Oral Delivery of Liraglutide-Loaded Zein/Eudragit-Chitosan Nanoparticles Provides Pharmacokinetic and Glycemic Outcomes Comparable to Its Subcutaneous Injection in Rats
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Development of Zein/Eudragit-Chitosan Nanoparticles Containing Liraglutide
2.3. Physicochemical Characterization
2.3.1. Mean Size, Polydispersity Index and Zeta Potential Analysis
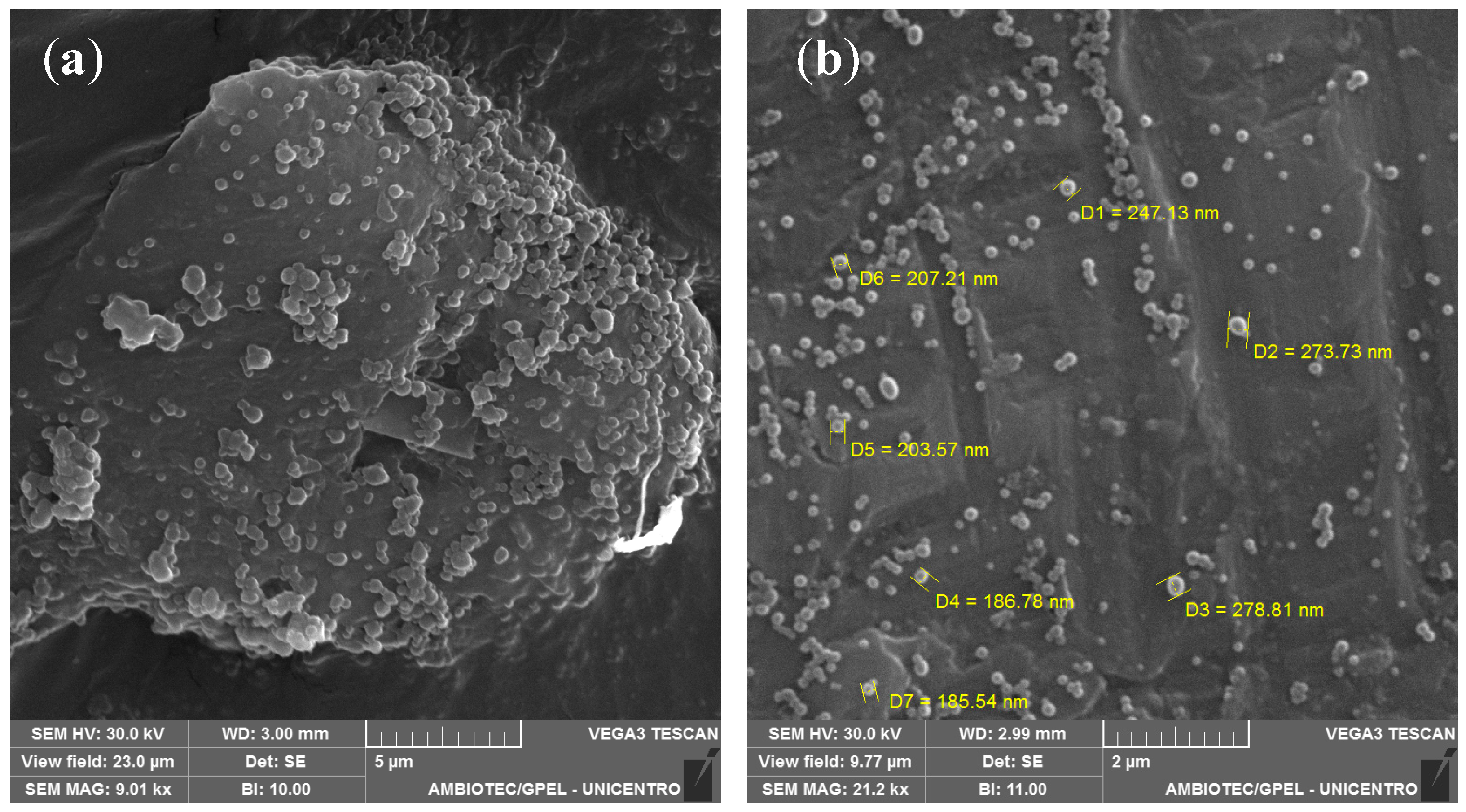
2.3.2. Morphological Analysis
2.3.3. Determination of the Encapsulation Efficiency
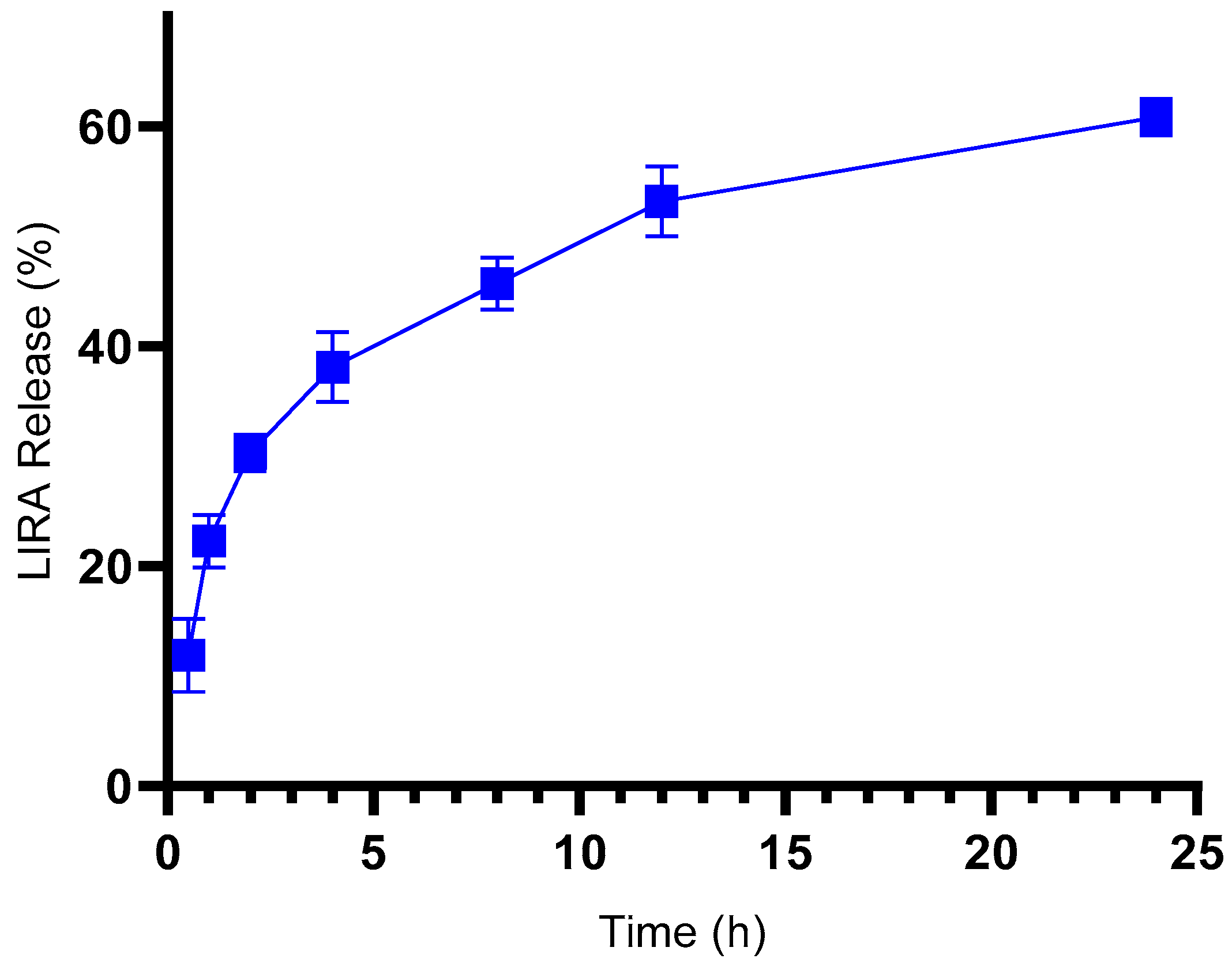
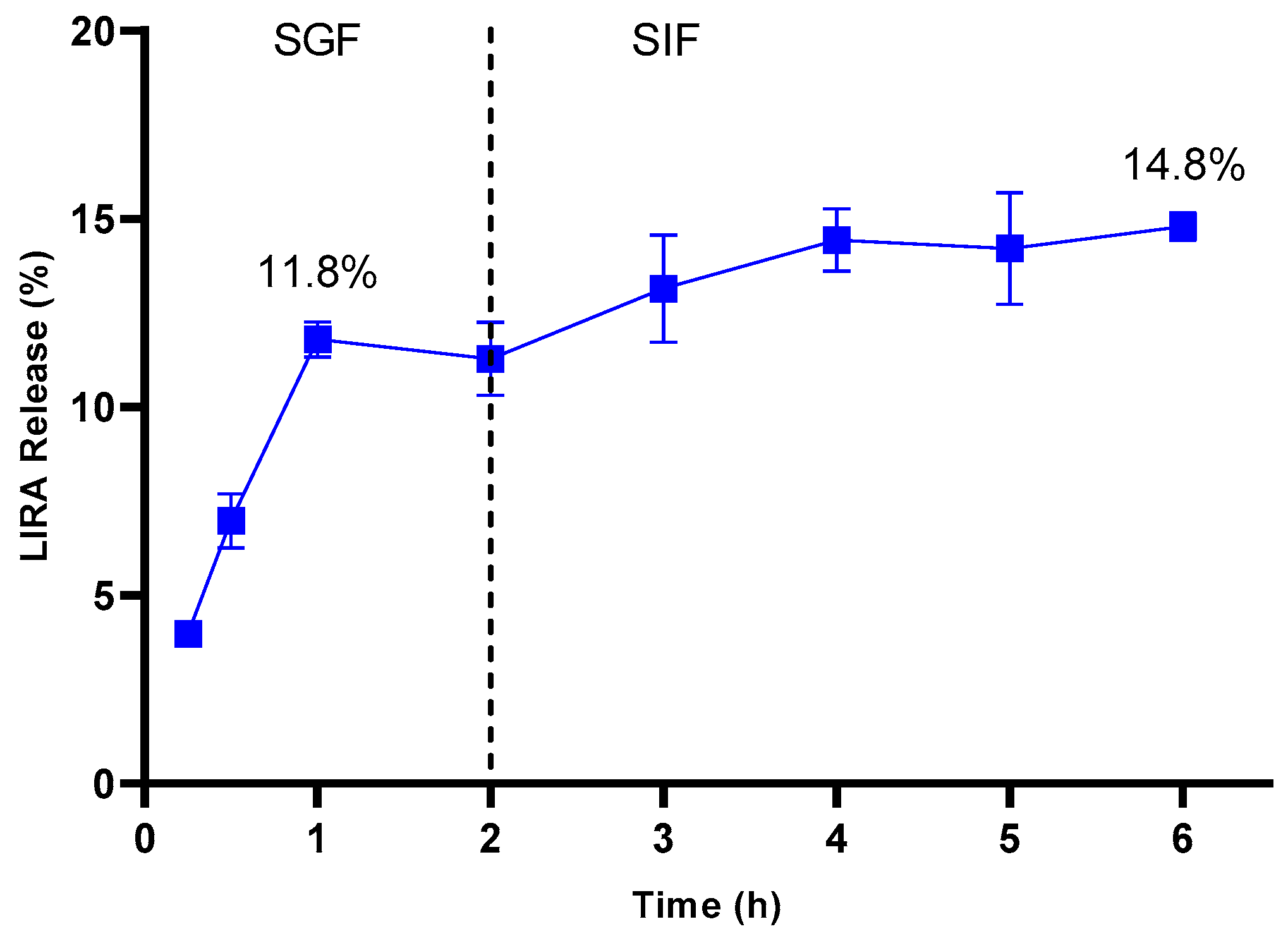
2.4. In Vitro Release Profile Assay
2.5. Pharmacokinetic Study
2.5.1. Ultra-Performance Liquid Chromatography Analysis
2.5.2. Pharmacokinetic Assay
2.5.3. Sample Preparation
2.5.4. Data Analysis
2.6. In Vivo Type 2 Diabetes Mellitus Experimental Model
2.7. Statistical Analysis
3. Results and Discussion
3.1. Development of Zein/Eudragit-Chitosan Nanoparticles Containing Liraglutide
3.2. Physicochemical Characterization
3.3. In Vitro Release Profile Assay
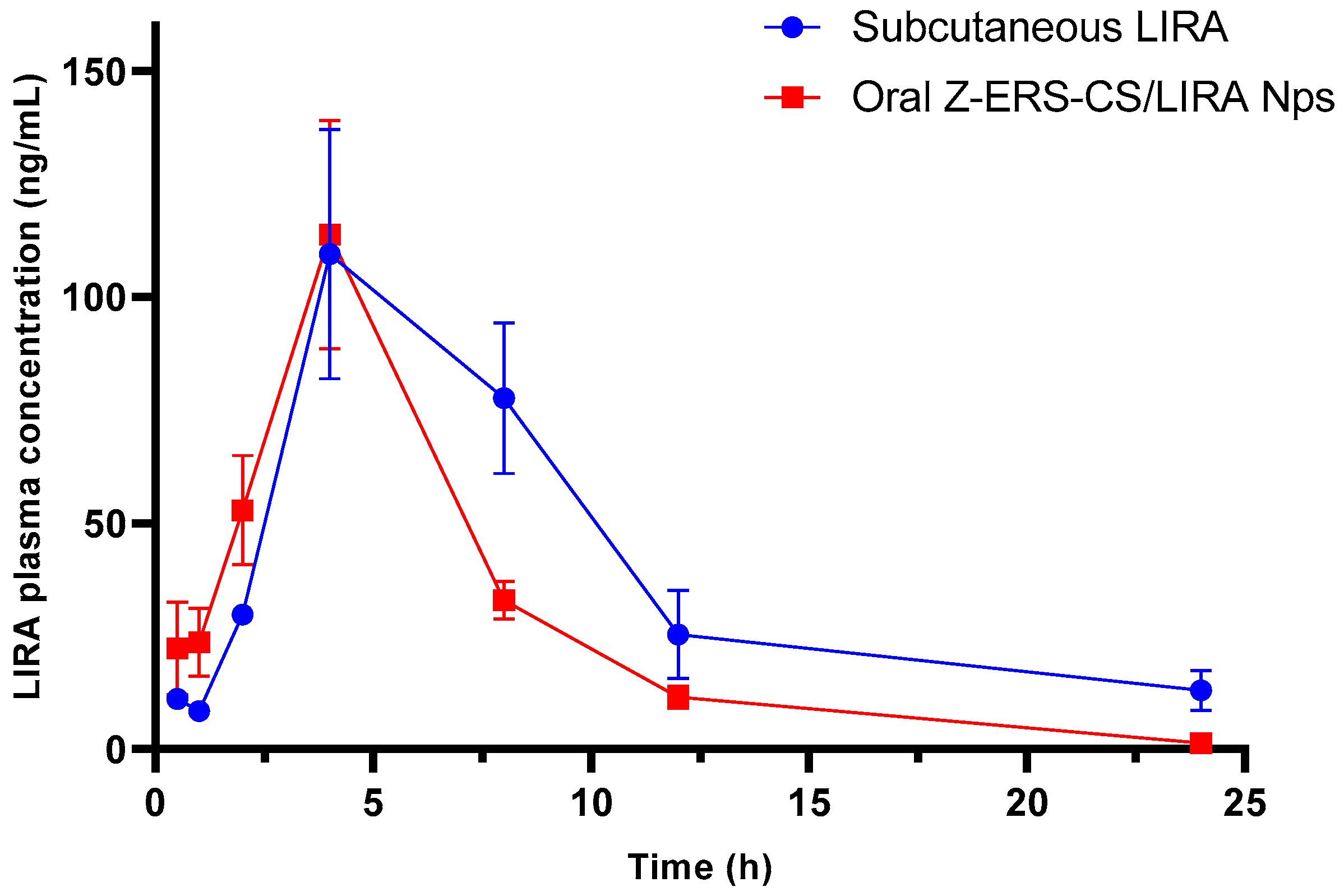
3.4. Pharmacokinetic Study
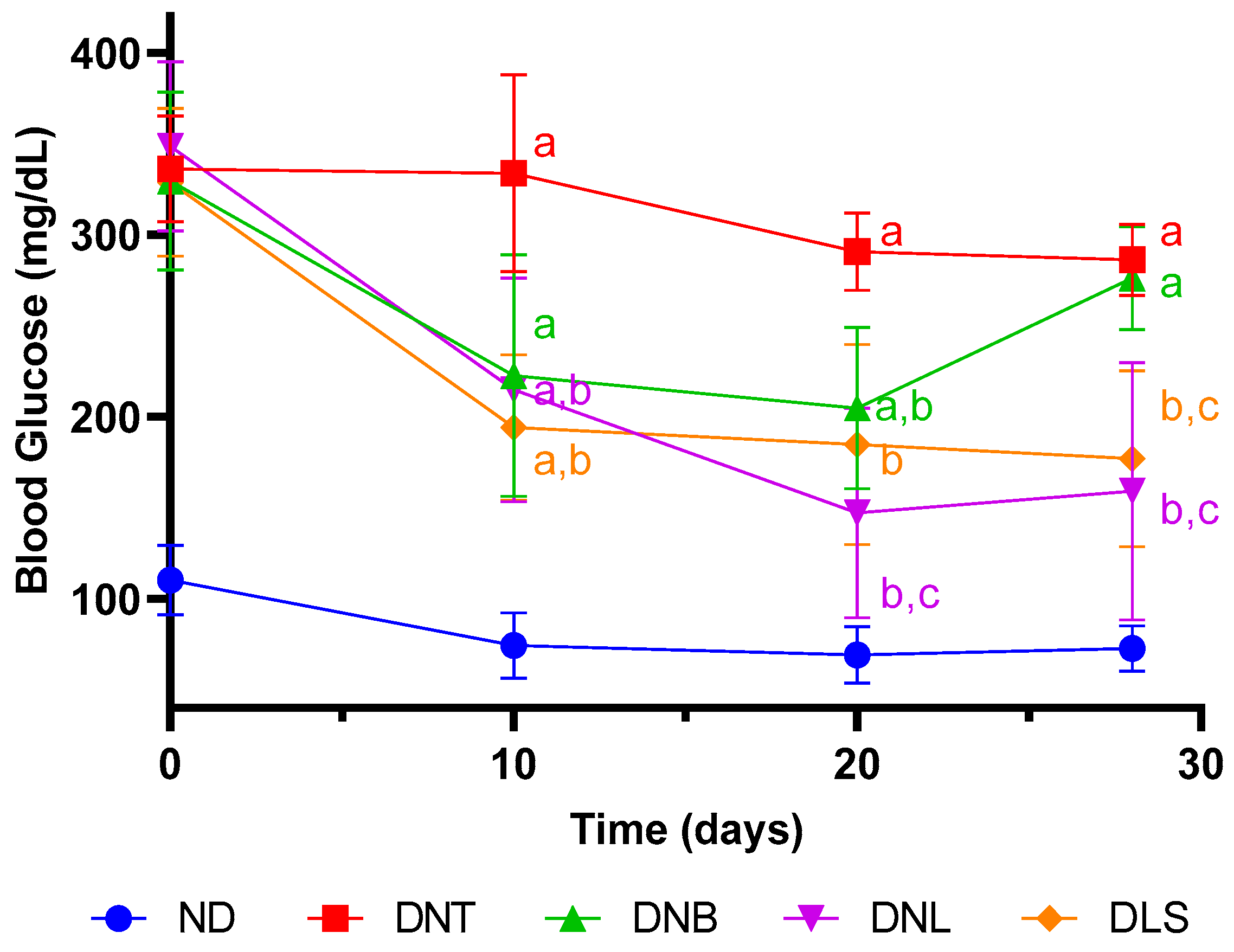
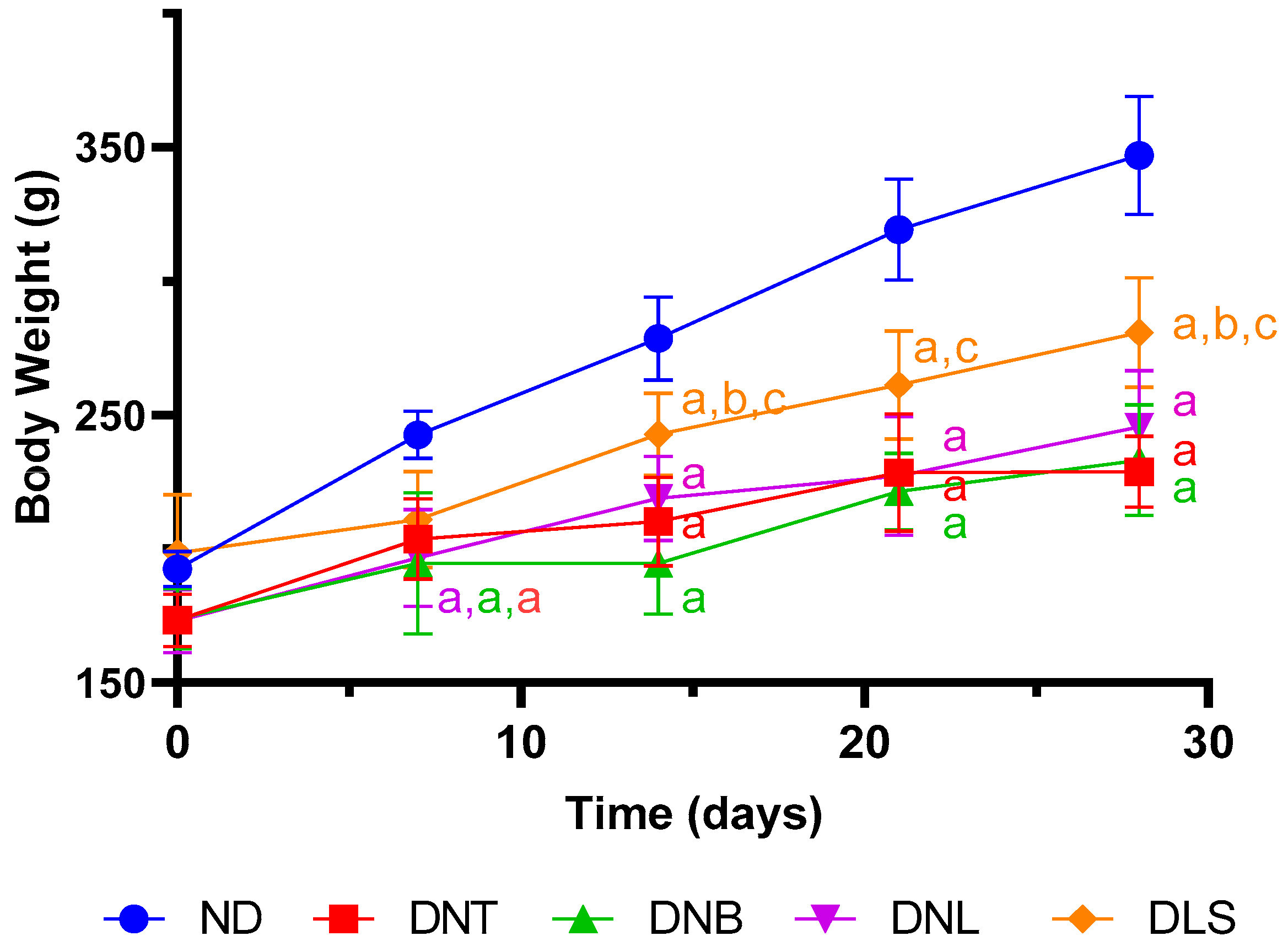
3.5. In Vivo Type 2 Diabetes Mellitus Experimental Model
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harreiter, J.; Roden, M. Diabetes Mellitus—Definition, Klassifikation, Diagnose, Screening Und Prävention (Update 2023). Wien. Klin. Wochenschr. 2023, 135, 7–17. [Google Scholar] [CrossRef]
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- Mahobiya, S.K.; Chauhan, N.; Balayan, S.; Kuchhal, N.K.; Islam, S.S.; Jain, U. Developing a Sensing Platform Based on Molecular Imprinting of HbA1c on Fe3O4 Nanoparticle Modified Screen-Printed Electrode. Biointerface Res. Appl. Chem. 2023, 13, 228. [Google Scholar] [CrossRef]
- Vasconcelos Silva, E.d.L.; de Jesus Oliveira, A.C.; de Carvalho Moreira, L.M.C.; Silva-Filho, E.C.; Wanderley, A.G.; Soares, M.F.d.L.R.; Soares-Sobrinho, J.L. Insulin-Loaded Nanoparticles Based on Acetylated Cashew Gum/Chitosan Complexes for Oral Administration and Diabetes Treatment. Int. J. Biol. Macromol. 2023, 242, 124737. [Google Scholar] [CrossRef]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and Regional Diabetes Prevalence Estimates for 2019 and Projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th Edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef] [PubMed]
