Liposome-Micelle-Hybrid (LMH) Carriers for Controlled Co-Delivery of 5-FU and Paclitaxel as Chemotherapeutics
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of PTX-Encapsulated Micelles
2.3. Preparation of PTX-Encapsulated Thermosensitive Liposomes
2.4. Preparation of PTX-Encapsulated Thermosensitive Liposome-Micelle Hybrid (LMHPTX)
2.5. Preparation of PTX-5-FU-Loaded LMHPTX-5-FU
2.6. Encapsulation Efficiency and Drug Loading
2.7. PTX Assay Method
2.8. 5-FU Assay Method
2.9. Characterization of Liposome-Micelle-Hybrid (LMH) Nanocarriers
2.9.1. Particle Diameter and Size Distribution
2.9.2. Differential Scanning Calorimetry
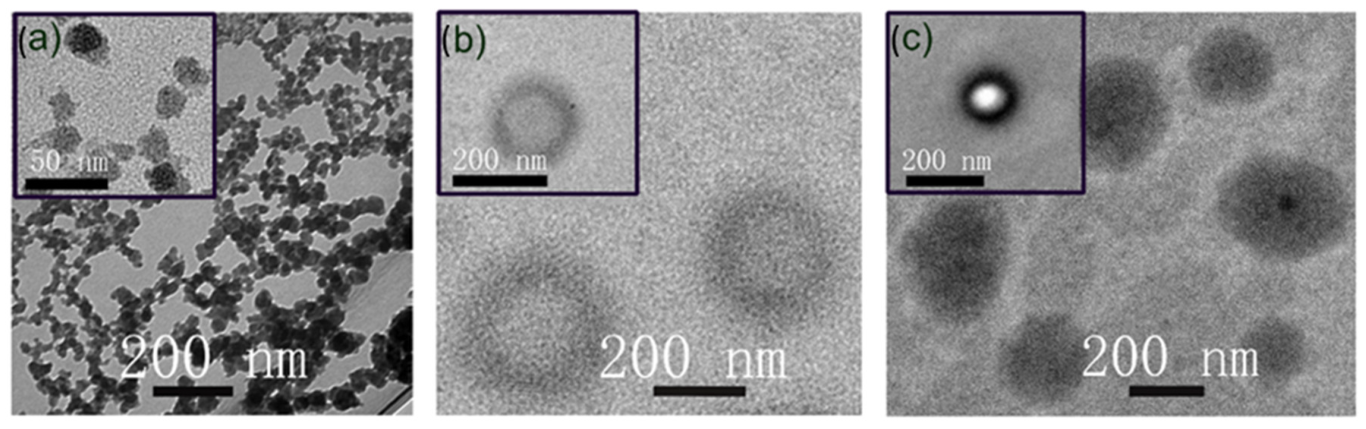
2.9.3. Morphological Characterization of Nanocarriers
2.10. Temperature-Triggered Release of PTX and 5-FU from Nanocarriers
2.11. In Vitro Drug Release Kinetics
2.12. Permeability Assessment
- a.
- The apparent PTX permeability (Papp × 10−6 µg/s) was calculated as follows:
- b.
