Insight into the Functional Dynamics and Challenges of Exosomes in Pharmaceutical Innovation and Precision Medicine
Abstract
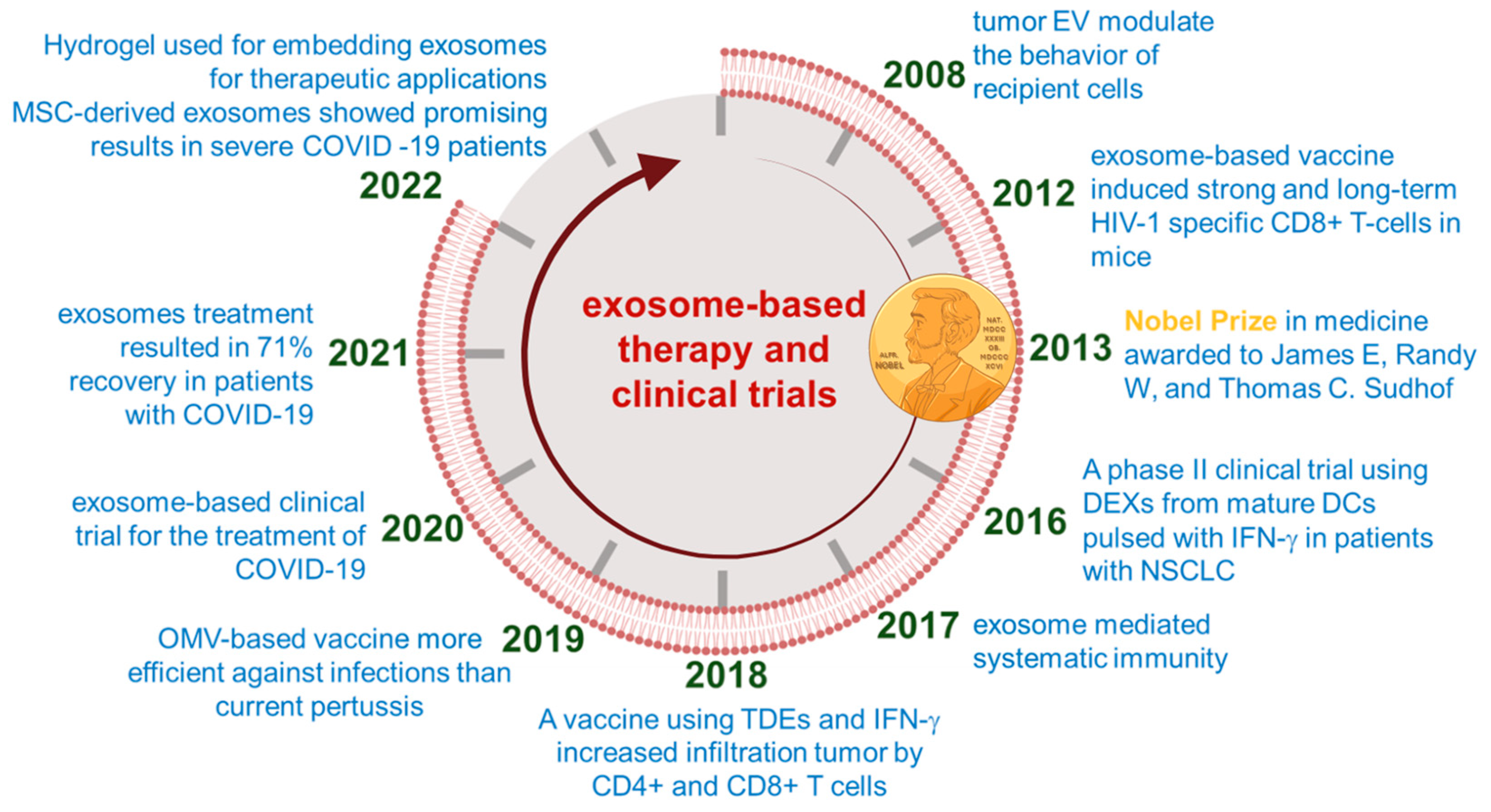
1. Introduction
2. Where Does the FDA Stand?
3. Challenges and Prospects Associated with the Translation of Exosome Therapy
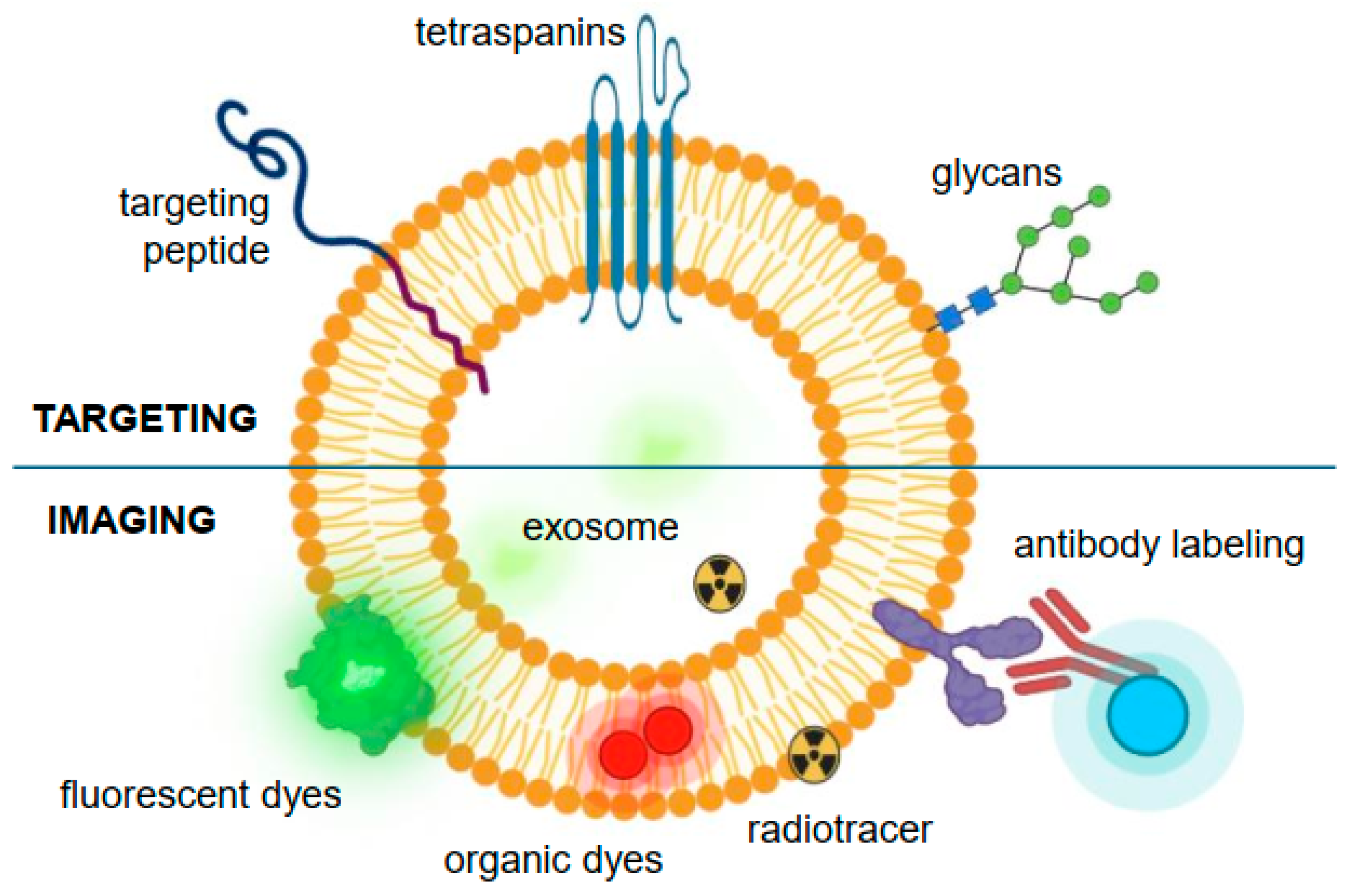
4. Factors Taken into Consideration for Exosomal Function Dictation
4.1. Protein Corona
| S. No. | Hard and Soft PC | Types of Interactions | Effect | References |
|---|---|---|---|---|
| 1. | Albumin | Connects to RNA/DNA on exosomes | Phagocytosis of exosomes | Malonga et al. 2006 [66] |
| 2. | ApoE and ApoB100 | Protein–protein interactions | Increases transfer rate in peripheral tissue | Bertrand et al. 2017 [67] |
| 3. | Apolipoprotein A1 | Interacts with CD63 on Exosome surface | Phagocytosis of exosomes | Toth et al. 2021 [60] |
| 4. | Apolipoprotein B | Interacts with CD63 on Exosome surface | Increases phagocytic activities and triggers secondary inflammation reactions | Toth et al. 2021 [60] |
| 5. | Complement factors 3 | Interacts with CD63 on Exosome surface | Increases phagocytic activities and triggers secondary inflammation reactions | Toth et al. 2021 [60] |
| 6. | Complement proteins C3b and C3ib | Protein–protein interactions | Prolonged chronic inflammatory conditions | Conde et al. 2012 [68] |
| 7. | Immunoglobulin heavy chains of (γ2 and γ4) | Protein–protein interactions | Reduces transit time and affects bio-distribution | Toth et al. 2021 [60] |
| 8. | Mismatched MHC-I and II | On the surface of Exosomes | T-cell immune responses | Hiltbrunner et al. 2016 [69] |
| 9. | S100-A8, LDL-receptor, CD14, HLA class I | Phosphatidylserine and tissue factor on Exosome surface | Dynamic activity | Buzas et al. 2018 [70] |
4.2. Interactions of Lipoproteins with Exosomes
4.3. Effects of Size, Morphology, and Surface Modification on Cellular Uptake of Exosomes
4.4. Cellular Environment
4.5. Entry and Departure of Exosomes from the Circulation
4.6. Functional Delivery of Exosomal Cargo
5. Current Attempts to Overcome Challenges Associated with the Therapeutic Application of Exosomes
5.1. Standardization of Research
5.2. Reporting Standards
5.3. Accurately Defining the Vesicles
5.4. Single-Exosome Studies
5.5. Exosome Storage
5.6. Modification of Exosomes for Specific Targeting
6. Bio-Engineered Exosome Therapy in Precision Medicine
7. Future Perspective and Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AFM | atomic force microscopy |
| BMP-2 | bone morphogenetic protein 2 |
| CMC | chemistry, manufacturing, and control |
| CNS | central nervous system |
| DNA | deoxyribonucleic acid |
| dSTORM | direct stochastic optical reconstruction microscopy |
| DCs | dendritic cells |
| DLS | dynamic light scattering |
| ED | effector domain |
| EM | electron microscopy |
| ELISA | enzyme-linked immunosorbent assay |
| ECM | extracellular matrix |
| EV | extracellular vesicle |
| FCM | flow cytometry |
| FDA | food and drug administration |
| GMP | good manufacturing practice |
| HDL | high density lipoproteins |
| HIF-1α | hypoxia-inducible factor 1-alpha |
| IFN-γ | interferon-gamma |
| ISEV | international society for extracellular vesicles |
| IND | investigational new drug |
| IDL | intermediate-density lipoproteins |
| LDL | low density lipoproteins |
| LPS | lipopolysaccharide |
| miRNA | microRNA |
| MISEV | minimal information for studies of extracellular vesicles |
| MARCKS | myristoylated alanine-rich C kinase substrate |
| NTA | nanoparticle tracking analysis |
| nFCM | nano-flow cytometry |
| PCR | polymerase chain reaction |
| PBS-HAT | phosphate buffered saline-human albumin and trehalose |
| PS | phosphatidylserine |
| Phe | phenylalanine |
| qPCR | quantitative polymerase chain reaction |
| RNA | ribonucleic acid |
| RVG | rabies viral glycoprotein |
| SEM | scanning electron microscopy |
| TNF-α | tumor necrosis factor-alpha |
| TEM | transmission electron microscopy |
| TRPS | tunable resistive pulse sensing |
| TIRF | total internal reflection fluorescence |
| TA | tannic acid |
| UV | ultraviolet light |
| VLDL | very low-density lipoproteins |
References
- Li, X.; Corbett, A.L.; Taatizadeh, E.; Tasnim, N.; Little, J.P.; Garnis, C.; Daugaard, M.; Guns, E.; Hoorfar, M.; Li, I.T.S. Challenges and opportunities in exosome research-Perspectives from biology, engineering, and cancer therapy. APL Bioeng. 2019, 3, 011503. [Google Scholar] [CrossRef] [PubMed]
- Zou, Z.; Li, H.; Xu, G.; Hu, Y.; Zhang, W.; Tian, K. Current Knowledge and Future Perspectives of Exosomes as Nanocarriers in Diagnosis and Treatment of Diseases. Int. J. Nanomed. 2023, 18, 4751–4778. [Google Scholar] [CrossRef] [PubMed]
- Rajput, A.; Varshney, A.; Bajaj, R.; Pokharkar, V. Exosomes as New Generation Vehicles for Drug Delivery: Biomedical Applications and Future Perspectives. Molecules 2022, 27, 7289. [Google Scholar] [CrossRef] [PubMed]
- Butreddy, A.; Kommineni, N.; Dudhipala, N. Exosomes as Naturally Occurring Vehicles for Delivery of Biopharmaceuticals: Insights from Drug Delivery to Clinical Perspectives. Nanomaterials 2021, 11, 1481. [Google Scholar] [CrossRef]
- Herrmann, I.K.; Wood, M.J.A.; Fuhrmann, G. Extracellular vesicles as a next-generation drug delivery platform. Nat. Nanotechnol. 2021, 16, 748–759. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Yang, Y.; Chen, Y.; Xu, Y.; Peng, J. Cell-based drug delivery systems and their in vivo fate. Adv. Drug Deliv. Rev. 2022, 187, 114394. [Google Scholar] [CrossRef] [PubMed]
- Rezaie, J.; Feghhi, M.; Etemadi, T. A review on exosomes application in clinical trials: Perspective, questions, and challenges. Cell Commun. Signal. 2022, 20, 145. [Google Scholar] [CrossRef] [PubMed]
- Koh, H.; Kim, H.; Kang, S.; Yoo, T.-H. Exosome-Based Drug Delivery: Translation from Bench to Clinic. Pharmaceutics 2023, 15, 2042. [Google Scholar] [CrossRef] [PubMed]
- Sousa, P.; Lopes, B.; Sousa, A.C.; Moreira, A.; Coelho, A.; Alvites, R.; Alves, N.; Geuna, S.; Maurício, A.C. Advancements and Insights in Exosome-Based Therapies for Wound Healing: A Comprehensive Systematic Review (2018-June 2023). Biomedicines 2023, 11, 2099. [Google Scholar] [CrossRef]
- Gao, J.; Li, A.; Hu, J.; Feng, L.; Liu, L.; Shen, Z. Recent developments in isolating methods for exosomes. Front. Bioeng. Biotechnol. 2022, 10, 1100892. [Google Scholar] [CrossRef]
- Kwon, Y.; Park, J. Methods to analyze extracellular vesicles at single particle level. Micro Nano Syst. Lett. 2022, 10, 14. [Google Scholar] [CrossRef]
- Song, Y.; Kim, Y.; Ha, S.; Sheller-Miller, S.; Yoo, J.; Choi, C.; Park, C.H. The emerging role of exosomes as novel therapeutics: Biology, technologies, clinical applications, and the next. Am. J. Reprod. Immunol. 2021, 85, e13329. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Xia, J.; Yang, L.; Dai, J.; He, L. Recent progress in exosome research: Isolation, characterization and clinical applications. Cancer Gene Ther. 2023, 30, 1051–1065. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Sun, X.; Liu, L.; Jiang, H.; Shen, Y.; Xu, X.; Li, J.; Zhang, G.; Huang, J.; Lin, Z.; et al. Exosomes and Their Therapeutic Potentials of Stem Cells. Stem Cells Int. 2016, 2016, 7653489. [Google Scholar] [CrossRef] [PubMed]
- Hong, P.; Yang, H.; Wu, Y.; Li, K.; Tang, Z. The functions and clinical application potential of exosomes derived from adipose mesenchymal stem cells: A comprehensive review. Stem Cell Res. Ther. 2019, 10, 242. [Google Scholar] [CrossRef] [PubMed]
- Tan, F.; Li, X.; Wang, Z.; Li, J.; Shahzad, K.; Zheng, J. Clinical applications of stem cell-derived exosomes. Signal Transduct. Target. Ther. 2024, 9, 17. [Google Scholar] [CrossRef]
- Asadpour, A.; Yahaya, B.H.; Bicknell, K.; Cottrell, G.S.; Widera, D. Uncovering the gray zone: Mapping the global landscape of direct-to-consumer businesses offering interventions based on secretomes, extracellular vesicles, and exosomes. Stem Cell Res. Ther. 2023, 14, 111. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.Q.; Akhtar, S.; Prabhu, K.S.; Zarif, L.; Khan, R.; Alam, M.; Buddenkotte, J.; Ahmad, A.; Steinhoff, M.; Uddin, S. Exosomes: Emerging Diagnostic and Therapeutic Targets in Cutaneous Diseases. Int. J. Mol. Sci. 2020, 21, 9264. [Google Scholar] [CrossRef] [PubMed]
- Colao, I.L.; Corteling, R.; Bracewell, D.; Wall, I. Manufacturing Exosomes: A Promising Therapeutic Platform. Trends Mol. Med. 2018, 24, 242–256. [Google Scholar] [CrossRef]
- Li, M.; Fang, F.; Sun, M.; Zhang, Y.; Hu, M.; Zhang, J. Extracellular vesicles as bioactive nanotherapeutics: An emerging paradigm for regenerative medicine. Theranostics 2022, 12, 4879–4903. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, X.; Xu, W.; Li, Y.; Lai, R.; Qiu, X.; Chen, X.; Chen, Z.; Mi, B.; Wu, M.; et al. Translational Challenges and Prospective Solutions in the Implementation of Biomimetic Delivery Systems. Pharmaceutics 2023, 15, 2623. [Google Scholar] [CrossRef] [PubMed]
- FDA. Public Safety Notification on Exosome Products. 2019. Available online: https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/public-safety-notification-exosome-products (accessed on 20 April 2024).