- Damanik, J.; Yunir, E. Type 2 Diabetes Mellitus and Cognitive Impairment. Acta Medica Indones. 2021, 53, 213–220. [Google Scholar]
- Majety, P.; Lozada Orquera, F.A.; Edem, D.; Hamdy, O. Pharmacological Approaches to the Prevention of Type 2 Diabetes Mellitus. Front. Endocrinol. 2023, 14, 1118848. [Google Scholar] [CrossRef]
- Deacon, C.F. Potential of Liraglutide in the Treatment of Patients with Type 2 Diabetes. Vasc. Health Risk Manag. 2009, 5, 199–211. [Google Scholar] [CrossRef] [PubMed]
- Perry, C.M. Liraglutide. Drugs 2011, 71, 2347–2373. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, L.V.; Flint, A.; Olsen, A.K.; Ingwersen, S.H. Liraglutide in Type 2 Diabetes Mellitus: Clinical Pharmacokinetics and Pharmacodynamics. Clin. Pharmacokinet. 2016, 55, 657–672. [Google Scholar] [CrossRef]
- AlSaadoun, A.R.; AlSaadoun, T.R.; Al Ghumlas, A.K. Liraglutide Overdose-Induced Acute Pancreatitis. Cureus 2022, 14, e21616. [Google Scholar] [CrossRef]
- Javed, H.; Kogilathota Jagirdhar, G.S.; Kashyap, R.; Vekaria, P.H. Liraglutide-Induced Pancreatitis: A Case Report and Literature Review. Cureus 2023, 15, e38263. [Google Scholar] [CrossRef] [PubMed]
- Tamborlane, W.V.; Barrientos-Pérez, M.; Fainberg, U.; Frimer-Larsen, H.; Hafez, M.; Hale, P.M.; Jalaludin, M.Y.; Kovarenko, M.; Libman, I.; Lynch, J.L.; et al. Liraglutide in Children and Adolescents with Type 2 Diabetes. N. Engl. J. Med. 2019, 381, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Mainardes, R.; Silva, L. Drug Delivery Systems: Past, Present, and Future. Curr. Drug Targets 2004, 5, 449–455. [Google Scholar] [CrossRef] [PubMed]
- De Jong, W.H.; Borm, P.J.A. Drug Delivery and Nanoparticles: Applications and Hazards. Int. J. Nanomed. 2008, 3, 133–149. [Google Scholar] [CrossRef] [PubMed]
- Parveen, S.; Misra, R.; Sahoo, S.K. Nanoparticles: A Boon to Drug Delivery, Therapeutics, Diagnostics and Imaging. Nanomedicine 2012, 8, 147–166. [Google Scholar] [CrossRef] [PubMed]
- Campos, L.A.d.A.; Neto, A.F.S.; Noronha, M.C.S.; de Lima, M.F.; Cavalcanti, I.M.F.; Santos-Magalhães, N.S. Zein Nanoparticles for Drug Delivery: Preparation Methods and Biological Applications. Int. J. Pharm. 2023, 635, 122754. [Google Scholar] [CrossRef] [PubMed]
- Reboredo, C.; Gonz, C.J.; Luisa, A.; Mart, C.; Sarmento, B.; Irache, J.M. Zein-Based Nanoparticles as Oral Carriers for Insulin Delivery. Pharmaceutics 2022, 14, 39. [Google Scholar] [CrossRef] [PubMed]
