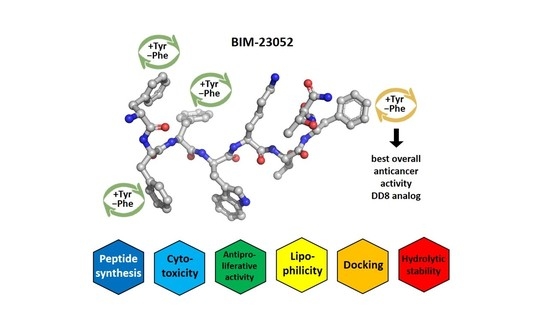
Synthesis, Antiproliferative Effect and In Silico LogP Prediction of BIM-23052 Analogs Containing Tyr Instead of Phe
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Peptide Synthesis and Chemical Analysis
- -
- amino acid/HBTU/DIPEA/resin 3/3/9/1;
- -
- amino acid/DIC/resin 3/3/1 with a catalytic amount of DMAP.
| Time (min) | 0.01 | 10.00 | 15.00 | 15.50 | 22.00 |
| m.ph. А (%) | 80 | 5 | 5 | 80 | 80 |
| m.ph. B (%) | 20 | 95 | 95 | 20 | 20 |
- -
- a column Agilent Poroshell 120, 100 × 4.6 mm;
- -
- elution flow: 0.30 mL/min;
- -
- temperature of column 40 °C.
2.3. Cell Lines
2.4. Safety Test (3T3 NRU Assay)
2.5. Cell Viability (MTT-Assay)
2.6. In Silico LogP Prediction
3. Results
3.1. Synthesis of Aimed Peptides
3.2. Cytotoxicity
3.3. Antiproliferative Activity
3.4. Selectivity
3.5. LogP Prediction
3.6. Hydrolytic Stability
- (i)
- Buffer with pH 2.0–6.57 g KCl was dissolved in water (CO2 free) and 119.0 mL 0.1 mol/L HCl was added. The obtained solution was completed to 1000.0 mL with distilled water (dH2O).
- (ii)
- Buffer with pH 9.0–1000.0 mL of solution I was mixed with 420.0 mL of solution II. Solution I: 6.18 g H3BO3 was dissolved in 0.1 mol/L KCl and was completed to 1000.0 mL with the same solvent; Solution II: 0.1 mol/L NaOH.
3.7. Docking Studies
4. Discussion
4.1. BIM-23052 Analogs Synthesis and Characterization
4.2. Cytotoxicity, Docking Calculations, Antiproliferative Effect and Lipophilicity
4.3. Hydrolytic Stability
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kath, R.; Höffken, K. (Eds.) The Significance of Somatostatin Analogues in the Antiproliferative Treatment of Carcinomas BT—Peptides in Oncology III; Springer: Berlin/Heidelberg, Germany, 2000; pp. 23–43. [Google Scholar]
- Breder, C.D.; Yamada, Y.; Yasuda, K.; Seino, S.; Saper, C.B.; Bell, G.I. Differential Expression of Somatostatin Receptor Subtypes in Brain. J. Neurosci. 1992, 12, 3920–3934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reisine, T.; Bell, G.I. Molecular Biology of Somatostatin Receptors. Endocr. Rev. 1995, 16, 427–442. [Google Scholar] [CrossRef] [PubMed]
- Patel, Y.C. Molecular Pharmacology of Somatostatin Receptor Subtypes. J. Endocrinol. Investig. 1997, 20, 348–367. [Google Scholar] [CrossRef]
- Meyerhof, W. The Elucidation of Somatostatin Receptor Functions: A Current View BT—Reviews of Physiology Biochemistry and Pharmacology; Springer: Berlin/Heidelberg, Germany, 1998; Volume 133, pp. 55–108. ISBN 978-3-540-69676-6. [Google Scholar]
- Patel, Y.C. Somatostatin and Its Receptor Family. Front. Neuroendocrinol. 1999, 20, 157–198. [Google Scholar] [CrossRef] [PubMed]
- Bruns, C.; Weckbecker, G.; Raulf, F.; Kaupmann, K.; Schooeffter, P.; Hoyeroyer, D.; Lübbert, H. Molecular Pharmacology of Somatostatin-Receptor Subtypes. Ann. N. Y. Acad. Sci. 1994, 733, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, S.; Reubi, J.C.; Kalkner, K.M.; Laissue, J.A.; Horisberger, U.; Olerud, C.; Westlin, J.E. Metastatic Hormone-Refractory Prostatic Adenocarcinoma Expresses Somatostatin Receptors and Is Visualized in Vivo by [111In]-Labeled DTPA-D-[Phe1]-Octreotide Scintigraphy. Cancer Res. 1995, 55, 5805s–5810s. [Google Scholar] [PubMed]
