Advances in Liposomal Interleukin and Liposomal Interleukin Gene Therapy for Cancer: A Comprehensive Review of Preclinical Studies
Abstract
1. Introduction
The Role of Interleukins (ILs) in Advancing Cancer Treatment
2. Clinical Potential of Liposomal Interleukin Formulations
3. Overview of Liposomal Nanoformulations
3.1. Methods of Liposome Preparation
3.2. Thin-Film Hydration Method
3.3. Alternative Methods for Liposome Preparation
3.4. Role of Excipients in Enhancing Liposomal Stability
3.5. Cationic Liposomes for Gene Delivery
3.6. Toxicity Studies of Liposomal Formulations
3.7. Liposomal Interleukin Formulations
4. Overview of Liposomal Drug Delivery Systems
5. Liposomal Interleukin Therapy
6. Preclinical Studies on Liposomal Interleukin Therapy
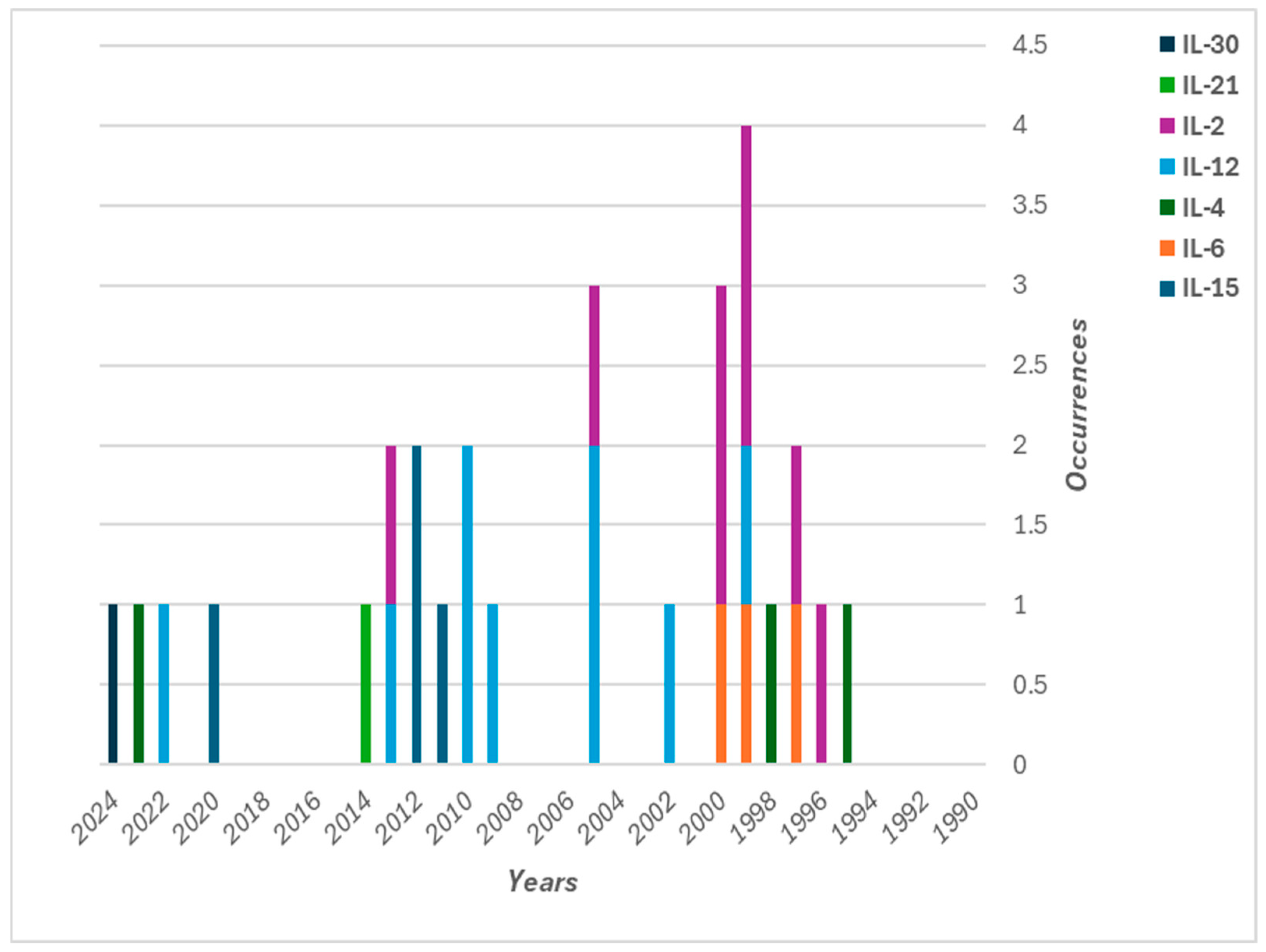
6.1. Liposomal IL-2 for Cancer Treatment in Preclinical Studies
6.2. Liposomal IL-1, IL-12, IL-13, and IL-15
7. Liposomal Interleukin Gene Therapy for Cancer Treatment
7.1. Liposomal IL-2 Gene Therapy
7.2. Liposomal IL-4 and IL-12 Gene Therapy
7.3. Liposomal IL-15, IL-21, and IL-30 Gene Therapy
8. Challenges in Liposomal Drug Delivery Systems and Future Perspectives
9. Methodology
9.1. Search Strategy
9.2. Inclusion and Exclusion Criteria
9.2.1. Inclusion Criteria
- Studies focusing on liposomal formulations of interleukins in cancer therapy.
- Preclinical studies utilizing in vitro or in vivo approaches.
- Studies addressing the development, optimization, or biological effects of liposomal interleukin delivery systems or gene therapy.
- Articles present original research, including pharmacokinetics, pharmacodynamics, and therapeutic outcomes.
9.2.2. Exclusion Criteria
- Clinical trials and meta-analyses.
- Studies not related to cancer treatment.
- Research focuses on non-liposomal formulations of interleukins.
9.2.3. Data Extraction and Analysis
- Study design and objectives.
- Type of interleukin and liposomal formulation.
- Experimental models (e.g., cell lines, animal models).
- Methods of gene delivery (if applicable).