- The efflux ratio (ER) was calculated as the ratio of Papp determined in the A-to-B direction to Papp determined in the B-to-A direction:where the ratio of the basolateral-apical (secretion) component Papp B–A to the apical-basolateral (absorption) component Papp A–B was assessed. Theoretically, an ER superior to unity implies the action of one or various efflux transporters on the tested compound.ER = (Papp B–A)/(Papp A–B)
2.13. Cell Viability Studies
2.14. Statistics Analysis Method
3. Results and Discussion
3.1. Preparation and Characterization of Liposome, Micelle, and LMH Formulations
3.2. Drug Loading Behaviour
3.3. Temperature-Dependent Drug Release from Micelles, Liposomes, and LMH
3.4. Analysis of Release Kinetics
3.5. Permeability Behavior of LMH Nanocarriers
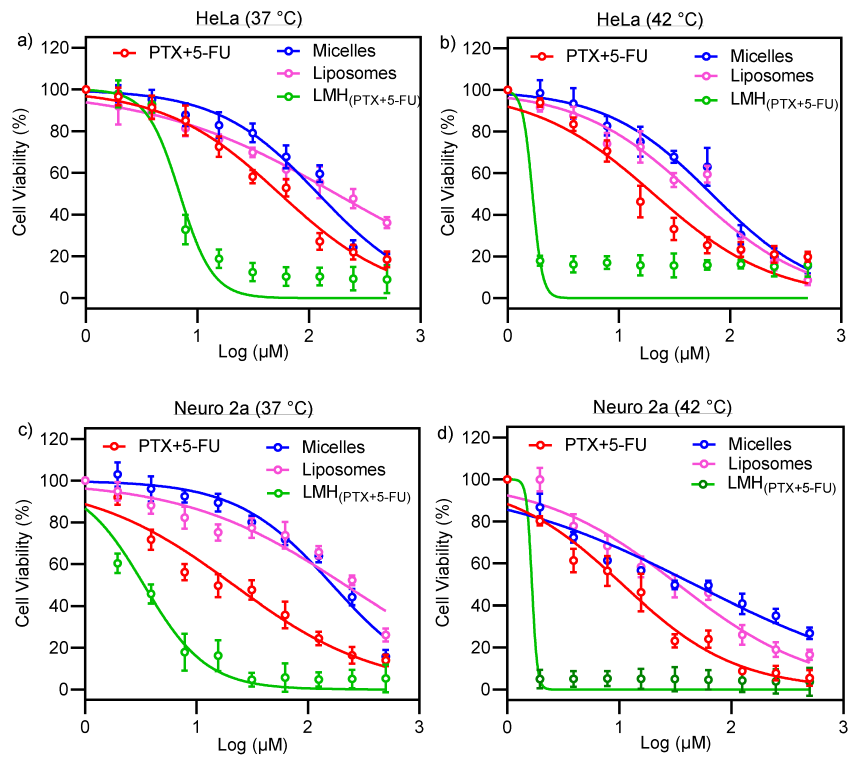
3.6. In Vitro Cell Viability Studies
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sparreboom, A.; Van Asperen, J.; Mayer, U.; Schinkel, A.H.; Smit, J.W.; Meijer, D.K.F.; Borst, P.; Nooijen, W.J.; Beijnen, J.H.; Van Tellingen, O. Limited oral bioavailability and active epithelial excretion of paclitaxel (Taxol) caused by P-glycoprotein in the intestine. Proc. Natl. Acad. Sci. USA 1997, 94, 2031–2035. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Zu, C.; Li, W.; Wu, W.; Ge, Y.; Wang, L.; Wang, L.; Li, Y.; Zhao, X. Enhanced Water Solubility and Oral Bioavailability of Paclitaxel Crystal Powders through an Innovative Antisolvent Precipitation Process: Antisolvent Crystallization Using Ionic Liquids as Solvent. Pharmaceutics 2020, 12, 1008. [Google Scholar] [CrossRef] [PubMed]
- Qu, X.; Zou, Y.; He, C.; Zhou, Y.; Jin, Y.; Deng, Y.; Wang, Z.; Li, X.; Zhou, Y.; Liu, Y. Improved intestinal absorption of paclitaxel by mixed micelles self-assembled from vitamin E succinate-based amphiphilic polymers and their transcellular transport mechanism and intracellular trafficking routes. Drug Deliv. 2018, 25, 210–225. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.-S.; Jo, B.-W.; Kim, Y.-C. Enhanced paclitaxel bioavailability after oral administration of paclitaxel or prodrug to rats pretreated with quercetin. Eur. J. Pharm. Biopharm. 2004, 57, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Panday, V.R.; Huizing, M.T.; Willemse, P.H.; De Graeff, A.; Huinink, W.W.T.B.; Vermorken, J.B.; Beijnen, J.H. Hepatic metabolism of paclitaxel and its impact in patients with altered hepatic function. Semin. Oncol. 1997, 24 (Suppl. S11), S11-34–S11-38. [Google Scholar]
- Singla, A.K.; Garg, A.; Aggarwal, D. Paclitaxel and its formulations. Int. J. Pharm. 2002, 235, 179–192. [Google Scholar] [CrossRef]
- Singh, S.; Dash, A.K. Paclitaxel in cancer treatment: Perspectives and prospects of its delivery challenges. Crit. Rev. Ther. Drug Carr. Syst. 2009, 26, 333–372. [Google Scholar] [CrossRef]
- Guo, W.; Dong, W.; Li, M.; Shen, Y. Mitochondria P-glycoprotein confers paclitaxel resistance on ovarian cancer cells. Onco Targets Ther. 2019, 12, 3881–3891. [Google Scholar] [CrossRef]
