Synergistic Enhancement of Carboplatin Efficacy through pH-Sensitive Nanoparticles Formulated Using Naturally Derived Boswellia Extract for Colorectal Cancer Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Extraction and Chemical Characterization of the Major Chemical Components of Boswellia Sacra Resin
2.3. Preparation of Cp@CS/BME NPs
2.4. Size, Polydispersity Index (PDI), and Zeta Potential Analysis
2.5. Transmission Electron Microscopy
2.6. Entrapment Efficiency (EE)
2.7. In Vitro Drug Release Studies
2.8. Release Kinetics
2.9. Cell Culture
2.10. Cell Viability
2.11. Apoptosis Assay
2.12. Cellular Uptake of Cp
2.13. Cell-Cycle Analysis
2.14. Gene Expression Analysis
2.15. Statistical Analysis
3. Results and Discussion
3.1. LC/ESI-MS-MS Analysis of the Boswellia Methanol Extract
3.2. Average Diameters, PDI, Zeta Potential, Morphology, and Entrapment Efficiency (EE%)
3.3. Cp Release from BME NPs In Vitro
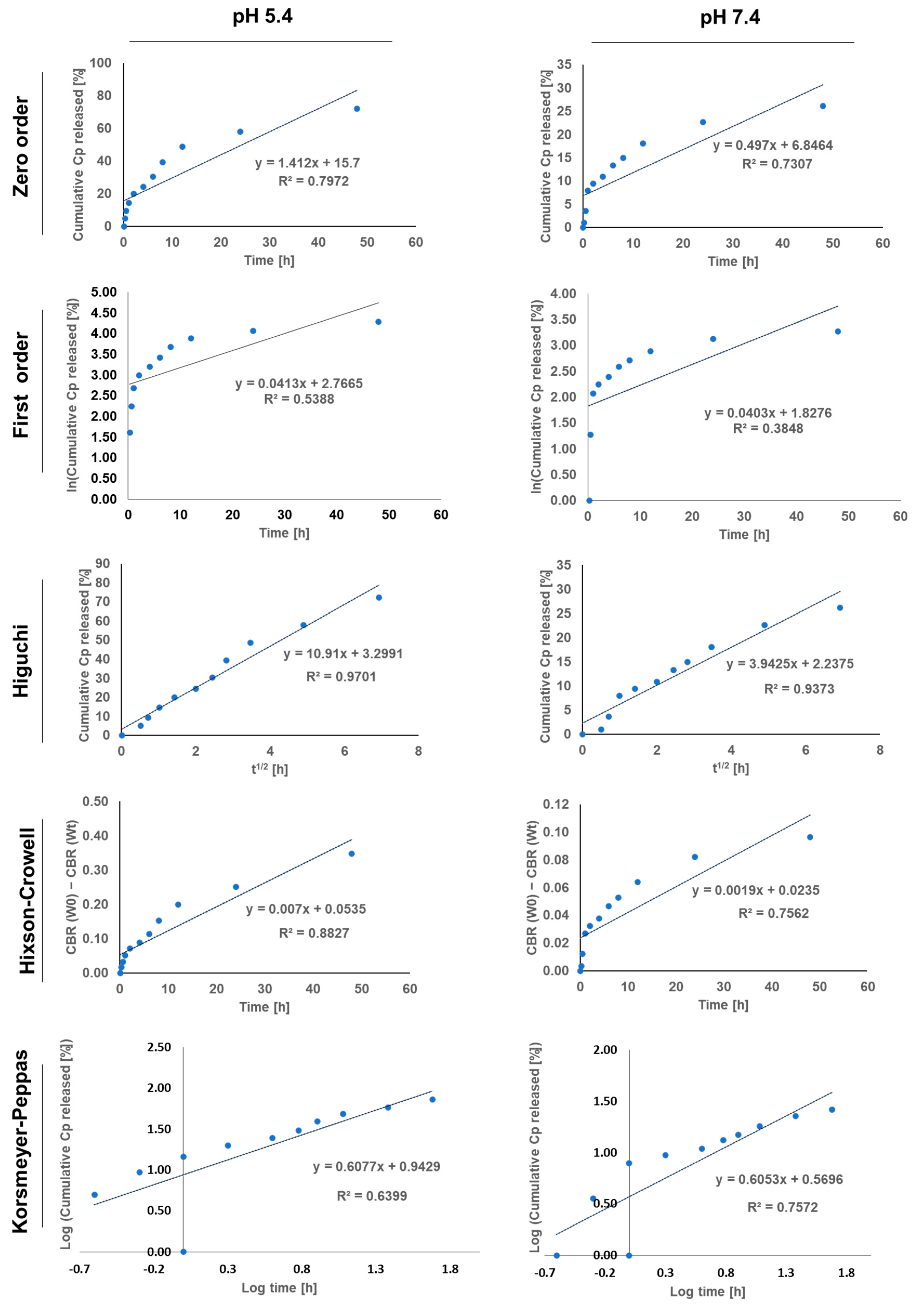
3.4. Release Kinetics of Cp from BME NPs
3.5. Cellular Uptake Assay
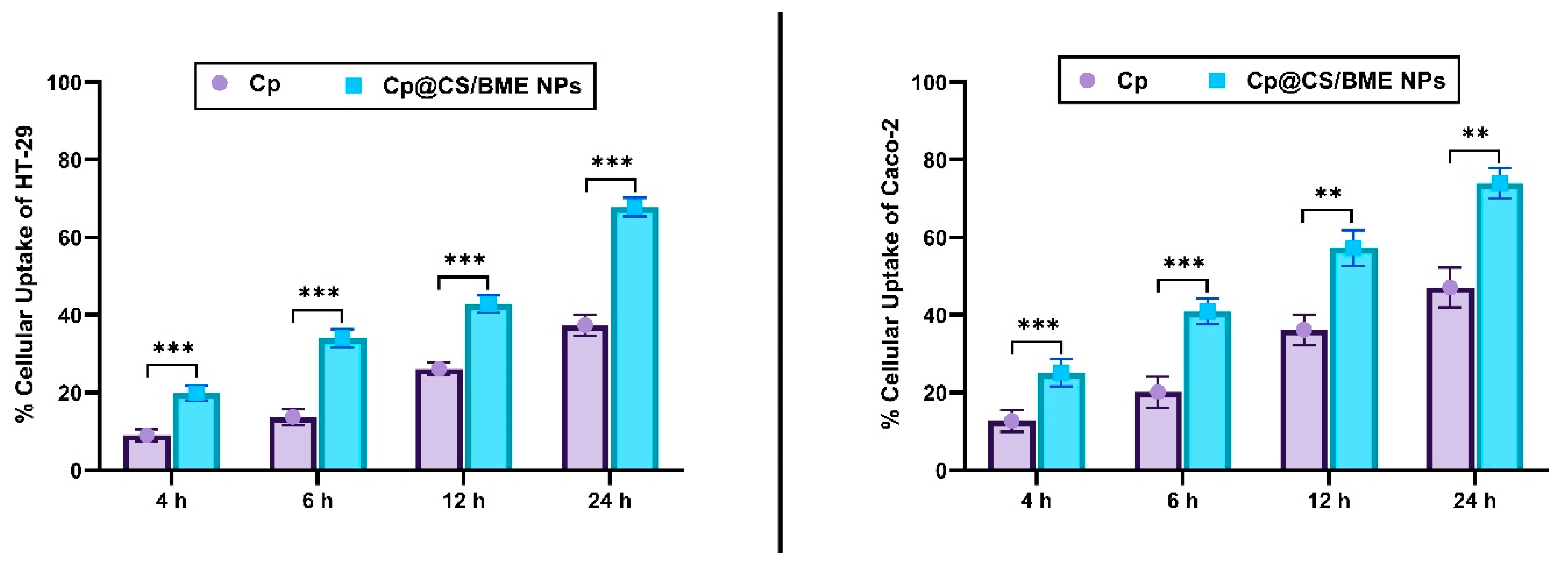
3.6. Cell Viability
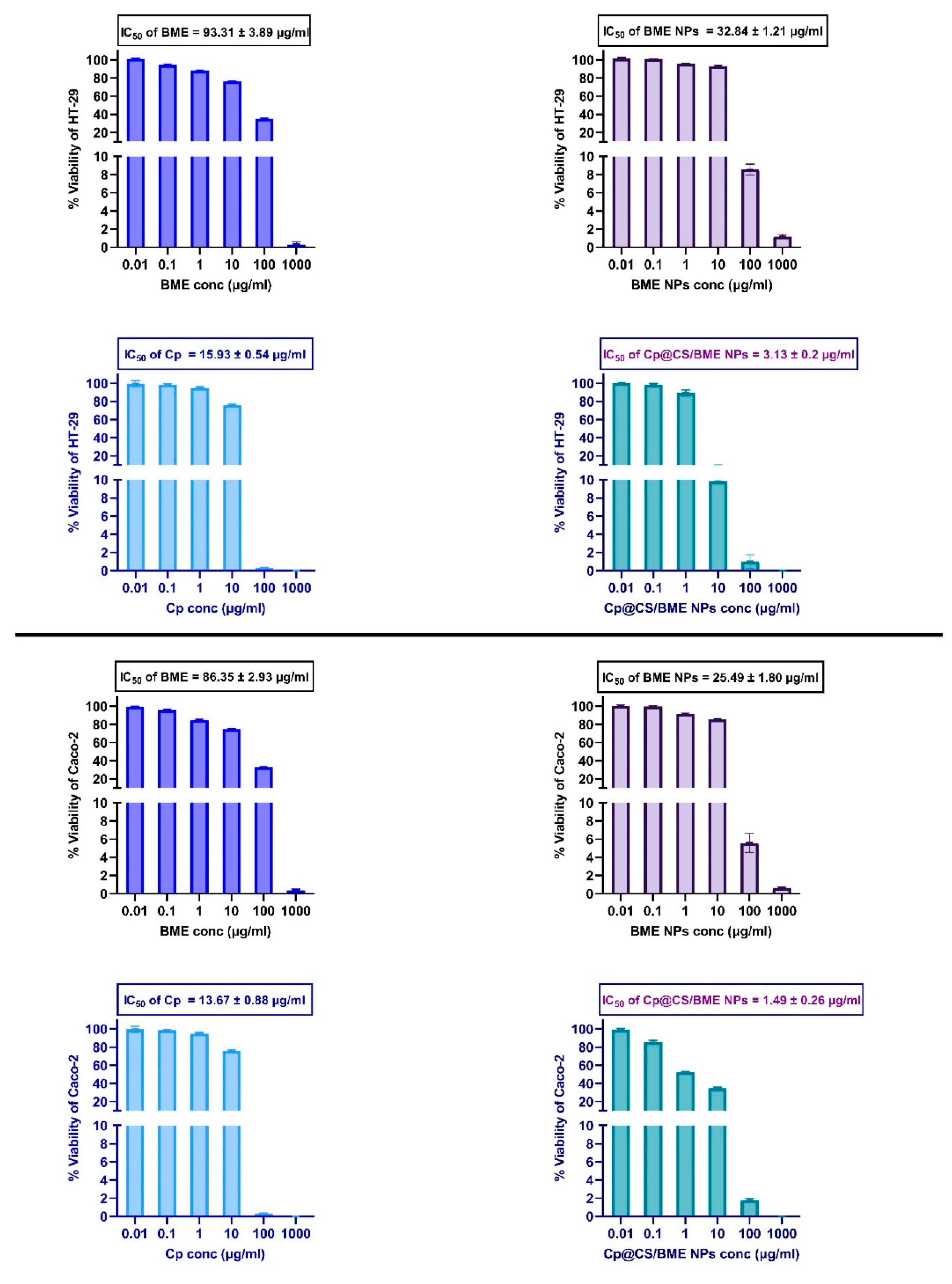
3.7. Apoptosis Assay
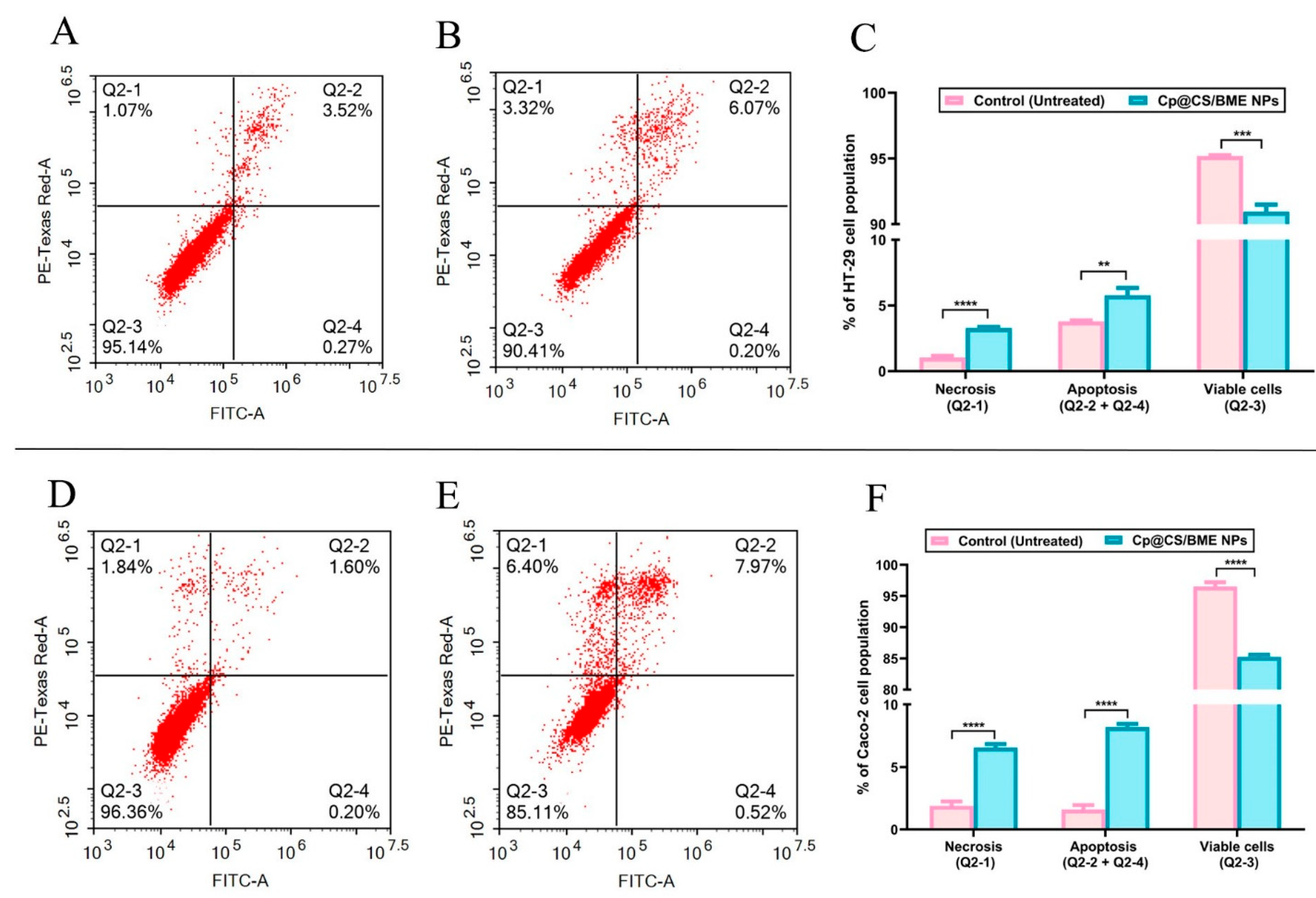
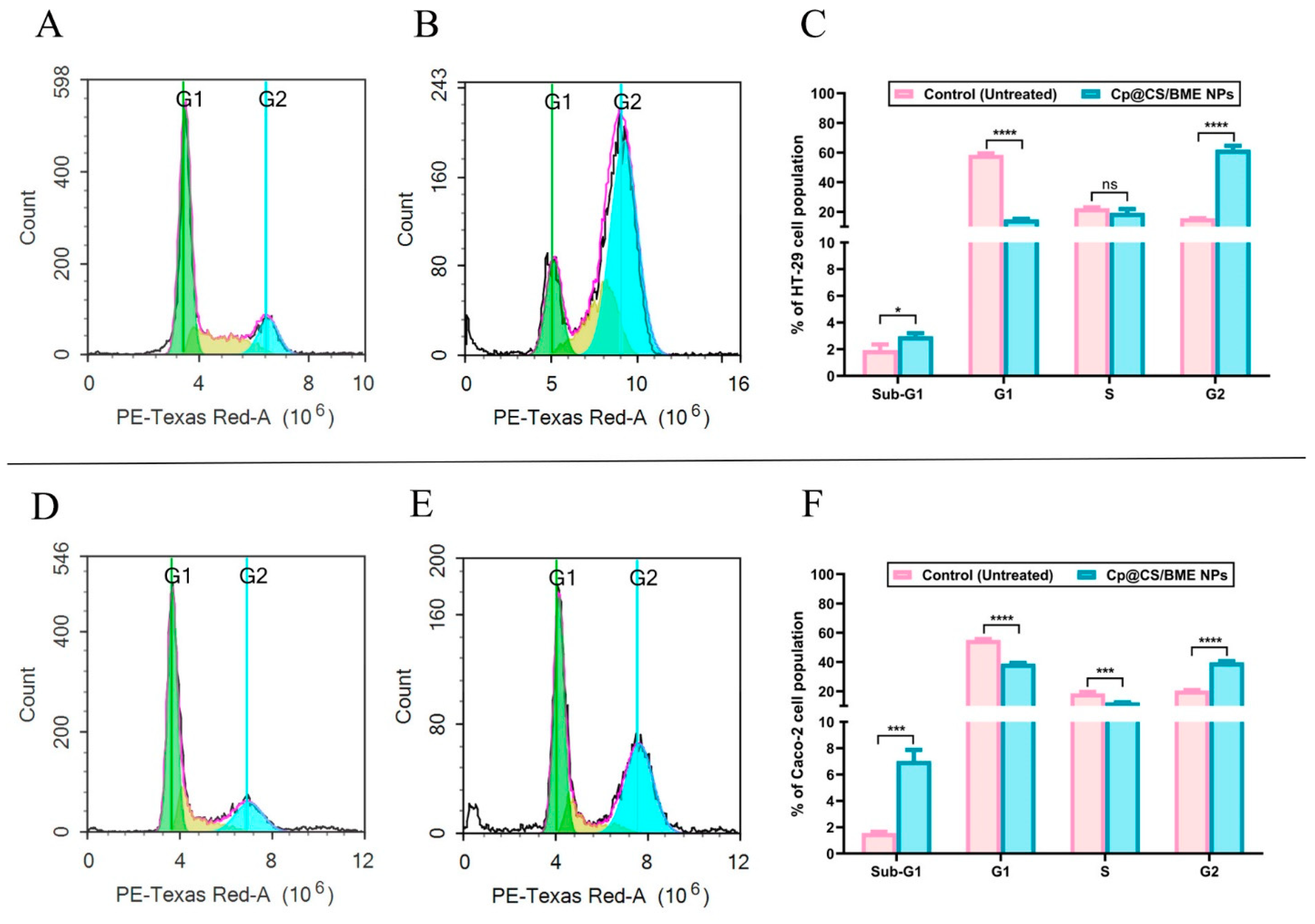
3.8. Cell-Cycle Analysis
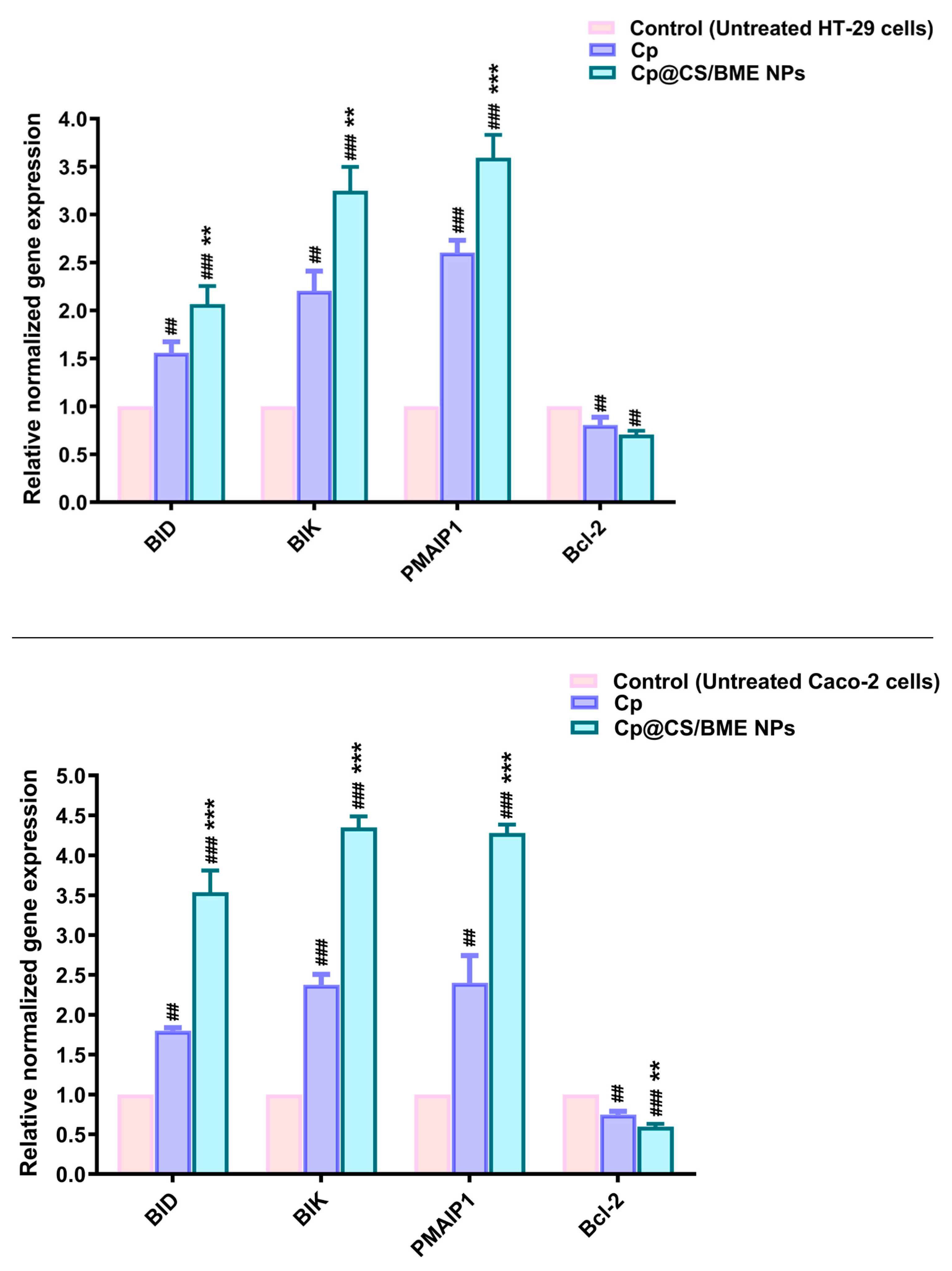
3.9. Gene Expression
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Biller, L.H.; Schrag, D. Diagnosis and Treatment of Metastatic Colorectal Cancer: A Review. JAMA 2021, 325, 669–685. [Google Scholar] [CrossRef]
- Xi, Y.; Xu, P. Global colorectal cancer burden in 2020 and projections to 2040. Transl. Oncol. 2021, 14, 101174. [Google Scholar] [CrossRef]
- Buyana, B.; Naki, T.; Alven, S.; Aderibigbe, B.A. Nanoparticles Loaded with Platinum Drugs for Colorectal Cancer Therapy. Int. J. Mol. Sci. 2022, 23, 11261. [Google Scholar] [CrossRef]
- Ritacco, I.; Al Assy, M.; Abd El-Rahman, M.K.; Fahmy, S.A.; Russo, N.; Shoeib, T.; Sicilia, E. Hydrolysis in Acidic Environment and Degradation of Satraplatin: A Joint Experimental and Theoretical Investigation. Inorg. Chem. 2017, 56, 6013–6026. [Google Scholar] [CrossRef]
- Sedky, N.K.; Abdel-Kader, N.M.; Issa, M.Y.; Abdelhady, M.M.M.; Shamma, S.N.; Bakowsky, U.; Fahmy, S.A. Co-Delivery of Ylang Ylang Oil of Cananga odorata and Oxaliplatin Using Intelligent pH-Sensitive Lipid-Based Nanovesicles for the Effective Treatment of Triple-Negative Breast Cancer. Int. J. Mol. Sci. 2023, 24, 8392. [Google Scholar] [CrossRef]
- Fahmy, S.A.; Ponte, F.; Grande, G.; Fawzy, I.M.; Mandour, A.A.; Sicilia, E.; Azzazy, H.M.E.-S. Synthesis, Characterization and Host-Guest Complexation of Asplatin: Improved In Vitro Cytotoxicity and Biocompatibility as Compared to Cisplatin. Pharmaceuticals 2022, 15, 259. [Google Scholar] [CrossRef]
- Fahmy, S.A.; Preis, E.; Dayyih, A.A.; Alawak, M.; El-Said Azzazy, H.M.; Bakowsky, U.; Shoeib, T. Thermosensitive Liposomes Encapsulating Nedaplatin and Picoplatin Demonstrate Enhanced Cytotoxicity against Breast Cancer Cells. ACS Omega 2022, 7, 42115–42125. [Google Scholar] [CrossRef]
- Sedky, N.K.; Braoudaki, M.; Mahdy, N.K.; Amin, K.; Fawzy, I.M.; Efthimiadou, E.K.; Youness, R.A.; Fahmy, S.A. Box–Behnken design of thermo-responsive nano-liposomes loaded with a platinum(iv) anticancer complex: Evaluation of cytotoxicity and apoptotic pathways in triple negative breast cancer cells. Nanoscale Adv. 2023, 5, 5399–5413. [Google Scholar] [CrossRef]
- Moses, S.; Edwards, V.; Brantley, E. Cytotoxicity in MCF-7 and MDA-MB-231 breast cancer cells, without harming MCF-10A healthy cells. J. Nanomed. Nanotechnol. 2016, 7, 1000369. [Google Scholar]
