization and in vivo investigation. Int. J. Nanomed. 2015, 10, 1819. [Google Scholar]
- Jahangir, M.A.; Imam, S.S.; Muheem, A.; Chettupalli, A.; Al-Abbasi, F.A.; Nadeem, M.S.; Kazmi, I.; Afzal, M.; Alshehri, S. Nanocrystals: Characterization overview, applications in drug delivery, and their toxicity concerns. J. Pharm. Innov. 2022, 17, 237–248. [Google Scholar] [CrossRef]
- Kumar, R.; Siril, P.F. Enhancing the Solubility of Fenofibrate by Nanocrystal Formation and Encapsulation. AAPS PharmSciTech 2018, 19, 284–292. [Google Scholar] [CrossRef]
- Gite, S.; Kakade, P.; Patravale, V. Surface Engineering of Fenofibrate Nanocrystals Using Nano-by-Design Multivariate Integration: A Biopharmaceutical and Pharmacokinetic Perspective. Curr. Drug Deliv. 2021, 18, 1314–1329. [Google Scholar] [CrossRef]
- Madgulkar, A.; Bhalekar, M.; Khabiya, P. Nanoparticulates of fenofibrate for solubility enhancement: Ex-vivo evaluation. J. Drug Deliv. Ther. 2019, 9, 155–163. [Google Scholar]
- Junghanns, J.-U.A.; Müller, R.H.J. Nanocrystal technology, drug delivery and clinical applications. Int. J. Nanomed. 2008, 3, 295. [Google Scholar]
- Tziomalos, K.; Athyros, V.G. Fenofibrate: A novel formulation (Triglide™) in the treatment of lipid disorders: A review. Int. J. Nanomed. 2006, 1, 129. [Google Scholar] [CrossRef] [PubMed]
- Rayner, C.R.; Smith, P.F.; Andes, D.; Andrews, K.; Derendorf, H.; Friberg, L.E.; Hanna, D.; Lepak, A.; Mills, E.; Polasek, T.M.; et al. Model-Informed Drug Development for Anti-Infectives: State of the Art and Future. Clin. Pharmcol. Ther. 2021, 109, 867–891. [Google Scholar] [CrossRef] [PubMed]
- Padberg, S. 2.6-Anti-infective Agents. In Drugs During Pregnancy and Lactation, 3rd ed.; Schaefer, C., Peters, P., Miller, R.K., Eds.; Academic Press: San Diego, CA, USA, 2015; pp. 115–176. [Google Scholar]
- Aoyagi, N.; Ogata, H.; Kaniwa, N.; Ejima, A. Effect of food on the bioavailability of griseofulvin from microsize and PEG ultramicrosize (GRIS-PEGR) plain tablets. J. Pharmcobio-Dyn. 1982, 5, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Ariyo, O.E.; Jones, C.E. Use of long-acting injectable antiretroviral agents for human immunodeficiency Virus: A review. J. Clin. Virol. 2022, 146, 105032. [Google Scholar] [CrossRef]
- Clement, M.E.; Kofron, R.; Landovitz, R.J. Long-acting injectable cabotegravir for the prevention of HIV infection. Curr. Opin. HIV AIDS 2020, 15, 19–26. [Google Scholar] [CrossRef]
- Flexner, C.; Owen, A.; Siccardi, M.; Swindells, S. Long-acting drugs and formulations for the treatment and prevention of HIV infection. Int. J. Antimicrob. Agents 2021, 57, 106220. [Google Scholar] [CrossRef]
- Lee, W.Y.; Asadujjaman, M.; Jee, J.-P. Long acting injectable formulations: The state of the arts and challenges of poly (lactic-co-glycolic acid) microsphere, hydrogel, organogel and liquid crystal. J. Pharm. Investig. 2019, 49, 459–476. [Google Scholar] [CrossRef]
- Markham, A. Cabotegravir Plus Rilpivirine: First Approval. Drugs 2020, 80, 915–922. [Google Scholar] [CrossRef]
- Kalhapure, R.S.; Palekar, S.; Patel, K.; Monpara, J. Nanocrystals for controlled delivery: State of the art and approved drug products. Expert Opin. Drug Deliv. 2022, 19, 1303–1316. [Google Scholar] [CrossRef]
- Kahan, B.D. Sirolimus: A comprehensive review. Expert Opin. Pharmcother. 2001, 2, 1903–1917. [Google Scholar] [CrossRef]
