3D Printed Pharmaceutical Systems for Personalized Treatment in Metabolic Syndrome
Abstract
:1. Introduction
2. Personalized Medicine and Its Significance in MS
2.1. Role of Pharmacogenomics/Metabolic Profiling to Determine Personalized Medicine
2.2. Role of 3D Printing Technology in the Design of Personalized Medicine
3. Types of 3D Printing Techniques Utilized in Product Development
| 3D Printing Technique | Category | Feed Material | Polymers/Excipients Used | Other Components | Ref. |
|---|---|---|---|---|---|
| FDM | Extrusion based | Drug loaded filament extruded through nozzle | Thermoplastic materials, such as PLA, PVA. Polymers, such as HPMC, Eudragit, and PVP. | Lubricant, filler and plasticizer. E.g., TEC, Talc, PEG 400, mannitol. | [70,71] |
| PAM | Extrusion based | Formulation paste filled in syringe extruded through nozzle | PVP, HPC, HPMC, EC, Carbopol, PVA, PEG. | Fillers, binders and disintegrants. E.g., mannitol, sodium starch glycolate, avicel. | [72,73] |
| Inkjet printing | Liquid based | Ink jetting on substrate | PLGA (poly lacto-co-glycolic acid) and PLA (poly-L-lactide), PEG/HPMC. | Substrate material: HPMC. PVA-CMC. Ink material: PEG 400, glycerol, ethanol. | [74] |
| Binder jet printing | Powder based | Binder jetting | PEO, Eudragit, PVP, EC, HPMC, mannitol, maltitol, maltodextrin | Binder: PCL, PVP K25, PVP K30. | [75] |
| SLA | Liquid based | Vat—photo polymerization | Monomers: polyethylene glycoldiacrylate (PEGDA), poly(propylene fumarate): diethyl fumarate (50:50), Dental SG resin, Elastic Resin | Photoinitiator: diphenyl(2,4,6-trimethylbenzoyl) phosphine oxide, Irgacure 184 (1-Hydroxycyclohexyl phenyl ketone) | [71,76] |
| SLS | Powder based | Laser-powder bed fusion. | PEO, Eudragit EPO, PVA, PEG, Kollicoat MAE, Kollicoat IR, Kollidon VA64, Eudragit RL, HPMC, Ethylcellulose, | Lactose monohydrate and microcrystalline cellulose, silicon dioxide, talc, Stearic acid, mannitol, cyclodextrin | [71,77] |
3.1. Inkjet Printing
3.2. Binder Jet Printing
3.3. Fused Deposition Modeling (FDM) 3D Printing
3.4. Pressure-Assisted Microsyringes (PAM) 3D Printing
3.5. Stereolithography (SLA)
3.6. Selective Laser Sintering (SLS)
4. Drug Delivery Approaches for Treatment of MS Utilizing 3D Printing Techniques
4.1. PAM-Based 3D Printing Technique Utilized in Drug Delivery of MS
4.2. FDM-Based 3D Printing Technique Utilized in Drug Delivery of MS
4.3. Inkjet and Laser-Based 3D Printing Technique Utilized in Drug Delivery of MS
5. Conclusions and Future Prospectives
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PM | Personalized medicine |
| MS | Metabolic syndrome |
| 3D | Three-dimensional |
| HDL | High-density lipoprotein |
| CVD | Cardiovascular disease |
| IND | Investigational New Drug |
| MED | Melt Extrusion Deposition |
| US-FDA | United States Food and Drug Administration |
| FDM | Fused deposition modelling |
| PAM | Pressure assisted micro syringes |
| SLA | Stereolithographic |
| SLS | Selective laser sintering |
| ODF | Orodispersible films |
| PVA | Polyvinyl alcohol |
| PLA | Polylactic acid |
| PVP | Polyvinylpyrrolidone |
| HPC | Hydroxypropyl cellulose |
| HPMC | Hydroxypropyl methylcellulose |
| EC | Ethylcellulose |
| HPMCAS | Hydroxypropyl methylcellulose acetate succinate |
| SNEDDS | Self-nano-emulsifying drug delivery system |
| PEGDA | Polyethylene glycoldiacrylate |
| NVP | N-vinyl-2-pyrrolidone |
| PEG | Polyethylene glycol |
| μCT | Microfocus computed tomography |
| XRD | X-ray diffractograms |
| PEO | Polyethylene oxide |
| APIs | Active pharmaceutical ingredients. |
References
- Reaven, G.M. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 1988, 37, 1595–1607. [Google Scholar] [CrossRef]
- O’Neill, S.; O’Driscoll, L. Metabolic syndrome: A closer look at the growing epidemic and its associated pathologies. Obes. Rev. 2015, 16, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Alberti, K.G.; Zimmet, P.; Shaw, J. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- do Vale Moreira, N.C.; Hussain, A.; Bhowmik, B.; Mdala, I.; Siddiquee, T.; Fernandes, V.O.; Montenegro Júnior, R.M.; Meyer, H.E. Prevalence of Metabolic Syndrome by different definitions, and its association with type 2 diabetes, pre-diabetes, and cardiovascular disease risk in Brazil. Diabetes Metab. Syndr. 2020, 14, 1217–1224. [Google Scholar] [CrossRef]
- Ranasinghe, P.; Mathangasinghe, Y.; Jayawardena, R.; Hills, A.P.; Misra, A. Prevalence and trends of metabolic syndrome among adults in the asia-pacific region: A systematic review. BMC Public Health 2017, 17, 101. [Google Scholar] [CrossRef] [Green Version]
- Friend, A.; Craig, L.; Turner, S. The prevalence of metabolic syndrome in children: A systematic review of the literature. Metab. Syndr. Relat. Disord. 2013, 11, 71–80. [Google Scholar] [CrossRef]
- Li, X.; Cao, C.; Tang, X.; Yan, X.; Zhou, H.; Liu, J.; Ji, L.; Yang, X.; Zhou, Z. Prevalence of Metabolic Syndrome and Its Determinants in Newly-Diagnosed Adult-Onset Diabetes in China: A Multi-Center, Cross-Sectional Survey. Front. Endocrinol. 2019, 10, 661. [Google Scholar] [CrossRef]
- Yadav, D.; Mahajan, S.; Subramanian, S.K.; Bisen, P.S.; Chung, C.H.; Prasad, G.B. Prevalence of metabolic syndrome in type 2 diabetes mellitus using NCEP-ATPIII, IDF and WHO definition and its agreement in Gwalior Chambal region of Central India. Glob. J. Health Sci. 2013, 5, 142–155. [Google Scholar] [CrossRef] [Green Version]
- Al-Rubeaan, K.; Bawazeer, N.; Al Farsi, Y.; Youssef, A.M.; Al-Yahya, A.A.; AlQumaidi, H.; Al-Malki, B.M.; Naji, K.A.; Al-Shehri, K.; Al Rumaih, F.I. Prevalence of metabolic syndrome in Saudi Arabia—A cross sectional study. BMC Endocr. Disord. 2018, 18, 16. [Google Scholar] [CrossRef]
- Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [CrossRef]
- Al-Nozha, M.M.; Al-Mazrou, Y.Y.; Al-Maatouq, M.A.; Arafah, M.R.; Khalil, M.Z.; Khan, N.B.; Al-Marzouki, K.; Abdullah, M.A.; Al-Khadra, A.H.; Al-Harthi, S.S.; et al. Obesity in Saudi Arabia. Saudi Med. J. 2005, 26, 824–829. [Google Scholar]
- Al-Nozha, M.; Al-Khadra, A.; Arafah, M.R.; Al-Maatouq, M.A.; Khalil, M.Z.; Khan, N.B.; Al-Mazrou, Y.Y.; Al-Marzouki, K.; Al-Harthi, S.S.; Abdullah, M.; et al. Metabolic syndrome in Saudi Arabia. Saudi Med. J. 2005, 26, 1918–1925. [Google Scholar]
- Al-Rubean, K.; Youssef, A.M.; AlFarsi, Y.; Al-Sharqawi, A.H.; Bawazeer, N.; AlOtaibi, M.T.; AlRumaih, F.I.; Zaidi, M.S. Anthropometric cutoff values for predicting metabolic syndrome in a Saudi community: From the SAUDI-DM study. Ann. Saudi Med. 2017, 37, 21–30. [Google Scholar] [CrossRef] [Green Version]
- Litman, T. Personalized medicine-concepts, technologies, and applications in inflammatory skin diseases. Apmis 2019, 127, 386–424. [Google Scholar] [CrossRef]