- FDA. Consumer Alert on Regenerative Medicine Products Including Stem Cells and Exosomes. 2020. Available online: https://www.fda.gov/vaccines-blood-biologics/consumers-biologics/consumer-alert-regenerative-medicine-products-including-stem-cells-and-exosomes (accessed on 20 April 2024).
- Ahn, S.H.; Ryu, S.W.; Choi, H.; You, S.; Park, J.; Choi, C. Manufacturing Therapeutic Exosomes: From Bench to Industry. Mol. Cells 2022, 45, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.C.; Kim, J.W.; Pauletti, G.M.; Hassett, D.J.; Kotagiri, N. Exosomes: Biological Pharmaceutical Nanovectors for Theranostics. Front. Bioeng. Biotechnol. 2021, 9, 808614. [Google Scholar] [CrossRef] [PubMed]
- Hussen, B.M.; Faraj, G.S.H.; Rasul, M.F.; Hidayat, H.J.; Salihi, A.; Baniahmad, A.; Taheri, M.; Ghafouri-Frad, S. Strategies to overcome the main challenges of the use of exosomes as drug carrier for cancer therapy. Cancer Cell Int. 2022, 22, 323. [Google Scholar] [CrossRef] [PubMed]
- Vyas, K.S.; Kaufman, J.; Munavalli, G.S.; Robertson, K.; Behfar, A.; Wyles, S.P. Exosomes: The latest in regenerative aesthetics. Regen. Med. 2023, 18, 181–194. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-S.; Lin, E.-Y.; Chiou, T.-W.; Harn, H.-J. Exosomes in clinical trial and their production in compliance with good manufacturing practice. Tzu Chi Med. J. 2020, 32, 113–120. [Google Scholar] [CrossRef]
- Syromiatnikova, V.; Prokopeva, A.; Gomzikova, M. Methods of the Large-Scale Production of Extracellular Vesicles. Int. J. Mol. Sci. 2022, 23, 10522. [Google Scholar] [CrossRef] [PubMed]
- Qu, Q.; Fu, B.; Long, Y.; Liu, Z.Y.; Tian, X.H. Current Strategies for Promoting the Large-scale Production of Exosomes. Curr. Neuropharmacol. 2023, 21, 1964–1979. [Google Scholar] [CrossRef]
- Huang, G.; Lin, G.; Zhu, Y.; Duan, W.; Jin, D. Emerging technologies for profiling extracellular vesicle heterogeneity. Lab Chip 2020, 20, 2423–2437. [Google Scholar] [CrossRef]
- Yang, B.; Lin, Y.; Huang, Y.; Zhu, N.; Shen, Y.-Q. Extracellular vesicles modulate key signalling pathways in refractory wound healing. Burns Trauma 2023, 11, tkad039. [Google Scholar] [CrossRef]
- Willms, E.; Cabañas, C.; Mäger, I.; Wood, M.J.A.; Vader, P. Extracellular Vesicle Heterogeneity: Subpopulations, Isolation Techniques, and Diverse Functions in Cancer Progression. Front. Immunol. 2018, 9, 738. [Google Scholar] [CrossRef] [PubMed]
- Meggiolaro, A.; Moccia, V.; Brun, P.; Pierno, M.; Mistura, G.; Zappulli, V.; Ferraro, D. Microfluidic Strategies for Extracellular Vesicle Isolation: Towards Clinical Applications. Biosensors 2022, 13, 50. [Google Scholar] [CrossRef] [PubMed]
- Konoshenko, M.Y.; Lekchnov, E.A.; Vlassov, A.V.; Laktionov, P.P. Isolation of Extracellular Vesicles: General Methodologies and Latest Trends. Biomed. Res. Int. 2018, 2018, 8545347. [Google Scholar] [CrossRef] [PubMed]
- Coughlan, C.; Bruce, K.D.; Burgy, O.; Boyd, T.D.; Michel, C.R.; Garcia-Perez, J.E.; Adame, V.; Anton, P.; Bettcher, B.M.; Chial, H.J.; et al. Exosome Isolation by Ultracentrifugation and Precipitation and Techniques for Downstream Analyses. Curr. Protoc. Cell Biol. 2020, 88, e110. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Li, P.; Zhang, T.; Xu, Z.; Huang, X.; Wang, R.; Du, L. Review on Strategies and Technologies for Exosome Isolation and Purification. Front. Bioeng. Biotechnol. 2022, 9, 811971. [Google Scholar] [CrossRef]
- Sidhom, K.; Obi, P.O.; Saleem, A. A Review of Exosomal Isolation Methods: Is Size Exclusion Chromatography the Best Option? Int. J. Mol. Sci. 2020, 21, 6466. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Zhang, W.; Zhang, H.; Zhang, F.; Chen, L.; Ma, L.; Larcher, L.M.; Chen, S.; Liu, N.; Zhao, Q.; et al. Progress, opportunity, and perspective on exosome isolation—Efforts for efficient exosome-based theranostics. Theranostics 2020, 10, 3684–3707. [Google Scholar] [CrossRef] [PubMed]
- Liangsupree, T.; Multia, E.; Riekkola, M.-L. Modern isolation and separation techniques for extracellular vesicles. J. Chromatogr. A 2021, 1636, 461773. [Google Scholar] [CrossRef]
- Gholizadeh, S.; Shehata Draz, M.; Zarghooni, M.; Sanati-Nezhad, A.; Ghavami, S.; Shafiee, H.; Akbari, M. Microfluidic approaches for isolation, detection, and characterization of extracellular vesicles: Current status and future directions. Biosens. Bioelectron. 2017, 91, 588–605. [Google Scholar] [CrossRef]
- Zhou, X.; Brown, B.A.; Siegel, A.P.; El Masry, M.S.; Zeng, X.; Song, W.; Das, A.; Khandelwal, P.; Clark, A.; Singh, K.; et al. Exosome-Mediated Crosstalk between Keratinocytes and Macrophages in Cutaneous Wound Healing. ACS Nano 2020, 14, 12732–12748. [Google Scholar] [CrossRef]
- Guda, P.R.; Sharma, A.; Anthony, A.J.; El Masry, M.S.; Couse, A.D.; Ghatak, P.D.; Das, A.; Timsina, L.; Trinidad, J.C.; Roy, S.; et al. Nanoscopic and functional characterization of keratinocyte-originating exosomes in the wound fluid of non-diabetic and diabetic chronic wound patients. Nano Today 2023, 52, 101954. [Google Scholar] [CrossRef] [PubMed]
- Clayton, A.; Boilard, E.; Buzas, E.I.; Cheng, L.; Falcón-Perez, J.M.; Gardiner, C.; Gustafson, D.; Gualerzi, A.; Hendrix, A.; Hoffman, A.; et al. Considerations towards a roadmap for collection, handling and storage of blood extracellular vesicles. J. Extracell. Vesicles 2019, 8, 1647027. [Google Scholar] [CrossRef] [PubMed]
- Venturella, M.; Carpi, F.M.; Zocco, D. Standardization of Blood Collection and Processing for the Diagnostic Use of Extracellular Vesicles. Curr. Pathobiol. Rep. 2019, 7, 1–8. [Google Scholar] [CrossRef]
- Coumans, F.A.W.; Brisson, A.R.; Buzas, E.I.; Dignat-George, F.; Drees, E.E.E.; El-Andaloussi, S.; Emanueli, C.; Gasecka, A.; Hendrix, A.; Hill, A.F.; et al. Methodological Guidelines to Study Extracellular Vesicles. Circ. Res. 2017, 120, 1632–1648. [Google Scholar] [CrossRef] [PubMed]
- Lacroix, R.; Judicone, C.; Poncelet, P.; Robert, S.; Arnaud, L.; Sampol, J.; Dignat-George, F. Impact of pre-analytical parameters on the measurement of circulating microparticles: Towards standardization of protocol. J. Thromb. Haemost. 2012, 10, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Buntsma, N.C.; Gąsecka, A.; Roos, Y.; van Leeuwen, T.G.; van der Pol, E.; Nieuwland, R. EDTA stabilizes the concentration of platelet-derived extracellular vesicles during blood collection and handling. Platelets 2022, 33, 764–771. [Google Scholar] [CrossRef] [PubMed]
- Lacroix, R.; Judicone, C.; Mooberry, M.; Boucekine, M.; Key, N.S.; Dignat-George, F. Standardization of pre-analytical variables in plasma microparticle determination: Results of the International Society on Thrombosis and Haemostasis SSC Collaborative workshop. J. Thromb. Haemost. 2013, 11, 1190–1193. [Google Scholar] [CrossRef] [PubMed]
- Holcar, M.; Kandušer, M.; Lenassi, M. Blood Nanoparticles—Influence on Extracellular Vesicle Isolation and Characterization. Front. Pharmacol. 2021, 12, 773844. [Google Scholar] [CrossRef] [PubMed]
- Vila-Liante, V.; Sánchez-López, V.; Martínez-Sales, V.; Ramón-Nuñez, L.A.; Arellano-Orden, E.; Cano-Ruiz, A.; Rodríguez-Martorell, F.J.; Gao, L.; Otero-Candelera, R. Impact of sample processing on the measurement of circulating microparticles: Storage and centrifugation parameters. Clin. Chem. Lab. Med. 2016, 54, 1759–1767. [Google Scholar]
- Aguilera-Rojas, M.; Sharbati, S.; Stein, T.; Candela Andrade, M.; Kohn, B.; Einspanier, R. Systematic analysis of different degrees of haemolysis on miRNA levels in serum and serum-derived extracellular vesicles from dogs. BMC Vet. Res. 2022, 18, 355. [Google Scholar] [CrossRef]
- Gurunathan, S.; Kang, M.H.; Jeyaraj, M.; Qasim, M.; Kim, J.H. Review of the Isolation, Characterization, Biological Function, and Multifarious Therapeutic Approaches of Exosomes. Cells 2019, 8, 307. [Google Scholar] [CrossRef] [PubMed]
- Mulcahy, L.A.; Pink, R.C.; Carter, D.R. Routes and mechanisms of extracellular vesicle uptake. J. Extracell. Vesicles 2014, 3, 24641. [Google Scholar] [CrossRef] [PubMed]
- Klyachko, N.L.; Arzt, C.J.; Li, S.M.; Gololobova, O.A.; Batrakova, E.V. Extracellular Vesicle-Based Therapeutics: Preclinical and Clinical Investigations. Pharmaceutics 2020, 12, 1171. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, K.; Ughetto, S.; Mahjoum, S.; Nair, A.V.; Breakefield, X.O. Uptake, functionality, and re-release of extracellular vesicle-encapsulated cargo. Cell Rep. 2022, 39, 110651. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, M.; Martin-Jaular, L.; Lavieu, G.; Théry, C. Specificities of secretion and uptake of exosomes and other extracellular vesicles for cell-to-cell communication. Nat. Cell Biol. 2019, 21, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Heidarzadeh, M.; Zarebkohan, A.; Rahbarghazi, R.; Sokullu, E. Protein corona and exosomes: New challenges and prospects. Cell Commun. Signal. 2023, 21, 64. [Google Scholar] [CrossRef]
- Capolla, S.; Colombo, F.; De Maso, L.; Mauro, P.; Bertoncin, P.; Kähne, T.; Engler, A.; Núñez, L.; Spretz, R.; Larsen, G.; et al. Surface antibody changes protein corona both in human and mouse serum but not final opsonization and elimination of targeted polymeric nanoparticles. J. Nanobiotechnol. 2023, 21, 376. [Google Scholar] [CrossRef] [PubMed]
- Tóth, E.; Turiák, L.; Visnovitz, T.; Cserép, C.; Mázló, A.; Sódar, B.W.; Försönits, A.I.; Petővári, G.; Sebestyén, A.; Komlósi, Z.; et al. Formation of a protein corona on the surface of extracellular vesicles in blood plasma. J. Extracell. Vesicles 2021, 10, e12140. [Google Scholar] [CrossRef]
- Wolfram, J.; Yang, Y.; Shen, J.; Moten, A.; Chen, C.; Shen, H.; Ferrari, M.; Zhao, Y. The nano-plasma interface: Implications of the protein corona. Colloids Surf B Biointerfaces 2014, 124, 17–24. [Google Scholar] [CrossRef]
- Ghebosu, R.E.; Pendiuk Goncalves, J.; Wolfram, J. Extracellular Vesicle and Lipoprotein Interactions. Nano Lett. 2024, 24, 1–8. [Google Scholar] [CrossRef]
- Nguyen, V.H.; Lee, B.J. Protein corona: A new approach for nanomedicine design. Int. J. Nanomed. 2017, 12, 3137–3151. [Google Scholar] [CrossRef] [PubMed]
- Tenzer, S.; Docter, D.; Rosfa, S.; Wlodarski, A.; Kuharev, J.; Rekik, A.; Knauer, S.K.; Bantz, C.; Nawroth, T.; Bier, C.; et al. Nanoparticle size is a critical physicochemical determinant of the human blood plasma corona: A comprehensive quantitative proteomic analysis. ACS Nano 2011, 5, 7155–7167. [Google Scholar] [CrossRef] [PubMed]
- Shang, L.; Wang, Y.; Jiang, J.; Dong, S. pH-dependent protein conformational changes in albumin:gold nanoparticle bioconjugates: A spectroscopic study. Langmuir 2007, 23, 2714–2721. [Google Scholar] [CrossRef] [PubMed]
- Malonga, H.; Neault, J.F.; Tajmir-Riahi, H.A. Transfer RNA binding to human serum albumin: A model for protein-RNA interaction. DNA and Cell Biol. 2006, 25, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, N.; Grenier, P.; Mahmoudi, M.; Lima, E.M.; Appel, E.A.; Dormont, F.; Lim, J.M.; Karnik, R.; Langer, R.; Farokhzad, O.C. Mechanistic understanding of in vivo protein corona formation on polymeric nanoparticles and impact on pharmacokinetics. Nat Commun. 2017, 8, 777. [Google Scholar] [CrossRef]
- Carrillo-Conde, B.R.; Ramer-Tait, A.E.; Wannemuehler, M.J.; Narasimhan, B. Chemistry-dependent adsorption of serum proteins onto polyanhydride microparticles diferentially influences dendritic cell uptake and activation. Acta Biomater 2012, 8, 3618–3628. [Google Scholar] [CrossRef]
- Hiltbrunner, S.; Larssen, P.; Eldh, M.; Martinez-Bravo, M.-J.; Wagner, A.K.; Karlsson, M.C.; Gabrielsson, S. Exosomal cancer immunotherapy is independent of MHC molecules on exosomes. Oncotarget 2016, 7, 387. [Google Scholar] [CrossRef] [PubMed]
- Buzás, E.I.; Tóth, E.Á.; Sódar, B.W.; Szabó-Taylor, K.É. Molecular interactions at the surface of extracellular vesicles. Semin Immunopathol 2018, 40, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Dietz, L.; Oberländer, J.; Mateos-Maroto, A.; Schunke, J.; Fichter, M.; Krämer-Albers, E.M.; Landfester, K.; Mailänder, V. Uptake of extracellular vesicles into immune cells is enhanced by the protein corona. J. Extracell. Vesicles 2023, 12, e12399. [Google Scholar] [CrossRef]
- Botha, J.; Handberg, A.; Simonsen, J.B. Lipid-based strategies used to identify extracellular vesicles in flow cytometry can be confounded by lipoproteins: Evaluations of annexin V, lactadherin, and detergent lysis. J. Extracell. Vesicles 2022, 11, e12200. [Google Scholar] [CrossRef]