- Al-Harrasi, A.; Al-Saidi, S. Phytochemical analysis of the essential oil from botanically certified oleogum resin of Boswellia sacra (Omani Luban). Molecules 2008, 13, 2181–2189. [Google Scholar] [CrossRef]
- Frank, M.B.; Yang, Q.; Osban, J.; Azzarello, J.T.; Saban, M.R.; Saban, R.; Ashley, R.A.; Welter, J.C.; Fung, K.M.; Lin, H.K. Frankincense oil derived from Boswellia carteri induces tumor cell specific cytotoxicity. BMC Complement. Altern. Med. 2009, 9, 6. [Google Scholar] [CrossRef]
- Azzazy, H.M.E.; Abdelnaser, A.; Al Mulla, H.; Sawy, A.M.; Shamma, S.N.; Elhusseiny, M.; Alwahibi, S.; Mahdy, N.K.; Fahmy, S.A. Essential Oils Extracted from Boswellia sacra Oleo Gum Resin Loaded into PLGA-PCL Nanoparticles: Enhanced Cytotoxic and Apoptotic Effects against Breast Cancer Cells. ACS Omega 2023, 8, 1017–1025. [Google Scholar] [CrossRef]
- Sedky, N.K.; Mahdy, N.K.; Abdel-kader, N.M.; Abdelhady, M.M.M.; Maged, M.; Allam, A.L.; Alfaifi, M.Y.; Shamma, S.N.; Hassan, H.A.F.M.; Fahmy, S.A. Facile sonochemically-assisted bioengineering of titanium dioxide nanoparticles and deciphering their potential in treating breast and lung cancers: Biological, molecular, and computational-based investigations. RSC Adv. 2024, 14, 8583–8601. [Google Scholar] [CrossRef]
- Hassan, H.A.F.M.; Haider, M.; Fahmy, S.A. From antigen uptake to immune modulation: The multifaceted potential of peptide nanofibers as vaccine nanocarriers. Mater. Adv. 2024, 5, 4112–4130. [Google Scholar] [CrossRef]
- Al Jayoush, A.R.; Hassan, H.A.F.M.; Asiri, H.; Jafar, M.; Saeed, R.; Harati, R.; Haider, M. Niosomes for nose-to-brain delivery: A non-invasive versatile carrier system for drug delivery in neurodegenerative diseases. J. Drug Deliv. Sci. Technol. 2023, 89, 105007. [Google Scholar] [CrossRef]
- Ma, G.; Kostevsek, N.; Monaco, I.; Ruiz, A.; Markelc, B.; Cheung, C.C.L.; Hudoklin, S.; Kreft, M.E.; Hassan, H.; Barker, M.; et al. PD1 blockade potentiates the therapeutic efficacy of photothermally-activated and MRI-guided low temperature-sensitive magnetoliposomes. J. Control Release 2021, 332, 419–433. [Google Scholar] [CrossRef]
- Hassan, H.; Diebold, S.S.; Smyth, L.A.; Walters, A.A.; Lombardi, G.; Al-Jamal, K.T. Application of carbon nanotubes in cancer vaccines: Achievements, challenges and chances. J. Control Release 2019, 297, 79–90. [Google Scholar] [CrossRef]
- Yan, X.; Bernard, J.; Ganachaud, F. Nanoprecipitation as a simple and straightforward process to create complex polymeric colloidal morphologies. Adv. Colloid. Interface Sci. 2021, 294, 102474. [Google Scholar] [CrossRef]
- Snima, K.S.; Nair, R.S.; Nair, S.V.; Kamath, C.R.; Lakshmanan, V.K. Combination of Anti-Diabetic Drug Metformin and Boswellic Acid Nanoparticles: A Novel Strategy for Pancreatic Cancer Therapy. J. Biomed. Nanotechnol. 2015, 11, 93–104. [Google Scholar] [CrossRef]
- Youness, R.A.; Al-Mahallawi, A.M.; Mahmoud, F.H.; Atta, H.; Braoudaki, M.; Fahmy, S.A. Oral Delivery of Psoralidin by Mucoadhesive Surface-Modified Bilosomes Showed Boosted Apoptotic and Necrotic Effects against Breast and Lung Cancer Cells. Polymers 2023, 15, 1464. [Google Scholar] [CrossRef]
- AbuBakr, A.H.; Hassan, H.; Abdalla, A.; Khowessah, O.M.; Abdelbary, G.A. Therapeutic potential of cationic bilosomes in the treatment of carrageenan-induced rat arthritis via fluticasone propionate gel. Int. J. Pharm. 2023, 635, 122776. [Google Scholar] [CrossRef]