- Prodan Žitnik, I.; Černe, D.; Mancini, I.; Simi, L.; Pazzagli, M.; Di Resta, C.; Podgornik, H.; Repič Lampret, B.; Trebušak Podkrajšek, K.; Sipeky, C.; et al. Personalized laboratory medicine: A patient-centered future approach. Clin. Chem. Lab. Med. 2018, 56, 1981–1991. [Google Scholar] [CrossRef] [Green Version]
- Florence, A.T.; Siepmann, J. Dosage forms for personlaized medicine: From the simple to the complex. In Modern Pharmaceutics, 5th ed.; Informa Healthcare USA, Inc.: New York, NY, USA, 2009; Volume 2, p. 493. [Google Scholar]
- Redekop, W.K.; Mladsi, D. The faces of personalized medicine: A framework for understanding its meaning and scope. Value Health 2013, 16, S4–S9. [Google Scholar] [CrossRef] [Green Version]
- Annas, G.J. Personalized medicine or public health? Bioethics, human rights, and choice. Rev. Port. Saúde Pública 2014, 32, 158–163. [Google Scholar] [CrossRef] [Green Version]
- Salari, P.; Larijani, B. Ethical Issues Surrounding Personalized Medicine: A Literature Review. Acta Med. Iran. 2017, 55, 209–217. [Google Scholar]
- Cohen, J.S. Ways to minimize adverse drug reactions. Individualized doses and common sense are key. Postgrad. Med. 1999, 106, 163–168, 171–172. [Google Scholar] [CrossRef]
- Herxheimer, A. How much drug in the tablet? Lancet 1991, 337, 346–348. [Google Scholar] [CrossRef]
- Florence, A.T.; Lee, V.H. Personalised medicines: More tailored drugs, more tailored delivery. Int. J. Pharm. 2011, 415, 29–33. [Google Scholar] [CrossRef]
- Lim, S.H.; Kathuria, H.; Tan, J.J.Y.; Kang, L. 3D printed drug delivery and testing systems—A passing fad or the future? Adv. Drug Deliv. Rev. 2018, 132, 139–168. [Google Scholar] [CrossRef] [PubMed]
- Khaled, S.A.; Burley, J.C.; Alexander, M.R.; Yang, J.; Roberts, C.J. 3D printing of five-in-one dose combination polypill with defined immediate and sustained release profiles. J. Control. Release 2015, 217, 308–314. [Google Scholar] [CrossRef]
- Yi, H.G.; Choi, Y.J.; Kang, K.S.; Hong, J.M.; Pati, R.G.; Park, M.N.; Shim, I.K.; Lee, C.M.; Kim, S.C.; Cho, D.W. A 3D-printed local drug delivery patch for pancreatic cancer growth suppression. J. Control. Release 2016, 238, 231–241. [Google Scholar] [CrossRef]
- Marcuello, C.; Chambel, L.; Rodrigues, M.S.; Ferreira, L.P.; Cruz, M.M. Magnetotactic Bacteria: Magnetism Beyond Magnetosomes. IEEE Trans. NanoBiosci. 2018, 17, 555–559. [Google Scholar] [CrossRef]
- Brero, F.; Albino, M.; Antoccia, A.; Arosio, P.; Avolio, M.; Berardinelli, F.; Bettega, D.; Calzolari, P.; Ciocca, M.; Corti, M.; et al. Hadron Therapy, Magnetic Nanoparticles and Hyperthermia: A Promising Combined Tool for Pancreatic Cancer Treatment. Nanomaterials 2020, 10, 1919. [Google Scholar] [CrossRef]
- Vogenberg, F.R.; Isaacson Barash, C.; Pursel, M. Personalized medicine: Part 1: Evolution and development into theranostics. Pharm. Ther. 2010, 35, 560–576. [Google Scholar]
- Ma, Q.; Lu, A.Y. Pharmacogenetics, pharmacogenomics, and individualized medicine. Pharm. Rev. 2011, 63, 437–459. [Google Scholar] [CrossRef] [Green Version]
- Basit, A. Recent innovations in 3D-printed personalized medicines: An interview with Abdul Basit. J. 3D Print. Med. 2020, 4, 5–7. [Google Scholar] [CrossRef]
- Schleidgen, S.; Marckmann, G. Re-focusing the ethical discourse on personalized medicine: A qualitative interview study with stakeholders in the German healthcare system. BMC Med. Ethics 2013, 14, 20. [Google Scholar] [CrossRef] [Green Version]
- Abul-Husn, N.S.; Owusu Obeng, A.; Sanderson, S.C.; Gottesman, O.; Scott, S.A. Implementation and utilization of genetic testing in personalized medicine. Pharmgenomics Pers. Med. 2014, 7, 227–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finkelman, B.S.; Gage, B.F.; Johnson, J.A.; Brensinger, C.M.; Kimmel, S.E. Genetic warfarin dosing: Tables versus algorithms. J. Am. Coll. Cardiol. 2011, 57, 612–618. [Google Scholar] [CrossRef] [Green Version]
- Mini, E.; Nobili, S. Pharmacogenetics: Implementing personalized medicine. Clin. Cases Min. Bone Metab. 2009, 6, 17–24. [Google Scholar]
- Diasio, R.B.; Beavers, T.L.; Carpenter, J.T. Familial deficiency of dihydropyrimidine dehydrogenase. Biochemical basis for familial pyrimidinemia and severe 5-fluorouracil-induced toxicity. J. Clin. Investig. 1988, 81, 47–51. [Google Scholar] [CrossRef] [Green Version]
- Luzzatto, L.; Seneca, E. G6PD deficiency: A classic example of pharmacogenetics with on-going clinical implications. Br. J. Haematol. 2014, 164, 469–480. [Google Scholar] [CrossRef]
- O’Dwyer, M.E.; Druker, B.J. Status of bcr-abl tyrosine kinase inhibitors in chronic myelogenous leukemia. Curr. Opin. Oncol. 2000, 12, 594–597. [Google Scholar] [CrossRef] [PubMed]
- Carlsten, C.; Brauer, M.; Brinkman, F.; Brook, J.; Daley, D.; McNagny, K.; Pui, M.; Royce, D.; Takaro, T.; Denburg, J. Genes, the environment and personalized medicine: We need to harness both environmental and genetic data to maximize personal and population health. EMBO Rep. 2014, 15, 736–739. [Google Scholar] [CrossRef]
- Patel, C.J.; Sivadas, A.; Tabassum, R.; Preeprem, T.; Zhao, J.; Arafat, D.; Chen, R.; Morgan, A.A.; Martin, G.S.; Brigham, K.L.; et al. Whole genome sequencing in support of wellness and health maintenance. Genome Med. 2013, 5, 58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goetz, L.H.; Schork, N.J. Personalized medicine: Motivation, challenges, and progress. Fertil. Steril. 2018, 109, 952–963. [Google Scholar] [CrossRef]
- Ruchi, C.; Varsha, R.; Mohini, M.; Krishan, K. Integrated Role of Nanotechnology and Pharmacogenetics in Diagnosis and Treatment of Diseases. In Pharmacogenetics; Islam, A.K., Ed.; IntechOpen: Rijeka, Croatia, 2021; p. Ch. 2. [Google Scholar]
- Hartmanshenn, C.; Scherholz, M.; Androulakis, I.P. Physiologically-based pharmacokinetic models: Approaches for enabling personalized medicine. J. Pharm. Pharm. 2016, 43, 481–504. [Google Scholar] [CrossRef] [Green Version]
- Mould, D.R.; Upton, R.N. Basic Concepts in Population Modeling, Simulation, and Model-Based Drug Development—Part 2: Introduction to Pharmacokinetic Modeling Methods. CPT Pharmacomet. Syst. Pharmacol. 2013, 2, 38. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, A.A.; Algahtani, M.S.; Ahmad, M.Z.; Ahmad, J.; Kotta, S. 3D printing in medicine: Technology overview and drug delivery applications. Ann. 3d Print. Med. 2021, 4, 100037. [Google Scholar] [CrossRef]
- United States Food and Drug Administration. OsteoFab Patient Specific Cranial Device. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf12/k121818.pdf (accessed on 15 January 2023).