- Deschamps, B.; Musaji, N.; Gillespie, J. Food effect on the bioavailability of two distinct formulations of megestrol acetate oral suspension. Int. J. Nanomed. 2009, 4, 185–192. [Google Scholar]
- Li, M.; Azad, M.; Davé, R.; Bilgili, E. Nanomilling of Drugs for Bioavailability Enhancement: A Holistic Formulation-Process Perspective. Pharmaceutics 2016, 8, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blair, H.A.J.D.; Perspectives, T. Paliperidone palmitate intramuscular 6-monthly formulation in schizophrenia: A profile of its use. Drug Ther. Perspect. 2022, 38, 335–342. [Google Scholar] [CrossRef]
- Balch, R.J.; Trescot, A. Extended-release morphine sulfate in treatment of severe acute and chronic pain. J. Pain Res. 2010, 3, 191–200. [Google Scholar]
- Markowitz, J.S.; Straughn, A.B.; Patrick, K.S. Advances in the pharmacotherapy of attention-deficit-hyperactivity disorder: Focus on methylphenidate formulations. Pharmacotherapy 2003, 23, 1227–1374. [Google Scholar] [CrossRef] [PubMed]
- Shayani, S.; Palmer, J.; Stiller, T.; Chan, H.; Keuylian, S.; Parker, P.; Thomas, S.; Pullarkat, V.; Nademanee, A.; Forman, S.J.; et al. Aprepitant (Emend) significantly increases sirolimus levels in patients undergoing allogeneic hematopoietic SCT. Bone Marrow Transplant. 2012, 47, 291–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chavda, V.P. Chapter 4—Nanobased Nano Drug Delivery: A Comprehensive Review. In Applications of Targeted Nano Drugs and Delivery Systems; Mohapatra, S.S., Ranjan, S., Dasgupta, N., Mishra, R.K., Thomas, S., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 69–92. [Google Scholar]
- American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacological Management of Persistent Pain in Older Persons. Pain Med. 2009, 10, 1062–1083. [Google Scholar] [CrossRef]
- Chue, P.; Chue, J. A review of paliperidone palmitate. Expert Rev. Neurother. 2012, 12, 1383–1397. [Google Scholar] [CrossRef]
- Chang, C.-L.; Huang, Y.-C.; Yang, P. Improving of Cognition and Quality of Life in Schizophrenia With One-month and Three-month Paliperidone Palmitate Treatment. Res. Sq. 2021; in press. [Google Scholar]
- Preda, A.; Shapiro, B.B. A safety evaluation of aripiprazole in the treatment of schizophrenia. Expert Opin. Drug Saf. 2020, 19, 1529–1538. [Google Scholar] [CrossRef]
- Ahlawat, J.; Henriquez, G.; Narayan, M. Enhancing the Delivery of Chemotherapeutics: Role of Biodegradable Polymeric Nanoparticles. Molecules 2018, 23, 2157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghosh, B.; Biswas, S. Polymeric micelles in cancer therapy: State of the art. J. Control. Release 2021, 332, 127–147. [Google Scholar] [CrossRef] [PubMed]
- Hwang, D.; Ramsey, J.D.; Kabanov, A.V. Polymeric micelles for the delivery of poorly soluble drugs: From nanoformulation to clinical approval. Adv. Drug Deliv Rev. 2020, 156, 80–118. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi, R.; Abdollahi, M.; Emamgholi Zadeh, E.; Khodabakhshi, K.; Badeli, A.; Bagheri, H.; Hosseinkhani, S. mPEG-PLA and PLA-PEG-PLA nanoparticles as new carriers for delivery of recombinant human Growth Hormone (rhGH). Sci. Rep. 2018, 8, 9854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- González-Henríquez, C.M.; Sarabia-Vallejos, M.A.; Rodríguez-Hernández, J. Strategies to Fabricate Polypeptide-Based Structures via Ring-Opening Polymerization of N-Carboxyanhydrides. Polymers 2017, 9, 551. [Google Scholar] [CrossRef] [Green Version]
