A Novel Trans-Tracheostomal Retrograde Inhalation Technique Increases Subglottic Drug Deposition Compared to Traditional Trans-Oral Inhalation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Case Series
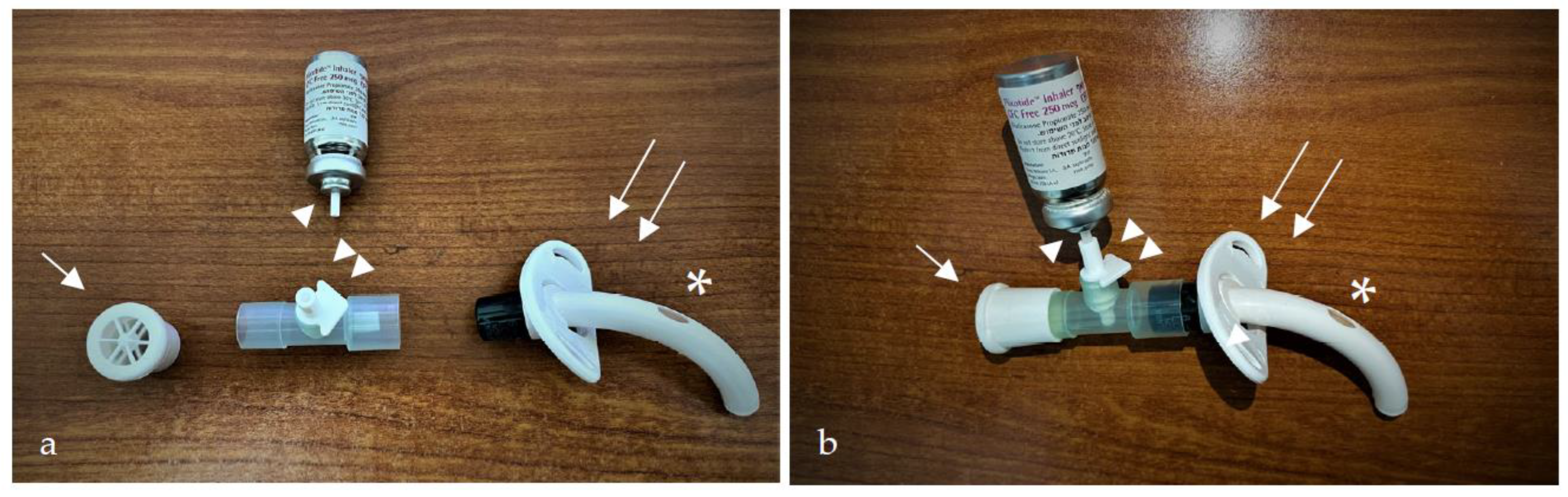
2.2. Trans-Tracheostomal, Retrograde, Corticosteroid Inhalation (TRCI) Technique
2.3. Extra-Thoracic In Silico Airway Model
2.4. Mesh Generation
2.5. Airflow and Aerosol Transport Simulations
3. Results
3.1. In Silico Aerosol Deposition
3.2. Patient Cases
- Case 1
- 2.
- Case 2
- 3.
- Case 3
- 4.
- Case 4
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Lang, M.; Brietzke, S.E. A Systematic Review and Meta-Analysis of Endoscopic Balloon Dilation of Pediatric Subglottic Stenosis. Otolaryngol. Neck Surg. 2014, 150, 174–179. [Google Scholar] [CrossRef]
- Feinstein, A.J.; Goel, A.; Raghavan, G.; Long, J.; Chhetri, D.K.; Berke, G.S.; Mendelsohn, A.H. Endoscopic Management of Subglottic Stenosis. JAMA Otolaryngol. Neck Surg. 2017, 143, 500–505. [Google Scholar] [CrossRef] [Green Version]
- Simpson, C.B.; James, J.C. The Efficacy of Mitomycin-C in the Treatment of Laryngotracheal Stenosis. Laryngoscope 2006, 116, 1923–1925. [Google Scholar] [CrossRef]
- Gelbard, A.; Donovan, D.T.; Ongkasuwan, J.; Nouraei, S.A.R.; Sandhu, G.; Benninger, M.S.; Bryson, P.C.; Lorenz, R.R.; Tierney, W.S.; Hillel, A.T. Disease Homogeneity and Treatment Heterogeneity in Idiopathic Subglottic Stenosis. Laryngoscope 2016, 126, 1390–1396. [Google Scholar] [CrossRef]
- Hseu, A.F.; Benninger, M.S.; Haffey, T.M.; Lorenz, R. Subglottic Stenosis: A Ten-year Review of Treatment Outcomes. Laryngoscope 2014, 124, 736–741. [Google Scholar] [CrossRef]
- Dwyer, C.D.; Qiabi, M.; Fortin, D.; Inculet, R.I.; Nichols, A.C.; MacNeil, S.D.; Malthaner, R.; Yoo, J.; Fung, K. Idiopathic Subglottic Stenosis: An Institutional Review of Outcomes With a Multimodality Surgical Approach. Otolaryngol. Neck Surg. 2021, 164, 1068–1076. [Google Scholar] [CrossRef]
- Lahav, Y.; Shoffel-Havakuk, H.; Halperin, D. Acquired Glottic Stenosis—The Ongoing Challenge: A Review of Etiology, Pathogenesis, and Surgical Management. J. Voice 2015, 29, 646.e1–646.e10. [Google Scholar] [CrossRef]
- Rhen, T.; Cidlowski, J.A. Antiinflammatory Action of Glucocorticoids—New Mechanisms for Old Drugs. N. Engl. J. Med. 2005, 353, 1711–1723. [Google Scholar] [CrossRef] [Green Version]
- Perepelitsyn, I.; Shapshay, S.M. Endoscopic Treatment of Laryngeal and Tracheal Stenosis—Has Mitomycin C Improved the Outcome? Otolaryngol. Neck Surg. 2004, 131, 16–20. [Google Scholar] [CrossRef]
- Bonchek, L.I. Successful Treatment of Postintubation Subglottic Stenosis with Intralesional Steroid Injections. Ann. Thorac. Surg. 1973, 15, 84–87. [Google Scholar] [CrossRef]
- Neevel, A.J.; Schuman, A.D.; Morrison, R.J.; Hogikyan, N.D.; Kupfer, R.A. Serial Intralesional Steroid Injection for Subglottic Stenosis: Systemic Side Effects and Impact on Surgery-Free Interval. OTO Open 2021, 5, 2473974X211054842. [Google Scholar] [CrossRef] [PubMed]