- United States Food and Drug Administration. OsteoFab Patient Specific Facial Device. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K161052 (accessed on 15 January 2023).
- US-FDA. SPRITAM (Levetiracetam) Tablets. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2015/207958Orig1s000ltr.pdf (accessed on 15 January 2023).
- Triastek’s. Triastek Receives FDA IND Clearance for 3D Printed Drug to Treat Rheumatoid Arthritis. Available online: https://3dprintingindustry.com/news/triastek-receives-fda-ind-clearance-for-3d-printed-drug-to-treat-rheumatoid-arthritis-184159/ (accessed on 15 January 2023).
- Triastek’s. Triastek Receives FDA IND Clearance for 3D Printed Product of Blockbuster Molecule. Available online: https://www.prnewswire.com/news-releases/triastek-receives-fda-ind-clearance-for-3d-printed-product-of-blockbuster-molecule-301519962.html (accessed on 15 January 2023).
- UPR. Clinical Trials Authorised for 3D-Printed Ulcerative Colitis Drug. Available online: https://www.europeanpharmaceuticalreview.com/news/176673/clinical-trials-authorised-ulcerative-colitis-3d-printed-drug/ (accessed on 5 January 2023).
- Seoane-Viaño, I.; Ong, J.J.; Luzardo-Álvarez, A.; González-Barcia, M.; Basit, A.W.; Otero-Espinar, F.J.; Goyanes, A. 3D printed tacrolimus suppositories for the treatment of ulcerative colitis. Asian J. Pharm. Sci. 2021, 16, 110–119. [Google Scholar] [CrossRef]
- Li, H.; Go, G.; Ko, S.; Park, J.-O.; Park, S. Magnetic actuated pH-responsive hydrogel-based soft micro-robot for targeted drug delivery. Smart Mater. Struct. 2016, 25, 027001. [Google Scholar] [CrossRef]
- Öblom, H.; Cornett, C.; Bøtker, J.; Frokjaer, S.; Hansen, H.; Rades, T.; Rantanen, J.; Genina, N. Data-enriched edible pharmaceuticals (DEEP) of medical cannabis by inkjet printing. Int. J. Pharm. 2020, 589, 119866. [Google Scholar] [CrossRef]
- Kyobula, M.; Adedeji, A.; Alexander, M.R.; Saleh, E.; Wildman, R.; Ashcroft, I.; Gellert, P.R.; Roberts, C.J. 3D inkjet printing of tablets exploiting bespoke complex geometries for controlled and tuneable drug release. J. Control. Release 2017, 261, 207–215. [Google Scholar] [CrossRef]
- Ahn, J.-H.; Hong, H.-J.; Lee, C.-Y. Temperature-Sensing Inks Using Electrohydrodynamic Inkjet Printing Technology. Materials 2021, 14, 5623. [Google Scholar] [CrossRef]
- Sen, K.; Mukherjee, R.; Sansare, S.; Halder, A.; Kashi, H.; Ma, A.W.K.; Chaudhuri, B. Impact of powder-binder interactions on 3D printability of pharmaceutical tablets using drop test methodology. Eur. J. Pharm. Sci. 2021, 160, 105755. [Google Scholar] [CrossRef]
- Infanger, S.; Haemmerli, A.; Iliev, S.; Baier, A.; Stoyanov, E.; Quodbach, J. Powder bed 3D-printing of highly loaded drug delivery devices with hydroxypropyl cellulose as solid binder. Int. J. Pharm. 2019, 555, 198–206. [Google Scholar] [CrossRef]
- Shi, K.; Tan, D.K.; Nokhodchi, A.; Maniruzzaman, M. Drop-On-Powder 3D Printing of Tablets with an Anti-Cancer Drug, 5-Fluorouracil. Pharmaceutics 2019, 11, 150. [Google Scholar] [CrossRef] [Green Version]
- Jiang, B.; Jiao, H.; Guo, X.; Chen, G.; Guo, J.; Wu, W.; Jin, Y.; Cao, G.; Liang, Z. Lignin-Based Materials for Additive Manufacturing: Chemistry, Processing, Structures, Properties, and Applications. Adv. Sci. 2023, 10, e2206055. [Google Scholar] [CrossRef] [PubMed]
- Gerbin, E.; Frapart, Y.M.; Marcuello, C.; Cottyn, B.; Foulon, L.; Pernes, M.; Crônier, D.; Molinari, M.; Chabbert, B.; Ducrot, P.H.; et al. Dual Antioxidant Properties and Organic Radical Stabilization in Cellulose Nanocomposite Films Functionalized by In Situ Polymerization of Coniferyl Alcohol. Biomacromolecules 2020, 21, 3163–3175. [Google Scholar] [CrossRef]
- Saadi, M.; Maguire, A.; Pottackal, N.T.; Thakur, M.S.H.; Ikram, M.M.; Hart, A.J.; Ajayan, P.M.; Rahman, M.M. Direct Ink Writing: A 3D Printing Technology for Diverse Materials. Adv. Mater. 2022, 34, e2108855. [Google Scholar] [CrossRef] [PubMed]
- Goyanes, A.; Buanz, A.B.M.; Basit, A.W.; Gaisford, S. Fused-filament 3D printing (3DP) for fabrication of tablets. Int. J. Pharm. 2014, 476, 88–92. [Google Scholar] [CrossRef]