- Busatto, S.; Walker, S.A.; Grayson, W.; Pham, A.; Tian, M.; Nesto, N.; Barklund, J.; Wolfram, J. Lipoprotein-based drug delivery. Adv. Drug Deliv. Rev. 2020, 159, 377–390. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Chen, C.; Wang, Z.; Bachman, H.; Ouyang, Y.; Huang, P.H.; Sadovsky, Y.; Huang, T.J. Separating extracellular vesicles and lipoproteins via acoustofluidics. Lab Chip 2019, 19, 1174–1182. [Google Scholar] [CrossRef] [PubMed]
- Karimi, N.; Cvjetkovic, A.; Jang, S.C.; Crescitelli, R.; Feizi, M.; Nieuwland, R.; Lotvall, J.; Lässer, C. Detailed analysis of the plasma extracellular vesicle proteome after separation from lipoproteins. Cell. Mol. Life Sci. 2018, 75, 2873–2886. [Google Scholar] [CrossRef]
- Mo, Z.-C.; Ren, K.; Liu, X.; Tang, Z.-L.; Yi, G.-H. A high-density lipoprotein-mediated drug delivery system. Adv. Drug Deliv. Rev. 2016, 106, 132–147. [Google Scholar] [CrossRef] [PubMed]
- Park, H.J.; Kuai, R.; Jeon, E.J.; Seo, Y.; Jung, Y.; Moon, J.J.; Schwendeman, A.; Cho, S.W. High-density lipoprotein-mimicking nanodiscs carrying peptide for enhanced therapeutic angiogenesis in diabetic hindlimb ischemia. Biomaterials 2018, 161, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Lozano-Andrés, E.; Enciso-Martinez, A.; Gijsbers, A.; Ridolfi, A.; Van Niel, G.; Libregts, S.; Pinheiro, C.; van Herwijnen, M.J.C.; Hendrix, A.; Brucale, M.; et al. Physical association of low density lipoprotein particles and extracellular vesicles unveiled by single particle analysis. J. Extracell. Vesicles 2023, 12, e12376. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, P.; Le, A.; Pek, J.; Pham, T.; Jayasinghe, M.; Do, D.; Cao Dai, P.; Le, M. Extracellular vesicles and lipoproteins—Smart messengers of blood cells in the circulation. J. Extracell. Biol. 2022, 1, e49. [Google Scholar] [CrossRef]
- Ridolfi, A.; Conti, L.; Brucale, M.; Frigerio, R.; Cardellini, J.; Musicò, A.; Romano, M.; Zendrini, A.; Polito, L.; Bergamaschi, G.; et al. Particle profiling of EV-lipoprotein mixtures by AFM nanomechanical imaging. J. Extracell. Vesicles 2023, 12, e12349. [Google Scholar] [CrossRef] [PubMed]
- Donoso-Quezada, J.; Ayala-Mar, S.; González-Valdez, J. The role of lipids in exosome biology and intercellular communication: Function, analytics and applications. Traffic 2021, 22, 204–220. [Google Scholar] [CrossRef]
- Salatin, S.; Maleki Dizaj, S.; Yari Khosroushahi, A. Effect of the surface modification, size, and shape on cellular uptake of nanoparticles. Cell Biol. Int. 2015, 39, 881–890. [Google Scholar] [CrossRef]
- Caponnetto, F.; Manini, I.; Skrap, M.; Palmai-Pallag, T.; Di Loreto, C.; Beltrami, A.P.; Cesselli, D.; Ferrari, E. Size-dependent cellular uptake of exosomes. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 1011–1020. [Google Scholar] [CrossRef] [PubMed]
- Gurung, S.; Perocheau, D.; Touramanidou, L.; Baruteau, J. The exosome journey: From biogenesis to uptake and intracellular signalling. Cell Commun. Signal. 2021, 19, 47. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.I.; Park, J.; Zhu, Y.; Wang, X.; Han, Y.; Zhang, D. Recent advances in extracellular vesicles for therapeutic cargo delivery. Exp. Mol. Med. 2024, 56, 836–849. [Google Scholar] [CrossRef] [PubMed]
- van der Pol, E.; Coumans, F.A.; Grootemaat, A.E.; Gardiner, C.; Sargent, I.L.; Harrison, P.; Sturk, A.; van Leeuwen, T.G.; Nieuwland, R. Particle size distribution of exosomes and microvesicles determined by transmission electron microscopy, flow cytometry, nanoparticle tracking analysis, and resistive pulse sensing. J. Thromb. Haemost. 2014, 12, 1182–1192. [Google Scholar] [CrossRef] [PubMed]
- Gong, J.; Wang, H.X.; Leong, K.W. Determination of Cellular Uptake and Endocytic Pathways. Bio-protocol 2019, 9, e3169. [Google Scholar] [CrossRef] [PubMed]
- Di Bella, M.A. Overview and Update on Extracellular Vesicles: Considerations on Exosomes and Their Application in Modern Medicine. Biology 2022, 11, 804. [Google Scholar] [CrossRef] [PubMed]
- Raposo, G.; Stoorvogel, W. Extracellular vesicles: Exosomes, microvesicles, and friends. J. Cell Biol. 2013, 200, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Karmacharya, M.; Kumar, S.; Cho, Y.K. Tuning the Extracellular Vesicles Membrane through Fusion for Biomedical Applications. J. Funct. Biomater. 2023, 14, 117. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Wang, L.; Zeng, X.; Schwarz, H.; Nanda, H.S.; Peng, X.; Zhou, Y. Exosomes, a New Star for Targeted Delivery. Front. Cell Dev. Biol. 2021, 9, 751079. [Google Scholar] [CrossRef]
- Salunkhe, S.; Dheeraj; Basak, M.; Chitkara, D.; Mittal, A. Surface functionalization of exosomes for target-specific delivery and in vivo imaging & tracking: Strategies and significance. J. Control Release 2020, 326, 599–614. [Google Scholar]
- Tian, T.; Zhang, H.X.; He, C.P.; Fan, S.; Zhu, Y.L.; Qi, C.; Huang, N.P.; Xiao, Z.D.; Lu, Z.H.; Tannous, B.A.; et al. Surface functionalized exosomes as targeted drug delivery vehicles for cerebral ischemia therapy. Biomaterials 2018, 150, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Xu, X.; Li, X.; Xiong, J.; Li, B.; Duan, L.; Wang, D.; Xia, J. Chondrocyte-Targeted MicroRNA Delivery by Engineered Exosomes toward a Cell-Free Osteoarthritis Therapy. ACS Appl. Mater. Interfaces 2020, 12, 36938–36947. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Hu, W.; Huang, Q.; Yang, J.; Li, B.; Ma, K.; Wei, Q.; Wang, Y.; Su, J.; Sun, M.; et al. MiR146a-loaded engineered exosomes released from silk fibroin patch promote diabetic wound healing by targeting IRAK1. Signal Transduct. Target. Ther. 2023, 8, 62. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Song, D.; Meng, C.; Cheng, Y.; Wang, B.; Yang, Z. Opportunities and challenges of engineered exosomes for diabetic wound healing. Giant 2024, 18, 100251. [Google Scholar] [CrossRef]
- Gartz, M.; Strande, J.L. Examining the Paracrine Effects of Exosomes in Cardiovascular Disease and Repair. J. Am. Heart Assoc. 2018, 7, e007954. [Google Scholar] [CrossRef]
- Yue, B. Biology of the extracellular matrix: An overview. J. Glaucoma 2014, 23 (Suppl. 1), S20–S23. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Liu, D.A.; Guan, L.; Myint, P.K.; Chin, L.; Dang, H.; Xu, Y.; Ren, J.; Li, T.; Yu, Z.; et al. Stiff matrix induces exosome secretion to promote tumour growth. Nat. Cell Biol. 2023, 25, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Logozzi, M.; Mizzoni, D.; Angelini, D.F.; Di Raimo, R.; Falchi, M.; Battistini, L.; Fais, S. Microenvironmental pH and Exosome Levels Interplay in Human Cancer Cell Lines of Different Histotypes. Cancers 2018, 10, 370. [Google Scholar] [CrossRef] [PubMed]
- Palomar-Alonso, N.; Lee, M.; Kim, M. Exosomes: Membrane-associated proteins, challenges and perspectives. Biochem. Biophys. Rep. 2024, 37, 101599. [Google Scholar] [CrossRef]
- Nakase, I.; Ueno, N.; Matsuzawa, M.; Noguchi, K.; Hirano, M.; Omura, M.; Takenaka, T.; Sugiyama, A.; Bailey Kobayashi, N.; Hashimoto, T.; et al. Environmental pH stress influences cellular secretion and uptake of extracellular vesicles. FEBS Open Bio. 2021, 11, 753–767. [Google Scholar] [CrossRef]
- Mahmood, A.; Otruba, Z.; Weisgerber, A.W.; Palay, M.D.; Nguyen, M.T.; Bills, B.L.; Knowles, M.K. Exosome secretion kinetics are controlled by temperature. Biophys. J. 2023, 122, 1301–1314. [Google Scholar] [CrossRef]
- Wang, Y.; Xiao, T.; Zhao, C.; Li, G. The Regulation of Exosome Generation and Function in Physiological and Pathological Processes. Int. J. Mol. Sci. 2023, 25, 255. [Google Scholar] [CrossRef]
- Whiteside, T.L. Tumor-Derived Exosomes and Their Role in Cancer Progression. Adv. Clin. Chem. 2016, 74, 103–141. [Google Scholar] [PubMed]
- Chiaradia, E.; Tancini, B.; Emiliani, C.; Delo, F.; Pellegrino, R.M.; Tognoloni, A.; Urbanelli, L.; Buratta, S. Extracellular Vesicles under Oxidative Stress Conditions: Biological Properties and Physiological Roles. Cells 2021, 10, 1763. [Google Scholar] [CrossRef] [PubMed]
- Kolesnikoff, N.; Chen, C.H.; Samuel, M.S. Interrelationships between the extracellular matrix and the immune microenvironment that govern epithelial tumour progression. Clin. Sci. 2022, 136, 361–377. [Google Scholar] [CrossRef]
- Jabbari, N.; Akbariazar, E.; Feqhhi, M.; Rahbarghazi, R.; Rezaie, J. Breast cancer-derived exosomes: Tumor progression and therapeutic agents. J. Cell Physiol. 2020, 235, 6345–6356. [Google Scholar] [CrossRef]
- Greening, D.W.; Gopal, S.K.; Xu, R.; Simpson, R.J.; Chen, W. Exosomes and their roles in immune regulation and cancer. Semin. Cell Dev. Biol. 2015, 40, 72–81. [Google Scholar] [CrossRef] [PubMed]
- Chaput, N.; Théry, C. Exosomes: Immune properties and potential clinical implementations. Semin. Immunopathol. 2011, 33, 419–440. [Google Scholar] [CrossRef] [PubMed]
- Shenoda, B.B.; Ajit, S.K. Modulation of Immune Responses by Exosomes Derived from Antigen-Presenting Cells. Clin. Med. Insights Pathol. 2016, 9 (Suppl. 1), 1–8. [Google Scholar] [CrossRef]
- Théry, C.; Amigorena, S. The cell biology of antigen presentation in dendritic cells. Curr. Opin. Immunol. 2001, 13, 45–51. [Google Scholar] [CrossRef]
- Théry, C.; Ostrowski, M.; Segura, E. Membrane vesicles as conveyors of immune responses. Nat. Rev. Immunol. 2009, 9, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Iannotta, D.; Kijas, A.W.; Rowan, A.E.; Wolfram, J. Entry and exit of extracellular vesicles to and from the blood circulation. Nat. Nanotechnol. 2024, 19, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zhao, Z.; Gao, B.; Zhang, L. Exosome mediated biological functions within skeletal microenvironment. Front. Bioeng. Biotechnol. 2022, 10, 953916. [Google Scholar] [CrossRef] [PubMed]
- Wolfram, J.; Ferrari, M. Clinical Cancer Nanomedicine. Nano Today 2019, 25, 85–98. [Google Scholar] [CrossRef] [PubMed]
- Rana, S.; Yue, S.; Stadel, D.; Zöller, M. Toward tailored exosomes: The exosomal tetraspanin web contributes to target cell selection. Int. J. Biochem. Cell Biol. 2012, 44, 1574–1584. [Google Scholar] [CrossRef]
- Rudt, S.; Müller, R.H. In vitro phagocytosis assay of nano- and microparticles by chemiluminescence. III. Uptake of differently sized surface-modified particles, and its correlation to particle properties and in vivo distribution. Eur. J. Pharm. Sci. 1993, 1, 31–39. [Google Scholar]
- Kalluri, R. The biology and function of exosomes in cancer. J. Clin. Investig. 2016, 126, 1208–1215. [Google Scholar] [CrossRef]
- Dai, J.; Su, Y.; Zhong, S.; Cong, L.; Liu, B.; Yang, J.; Tao, Y.; He, Z.; Chen, C.; Jiang, Y. Exosomes: Key players in cancer and potential therapeutic strategy. Signal Transduct. Target. Ther. 2020, 5, 145. [Google Scholar] [CrossRef]
- Wei, H.; Chen, Q.; Lin, L.; Sha, C.; Li, T.; Liu, Y.; Yin, X.; Xu, Y.; Chen, L.; Gao, W.; et al. Regulation of exosome production and cargo sorting. Int. J. Biol. Sci. 2021, 17, 163–177. [Google Scholar] [CrossRef]
- Essola, J.M.; Zhang, M.; Yang, H.; Li, F.; Xia, B.; Mavoungou, J.F.; Hussain, A.; Huang, Y. Exosome regulation of immune response mechanism: Pros and cons in immunotherapy. Bioact. Mater. 2024, 32, 124–146. [Google Scholar] [CrossRef]
- Ha, D.; Yang, N.; Nadithe, V. Exosomes as therapeutic drug carriers and delivery vehicles across biological membranes: Current perspectives and future challenges. Acta Pharm. Sin. B 2016, 6, 287–296. [Google Scholar] [CrossRef]
- Kobayashi, M.; Sawada, K.; Miyamoto, M.; Shimizu, A.; Yamamoto, M.; Kinose, Y.; Nakamura, K.; Kawano, M.; Kodama, M.; Hashimoto, K.; et al. Exploring the potential of engineered exosomes as delivery systems for tumor-suppressor microRNA replacement therapy in ovarian cancer. Biochem. Biophys. Res. Commun. 2020, 527, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Raguraman, R.; Bhavsar, D.; Kim, D.; Ren, X.; Sikavitsas, V.; Munshi, A.; Ramesh, R. Tumor-targeted exosomes for delivery of anticancer drugs. Cancer Lett. 2023, 558, 216093. [Google Scholar] [CrossRef] [PubMed]
- Kase, Y.; Uzawa, K.; Wagai, S.; Yoshimura, S.; Yamamoto, J.-I.; Toeda, Y.; Okubo, M.; Eizuka, K.; Ando, T.; Nobuchi, T.; et al. Engineered exosomes delivering specific tumor-suppressive RNAi attenuate oral cancer progression. Sci. Rep. 2021, 11, 5897. [Google Scholar] [CrossRef]
- Perocheau, D.; Touramanidou, L.; Gurung, S.; Gissen, P.; Baruteau, J. Clinical applications for exosomes: Are we there yet? Br. J. Pharmacol. 2021, 178, 2375–2392. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, L.; Engel, K.B.; Greytak, S.R.; Moore, H.M. Understanding preanalytical variables and their effects on clinical biomarkers of oncology and immunotherapy. Semin. Cancer Biol. 2018, 52 Pt 2, 26–38. [Google Scholar] [CrossRef]