- Song, S.A.; Franco, R.A., Jr. Serial Intralesional Steroid Injection for Subglottic Stenosis. Laryngoscope 2020, 130, 698–701. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, M.R.; Coughlin, A.R.; Dailey, S.H. Serial Office-based Steroid Injections for Treatment of Idiopathic Subglottic Stenosis. Laryngoscope 2017, 127, 2475–2481. [Google Scholar] [CrossRef]
- Woliansky, J.; Phyland, D.; Paddle, P. Systemic Safety of Serial Intralesional Steroid Injection for Subglottic Stenosis. Laryngoscope 2019, 129, 1634–1639. [Google Scholar] [CrossRef] [PubMed]
- Gelbard, A.; Anderson, C.; Berry, L.D.; Amin, M.R.; Benninger, M.S.; Blumin, J.H.; Bock, J.M.; Bryson, P.C.; Castellanos, P.F.; Chen, S.-C.; et al. Comparative Treatment Outcomes for Patients With Idiopathic Subglottic Stenosis. JAMA Otolaryngol. Neck Surg. 2020, 146, 20–29. [Google Scholar] [CrossRef] [Green Version]
- Maldonado, F.; Loiselle, A.; DePew, Z.S.; Edell, E.S.; Ekbom, D.C.; Malinchoc, M.; Hagen, C.E.; Alon, E.; Kasperbauer, J.L. Idiopathic Subglottic Stenosis: An Evolving Therapeutic Algorithm. Laryngoscope 2014, 124, 498–503. [Google Scholar] [CrossRef]
- Yokoi, A.; Nakao, M.; Bitoh, Y.; Arai, H.; Oshima, Y.; Nishijima, E. Treatment of Postoperative Tracheal Granulation Tissue with Inhaled Budesonide in Congenital Tracheal Stenosis. J. Pediatr. Surg. 2014, 49, 293–295. [Google Scholar] [CrossRef]
- Alrabiah, A.; Alsayed, A.; Aljasser, A.; Zakzouk, A.; Habib, S.S.; Almohizea, M.; Bukhari, M.; Alammar, A. Effect of Inhaled Fluticasone Propionate on Laryngotracheal Stenosis after Balloon Dilation: A Randomized Controlled Trial. Eur. Arch. Oto-Rhino-Laryngol. 2021, 278, 1505–1513. [Google Scholar] [CrossRef] [PubMed]
- Frank-Ito, D.O.; Cohen, S.M. Orally Inhaled Drug Particle Transport in Computerized Models of Laryngotracheal Stenosis. Otolaryngol. Neck Surg. 2021, 164, 829–840. [Google Scholar] [CrossRef]
- Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; Sox, H.; Riley, D.; CARE Group. The CARE Guidelines: Consensus-Based Clinical Case Report Guideline Development. J. Clin. Epidemiol. 2014, 67, 46–51. [Google Scholar] [CrossRef]
- Lizal, F.; Elcner, J.; Hopke, P.K.; Jedelsky, J.; Jicha, M. Development of a Realistic Human Airway Model. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2012, 226, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Lizal, F.; Belka, M.; Adam, J.; Jedelsky, J.; Jicha, M. A Method for in Vitro Regional Aerosol Deposition Measurement in a Model of the Human Tracheobronchial Tree by the Positron Emission Tomography. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2015, 229, 750–757. [Google Scholar] [CrossRef] [PubMed]
- Koullapis, P.; Kassinos, S.C.; Muela, J.; Perez-Segarra, C.; Rigola, J.; Lehmkuhl, O.; Cui, Y.; Sommerfeld, M.; Elcner, J.; Jicha, M. Regional Aerosol Deposition in the Human Airways: The SimInhale Benchmark Case and a Critical Assessment of in Silico Methods. Eur. J. Pharm. Sci. 2018, 113, 77–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, K.-H.; Cheng, Y.-S.; Yeh, H.-C.; Swift, D.L. Measurements of Airway Dimensions and Calculation of Mass Transfer Characteristics of the Human Oral Passage. J. Biomech. Eng. 1997, 119, 476–482. [Google Scholar] [CrossRef]