- Elbadawi, M.; Muñiz Castro, B.; Gavins, F.K.H.; Ong, J.J.; Gaisford, S.; Pérez, G.; Basit, A.W.; Cabalar, P.; Goyanes, A. M3DISEEN: A novel machine learning approach for predicting the 3D printability of medicines. Int. J. Pharm. 2020, 590, 119837. [Google Scholar] [CrossRef] [PubMed]
- Ghanizadeh Tabriz, A.; Nandi, U.; Hurt, A.P.; Hui, H.-W.; Karki, S.; Gong, Y.; Kumar, S.; Douroumis, D. 3D printed bilayer tablet with dual controlled drug release for tuberculosis treatment. Int. J. Pharm. 2021, 593, 120147. [Google Scholar] [CrossRef]
- Tagami, T.; Ito, E.; Kida, R.; Hirose, K.; Noda, T.; Ozeki, T. 3D printing of gummy drug formulations composed of gelatin and an HPMC-based hydrogel for pediatric use. Int. J. Pharm. 2021, 594, 120118. [Google Scholar] [CrossRef]
- Huang, J.; Qin, Q.; Wang, J. A Review of Stereolithography: Processes and Systems. Processes 2020, 8, 1138. [Google Scholar] [CrossRef]
- Melchels, F.P.W.; Feijen, J.; Grijpma, D.W. A review on stereolithography and its applications in biomedical engineering. Biomaterials 2010, 31, 6121–6130. [Google Scholar] [CrossRef] [Green Version]
- Hamed, R.; Mohamed, E.M.; Rahman, Z.; Khan, M.A. 3D-printing of lopinavir printlets by selective laser sintering and quantification of crystalline fraction by XRPD-chemometric models. Int. J. Pharm. 2021, 592, 120059. [Google Scholar] [CrossRef]
- Charoo, N.A.; Barakh Ali, S.F.; Mohamed, E.M.; Kuttolamadom, M.A.; Ozkan, T.; Khan, M.A.; Rahman, Z. Selective laser sintering 3D printing—An overview of the technology and pharmaceutical applications. Drug Dev. Ind. Pharm. 2020, 46, 869–877. [Google Scholar] [CrossRef]
- Pereira, G.G.; Figueiredo, S.; Fernandes, A.I.; Pinto, J.F. Polymer Selection for Hot-Melt Extrusion Coupled to Fused Deposition Modelling in Pharmaceutics. Pharmaceutics 2020, 12, 795. [Google Scholar] [CrossRef]
- Kafle, A.; Luis, E.; Silwal, R.; Pan, H.M.; Shrestha, P.L.; Bastola, A.K. 3D/4D Printing of Polymers: Fused Deposition Modelling (FDM), Selective Laser Sintering (SLS), and Stereolithography (SLA). Polymers 2021, 13, 3101. [Google Scholar] [CrossRef]
- Algahtani, M.S.; Mohammed, A.A.; Ahmad, J. Extrusion-Based 3D Printing for Pharmaceuticals: Contemporary Research and Applications. Curr. Pharm. Des. 2018, 24, 4991–5008. [Google Scholar] [CrossRef] [PubMed]
- Seoane-Viaño, I.; Januskaite, P.; Alvarez-Lorenzo, C.; Basit, A.W.; Goyanes, A. Semi-solid extrusion 3D printing in drug delivery and biomedicine: Personalised solutions for healthcare challenges. J. Control. Release 2021, 332, 367–389. [Google Scholar] [CrossRef] [PubMed]
- Blynskaya, E.V.; Tishkov, S.V.; Alekseev, K.V.; Vetcher, A.A.; Marakhova, A.I.; Rejepov, D.T. Polymers in Technologies of Additive and Inkjet Printing of Dosage Formulations. Polymers 2022, 14, 2543. [Google Scholar] [CrossRef] [PubMed]
- Goole, J.; Amighi, K. 3D printing in pharmaceutics: A new tool for designing customized drug delivery systems. Int. J. Pharm. 2016, 499, 376–394. [Google Scholar] [CrossRef]
- Lakkala, P.; Munnangi, S.R.; Bandari, S.; Repka, M. Additive manufacturing technologies with emphasis on stereolithography 3D printing in pharmaceutical and medical applications: A review. Int. J. Pharm. X 2023, 5, 100159. [Google Scholar] [CrossRef]
- Gueche, Y.A.; Sanchez-Ballester, N.M.; Cailleaux, S.; Bataille, B.; Soulairol, I. Selective Laser Sintering (SLS), a New Chapter in the Production of Solid Oral Forms (SOFs) by 3D Printing. Pharmaceutics 2021, 13, 1212. [Google Scholar] [CrossRef]
- Gutiérrez, E.; Barreto, J.d.J.; Garcia-Hernandez, S.; Morales, R.; González-Solorzano, M.G. Decrease of Nozzle Clogging through Fluid Flow Control. Metals 2020, 10, 1420. [Google Scholar] [CrossRef]
- Oktavianty, O.; Haruyama, S.; Ishii, Y. Enhancing Droplet Quality of Edible Ink in Single and Multi-Drop Methods by Optimization the Waveform Design of DoD Inkjet Printer. Processes 2022, 10, 91. [Google Scholar] [CrossRef]
- Clark, E.A.; Alexander, M.R.; Irvine, D.J.; Roberts, C.J.; Wallace, M.J.; Sharpe, S.; Yoo, J.; Hague, R.J.M.; Tuck, C.J.; Wildman, R.D. 3D printing of tablets using inkjet with UV photoinitiation. Int. J. Pharm. 2017, 529, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Thabet, Y.; Lunter, D.; Breitkreutz, J. Continuous inkjet printing of enalapril maleate onto orodispersible film formulations. Int. J. Pharm. 2018, 546, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Vakili, H.; Nyman, J.O.; Genina, N.; Preis, M.; Sandler, N. Application of a colorimetric technique in quality control for printed pediatric orodispersible drug delivery systems containing propranolol hydrochloride. Int. J. Pharm. 2016, 511, 606–618. [Google Scholar] [CrossRef] [PubMed]