- Nieuwland, R.; Siljander, P.R.M.; Falcón-Pérez, J.M.; Witwer, K.W. Reproducibility of extracellular vesicle research. Eur. J. Cell Biol. 2022, 101, 151226. [Google Scholar] [CrossRef]
- Yakubovich, E.I.; Polischouk, A.G.; Evtushenko, V.I. Principles and Problems of Exosome Isolation from Biological Fluids. Biochem. Suppl. Ser. A Membr. Cell Biol. 2022, 16, 115–126. [Google Scholar] [CrossRef]
- Helwa, I.; Cai, J.; Drewry, M.D.; Zimmerman, A.; Dinkins, M.B.; Khaled, M.L.; Seremwe, M.; Dismuke, W.M.; Bieberich, E.; Stamer, W.D.; et al. A Comparative Study of Serum Exosome Isolation Using Differential Ultracentrifugation and Three Commercial Reagents. PLoS ONE 2017, 12, e0170628. [Google Scholar] [CrossRef]
- Soares Martins, T.; Catita, J.; Martins Rosa, I.; AB da Cruz e Silva, O.; Henriques, A.G. Exosome isolation from distinct biofluids using precipitation and column-based approaches. PLoS ONE 2018, 13, e0198820. [Google Scholar] [CrossRef]
- Chitti, S.V.; Gummadi, S.; Kang, T.; Shahi, S.; Marzan, A.L.; Nedeva, C.; Sanwlani, R.; Bramich, K.; Stewart, S.; Petrovska, M.; et al. Vesiclepedia 2024: An extracellular vesicles and extracellular particles repository. Nucleic Acids Res. 2023, 52, D1694–D1698. [Google Scholar] [CrossRef] [PubMed]
- Kalra, H.; Simpson, R.J.; Ji, H.; Aikawa, E.; Altevogt, P.; Askenase, P.; Bond, V.C.; Borràs, F.E.; Breakefield, X.; Budnik, V.; et al. Vesiclepedia: A compendium for extracellular vesicles with continuous community annotation. PLoS Biol. 2012, 10, e1001450. [Google Scholar] [CrossRef] [PubMed]
- Witwer, K.W.; Buzás, E.I.; Bemis, L.T.; Bora, A.; Lässer, C.; Lötvall, J.; Nolte-’t Hoen, E.N.; Piper, M.G.; Sivaraman, S.; Skog, J.; et al. Standardization of sample collection, isolation and analysis methods in extracellular vesicle research. J. Extracell. Vesicles 2013, 2, 20360. [Google Scholar] [CrossRef]
- Welsh, J.A.; Goberdhan, D.C.I.; O’Driscoll, L.; Buzas, E.I.; Blenkiron, C.; Bussolati, B.; Cai, H.; Di Vizio, D.; Driedonks, T.A.P.; Erdbrügger, U.; et al. Minimal information for studies of extracellular vesicles (MISEV2023): From basic to advanced approaches. J. Extracell. Vesicles 2024, 13, e12404. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.J.; Chau, Z.L.; Chen, S.Y.; Hill, J.J.; Korpany, K.V.; Liang, N.W.; Lin, L.H.; Lin, Y.H.; Liu, J.K.; Liu, Y.C.; et al. Exosome Processing and Characterization Approaches for Research and Technology Development. Adv. Sci. 2022, 9, e2103222. [Google Scholar] [CrossRef]
- Hartjes, T.A.; Mytnyk, S.; Jenster, G.W.; van Steijn, V.; van Royen, M.E. Extracellular Vesicle Quantification and Characterization: Common Methods and Emerging Approaches. Bioengineering 2019, 6, 7. [Google Scholar] [CrossRef] [PubMed]
- Corona, M.L.; Hurbain, I.; Raposo, G.; van Niel, G. Characterization of Extracellular Vesicles by Transmission Electron Microscopy and Immunolabeling Electron Microscopy. Methods Mol. Biol. 2023, 2668, 33–43. [Google Scholar]
- Tanasi, I.; Adamo, A.; Kamga, P.T.; Bazzoni, R.; Krampera, M. High-throughput analysis and functional interpretation of extracellular vesicle content in hematological malignancies. Comput. Struct. Biotechnol. J. 2020, 18, 2670–2677. [Google Scholar] [CrossRef]
- Jiang, C.; Fu, Y.; Liu, G.; Shu, B.; Davis, J.; Tofaris, G.K. Multiplexed Profiling of Extracellular Vesicles for Biomarker Development. Nano-Micro Lett. 2021, 14, 3. [Google Scholar] [CrossRef]
- He, A.; Wang, M.; Li, X.; Chen, H.; Lim, K.; Lu, L.; Zhang, C. Role of Exosomes in the Pathogenesis and Theranostic of Alzheimer’s Disease and Parkinson’s Disease. Int. J. Mol. Sci. 2023, 24, 11054. [Google Scholar] [CrossRef]
- D’Argenio, V. The High-Throughput Analyses Era: Are We Ready for the Data Struggle? High Throughput 2018, 7, 8. [Google Scholar] [CrossRef] [PubMed]
- Huber, M.J.; Ivleva, N.P.; Booth, A.M.; Beer, I.; Bianchi, I.; Drexel, R.; Geiss, O.; Mehn, D.; Meier, F.; Molska, A.; et al. Physicochemical characterization and quantification of nanoplastics: Applicability, limitations and complementarity of batch and fractionation methods. Anal. Bioanal. Chem. 2023, 415, 3007–3031. [Google Scholar] [CrossRef] [PubMed]
- Omrani, M.; Beyrampour-Basmenj, H.; Jahanban-Esfahlan, R.; Talebi, M.; Raeisi, M.; Serej, Z.A.; Akbar-Gharalari, N.; Khodakarimi, S.; Wu, J.; Ebrahimi-Kalan, A. Global trend in exosome isolation and application: An update concept in management of diseases. Mol. Cell Biochem. 2024, 479, 679–691. [Google Scholar] [CrossRef] [PubMed]
- Allelein, S.; Medina-Perez, P.; Lopes, A.L.H.; Rau, S.; Hause, G.; Kölsch, A.; Kuhlmeier, D. Potential and challenges of specifically isolating extracellular vesicles from heterogeneous populations. Sci. Rep. 2021, 11, 11585. [Google Scholar] [CrossRef] [PubMed]
- Kurian, T.K.; Banik, S.; Gopal, D.; Chakrabarti, S.; Mazumder, N. Elucidating Methods for Isolation and Quantification of Exosomes: A Review. Mol. Biotechnol. 2021, 63, 249–266. [Google Scholar] [CrossRef] [PubMed]
- Rastogi, S.; Sharma, V.; Bharti, P.S.; Rani, K.; Modi, G.P.; Nikolajeff, F.; Kumar, S. The Evolving Landscape of Exosomes in Neurodegenerative Diseases: Exosomes Characteristics and a Promising Role in Early Diagnosis. Int. J. Mol. Sci. 2021, 22, 440. [Google Scholar] [CrossRef] [PubMed]
- Hilton, S.H.; White, I.M. Advances in the analysis of single extracellular vesicles: A critical review. Sens. Actuators Rep. 2021, 3, 100052. [Google Scholar] [CrossRef]
- Zhu, J.; Wu, F.; Li, C.; Mao, J.; Wang, Y.; Zhou, X.; Xie, H.; Wen, C. Application of Single Extracellular Vesicle Analysis Techniques. Int. J. Nanomed. 2023, 18, 5365–5376. [Google Scholar] [CrossRef]
- Groot Kormelink, T.; Arkesteijn, G.J.; Nauwelaers, F.A.; van den Engh, G.; Nolte-’t Hoen, E.N.; Wauben, M.H. Prerequisites for the analysis and sorting of extracellular vesicle subpopulations by high-resolution flow cytometry. Cytometry A 2016, 89, 135–147. [Google Scholar] [CrossRef]
- McNamara, R.P.; Zhou, Y.; Eason, A.B.; Landis, J.T.; Chambers, M.G.; Willcox, S.; Peterson, T.A.; Schouest, B.; Maness, N.J.; MacLean, A.G.; et al. Imaging of surface microdomains on individual extracellular vesicles in 3-D. J. Extracell. Vesicles 2022, 11, e12191. [Google Scholar] [CrossRef]
- Nizamudeen, Z.; Markus, R.; Lodge, R.; Parmenter, C.; Platt, M.; Chakrabarti, L.; Sottile, V. Rapid and accurate analysis of stem cell-derived extracellular vesicles with super resolution microscopy and live imaging. Biochim. Biophys. Acta Mol. Cell Res. 2018, 1865, 1891–1900. [Google Scholar] [CrossRef]
- Bond, C.; Santiago-Ruiz, A.N.; Tang, Q.; Lakadamyali, M. Technological advances in super-resolution microscopy to study cellular processes. Mol. Cell 2022, 82, 315–332. [Google Scholar] [CrossRef]
- Endesfelder, U.; Heilemann, M. Direct Stochastic Optical Reconstruction Microscopy (dSTORM). Methods Mol. Biol. 2015, 1251, 263–276. [Google Scholar]
- Lehmann, M.; Gottschalk, B.; Puchkov, D.; Schmieder, P.; Schwagerus, S.; Hackenberger, C.P.; Haucke, V.; Schmoranzer, J. Multicolor Caged dSTORM Resolves the Ultrastructure of Synaptic Vesicles in the Brain. Angew. Chem. Int. Ed. 2015, 54, 13230–13235. [Google Scholar] [CrossRef]
- Kudalkar, E.M.; Davis, T.N.; Asbury, C.L. Single-Molecule Total Internal Reflection Fluorescence Microscopy. Cold Spring Harb. Protoc. 2016, 2016, pdb.top077800. [Google Scholar] [CrossRef]
- Ter-Ovanesyan, D.; Kowal, E.J.K.; Regev, A.; Church, G.M.; Cocucci, E. Imaging of Isolated Extracellular Vesicles Using Fluorescence Microscopy. Methods Mol. Biol. 2017, 1660, 233–241. [Google Scholar]
- Skotland, T.; Hessvik, N.P.; Sandvig, K.; Llorente, A. Exosomal lipid composition and the role of ether lipids and phosphoinositides in exosome biology. J. Lipid Res. 2019, 60, 9–18. [Google Scholar] [CrossRef]
- Gardiner, C.; Shaw, M.; Hole, P.; Smith, J.; Tannetta, D.; Redman, C.W.; Sargent, I.L. Measurement of refractive index by nanoparticle tracking analysis reveals heterogeneity in extracellular vesicles. J. Extracell. Vesicles 2014, 3, 25361. [Google Scholar] [CrossRef]
- Hickey, S.M.; Ung, B.; Bader, C.; Brooks, R.; Lazniewska, J.; Johnson, I.R.D.; Sorvina, A.; Logan, J.; Martini, C.; Moore, C.R.; et al. Fluorescence Microscopy-An Outline of Hardware, Biological Handling, and Fluorophore Considerations. Cells 2021, 11, 35. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Ma, L.; Wang, S.; Chen, C.; Zhang, W.; Yang, L.; Hang, W.; Nolan, J.P.; Wu, L.; Yan, X. Light-scattering detection below the level of single fluorescent molecules for high-resolution characterization of functional nanoparticles. ACS Nano 2014, 8, 10998–11006. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; LeClaire, M.; Gimzewski, J.K. Ascent of atomic force microscopy as a nanoanalytical tool for exosomes and other extracellular vesicles. Nanotechnology 2018, 29, 132001. [Google Scholar] [CrossRef]
- Shao, H.; Im, H.; Castro, C.M.; Breakefield, X.; Weissleder, R.; Lee, H. New Technologies for Analysis of Extracellular Vesicles. Chem. Rev. 2018, 118, 1917–1950. [Google Scholar] [CrossRef]
- Li, X.H.; Zhang, J.; Li, D.F.; Wu, W.; Xie, Z.W.; Liu, Q. Physiological and pathological insights into exosomes in the brain. Zool. Res. 2020, 41, 365–372. [Google Scholar] [CrossRef]
- Liu, S.-L.; Sun, P.; Li, Y.; Liu, S.-S.; Lu, Y. Exosomes as critical mediators of cell-to-cell communication in cancer pathogenesis and their potential clinical application. Transl. Cancer Res. 2019, 8, 298–311. [Google Scholar] [CrossRef]
- Bahr, M.M.; Amer, M.S.; Abo-El-Sooud, K.; Abdallah, A.N.; El-Tookhy, O.S. Preservation techniques of stem cells extracellular vesicles: A gate for manufacturing of clinical grade therapeutic extracellular vesicles and long-term clinical trials. Int. J. Vet. Sci. Med. 2020, 8, 1–8. [Google Scholar] [CrossRef]
- Wu, J.Y.; Li, Y.J.; Hu, X.B.; Huang, S.; Xiang, D.X. Preservation of small extracellular vesicles for functional analysis and therapeutic applications: A comparative evaluation of storage conditions. Drug Deliv. 2021, 28, 162–170. [Google Scholar] [CrossRef]
- Jeyaram, A.; Jay, S.M. Preservation and Storage Stability of Extracellular Vesicles for Therapeutic Applications. AAPS J. 2017, 20, 1–7. [Google Scholar] [CrossRef]
- Qazi, R.E.M.; Sajid, Z.; Zhao, C.; Hussain, I.; Iftikhar, F.; Jameel, M.; Rehman, F.U.; Mian, A.A. Lyophilization Based Isolation of Exosomes. Int. J. Mol. Sci. 2023, 24, 10477. [Google Scholar] [CrossRef]
- Cottle, C.; Porter, A.P.; Lipat, A.; Turner-Lyles, C.; Nguyen, J.; Moll, G.; Chinnadurai, R. Impact of Cryopreservation and Freeze-Thawing on Therapeutic Properties of Mesenchymal Stromal/Stem Cells and Other Common Cellular Therapeutics. Curr. Stem Cell Rep. 2022, 8, 72–92. [Google Scholar] [CrossRef] [PubMed]
- Görgens, A.; Corso, G.; Hagey, D.W.; Jawad Wiklander, R.; Gustafsson, M.O.; Felldin, U.; Lee, Y.; Bostancioglu, R.B.; Sork, H.; Liang, X.; et al. Identification of storage conditions stabilizing extracellular vesicles preparations. J. Extracell. Vesicles 2022, 11, e12238. [Google Scholar] [CrossRef] [PubMed]
- Kusuma, G.D.; Barabadi, M.; Tan, J.L.; Morton, D.A.V.; Frith, J.E.; Lim, R. To Protect and to Preserve: Novel Preservation Strategies for Extracellular Vesicles. Front. Pharmacol. 2018, 9, 417722. [Google Scholar] [CrossRef]
- Gelibter, S.; Marostica, G.; Mandelli, A.; Siciliani, S.; Podini, P.; Finardi, A.; Furlan, R. The impact of storage on extracellular vesicles: A systematic study. J. Extracell. Vesicles 2022, 11, e12162. [Google Scholar] [CrossRef]
- Sivanantham, A.; Jin, Y. Impact of Storage Conditions on EV Integrity/Surface Markers and Cargos. Life 2022, 12, 697. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, S.; Tehrani, F.R.; Tahmasebi, S.; Shafiee, A.; Hashemi, S.M. Exosome engineering in cell therapy and drug delivery. Inflammopharmacology 2023, 31, 145–169. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.; Guo, S.; Ren, X.; Wu, Z.; Liu, S.; Yao, X. Current Strategies for Exosome Cargo Loading and Targeting Delivery. Cells 2023, 12, 1416. [Google Scholar] [CrossRef]
- Chen, H.; Yao, H.; Chi, J.; Li, C.; Liu, Y.; Yang, J.; Yu, J.; Wang, J.; Ruan, Y.; Pi, J.; et al. Engineered exosomes as drug and RNA co-delivery system: New hope for enhanced therapeutics? Front. Bioeng. Biotechnol. 2023, 11, 1254356. [Google Scholar] [CrossRef] [PubMed]