- Abonashey, S.G.; Hassan, H.; Shalaby, M.A.; Fouad, A.G.; Mobarez, E.; El-Banna, H.A. Formulation, pharmacokinetics, and antibacterial activity of florfenicol-loaded niosome. Drug Deliv. Transl. Res. 2024, 14, 1077–1092. [Google Scholar] [CrossRef]
- Amin, M.U.; Ali, S.; Ali, M.Y.; Tariq, I.; Nasrullah, U.; Pinnapreddy, S.R.; Wolk, C.; Bakowsky, U.; Brussler, J. Enhanced efficacy and drug delivery with lipid coated mesoporous silica nanoparticles in cancer therapy. Eur. J. Pharm. Biopharm. 2021, 165, 31–40. [Google Scholar] [CrossRef]
- Fahmy, S.A.; Ponte, F.; Sicilia, E.; El-Said Azzazy, H.M. Experimental and Computational Investigations of Carboplatin Supramolecular Complexes. ACS Omega 2020, 5, 31456–31466. [Google Scholar] [CrossRef]
- Sedky, N.K.; Arafa, K.K.; Abdelhady, M.M.M.; Issa, M.Y.; Abdel-Kader, N.M.; Mahdy, N.K.; Mokhtar, F.A.; Alfaifi, M.Y.; Fahmy, S.A. Nedaplatin/Peganum harmala Alkaloids Co-Loaded Electrospun, Implantable Nanofibers: A Chemopreventive Nano-Delivery System for Treating and Preventing Breast Cancer Recurrence after Tumorectomy. Pharmaceutics 2023, 15, 2367. [Google Scholar] [CrossRef]
- Pooresmaeil, M.; Namazi, H. Facile preparation of pH-sensitive chitosan microspheres for delivery of curcumin; characterization, drug release kinetics and evaluation of anticancer activity. Int. J. Biol. Macromol. 2020, 162, 501–511. [Google Scholar] [CrossRef]
- Yu, L.; Xie, X.; Cao, X.; Chen, J.; Chen, G.; Chen, Y.; Li, G.; Qin, J.; Peng, F.; Peng, C. The Anticancer Potential of Maslinic Acid and Its Derivatives: A Review. Drug Des. Devel. Ther. 2021, 15, 3863–3879. [Google Scholar] [CrossRef]
- Rosellini, M.; Schulze, A.; Omer, E.A.; Ali, N.T.; Marini, F.; Kupper, J.H.; Efferth, T. The Effect of Plastic-Related Compounds on Transcriptome-Wide Gene Expression on CYP2C19-Overexpressing HepG2 Cells. Molecules 2023, 28, 5952. [Google Scholar] [CrossRef]
- Dawoud, M. Chitosan coated solid lipid nanoparticles as promising carriers for docetaxel. J. Drug Deliv. Sci. Technol. 2021, 62, 102409. [Google Scholar] [CrossRef]
- Park, S.N.; Jo, N.R.; Jeon, S.H. Chitosan-coated liposomes for enhanced skin permeation of resveratrol. J. Ind. Eng. Chem. 2014, 20, 1481–1485. [Google Scholar] [CrossRef]
- Prabha, S.; Arya, G.; Chandra, R.; Ahmed, B.; Nimesh, S. Effect of size on biological properties of nanoparticles employed in gene delivery. Artif. Cells Nanomed. Biotechnol. 2016, 44, 83–91. [Google Scholar] [CrossRef]
- Elkomy, M.H.; Ali, A.A.; Eid, H.M. Chitosan on the surface of nanoparticles for enhanced drug delivery: A comprehensive review. J. Control Release 2022, 351, 923–940. [Google Scholar] [CrossRef]
- Durán, V.; Yasar, H.; Becker, J.; Thiyagarajan, D.; Loretz, B.; Kalinke, U.; Lehr, C.-M. Preferential uptake of chitosan-coated PLGA nanoparticles by primary human antigen presenting cells. Nanomed. Nanotechnol. Biol. Med. 2019, 21, 102073. [Google Scholar] [CrossRef]
- Hassan, H.A.F.M.; Ali, A.I.; ElDesawy, E.M.; ElShafeey, A.H. Pharmacokinetic and Pharmacodynamic Evaluation of Gemifloxacin Chitosan Nanoparticles As an Antibacterial Ocular Dosage Form. J. Pharm. Sci. 2022, 111, 1497–1508. [Google Scholar] [CrossRef]
- Boedtkjer, E.; Pedersen, S.F. The Acidic Tumor Microenvironment as a Driver of Cancer. Annu. Rev. Physiol. 2020, 82, 103–126. [Google Scholar] [CrossRef]
- Sharma, S.; Gupta, P.; Kawish, S.; Ahmad, S.; Iqbal, Z.; Vohora, D.; Kohli, K. Novel Chitosan-Coated Liposomes Coloaded with Exemestane and Genistein for an Effective Breast Cancer Therapy. ACS Omega 2024, 9, 9735–9752. [Google Scholar] [CrossRef]