- Das, P.; Nof, E.; Amirav, I.; Kassinos, S.C.; Sznitman, J. Targeting Inhaled Aerosol Delivery to Upper Airways in Children: Insight from Computational Fluid Dynamics (CFD). PLoS ONE 2018, 13, e0207711. [Google Scholar] [CrossRef] [Green Version]
- Inthavong, K.; Ma, J.; Shang, Y.; Dong, J.; Chetty, A.S.R.; Tu, J.; Frank-Ito, D. Geometry and Airflow Dynamics Analysis in the Nasal Cavity during Inhalation. Clin. Biomech. 2019, 66, 97–106. [Google Scholar] [CrossRef]
- Kleinstreuer, C.; Zhang, Z. Airflow and Particle Transport in the Human Respiratory System. Annu. Rev. Fluid Mech. 2010, 42, 301–334. [Google Scholar] [CrossRef]
- Martonen, T.B.; Zhang, Z.; Lessmann, R.C. Fluid Dynamics of the Human Larynx and Upper Tracheobronchial Airways. Aerosol Sci. Technol. 1993, 19, 133–156. [Google Scholar] [CrossRef]
- Tu, J.; Inthavong, K.; Ahmadi, G. Computational Fluid and Particle Dynamics in the Human Respiratory System; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2012; ISBN 9400744870. [Google Scholar]
- Oliveira, R.F.; Ferreira, A.C.; Teixeira, S.F.; Teixeira, J.C.; Marques, H.C. PMDI Spray Plume Analysis: A CFD Study. In Proceedings of the World Congress on Engineering, London, UK, 3–5 July 2013; Volume 3, pp. 1–6. [Google Scholar]
- Ahookhosh, K.; Saidi, M.; Mohammadpourfard, M.; Aminfar, H.; Hamishehkar, H.; Farnoud, A.; Schmid, O. Flow Structure and Particle Deposition Analyses for Optimization of a Pressurized Metered Dose Inhaler (PMDI) in a Model of Tracheobronchial Airway. Eur. J. Pharm. Sci. 2021, 164, 105911. [Google Scholar] [CrossRef]
- Gosman, R.E.; Sicard, R.M.; Cohen, S.M.; Frank-Ito, D.O. Comparison of Inhaled Drug Delivery in Patients With One-and Two-level Laryngotracheal Stenosis. Laryngoscope 2022, 133, 366–374. [Google Scholar] [CrossRef]
- Taherian, S.; Rahai, H.R.; Bonifacio, J.; Gomez, B.Z.; Waddington, T. Particulate Deposition in a Patient With Tracheal Stenosis. J. Eng. Sci. Med. Diagn. Ther. 2017, 1, 011005. [Google Scholar] [CrossRef] [Green Version]
- Taherian, S.; Rahai, H.; Gomez, B.Z.; Waddington, T.; Bonifacio, J.R. Tracheal Stenosis: A CFD Approach for Evaluation of Drug Delivery. In Proceedings of the ASME International Mechanical Engineering Congress and Exposition; American Society of Mechanical Engineers: New York, NY, USA, 2015; Volume 57380, p. V003T03A096. [Google Scholar]
- Longest, P.; Tian, G.; Walenga, R.L.; Hindle, M. Comparing MDI and DPI Aerosol Deposition Using in Vitro Experiments and a New Stochastic Individual Path (SIP) Model of the Conducting Airways. Pharm. Res. 2012, 29, 1670–1688. [Google Scholar] [CrossRef] [PubMed]
- Rau, J.L. Practical Problems with Aerosol Therapy in COPD. Respir. Care 2006, 51, 158–172. [Google Scholar]
- Scholfield, D.W.; Warner, E.; Ahmed, J.; Ghufoor, K. Subglottic and Tracheal Stenosis Associated with Coronavirus Disease 2019. J. Laryngol. Otol. 2021, 135, 656–658. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.J.; Gochman, G.E.; Stasyuk, A.; Del Rosario, K.L.; Cates, D.J.; Madden, L.L.; Young, V.N. Interventions and Outcomes in Glottic Versus Multi-level Airway Stenosis: A Multi-institutional Review. Laryngoscope 2022, 133, 528–534. [Google Scholar] [CrossRef]
- Lewis, S.; Earley, M.; Rosenfeld, R.; Silverman, J. Systematic Review for Surgical Treatment of Adult and Adolescent Laryngotracheal Stenosis. Laryngoscope 2017, 127, 191–198. [Google Scholar] [CrossRef]