- Reubi, J.C.; Waser, B.; Schaer, J.C.; Markwalder, R. Somatostatin Receptors in Human Prostate and Prostate Cancer. J. Clin. Endocrinol. Metab. 1995, 80, 2806–2814. [Google Scholar] [CrossRef]
- Patel, Y.C.; Greenwood, M.T.; Panetta, R.; Demchyshyn, L.; Niznik, H.; Srikant, C.B. The Somatostatin Receptor Family. Life Sci. 1995, 57, 1249–1265. [Google Scholar] [CrossRef]
- Reubi, J.; Waser, B.; Schaer, J.-C.; Laissue, J.A. Somatostatin Receptor Sst1–Sst5 Expression in Normal and Neoplastic Human Tissues Using Receptor Autoradiography with Subtype-Selective Ligands. Eur. J. Nucl. Med. 2001, 28, 836–846. [Google Scholar] [CrossRef]
- Susini, C.; Buscail, L. Rationale for the Use of Somatostatin Analogs as Antitumor Agents. Ann. Oncol. 2006, 17, 1733–1742. [Google Scholar] [CrossRef]
- Weckbecker, G.; Lewis, I.; Albert, R.; Schmid, H.A.; Hoyer, D.; Bruns, C. Opportunities in Somatostatin Research: Biological, Chemical and Therapeutic Aspects. Nat. Rev. Drug Discov. 2003, 2, 999–1017. [Google Scholar] [CrossRef]
- Coy, D.H.; Murphy, W.A. Linear Somatostatin Analogs. U.S. Patent 5633263A, 27 May 1997. [Google Scholar]
- Veber, D.F.; Freidinger, R.M.; Perlow, D.S.; Paleveda, W.J.; Holly, F.W.; Strachan, R.G.; Nutt, R.F.; Arison, B.H.; Homnick, C.; Randall, W.C.; et al. A Potent Cyclic Hexapeptide Analogue of Somatostatin. Nature 1981, 292, 55–58. [Google Scholar] [CrossRef]
- Modlin, I.M.; Pavel, M.; Kidd, M.; Gustafsson, B.I. Review Article: Somatostatin Analogues in the Treatment of Gastroenteropancreatic Neuroendocrine (Carcinoid) Tumours. Aliment. Pharmacol. Ther. 2010, 31, 169–188. [Google Scholar] [CrossRef]
- Appetecchia, M.; Baldelli, R. Somatostatin Analogues in the Treatment of Gastroenteropancreatic Neuroendocrine Tumours, Current Aspects and New Perspectives. J. Exp. Clin. Cancer Res. 2010, 29, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strosberg, J.; Kvols, L. Antiproliferative Effect of Somatostatin Analogs in Gastroenteropancreatic Neuroendocrine Tumors. World J. Gastroenterol. 2010, 16, 2963–2970. [Google Scholar] [CrossRef]
- Zou, Y.; Xiao, X.; Li, Y.; Zhou, T. Somatostatin Analogues Inhibit Cancer Cell Proliferation in an SSTR2-Dependent Manner via Both Cytostatic and Cytotoxic Pathways. Oncol. Rep. 2009, 21, 379–386. [Google Scholar]
- Pyronnet, S.; Bousquet, C.; Najib, S.; Azar, R.; Laklai, H.; Susini, C. Antitumor Effects of Somatostatin. Mol. Cell. Endocrinol. 2008, 286, 230–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Staykova, S.; Naydenova, E.; Wesselinova, D.; Kalistratova, A.; Vezenkov, L. Synthesis and In Vitro Study of the Anticancer Activity of New Analogs of Octreotide. Protein Pept. Lett. 2012, 19, 1257–1262. [Google Scholar] [CrossRef] [PubMed]