- Dhavale, R.P.; Dhavale, R.; Sahoo, S.; Kollu, P.; Jadhav, S.; Patil, P.; Dongale, T.; Chougale, A.; Patil, P. Chitosan coated magnetic nanoparticles as carriers of anticancer drug Telmisartan: pH-responsive controlled drug release and cytotoxicity studies. J. Phys. Chem. Solids 2021, 148, 109749. [Google Scholar] [CrossRef]
- Hu, X.; Wang, Y.; Peng, B. Chitosan-capped mesoporous silica nanoparticles as pH-responsive nanocarriers for controlled drug release. Chem.–Asian J. 2014, 9, 319–327. [Google Scholar] [CrossRef]
- Ahmadifard, Z.; Ahmeda, A.; Rasekhian, M.; Moradi, S.; Arkan, E. Chitosan-coated magnetic solid lipid nanoparticles for controlled release of letrozole. J. Drug Deliv. Sci. Technol. 2020, 57, 101621. [Google Scholar] [CrossRef]
- Thomas, M.B.; Radhakrishnan, K.; Gnanadhas, D.P.; Chakravortty, D.; Raichur, A.M. Intracellular delivery of doxorubicin encapsulated in novel pH-responsive chitosan/heparin nanocapsules. Int. J. Nanomed. 2013, 8, 267–273. [Google Scholar] [CrossRef]
- Zolnik, B.S.; Burgess, D.J. Effect of acidic pH on PLGA microsphere degradation and release. J. Control Release 2007, 122, 338–344. [Google Scholar] [CrossRef]
- Shinn, J.; Kwon, N.; Lee, S.A.; Lee, Y. Smart pH-responsive nanomedicines for disease therapy. J. Pharm. Investig. 2022, 52, 427–441. [Google Scholar] [CrossRef]
- AlSawaftah, N.M.; Awad, N.S.; Pitt, W.G.; Husseini, G.A. pH-Responsive Nanocarriers in Cancer Therapy. Polymers 2022, 14, 936. [Google Scholar] [CrossRef]
- Pourtalebi Jahromi, L.; Ghazali, M.; Ashrafi, H.; Azadi, A. A comparison of models for the analysis of the kinetics of drug release from PLGA-based nanoparticles. Heliyon 2020, 6, e03451. [Google Scholar] [CrossRef]
- Paul, D.R. Elaborations on the Higuchi model for drug delivery. Int. J. Pharm. 2011, 418, 13–17. [Google Scholar] [CrossRef]
- Bai, X.; Smith, Z.L.; Wang, Y.; Butterworth, S.; Tirella, A. Sustained Drug Release from Smart Nanoparticles in Cancer Therapy: A Comprehensive Review. Micromachines 2022, 13, 1623. [Google Scholar] [CrossRef]
- Wu, I.Y.; Bala, S.; Škalko-Basnet, N.; di Cagno, M.P. Interpreting non-linear drug diffusion data: Utilizing Korsmeyer-Peppas model to study drug release from liposomes. Eur. J. Pharm. Sci. 2019, 138, 105026. [Google Scholar] [CrossRef]
- Chou, Y.-H.; Liu, Y.-L.; Hsu, T.-C.; Yow, J.-L.; Tzang, B.-S.; Chiang, W.-H. Tumor acidity-responsive polymeric nanoparticles to promote intracellular delivery of zoledronic acid by PEG detachment and positive charge exposure for enhanced antitumor potency. J. Mater. Chem. B 2022, 10, 4363–4374. [Google Scholar] [CrossRef]
- Choi, S.Y.; Jang, S.H.; Park, J.; Jeong, S.; Park, J.H.; Ock, K.S.; Lee, K.; Yang, S.I.; Joo, S.-W.; Ryu, P.D.; et al. Cellular uptake and cytotoxicity of positively charged chitosan gold nanoparticles in human lung adenocarcinoma cells. J. Nanoparticle Res. 2012, 14, 1234. [Google Scholar] [CrossRef]
- Barlogie, B.; Drewinko, B.; Schumann, J.; Gohde, W.; Dosik, G.; Latreille, J.; Johnston, D.A.; Freireich, E.J. Cellular DNA content as a marker of neoplasia in man. Am. J. Med. 1980, 69, 195–203. [Google Scholar] [CrossRef]
- Kodiha, M.; Wang, Y.M.; Hutter, E.; Maysinger, D.; Stochaj, U. Off to the organelles—Killing cancer cells with targeted gold nanoparticles. Theranostics 2015, 5, 357–370. [Google Scholar] [CrossRef]
- Suhail, M.M.; Wu, W.; Cao, A.; Mondalek, F.G.; Fung, K.-M.; Shih, P.-T.; Fang, Y.-T.; Woolley, C.; Young, G.; Lin, H.-K. Boswellia sacra essential oil induces tumor cell-specific apoptosis and suppresses tumor aggressiveness in cultured human breast cancer cells. BMC Complement. Altern. Med. 2011, 11, 129. [Google Scholar] [CrossRef]