- Ilyas, R.; Zuhri, M.; Aisyah, H.; Asyraf, M.; Hassan, S.; Zainudin, E.; Sapuan, S.; Sharma, S.; Bangar, S.; Jumaidin, R. Natural fiber-reinforced polylactic acid, polylactic acid blends and their composites for advanced applications. Polymers 2022, 14, 202. [Google Scholar] [CrossRef] [PubMed]
- Pan, Z.; Yang, G.; Yuan, J.; Pan, M.; Li, J.; Tan, H. Effect of the disulfide bond and polyethylene glycol on the degradation and biophysicochemical properties of polyurethane micelles. Biomater. Sci. 2022, 10, 794–807. [Google Scholar] [CrossRef]
- Lamptey, R.N.L.; Gothwal, A.; Trivedi, R.; Arora, S.; Singh, J. Synthesis and Characterization of Fatty Acid Grafted Chitosan Polymeric Micelles for Improved Gene Delivery of VGF to the Brain through Intranasal Route. Biomedicines 2022, 10, 493. [Google Scholar] [CrossRef]
- Suzuki, K.; Yoshizaki, Y.; Horii, K.; Murase, N.; Kuzuya, A.; Ohya, Y. Preparation of hyaluronic acid-coated polymeric micelles for nasal vaccine delivery. Biomater. Sci. 2022, 10, 1920–1928. [Google Scholar] [CrossRef]
- Owens, D.E., 3rd; Peppas, N.A. Opsonization, biodistribution, and pharmacokinetics of polymeric nanoparticles. Int. J. Pharm. 2006, 307, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Zielińska, A.; Carreiró, F.; Oliveira, A.M.; Neves, A.; Pires, B.; Venkatesh, D.N.; Durazzo, A.; Lucarini, M.; Eder, P.; Silva, A.M.; et al. Polymeric Nanoparticles: Production, Characterization, Toxicology and Ecotoxicology. Molecules 2020, 25, 3731. [Google Scholar] [CrossRef] [PubMed]
- Lübtow, M.M.; Marciniak, H.; Schmiedel, A.; Roos, M.; Lambert, C.; Luxenhofer, R. Ultra-High to Ultra-Low Drug-Loaded Micelles: Probing Host-Guest Interactions by Fluorescence Spectroscopy. Chemistry 2019, 25, 12601–12610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiao, K.; Li, Y.; Luo, J.; Lee, J.S.; Xiao, W.; Gonik, A.M.; Agarwal, R.G.; Lam, K.S. The effect of surface charge on in vivo biodistribution of PEG-oligocholic acid based micellar nanoparticles. Biomaterials 2011, 32, 3435–3446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Photos, P.J.; Bacakova, L.; Discher, B.; Bates, F.S.; Discher, D.E. Polymer vesicles in vivo: Correlations with PEG molecular weight. J. Control. Release 2003, 90, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, K.; Sanada, Y.; Mochizuki, S.; Kawano, K.; Maitani, Y.; Sakurai, K.; Yokoyama, M. Determination of polymeric micelles’ structural characteristics, and effect of the characteristics on pharmacokinetic behaviors. J. Control. Release 2015, 203, 77–84. [Google Scholar] [CrossRef] [Green Version]
- Velluto, D.; Demurtas, D.; Hubbell, J.A. PEG-b-PPS diblock copolymer aggregates for hydrophobic drug solubilization and release: Cyclosporin A as an example. Mol. Pharm. 2008, 5, 632–642. [Google Scholar] [CrossRef]
- Lübtow, M.M.; Haider, M.S.; Kirsch, M.; Klisch, S.; Luxenhofer, R. Like Dissolves Like? A Comprehensive Evaluation of Partial Solubility Parameters to Predict Polymer-Drug Compatibility in Ultrahigh Drug-Loaded Polymer Micelles. Biomacromolecules 2019, 20, 3041–3056. [Google Scholar] [CrossRef] [Green Version]
- Salimi, A.; Sharif Makhmal Zadeh, B.; Kazemi, M. Preparation and optimization of polymeric micelles as an oral drug delivery system for deferoxamine mesylate: In vitro and ex vivo studies. Res. Pharm. Sci. 2019, 14, 293–307. [Google Scholar]