- Patel, G.; Agnihotri, T.G.; Gitte, M.; Shinde, T.; Gomte, S.S.; Goswami, R.; Jain, A. Exosomes: A potential diagnostic and treatment modality in the quest for counteracting cancer. Cell Oncol. 2023, 46, 1159–1179. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Yang, Q.; Sun, X.; Wang, Y. Recent Advancements in the Loading and Modification of Therapeutic Exosomes. Front. Bioeng. Biotechnol. 2020, 8, 586130. [Google Scholar] [CrossRef]
- Kim, M.S.; Haney, M.J.; Zhao, Y.; Mahajan, V.; Deygen, I.; Klyachko, N.L.; Inskoe, E.; Piroyan, A.; Sokolsky, M.; Okolie, O.; et al. Development of exosome-encapsulated paclitaxel to overcome MDR in cancer cells. Nanomedicine 2016, 12, 655–664. [Google Scholar] [CrossRef]
- Ohno, S.; Takanashi, M.; Sudo, K.; Ueda, S.; Ishikawa, A.; Matsuyama, N.; Fujita, K.; Mizutani, T.; Ohgi, T.; Ochiya, T.; et al. Systemically injected exosomes targeted to EGFR deliver antitumor microRNA to breast cancer cells. Mol. Ther. 2013, 21, 185–191. [Google Scholar] [CrossRef]
- Kučuk, N.; Primožič, M.; Knez, Ž.; Leitgeb, M. Exosomes Engineering and Their Roles as Therapy Delivery Tools, Therapeutic Targets, and Biomarkers. Int. J. Mol. Sci. 2021, 22, 9543. [Google Scholar] [CrossRef]
- Xu, M.; Feng, T.; Liu, B.; Qiu, F.; Xu, Y.; Zhao, Y.; Zheng, Y. Engineered exosomes: Desirable target-tracking characteristics for cerebrovascular and neurodegenerative disease therapies. Theranostics 2021, 11, 8926–8944. [Google Scholar] [CrossRef]
- Zhu, Q.; Ling, X.; Yang, Y.; Zhang, J.; Li, Q.; Niu, X.; Hu, G.; Chen, B.; Li, H.; Wang, Y.; et al. Embryonic Stem Cells-Derived Exosomes Endowed with Targeting Properties as Chemotherapeutics Delivery Vehicles for Glioblastoma Therapy. Adv. Sci. 2019, 6, 1801899. [Google Scholar] [CrossRef]
- Pham, T.C.; Jayasinghe, M.K.; Pham, T.T.; Yang, Y.; Wei, L.; Usman, W.M.; Chen, H.; Pirisinu, M.; Gong, J.; Kim, S.; et al. Covalent conjugation of extracellular vesicles with peptides and nanobodies for targeted therapeutic delivery. J. Extracell. Vesicles 2021, 10, e12057. [Google Scholar] [CrossRef]
- Wang, J.; Wang, M.; Jiang, N.; Ding, S.; Peng, Q.; Zheng, L. Emerging chemical engineering of exosomes as “bioscaffolds” in diagnostics and therapeutics. Genes Dis. 2023, 10, 1494–1512. [Google Scholar] [CrossRef]
- Sharma, V.; Mukhopadhyay, C.D. Exosome as drug delivery system: Current advancements. Extracell. Vesicle 2024, 3, 100032. [Google Scholar] [CrossRef]
- Li, T.; Li, X.; Han, G.; Liang, M.; Yang, Z.; Zhang, C.; Huang, S.; Tai, S.; Yu, S. The Therapeutic Potential and Clinical Significance of Exosomes as Carriers of Drug Delivery System. Pharmaceutics 2022, 15, 21. [Google Scholar] [CrossRef]
- Krylova, S.V.; Feng, D. The Machinery of Exosomes: Biogenesis, Release, and Uptake. Int. J. Mol. Sci. 2023, 24, 1337. [Google Scholar] [CrossRef]
- Ghadami, S.; Dellinger, K. The lipid composition of extracellular vesicles: Applications in diagnostics and therapeutic delivery. Front. Mol. Biosci. 2023, 10, 1198044. [Google Scholar] [CrossRef] [PubMed]
- Morton, L.A.; Yang, H.; Saludes, J.P.; Fiorini, Z.; Beninson, L.; Chapman, E.R.; Fleshner, M.; Xue, D.; Yin, H. MARCKS-ED peptide as a curvature and lipid sensor. ACS Chem. Biol. 2013, 8, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Unterreitmeier, S.; Fuchs, A.; Schäffler, T.; Heym, R.G.; Frishman, D.; Langosch, D. Phenylalanine promotes interaction of transmembrane domains via GxxxG motifs. J. Mol. Biol. 2007, 374, 705–718. [Google Scholar] [CrossRef]
- Yan, L.; de Jesus, A.J.; Tamura, R.; Li, V.; Cheng, K.; Yin, H. Curvature sensing MARCKS-ED peptides bind to membranes in a stereo-independent manner. J. Pept. Sci. 2015, 21, 577–585. [Google Scholar] [CrossRef] [PubMed]
- Flynn, A.D.; Yin, H. Lipid-Targeting Peptide Probes for Extracellular Vesicles. J. Cell Physiol. 2016, 231, 2327–2332. [Google Scholar] [CrossRef] [PubMed]
- Babatunde, K.A.; Yesodha Subramanian, B.; Ahouidi, A.D.; Martinez Murillo, P.; Walch, M.; Mantel, P.Y. Role of Extracellular Vesicles in Cellular Cross Talk in Malaria. Front. Immunol. 2020, 11, 22. [Google Scholar] [CrossRef] [PubMed]
- Regev-Rudzki, N.; Wilson, D.W.; Carvalho, T.G.; Sisquella, X.; Coleman, B.M.; Rug, M.; Bursac, D.; Angrisano, F.; Gee, M.; Hill, A.F.; et al. Cell-cell communication between malaria-infected red blood cells via exosome-like vesicles. Cell 2013, 153, 1120–1133. [Google Scholar] [CrossRef] [PubMed]
- Ngambenjawong, C.; Pineda, J.M.; Pun, S.H. Engineering an Affinity-Enhanced Peptide through Optimization of Cyclization Chemistry. Bioconjug. Chem. 2016, 27, 2854–2862. [Google Scholar] [CrossRef] [PubMed]
- Xu, K.; Jin, Y.; Li, Y.; Huang, Y.; Zhao, R. Recent Progress of Exosome Isolation and Peptide Recognition-Guided Strategies for Exosome Research. Front. Chem. 2022, 10, 844124. [Google Scholar] [CrossRef] [PubMed]
- Morton, L.A.; Tamura, R.; de Jesus, A.J.; Espinoza, A.; Yin, H. Biophysical investigations with MARCKS-ED: Dissecting the molecular mechanism of its curvature sensing behaviors. Biochim. Biophys. Acta 2014, 1838, 3137–3144. [Google Scholar] [CrossRef] [PubMed]
- Quadri, Z.; Elsherbini, A.; Bieberich, E. Extracellular vesicles in pharmacology: Novel approaches in diagnostics and therapy. Pharmacol. Res. 2022, 175, 105980. [Google Scholar] [CrossRef]
- Morishita, M.; Takahashi, Y.; Nishikawa, M.; Takakura, Y. Pharmacokinetics of Exosomes-An Important Factor for Elucidating the Biological Roles of Exosomes and for the Development of Exosome-Based Therapeutics. J. Pharm. Sci. 2017, 106, 2265–2269. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, Q.; Zhang, X.; Huang, H.; Tang, S.; Chai, Y.; Xu, Z.; Li, M.; Chen, X.; Liu, J.; et al. Recent advances in exosome-mediated nucleic acid delivery for cancer therapy. J. Nanobiotechnol. 2022, 20, 279. [Google Scholar] [CrossRef]
- Bao, C.; Xiang, H.; Chen, Q.; Zhao, Y.; Gao, Q.; Huang, F.; Mao, L. A Review of Labeling Approaches Used in Small Extracellular Vesicles Tracing and Imaging. Int. J. Nanomed. 2023, 18, 4567–4588. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.; Choi, Y.; Yim, H.Y.; Mirzaaghasi, A.; Yoo, J.K.; Choi, C. Biodistribution of Exosomes and Engineering Strategies for Targeted Delivery of Therapeutic Exosomes. Tissue Eng. Regen. Med. 2021, 18, 499–511. [Google Scholar] [CrossRef]
- Bruno, B.J.; Miller, G.D.; Lim, C.S. Basics and recent advances in peptide and protein drug delivery. Ther. Deliv. 2013, 4, 1443–1467. [Google Scholar] [CrossRef]
- Samanta, S.; Rajasingh, S.; Drosos, N.; Zhou, Z.; Dawn, B.; Rajasingh, J. Exosomes: New molecular targets of diseases. Acta Pharmacol. Sin. 2018, 39, 501–513. [Google Scholar] [CrossRef] [PubMed]
- Susa, F.; Limongi, T.; Dumontel, B.; Vighetto, V.; Cauda, V. Engineered Extracellular Vesicles as a Reliable Tool in Cancer Nanomedicine. Cancers 2019, 11, 1979. [Google Scholar] [CrossRef]
- Kooijmans, S.A.A.; de Jong, O.G.; Schiffelers, R.M. Exploring interactions between extracellular vesicles and cells for innovative drug delivery system design. Adv. Drug Deliv. Rev. 2021, 173, 252–278. [Google Scholar] [CrossRef] [PubMed]
- Santelices, J.; Ou, M.; Hui, W.W.; Maegawa, G.H.B.; Edelmann, M.J. Fluorescent Labeling of Small Extracellular Vesicles (EVs) Isolated from Conditioned Media. Bio-protocol 2022, 12, e4447. [Google Scholar] [CrossRef] [PubMed]
- N’Diaye, E.R.; Orefice, N.S.; Ghezzi, C.; Boumendjel, A. Chemically Modified Extracellular Vesicles and Applications in Radiolabeling and Drug Delivery. Pharmaceutics 2022, 14, 653. [Google Scholar] [CrossRef]
- Szymanowski, W.; Szymanowska, A.; Bielawska, A.; Lopez-Berestein, G.; Rodriguez-Aguayo, C.; Amero, P. Aptamers as Potential Therapeutic Tools for Ovarian Cancer: Advancements and Challenges. Cancers 2023, 15, 5300. [Google Scholar] [CrossRef]
- Chen, Z.; Xiong, M.; Tian, J.; Song, D.; Duan, S.; Zhang, L. Encapsulation and assessment of therapeutic cargo in engineered exosomes: A systematic review. J. Nanobiotechnol. 2024, 22, 18. [Google Scholar] [CrossRef]
- Zhang, Z.; Jia, J.; Lai, Y.; Ma, Y.; Weng, J.; Sun, L. Conjugating folic acid to gold nanoparticles through glutathione for targeting and detecting cancer cells. Bioorganic Med. Chem. 2010, 18, 5528–5534. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Wang, X.; Liu, X.; Cui, Z.; Yang, X.; Yeung, K.W.K.; Chung, J.C.; Chu, P.K.; Wu, S. Tannic Acid/Fe3+/Ag Nanofilm Exhibiting Superior Photodynamic and Physical Antibacterial Activity. ACS Appl. Mater. Interfaces 2017, 9, 39657–39671. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Bi, J.; Huang, J.; Tang, Y.; Du, S.; Li, P. Exosome: A Review of Its Classification, Isolation Techniques, Storage, Diagnostic and Targeted Therapy Applications. Int. J. Nanomed. 2020, 15, 6917–6934. [Google Scholar] [CrossRef]
- Muthu, S.; Bapat, A.; Jain, R.; Jeyaraman, N.; Jeyaraman, M. Exosomal therapy-a new frontier in regenerative medicine. Stem Cell Investig. 2021, 8, 7. [Google Scholar] [CrossRef] [PubMed]
- Huda, M.N.; Nafiujjaman, M.; Deaguero, I.G.; Okonkwo, J.; Hill, M.L.; Kim, T.; Nurunnabi, M. Potential Use of Exosomes as Diagnostic Biomarkers and in Targeted Drug Delivery: Progress in Clinical and Preclinical Applications. ACS Biomater. Sci. Eng. 2021, 7, 2106–2149. [Google Scholar] [CrossRef]
- Beetler, D.J.; Di Florio, D.N.; Bruno, K.A.; Ikezu, T.; March, K.L.; Cooper, L.T.; Jr Wolfram, J.; Fairweather, D. Extracellular vesicles as personalized medicine. Mol. Aspects Med. 2023, 91, 101155. [Google Scholar] [CrossRef] [PubMed]
- Mosquera-Heredia, M.I.; Morales, L.C.; Vidal, O.M.; Barceló, E.; Silvera-Redondo, C.; Vélez, J.I.; Garavito-Galofre, P. Exosomes: Potential Disease Biomarkers and New Therapeutic Targets. Biomedicines 2021, 9, 1061. [Google Scholar] [CrossRef]
- Del Bene, M.; Osti, D.; Faletti, S.; Beznoussenko, G.V.; DiMeco, F.; Pelicci, G. Extracellular vesicles: The key for precision medicine in glioblastoma. Neuro-Oncology 2021, 24, 184–196. [Google Scholar] [CrossRef]
- Shang, M.; Ji, J.S.; Song, C.; Gao, B.J.; Jin, J.G.; Kuo, W.P.; Kang, H. Extracellular Vesicles: A Brief Overview and Its Role in Precision Medicine, in Extracellular Vesicles: Methods and Protocols; Kuo, W.P., Jia, S., Eds.; Springer: New York, NY, USA, 2017; pp. 1–14. [Google Scholar]
- Lone, S.N.; Nisar, S.; Masoodi, T.; Singh, M.; Rizwan, A.; Hashem, S.; El-Rifai, W.; Bedognetti, D.; Batra, S.K.; Haris, M.; et al. Liquid biopsy: A step closer to transform diagnosis, prognosis and future of cancer treatments. Mol. Cancer 2022, 21, 79. [Google Scholar] [CrossRef]
- Areny-Balagueró, A.; Solé-Porta, A.; Camprubí-Rimblas, M.; Campaña-Duel, E.; Ceccato, A.; Roig, A.; Closa, D.; Artigas, A. Bioengineered extracellular vesicles: Future of precision medicine for sepsis. Intensive Care Med. Exp. 2023, 11, 11. [Google Scholar] [CrossRef] [PubMed]
- Mora, E.M.; Álvarez-Cubela, S.; Oltra, E. Biobanking of Exosomes in the Era of Precision Medicine: Are We There Yet? Int. J. Mol. Sci. 2015, 17, 13. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Shin, T.-S.; Kim, J.S.; Jee, Y.-K.; Kim, Y.-K. A new horizon of precision medicine: Combination of the microbiome and extracellular vesicles. Exp. Mol. Med. 2022, 54, 466–482. [Google Scholar] [CrossRef] [PubMed]
- Desdín-Micó, G.; Mittelbrunn, M. Role of exosomes in the protection of cellular homeostasis. Cell Adhes. Migr. 2017, 11, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Chutipongtanate, S.; Pattanapanyasat, K.; Meller, J.; Serrano López, J. Editorial: Driving extracellular vesicles toward applications in precision medicine. Front. Med. 2022, 9, 1049697. [Google Scholar] [CrossRef]
- Arraud, N.; Linares, R.; Tan, S.; Gounou, C.; Pasquet, J.M.; Mornet, S.; Brisson, A.R. Extracellular vesicles from blood plasma: Determination of their morphology, size, phenotype and concentration. J. Thromb. Haemost. 2014, 12, 614–627. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Waheed, S.; Wang, C.; Shekh, M.; Li, Z.; Wu, J. Exosomes and Their Bioengineering Strategies in the Cutaneous Wound Healing and Related Complications: Current Knowledge and Future Perspectives. Int. J. Biol. Sci. 2023, 19, 1430–1454. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Lv, G.; Wei, F. Engineering exosomes to reshape the immune microenvironment in breast cancer: Molecular insights and therapeutic opportunities. Clin. Transl. Med. 2024, 14, e1645. [Google Scholar] [CrossRef] [PubMed]
- FDA. Public Safety Alert Due to Marketing of Unapproved Stem Cell and Exosome Products. 2019. Available online: https://www.fda.gov/safety/medical-product-safety-information/public-safety-alert-due-marketing-unapproved-stem-cell-and-exosome-products (accessed on 20 April 2024).