- Staykova, S.; Naydenova, E.; Wesselinova, D.; Vezenkov, L. Synthesis and in Vitro Antitumor Activity of New Linear Somatostatin Analogs. J. Univ. Chem. Technol. Metall. 2012, 47, 297–302. [Google Scholar]
- Staykova, S.T.; Wesselinova, D.W.; Vezenkov, L.T.; Naydenova, E.D. Synthesis and in Vitro Antitumor Activity of New Octapeptide Analogs of Somatostatin Containing Unnatural Amino Acids. Amino Acids 2015, 47, 1007–1013. [Google Scholar] [CrossRef]
- Allaw, M.B.; Switchenko, J.M.; Khalil, L.; Wu, C.; Alese, O.B.; Akce, M.; Draper, A.; Jones, A.T.; El-Rayes, B.; Shaib, W. Comparing Somatostatin Analogs in the Treatment of Advanced Gastroenteropancreatic Neuroendocrine Tumors. Oncology 2022, 100, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Gomes-Porras, M.; Cárdenas-Salas, J.; Álvarez-Escolá, C. Somatostatin Analogs in Clinical Practice: A Review. Int. J. Mol. Sci. 2020, 21, 1682. [Google Scholar] [CrossRef] [Green Version]
- Naydenova, E.; Wesselinova, D.; Staykova, S.; Danalev, D.; Dzimbova, T. Synthesis, in Vitro Biological Activity and Docking of New Analogs of BIM-23052 Containing Unnatural Amino Acids. Amino Acids 2019, 51, 1247–1257. [Google Scholar] [CrossRef] [PubMed]
- Danalev, D.; Borisova, D.; Yaneva, S.; Georgieva, M.; Balacheva, A.; Dzimbova, T.; Iliev, I.; Pajpanova, T.; Zaharieva, Z.; Givechev, I.; et al. Synthesis, in Vitro Biological Activity, Hydrolytic Stability and Docking of New Analogs of BIM-23052 Containing Halogenated Amino Acids. Amino Acids 2020, 52, 1581–1592. [Google Scholar] [CrossRef] [PubMed]
- Bhal, S.K. Log P—Making Sense of the Value. Adv. Chem. Dev. 2007, 1–4. [Google Scholar]
- Lipinski, C.A.; Lombardo, F.; Dominy, B.W.; Feeney, P.J. Experimental and Computational Approaches to Estimate Solubility and Permeability in Drug Discovery and Development Settings. Adv. Drug Deliv. Rev. 1997, 23, 3, reprinted in Adv. Drug Deliv. Rev. 2001, 46, 3–26. [Google Scholar] [CrossRef]
- Borenfreund, E.; Puerner, J.A. Toxicity Determined in Vitro by Morphological Alterations and Neutral Red Absorption. Toxicol. Lett. 1985, 24, 119–124. [Google Scholar] [CrossRef]
- Spielmann, H.; Balls, M.; Dupuis, J.; Pape, W.J.; Pechovitch, G.; de Silva, O.; Holzhütter, H.-G.; Clothier, R.; Desolle, P.; Gerberick, F.; et al. The International EU/COLIPA In Vitro Phototoxicity Validation Study: Results of Phase II (Blind Trial). Part 1: The 3T3 NRU Phototoxicity Test. Toxicol. In Vitro 1998, 12, 305–327. [Google Scholar] [CrossRef]
- Mosmann, T. Rapid Colorimetric Assay for Cellular Growth and Survival: Application to Proliferation and Cytotoxicity Assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef]
- Froimowitz, M. HyperChem: A Software Package for Computational Chemistry and Molecular Modeling. Biotechniques 1993, 14, 1010–1013. [Google Scholar]
- Dewar, M.J.S.; Zoebisch, E.G.; Healy, E.F.; Stewart, J.J.P. Development and Use of Quantum Mechanical Molecular Models. 76. AM1: A New General Purpose Quantum Mechanical Molecular Model. J. Am. Chem. Soc. 1985, 107, 3902–3909. [Google Scholar] [CrossRef]