- Pharmacological and therapeutic outcomes.
- Adverse effects and safety profile.
9.2.4. Data Synthesis
- Overview of liposomal drug delivery systems;
- Liposomal interleukin therapy;
- Preclinical studies on liposomal interleukin therapy;
- Liposomal interleukin gene therapy for cancer treatment.
10. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef] [PubMed]
- Danhier, F.; Feron, O.; Préat, V. To exploit the tumor microenvironment: Passive and active tumor targeting of nanocarriers for anti-cancer drug delivery. J. Control Release 2010, 148, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, A.H.; Almatroudi, A.; Allemailem, K.S.; Alwanian, W.M.; Alharbi, B.F.; Alrumaihi, F.; Khan, A.A.; Almatroodi, S.A. Myricetin: A significant emphasis on its anticancer potential via the modulation of inflammation and signal transduction pathways. Int. J. Mol. Sci. 2023, 24, 9665. [Google Scholar] [CrossRef]
- Chidambaram, M.; Manavalan, R.; Kathiresan, K. Nanotherapeutics to overcome conventional cancer chemotherapy limitations. J. Pharm. Sci. 2011, 14, 67–77. [Google Scholar] [CrossRef]
- Chakraborty, S.; Rahman, T. The difficulties in cancer treatment. Ecancermedicalscience 2012, 6, ed16. [Google Scholar] [CrossRef] [PubMed]
- Wayteck, L.; Breckpot, K.; Demeester, J.; De Smedt, S.C.; Raemdonck, K. A personalized view on cancer immunotherapy. Cancer Lett. 2014, 352, 113–125. [Google Scholar] [CrossRef]
- Ling, S.P.; Ming, L.C.; Dhaliwal, J.S.; Gupta, M.; Ardianto, C.; Goh, K.W.; Hussain, Z.; Shafqat, N. Role of immunotherapy in the treatment of cancer: A systematic review. Cancers 2022, 14, 5205. [Google Scholar] [CrossRef]
- Shimu, A.S.; Wei, H.X.; Li, Q.; Zheng, X.; Li, B. The new progress in cancer immunotherapy. Clin. Exp. Med. 2023, 23, 553–567. [Google Scholar] [CrossRef]
- Conlon, K.C.; Miljkovic, M.D.; Waldmann, T.A. Cytokines in the treatment of cancer. J. Interferon Cytokine Res. 2019, 39, 6–21. [Google Scholar] [CrossRef]
- Propper, D.J.; Balkwill, F.R. Harnessing cytokines and chemokines for cancer therapy. Nat. Rev. Clin. Oncol. 2022, 19, 237–253. [Google Scholar] [CrossRef]
- Lee, S.; Margolin, K. Cytokines in cancer immunotherapy. Cancers 2011, 3, 3856–3893. [Google Scholar] [CrossRef] [PubMed]
- Justiz Vaillant, A.A.; Qurie, A. Interleukin; StatPearls: Treasure Island, FL, USA, 2024. [Google Scholar]
- Waldmann, T.A. Cytokines in cancer immunotherapy. Cold Spring Harb. Perspect. Biol. 2018, 10, a028472. [Google Scholar] [CrossRef]
- Rosenberg, S.A.; Yang, J.C.; Topalian, S.L.; Schwartzentruber, D.J.; Weber, J.S.; Parkinson, D.R.; Seipp, C.A.; Einhorn, J.H.; White, D.E. Treatment of 283 consecutive patients with metastatic melanoma or renal cell cancer using high-dose bolus interleukin 2. JAMA 1994, 271, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, S.A.; Lotze, M.T.; Yang, J.C.; Aebersold, P.M.; Linehan, W.M.; Seipp, C.A.; White, D.E. Experience with the use of high-dose interleukin-2 in the treatment of 652 cancer patients. Ann. Surg. 1989, 210, 474–484. [Google Scholar] [CrossRef]
- Radi, H.; Ferdosi-Shahandashti, E.; Kardar, G.A.; Hafezi, N. An updated review of interleukin-2 therapy in cancer and autoimmune diseases. J. Interferon Cytokine Res. 2024, 44, 143–157. [Google Scholar] [CrossRef]
- Liu, J.Q.; Zhu, J.; Hu, A.; Zhang, A.; Yang, C.; Yu, J.; Ghoshal, K.; Basu, S.; Bai, X.-F. Is AAV-delivered IL-27 a potential immunotherapeutic for cancer? Am. J. Cancer Res. 2020, 10, 3565–3574. [Google Scholar] [PubMed]
- Fyfe, G.; Fisher, R.I.; Rosenberg, S.A.; Sznol, M.; Parkinson, D.R.; Louie, A.C. Results of treatment of 255 patients with metastatic renal cell carcinoma who received high-dose recombinant interleukin-2 therapy. J. Clin. Oncol. 1995, 13, 688–696. [Google Scholar] [CrossRef]
- Liang, X.; De Vera, M.E.; Buchser, W.J.; Romo de Vivar Chavez, A.; Loughran, P.; Beer Stolz, D.; Basse, P.; Wang, T.; Van Houten, B.; Zeh, H.J., 3rd; et al. Inhibiting systemic autophagy during interleukin 2 immunotherapy promotes long-term tumor regression. Cancer Res. 2012, 72, 2791–2801. [Google Scholar] [CrossRef]
- Milling, L.; Zhang, Y.; Irvine, D.J. Delivering safer immunotherapies for cancer. Adv. Drug Deliv. Rev. 2017, 114, 79–101. [Google Scholar] [CrossRef]
- Ryffel, B. Interleukin-12: Role of interferon-gamma in IL-12 adverse effects. Clin. Immunol. Immunopathol. 1997, 83, 18–20. [Google Scholar] [CrossRef] [PubMed]
- Colombo, M.P.; Trinchieri, G. Interleukin-12 in anti-tumor immunity and immunotherapy. Cytokine Growth Factor. Rev. 2002, 13, 155–168. [Google Scholar] [CrossRef]
- Salem, M.L.; Gillanders, W.E.; Kadima, A.N.; El-Naggar, S.; Rubinstein, M.P.; Demcheva, M.; Vournakis, J.N.; Cole, D.J. Review: Novel nonviral delivery approaches for interleukin-12 protein and gene systems: Curbing toxicity and enhancing adjuvant activity. J. Interferon Cytokine Res. 2006, 26, 593–608. [Google Scholar] [CrossRef]