- Becer, E.; Kabadayı, H.; Başer, K.H.C.; Vatansever, H.S. Boswellia sacra essential oil manages colon cancer stem cells proliferation and apoptosis: A new perspective for cure. J. Essent. Oil Res. 2021, 33, 53–62. [Google Scholar] [CrossRef]
- Rostami, E. Progresses in targeted drug delivery systems using chitosan nanoparticles in cancer therapy: A mini-review. J. Drug Deliv. Sci. Technol. 2020, 58, 101813. [Google Scholar] [CrossRef]
- El-Fakharany, Z.S.; Nissan, Y.M.; Sedky, N.K.; Arafa, R.K.; Abou-Seri, S.M. New proapoptotic chemotherapeutic agents based on the quinolone-3-carboxamide scaffold acting by VEGFR-2 inhibition. Sci. Rep. 2023, 13, 11346. [Google Scholar] [CrossRef]
- Oliveira, P.F.d.; Alves, J.M.; Damasceno, J.L.; Oliveira, R.A.M.; Dias, H.J.; Crotti, A.E.M.; Tavares, D.C. Cytotoxicity screening of essential oils in cancer cell lines. Rev. Bras. Farmacogn. 2015, 25, 183–188. [Google Scholar] [CrossRef]
- Van Hees, S.; Elbrink, K.; De Schryver, M.; Delputte, P.L.; Kiekens, F. Improving cellular uptake and cytotoxicity of chitosan-coated poly(lactic-co-glycolic acid) nanoparticles in macrophages. Nanomedicine 2020, 15, 2671–2688. [Google Scholar] [CrossRef]
- Liu, J.; Xu, L.; Liu, C.; Zhang, D.; Wang, S.; Deng, Z.; Lou, W.; Xu, H.; Bai, Q.; Ma, J. Preparation and characterization of cationic curcumin nanoparticles for improvement of cellular uptake. Carbohydr. Polym. 2012, 90, 16–22. [Google Scholar] [CrossRef]
- Becer, E.; Altundag, E.M.; Özbilenler, C.; Vatansever, H.S.; Baser, K.H.C. Antiproliferative, antioxidant and anti-inflammatory effects of Boswellia Sacra on human pancreatic cancer cells. J. Essent. Oil Bear. Plants 2023, 26, 836–847. [Google Scholar] [CrossRef]
- Kilic, A.; Barlak, N.; Sanli, F.; Aytatli, A.; Capik, O.; Karatas, O.F. Mode of action of carboplatin via activating p53/miR-145 axis in head and neck cancers. Laryngoscope 2020, 130, 2818–2824. [Google Scholar] [CrossRef]
- Jakimov, D.; Bogdanović, V.; Djuran, M.I.; Jurišić, V.; Kojić, V. In vitro antitumor activity of carboplatin and analogues. J. Coord. Chem. 2024, 77, 697–709. [Google Scholar] [CrossRef]
- Aborehab, N.M.; Abd-Elmawla, M.A.; ElSayed, A.M.; Sabry, O.; Ezzat, S.M. Acovenoside A as a novel therapeutic approach to boost taxol and carboplatin apoptotic and antiproliferative activities in NSCLC: Interplay of miR-630/miR-181a and apoptosis genes. Bioorg. Chem. 2023, 139, 106743. [Google Scholar] [CrossRef]
- Vidot, S.; Witham, J.; Agarwal, R.; Greenhough, S.; Bamrah, H.S.; Tigyi, G.J.; Kaye, S.B.; Richardson, A. Autotaxin delays apoptosis induced by carboplatin in ovarian cancer cells. Cell. Signal. 2010, 22, 926–935. [Google Scholar] [CrossRef]
- Singh, S.; Upadhyay, A.K.; Ajay, A.K.; Bhat, M.K. p53 regulates ERK activation in carboplatin induced apoptosis in cervical carcinoma: A novel target of p53 in apoptosis. FEBS Lett. 2007, 581, 289–295. [Google Scholar] [CrossRef]
- De Oliveira, L.Z.; Farias, I.L.G.; Rigo, M.L.; Glanzner, W.G.; Gonçalves, P.B.D.; Cadoná, F.C.; Cruz, I.B.; Farias, J.G.; Duarte, M.M.; Franco, L. Effect of Uncaria tomentosa extract on apoptosis triggered by oxaliplatin exposure on HT29 cells. Evid.-Based Complement. Altern. Med. 2014, 2014, 274786. [Google Scholar] [CrossRef]
- Zhang, G.; Zhang, Z.; Yang, J. DNA tetrahedron delivery enhances doxorubicin-induced apoptosis of HT-29 colon cancer cells. Nanoscale Res. Lett. 2017, 12, 495. [Google Scholar] [CrossRef]