- Heep, G.; Almeida, A.; Marcano, R.; Vieira, D.; Mainardes, R.M.; Khalil, N.M.; Sarmento, B. Zein-Casein-Lysine Multicomposite Nanoparticles Are Effective in Modulate the Intestinal Permeability of Ferulic Acid. Int. J. Biol. Macromol. 2019, 138, 244–251. [Google Scholar] [CrossRef]
- Escamilla-García, M.; Calderón-Domínguez, G.; Chanona-Pérez, J.J.; Farrera-Rebollo, R.R.; Andraca-Adame, J.A.; Arzate-Vázquez, I.; Mendez-Mendez, J.V.; Moreno-Ruiz, L.A. Physical and Structural Characterisation of Zein and Chitosan Edible Films Using Nanotechnology Tools. Int. J. Biol. Macromol. 2013, 61, 196–203. [Google Scholar] [CrossRef]
- Corradini, E.; Curti, P.; Meniqueti, A.; Martins, A.; Rubira, A.; Muniz, E. Recent Advances in Food-Packing, Pharmaceutical and Biomedical Applications of Zein and Zein-Based Materials. Int. J. Mol. Sci. 2014, 15, 22438–22470. [Google Scholar] [CrossRef]
- Wang, Y.; Wusigale; Luo, Y. Colloidal Nanoparticles Prepared from Zein and Casein: Interactions, Characterizations and Emerging Food Applications. Food Sci. Hum. Wellness 2023, 12, 337–350. [Google Scholar] [CrossRef]
- Yu, X.; Afreen, S.; Kong, Q.; Wang, J. Study on Self-Assembled Morphology and Structure Regulation of α-Zein in Ethanol-Water Mixtures. Langmuir 2020, 36, 11975–11984. [Google Scholar] [CrossRef]
- Chen, S.; Guo, F.; Deng, T.; Zhu, S.; Liu, W.; Zhong, H.; Yu, H.; Luo, R.; Deng, Z. Eudragit S100-Coated Chitosan Nanoparticles Co-Loading Tat for Enhanced Oral Colon Absorption of Insulin. AAPS PharmSciTech 2017, 18, 1277–1287. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, O.; Shah, S.; Abbas, G.; Rasul, A.; Hanif, M.; Ashfaq, M.; Afzal, Z. Moxifloxacin Loaded Nanoparticles of Disulfide Bridged Thiolated Chitosan-Eudragit RS100 for Controlled Drug Delivery. Int. J. Biol. Macromol. 2021, 182, 2087–2096. [Google Scholar] [CrossRef]
- Farris, E.; Brown, D.M.; Ramer-Tait, A.E.; Pannier, A.K. Chitosan-Zein Nano-in-Microparticles Capable of Mediating in Vivo Transgene Expression Following Oral Delivery. J. Control. Release 2017, 249, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Hu, K.; Mcclements, D.J. Fabrication of Biopolymer Nanoparticles by Antisolvent Precipitation and Electrostatic Deposition: Zein-Alginate Core/Shell Nanoparticles. Food Hydrocoll. 2014, 44, 101–108. [Google Scholar] [CrossRef]
- Yuan, Y.; Li, H.; Zhu, J.; Liu, C.; Sun, X.; Wang, D.; Xu, Y. Fabrication and Characterization of Zein Nanoparticles by Dextran Sulfate Coating as Vehicles for Delivery of Curcumin. Int. J. Biol. Macromol. 2020, 151, 1074–1083. [Google Scholar] [CrossRef]