- Hida, K.; Kikuchi, H.; Maishi, N.; Hida, Y. ATP-binding cassette transporters in tumor endothelial cells and resistance to metronomic chemotherapy. Cancer Lett. 2017, 400, 305–310. [Google Scholar] [CrossRef]
- Gottesman, M.M.; Fojo, T.; Bates, S.E. Multidrug resistance in cancer: Role of ATP–dependent transporters. Nat. Rev. Cancer 2002, 2, 48–58. [Google Scholar] [CrossRef]
- Wu, Q.; Yang, Z.; Nie, Y.; Shi, Y.; Fan, D. Multi-drug resistance in cancer chemotherapeutics: Mechanisms and lab approaches. Cancer Lett. 2014, 347, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Bukowski, K.; Kciuk, M.; Kontek, R. Mechanisms of multidrug resistance in cancer chemotherapy. Int. J. Mol. Sci. 2020, 21, 3233. [Google Scholar] [CrossRef] [PubMed]
- Halder, J.; Pradhan, D.; Kar, B.; Ghosh, G.; Rath, G. Nanotherapeutics approaches to overcome P-glycoprotein-mediated multi-drug resistance in cancer. Nanomed. Nanotechnol. Biol. Med. 2021, 40, 102494. [Google Scholar] [CrossRef] [PubMed]
- Keil, F.; Selzer, E.; Berghold, A.; Reinisch, S.; Kapp, K.S.; De Vries, A.; Greil, R.; Bachtiary, B.; Tinchon, C.; Anderhuber, W.; et al. Induction chemotherapy with docetaxel, cisplatin and 5-fluorouracil followed by radiotherapy with cetuximab for locally advanced squamous cell carcinoma of the head and neck. Eur. J. Cancer 2013, 49, 352–359. [Google Scholar] [CrossRef]
- Wang, D.; Tang, J.; Wang, Y.; Ramishetti, S.; Fu, Q.; Racette, K.; Liu, F. Multifunctional nanoparticles based on a single-molecule modification for the treatment of drug-resistant cancer. Mol. Pharm. 2013, 10, 1465–1469. [Google Scholar] [CrossRef]
- Giacchetti, S.; Perpoint, B.; Zidani, R.; Le Bail, N.; Faggiuolo, R.; Focan, C.; Chollet, P.; Llory, J.; Letourneau, Y.; Coudert, B. Phase III multicenter randomized trial of oxaliplatin added to chronomodulated fluorouracil–leucovorin as first-line treatment of metastatic colorectal cancer. J. Clin. Oncol. 2000, 18, 136. [Google Scholar] [CrossRef]
- Jeong, S.H.; Chavani, O.; Burns, K.; Porter, D.; Findlay, M.; Helsby, N. Severe 5-Fluorouracil-Associated Gastrointestinal Toxicity Unexplained by Dihydropyrimidine Dehydrogenase Deficiency and Renal Impairment: Should We Be Investigating Other Elimination Pathways to Assess the Risk of 5-Fluorouracil Toxicity? Eur. J. Drug Metab. Pharmacokinet. 2021, 46, 817–820. [Google Scholar] [CrossRef]
- More, L.A.; Lane, S.; Asnani, A. 5-FU cardiotoxicity: Vasospasm, myocarditis, and sudden death. Curr. Cardiol. Rep. 2021, 23, 17. [Google Scholar] [CrossRef]
- Gupte, A.; Ciftci, K. Formulation and characterization of Paclitaxel, 5-FU and Paclitaxel + 5-FU microspheres. Int. J. Pharm. 2004, 276, 93–106. [Google Scholar] [CrossRef]
- Chandran, S.P.; Natarajan, S.B.; Chandraseharan, S.; Shahimi, M.S.B.M. Nano drug delivery strategy of 5-fluorouracil for the treatment of colorectal cancer. J. Cancer Res. Pract. 2017, 4, 45–48. [Google Scholar] [CrossRef]
- Jain, K.K. Role of nanobiotechnology in drug delivery. In Drug Delivery Systems; Springer: Humana, New York, USA, 2020; pp. 55–73. [Google Scholar]