- Cheng, K.; Kalluri, R. Guidelines for clinical translation and commercialization of extracellular vesicles and exosomes based therapeutics. Extracell. Vesicle 2023, 2, 100029. [Google Scholar] [CrossRef]
- Tzng, E.; Bayardo, N.; Yang, P.C. Current challenges surrounding exosome treatments. Extracell. Vesicle 2023, 2, 100023. [Google Scholar] [CrossRef]


| Vesicle Type | Advantages | Disadvantages |
|---|---|---|
| Exosomes |
|
|
| Microvesicles |
|
|
| Liposomes |
|
|
| NCT Number | Study Title | Conditions | Phases |
|---|---|---|---|
| NCT05218759 | Exosomes Detection for the Prediction of the Efficacy and Adverse Reactions of Anlotinib in Patients with Advanced NSCLC | Non-Small-Cell Lung Cancer | NA |
| NCT02822131 | Phosphate in Blood Pressure Regulation | Hypertension | NA |
| NCT02579460 | Reflux-Induced Oxidative Stress in Barrett’s Esophagus: Response, Repair, and Epithelial-Mesenchymal-Transition | Barrett’s Esophagus|Gastroesophageal Reflux Disease | NA |
| NCT06072794 | A Proof-of-Concept Study to Evaluate Exosomes from Human Mesenchymal Stem Cells in Women with Premature Ovarian Insufficiency (POI) | Premature Ovarian Insufficiency|Diminished Ovarian Reserve | Phase 1 |
| NCT05658094 | Exosome Effect on Prevention of Hair loss | Hair Loss|Alopecia | NA |
| NCT02649465 | SGLT2 Inhibitor Versus Sulfonylurea on Type 2 Diabetes With NAFLD | Non-alcoholic Fatty Liver Disease | Phase 4 |
| NCT03109873 | Metformin Hydrochloride in Affecting Cytokines and Exosomes in Patients with Head and Neck Cancer | Larynx|Lip|Oral Cavity|Pharynx | Early Phase 1 |
| NCT04184076 | Randomized Controlled Trial of Time-Restricted Feeding (TRF) in Acute Ischemic Stroke Patients | Fasting | NA |
| NCT05490173 | The Pilot Experimental Study of the Neuroprotective Effects of Exosomes in Extremely Low Birth Weight Infants | Premature Birth|Extreme Prematurity|Preterm Intraventricular Hemorrhage|Hypoxia-Ischemia, Cerebral|Neurodevelopmental Disorders | NA |
| NCT02138331 | Effect of Microvesicles and Exosomes Therapy on β-cell Mass in Type I Diabetes Mellitus (T1DM) | Diabetes Mellitus Type 1 | Phase 2|Phase 3 |
| NCT04459182 | Circulating Exosomes and Endothelial Dysfunction in Patients with Obstructive Sleep Apneas Hypopneas Syndrome | Endothelial Dysfunction | NA |
| NCT03608631 | iExosomes in Treating Participants with Metastatic Pancreas Cancer with KrasG12D Mutation | KRAS NP_004976.2: p. G12D|Metastatic Pancreatic Adenocarcinoma Pancreatic Ductal Adenocarcinoma Stage IV Pancreatic Cancer AJCC v8 | Phase 1 |
| NCT04388982 | the Safety and the Efficacy Evaluation of Allogenic Adipose MSC-Exos in Patients with Alzheimer’s Disease | Alzheimer’s Disease | Phase 1|Phase 2 |
| NCT01104220 | Role of Immune System in Obesity-related Inflammation and Cardiometabolic Risk | Non-alcoholic Fatty Liver Disease|Metabolic Syndrome|Metabolically Abnormal Obesity|Metabolically Normal Obesity|Obesity | NA |
| NCT05073627 | The Effect of Dicloxacillin on Oral Absorption of Drugs | Healthy Volunteers|Drug–Drug Interaction | Phase 1 |
| NCT04153539 | Acute Health Effects of Traffic-Related Air Pollution Exposure | Cardiovascular System|Respiratory System | NA |
| NCT05871463 | Effect of Mesenchymal Stem Cells-derived Exosomes in Decompensated Liver Cirrhosis | Decompensated Liver Cirrhosis | Phase 2 |
| NCT05692635 | Reducing the Incidence of Symptomatic Brain Metastases with MRI Surveillance | Brain Metastases|Non-Small-Cell Lung Cancer Stage III | Phase 2 |
| NCT05163626 | Combined Aerobic Exercise and Cognitive Training in Seniors at Increased Risk for Alzheimer’s Disease | Alzheimer’s Disease | NA |
| NCT04131166 | Precision Nutrition and Metabolic Function | Obesity|Insulin Resistance | NA |
| NCT03217266 | Navtemadlin and Radiation Therapy in Treating Patients with Soft Tissue Sarcoma | Resectable Soft Tissue Sarcoma|Soft Tissue Sarcoma | Phase 1 |
| NCT03027726 | Prevention of Diabetes in Overweight/Obese Preadolescent Children | Overweight Children with Type 2 Diabetes Risk | NA |
| NCT06259435 | Modulating Energy Density in Time-Restricted Eating | Insulin Resistance|Body Weight | NA |
| NCT04134676 | Therapeutic Potential of Stem Cell Conditioned Medium on Chronic Ulcer Wounds | Chronic Ulcer | Phase 1 |
| NCT05777876 | Early Identification of TRD and Construction and Clinical Validation of NTBS Precision Technology | Treatment-Resistant Depression | NA |
| NCT05563766 | A Phase II Trial to Evaluate the Effect of Itraconazole on Pathologic Complete Response Rates in Resectable Esophageal Cancer | Esophageal Adenocarcinoma|Esophageal Squamous Cell Carcinoma|Gastroesophageal Junction Carcinoma | Phase 2 |
| NCT04460963 | Role of Adrenomedullin in Leukemic Endosteal/Vascular Niches | Acute Myeloid Leukemia | NA |
| NCT04258735 | Genetic Characteristics of Metastatic Breast Cancer Patients | Metastatic Breast Cancer | NA |
| NCT03410030 | Trial of Ascorbic Acid (AA) + Nanoparticle Paclitaxel Protein Bound + Cisplatin + Gemcitabine (AA NABPLAGEM) | Pancreatic Cancer|Pancreas Cancer|Pancreatic Adenocarcinoma Resectable|Pancreatic Ductal Adenocarcinoma|Pancreas Metastases | Phase 1|Phase 2 |
| NCT04747574 | Evaluation of the Safety of CD24-Exosomes in Patients With COVID-19 Infection | SARS-CoV-2 | Phase 1 |
| NCT05969717 | Induced Pluripotent Stem Cell Derived Exosomes for the Treatment of Atopic Dermatitis | Atopic Dermatitis | Early Phase 1 |
| NCT02653339 | Effectiveness of Qufeng Shengshi Fang on Treatment of Allergic Rhinitis. | Rhinitis, Allergic, Perennial | NA |
| NCT04266639 | Rheo-Erythrocrine Dysfunction as a Biomarker for RIC Treatment in Acute Ischemic Stroke | Stroke, Acute|Ischemic Stroke|Cerebrovascular Disorders|Central Nervous System Diseases | NA |
| NCT05354141 | Extracellular Vesicle Treatment for Acute Respiratory Distress Syndrome (ARDS) (EXTINGUISH ARDS) | Acute Respiratory Distress Syndrome|ARDS | Phase 3 |
| NCT05616234 | Exercise-induced Changes in Exosomes | Exosomes|Connective Tissue|Exercise | NA |
| NCT06279039 | Clinical Observation of Exosomes in Patients After Q-switched Laser Surgery | Exosome|Skin Regeneration|Laser | NA |
| NCT03230019 | Two-Lumen Catheterization for Lung Wedge Resection | Thoracic Surgery, Video-Assisted | NA |
| NCT03392441 | Insulin Deprivation on Brain Structure and Function in Humans with Type 1 Diabetes | Diabetes Mellitus, Type 1|Diabetes|Diabetes Complications | NA |
| NCT04483219 | Tyrosine Kinase Inhibitor (TKI) + Anti-PD-1 Antibody in TKI-responded Microsatellite Stability/Proficient Mismatch Repair (MSS/pMMR) Metastatic Colorectal Adenocarcinoma. | MSS|pMMR|Metastatic Colorectal Adenocarcinoma | Phase 2 |
| NCT05475418 | Pilot Study of Human Adipose Tissue Derived Exosomes Promoting Wound Healing | Wounds and Injuries | NA |
| NCT06110130 | Effect of Empagliflozin on Podocyte Specific Proteins in African American Veterans With NDKD | Chronic Kidney Diseases | Phase 4 |
| NCT05413148 | The Effect of Stem Cells and Stem Cell Exosomes on Visual Functions in Patients with Retinitis Pigmentosa | Retinitis Pigmentosa | Phase 2|Phase 3 |
| NCT04213248 | Effect of UMSCs Derived Exosomes on Dry Eye in Patients With cGVHD | Dry Eye Disease | Phase 1|Phase 2 |
| NCT05402748 | Safety and Efficacy of Injection of Human Placenta Mesenchymal Stem Cells Derived Exosomes for Treatment of Complex Anal Fistula | Fistula Perianal | Phase 1|Phase 2 |
| NCT03985696 | Exosomes and Immunotherapy in Non-Hodgkin B-cell Lymphomas | Lymphoma, B-cell, Aggressive Non-Hodgkin (B-NHL) | NA |
| NCT05166616 | Minnelide and Osimertinib for the Treatment of Advanced EGFR Mutated Non-Small Cell Lung Cancer | Advanced Lung Non-Small-Cell Carcinoma|Locally Advanced Lung Non-Small-Cell Carcinoma|Stage III Lung Cancer AJCC v8|Stage IIIA Lung Cancer AJCC v8|Stage IIIB Lung Cancer AJCC v8|Stage IIIC Lung Cancer AJCC v8|Stage IV Lung Cancer AJCC v8|Stage IVA Lung Cancer AJCC v8|Stage IVB Lung Cancer AJCC v8|Unresectable Lung Non-Small-Cell Carcinoma | Phase 1 |
| NCT04556916 | Early Detection of Prostate Cancer | Prostate Cancer | NA |
| NCT05815524 | Physical Activity in Patients with Parkinson’s Disease: A “Disease Modifying” Intervention? | Parkinson’s Disease | NA |
| NCT04998058 | Autogenous Mesenchymal Stem Cell Culture-Derived Signaling Molecules as Enhancers of Bone Formation in Bone Grafting | Bone Loss, Osteoclastic|Bone Loss, Alveolar|Alveolar Bone Loss|Alveolar Bone Atrophy|Grafting Bone | Phase 1|Phase 2 |
| NCT02892734 | Ipilimumab and Nivolumab in Treating Patients with Recurrent Stage IV HER2 Negative Inflammatory Breast Cancer | HER2/Neu Negative|Recurrent Inflammatory Breast Carcinoma|Stage IV Breast Cancer|Stage IV Inflammatory Breast Carcinoma | Phase 2 |
| NCT04493242 | Extracellular Vesicle Infusion Treatment for COVID-19 Associated ARDS | COVID-19|ARDS | Phase 2 |
| NCT05698524 | A Study of Temodar with Abexinostat (PCI-24781) for Patients with Recurrent Glioma | Recurrent High-Grade Glioma|Anaplastic Astrocytoma|Anaplastic Oligodendroglioma|Glioblastoma|Gliosarcoma | Phase 1 |
| NCT04798716 | The Use of Exosomes for the Treatment of Acute Respiratory Distress Syndrome or Novel Coronavirus Pneumonia Caused by COVID-19 | COVID-19|Novel Coronavirus Pneumonia|Acute Respiratory Distress Syndrome | Phase 1|Phase 2 |
| NCT04939324 | Molecular Profiling of Exosomes in Tumor-draining Vein of Early-staged Lung Cancer | Lung Cancer|Exosomes|Non-Small-Cell Lung Cancer | NA |
| NCT05326724 | The Role of Acupuncture-induced Exosome in Treating Post-stroke Dementia | Exosome|Post-stroke Dementia|Acupuncture | NA |
| NCT05621109 | PRE-Pregnancy Weight Loss and the Reducing Effect on Childhood Overweight—Copenhagen | Overweight and Obesity|Weight Loss|Pregnancy Related | NA |
| NCT04641585 | Brugada Syndrome and Artificial Intelligence Applications to Diagnosis | Brugada Syndrome 1 | NA |
| NCT05610332 | Clinical Efficacy in Neoadjuvant Treatment of Locally Advanced Gastric Cancer with Different Immunotypes | Locally Advanced Gastric Cancer | Phase 3 |
| NCT02869685 | Consistency Analysis of PD-L1s in Advanced NSCLC Tissues and in Plasma Exosomes Before and After Radiotherapy | NSCLC | NA |
| NCT06361485 | Safety and Feasibility of Umbilical Cord Wharton’s Jelly Allograft Injections for Lumbar Pain | Low Back Pain | Phase 1 |
| NCT02928432 | SWITCH: Study of the Prednisone to Dexamethasone Change in mCRPC Patients Treated with Abiraterone | Prostate Cancer | Phase 2 |
| NCT04765137 | Evaluate the Effect of Atorvastatin on Cerebrovascular Reactivity in MCI | Mild Cognitive Impairment | Phase 2 |
| NCT03854032 | Nivolumab and BMS986205 in Treating Patients with Stage II-IV Squamous Cell Cancer of the Head and Neck | Lip|Oral Cavity Squamous Cell Carcinoma|Pharynx|Larynx|Squamous Cell Carcinoma | Phase 2 |
| NCT04585932 | Androgen Deprivation Therapy and Apalutamide With or Without Radiation Therapy for the Treatment of Biochemically Recurrent Prostate Cancer, RESTART Study | Biochemically Recurrent Prostate Carcinoma|Metastatic Prostate Carcinoma|Oligometastatic Prostate Carcinoma|Stage IV Prostate Cancer AJCC v8|Stage IVA Prostate Cancer AJCC v8|Stage IVB Prostate Cancer AJCC v8 | Phase 2 |
| NCT05669144 | Co-transplantation of Mesenchymal Stem Cell Derived Exosomes and Autologous Mitochondria for Patients Candidate for CABG Surgery | Myocardial Infarction|Myocardial Ischemia|Myocardial Stunning | Phase 1 |Phase 2 |
| NCT04029740 | Exosomal microRNAs as a Biomarker in Panic Disorder and in Response to CBT | Panic Disorder | NA |
| NCT06339840 | The Impact of Lifestyle Intervention on Weight and Fertility in Obese Males | Obesity|Weight Loss|Male Fertility|Artificial Insemination|IVF-ET | NA |