- Antonio, E.; dos Reis Antunes Junior, O.; Marcano, R.G.D.J.V.; Diedrich, C.; da Silva Santos, J.; Machado, C.S.; Khalil, N.M.; Mainardes, R.M. Chitosan Modified Poly (Lactic Acid) Nanoparticles Increased the Ursolic Acid Oral Bioavailability. Int. J. Biol. Macromol. 2021, 172, 133–142. [Google Scholar] [CrossRef]
- Ziebarth, J.; Diedrich, C.; Schineider Machado, C.; Mara Mainardes, R. Optimized LC-MS/MS Method for Quantifying Insulin Degludec and Liraglutide in Rat Plasma and Tissues: Application in Pharmacokinetics and Biodistribution. J. Chromatogr. B 2024, 1234, 124015. [Google Scholar] [CrossRef]
- Yuan, Y.; Li, H.; Liu, C.; Zhu, J.; Xu, Y.; Zhang, S.; Fan, M.; Zhang, D.; Zhang, Y.; Zhang, Z.; et al. Fabrication of Stable Zein Nanoparticles by Chondroitin Sulfate Deposition Based on Antisolvent Precipitation Method. Int. J. Biol. Macromol. 2019, 139, 30–39. [Google Scholar] [CrossRef]
- Huang, W.; Liu, S.; Li, Z.; Liu, Y.; Xie, Q.; Jiang, Y. Analysis of the Differences in Self-Assembly Behaviour, Molecular Structure and Drug Delivery Performance between α and β-Zein. Ind. Crops Prod. 2022, 181, 114822. [Google Scholar] [CrossRef]
- Sánchez-Juárez, C.; Reyes-Duarte, D.; Hernández-Guerrero, M.; Morales-Ibarría, M.; Campos-Terán, J.; Arroyo-Maya, I.J. α-Zein Nanoparticles as Delivery Systems for Hydrophobic Compounds: Effect of Assembly Parameters. Rev. Mex. Ing. Quim. 2020, 19, 793–801. [Google Scholar] [CrossRef]
- Bao, X.; Qian, K.; Xu, M.; Chen, Y.; Wang, H.; Pan, T.; Wang, Z.; Yao, P.; Lin, L. Intestinal Epithelium Penetration of Liraglutide via Cholic Acid Pre-Complexation and Zein/Rhamnolipids Nanocomposite Delivery. J. Nanobiotechnol. 2023, 21, 16. [Google Scholar] [CrossRef]
- Ji, N.; Hong, Y.; Gu, Z.; Cheng, L.; Li, Z.; Li, C. Preparation and Characterization of Insulin-Loaded Zein/Carboxymethylated Short-Chain Amylose Complex Nanoparticles. J. Agric. Food Chem. 2018, 66, 9335–9343. [Google Scholar] [CrossRef]
- Pauluk, D.; Padilha, A.K.; Khalil, N.M.; Mainardes, R.M. Chitosan-Coated Zein Nanoparticles for Oral Delivery of Resveratrol: Formation, Characterization, Stability, Mucoadhesive Properties and Antioxidant Activity. Food Hydrocoll. 2019, 94, 411–417. [Google Scholar] [CrossRef]