- Wang, W.; Joyce, P.; Bremmell, K.; Milne, R.; Prestidge, C.A. Liposomal 5-Fluorouracil Polymer Complexes Facilitate Tumor-Specific Delivery: Pharmaco-Distribution Kinetics Using Microdialysis. Pharmaceutics 2022, 14, 221. [Google Scholar] [CrossRef]
- Saraf, S.; Jain, A.; Tiwari, A.; Verma, A.; Panda, P.K.; Jain, S.K. Advances in liposomal drug delivery to cancer: An overview. J. Drug Deliv. Sci. Technol. 2020, 56, 101549. [Google Scholar] [CrossRef]
- Filipczak, N.; Pan, J.; Yalamarty, S.S.K.; Torchilin, V.P. Recent advancements in liposome technology. Adv. Drug Deliv. Rev. 2020, 156, 4–22. [Google Scholar] [CrossRef]
- Barenholz, Y.C. Doxil®—The first FDA-approved nano-drug: From an idea to a product. In Handbook of Harnessing Biomaterials in Nanomedicine; Peer, D., Ed.; Jenny Stanford Publishing: New York, USA, 2021; pp. 463–528. [Google Scholar]
- Koudelka, Š.; Turánek, J. Liposomal paclitaxel formulations. J. Control. Release 2012, 163, 322–334. [Google Scholar] [CrossRef] [PubMed]
- Pereira Gomes, I.; Aparecida Duarte, J.; Chaves Maia, A.L.; Rubello, D.; Townsend, D.M.; Branco de Barros, A.L.; Leite, E.A. Thermosensitive Nanosystems Associated with Hyperthermia for Cancer Treatment. Pharmaceuticals 2019, 12, 171. [Google Scholar] [CrossRef] [PubMed]
- Needham, D.; Anyarambhatla, G.; Kong, G.; Dewhirst, M.W. A New Temperature-sensitive Liposome for Use with Mild Hyperthermia: Characterization and Testing in a Human Tumor Xenograft Model1. Cancer Res. 2000, 60, 1197–1201. [Google Scholar] [PubMed]
- Riganti, C.; Voena, C.; Kopecka, J.; Corsetto, P.A.; Montorfano, G.; Enrico, E.; Costamagna, C.; Rizzo, A.M.; Ghigo, D.; Bosia, A. Liposome-encapsulated doxorubicin reverses drug resistance by inhibiting P-glycoprotein in human cancer cells. Mol. Pharm. 2011, 8, 683–700. [Google Scholar] [CrossRef]
- Mohan, A.; Narayanan, S.; Sethuraman, S.; Krishnan, U.M. Novel resveratrol and 5-fluorouracil coencapsulated in PEGylated nanoliposomes improve chemotherapeutic efficacy of combination against head and neck squamous cell carcinoma. BioMed Res. Int. 2014, 2014, 424239. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Luo, J.; Tan, S.; Otieno, B.O.; Zhang, Z. The applications of Vitamin E TPGS in drug delivery. Eur. J. Pharm. Sci. 2013, 49, 175–186. [Google Scholar] [CrossRef]
- Sezgin, Z.; Yüksel, N.; Baykara, T. Preparation and characterization of polymeric micelles for solubilization of poorly soluble anticancer drugs. Eur. J. Pharm. Biopharm. 2006, 64, 261–268. [Google Scholar] [CrossRef]
- Nimtrakul, P.; Williams, D.B.; Tiyaboonchai, W.; Prestidge, C.A. Copolymeric Micelles Overcome the Oral Delivery Challenges of Amphotericin B. Pharmaceuticals 2020, 13, 121. [Google Scholar] [CrossRef] [PubMed]
- Mandal, A.; Gote, V.; Pal, D.; Ogundele, A.; Mitra, A.K. Ocular Pharmacokinetics of a Topical Ophthalmic Nanomicellar Solution of Cyclosporine (Cequa®) for Dry Eye Disease. Pharm. Res. 2019, 36, 36. [Google Scholar] [CrossRef] [PubMed]
- Allen, T.; Hansen, C. Pharmacokinetics of stealth versus conventional liposomes: Effect of dose. Biochim. Biophys. Acta-Biomembr. 1991, 1068, 133–141. [Google Scholar] [CrossRef]