- Adler, A.; Schachter, J.; Barenholz, Y.; Bar, L.K.; Klein, T.; Korytnaya, R.; Sulkes, A.; Michowiz, R.; Cohen, Y.; Kedar, I. Allogeneic human liposomal melanoma vaccine with or without IL-2 in metastatic melanoma patients: Clinical and immunobiological effects. Cancer Biother. 1995, 10, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Ren, H.; Boulikas, T.; Lundstrom, K.; Söling, A.; Warnke, P.C.; Rainov, N.G. Immunogene therapy of recurrent glioblastoma multiforme with a liposomally encapsulated replication-incompetent Semliki Forest virus vector carrying the human interleukin-12 gene—A phase I/II clinical protocol. J. Neurooncol 2003, 64, 147–154. [Google Scholar] [CrossRef]
- Skubitz, K.M.; Anderson, P.M. Inhalational interleukin-2 liposomes for pulmonary metastases: A phase I clinical trial. Anticancer. Drugs 2000, 11, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Ishida, T.; Harashima, H.; Kiwada, H. Liposome Clearance. Biosci. Rep. 2002, 22, 197–224. [Google Scholar] [CrossRef]
- Kraft, J.C.; Freeling, J.P.; Wang, Z.; Ho, R.J.Y. Emerging Research and Clinical Development Trends of Liposome and Lipid Nanoparticle Drug Delivery Systems. J. Pharm. Sci. 2014, 103, 29–52. [Google Scholar] [CrossRef]
- Allen, T.M.; Cullis, P.R. Liposomal drug delivery systems: From concept to clinical applications. Adv. Drug Deliv. Rev. 2013, 65, 36–48. [Google Scholar] [CrossRef]
- Akbarzadeh, A.; Rezaei-Sadabady, R.; Davaran, S.; Joo, S.W.; Zarghami, N.; Hanifehpour, Y.; Samiei, M.; Kouhi, M.; Nejati-Koshki, K. Liposome: Classification, Preparation, and Applications. Nanoscale Res. Lett. 2013, 8, 102. [Google Scholar] [CrossRef]
- Sercombe, L.; Veerati, T.; Moheimani, F.; Wu, S.Y.; Sood, A.K.; Hua, S. Advances and Challenges of Liposome-Assisted Drug Delivery. Front. Pharmacol. 2015, 6, 286. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, D.; Kiselev, M.A. Methods of Liposomes Preparation: Formation and Control Factors of Versatile Nanocarriers for Biomedical and Nanomedicine Application. Pharmaceutics 2022, 14, 543. [Google Scholar] [CrossRef] [PubMed]
- Wagner, A.; Vorauer-Uhl, K. Liposome technology for industrial purposes. J. Drug Deliv. 2011, 2011, 591325. [Google Scholar] [CrossRef] [PubMed]
- Lasic, D.D. Liposomes: From Physics to Application; Elsevier Science Publishers B.V.: Amsterdam, The Netherlands, 1993; p. 575. [Google Scholar]
- Šturm, L.; Ulrih, N.P. Basic Methods for Preparation of Liposomes and Studying Their Interactions with Different Compounds, with the Emphasis on Polyphenols. Int. J. Mol. Sci. 2021, 22, 6547. [Google Scholar] [CrossRef]
- Lasch, J.; Weissig, V.; Brandl, M. Preparation of Liposomes. In Liposomes—A Practical Approach, 2nd ed.; Torchilin, V.P., Weissig, V., Eds.; Oxford University Press: Oxford, UK, 2003; pp. 3–30. [Google Scholar]
- Johnston, D.; Reynolds, S.R.; Bystryn, J.C. Interleukin-2/Liposomes Potentiate Immune Responses to a Soluble Protein Cancer Vaccine in Mice. Cancer Immunol. Immunother. 2006, 55, 412–419. [Google Scholar] [CrossRef]
- Pasarin, D.; Ghizdareanu, A.-I.; Enascuta, C.E.; Matei, C.B.; Bilbie, C.; Paraschiv-Palada, L.; Veres, P.-A. Coating Materials to Increase the Stability of Liposomes. Polymers 2023, 15, 782. [Google Scholar] [CrossRef]
- Subramanian, P. Lipid-Based Nanocarrier System for the Effective Delivery of Nutraceuticals. Molecules 2021, 26, 5510. [Google Scholar] [CrossRef]
- Lee, D.E.; Lew, M.G.; Woodbury, D.J. Vesicle Fusion to Planar Membranes Is Enhanced by Cholesterol and Low Temperature. Chem. Phys. Lipids 2013, 166, 45–54. [Google Scholar] [CrossRef]
- Gibis, M.; Zeeb, B.; Weiss, J. Formation, Characterization, and Stability of Encapsulated Hibiscus Extract in Multilayered Liposomes. Food Hydrocoll. 2014, 38, 28–39. [Google Scholar] [CrossRef]
- Sepúlveda, C.T.; Alemán, A.; Zapata, J.E.; Montero, M.P.; Gómez-Guillén, M.C. Characterization and Storage Stability of Spray Dried Soy-Rapeseed Lecithin/Trehalose Liposomes Loaded with a Tilapia Viscera Hydrolysate. Innov. Food Sci. Emerg. Technol. 2021, 71, 102708. [Google Scholar] [CrossRef]
- Boafo, G.F.; Magar, K.T.; Ekpo, M.D.; Qian, W.; Tan, S.; Chen, C. The Role of Cryoprotective Agents in Liposome Stabilization and Preservation. Int. J. Mol. Sci. 2022, 23, 12487. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Ye, A.; Han, F.; Han, J. Advances and Challenges in Liposome Digestion: Surface Interaction, Biological Fate, and GIT Modeling. Adv. Colloid. Interface Sci. 2019, 263, 52–67. [Google Scholar] [CrossRef]