- Zhou, J.-F.; Zheng, G.-D.; Wang, W.-J.; Yin, Z.-P.; Chen, J.-G.; Li, J.-E.; Zhang, Q.-F. Physicochemical Properties and Bioavailability Comparison of Two Quercetin Loading Zein Nanoparticles with Outer Shell of Caseinate and Chitosan. Food Hydrocoll. 2021, 120, 106959. [Google Scholar] [CrossRef]
- Liang, X.; Cao, K.; Li, W.; Li, X.; McClements, D.J.; Hu, K. Tannic Acid-Fortified Zein-Pectin Nanoparticles: Stability, Properties, Antioxidant Activity, and in Vitro Digestion. Food Res. Int. 2021, 145, 110425. [Google Scholar] [CrossRef]
- De Souza, V.B.; Thomazini, M.; Echalar Barrientos, M.A.; Nalin, C.M.; Ferro-Furtado, R.; Genovese, M.I.; Favaro-Trindade, C.S. Functional Properties and Encapsulation of a Proanthocyanidin-Rich Cinnamon Extract (Cinnamomum zeylanicum) by Complex Coacervation Using Gelatin and Different Polysaccharides. Food Hydrocoll. 2018, 77, 297–306. [Google Scholar] [CrossRef]
- Donsì, F.; Voudouris, P.; Veen, S.J.; Velikov, K.P. Zein-Based Colloidal Particles for Encapsulation and Delivery of Epigallocatechin Gallate. Food Hydrocoll. 2017, 63, 508–517. [Google Scholar] [CrossRef]
- Bao, X.; Qian, K.; Yao, P. Oral Delivery of Exenatide-Loaded Hybrid Zein Nanoparticles for Stable Blood Glucose Control and β-Cell Repair of Type 2 Diabetes Mice. J. Nanobiotechnol. 2020, 18, 67. [Google Scholar] [CrossRef]
- Valderrama, A.N.; Jacinto, H.C.; Lay, J.; Flores, E.Y.; Zavaleta, C.D.; Delfín, A.R. Factorial Design for Preparing Chitosan Nanoparticles and Its Use for Loading and Controlled Release of Indole-3-Acetic Acid with Effect on Hydroponic Lettuce Crops. Biocatal. Agric. Biotechnol. 2020, 26, 101640. [Google Scholar] [CrossRef]
- Ghobadi-Oghaz, N.; Asoodeh, A.; Mohammadi, M. Fabrication, Characterization and in Vitro Cell Exposure Study of Zein-Chitosan Nanoparticles for Co-Delivery of Curcumin and Berberine. Int. J. Biol. Macromol. 2022, 204, 576–586. [Google Scholar] [CrossRef] [PubMed]
- Vale, E.P.; de Souza Tavares, W.; Hafidi, Z.; Pérez, L.; del Carmen Morán, M.; Martin-Pastor, M.; de Sousa, F.F.O. Epigallocatechin-3-Gallate Loaded-Zein Nanoparticles: Molecular Interaction, Antioxidant, Antienzimatic, Hemolytic and Cytotoxic Activities. J. Mol. Liq. 2024, 394, 123718. [Google Scholar] [CrossRef]
- Ziebarth, J.; Mainardes, R.M. Preparation, Characterization and in Vitro Evaluation of Chitosan Nanoparticles for the Oral Delivery of GLP-1 Analog Liraglutide. J. Therm. Anal. Calorim. 2023, 148, 2443–2455. [Google Scholar] [CrossRef]