- Lo, Y.-L. Phospholipids as multidrug resistance modulators of the transport of epirubicin in human intestinal epithelial Caco-2 cell layers and everted gut sacs of rats. Biochem. Pharmacol. 2000, 60, 1381–1390. [Google Scholar] [CrossRef] [PubMed]
- Dintaman, J.M.; Silverman, J.A. Inhibition of P-Glycoprotein by D-α-Tocopheryl Polyethylene Glycol 1000 Succinate (TPGS). Pharm. Res. 1999, 16, 1550–1556. [Google Scholar] [CrossRef]
- Owen, S.C.; Chan, D.P.Y.; Shoichet, M.S. Polymeric micelle stability. Nano Today 2012, 7, 53–65. [Google Scholar] [CrossRef]
- Romana, B.; Hassan, M.M.; Sonvico, F.; Garrastazu Pereira, G.; Mason, A.F.; Thordarson, P.; Bremmell, K.E.; Barnes, T.J.; Prestidge, C.A. A liposome-micelle-hybrid (LMH) oral delivery system for poorly water-soluble drugs: Enhancing solubilisation and intestinal transport. Eur. J. Pharm. Biopharm. 2020, 154, 338–347. [Google Scholar] [CrossRef]
- Li, Y.; Chen, Z.; Cui, Y.; Zhai, G.; Li, L. The construction and characterization of hybrid paclitaxel-in-micelle-in-liposome systems for enhanced oral drug delivery. Colloids Surf. B Biointerfaces 2017, 160, 572–580. [Google Scholar] [CrossRef]
- Ruysschaert, T.; Germain, M.; da Silva Gomes, J.P.; Fournier, D.; Sukhorukov, G.B.; Meier, W.; Winterhalter, M. Liposome-based nanocapsules. IEEE Trans. NanoBiosci. 2004, 3, 49–55. [Google Scholar] [CrossRef]
- Gong, J.; Chen, M.; Zheng, Y.; Wang, S.; Wang, Y. Polymeric micelles drug delivery system in oncology. J. Control. Release 2012, 159, 312–323. [Google Scholar] [CrossRef]
- Dou, Y.; Hynynen, K.; Allen, C. To heat or not to heat: Challenges with clinical translation of thermosensitive liposomes. J. Control. Release 2017, 249, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Bangham, A.; Standish, M.; Watkins, J. Diffusion of univalent ions across the lamellae of swollen phospholipids. J. Mol. Biol. 1965, 13, 238. [Google Scholar] [CrossRef] [PubMed]
- Korsmeyer, R.W.; Gurny, R.; Doelker, E.; Buri, P.; Peppas, N.A. Mechanisms of solute release from porous hydrophilic polymers. Int. J. Pharm. 1983, 15, 25–35. [Google Scholar] [CrossRef]
- Liang, E.; Chessic, K.; Yazdanian, M. Evaluation of an accelerated Caco-2 cell permeability model. J. Pharm. Sci. 2000, 89, 336–345. [Google Scholar] [CrossRef]
- Zidan, A.S.; Spinks, C.B.; Habib, M.J.; Khan, M.A. Formulation and transport properties of tenofovir loaded liposomes through Caco-2 cell model. J. Liposome Res. 2013, 23, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Hope, M.J.; Nayar, R.; Mayer, L.D.; Cullis, P. Reduction of liposome size and preparation of unilamellar vesicles by extrusion techniques. In Liposome Technology: Interactions of Liposomes with the Biological Milieu; Gregoriadis, G., Ed.; CRC Press, Inc.: Boca Raton, FL, USA, 1993; pp. 123–139. [Google Scholar]
- Selvamani, V. Stability studies on nanomaterials used in drugs. In Characterization and Biology of Nanomaterials for Drug Delivery; Simon, H., Ed.; Matthew Dean Press: London, UK, 2019; pp. 425–444. [Google Scholar]