- Pere, C.P.P.; Economidou, S.N.; Lall, G.; Ziraud, C.; Boateng, J.S.; Alexander, B.D.; Lamprou, D.A.; Douroumis, D. 3D printed microneedles for insulin skin delivery. Int. J. Pharm. 2018, 544, 425–432. [Google Scholar] [CrossRef] [Green Version]
- Içten, E.; Purohit, H.S.; Wallace, C.; Giridhar, A.; Taylor, L.S.; Nagy, Z.K.; Reklaitis, G.V. Dropwise additive manufacturing of pharmaceutical products for amorphous and self emulsifying drug delivery systems. Int. J. Pharm. 2017, 524, 424–432. [Google Scholar] [CrossRef] [Green Version]
- López-Iglesias, C.; Casielles, A.M.; Altay, A.; Bettini, R.; Alvarez-Lorenzo, C.; García-González, C.A. From the printer to the lungs: Inkjet-printed aerogel particles for pulmonary delivery. Chem. Eng. J. 2019, 357, 559–566. [Google Scholar] [CrossRef]
- Wickström, H.; Hilgert, E.; Nyman, J.O.; Desai, D.; Şen Karaman, D.; de Beer, T.; Sandler, N.; Rosenholm, J.M. Inkjet Printing of Drug-Loaded Mesoporous Silica Nanoparticles-A Platform for Drug Development. Molecules 2017, 22, 2020. [Google Scholar] [CrossRef] [Green Version]
- Katstra, W.E.; Palazzolo, R.D.; Rowe, C.W.; Giritlioglu, B.; Teung, P.; Cima, M.J. Oral dosage forms fabricated by three dimensional printing. J. Control. Release 2000, 66, 1–9. [Google Scholar] [CrossRef]
- Yu, D.G.; Branford-White, C.; Ma, Z.H.; Zhu, L.M.; Li, X.Y.; Yang, X.L. Novel drug delivery devices for providing linear release profiles fabricated by 3DP. Int. J. Pharm. 2009, 370, 160–166. [Google Scholar] [CrossRef]
- Lee, W.L.; Yu, P.O.; Hong, M.; Widjaja, E.; Loo, S.C. Designing multilayered particulate systems for tunable drug release profiles. Acta Biomater. 2012, 8, 2271–2278. [Google Scholar] [CrossRef]
- Wilts, E.M.; Ma, D.; Bai, Y.; Williams, C.B.; Long, T.E. Comparison of Linear and 4-Arm Star Poly(vinyl pyrrolidone) for Aqueous Binder Jetting Additive Manufacturing of Personalized Dosage Tablets. ACS Appl. Mater. Interfaces 2019, 11, 23938–23947. [Google Scholar] [CrossRef]
- Yu, D.-G.; Branford-White, C.; Yang, Y.-C.; Zhu, L.-M.; Welbeck, E.W.; Yang, X.-L. A novel fast disintegrating tablet fabricated by three-dimensional printing. Drug Dev. Ind. Pharm. 2009, 35, 1530–1536. [Google Scholar] [CrossRef] [PubMed]
- Rowe, C.W.; Katstra, W.E.; Palazzolo, R.D.; Giritlioglu, B.; Teung, P.; Cima, M.J. Multimechanism oral dosage forms fabricated by three dimensional printing™. J. Control. Release 2000, 66, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Pereira, B.C.; Isreb, A.; Forbes, R.T.; Dores, F.; Habashy, R.; Petit, J.B.; Alhnan, M.A.; Oga, E.F. ‘Temporary Plasticiser’: A novel solution to fabricate 3D printed patient-centred cardiovascular ‘Polypill’ architectures. Eur. J. Pharm. Biopharm. 2019, 135, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Sadia, M.; Sośnicka, A.; Arafat, B.; Isreb, A.; Ahmed, W.; Kelarakis, A.; Alhnan, M.A. Adaptation of pharmaceutical excipients to FDM 3D printing for the fabrication of patient-tailored immediate release tablets. Int. J. Pharm. 2016, 513, 659–668. [Google Scholar] [CrossRef] [PubMed]
- Ilyés, K.; Balogh, A.; Casian, T.; Igricz, T.; Borbás, E.; Démuth, B.; Vass, P.; Menyhárt, L.; Kovács, N.K.; Marosi, G.; et al. 3D floating tablets: Appropriate 3D design from the perspective of different in vitro dissolution testing methodologies. Int. J. Pharm. 2019, 567, 118433. [Google Scholar] [CrossRef] [PubMed]
- Alhijjaj, M.; Belton, P.; Qi, S. An investigation into the use of polymer blends to improve the printability of and regulate drug release from pharmaceutical solid dispersions prepared via fused deposition modeling (FDM) 3D printing. Eur. J. Pharm. Biopharm. 2016, 108, 111–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gioumouxouzis, C.I.; Baklavaridis, A.; Katsamenis, O.L.; Markopoulou, C.K.; Bouropoulos, N.; Tzetzis, D.; Fatouros, D.G. A 3D printed bilayer oral solid dosage form combining metformin for prolonged and glimepiride for immediate drug delivery. Eur. J. Pharm. Sci. 2018, 120, 40–52. [Google Scholar] [CrossRef] [Green Version]