- Öztürk, A.A.; Aygül, A.; Şenel, B. Influence of Glyceryl Behenate, Tripalmitin and Stearic Acid on the Properties of Clarithromycin Incorporated Solid Lipid Nanoparticles (SLNs): Formulation, Characterization, Antibacterial Activity and Cytotoxicity. J. Drug Deliv. Sci. Technol. 2019, 54, 101240. [Google Scholar] [CrossRef]
- Hassanzadeh, S.; Nematollahzadeh, A.; Mirzayi, B.; Fatemeh Kaboli, S. Protein-Based Nanoparticles Synthesized at a High Shear Rate and Optimized for Drug Delivery Applications. J. Mol. Liq. 2021, 335, 116133. [Google Scholar] [CrossRef]
- Shi, Y.; Yin, M.; Song, Y.; Wang, T.; Guo, S.; Zhang, X.; Sun, K.; Li, Y. Oral Delivery of Liraglutide-Loaded Poly-N-(2-Hydroxypropyl) Methacrylamide/Chitosan Nanoparticles: Preparation, Characterization, and Pharmacokinetics. J. Biomater. Appl. 2021, 35, 754–761. [Google Scholar] [CrossRef] [PubMed]
- Tong, M.-Q.; Luo, L.-Z.; Xue, P.-P.; Han, Y.-H.; Wang, L.-F.; Zhuge, D.-L.; Yao, Q.; Chen, B.; Zhao, Y.-Z.; Xu, H.-L. Glucose-Responsive Hydrogel Enhances the Preventive Effect of Insulin and Liraglutide on Diabetic Nephropathy of Rats. Acta Biomater. 2021, 122, 111–132. [Google Scholar] [CrossRef]
- Eissa, R.G.; Eissa, N.G.; Eissa, R.A.; Diab, N.H.; Abdelshafi, N.A.; Shaheen, M.A.; Elsabahy, M.; Hammad, S.K. Oral Proniosomal Amitriptyline and Liraglutide for Management of Diabetic Neuropathy: Exceptional Control over Hyperglycemia and Neuropathic Pain. Int. J. Pharm. 2023, 647, 123549. [Google Scholar] [CrossRef]
- Senduran, N.; Yadav, H.N.; Vishwakarma, V.K.; Bhatnagar, P.; Gupta, P.; Bhatia, J.; Dinda, A.K. Orally Deliverable Nanoformulation of Liraglutide against Type 2 Diabetic Rat Model. J. Drug Deliv. Sci. Technol. 2020, 56, 101513. [Google Scholar] [CrossRef]
- Hendarto, H.; Inoguchi, T.; Maeda, Y.; Ikeda, N.; Zheng, J.; Takei, R.; Yokomizo, H.; Hirata, E.; Sonoda, N.; Takayanagi, R. GLP-1 Analog Liraglutide Protects against Oxidative Stress and Albuminuria in Streptozotocin-Induced Diabetic Rats via Protein Kinase A-Mediated Inhibition of Renal NAD(P)H Oxidases. Metabolism 2012, 61, 1422–1434. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Nie, T.; Hu, Y.; Zhou, Y.; Zhu, J.; Liu, Z.; Liu, L.; Leong, K.W.; Chen, Y.; Mao, H.Q. A Polyphenol-Metal Nanoparticle Platform for Tunable Release of Liraglutide to Improve Blood Glycemic Control and Reduce Cardiovascular Complications in a Mouse Model of Type II Diabetes. J. Control. Release 2020, 318, 86–97. [Google Scholar] [CrossRef] [PubMed]