- Pietro, W.J.; Francl, M.M.; Hehre, W.J.; DeFrees, D.J.; Pople, J.A.; Binkley, J.S. Self-Consistent Molecular Orbital Methods. 24. Supplemented Small Split-Valence Basis Sets for Second-Row Elements. J. Am. Chem. Soc. 1982, 104, 5039–5048. [Google Scholar] [CrossRef]
- Frisch, M.J.; Trucks, G.W.; Schlegel, H.B.; Scuseria, G.E.; Robb, M.A.; Cheeseman, J.R.; Scalmani, G.; Barone, V.; Mennucci, B.; Petersson, G.A.; et al. Gaussian 09; Gaussian, Inc.: Wallingford, CT, USA, 2013. [Google Scholar]
- Møller, L.N.; Stidsen, C.E.; Hartmann, B.; Holst, J.J. Somatostatin Receptors. Biochim. Biophys. Acta Biomembr. 2003, 1616, 1–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naef, R. A Generally Applicable Computer Algorithm Based on the Group Additivity Method for the Calculation of Seven Molecular Descriptors: Heat of Combustion, LogPO/W, LogS, Refractivity, Polarizability, Toxicity and LogBB of Organic Compounds; Scope and Limits O. Molecules 2015, 20, 18279–18351. [Google Scholar] [CrossRef] [Green Version]
- Tao, P.; Wang, R.; Lai, L. Calculating Partition Coefficients of Peptides by the Addition Method. Mol. Model. Annu. 1999, 5, 189–195. [Google Scholar] [CrossRef]
- Wolfenden, R. Experimental Measures of Amino Acid Hydrophobicity and the Topology of Transmembrane and Globular Proteins. J. Gen. Physiol. 2007, 129, 357–362. [Google Scholar] [CrossRef] [Green Version]





| Code | Structure | Molecular Formula | Mw Exact | [M + H]+ Found | RT (min) | M.p. (°C) | |
|---|---|---|---|---|---|---|---|
| D11 | D-Tyr1-Phe-Phe-D-Trp-Lys-Thr-Phe-Thr-NH2 | C61H75N11O11 | 1137.57 | 1138.70 | 3.531 | 121–123 | +8 |
| DD8 | D-Phe-Phe-Phe-D-Trp-Lys-Thr-Tyr7-Thr-NH2 | C61H75N11O11 | 1137.57 | 1138.65 | 6.845 | 108–110 | −10 |
| D101 | D-Phe-Tyr2-Tyr3-D-Trp-Lys-Thr-Phe-Thr-NH2 | C61H75N11O12 | 1153.56 | 1154.60 | 4.322 | 118–120 | −74 |
| D61 | D-Phe-Tyr2-Tyr3-D-Trp-Lys-Thr-Tyr7-Thr-NH2 | C61H75N11O13 | 1169.55 | 1170.80 | 4.009 | 123–125 | +2 |
| D91 | D-Tyr1-Tyr2-Tyr3-D-Trp-Lys-Thr-Tyr7-Thr-NH2 | C61H75N11O14 | 1185.55 | 1186.80 | 3.420 | 125–127 | −46 |
| Code | Structure | Molecular Formula | Mw Exact | [M + H]+ Found | RT (min) | M.p. (°C) | |
|---|---|---|---|---|---|---|---|
| D6 | L-Tyr1-Tyr2-Tyr3-D-Trp-Lys-Thr-Phe-Thr-NH2 | C61H75N11O13 | 1169.56 | 1170.60 | 3.567 | 110–112 | −20 |
| D7 | L-Tyr1-Tyr2-Phe-D-Trp-Lys-Thr-Tyr7-Thr-NH2 | C61H75N11O13 | 1169.56 | 1170.65 | 1.869 | 81–83 | −28 |
| D9 | L-Tyr1-Tyr2-Tyr3-D-Trp-Lys-Thr-Tyr7-Thr-NH2 | C61H75N11O14 | 1185.55 | 1186.65 | 1.606 | 78–80 | −16 |
| Compounds | Mean IC50 ± SD (μm) | |||
|---|---|---|---|---|
| Cytotoxicity | Antiproliferative Effect | |||
| BALB 3T3 | MCF-10A | MCF-7 | MDA-MB-231 | |
| BIM-23052 | 483.10 ± 32.11 | 203.80 ± 6.32 | 120.00 ± 6.53 | 334.80 ± 15.40 |
| D11 | 1634.40 ± 51.18 | 864.04 ± 52.27 | 873.15 ± 26.55 | 1722.97 ± 58.60 |
| D6 | 1324.11 ± 53.7 | 190.98 ± 6.8 | 358.87 ± 16.13 | 290.54 ± 12.68 |
| D7 | 736.91 ± 19.98 | 432.82 ± 23.15 | 402.84 ± 24.93 | 781.99 ± 18.97 |