- Shao, P.; Wang, P.; Niu, B.; Kang, J. Environmental Stress Stability of Pectin-Stabilized Resveratrol Liposomes with Different Degrees of Esterification. Int. J. Biol. Macromol. 2018, 119, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Tamaddon, L.; Mohamadi, N.; Bavarsad, N. Preparation and Characterization of Mucoadhesive Loratadine Nanoliposomes for Intranasal Administration. Turk. J. Pharm. Sci. 2021, 18, 492–497. [Google Scholar] [CrossRef] [PubMed]
- Zamani Ghaleshahi, A.; Rajabzadeh, G.; Ezzatpanah, H. Influence of Sodium Alginate and Genipin on Stability of Chitosome Containing Perilla Oil in Model and Real Drink. Eur. J. Lipid Sci. Technol. 2020, 122, 1900438. [Google Scholar] [CrossRef]
- Immordino, M.L.; Dosio, F.; Cattel, L. Stealth Liposomes: Review of the Basic Science, Rationale, and Clinical Applications, Existing and Potential. Int. J. Nanomed. 2006, 1, 297–315. [Google Scholar]
- Tenchov, R.; Sasso, J.M.; Zhou, Q.A. PEGylated Lipid Nanoparticle Formulations: Immunological Safety and Efficiency Perspective. Bioconjug Chem. 2023, 34, 941–960. [Google Scholar] [CrossRef]
- Davis, F.F. The origin of pegnology. Adv. Drug Deliv. Rev. 2002, 54, 457–458. [Google Scholar] [CrossRef]
- Torchilin, V.P.; Klibanov, A.L.; Huang, L.; O’Donnell, S.; Nossiff, N.D.; Khaw, B.A. Targeted accumulation of polyethylene glycol-coated immunoliposomes in infarcted rabbit myocardium. FASEB J. 1992, 6, 2716–2719. [Google Scholar] [CrossRef]
- Northfelt, D.W.; Martin, F.J.; Working, P.; Volberding, P.A.; Russell, J.; Newman, M.; Amantea, M.A.; Kaplan, L.D. Doxorubicin encapsulated in liposomes containing surface-bound polyethylene glycol: Pharmacokinetics, tumor localization, and safety in patients with AIDS-related Kaposi’s sarcoma. J. Clin. Pharmacol. 1996, 36, 55–63. [Google Scholar] [CrossRef]
- Ishida, T.; Kirchmeier, M.J.; Moase, E.H.; Zalipsky, S.; Allen, T.M. Targeted delivery and triggered release of liposomal doxorubicin enhances cytotoxicity against human B lymphoma cells. Biochim. Biophys. Acta 2001, 1515, 144–158. [Google Scholar] [CrossRef] [PubMed]
- Gabizon, A.; Papahadjopoulos, D. Liposome formulations with prolonged circulation time in blood and enhanced uptake by tumors. Proc. Natl. Acad. Sci. USA 1988, 85, 6949–6953. [Google Scholar] [CrossRef] [PubMed]
- Lasic, D.D.; Martin, F.J.; Gabizon, A.; Huang, S.K.; Papahadjopoulos, D. Sterically stabilized liposomes: A hypothesis on the molecular origin of the extended circulation times. Biochim. Biophys. Acta 1991, 1070, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Woodle, M.C. Surface-modified liposomes: Assessment and characterization for increased stability and prolonged blood circulation. Chem. Phys. Lipids 1993, 64, 249–262. [Google Scholar] [CrossRef]
- Senior, J.; Delgado, C.; Fisher, D.; Tilcock, C.; Gregoriadis, G. Influence of surface hydrophilicity of liposomes on their interaction with plasma protein and clearance from the circulation: Studies with poly(ethylene glycol)-coated vesicles. Biochim. Biophys. Acta 1991, 1062, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Senior, J.H. Fate and behavior of liposomes in vivo: A review of controlling factors. Crit. Rev. Ther. Drug Carr. Syst. 1987, 3, 123–193. [Google Scholar]
- Mastrotto, F.; Brazzale, C.; Bellato, F.; De Martin, S.; Grange, G.; Mahmoudzadeh, M.; Magarkar, A.; Bunker, A.; Salmaso, S.; Caliceti, P. In Vitro and In Vivo Behavior of Liposomes Decorated with PEGs with Different Chemical Features. Mol. Pharm. 2020, 17, 472–487. [Google Scholar] [CrossRef]
- Hatakeyama, H.; Akita, H.; Harashima, H. The Polyethyleneglycol Dilemma: Advantage and Disadvantage of PEGylation of Liposomes for Systemic Genes and Nucleic Acids Delivery to Tumors. Biol. Pharm. Bull. 2013, 36, 892–899. [Google Scholar] [CrossRef] [PubMed]
- Gaber, M.; Medhat, W.; Hany, M.; Saher, N.; Fang, J.-Y.; Elzoghby, A. Protein-Lipid Nanohybrids as Emerging Platforms for Drug and Gene Delivery: Challenges and Outcomes. J. Control. Release 2017, 254, 75–91. [Google Scholar] [CrossRef]
- Taguchi, K.; Okamoto, Y.; Matsumoto, K.; Otagiri, M.; Chuang, V.T.G. When Albumin Meets Liposomes: A Feasible Drug Carrier for Biomedical Applications. Pharmaceuticals 2021, 14, 296. [Google Scholar] [CrossRef]
- Dong, Y.; Dong, P.; Huang, D.; Mei, L.; Xia, Y.; Wang, Z.; Pan, X.; Li, G.; Wu, C. Fabrication and Characterization of Silk Fibroin-Coated Liposomes for Ocular Drug Delivery. Eur. J. Pharm. Biopharm. 2015, 91, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Battogtokh, G.; Joo, Y.; Abuzar, S.M.; Park, H.; Hwang, S.-J. Gelatin Coating for the Improvement of Stability and Cell Uptake of Hydrophobic Drug-Containing Liposomes. Molecules 2022, 27, 1041. [Google Scholar] [CrossRef] [PubMed]
- Mosafer, J.; Sabbaghi, A.-H.; Badiee, A.; Dehghan, S.; Tafaghodi, M. Preparation, Characterization and In Vivo Evaluation of Alginate-Coated Chitosan and Trimethylchitosan Nanoparticles Loaded with PR8 Influenza Virus for Nasal Immunization. Asian J. Pharm. Sci. 2019, 14, 216–221. [Google Scholar] [CrossRef]