| NCT05192694 | Evaluation of Fapi-pet in Prostate Cancer. | Prostate Cancer | NA |
| NCT04781062 | Development of a Horizontal Data Integration Classifier for Noninvasive Early Diagnosis of Breast Cancer | Breast Cancer | NA |
| NCT03762629 | Exercise and Diet Restriction on Cardiovascular Function in Obese Children and Adolescents | Childhood Obesity|Adolescent Obesity | NA |
| NCT04849429 | Intra-discal Injection of Platelet-rich Plasma (PRP) Enriched with Exosomes in Chronic Low Back Pain | Chronic Low Back Pain|Degenerative Disc Disease | Phase 1 |
| NCT05927129 | Research on the Biological Mechanism of the Efficacy of Psychotherapy for Depression Based on the fNIRS | Depressive Disorder | NA |
| NCT05738629 | Safety and Efficacy of Pluripotent Stem Cell-derived Mesenchymal Stem Cell Exosome (PSC-MSC-Exo) Eye Drops Treatment for Dry Eye Diseases Post Refractive Surgery and Associated with Blepharospasm | Dry Eye Disease | Phase 1|Phase 2 |
| NCT05798494 | PRE-Pregnancy Weight Loss and the Reducing Effect on Childhood Overweight - Aarhus | Overweight and Obesity|Weight Loss|Pregnancy Related|Child Nutrition Sciences|Body Composition | NA |
| NCT05261360 | Clinical Efficacy of Exosome in Degenerative Meniscal Injury | Knee; Injury, Meniscus (Lateral) (Medial)|Meniscus Tear|Meniscus Lesion|Meniscus; Degeneration|Meniscus; Laceration|Meniscus Injury, Tibial|Knee Injuries|Knee Pain Swelling|Arthralgia | Phase 2 |
| NCT03406780 | A Study of CAP-1002 in Ambulatory and Non-Ambulatory Patients with Duchenne Muscular Dystrophy | Muscular Dystrophies|Muscular Dystrophy, Duchenne|Muscular Disorders, Atrophic|Muscular Diseases|Neuromuscular diseases|Nervous System Diseases|Genetic Diseases, X-Linked|Genetic Diseases, Inborn | Phase 2 |
| NCT04334603 | Exercise Intervention in Heart Failure | Heart Failure | NA |
| NCT04595903 | Treatment of SARS-CoV-2 Virus Disease (COVID-19) in Humans with Hemopurifier® Device | COVID-19 | NA |
| NCT03711890 | Ultra-High Resolution Optical Coherence Tomography in Detecting Micrometer Sized Early-Stage Pancreatic Cancer in Participants With Pancreatic Cancer | Pancreatic Carcinoma|Pancreatic Intraductal Papillary Mucinous Neoplasm, Pancreatobiliary-Type | NA |
| NCT05955521 | Exosome as the Prognostic and Predictive Biomarker in EBC Patients | Triple Negative Breast Cancer|HER2-positive Breast Cancer | NA |
| NCT03493984 | Plant Exosomes and Patients Diagnosed with Polycystic Ovary Syndrome (PCOS) 17 | Polycystic Ovary Syndrome | NA |
| NCT03260179 | Study to Evaluate the Safety, Preliminary Efficacy and Pharmacokinetics of 3810 | Advanced Solid Tumor|Advanced/Metastatic Colorectal Cancer | Phase 1 |
| NCT05286684 | Feasibility of Exosome Analysis in Cerebrospinal Fluid During the Diagnostic Workup of Metastatic Meningitis (Exo-LCR) | Breast Cancer | NA |
| NCT04173650 | MSC EVs in Dystrophic Epidermolysis Bullosa | Dystrophic Epidermolysis Bullosa | Phase 1|Phase 2 |
| NCT05243368 | Evaluation of Personalized Nutritional Intervention on Wound Healing of Cutaneous Ulcers in Diabetics | Foot, Diabetics | NA |
| NCT04421872 | The Disorder of Circadian Clock Gene and Early Cognitive Dysfunction After General Anesthesia | Postoperative Delirium|General Anesthesia|Exosomes|Clock Gene Circadian Rhythm Disorders | NA |
| NCT04969172 | A Phase II Randomized, Double-blind, Placebo-controlled Study to Evaluate the Safety and Efficacy of Exosomes Overexpressing CD24 to Prevent Clinical Deterioration in Patients with Moderate or Severe COVID-19 Infection | COVID-19 Disease | Phase 2 |
| NCT01294072 | Study Investigating the Ability of Plant Exosomes to Deliver Curcumin to Normal and Colon Cancer Tissue | Colon Cancer | NA |
| NCT04879810 | Plant Exosomes +/− Curcumin to Abrogate Symptoms of Inflammatory Bowel Disease | Irritable Bowel Disease | NA |
| NCT01550523 | Pilot Immunotherapy Trial for Recurrent Malignant Gliomas | Malignant Glioma of Brain | Phase 1 |
| NCT02439008 | Early Biomarkers of Tumor Response in High Dose Hypo Fractionated Radiotherapy Word Package 3: Immune Response | Carcinoma, Hepatocellular|Colorectal Neoplasms|Melanoma|Kidney Neoplasms | NA |
| NCT03974204 | Analyses of Exosomes in the Cerebrospinal Fluid for Breast Cancer Patients with Suspicion of Leptomeningeal Metastasis. | Breast Cancer|Leptomeningeal Metastasis | NA |
| NCT05913960 | Accelerated Intermittent Theta-Burst Stimulation Ameliorate Major Depressive Disorder by Regulating CAMKII Pathway | Major Depressive Disorder|Major Depressive Disorder, Recurrent | NA |
| NCT05375604 | A Study of exoASO-STAT6 (CDK-004) in Patients with Advanced Hepatocellular Carcinoma (HCC) and Patients with Liver Metastases from Either Primary Gastric Cancer or Colorectal Cancer (CRC) | Advanced Hepatocellular Carcinoma (HCC)|Gastric Cancer Metastatic to Liver|Colorectal Cancer Metastatic to Liver | Phase 1 |
| NCT02706262 | Complex Effects of Dietary Manipulation on Metabolic Function, Inflammation and Health | Obesity|Insulin Resistance | NA |
| NCT05216562 | Efficacy and Safety of EXOSOME-MSC Therapy to Reduce Hyper-inflammation In Moderate COVID-19 Patients | SARS-CoV2 Infection | Phase 2|Phase 3 |
| NCT05775146 | SBRT of Metastases Following Neo-Adjuvant Treatment for Colorectal Cancer with Synchronous Liver Metastases | Colorectal Cancer|Liver Metastasis Colon Cancer | Phase 2 |
| NCT02737267 | Development of a Nutrigenetic Test for Personalized Prescription of Body Weight Loss Diets (Obekit) | Body Weight Changes | NA |
| NCT05524974 | Clinical Study of Camrelizumab, Apatinib Mesylate and Nab-paclitaxel Combined with Oxplatin and S-1 in the Neoadjuvant Treatment of Locally Advanced Gastric Cancer With Different Genotypes | Locally Advanced Gastric Cancer | Phase 2 |
| NCT06116903 | Clinical Relevance of Detecting Molecular Abnormalities in Glial Tumor Exosomes | Glioma | NA |
| NCT04664738 | PEP on a Skin Graft Donor Site Wound | Skin Graft | Phase 1 |
| NCT04530890 | Interest of Circulating Tumor DNA in Digestive and Gynecologic/Breast Cancer | Breast Cancer|Digestive Cancer|Gynecologic Cancer|Circulating Tumor DNA|Exosomes | NA |
| NCT02565264 | Effect of Plasma Derived Exosomes on Cutaneous Wound Healing | Ulcer | Early Phase 1 |
| NCT04542902 | Non-coding RNAs Analysis of Eosinophil Subtypes in Asthma | Allergic Asthma|Severe Eosinophilic Asthma | NA |
| NCT02662621 | Pilot Study with the Aim to Quantify a Stress Protein in the Blood and in the Urine for the Monitoring and Early Diagnosis of Malignant Solid Tumors | Cancer | NA |
| NCT05813379 | Mesenchymal Stem Cells Derived Exosomes in Skin Rejuvenation | Anti-Aging | Phase 1|Phase 2 |
| NCT03255408 | Cerebral Blood Flow and Ventilatory Responses During Sleep in Normoxia and Intermittent Hypoxia | Obstructive Sleep Apnea of Adult|Hypoxia, Brain|Sleep Apnea|Sleep Disorder|Stroke|Blood Pressure|Endothelial Dysfunction|Oxidative Stress | Phase 1|Phase 2 |
| NCT05043181 | Exosome-based Nanoplatform for Ldlr mRNA Delivery in FH | Familial Hypercholesterolemia | Phase 1 |
| NCT05110781 | Atezolizumab Before Surgery for the Treatment of Regionally Metastatic Head and Neck Squamous Cell Cancer with an Unknown or Historic Primary Site | Locally Advanced Cutaneous Squamous Cell Carcinoma of the Head and Neck|Resectable Cutaneous Squamous-Cell Carcinoma of the Head and Neck|Stage III Cutaneous Squamous Cell Carcinoma of the Head and Neck AJCC v8 | Phase 2 |
| NCT05243381 | Inflammation, NK Cells, Antisense Protein and Exosomes, and Correlation with Immune Response During HIV Infection | HIV Infections | NA |
| NCT05373381 | The KetoGlioma (Ketogenic Glioma) Study | Glioma | NA |
| NCT03202212 | Effect of Mixed On-line Hemodiafiltration on Circulating Markers of Inflammation and Vascular Dysfunction | Chronic Kidney Failure|Dialysis-Related Complication | Phase 1|Phase 2 |
| NCT01811381 | Curcumin and Yoga Therapy for Those at Risk for Alzheimer’s Disease | Mild Cognitive Impairment | Phase 2 |
| NCT03459703 | Effect of Time-Restricted Feeding on Fat Loss and Cardiometabolic Risk Factors in Overweight Adults | Obesity | NA |
| NCT05624203 | Clinical Efficacy of Extracorporeal Cardiac Shock Wave Therapy in Patients with Ischemia-reperfusion Injury | Myocardial Reperfusion Injury|Treatment Outcome|Prognosis|ST Elevation Myocardial Infarction | NA |
| NCT04235023 | PTP1B Implication in the Vascular Dysfunction Associated with Obstructive Sleep Apnea | Sleep Apnea|Inflammation|Atherosclerosis | NA |
| NCT05480150 | Chinese Longitudinal and Systematic Study of Bioplar Disorder | Major Depressive Disorder|Bipolar Disorder, Mixed|Affective; Disorder, Organic | NA |
| NCT05832255 | An Investigation of Psilocybin on Behavioural and Cognitive Symptoms of Adults with Fragile X Syndrome | Fragile X Syndrome|Behavior|Cognitive Dysfunction | Phase 2 |
| NCT06245746 | UCMSC-Exo for Chemotherapy-induced Myelosuppression in Acute Myeloid Leukemia | Acute Myeloid Leukemia|Neutropenia|Anemia|Thrombocytopenia|Infections|Bleeding | Phase 1 |
| NCT04453046 | Hemopurifier Plus Pembrolizumab in Head and Neck Cancer | Squamous Cell Carcinoma of the Head and Neck | NA |
| NCT04142138 | When the Kidney Reacts to Nutritional Changes | Prehypertension | NA |
| NCT05833568 | Five-day 20-min 10-Hz tACS in Patients with a Disorder of Consciousness | Brain Injury Traumatic Severe|Disorder of Consciousness|Brain Injuries | NA |
| NCT02977468 | Effects of MK-3475 (Pembrolizumab) on the Breast Tumor Microenvironment in Triple Negative Breast Cancer | Triple Negative Breast Cancer | Phase 1 |
| NCT06236568 | Impact of Graft Reconditioning with Hypothermic Machine Perfusion on HCC Recurrence After Liver Transplantation | Hepatocellular Carcinoma|Liver Transplant; Complications | NA |
| NCT02748369 | In vivo Assessment of Cellular Metabolism in Humans | Normal Cellular Metabolism | Phase 1 |
| NCT04500769 | Training Induced Muscle Exosome Release | Metabolism | NA |
| NCT02051101 | Pathogenic Mechanisms of Port Wine Stain and Repository of Port Wine Stain Biopsy Samples | Port-Wine Stain | NA |
| NCT04602104 | A Clinical Study of Mesenchymal Stem Cell Exosomes Nebulizer for the Treatment of ARDS | Acute Respiratory Distress Syndrome | Phase 1|Phase 2 |
| NCT04491240 | Evaluation of Safety and Efficiency of Method of Exosome Inhalation in SARS-CoV-2 Associated Pneumonia. | COVID-19|SARS-CoV-2 PNEUMONIA|COVID-19 | Phase 1|Phase 2 |
| NCT04653740 | Omic Technologies to Track Resistance to Palbociclib in Metastatic Breast Cancer | Advanced Breast Cancer | NA |
| NCT03096340 | Safety and Pharmacokinetic Study of IT-141 in Monotherapy in Patients with Advanced Cancer | Cancer|Neoplasms|Tumors|Refractory Solid Tumors|Recurrent Solid Tumors | Phase 1 |
| NCT03478410 | Role of Exosomes Derived from Epicardial Fat in Atrial Fibrillation | Atrial Fibrillation | NA |
| NCT06138210 | The Effect of GD-iExo-003 in Acute Ischemic Stroke | Acute Ischemic Stroke | Phase 1 |
| NCT05787288 | A Clinical Study on Safety and Effectiveness of Mesenchymal Stem Cell Exosomes for the Treatment of COVID-19. | COVID-19 Pneumonia | Early Phase 1 |
| NCT04965961 | The Effect of Micro-doses Erytropoietin on Exercise Capacity in Male and Females | Sports Drug Abuse | NA |
| NCT03384433 | Allogenic Mesenchymal Stem Cell Derived Exosome in Patients with Acute Ischemic Stroke | Cerebrovascular Disorders | Phase 1|Phase 2 |
| NCT06319287 | Phase 2a Multi-Center Prospective, Randomized Trial to Evaluate the Safety & Efficacy of Topical PEP-TISSEEL for Diabetic Foot Ulcers (DFU) | Diabetic Foot Ulcer | Phase 2 |