- Zhang, Y.-Q.; Tang, X.-Q.; Sun, L.; Dong, L.; Qin, Y.; Liu, H.-Q.; Xia, H.; Cao, J.-G. Rosiglitazone enhances fluorouracil-induced apoptosis of HT-29 cells by activating peroxisome proliferator-activated receptor γ. World J. Gastroenterol. WJG 2007, 13, 1534. [Google Scholar] [CrossRef][Green Version]
- Alsufiani, H.M. The synergistic effect of oxaliplatin and punicalagin on colon cancer cells Caco-2 death. Int. J. Health Sci. 2024, 18, 33. [Google Scholar]
- Jadid, M.F.S.; Aghaei, E.; Taheri, E.; Seyyedsani, N.; Chavoshi, R.; Abbasi, S.; Khorrami, A.; Goleij, P.; Hajazimian, S.; Taefehshokr, S. Melatonin increases the anticancer potential of doxorubicin in Caco-2 colorectal cancer cells. Environ. Toxicol. 2021, 36, 1061–1069. [Google Scholar] [CrossRef]
- Abo El-Maali, N.; Wahman, A.Y.; Aly, A.A.; Nassar, A.Y.; Sayed, D.M. Anticancer activity of lanthanum (III) and europium (III) 5-fluorouracil complexes on Caco-2 cell line. Appl. Organomet. Chem. 2020, 34, e5594. [Google Scholar] [CrossRef]
- Pozarowski, P.; Darzynkiewicz, Z. Analysis of Cell Cycle by Flow Cytometry. In Checkpoint Controls and Cancer: Volume 2: Activation and Regulation Protocols; Schönthal, A.H., Ed.; Humana Press: Totowa, NJ, USA, 2004; pp. 301–311. [Google Scholar]
- Park, M.T.; Lee, S.J. Cell cycle and cancer. J. Biochem. Mol. Biol. 2003, 36, 60–65. [Google Scholar] [CrossRef]
- Williams, G.H.; Stoeber, K. The cell cycle and cancer. J. Pathol. 2012, 226, 352–364. [Google Scholar] [CrossRef]
- Zhu, X.; Peng, Y.; Qiu, L. Amino-functionalized nano-vesicles for enhanced anticancer efficacy and reduced myelotoxicity of carboplatin. Colloids Surf. B Biointerfaces 2017, 157, 56–64. [Google Scholar] [CrossRef]
- Tessoulin, B.; Papin, A.; Gomez-Bougie, P.; Bellanger, C.; Amiot, M.; Pellat-Deceunynck, C.; Chiron, D. BCL2-Family Dysregulation in B-Cell Malignancies: From Gene Expression Regulation to a Targeted Therapy Biomarker. Front. Oncol. 2018, 8, 645. [Google Scholar] [CrossRef]
- Sinicrope, F.A.; Rego, R.L.; Foster, N.R.; Thibodeau, S.N.; Alberts, S.R.; Windschitl, H.E.; Sargent, D.J. Proapoptotic Bad and Bid Protein Expression Predict Survival in Stages II and III Colon Cancers. Clin. Cancer Res. 2008, 14, 4128–4133. [Google Scholar] [CrossRef]
- Morsi, Z.R.; Hage-Sleiman, R.; Kobeissy, H.; Dbaibo, G. Noxa: Role in Cancer Pathogenesis and Treatment. Curr. Cancer Drug Targets 2018, 18, 914–928. [Google Scholar] [CrossRef]
- Kutuk, O.; Aytan, N.; Karakas, B.; Kurt, A.G.; Acikbas, U.; Temel, S.G.; Basaga, H. Biphasic ROS production, p53 and BIK dictate the mode of cell death in response to DNA damage in colon cancer cells. PLoS ONE 2017, 12, e0182809. [Google Scholar] [CrossRef]
- Kazhdan, I.; Long, L.; Montellano, R.; Cavazos, D.A.; Marciniak, R.A. Targeted gene therapy for breast cancer with truncated Bid. Cancer Gene Ther. 2006, 13, 141–149. [Google Scholar] [CrossRef]
- Madesh, M.; Antonsson, B.; Srinivasula, S.M.; Alnemri, E.S.; Hajnoczky, G. Rapid kinetics of tBid-induced cytochrome c and Smac/DIABLO release and mitochondrial depolarization. J. Biol. Chem. 2002, 277, 5651–5659. [Google Scholar] [CrossRef]
- Chinnadurai, G.; Vijayalingam, S.; Rashmi, R. BIK, the founding member of the BH3-only family proteins: Mechanisms of cell death and role in cancer and pathogenic processes. Oncogene 2008, 27, S20–S29. [Google Scholar] [CrossRef]
- Hagenbuchner, J.; Ausserlechner, M.J.; Porto, V.; David, R.; Meister, B.; Bodner, M.; Villunger, A.; Geiger, K.; Obexer, P. The anti-apoptotic protein BCL2L1/Bcl-xL is neutralized by pro-apoptotic PMAIP1/Noxa in neuroblastoma, thereby determining bortezomib sensitivity independent of prosurvival MCL1 expression. J. Biol. Chem. 2010, 285, 6904–6912. [Google Scholar] [CrossRef]