- Parchen, G.P.; Jacumazo, J.; Siebert Koop, H.; Biscaia, S.M.P.; Trindade, E.S.; Silveira, J.L.M.; de Freitas, R.A. Modulation of Epidermal Growth Factor Release by Biopolymer-Coated Liposomes. J. Pharm. Sci. 2020, 109, 2294–2301. [Google Scholar] [CrossRef] [PubMed]
- Raj, V.; Raorane, C.J.; Lee, J.-H.; Lee, J. Appraisal of Chitosan-Gum Arabic-Coated Bipolymeric Nanocarriers for Efficient Dye Removal and Eradication of the Plant Pathogen Botrytis cinerea. ACS Appl. Mater. Interfaces 2021, 13, 47354–47370. [Google Scholar] [CrossRef]
- Rezvani, M.; Manca, M.L.; Muntoni, A.; De Gioannis, G.; Pedraz, J.L.; Gutierrez, G.; Matos, M.; Fadda, A.M.; Manconi, M. From Process Effluents to Intestinal Health Promotion: Developing Biopolymer-Whey Liposomes Loaded with Gingerol to Heal Intestinal Wounds and Neutralize Oxidative Stress. Int. J. Pharm. 2022, 613, 121389. [Google Scholar] [CrossRef]
- Shah, V.; Jobanputra, A.; Saxena, B.; Nivsarkar, M. Development and Characterization of Saturated Fatty Acid-Engineered, Silica-Coated Lipid Vesicular System for Effective Oral Delivery of Alfa-Choriogonadotropin. AAPS Pharm. Sci. Tech. 2021, 22, 118. [Google Scholar] [CrossRef] [PubMed]
- Pham, X.-H.; Park, S.-M.; Ham, K.-M.; Kyeong, S.; Son, B.S.; Kim, J.; Hahm, E.; Kim, Y.-H.; Bock, S.; Kim, W.; et al. Synthesis and Application of Silica-Coated Quantum Dots in Biomedicine. Int. J. Mol. Sci. 2021, 22, 10116. [Google Scholar] [CrossRef]
- Wu, S.; Jiang, M.; Mao, H.; Zhao, N.; He, D.; Chen, Q.; Liu, D.; Zhang, W.; Song, X.-M. A Sensitive Cholesterol Electrochemical Biosensor Based on Biomimetic Cerasome and Graphene Quantum Dots. Anal. Bioanal. Chem. 2022, 414, 3593–3603. [Google Scholar] [CrossRef]
- Du, Z.; Munye, M.M.; Tagalakis, A.D.; Manunta, M.D.I.; Hart, S.L. The role of the helper lipid on the DNA transfection efficiency of lipopolyplex formulations. Sci. Rep. 2014, 4, 7107. [Google Scholar] [CrossRef]
- Filipczak, N.; Pan, J.; Yalamarty, S.S.K.; Torchilin, V.P. Recent Advancements in Liposome Technology. Adv. Drug Deliv. Rev. 2020, 156, 4–22. [Google Scholar] [CrossRef] [PubMed]
- Batenjany, M.M.; Boni, L.T.; Guo, Y.; Neville, M.E.; Bansal, S.; Robb, R.J.; Popescu, M.C. The effect of cholesterol in a liposomal Muc1 vaccine. Biochim. Biophys. Acta 2001, 1514, 280–290. [Google Scholar] [CrossRef] [PubMed]
- Demel, R.A.; Kinsky, S.C.; Kinsky, C.B.; van Deenen, L.L. Effects of temperature and cholesterol on the glucose permeability of liposomes prepared with natural and synthetic lecithins. Biochim. Biophys. Acta 1968, 150, 655–665. [Google Scholar] [CrossRef] [PubMed]
- Briuglia, M.-L.; Rotella, C.; McFarlane, A.; Lamprou, D.A. Influence of cholesterol on liposome stability and on in vitro drug release. Drug Deliv. Transl. Res. 2015, 5, 231–242. [Google Scholar] [CrossRef]
- Kirby, C.; Clarke, J.; Gregoriadis, G. Effect of the cholesterol content of small unilamellar liposomes on their stability in vivo and in vitro. Biochem. J. 1980, 186, 591–598. [Google Scholar] [CrossRef]
- Smaby, J.M.; Momsen, M.M.; Brockman, H.L.; Brown, R.E. Phosphatidylcholine acyl unsaturation modulates the decrease in interfacial elasticity induced by cholesterol. Biophys. J. 1997, 73, 1492–1505. [Google Scholar] [CrossRef]
- Misra, S.K.; Naz, S.; Kondaiah, P.; Bhattacharya, S. A cationic cholesterol-based nanocarrier for the delivery of p53-EGFP-C3 plasmid to cancer cells. Biomaterials 2014, 35, 1334–1346. [Google Scholar] [CrossRef]
- Alshehri, A.; Grabowska, A.; Stolnik, S. Pathways of cellular internalisation of liposomes delivered siRNA and effects on siRNA engagement with target mRNA and silencing in cancer cells. Sci. Rep. 2018, 8, 3748. [Google Scholar]
- Zhang, H. Thin-Film Hydration Followed by Extrusion Method for Liposome Preparation. Methods Mol. Biol. 2017, 1522, 17–22. [Google Scholar]
- Rädler, J.O.; Koltover, I.; Salditt, T.; Safinya, C.R. Structure of DNA-cationic liposome complexes: DNA intercalation in multilamellar membranes in distinct interhelical packing regimes. Science 1997, 275, 810–814. [Google Scholar] [CrossRef]
- Saxena, V. Preparation and Physical Characterization of DNA-Binding Cationic Liposomes. Methods Mol. Biol. 2017, 1522, 245–250. [Google Scholar]
- Monnard, P.A.; Oberholzer, T.; Luisi, P. Entrapment of nucleic acids in liposomes. Biochim. Biophys. Acta 1997, 1329, 39–50. [Google Scholar] [CrossRef]
- Sun, D.; Lu, Z.-R. Structure and function of cationic and ionizable lipids for nucleic acid delivery. Pharm. Res. 2023, 40, 27–46. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, X.; Zhang, T.; Wang, C.; Huang, Z.; Luo, X.; Deng, Y. A review on phospholipids and their main applications in drug delivery systems. Asian J. Pharm. Sci. 2015, 10, 81–98. [Google Scholar] [CrossRef]