| DD8 | 482.93 ± 33.88 | 161.28 ± 7.97 | 235.43 ± 14.3 | 240.89 ± 13.36 |
| D61 | 1200.52 ± 100.13 | 554.69 ± 21.28 | 426.42 ± 23.87 | 798.18 ± 24.38 |
| D9 | 1429.3 ± 40.72 | 394.97 ± 15.29 | 476.81 ± 31.44 | 1411.66 ± 19.08 |
| D91 | 974.67 ± 81.71 | 540.27 ± 27.21 | 527.48 ± 54.19 | 849.45 ± 21.21 |
| D101 | 1401.35 ± 52.31 | 604.46 ± 24.66 | 717.13 ± 20.76 | 1399.37± 19.98 |
| Cisplatin | 537.35 ± 40.27 | 64.35 ± 2.11 | 43.07 ± 3.16 | 6.94 ± 0.47 |
| Code | SI * | |
|---|---|---|
| MCF-7 | MDA-MB-231 | |
| BIM-23052 | 1.7 | 0.61 |
| D11 | 0.99 | 0.50 |
| D6 | 0.53 | 0.66 |
| D7 | 1.07 | 0.55 |
| DD8 | 0.69 | 0.67 |
| D61 | 1.3 | 0.69 |
| D9 | 0.83 | 0.28 |
| D91 | 1.02 | 0.64 |
| D101 | 0.84 | 0.43 |
| Cisplatin | 1.49 | 9.27 |
| Code | Structure | LogP | |
|---|---|---|---|
| Non-Pre-Optimized Structures | Pre-Optimized Structures | ||
| BIM-23052 | H-D-Phe-Phe-Phe-D-Trp-Lys-Thr-Phe-Thr-NH2 | 0.74 | 0.83 |
| DD8 | H-D-Phe-Phe-Phe-D-Trp-Lys-Thr-Tyr7-Thr-NH2 | 0.46 | 1.17 |
| D101 | H-D-Phe-Tyr2-Tyr3-D-Trp-Lys-Thr-Phe-Thr-NH2 | 0.17 | 0.88 |
| D61 | H-D-Phe-Tyr2-Tyr3-D-Trp-Lys-Thr-Tyr7-Thr-NH2 | −0.11 | 0.60 |
| D9 | H-L-Tyr1-Tyr2-Tyr3-D-Trp-Lys-Thr-Tyr7-Thr-NH2 | −0.40 | 0.38 |
| D91 | H-D-Tyr1-Tyr2-Tyr3-D-Trp-Lys-Thr-Tyr7-Thr-NH2 | −0.40 | 0.31 |
| D6 | H-L-Tyr1-Tyr2-Tyr3-D-Trp-Lys-Thr-Phe-Thr-NH2 | −0.11 | 0.55 |
| D7 | H-L-Tyr1-Tyr2-Phe-D-Trp-Lys-Thr-Tyr7-Thr-NH2 | 0.17 | 0.55 |
| D11 | H- D-Tyr1-Phe-Phe-D-Trp-Lys-Thr-Phe-Thr-NH2 | 0.46 | 1.14 |
| Code | % Non-Hydrolyzed Product |
|---|---|
| D6 | 47 |
| D61 | 74 |
| D7 | 54 |
| DD8 | 72 |
| D9 | 78 |
| D91 | 59 |
| D11 | 61 |
| D101 | 70 |
| Ligand | Total Energies of the Ligand with the Respective Receptor Type, kJ mol−1 | ||||
|---|---|---|---|---|---|
| SSTR1 | SSTR2 | SSTR3 | SSTR4 | SSTR5 | |
| S1 * | −175.29 | −159.55 | −322.74 | −234.00 | −283.73 |
| D6 | −114.29 | −137.57 | −295.45 | −251.96 | −240.35 |
| DD8 | −236.00 | −189.25 | −152.94 | −147.97 | −125.25 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Danalev, D.; Iliev, I.; Dobrev, S.; Angelova, S.; Petrin, S.; Dzimbova, T.; Ivanova, E.; Borisova, D.; Naydenova, E. Synthesis, Antiproliferative Effect and In Silico LogP Prediction of BIM-23052 Analogs Containing Tyr Instead of Phe. Pharmaceutics 2023, 15, 1123. https://doi.org/10.3390/pharmaceutics15041123
Danalev D, Iliev I, Dobrev S, Angelova S, Petrin S, Dzimbova T, Ivanova E, Borisova D, Naydenova E. Synthesis, Antiproliferative Effect and In Silico LogP Prediction of BIM-23052 Analogs Containing Tyr Instead of Phe. Pharmaceutics. 2023; 15(4):1123. https://doi.org/10.3390/pharmaceutics15041123
Chicago/Turabian StyleDanalev, Dancho, Ivan Iliev, Stefan Dobrev, Silvia Angelova, Stoiko Petrin, Tatyana Dzimbova, Elena Ivanova, Dessislava Borisova, and Emilia Naydenova. 2023. "Synthesis, Antiproliferative Effect and In Silico LogP Prediction of BIM-23052 Analogs Containing Tyr Instead of Phe" Pharmaceutics 15, no. 4: 1123. https://doi.org/10.3390/pharmaceutics15041123