- Freitas, C.; Müller, R.H. Effect of light and temperature on zeta potential and physical stability in solid lipid nanoparticle (SLN™) dispersions. Int. J. Pharm. 1998, 168, 221–229. [Google Scholar] [CrossRef]
- Yang, T.; Cui, F.-D.; Choi, M.-K.; Cho, J.-W.; Chung, S.-J.; Shim, C.-K.; Kim, D.-D. Enhanced solubility and stability of PEGylated liposomal paclitaxel: In vitro and in vivo evaluation. Int. J. Pharm. 2007, 338, 317–326. [Google Scholar] [CrossRef]
- Bulbake, U.; Doppalapudi, S.; Kommineni, N.; Khan, W. Liposomal Formulations in Clinical Use: An Updated Review. Pharmaceutics 2017, 9, 12. [Google Scholar] [CrossRef]
- Gaber, M.H.; Hong, K.; Huang, S.K.; Papahadjopoulos, D. Thermosensitive Sterically Stabilized Liposomes: Formulation and in Vitro Studies on Mechanism of Doxorubicin Release by Bovine Serum and Human Plasma. Pharm. Res. 1995, 12, 1407–1416. [Google Scholar] [CrossRef]
- Genz, A.; Holzwarth, J.; Tsong, T. The influence of cholesterol on the main phase transition of unilamellar dipalmytoylphosphatidylcholine vesicles. A differential scanning calorimetry and iodine laser T-jump study. Biophys. J. 1986, 50, 1043–1051. [Google Scholar] [CrossRef]
- Demetzos, C. Differential Scanning Calorimetry (DSC): A Tool to Study the Thermal Behavior of Lipid Bilayers and Liposomal Stability. J. Liposome Res. 2008, 18, 159–173. [Google Scholar] [CrossRef]
- Hanpft, R.; Mohr, K. Influence of cationic amphiphilic drugs on the phase-transition temperature of phospholipids with different polar headgroups. Biochim. Biophys. Acta (BBA)-Biomembr. 1985, 814, 156–162. [Google Scholar] [CrossRef]
- Ji, X.; Gao, Y.; Chen, L.; Zhang, Z.; Deng, Y.; Li, Y. Nanohybrid systems of non-ionic surfactant inserting liposomes loading paclitaxel for reversal of multidrug resistance. Int. J. Pharm. 2012, 422, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Costa, P.; Lobo, J.M.S. Modeling and comparison of dissolution profiles. Eur. J. Pharm. Sci. 2001, 13, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.H. Studies in diffusion. II. A kinetic theory of diffusion in liquid systems. J. Am. Chem. Soc. 1930, 52, 3937–3955. [Google Scholar] [CrossRef]
- Hossain, Z.; Kurihara, H.; Hosokawa, M.; Takahashi, K. Docosahexaenoic acid and eicosapentaenoic acid-enriched phosphatidylcholine liposomes enhance the permeability, transportation and uptake of phospholipids in Caco-2 cells. Mol. Cell. Biochem. 2006, 285, 155–163. [Google Scholar] [CrossRef]
- Mathot, F.; van Beijsterveldt, L.; Préat, V.; Brewster, M.; Ariën, A. Intestinal uptake and biodistribution of novel polymeric micelles after oral administration. J. Control. Release 2006, 111, 47–55. [Google Scholar] [CrossRef]
- Cheng, H.C.; Chang, C.Y.; Hsieh, F.I.; Yeh, J.J.; Chien, M.Y.; Pan, R.N.; Deng, M.C.; Liu, D.Z. Effects of tremella-alginate-liposome encapsulation on oral delivery of inactivated H5N3 vaccine. J. Microencapsul. 2011, 28, 55–61. [Google Scholar] [CrossRef]
- Liu, B.-Y.; Wu, C.; He, X.-Y.; Zhuo, R.-X.; Cheng, S.-X. Multi-drug loaded vitamin E-TPGS nanoparticles for synergistic drug delivery to overcome drug resistance in tumor treatment. Sci. Bull. 2016, 61, 552–560. [Google Scholar] [CrossRef]