- Aliabadi, H.M.; Brocks, D.R.; Lavasanifar, A. Polymeric micelles for the solubilization and delivery of cyclosporine A: Pharmacokinetics and biodistribution. Biomaterials 2005, 26, 7251–7259. [Google Scholar] [CrossRef]
- Fournier, E.; Dufresne, M.H.; Smith, D.C.; Ranger, M.; Leroux, J.C. A novel one-step drug-loading procedure for water-soluble amphiphilic nanocarriers. Pharm. Res. 2004, 21, 962–968. [Google Scholar] [CrossRef]
- Kedar, U.; Phutane, P.; Shidhaye, S.; Kadam, V. Advances in polymeric micelles for drug delivery and tumor targeting. Nanomed. Nanotechnol. 2010, 6, 714–729. [Google Scholar] [CrossRef] [PubMed]
- Chakravarty, P.; Famili, A.; Nagapudi, K.; Al-Sayah, M.A. Using Supercritical Fluid Technology as a Green Alternative During the Preparation of Drug Delivery Systems. Pharmaceutics 2019, 11, 629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.C.; Kim, D.W.; Shim, Y.H.; Bang, J.S.; Oh, H.S.; Kim, S.W.; Seo, M.H. In vivo evaluation of polymeric micellar paclitaxel formulation: Toxicity and efficacy. J. Control. Release 2001, 72, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.Y.; Kim, D.W.; Chung, J.Y.; Shin, S.G.; Kim, S.C.; Heo, D.S.; Kim, N.K.; Bang, Y.J. Phase I and pharmacokinetic study of Genexol-PM, a cremophor-free, polymeric micelle-formulated paclitaxel, in patients with advanced malignancies. Clin. Cancer Res. 2004, 10, 3708–3716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, D.W.; Kim, S.Y.; Kim, H.K.; Kim, S.W.; Shin, S.W.; Kim, J.S.; Park, K.; Lee, M.Y.; Heo, D.S. Multicenter phase II trial of Genexol-PM, a novel Cremophor-free, polymeric micelle formulation of paclitaxel, with cisplatin in patients with advanced non-small-cell lung cancer. Ann. Oncol. 2007, 18, 2009–2014. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.W.; Yun, M.H.; Jeong, S.W.; In, C.H.; Kim, J.Y.; Seo, M.H.; Pai, C.M.; Kim, S.O. Development of docetaxel-loaded intravenous formulation, Nanoxel-PM™ using polymer-based delivery system. J. Control. Release 2011, 155, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Bernabeu, E.; Cagel, M.; Lagomarsino, E.; Moretton, M.; Chiappetta, D.A. Paclitaxel: What has been done and the challenges remain ahead. Int. J. Pharm. 2017, 526, 474–495. [Google Scholar] [CrossRef] [PubMed]
- Vergote, I.; Bergfeldt, K.; Franquet, A.; Lisyanskaya, A.S.; Bjermo, H.; Heldring, N.; Buyse, M.; Brize, A. A randomized phase III trial in patients with recurrent platinum sensitive ovarian cancer comparing efficacy and safety of paclitaxel micellar and Cremophor EL-paclitaxel. Gynecol. Oncol. 2020, 156, 293–300. [Google Scholar] [CrossRef]
- Sahoo, S.K.; Labhasetwar, V. Nanotech approaches to drug delivery and imaging. Drug Discov. Today 2003, 8, 1112–1120. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Giottonini, K.Y.; Rodríguez-Córdova, R.J.; Gutiérrez-Valenzuela, C.A.; Peñuñuri-Miranda, O.; Zavala-Rivera, P.; Guerrero-Germán, P.; Lucero-Acuña, A. PLGA nanoparticle preparations by emulsification and nanoprecipitation techniques: Effects of formulation parameters. RSC Adv. 2020, 10, 4218–4231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez-Herrero, E.; Fernández-Medarde, A. Advanced targeted therapies in cancer: Drug nanocarriers, the future of chemotherapy. Eur. J. Pharm. Biopharm. 2015, 93, 52–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, C.M.; Aryal, S.; Zhang, L. Nanoparticle-assisted combination therapies for effective cancer treatment. Ther. Deliv. 