- Li, Q.; Wen, H.; Jia, D.; Guan, X.; Pan, H.; Yang, Y.; Yu, S.; Zhu, Z.; Xiang, R.; Pan, W. Preparation and investigation of controlled-release glipizide novel oral device with three-dimensional printing. Int. J. Pharm. 2017, 525, 5–11. [Google Scholar] [CrossRef]
- Kollamaram, G.; Croker, D.M.; Walker, G.M.; Goyanes, A.; Basit, A.W.; Gaisford, S. Low temperature fused deposition modeling (FDM) 3D printing of thermolabile drugs. Int. J. Pharm. 2018, 545, 144–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kukkonen, J.; Ervasti, T.; Laitinen, R. Production and characterization of glibenclamide incorporated PLA filaments for 3D printing by fused deposition modeling. J. Drug Deliv. Sci. Technol. 2022, 77, 103843. [Google Scholar] [CrossRef]
- Mohammed, A.A.; Algahtani, M.S.; Ahmad, M.Z.; Ahmad, J. Optimization of semisolid extrusion (pressure-assisted microsyringe)-based 3D printing process for advanced drug delivery application. Ann. 3d Print. Med. 2021, 2, 100008. [Google Scholar] [CrossRef]
- Khaled, S.A.; Burley, J.C.; Alexander, M.R.; Yang, J.; Roberts, C.J. 3D printing of tablets containing multiple drugs with defined release profiles. Int. J. Pharm. 2015, 494, 643–650. [Google Scholar] [CrossRef]
- Algahtani, M.S.; Mohammed, A.A.; Ahmad, J.; Saleh, E. Development of a 3D Printed Coating Shell to Control the Drug Release of Encapsulated Immediate-Release Tablets. Polymers 2020, 12, 1395. [Google Scholar] [CrossRef]
- Ahmed, T.A.; Alotaibi, H.A.; Alharbi, W.S.; Safo, M.K.; El-Say, K.M. Development of 3D-Printed, Liquisolid and Directly Compressed Glimepiride Tablets, Loaded with Black Seed Oil Self-Nanoemulsifying Drug Delivery System: In Vitro and In Vivo Characterization. Polymers 2022, 15, 68. [Google Scholar] [CrossRef]
- Ahmed, T.A.; Felimban, R.I.; Tayeb, H.H.; Rizg, W.Y.; Alnadwi, F.H.; Alotaibi, H.A.; Alhakamy, N.A.; Abd-Allah, F.I.; Mohamed, G.A.; Zidan, A.S.; et al. Development of Multi-Compartment 3D-Printed Tablets Loaded with Self-Nanoemulsified Formulations of Various Drugs: A New Strategy for Personalized Medicine. Pharmaceutics 2021, 13, 1733. [Google Scholar] [CrossRef]
- Algahtani, M.S.; Mohammed, A.A.; Ahmad, J.; Abdullah, M.M.; Saleh, E. 3D Printing of Dapagliflozin Containing Self-Nanoemulsifying Tablets: Formulation Design and In Vitro Characterization. Pharmaceutics 2021, 13, 993. [Google Scholar] [CrossRef]
- Xu, X.; Robles-Martinez, P.; Madla, C.M.; Joubert, F.; Goyanes, A.; Basit, A.W.; Gaisford, S. Stereolithography (SLA) 3D printing of an antihypertensive polyprintlet: Case study of an unexpected photopolymer-drug reaction. Addit. Manuf. 2020, 33, 101071. [Google Scholar] [CrossRef]
- Wang, J.; Goyanes, A.; Gaisford, S.; Basit, A.W. Stereolithographic (SLA) 3D printing of oral modified-release dosage forms. Int. J. Pharm. 2016, 503, 207–212. [Google Scholar] [CrossRef]
- Xu, X.; Seijo-Rabina, A.; Awad, A.; Rial, C.; Gaisford, S.; Basit, A.W.; Goyanes, A. Smartphone-enabled 3D printing of medicines. Int. J. Pharm. 2021, 609, 121199. [Google Scholar] [CrossRef] [PubMed]
- Burke, G.; Devine, D.M.; Major, I. Effect of Stereolithography 3D Printing on the Properties of PEGDMA Hydrogels. Polymers 2020, 12, 2015. [Google Scholar] [CrossRef] [PubMed]
- Karakurt, I.; Aydoğdu, A.; Çıkrıkcı, S.; Orozco, J.; Lin, L. Stereolithography (SLA) 3D printing of ascorbic acid loaded hydrogels: A controlled release study. Int. J. Pharm. 2020, 584, 119428. [Google Scholar] [CrossRef] [PubMed]
- Uddin, M.J.; Scoutaris, N.; Economidou, S.N.; Giraud, C.; Chowdhry, B.Z.; Donnelly, R.F.; Douroumis, D. 3D printed microneedles for anticancer therapy of skin tumours. Mater. Sci. Eng. C 2020, 107, 110248. [Google Scholar] [CrossRef]
- Triacca, A.; Pitzanti, G.; Mathew, E.; Conti, B.; Dorati, R.; Lamprou, D.A. Stereolithography 3D printed implants: A preliminary investigation as potential local drug delivery systems to the ear. Int. J. Pharm. 2022, 616, 121529. [Google Scholar] [CrossRef]
- Goyanes, A.; Det-Amornrat, U.; Wang, J.; Basit, A.W.; Gaisford, S. 3D scanning and 3D printing as innovative technologies for fabricating personalized topical drug delivery systems. J. Control. Release 2016, 234, 41–48. [Google Scholar] [CrossRef]