- Cui, M.; Wu, W.; Hovgaard, L.; Lu, Y.; Chen, D.; Qi, J. Liposomes containing cholesterol analogues of botanical origin as drug delivery systems to enhance the oral absorption of insulin. Int. J. Pharm. 2015, 489, 277–284. [Google Scholar] [CrossRef]





| Nanocarrier Type | Mean Diameter (nm) | PDI | Zeta Potential (mV) | |
|---|---|---|---|---|
| Micelle | Blank | 13 ± 0.4 | 0.242 ± 0.027 | |
| 5-FU-Loaded | 12 ± 0.3 | 0.059 ± 0.005 | ||
| PTX-Loaded | 10 ± 0.1 | 0.039 ± 0.007 | ||
| Liposomes | Blank | 154 ± 2.3 | 0.121 ± 0.015 | −32.8 ± 0.4 |
| PTX-Loaded | 167 ± 4.5 | 0.276 ± 0.024 | −31.1 ± 0.1 | |
| LMH | Blank | 151 ± 2.6 | 0.087 ± 0.021 | −34.1 ± 0.2 |
| LMHPTX | 157 ± 2.5 | 0.256 ± 0.029 | −29.6 ± 0.7 | |
| LMHPTX-5-FU | 164 ± 1.9 | 0.171 ± 0.028 | −32.9 ± 0.6 | |
| LMHPTX-PTX | 175 ± 1.7 | 0.217 ± 0.0208 | −30.0 ± 0.7 | |
| Nanocarrier Type (Loaded Phase) | Drug Loading (mg/mL) | Aqueous Solubility Improvement (Fold Increase) | |
|---|---|---|---|
| PTX | 5-FU | PTX * | |
| Micelle (core) | 2.20 ± 0.14 | 3.16 ± 0.36 | 73.4 |
| Liposome (bilayer) | 4.72 ± 0.40 | - | 157.3 |
| LMHPTX (core) | 1.42 ± 0.03 | - | 47.3 |
| LMHPTX-5-FU (PTX bilayer and 5-FU core) | 3.12 ± 0.53 | 2.91 ± 0.41 | 103.3 |
| LMHPTX-PTX (bilayer and micelles in the core) | 6.04 ± 0.13 | - | 208.6 |
| Nanocarrier Type | 37 °C | 42 °C | ||||
|---|---|---|---|---|---|---|
| K | n | D (m2/s) ×10−10 | K | n | D (m2/s) ×10−10 | |
| LMHPTX-5-FU | 0.187 | 0.408 | 0.138 | 0.447 | 0.357 | 0.215 |
| LMHPTX | 0.290 | 0.433 | 0.699 | 0.900 | 0.361 | 1.301 |
| Liposome | 6.117 | 0.204 | 2.491 | 8.501 | 0.195 | 2.850 |
| Micelle | 5.957 | 0.205 | 1.532 | 7.447 | 0.214 | 2.532 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hassan, M.M.; Romana, B.; Mao, G.; Kumar, N.; Sonvico, F.; Thordarson, P.; Joyce, P.; Bremmell, K.E.; Barnes, T.J.; Prestidge, C.A. Liposome-Micelle-Hybrid (LMH) Carriers for Controlled Co-Delivery of 5-FU and Paclitaxel as Chemotherapeutics. Pharmaceutics 2023, 15, 1886. https://doi.org/10.3390/pharmaceutics15071886
Hassan MM, Romana B, Mao G, Kumar N, Sonvico F, Thordarson P, Joyce P, Bremmell KE, Barnes TJ, Prestidge CA. Liposome-Micelle-Hybrid (LMH) Carriers for Controlled Co-Delivery of 5-FU and Paclitaxel as Chemotherapeutics. Pharmaceutics. 2023; 15(7):1886. https://doi.org/10.3390/pharmaceutics15071886
Chicago/Turabian StyleHassan, Md. Musfizur, Bilquis Romana, Guangzhao Mao, Naresh Kumar, Fabio Sonvico, Pall Thordarson, Paul Joyce, Kristen E. Bremmell, Timothy J. Barnes, and Clive A. Prestidge. 2023. "Liposome-Micelle-Hybrid (LMH) Carriers for Controlled Co-Delivery of 5-FU and Paclitaxel as Chemotherapeutics" Pharmaceutics 15, no. 7: 1886. https://doi.org/10.3390/pharmaceutics15071886
APA StyleHassan, M. M., Romana, B., Mao, G., Kumar, N., Sonvico, F., Thordarson, P., Joyce, P., Bremmell, K. E., Barnes, T. J., & Prestidge, C. A. (2023). Liposome-Micelle-Hybrid (LMH) Carriers for Controlled Co-Delivery of 5-FU and Paclitaxel as Chemotherapeutics. Pharmaceutics, 15(7), 1886. https://doi.org/10.3390/pharmaceutics15071886