2010, 1, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Kono, K.; Ozawa, T.; Yoshida, T.; Ozaki, F.; Ishizaka, Y.; Maruyama, K.; Kojima, C.; Harada, A.; Aoshima, S. Highly temperature-sensitive liposomes based on a thermosensitive block copolymer for tumor-specific chemotherapy. Biomaterials 2010, 31, 7096–7105. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wang, Y.; Chen, Z.G.; Shin, D.M. Advances of cancer therapy by nanotechnology. Cancer Res. Treat. 2009, 41, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elsadek, B.; Kratz, F. Impact of albumin on drug delivery--new applications on the horizon. J. Control. Release 2012, 157, 4–28. [Google Scholar] [CrossRef] [PubMed]
- Gradishar, W.J.; Tjulandin, S.; Davidson, N.; Shaw, H.; Desai, N.; Bhar, P.; Hawkins, M.; O’Shaughnessy, J. Phase III trial of nanoparticle albumin-bound paclitaxel compared with polyethylated castor oil-based paclitaxel in women with breast cancer. J. Clin. Oncol. 2005, 23, 7794–7803. [Google Scholar] [CrossRef]
- Satouchi, M.; Okamoto, I.; Sakai, H.; Yamamoto, N.; Ichinose, Y.; Ohmatsu, H.; Nogami, N.; Takeda, K.; Mitsudomi, T.; Kasahara, K.; et al. Efficacy and safety of weekly nab-paclitaxel plus carboplatin in patients with advanced non-small cell lung cancer. Lung Cancer 2013, 81, 97–101. [Google Scholar] [CrossRef]
- Kottschade, L.A.; Suman, V.J.; Amatruda, T., 3rd; McWilliams, R.R.; Mattar, B.I.; Nikcevich, D.A.; Behrens, R.; Fitch, T.R.; Jaslowski, A.J.; Markovic, S.N. A phase II trial of nab-paclitaxel (ABI-007) and carboplatin in patients with unresectable stage IV melanoma: A North Central Cancer Treatment Group Study, N057E(1). Cancer 2011, 117, 1704–1710. [Google Scholar] [CrossRef] [Green Version]
- Helms, B.; Meijer, E.W. Chemistry. Dendrimers at work. Science 2006, 313, 929–930. [Google Scholar] [CrossRef]
- Ouyang, Z.; Gao, Y.; Shen, M.; Shi, X. Dendrimer-based nanohybrids in cancer photomedicine. Mater. Today Bio 2021, 10, 100111. [Google Scholar] [CrossRef]
- Zhou, Z.; Wang, Y.; Yan, Y.; Zhang, Q.; Cheng, Y. Dendrimer-Templated Ultrasmall and Multifunctional Photothermal Agents for Efficient Tumor Ablation. ACS Nano 2016, 10, 4863–4872. [Google Scholar] [CrossRef] [PubMed]
- Xiong, X.; Xu, Z.; Huang, H.; Wang, Y.; Zhao, J.; Guo, X.; Zhou, S. A NIR light triggered disintegratable nanoplatform for enhanced penetration and chemotherapy in deep tumor tissues. Biomaterials 2020, 245, 119840. [Google Scholar] [CrossRef] [PubMed]
- Wen, S.; Zhao, L.; Zhao, Q.; Li, D.; Liu, C.; Yu, Z.; Shen, M.; Majoral, J.P.; Mignani, S.; Zhao, J.; et al. A promising dual mode SPECT/CT imaging platform based on (99m)Tc-labeled multifunctional dendrimer-entrapped gold nanoparticles. J. Mater. Chem. B 2017, 5, 3810–3815. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Zhao, L.; Li, X.; Wang, P.; Zhao, J.; Shi, X.; Shen, M. Targeted tumor SPECT/CT dual mode imaging using multifunctional RGD-modified low generation dendrimer-entrapped gold nanoparticles. Biomater. Sci. 2017, 5, 2393–2397. [Google Scholar] [CrossRef] [PubMed]
- Xiao, T.; Li, D.; Shi, X.; Shen, M. PAMAM Dendrimer-Based Nanodevices for Nuclear Medicine Applications. Macromol. Biosci. 2020, 20, e1900282. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Xiong, Z.; Zhang, J.; Peng, C.; Klajnert-Maculewicz, B.; Shen, M.; Shi, X. Zwitterionic Gadolinium(III)-Complexed Dendrimer-Entrapped Gold Nanoparticles for Enhanced Computed Tomography/Magnetic Resonance Imaging of Lung Cancer Metastasis. ACS Appl. Mater. Interfaces 2019, 11, 15212–15221. [Google Scholar] [CrossRef]