- Corbo, C.; Molinaro, R.; Taraballi, F.; Toledano Furman, N.E.; Sherman, M.B.; Parodi, A.; Salvatore, F.; Tasciotti, E. Effects of the protein corona on liposome-liposome and liposome-cell interactions. Int. J. Nanomed. 2016, 11, 3049–3063. [Google Scholar]
- Corbo, C.; Molinaro, R.; Parodi, A.; Toledano Furman, N.E.; Salvatore, F.; Tasciotti, E. The impact of nanoparticle protein corona on cytotoxicity, immunotoxicity and target drug delivery. Nanomedicine 2016, 11, 81–100. [Google Scholar] [CrossRef]
- Barbero, F.; Russo, L.; Vitali, M.; Piella, J.; Salvo, I.; Borrajo, M.L.; Busquets-Fité, M.; Grandori, R.; Bastús, N.G.; Casals, E.; et al. Formation of the Protein Corona: The Interface between Nanoparticles and the Immune System. Semin. Immunol. 2017, 34, 52–60. [Google Scholar] [CrossRef]
- Papahadjopoulos, D.; Poste, G.; Schaeffer, B.E. Fusion of Mammalian Cells by Unilamellar Lipid Vesicles: Influence of Lipid Surface Charge, Fluidity, and Cholesterol. Biochim. Biophys. Acta 1973, 323, 23–42. [Google Scholar] [CrossRef]
- Adams, D.H.; Joyce, G.; Richardson, V.J.; Ryman, B.E.; Wiśniewski, H.M. Liposome Toxicity in the Mouse Central Nervous System. J. Neurol. Sci. 1977, 31, 173–179. [Google Scholar] [CrossRef]
- Abu Lila, A.S.; Kiwada, H.; Ishida, T. The accelerated blood clearance (ABC) phenomenon: Clinical challenge and approaches to manage. J. Control. Release 2013, 172, 38–47. [Google Scholar] [CrossRef]
- Wang, X.Y.; Ishida, T.; Kiwada, H. Anti-PEG IgM elicited by injection of liposomes is involved in the enhanced blood clearance of a subsequent dose of PEGylated liposomes. J. Control. Release 2007, 119, 236–244. [Google Scholar] [CrossRef]
- Dézsi, L.; Fülöp, T.; Mészáros, T.; Szénási, G.; Urbanics, R.; Vázsonyi, C.; Őrfi, E.; Rosivall, L.; Nemes, R.; Kok, R.J.; et al. Features of complement activation-related pseudoallergy to liposomes with different surface charge and PEGylation: Comparison of the porcine and rat responses. J. Control. Release 2014, 195, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Szebeni, J. Complement activation-related pseudoallergy: A new class of drug-induced acute immune toxicity. Toxicology 2005, 216, 106–121. [Google Scholar] [CrossRef] [PubMed]
- Kozma, G.T.; Mészáros, T.; Vashegyi, I.; Fülöp, T.; Őrfi, E.; Dézsi, L.; Rosivall, L.; Bavli, Y.; Urbanics, R.; Mollnes, T.E.; et al. Pseudo-anaphylaxis to Polyethylene Glycol (PEG)-Coated Liposomes: Roles of Anti-PEG IgM and Complement Activation in a Porcine Model of Human Infusion Reactions. ACS Nano 2019, 13, 9315–9324. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, K.; Hamano, M.; Ma, H.; Kawano, K.; Maitani, Y.; Aoshi, T.; Ishii, K.J.; Yokoyama, M. Hydrophobic blocks of PEG-conjugates play a significant role in the accelerated blood clearance (ABC) phenomenon. J. Control. Release 2013, 165, 183–190. [Google Scholar] [CrossRef]
- Inglut, C.T.; Sorrin, A.J.; Kuruppu, T.; Vig, S.; Cicalo, J.; Ahmad, H.; Huang, H.-C. Immunological and Toxicological Considerations for the Design of Liposomes. Nanomaterials 2020, 10, 190. [Google Scholar] [CrossRef]
- Takano, S.; Aramaki, Y.; Tsuchiya, S. Physicochemical properties of liposomes affecting apoptosis induced by cationic liposomes in macrophages. Pharm. Res. 2003, 20, 962–968. [Google Scholar] [CrossRef]
- Aramaki, Y.; Takano, S.; Tsuchiya, S. Induction of apoptosis in macrophages by cationic liposomes. FEBS Lett. 1999, 460, 472–476. [Google Scholar] [CrossRef]
- Kedmi, R.; Ben-Arie, N.; Peer, D. The systemic toxicity of positively charged lipid nanoparticles and the role of Toll-like receptor 4 in immune activation. Biomaterials 2010, 31, 6867–6875. [Google Scholar] [CrossRef]
- Knudsen, K.B.; Northeved, H.; Kumar, P.E.K.; Permin, A.; Gjetting, T.; Andresen, T.L.; Larsen, S.; Wegener, K.M.; Lykkesfeldt, J.; Jantzen, K.; et al. In vivo toxicity of cationic micelles and liposomes. Nanomedicine 2015, 11, 467–477. [Google Scholar] [CrossRef]
- Filion, M.C.; Phillips, N.C. Toxicity and immunomodulatory activity of liposomal vectors formulated with cationic lipids toward immune effector cells. Biochim. Biophys. Acta 1997, 1329, 345–356. [Google Scholar] [CrossRef]
- Soenen, S.J.H.; Brisson, A.R.; De Cuyper, M. Addressing the problem of cationic lipid-mediated toxicity: The magnetoliposome model. Biomaterials 2009, 30, 3691–3701. [Google Scholar] [CrossRef] [PubMed]
- Pisani, S.; Di Martino, D.; Cerri, S.; Genta, I.; Dorati, R.; Bertino, G.; Benazzo, M.; Conti, B. Investigation and Comparison of Active and Passive Encapsulation Methods for Loading Proteins into Liposomes. Int. J. Mol. Sci. 2023, 24, 13542. [Google Scholar] [CrossRef]