- Reboredo, C.; González-Navarro, C.J.; Martínez-López, A.L.; Irache, J.M. Oral Administration of Zein-Based Nanoparticles Reduces Glycemia and Improves Glucose Tolerance in Rats. Int. J. Pharm. 2022, 628, 122255. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.S.H.; Chang, L.W.; Yang, C.S.; Lin, P. Pharmacokinetics and Physiologically-Based Pharmacokinetic Modeling of Nanoparticles. J. Nanosci. Nanotechnol. 2010, 10, 8482–8490. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Chi, Y.; Burkhardt, B.R.; Guan, Y.; Wolf, B.A. Leucine Metabolism in Regulation of Insulin Secretion from Pancreatic Beta Cells. Nutr. Rev. 2010, 68, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Rubino, D.M.; Greenway, F.L.; Khalid, U.; O’Neil, P.M.; Rosenstock, J.; Sørrig, R.; Wadden, T.A.; Wizert, A.; Garvey, W.T.; Arauz-Pacheco, C.; et al. Effect of Weekly Subcutaneous Semaglutide vs Daily Liraglutide on Body Weight in Adults With Overweight or Obesity Without Diabetes. JAMA 2022, 327, 138. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, G.W.; Bocco, B.M.L.C. Hepatic Mediators of Lipid Metabolism and Ketogenesis: Focus on Fatty Liver and Diabetes. Curr. Diabetes Rev. 2021, 17, e110320187539. [Google Scholar] [CrossRef]
- Figueiredo, I.D.; Lima, T.F.O.; Inácio, M.D.; Costa, M.C.; Assis, R.P.; Brunetti, I.L.; Baviera, A.M. Lycopene Improves the Metformin Effects on Glycemic Control and Decreases Biomarkers of Glycoxidative Stress in Diabetic Rats. Diabetes Metab. Syndr. Obes. 2020, 13, 3117–3135. [Google Scholar] [CrossRef]
- Song, J.G.; Kim, D.H.; Han, H.K. Fabrication and Evaluation of a PH-Responsive Nanocomposite-Based Colonic Delivery System for Improving the Oral Efficacy of Liraglutide. Int. J. Nanomed. 2023, 18, 3937–3949. [Google Scholar] [CrossRef]
- Jakhar, D.K.; Vishwakarma, V.K.; Singh, R.; Jadhav, K.; Shah, S.; Arora, T.; Verma, R.K.; Yadav, H.N. Fat Fighting Liraglutide Based Nano-Formulation to Reverse Obesity: Design, Development and Animal Trials. Int. J. Pharm. 2023, 634, 122585. [Google Scholar] [CrossRef]
- Ladenheim, E. Liraglutide and Obesity: A Review of the Data so Far. Drug Des. Devel Ther. 2015, 9, 1867–1875. [Google Scholar] [CrossRef] [PubMed]
| Sample | Mean Size ± SD (nm) | PDI ± SD | Zeta Potential ± SD (mV) | EE% ± SD |
|---|---|---|---|---|
| Z-ERS-CS | 225.9 ± 11.7 a | 0.070 ± 0.015 a | +40.5 ± 2.6 a | - |
| Z-ERS-CS/LIRA | 238.6 ± 10.2 a | 0.099 ± 0.026 a | +40.9 ± 3.6 a | 41.1 ± 2.6 |
| Model | a | b | r | n |
|---|---|---|---|---|