- Baker, J.R., Jr. Dendrimer-based nanoparticles for cancer therapy. Hematology 2009, 2009, 708–719. [Google Scholar] [CrossRef] [Green Version]
- Shen, M.; Shi, X. Dendrimer-based organic/inorganic hybrid nanoparticles in biomedical applications. Nanoscale 2010, 2, 1596–1610. [Google Scholar] [CrossRef]
- Tyssen, D.; Henderson, S.A.; Johnson, A.; Sterjovski, J.; Moore, K.; La, J.; Zanin, M.; Sonza, S.; Karellas, P.; Giannis, M.P.; et al. Structure activity relationship of dendrimer microbicides with dual action antiviral activity. PLoS ONE 2010, 5, e12309. [Google Scholar] [CrossRef] [Green Version]
- Gong, E.; Matthews, B.; McCarthy, T.; Chu, J.; Holan, G.; Raff, J.; Sacks, S. Evaluation of dendrimer SPL7013, a lead microbicide candidate against herpes simplex viruses. Antivir. Res. 2005, 68, 139–146. [Google Scholar] [CrossRef]
- Dezzutti, C.S.; James, V.N.; Ramos, A.; Sullivan, S.T.; Siddig, A.; Bush, T.J.; Grohskopf, L.A.; Paxton, L.; Subbarao, S.; Hart, C.E. In vitro comparison of topical microbicides for prevention of human immunodeficiency virus type 1 transmission. Antimicrob. Agents Chemother. 2004, 48, 3834–3844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, Y.H.; Emau, P.; Cairns, J.S.; Flanary, L.; Morton, W.R.; McCarthy, T.D.; Tsai, C.C. SPL7013 gel as a topical microbicide for prevention of vaginal transmission of SHIV89.6P in macaques. AIDS Res. Hum. Retrovir. 2005, 21, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Rupp, R.; Rosenthal, S.L.; Stanberry, L.R. VivaGel (SPL7013 Gel): A candidate dendrimer--microbicide for the prevention of HIV and HSV infection. Int. J. Nanomed. 2007, 2, 561–566. [Google Scholar]
- Price, C.F.; Tyssen, D.; Sonza, S.; Davie, A.; Evans, S.; Lewis, G.R.; Xia, S.; Spelman, T.; Hodsman, P.; Moench, T.R.; et al. SPL7013 Gel (VivaGel®) retains potent HIV-1 and HSV-2 inhibitory activity following vaginal administration in humans. PLoS ONE 2011, 6, e24095. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, L.P.; Wang, D.Y.; Li, Z.B. Grand challenges in nanomedicine. Mat. Sci. Eng. C-Mater. 2020, 106, 110302. [Google Scholar] [CrossRef]
- Sato, Y.; Nakamura, T.; Yamada, Y.; Harashima, H. The nanomedicine rush: New strategies for unmet medical needs based on innovative nano DDS. J. Control. Release 2021, 330, 305–316. [Google Scholar] [CrossRef]
- Lombardo, D.; Kiselev, M.A.; Caccamo, M.T. Smart Nanoparticles for Drug Delivery Application: Development of Versatile Nanocarrier Platforms in Biotechnology and Nanomedicine. J. Nanomater. 2019, 2019, 3702518. [Google Scholar] [CrossRef]
- Zhang, Y.; Xu, C.; Yang, X.L.; Pu, K.Y. Photoactivatable Protherapeutic Nanomedicine for Cancer. Adv. Mater. 2020, 32, 2002661. [Google Scholar] [CrossRef]
- Soares, S.; Sousa, J.; Pais, A.; Vitorino, C. Nanomedicine: Principles, Properties, and Regulatory Issues. Front. Chem. 2018, 6, 523–565. [Google Scholar] [CrossRef]
- Talpur, R.; Apisarnthanarax, N.; Ward, S.; Duvic, M. Treatment of refractory peripheral T-cell lymphoma with denileukin diftitox (ONTAK (R)). Leuk. Lymphoma 2002, 43, 121–126. [Google Scholar] [CrossRef]