- Leong, K.F.; Chua, C.K.; Gui, W.S.; Verani. Building Porous Biopolymeric Microstructures for Controlled Drug Delivery Devices Using Selective Laser Sintering. Int. J. Adv. Manuf. Technol. 2006, 31, 483–489. [Google Scholar] [CrossRef]
- Davis, D.A., Jr.; Thakkar, R.; Su, Y.; Williams, R.O., 3rd; Maniruzzaman, M. Selective Laser Sintering 3-Dimensional Printing as a Single Step Process to Prepare Amorphous Solid Dispersion Dosage Forms for Improved Solubility and Dissolution Rate. J. Pharm. Sci. 2021, 110, 1432–1443. [Google Scholar] [CrossRef]
- Allahham, N.; Fina, F.; Marcuta, C.; Kraschew, L.; Mohr, W.; Gaisford, S.; Basit, A.W.; Goyanes, A. Selective Laser Sintering 3D Printing of Orally Disintegrating Printlets Containing Ondansetron. Pharmaceutics 2020, 12, 110. [Google Scholar] [CrossRef] [Green Version]
- Awad, A.; Fina, F.; Trenfield, S.J.; Patel, P.; Goyanes, A.; Gaisford, S.; Basit, A.W. 3D Printed Pellets (Miniprintlets): A Novel, Multi-Drug, Controlled Release Platform Technology. Pharmaceutics 2019, 11, 148. [Google Scholar] [CrossRef] [Green Version]
- Trenfield, S.J.; Tan, H.X.; Goyanes, A.; Wilsdon, D.; Rowland, M.; Gaisford, S.; Basit, A.W. Non-destructive dose verification of two drugs within 3D printed polyprintlets. Int. J. Pharm. 2020, 577, 119066. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.; Barnes, M.; McMillin, R.; Cook, D.W.; Smith, S.; Halquist, M.; Wijesinghe, D.; Roper, T.D. 3D Printing of Metformin HCl PVA Tablets by Fused Deposition Modeling: Drug Loading, Tablet Design, and Dissolution Studies. AAPS PharmSciTech 2019, 20, 195. [Google Scholar] [CrossRef] [PubMed]
- Sadia, M.; Isreb, A.; Abbadi, I.; Isreb, M.; Aziz, D.; Selo, A.; Timmins, P.; Alhnan, M.A. From ‘fixed dose combinations’ to ‘a dynamic dose combiner’: 3D printed bi-layer antihypertensive tablets. Eur. J. Pharm. Sci. 2018, 123, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Clark, E.A.; Alexander, M.R.; Irvine, D.J.; Roberts, C.J.; Wallace, M.J.; Yoo, J.; Wildman, R.D. Making tablets for delivery of poorly soluble drugs using photoinitiated 3D inkjet printing. Int. J. Pharm. 2020, 578, 118805. [Google Scholar] [CrossRef]
- Acosta-Vélez, G.F.; Linsley, C.S.; Zhu, T.Z.; Wu, W.; Wu, B.M. Photocurable Bioinks for the 3D Pharming of Combination Therapies. Polymers 2018, 10, 1372. [Google Scholar] [CrossRef] [Green Version]

| Approval Status | Company | Product Name | Drug Delivery System/Device | Technique | Ref. |
|---|---|---|---|---|---|
| US FDA approved in market | Aprecia 3DP Pharmaceuticals Company | Spritam | Zip dose fast disintegrating tablet containing Levetiracetam, antiepileptic drug | Powder-based Binder Jet 3D Printing Technique | [47] |
| US FDA approved | Oxford Performance Materials Inc. | Osteofab | Patient-specific facial device | SLS | [46] |
| US FDA approved | Oxford Performance Materials Inc. | Osteofab | Patient-specific implants | SLS | [45] |
| Investigational New Drug (IND) approval by US FDA | Triastek Inc. | T19 | Chrono therapeutic drug delivery system to treat patients with rheumatoid arthritis | MED | [48] |
| IND approval by US FDA | Triastek Inc. | T20 | Once-a-day treatment for cardiovascular and clotting disorder | MED | [49] |
| IND approval by US FDA | Triastek Inc. | T21 | Site-specific delivery of drugs for the treatment of ulcerative colitis | MED | [50] |
| Drug | Disease | Dosage Forms and Its Critical Attributes | Outcome | Ref. |
|---|---|---|---|---|
| Captopril, Nifidipine, glipizide. | Diabetic and hypertensive patient | Three drugs containing tablet (multipill) with defined drug release profiles for a complex dosage regimen | The designed multipill exhibited an osmotic and diffusion control sustained release of the drug for a period of 14 h. | [102] |
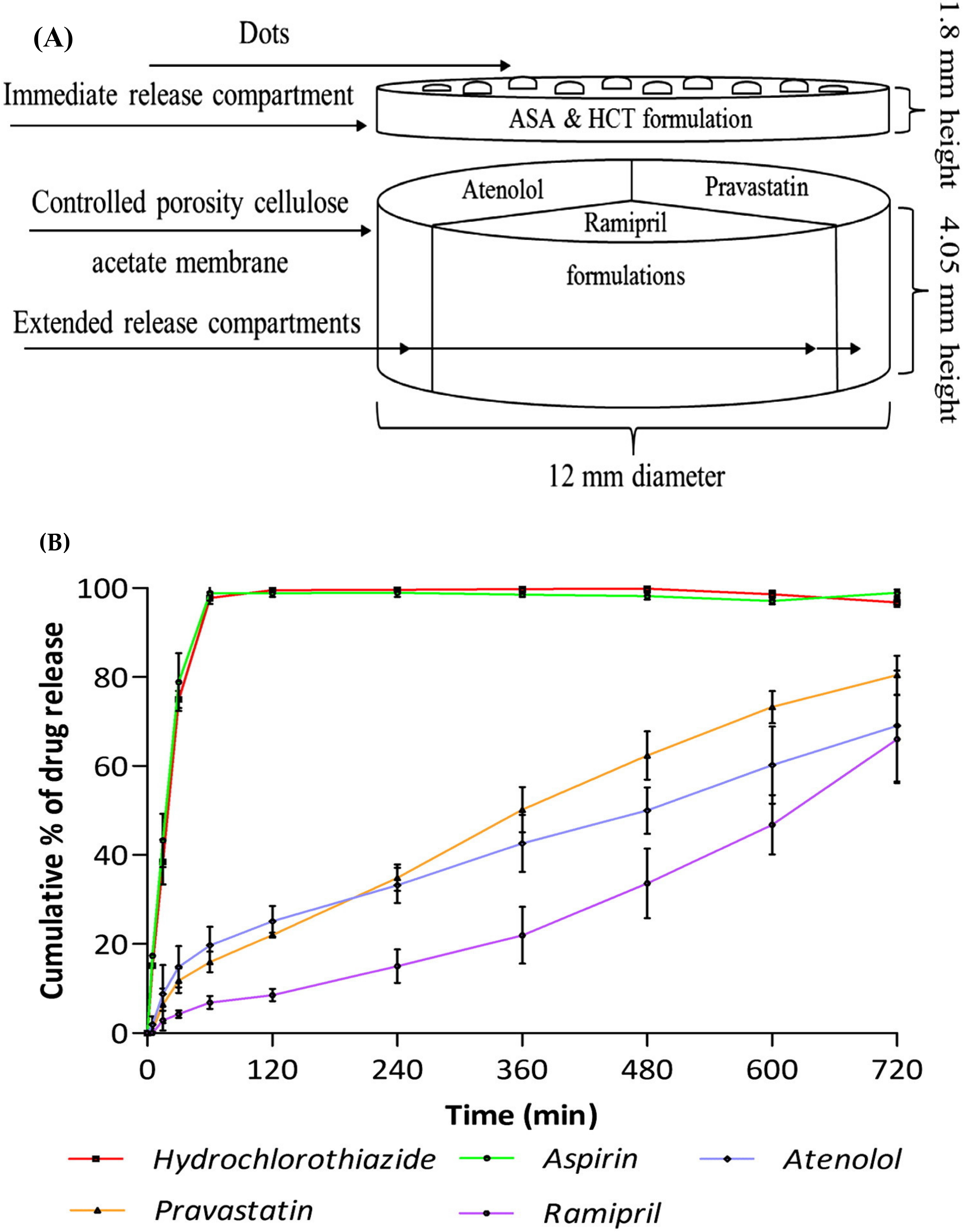
| Aspirin, hydrochloro thiazide, pravastatin, atenolol, and ramipril | Cardiovascular disease and high blood pressure | Five drugs in a tablet (polypill) with tailored drug combinations and release characteristic for complex dosage regimen | The designed polypill showed an immediate drug release of 75% within 30 min by aspirin and hydrochlorothiazide drug compartment, whereas a sustained release of 69%, 81%, and 66% for a period of 720 min was achieved by pravastatin, atenolol, and ramipril compartment, respectively. | [24] |