- Li, T.; Yuan, J.; Xu, P.; Jia, J.; Zhao, J.; Zhang, J.; Ding, R.; Zhao, X.; He, D.; Wu, T.; et al. PMAIP1, a novel diagnostic and potential therapeutic biomarker in osteoporosis. Aging 2024, 16, 3694–3715. [Google Scholar] [CrossRef]
- Schmiech, M.; Lang, S.; Werner, K.; Schmidt, C.Q.; Syrovets, T.; Simmet, T. Boswellic Acid Composition of Frankincense Dietary Supplements and Correlation to Cytotoxic Efficacy against Treatment-Resistant Triple Negative Breast Cancer Cells. FASEB J. 2019, 33, 816.5. [Google Scholar] [CrossRef]


| Primer ID | Primer Sequence (5′-3′) |
|---|---|
| β-actin F | CACCATTGGCAATGAGCGGTTC |
| β-actin R | AGGTCTTTGCGGATGTCCACGT |
| BID F | TGGTGTTTGGCTTCCTCCAA |
| BID R | GAATCTGCCTCTATTCTTCCC |
| BIK F | GAGACATCTTGATGGAGACC |
| BIK R | TCTAAGAACATCCCTGATGT |
| Noxa (PMAIP1) F | AGCAGAGCTGGAAGTCGAGTGTG |
| Noxa (PMAIP1) R | TGATGCAGTCAGGTTCCTGAGC |
| Bcl-2 F | ATCGCCCTGTGGATGACTGAGT |
| Bcl-2 R | GCCAGGAGAAATCAAACAGAGGC |
| Peak | Rt | Assignment | Precursor Ion (m/z) | Molecular Formula | Productions MS/MS | Class |
|---|---|---|---|---|---|---|
| 1. | 2.65 | Quinic acid | 191.0455 | C7H12O6 | 191, 173, 147, 127, 109, 93, 87, 85, 67 | Organic acid |
| 2. | 2.77 | D-(+)-Trehalose | 341.1519 | C12H22O11 | 341, 211, 179, 89 | Disaccharide |
| 3. | 2.84 | Quinic acid | 191.0819 | C7H12O6 | 191, 173, 147, 127, 109, 93, 87, 85, 67 | Organic acid |
| 4. | 3.11 | Ureidosuccinic acid | 174.9804 | C5H8N2O5 | 175, 132 | Organic acid |
| 5. | 3.18 | Quinic acid | 191.0457 | C7H12O6 | 191, 173, 147, 127, 109, 93, 87, 85, 67 | Organic acid |
| 6. | 5.64 | Methylmalonic acid | 117.0362 | C4H6O4 | 117, 116, 115 | Organic acid |
| 7. | 10.56 | Oxalacetic acid | 131.0534 | C4H4O5 | 131, 130, 129, 128 | Organic acid |
| 8. | 10.64 | Neochlorogenic acid | 353.1439 | C16H18O9 | 353, 259, 191, 180 135, 134 | Phenolic acid |
| 9. | 10.79 | Tridecanoyl-sn-glycero-3-phosphate | 367.2089 | C21H44NO7P | 367, 311, 215, 153, 123 | Phospholipid |
| 10. | 10.83 | Neochlorogenic acid | 353.0947 | C16H18O9 | 353, 259, 191, 180 135, 134 | Phenolic acid |
| 11. | 11.05 | Neochlorogenic acid | 353.1336 | C16H18O9 | 353, 259, 191, 180 135, 134 | Phenolic acid |
| 12. | 11.24 | 2-(2-Hydroxyethoxy)phenol | 153.0406 | C8H10O3 | 153, 150, 109, 91 | Phenol |
| 13. | 12.80 | Gabapentin-related compound E | 185.1069 | C9H14O4 | 185, 142, 141, 123, 99, 81, 71, 57 | Organic acid |
| 14. | 14.54 | 6-Fluoro-4-hydroxycoumarin | 381.1810 | C9H5FO3 | 381, 309, 180, 179, 136, 135, 94 | Hydroxycoumarin |
| 15. | 15.07 | 2′-Hydroxy-4′-methoxyacetophenone | 165.0776 | C9H10O3 | 165, 150, 122, 108, 71 | Phenol |
| 16. | 15.22 | Madecassic acid | 503.4005 | C30H48O6 | 503, 499, 443, 371, 248 | Triterpene |
| 17. | 15.71 | 2′-Hydroxy-4′-methoxyacetophenone | 165.0785 | C9H10O3 | 165, 150, 122, 108, 71 | Phenol |
| 18. | 16.01 | Madecassic acid | 503.3997 | C30H48O6 | 503, 443, 399 | Triterpene |
| 19. | 16.35 | Maslinic acid | 471.3008 | C30H48O4 | 471, 427, 397, 353, 314, 263, 217, 189, 145, 113 | Triterpene |
| 20. | 16.47 | 4-Androsten-17.beta-ol-3-one sulfate | 367.2594 | C19H27O5S | 367, 287, 243, 85 | Steroid |
| 21. | 17.15 | 7,7-Dimethyl-(5Z,8Z)-eicosadienoic acid | 335.2658 | C22H40O2 | 335, 291 | Fatty acid |
| 22. | 17.26 | N-2-Hydroxyethylpiperazine | 251.1983 | C6H14N2O | 251 | Alkaloid |
| 23. | 17.34 | 3-Phenylbutyric acid | 163.0985 | C10H12O2 | 163, 148, 134 | Organic acid |
| 24. | 17.34 | Thomboxane B3 | 367.2588 | C20H32O6 | 367, 352, 331, 251, 230, 170, 169, 122, 97 | Eicosanoid |