- Bergers, J.J.; Den Otter, W.; Dullens, H.F.J.; Kerkvliet, C.T.M.; Crommelin, D.J.A. Interleukin-2-containing liposomes: Interaction of interleukin-2 with liposomal bilayers and preliminary studies on application in cancer vaccines. Pharm. Res. 1993, 10, 1715–1721. [Google Scholar] [CrossRef] [PubMed]
- Bangham, A.D. Physical structure and behavior of lipids and lipid enzymes. Adv. Lipid Res. 1963, 1, 65–104. [Google Scholar] [PubMed]
- Hua, S.; Wu, S.Y. The use of lipid-based nanocarriers for targeted pain therapies. Front. Pharmacol. 2013, 4, 143. [Google Scholar] [CrossRef]
- Alavi, M.; Karimi, N.; Safaei, M. Application of various types of liposomes in drug delivery systems. Adv. Pharm. Bull. 2017, 7, 3–9. [Google Scholar] [CrossRef]
- Olusanya, T.O.B.; Haj Ahmad, R.R.; Ibegbu, D.M.; Smith, J.R.; Elkordy, A.A. Liposomal drug delivery systems and anticancer drugs. Molecules 2018, 23, 907. [Google Scholar] [CrossRef]
- Hofheinz, R.D.; Gnad-Vogt, S.U.; Beyer, U.; Hochhaus, A. Liposomal encapsulated anti-cancer drugs. Anticancer. Drugs 2005, 16, 691–707. [Google Scholar] [CrossRef]
- Takechi-Haraya, Y.; Goda, Y.; Sakai-Kato, K. Control of liposomal penetration into three-dimensional multicellular tumor spheroids by modulating liposomal membrane rigidity. Mol. Pharm. 2017, 14, 2158–2165. [Google Scholar] [CrossRef]
- Perche, F.; Torchilin, V.P. Recent trends in multifunctional liposomal nanocarriers for enhanced tumor targeting. J. Drug Deliv. 2013, 2013, 705265. [Google Scholar] [CrossRef]
- Willis, M.; Forssen, E. Ligand-targeted liposomes. Adv. Drug Deliv. Rev. 1998, 29, 249–271. [Google Scholar]
- Markman, J.L.; Rekechenetskiy, A.; Holler, E.; Ljubimova, J.Y. Nanomedicine therapeutic approaches to overcome cancer drug resistance. Adv. Drug Deliv. Rev. 2013, 65, 1866–1879. [Google Scholar] [CrossRef]
- Oku, N.; Namba, Y. Long-circulating liposomes. Crit. Rev. Ther. Drug Carrier Syst. 1994, 11, 231–270. [Google Scholar] [PubMed]
- Oussoren, C.; Zuidema, J.; Crommelin, D.J.A.; Storm, G. Lymphatic uptake and biodistribution of liposomes after subcutaneous injection.: II. Influence of liposomal size, lipid composition and lipid dose. Biochim. Biophys. Acta 1997, 1328, 261–272. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Ahn, H.J. PEGylated DC-Chol/DOPE cationic liposomes containing KSP siRNA as a systemic siRNA delivery carrier for ovarian cancer therapy. Biochem. Biophys. Res. Commun. 2018, 503, 1716–1722. [Google Scholar] [CrossRef] [PubMed]
- Verhoef, J.J.; Anchordoquy, T.J. Questioning the use of PEGylation for drug delivery. Drug Deliv. Transl. Res. 2013, 3, 499–503. [Google Scholar] [CrossRef]
- Pellequer, Y.; Ollivon, M.; Barratt, G. Formulation of liposomes associated with recombinant interleukin-2: Effect on interleukin-2 activity. Biomed. Pharmacother. 2004, 58, 162–167. [Google Scholar] [CrossRef]
- Neville, M.E.; Richau, K.W.; Boni, L.T.; Pflug, L.E.; Robb, R.J.; Popescu, M.C. A comparison of biodistribution of liposomal and soluble il-2 by a new method based on time-resolved fluorometry of europium. Cytokine 2000, 12, 1702–1711. [Google Scholar] [CrossRef]
- Rudokas, M.; Najlah, M.; Alhnan, M.A.; Elhissi, A. Liposome delivery systems for inhalation: A critical review highlighting formulation issues and anticancer applications. Med. Princ. Pract. 2016, 25, 60–72. [Google Scholar] [CrossRef]
- Bangham, A.D.; Standish, M.M.; Watkins, J.C. Diffusion of univalent ions across the lamellae of swollen phospholipids. J. Mol. Biol. 1965, 13, 238–252. [Google Scholar] [CrossRef] [PubMed]
- Hope, M.J.; Bally, M.B.; Webb, G.; Cullis, P.R. Production of large unilamellar vesicles by a rapid extrusion procedure: Characterization of size distribution, trapped volume and ability to maintain a membrane potential. Biochim. Biophys. Acta 1985, 812, 55–65. [Google Scholar] [CrossRef]
- Szoka, F., Jr.; Papahadjopoulos, D. Procedure for preparation of liposomes with large internal aqueous space and high capture by reverse-phase evaporation. Proc. Natl. Acad. Sci. USA 1978, 75, 4194–4198. [Google Scholar] [CrossRef] [PubMed]
- Perrett, S.; Golding, M.; Williams, W.P. A simple method for the preparation of liposomes for pharmaceutical applications: Characterization of the liposomes. J. Pharm. Pharmacol. 1991, 43, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Bao, A.; Phillips, W.T.; Goins, B.; Zheng, X.; Sabour, S.; Natarajan, M.; Ross Woolley, F.; Zavaleta, C.; Otto, R.A. Potential use of drug carried-liposomes for cancer therapy via direct intratumoral injection. Int. J. Pharm. 2006, 316, 162–169. [Google Scholar] [CrossRef]
- Li, Y.; Yao, R.; Ren, M.; Yuan, K.; Du, Y.; He, Y.; Kang, H.; Yuan, S.; Ju, W.; Qiao, J.; et al. Liposomes trigger bone marrow niche macrophage “foam” cell formation and affect hematopoiesis in mice. J. Lipid Res. 2022, 63, 100273. [Google Scholar] [CrossRef]