| Zero order | 1.82 | 24.1 | 0.780 | |
| First order | 0.05 | 3.12 | 0.588 | |
| Second order | −0.002 | 0.048 | 0.392 | |
| Third order | −0.0001 | 0.003 | 0.261 | |
| Korsmeyer-Peppas | 0.394 | 2.991 | 0.935 | 0.394 |
| Higuchi | 0.500 | 2.853 | 0.593 | |
| Weibull | 0.487 | −1.497 | 0.961 | |
| Hickson-Crowell | 0.055 | 2.856 | 0.656 |
| Pharmacokinetic Parameters | Z-ERS-CS/LIRA Nps | Free LIRA |
|---|---|---|
| Cmax (ng/mL) | 113.82 ± 25.24 a | 109.49 ± 27.54 a |
| Tmax (h) | 4.0 a | 4.0 a |
| Kel (1/h) | 0.134 ± 0.039 a | 0.115 ± 0.019 a |
| Cl (L/h) | 0.284 ± 0.077 a | 0.183 ± 0.015 b |
| T1/2 (h) | 5.50 ± 1.38 a | 6.09 ± 0.96 a |
| AUC0–24h (ng.h/mL) | 692.86 ± 37.59 a | 977.79 ± 46.23 b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziebarth, J.; da Silva, L.M.; Lorenzett, A.K.P.; Figueiredo, I.D.; Carlstrom, P.F.; Cardoso, F.N.; de Freitas, A.L.F.; Baviera, A.M.; Mainardes, R.M. Oral Delivery of Liraglutide-Loaded Zein/Eudragit-Chitosan Nanoparticles Provides Pharmacokinetic and Glycemic Outcomes Comparable to Its Subcutaneous Injection in Rats. Pharmaceutics 2024, 16, 634. https://doi.org/10.3390/pharmaceutics16050634
Ziebarth J, da Silva LM, Lorenzett AKP, Figueiredo ID, Carlstrom PF, Cardoso FN, de Freitas ALF, Baviera AM, Mainardes RM. Oral Delivery of Liraglutide-Loaded Zein/Eudragit-Chitosan Nanoparticles Provides Pharmacokinetic and Glycemic Outcomes Comparable to Its Subcutaneous Injection in Rats. Pharmaceutics. 2024; 16(5):634. https://doi.org/10.3390/pharmaceutics16050634
Chicago/Turabian StyleZiebarth, Jeferson, Letícia Marina da Silva, Ariane Krause Padilha Lorenzett, Ingrid Delbone Figueiredo, Paulo Fernando Carlstrom, Felipe Nunes Cardoso, André Luiz Ferreira de Freitas, Amanda Martins Baviera, and Rubiana Mara Mainardes. 2024. "Oral Delivery of Liraglutide-Loaded Zein/Eudragit-Chitosan Nanoparticles Provides Pharmacokinetic and Glycemic Outcomes Comparable to Its Subcutaneous Injection in Rats" Pharmaceutics 16, no. 5: 634. https://doi.org/10.3390/pharmaceutics16050634
APA StyleZiebarth, J., da Silva, L. M., Lorenzett, A. K. P., Figueiredo, I. D., Carlstrom, P. F., Cardoso, F. N., de Freitas, A. L. F., Baviera, A. M., & Mainardes, R. M. (2024). Oral Delivery of Liraglutide-Loaded Zein/Eudragit-Chitosan Nanoparticles Provides Pharmacokinetic and Glycemic Outcomes Comparable to Its Subcutaneous Injection in Rats. Pharmaceutics, 16(5), 634. https://doi.org/10.3390/pharmaceutics16050634