| Dafagliflozin | Diabetes | SNEDDS tablet with customized dosing and tuned drug release profile for poorly soluble drug. | The SNEDDS tablet exhibited an enhanced solubility and drug release of dapagliflozin and attributed to customized dosing. | [106] |
| Glimepiride and rosuvastatin | Hyperlipidemic patients with diabetes | Multicompartment 3D printed SNEDDS tablet for combined drug therapy | The multicompartment 3D printed SNEDDS tablets showed superior drug release characteristics in compare to liquisolid and directly compressible tablets. The relative bioavailability was found to be 159.50% and 245.16% for glimepiride and rosuvastatin, respectively. | [105] |
| Drugs | Disease | Dosage Form and Its Critical Attributes | 3D Technique | Outcome | Ref. |
|---|---|---|---|---|---|
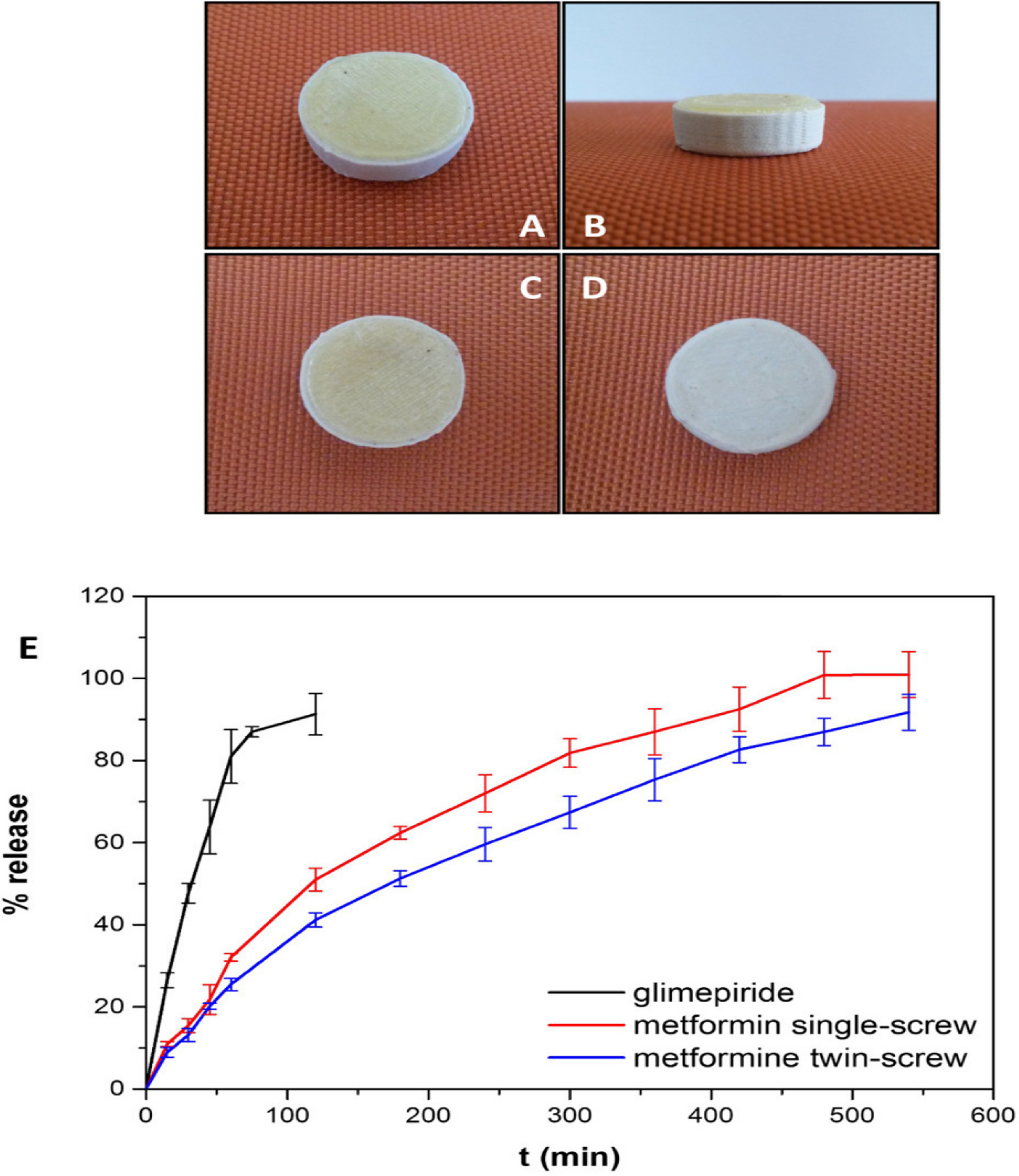
| Metformin and glimiperide | Diabetes | Tailored made bilayered tablet for combined pharmacotherapy | FDM | The 3D printed bilayered tablet showed an immediate release of glimepiride and a sustained release of the metformin. | [97] |
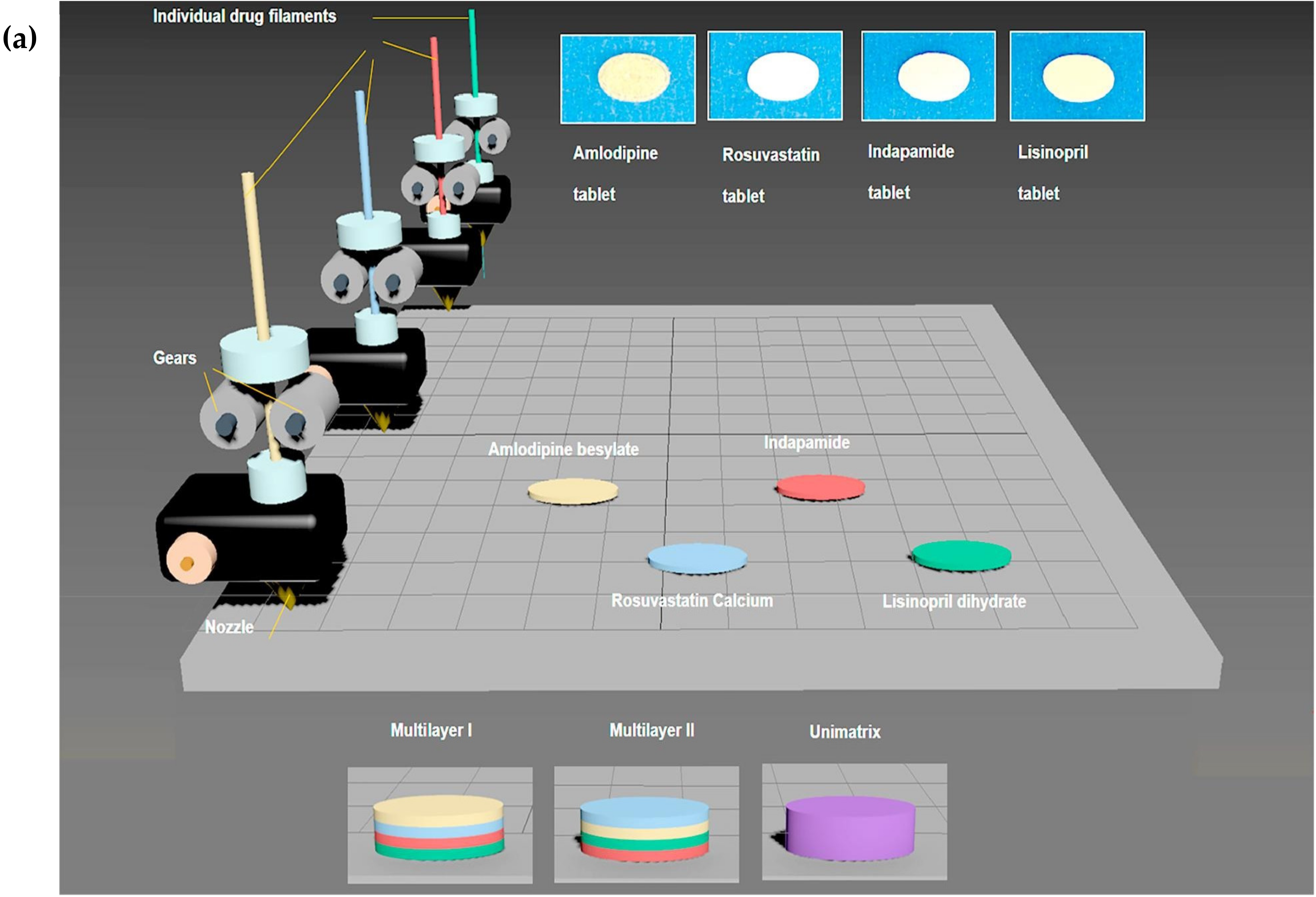
| Lisinopril, indapamide, amlodipine and rosuvastatin | Cardiovascular disease | Multilayered polypill for patient-centred therapy with orchestrating release profiles | FDM | The drug release from the multilayered tablet for each drug depends on the position of the drug layer in the tablet. The multilayered tablet exhibited biphasic drug release showing faster drug release for the outer layers and initial slow drug release for the inner layers, which become rapid after a lag time of 15 min. | [93] |
| Glipizide | Diabetes | Specialized designed duo tablet with variable drug concentration distribution for tuned drug release | FDM | The duo tablet exhibited controlled and delayed release behavior of glipizide due to the customized dose in each tablet. From the external tablet, 90% drug release was achieved in the first two hours and from the internal tablet, the drug release commenced after a lag time of 85 min. | [98] |
| Enalapril maleate and hydrochlorothiazide | Hypertension | Bi-layered tablet in a customized flexible dose combination | FDM | The bi-layered tablet designed with six different dose combinations indicated a similar drug release pattern for three sets of a bi-layered tablets. Thus this approach provides evidence that dynamic dose dispensing can be achieved for fixed-dose combinations according to the patient’s needs. | [121] |
| Amlodipine and lisinopril | Hypertension | Multidrug-loaded poly printlets with customized dosing characterisation | SLS | Provides a novel non-destructive dose quantification method for multiple drugs in a 3D-printed polypill. | [119] |
| Insulin | Diabetes | Microneedle patches for personalized transdermal delivery of insulin | SLA | The drug release from the designed microneedles was rapid within 30 min. The selected carrier preserves the integrity, stability of insulin, as well as provides a rapid release of insulin from cone, and pyramid shaped microneedles. | [83] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqahtani, A.A.; Ahmed, M.M.; Mohammed, A.A.; Ahmad, J. 3D Printed Pharmaceutical Systems for Personalized Treatment in Metabolic Syndrome. Pharmaceutics 2023, 15, 1152. https://doi.org/10.3390/pharmaceutics15041152
Alqahtani AA, Ahmed MM, Mohammed AA, Ahmad J. 3D Printed Pharmaceutical Systems for Personalized Treatment in Metabolic Syndrome. Pharmaceutics. 2023; 15(4):1152. https://doi.org/10.3390/pharmaceutics15041152
Chicago/Turabian StyleAlqahtani, Abdulsalam A., Mohammed Muqtader Ahmed, Abdul Aleem Mohammed, and Javed Ahmad. 2023. "3D Printed Pharmaceutical Systems for Personalized Treatment in Metabolic Syndrome" Pharmaceutics 15, no. 4: 1152. https://doi.org/10.3390/pharmaceutics15041152
APA StyleAlqahtani, A. A., Ahmed, M. M., Mohammed, A. A., & Ahmad, J. (2023). 3D Printed Pharmaceutical Systems for Personalized Treatment in Metabolic Syndrome. Pharmaceutics, 15(4), 1152. https://doi.org/10.3390/pharmaceutics15041152