- Lemp, M.A.; Baudouin, C.; Baum, J.; Dogru, M.; Foulks, G.N.; Kinoshita, S.; Laibson, P.; McCulley, J.; Murube, J.; Pflugfelder, S.C.; et al. The definition and classification of dry eye disease: Report of the Definition and Classification Subcommittee of the international Dry Eye WorkShop (2007). Ocul. Surf. 2007, 5, 75–92. [Google Scholar]
- Nagai, N.; Otake, H. Novel drug delivery systems for the management of dry eye. Adv. Drug Deliv. Rev. 2022, 191, 114582. [Google Scholar] [CrossRef] [PubMed]
- Ji, Y.W.; Kim, H.M.; Ryu, S.Y.; Oh, J.W.; Yeo, A.; Choi, C.Y.; Kim, M.J.; Song, J.S.; Kim, H.S.; Seo, K.Y.; et al. Changes in Human Tear Proteome Following Topical Treatment of Dry Eye Disease: Cyclosporine A Versus Diquafosol Tetrasodium. Investig. Opthalmol. Vis. Sci. 2019, 60, 5035–5044. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, L.M.; Woloshin, S. A Clear-eyed View of Restasis and Chronic Dry Eye Disease. Jama Intern. Med. 2018, 178, 181–182. [Google Scholar] [CrossRef] [PubMed]
- Dinndorf, P.A.; Gootenberg, J.; Cohen, M.H.; Keegan, P.; Pazdur, R. FDA drug approval summary: Pegaspargase (Oncaspar (R)) for the first-line treatment of children with acute lymphoblastic leukemia (ALL). Oncologist 2007, 12, 991–998. [Google Scholar] [CrossRef]
- Toth, G.B.; Varallyay, C.G.; Horvath, A.; Bashir, M.R.; Choyke, P.L.; Daldrup-Link, H.E.; Dosa, E.; Finn, J.P.; Gahramanov, S.; Harisinghani, M.; et al. Current and potential imaging applications of ferumoxytol for magnetic resonance imaging. Kidney Int. 2017, 92, 47–66. [Google Scholar] [CrossRef]
- Keating, G.M. Ferric Carboxymaltose: A Review of Its Use in Iron Deficiency. Drugs 2015, 75, 101–127. [Google Scholar] [CrossRef]
- Jahn, M.R.; Andreasen, H.B.; Futterer, S.; Nawroth, T.; Schunemann, V.; Kolb, U.; Hofmeister, W.; Munoz, M.; Bock, K.; Meldal, M.; et al. A comparative study of the physicochemical properties of iron isomaltoside 1000 (Monofer (R)), a new intravenous iron preparation and its clinical implications. Eur. J. Pharm. Biopharm. 2011, 78, 480–491. [Google Scholar] [CrossRef]
- Sanchez-Fructuoso, A.; Guirado, L.; Ruiz, J.C.; Torregrosa, V.; Gonzalez, E.; Suarez, M.L.; Gallego, R.; Grp, A.T.S. Anemia Control in Kidney Transplant Patients Treated With Methoxy Polyethylene Glycol-Epoetin Beta (Mircera): The Anemiatrans Group. Transplant. Proc. 2010, 42, 2931–2934. [Google Scholar] [CrossRef]
- Turecek, P.L.; Romeder-Finger, S.; Apostol, C.; Bauer, A.; Crocker-Buque, A.; Burger, D.A.; Schall, R.; Gritsch, H. A world-wide survey and field study in clinical haemostasis laboratories to evaluate FVIII:C activity assay variability of ADYNOVATE and OBIZUR in comparison with ADVATE. Haemophilia 2016, 22, 957–965. [Google Scholar] [CrossRef]
- Piedmonte, D.M.; Treuheit, M.J. Formulation of Neulasta (R) (pegfilgrastim). Adv. Drug Deliv. Rev. 2008, 60, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Ferenci, P. Peginterferon alfa-2a (40KD) (Pegasys®) for the treatment of patients with chronic hepatitis C. Int. J. Clin. Pract. 2003, 57, 610–615. [Google Scholar] [PubMed]
- Wang, Y.S.; Youngster, S.; Grace, M.; Bausch, J.; Bordens, R.; Wyss, D.F. Structural and biological characterization of pegylated recombinant interferon alpha-2b and its therapeutic implications. Adv. Drug Deliv. Rev. 2002, 54, 547–570. [Google Scholar] [CrossRef] [PubMed]
- Dhib-Jalbut, S. Glatiramer acetate (Copaxone (R)) therapy for multiple sclerosis. Pharmcol. Ther. 2003, 98, 245–255. [Google Scholar] [CrossRef]