| 25. | 17.60 | (+)-trans-Chrysanthemic acid | 167.1306 | C10H16O2 | 167, 133, 109 | Monoterpene |
| 26. | 17.87 | cis-4,10,13,16-Docosatetraenoic acid | 331.2335 | C22H36O2 | 331, 288, 287, 236, 83 | Fatty acid |
| 27. | 17.98 | Genkwanin | 283.0990 | C16H12O5 | 283, 268, 251, 179, 135, 79 | Flavonoid |
| 28. | 22.33 | 4-Chloro-alpha-(4-chlorophenyl)-benzeneacetic acid | 279.2334 | C14H9Cl2O2- | 279, 236, 235, 199, 183, 153, 134, 97, 71 | Organic acid |
| 29. | 22.90 | 11-Keto-beta-boswellic acid | 469.3891 | C30H46O4 | 469, 452, 407, 391, 376, 271, 61 | Triterpene |
| 30. | 23.58 | Trihydroxycholestanoic acid | 449.3703 | C27H46O | 449, 327 | Bile acid |
| 31. | 23.70 | 2,2′-Methylene-bis(6-tert-butyl-4-methylphenol) | 339.2758 | C23H32O2 | 339, 327, 165, 164, 163, 147 | Phenol |
| 32. | 24.38 | 3beta,7alpha-Dihydroxy-5-cholestenoic acid | 431.3579 | C27H44O4 | 431 | Bile acid |
| 33. | 24.53 | Maslinic acid | 471.4052 | C30H48O4 | 471 | Triterpene |
| 34. | 26.57 | 3-Acetyl-11-keto-beta-boswellic acid | 511.4039 | C32H48O5 | 511, 60, 59 | Triterpene |
| 35. | 27.37 | 3-Acetyl-11-keto-beta-boswellic acid | 511.4054 | C32H48O5 | 511, 60, 59 | Triterpene |
| Samples | Average Particle Size (nm) | PDI | EE (%) |
|---|---|---|---|
| BME NPs | 120.10 ± 5.10 | 0.11 ± 0.33 | - |
| Cp@CS/BME NPs | 160.20 ± 4.60 | 0.14 ± 0.04 | 86.50 ± 2.80 |
| pH 5.4 | pH 7.4 | ||
|---|---|---|---|
| Zero-order | k0 | 1.412 | 0.497 |
| R2 | 0.797 | 0.731 | |
| First-order | k1 | 0.041 | 0.040 |
| R2 | 0.539 | 0.385 | |
| Higuchi matrix | Kh | 10.910 | 3.943 |
| R2 | 0.970 | 0.937 | |
| Korsmeyer–Peppas | n | 0.608 | 0.605 |
| R2 | 0.640 | 0.757 | |
| Hixson–Crowell | κ t | 0.007 | 0.002 |
| R2 | 0.883 | 0.756 |
| Sample | CC50 a | SI for HT-29 Cancer Cells b | SI for Caco-2 Cancer Cells c |
|---|---|---|---|
| BME | 296.03 ± 3.99 | 3.17 | 3.42 |
| BME NPs | 190.00 ± 6.98 | 5.79 | 7.45 |
| Cp | 32.21 ± 1.97 | 2.02 | 2.36 |
| Cp@CS/BME NPs | 40.69 ± 2.29 | 13.00 | 27.31 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fahmy, S.A.; Sedky, N.K.; Hassan, H.A.F.M.; Abdel-Kader, N.M.; Mahdy, N.K.; Amin, M.U.; Preis, E.; Bakowsky, U. Synergistic Enhancement of Carboplatin Efficacy through pH-Sensitive Nanoparticles Formulated Using Naturally Derived Boswellia Extract for Colorectal Cancer Therapy. Pharmaceutics 2024, 16, 1282. https://doi.org/10.3390/pharmaceutics16101282
Fahmy SA, Sedky NK, Hassan HAFM, Abdel-Kader NM, Mahdy NK, Amin MU, Preis E, Bakowsky U. Synergistic Enhancement of Carboplatin Efficacy through pH-Sensitive Nanoparticles Formulated Using Naturally Derived Boswellia Extract for Colorectal Cancer Therapy. Pharmaceutics. 2024; 16(10):1282. https://doi.org/10.3390/pharmaceutics16101282
Chicago/Turabian StyleFahmy, Sherif Ashraf, Nada K. Sedky, Hatem A. F. M. Hassan, Nour M. Abdel-Kader, Noha Khalil Mahdy, Muhammad Umair Amin, Eduard Preis, and Udo Bakowsky. 2024. "Synergistic Enhancement of Carboplatin Efficacy through pH-Sensitive Nanoparticles Formulated Using Naturally Derived Boswellia Extract for Colorectal Cancer Therapy" Pharmaceutics 16, no. 10: 1282. https://doi.org/10.3390/pharmaceutics16101282
APA StyleFahmy, S. A., Sedky, N. K., Hassan, H. A. F. M., Abdel-Kader, N. M., Mahdy, N. K., Amin, M. U., Preis, E., & Bakowsky, U. (2024). Synergistic Enhancement of Carboplatin Efficacy through pH-Sensitive Nanoparticles Formulated Using Naturally Derived Boswellia Extract for Colorectal Cancer Therapy. Pharmaceutics, 16(10), 1282. https://doi.org/10.3390/pharmaceutics16101282