- Saghebi, S.R.; Zangi, M.; Tajali, T.; Farzanegan, R.; Farsad, S.M.; Abbasidezfouli, A.; Sheikhy, K.; Shadmehr, M.B. The Role of T-Tubes in the Management of Airway Stenosis. Eur. J. Cardio-Thoracic. Surg. 2013, 43, 934–939. [Google Scholar] [CrossRef] [Green Version]
- Hu, H.; Wu, F.; Zhang, J.; Chen, E. Treatment of Secondary Benign Airway Stenosis after Tracheotomy with Montgomery T-Tube. Math. Biosci. Eng. 2019, 16, 7839–7849. [Google Scholar] [CrossRef]
- Ko, P.; Liu, C.; Wu, Y.; Chao, Y.; Hsieh, M.; Wu, C.; Wang, C.; Liu, Y.; Liu, H. Granulation Formation Following Tracheal Stenosis Stenting: Influence of Stent Position. Laryngoscope 2009, 119, 2331–2336. [Google Scholar] [CrossRef]








| Case Num. | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Age | 60 | 58 | 58 | 49 |
| Sex | M | F | F | F |
| Clinical presentation | Dyspnea, stridor | Dyspnea, stridor aphonia | Dyspnea, stridor | Dyspnea, aphonia |
| Etiology of stenosis | Prolonged intubation and tracheostomy | Prolonged intubation and tracheostomy | Prolonged intubation and tracheostomy | Irradiation induced stenosis |
| Laryngeal Findings at presentation | Subglottic stenosis | Bilateral vocal fold immobility, multilevel glottic, subglottic and tracheal stenosis | Posterior glottic stenosis and subglottic stenosis | Glottic, subglottic and tracheal stenosis |
| Cotton Myers grade at presentation | 3 | 3 | 2 | 3 |
| Surgical Interventions | Co2 laser radial incisions, balloon dilation, granulation tissue resection, stent insertion | Posterior cricoid split with placement of costal graft, balloon dilation, stent insertion | Balloon dilation, submucosal arytenoidectomy and lateralization stent insertion | Balloon dilation, granulation tissue resection, stent insertion |
| Cotton Myers grade following interventions | 1 | 1 | 1 | 1 |
| TRCI treatment length (months) | 6 | 16 | 10 | 10 |
| Cotton Myers grade following TRCI treatment | 1 | 1 | 1 | 1 |
| Decannulation | Y | N | Y | Y |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allon, R.; Bhardwaj, S.; Sznitman, J.; Shoffel-Havakuk, H.; Pinhas, S.; Zloczower, E.; Shapira-Galitz, Y.; Lahav, Y. A Novel Trans-Tracheostomal Retrograde Inhalation Technique Increases Subglottic Drug Deposition Compared to Traditional Trans-Oral Inhalation. Pharmaceutics 2023, 15, 903. https://doi.org/10.3390/pharmaceutics15030903
Allon R, Bhardwaj S, Sznitman J, Shoffel-Havakuk H, Pinhas S, Zloczower E, Shapira-Galitz Y, Lahav Y. A Novel Trans-Tracheostomal Retrograde Inhalation Technique Increases Subglottic Drug Deposition Compared to Traditional Trans-Oral Inhalation. Pharmaceutics. 2023; 15(3):903. https://doi.org/10.3390/pharmaceutics15030903
Chicago/Turabian StyleAllon, Raviv, Saurabh Bhardwaj, Josué Sznitman, Hagit Shoffel-Havakuk, Sapir Pinhas, Elchanan Zloczower, Yael Shapira-Galitz, and Yonatan Lahav. 2023. "A Novel Trans-Tracheostomal Retrograde Inhalation Technique Increases Subglottic Drug Deposition Compared to Traditional Trans-Oral Inhalation" Pharmaceutics 15, no. 3: 903. https://doi.org/10.3390/pharmaceutics15030903