- Simon, J.; Heuer, M.; Shear, M.; Jackson, R.; Wright, D. The safety of estrasorb, a new topical emulsion technology for systemic delivery of estradiol. Obs. Gynecol. 2002, 99, 61. [Google Scholar]
- Gommans, G.; van Dongen, A.; van der Schors, T.; Gommans, E.; Visser, J.; Clarijs, W.J.W.; de Waard, J.; van de Bos, J.; Boer, R. Further optimisation of 99mTc-Nanocoll sentinel node localisation in carcinoma of the breast by improved labelling. Eur. J. Nucl. Med. 2001, 28, 1450–1455. [Google Scholar] [PubMed]
- Medvedeva, A.A.; Sinilkin, I.G.; Zelchan, R.V.; Chernov, V.I.; Lyapunov, A.Y.; Bragina, O.D.; Varlamova, N.; Skuridin, V.; Dergilev, A.P. The Study of 99m Tc-Aluminum Oxide Using for Sentinel Lymph Nodes Detection in Experiment. IOP Conf. Ser. Mater. Sci. Eng. 2016, 135, 012027. [Google Scholar] [CrossRef] [Green Version]
- D’Mello, S.R.; Cruz, C.N.; Chen, M.-L.; Kapoor, M.; Lee, S.L.; Tyner, K.M. The evolving landscape of drug products containing nanomaterials in the United States. Nat. Nanotechnol. 2017, 12, 523–529. [Google Scholar] [CrossRef]
- Lammers, T.; Ferrari, M. The success of nanomedicine. Nano Today 2020, 31, 100853. [Google Scholar] [CrossRef] [PubMed]
- Greish, K.; Mathur, A.; Bakhiet, M.; Taurin, S. Nanomedicine: Is it lost in translation? Ther. Deliv. 2018, 9, 269–285. [Google Scholar] [CrossRef]
- Huang, H.M.; Li, H.X. Tumor heterogeneity and the potential role of liquid biopsy in bladder cancer. Cancer Commun. 2021, 41, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Sato, Y.; Yamada, Y.; Abd Elwakil, M.M.; Kimura, S.; Younis, M.A.; Harashima, H. Extrahepatic targeting of lipid nanoparticles in vivo with intracellular targeting for future nanomedicines. Adv. Drug Deliv. Rev. 2022, 188, 114417. [Google Scholar] [CrossRef] [PubMed]
- Yan, L.; Zhang, Y.; Xu, B.; Tian, W. Fluorescent nanoparticles based on AIE fluorogens for bioimaging. Nanoscale 2016, 8, 2471–2487. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Qi, J.; Lu, Y.; He, H.; Wu, W. The in vivo fate of polymeric micelles. Adv. Drug Deliv. Rev. 2022, 188, 114463. [Google Scholar] [CrossRef]
- He, H.; Wang, L.; Ma, Y.; Yang, Y.; Lv, Y.; Zhang, Z.; Qi, J.; Dong, X.; Zhao, W.; Lu, Y. The biological fate of orally administered mPEG-PDLLA polymeric micelles. J. Control. Release 2020, 327, 725–736. [Google Scholar] [CrossRef]
- Xiao, Q.; Zoulikha, M.; Qiu, M.; Teng, C.; Lin, C.; Li, X.; Sallam, M.A.; Xu, Q.; He, W. The effects of protein corona on in vivo fate of nanocarriers. Adv. Drug Deliv. Rev. 2022, 186, 114356. [Google Scholar] [CrossRef]
- Colombo, S.; Beck-Broichsitter, M.; Bøtker, J.P.; Malmsten, M.; Rantanen, J.; Bohr, A. Transforming nanomedicine manufacturing toward Quality by Design and microfluidics. Adv. Drug Deliv. Rev. 2018, 128, 115–131. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jia, Y.; Jiang, Y.; He, Y.; Zhang, W.; Zou, J.; Magar, K.T.; Boucetta, H.; Teng, C.; He, W. Approved Nanomedicine against Diseases. Pharmaceutics 2023, 15, 774. https://doi.org/10.3390/pharmaceutics15030774
Jia Y, Jiang Y, He Y, Zhang W, Zou J, Magar KT, Boucetta H, Teng C, He W. Approved Nanomedicine against Diseases. Pharmaceutics. 2023; 15(3):774. https://doi.org/10.3390/pharmaceutics15030774
Chicago/Turabian StyleJia, Yuanchao, Yuxin Jiang, Yonglong He, Wanting Zhang, Jiahui Zou, Kosheli Thapa Magar, Hamza Boucetta, Chao Teng, and Wei He. 2023. "Approved Nanomedicine against Diseases" Pharmaceutics 15, no. 3: 774. https://doi.org/10.3390/pharmaceutics15030774