| NCT04276987 | A Pilot Clinical Study on Inhalation of Mesenchymal Stem Cells Exosomes Treating Severe Novel Coronavirus Pneumonia | Coronavirus | Phase 1 |
| NCT06051461 | Deciphering the Role of Dietary Fatty Acids on Extracellular Vesicles-mediated Intercellular Communication | Obesity|Metabolic Syndrome|Metabolic Disorder|Inflammation|Immune System and Related Disorders | NA |
| NCT06239207 | Efficacy and Safety of Exosomes Versus Platelet Rich Plasma in Patients of Androgenetic Alopecia | Androgenetic Alopecia | Phase 2 |
| NCT05933707 | Small Extracellular Vesicles and Insulin Action | Obesity|Insulin Resistance|Metabolically Healthy Obesity|Obesity, Metabolically Benign | NA |
| NCT01159288 | Trial of a Vaccination with Tumor Antigen-loaded Dendritic Cell-derived Exosomes | Non-Small-Cell Lung Cancer | Phase 2 |
| NCT04536688 | A Study of RGLS4326 in Patients with Autosomal Dominant Polycystic Kidney Disease | Polycystic Kidney Disease, Autosomal Dominant | Phase 1 |
| NCT05060107 | Intra-articular Injection of MSC-derived Exosomes in Knee Osteoarthritis (ExoOA-1) | Osteoarthritis, Knee | Phase 1 |
| NCT04250493 | Insulin Resistance in Multiple System Atrophy | Multiple System Atrophy | NA |
| NCT05523011 | Safety and Tolerability Study of MSC Exosome Ointment | Psoriasis | Phase 1 |
| NCT05669261 | Treatment of Long COVID Symptoms Utilizing Autologous Stem Cells Following COVID-19 Infection | Long COVID | Phase 1 |
| NCT05499156 | Safety of Injection of Placental Mesenchymal Stem Cell Derived Exosomes for Treatment of Resistant Perianal Fistula in Crohn’s Patients | Perianal Fistula in Patients with Crohn’s Disease | Phase 1|Phase 2 |
| NCT02507583 | Antisense102: Pilot Immunotherapy for Newly Diagnosed Malignant Glioma | Malignant Glioma|Neoplasms | Phase 1 |
| NCT03660683 | Effect of Saxagliptin and Dapagliflozin on Endothelial Progenitor Cell in Patients with Type 2 Diabetes Mellitus | Diabetes Mellitus, Type 2|Cardiovascular diseases | Phase 4 |
| NCT05318898 | Effect of Dietary Protein on the Regulation of Exosome microRNA Expression in Patients with Insulin Resistance. | Insulin Resistance | NA |
| NCT06244849 | Toward a Better Understanding of the Autophagy Machinery for the Identification of Potential Novel Biomarkers and Therapeutic Targets in Crohn’s Disease - TOPIC Study | Crohn’s Disease | NA |
| NCT03824275 | 18F-DCFPyL Positron Emission Tomography (PET)/Computed Tomography (CT) in Men with Prostate Cancer | Prostatic Neoplasms | Phase 2|Phase 3 |
| NCT05864534 | Phase 2a Immune Modulation with Ultrasound for Newly Diagnosed Glioblastoma | Newly Diagnosed Glioblastoma|Glioblastoma, Isocitric Dehydrogenase (IDH)-Wildtype|Gliosarcoma|Glioblastoma Multiforme | Phase 2 |
| NCT04202770 | Focused Ultrasound and Exosomes to Treat Depression, Anxiety, and Dementias | Refractory Depression|Anxiety disorders|neurodegenerative diseases | NA |
| NCT01668849 | Edible Plant Exosome Ability to Prevent Oral Mucositis Associated with Chemoradiation Treatment of Head and Neck Cancer | Head and Neck Cancer|Oral Mucositis | Phase 1 |
| NCT05843799 | A Study to Evaluate the Safety and Tolerability of ILB-202 | Healthy | Phase 1 |
| NCT05228899 | Zofin to Treat COVID-19 Long Haulers | COVID-19 | Phase 1|Phase 2 |
| NCT04270006 | Evaluation of Adipose Derived Stem Cells Exo.in Treatment of Periodontitis | Periodontitis | Early Phase 1 |
| NCT05259449 | Efficacy of Educational Nutrition and Exercise on the Regulation of Appetite Through Exosomes in Type 2 Diabetics | Diabetes Mellitus, Type 2 | NA |
| NCT02890849 | Clinical Research for the Consistency Analysis of PD-L1 in Cancer Tissue and Plasma Exosome | NSCLC | NA |
| NCT02823613 | The Influence of High and Low Salt on Exosomes in the Urine | Healthy | NA |
| NCT05871359 | Transcranial Direct Current Stimulation and Dual Tasks | Parkinson’s Disease | NA |
| NCT03437759 | MSC-Exos Promote Healing of MHs | Macular Holes | Early Phase 1 |
| NCT03419000 | Circulating microRNAs as Biomarkers of Respiratory Dysfunction in Patients with Refractory Epilepsy | Drug-Resistant Epilepsy | NA |
| NCT04427475 | Prediction of Immunotherapeutic Effect of Advanced Non-small Cell Lung Cancer | NSCLC Patients | NA |
| NCT04602442 | Safety and Efficiency of Method of Exosome Inhalation in COVID-19 Associated Pneumonia | COVID-19|SARS-CoV-2 PNEUMONIA|COVID-19 | Phase 2 |
| NCT03837470 | Evaluation of Renal Sodium Excretion After Salt Loading in Heart Failure with Preserved Ejection Fraction | Heart Failure with Preserved Ejection Fraction | Early Phase 1 |
| NCT03083678 | Afatinib in Locally Advanced and Metastatic Chordoma | Chordoma | Phase 2 |
| NCT05977088 | Prediction of Effectiveness of rTMS Application in Alzheimer’s Patients | Alzheimer’s Disease | NA |
| NCT02706288 | Effects of a Calorie Restricted, Very Low-Fat Plant-based Diet and Multi-component Exercise Program on Metabolic Health | Obesity|Insulin Resistance | NA |
| NCT06391307 | The Role of Mesenchymal Stem Cell and Exosome in Treating Pilonidal Sinus Disease in Children | Pilonidal Sinus|Pilonidal Disease | NA |
| NCT04636788 | Circulating Extracellular Exosomal Small RNA as Potential Biomarker for Human Pancreatic Cancer | Pancreas Adenocarcinoma | NA |
| NCT03700515 | Exosome Proteomics to Detect EPO | Healthy | NA |
| NCT05387278 | Safety and Effectiveness of Placental Derived Exosomes and Umbilical Cord Mesenchymal Stem Cells in Moderate to Severe Acute Respiratory Distress Syndrome (ARDS) Associated with the Novel Corona Virus Infection (COVID-19) | COVID-19 Acute Respiratory Distress Syndrome|Respiratory Distress Syndrome | Phase 1 |
| NCT05834413 | Clinical Study on the Prevention of Driver Gene Negative II-IIIa Lung Cancer Recurrence and Metastasis by Staged Chinese Herbal Medicine Combined With Chemotherapy and Immune Checkpoint Inhibitors | Lung Cancer | NA |
| NCT04389385 | COVID-19 Specific T Cell Derived Exosomes (CSTC-Exo) | Corona Virus Infection|Pneumonia | Phase 1 |
| NCT05808400 | Safety and Efficacy of Umbilical Cord Mesenchymal Stem Cell Exosomes in Treating Chronic Cough After COVID-19 | Long COVID-19 Syndrome | Early Phase 1 |
| NCT04356300 | Exosome of Mesenchymal Stem Cells for Multiple Organ Dysfunction Syndrome After Surgical Repair of Acute Type A Aortic Dissection | Multiple Organ Failure | NA |
| NCT03537599 | Daratumumab and Donor Lymphocyte Infusion in Treating Participants with Relapsed Acute Myeloid Leukemia After Stem Cell Transplant | Minimal Residual Disease|Recurrent Acute Myeloid Leukemia with Myelodysplasia-Related Changes|Recurrent Adult Acute Myeloid Leukemia|Recurrent Childhood Acute Myeloid Leukemia | Phase 1|Phase 2 |
| NCT04544215 | A Clinical Study of Mesenchymal Progenitor Cell Exosomes Nebulizer for the Treatment of Pulmonary Infection | Drug-resistant | Phase 1|Phase 2 |
| NCT03627611 | Identification of Non-responders to Levothyroxine Therapy | Hypothyroidism|Biomarkers|Endocrine System Diseases | Phase 2 |
| NCT04202783 | The Use of Exosomes in Craniofacial Neuralgia | Neuralgia | NA |
| NCT05886205 | Induced Pluripotent Stem Cell Derived Exosomes Nasal Drops for the Treatment of Refractory Focal Epilepsy | Refractory Focal Epilepsy | Early Phase 1 |
| NCT04902183 | Safety and Efficacy of Exosomes Overexpressing CD24 in Two Doses for Patients with Moderate or Severe COVID-19 | COVID-19 | Phase 2 |
| NCT02535247 | Study of MK-3475 Alone or in Combination with Copanlisib in Relapsed or Refractory NK and T-cell Non-Hodgkin Lymphoma | Lymphoma, T-Cell, Peripheral | Phase 1|Phase 2 |
| NCT03228277 | Olmutinib Trial in T790M (+) NSCLC Patients Detected by Liquid Biopsy Using BALF Extracellular Vesicular DNA | Non-Small-Cell Lung Cancer | Phase 2 |
| NCT04313647 | A Tolerance Clinical Study on Aerosol Inhalation of Mesenchymal Stem Cells Exosomes in Healthy Volunteers | Healthy | Phase 1 |
| NCT04623671 | Intravenous Infusion of CAP-1002 in Patients With COVID-19 | COVID-19 | Phase 2 |
| NCT00285805 | The Influence of Rosiglitazone on the Diuretic Effect of Furosemide and Amiloride | Insulin Resistance | NA |
| NCT04177498 | Rigosertib in Patients with Recessive Dystrophic Epidermolysis Bullosa Associated SCC | Recessive Dystrophic Epidermolysis Bullosa | Early Phase 1 |
| NCT01629498 | Image-Guided, Intensity-Modulated Photon or Proton Beam Radiation Therapy in Treating Patients with Stage II-IIIB Non-small Cell Lung Cancer | Recurrent Lung Non-Small-Cell Carcinoma|Stage II Non-Small-Cell Lung Cancer AJCC v7|Stage IIA Non-Small-Cell Lung Carcinoma AJCC v7|Stage IIB Non-Small-Cell Lung Carcinoma AJCC v7|Stage IIIA Non-Small-Cell Lung Cancer AJCC v7|Stage IIIB Lung Non-Small-Cell Cancer AJCC v7 | Phase 1|Phase 2 |
| NCT03927898 | Phase II Study of Toripalimab Plus Stereotactic Body Radiotherapy in Colorectal Cancer Patients with Oligometastasis | Metastatic Colorectal Cancer | Phase 2 |
| NCT05947747 | Safety and Efficacy of EXO-CD24 in Preventing Clinical Deterioration in Patients with Mild-Moderate ARDS | ARDS | Phase 2 |
| NCT02594345 | Effect of Exosomes Derived from Red Blood Cell Units on Platelet Function and Blood Coagulation | Blood Coagulation|Platelet Function | NA |
| NCT04384445 | Zofin (Organicell Flow) for Patients With COVID-19 | Corona Virus Infection|COVID-19|SARS|Acute Respiratory Distress Syndrome | Phase 1|Phase2 |
| NCT04298398 | Impact of Group Psychological Interventions on Extracellular Vesicles in People Who Had Cancer | Cancer | NA |
| NCT03109847 | Metformin Hydrochloride in Mitigating Side Effects of Radioactive Iodine Treatment in Patients with Differentiated Thyroid Cancer | Thyroid | Phase 2 |
| NCT04350177 | A Study to Assess Single and Multiple Doses of IkT-148009 in Healthy Elderly Participants and Parkinson’s Patients | Healthy Elderly|Parkinson’s Disease | Phase 1 |
| NCT05559177 | An Open, Dose-escalation Clinical Study of Chimeric Exosomal Tumor Vaccines for Recurrent or Metastatic Bladder Cancer | Recurrent or Metastatic Bladder Cancer | Early Phase 1 |
| NCT05607654 | The Mechanisms of Underlying Accelerated Repetitive Transcranial Magnetic Stimulation for Treatment-resistant Depression | Treatment-Resistant Depression | NA |
| NCT06221787 | Stem Cell Derived Exosomes in the Treatment of Melasma and Its Percutaneous Penetration | Melasma | NA |
| NCT02921854 | Detection of Circulating Biomarkers of Immunogenic Cell Death | Non-Small-Cell Lung Cancer | NA |
| NCT02310451 | Study of Molecular Mechanisms Implicated in the Pathogenesis of Melanoma. Role of Exosomes | Metastatic Melanoma | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharma, A.; Yadav, A.; Nandy, A.; Ghatak, S. Insight into the Functional Dynamics and Challenges of Exosomes in Pharmaceutical Innovation and Precision Medicine. Pharmaceutics 2024, 16, 709. https://doi.org/10.3390/pharmaceutics16060709
Sharma A, Yadav A, Nandy A, Ghatak S. Insight into the Functional Dynamics and Challenges of Exosomes in Pharmaceutical Innovation and Precision Medicine. Pharmaceutics. 2024; 16(6):709. https://doi.org/10.3390/pharmaceutics16060709
Chicago/Turabian StyleSharma, Anu, Anita Yadav, Aparajita Nandy, and Subhadip Ghatak. 2024. "Insight into the Functional Dynamics and Challenges of Exosomes in Pharmaceutical Innovation and Precision Medicine" Pharmaceutics 16, no. 6: 709. https://doi.org/10.3390/pharmaceutics16060709
APA StyleSharma, A., Yadav, A., Nandy, A., & Ghatak, S. (2024). Insight into the Functional Dynamics and Challenges of Exosomes in Pharmaceutical Innovation and Precision Medicine. Pharmaceutics, 16(6), 709. https://doi.org/10.3390/pharmaceutics16060709