- Ulrich, A.S. Biophysical aspects of using liposomes as delivery vehicles. Biosci. Rep. 2002, 22, 129–150. [Google Scholar] [CrossRef]
- Sawant, R.R.; Torchilin, V.P. Challenges in development of targeted liposomal therapeutics. AAPS J. 2012, 14, 303–315. [Google Scholar] [CrossRef]
- Sapra, P.; Allen, T.M. Ligand-targeted liposomal anticancer drugs. Prog. Lipid Res. 2003, 42, 439–462. [Google Scholar] [CrossRef]
- Maeda, H.; Wu, J.; Sawa, T.; Matsumura, Y.; Hori, K. Tumor vascular permeability and the EPR effect in macromolecular therapeutics: A review. J. Control. Release 2000, 65, 271–284. [Google Scholar] [CrossRef]
- Shahid, A.; Khan, M.M.; Ahmad, U.; Haider, M.F.; Ali, A. Exploring liposomes for lung cancer therapy. Crit. Rev. Ther. Drug Carr. Syst. 2022, 39, 1–47. [Google Scholar] [CrossRef] [PubMed]
- Astruc, D. Introduction to nanomedicine. Molecules 2015, 21, E4. [Google Scholar] [CrossRef]
- Joffret, M.L.; Morgeaux, S.; Laclerc, C.; Oth, D.; Zanetti, C.; Sureau, P.; Perrin, P. Enhancement of interleukin-2 activity by liposomes. Vaccine 1990, 8, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Khanna, C.; Waldrep, J.C.; Anderson, P.M.; Weischelbaum, R.W.; Hasz, D.E.; Katsanis, E.; Klausneer, J.S. Nebulized interleukin 2 liposomes: Aerosol characteristics and biodistribution. J. Pharm. Pharmacol. 1997, 49, 960–971. [Google Scholar] [CrossRef] [PubMed]
- Koppenhagen, F.J.; Balemans, L.T.M.; Steerenberg, P.A.; Jagmont, T.M.; Otter, W.D.; Storm, G. The design of a pharmaceuttcally acceptable liposomal formulation of recombinant interleukin-2 (Ril-2) for locoregional anticancer immunotherapy. J. Liposome Res. 1999, 9, 313–329. [Google Scholar] [CrossRef]
- Konno, H.; Maruo, Y.; Matin, A.F.; Tanaka, T.; Nakamura, S.; Baba, S.; Yamashita, A.; Tadakuma, T. Effect of liposomal interleukin-2 on ascites-forming rat hepatoma. J. Surg. Oncol. 1992, 51, 33–37. [Google Scholar] [CrossRef]
- Kanaoka, E.; Takahashi, K.; Yoshikawa, T.; Jizomoto, H.; Nishihara, Y.; Hirano, K. A novel and simple type of liposome carrier for recombinant interleukin-2. J. Pharm. Pharmacol. 2001, 53, 295–302. [Google Scholar] [CrossRef]
- Kedar, E.; Gur, H.; Babai, I.; Samira, S.; Even-Chen, S.; Barenholz, Y. Delivery of cytokines by liposomes: Hematopoietic and immunomodulatory activity of interleukin-2 encapsulated in conventional liposomes and in long-circulating liposomes. J. Immunother. 2000, 23, 131–145. [Google Scholar] [CrossRef]
- Kedar, E.; Rutkowski, Y.; Braun, E.; Emanuel, N.; Barenholz, Y. Delivery of cytokines by liposomes. I. Preparation and characterization of interleukin-2 encapsulated in long-circulating sterically stabilized liposomes. J. Immunother. Emphas. Tumor Immunol. 1994, 16, 47–59. [Google Scholar] [CrossRef]
- Kedar, E.; Braun, E.; Rutkowski, Y.; Emanuel, N.; Barenholz, Y. Delivery of cytokines by liposomes. II. Interleukin-2 encapsulated in long-circulating sterically stabilized liposomes: Immunomodulatory and anti-tumor activity in mice. J. Immunother. Emphas. Tumor Immunol. 1994, 16, 115–124. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, N.; Suh, H.; Irvine, D.J. Nanoparticle anchoring targets immune agonists to tumors enabling anti-cancer immunity without systemic toxicity. Nat. Commun. 2018, 9, 6. [Google Scholar] [CrossRef]
- Kwong, B.; Gai, S.A.; Elkhader, J.; Wittrup, K.D.; Irvine, D.J. Localized immunotherapy via liposome-anchored Anti-CD137 + IL-2 prevents lethal toxicity and elicits local and systemic antitumor immunity. Cancer Res. 2013, 73, 1547–1558. [Google Scholar] [CrossRef]
- Ou, W.Q.; Jiang, L.Y.; Gu, Y.; Soe, Z.C.; Kim, B.K.; Gautam, M.; Poudel, K.; Pham, L.M.; Phung, C.D.; Chang, J.H.; et al. Regulatory T cells tailored with pH-responsive liposomes shape an immuno-antitumor milieu against tumors. ACS Appl. Mater. Interfaces 2019, 11, 36333–36346. [Google Scholar] [CrossRef]
- Adibzadeh, M.; Weder, H.G.; Rehbein, A.; Schwuléra, U.; Obermeier, J.; Pawelec, G. Activity of liposomal interleukin-2 in vitro. Mol. Biother. 1992, 4, 24–28. [Google Scholar] [PubMed]
- Kanaoka, E.; Takahashi, K.; Yoshikawa, T.; Jizomoto, H.; Nishihara, Y.; Hirano, K. Continuous release of interleukin-2 from liposomal IL-2 (mixture of interleukin-2 and liposomes) after subcutaneous administration to mice. Drug Dev. Ind. Pharm. 2003, 29, 1149–1153. [Google Scholar] [CrossRef] [PubMed]
- Kanaoka, E.; Takahashi, K.; Yoshikawa, T.; Jizomoto, H.; Nishihara, Y.; Uchida, N.; Maekawa, R.; Hirano, K. A significant enhancement of therapeutic effect against hepatic metastases of M5076 in mice by a liposomal interleukin-2 (mixture). J. Control Release 2002, 82, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Okuno, K.; Nakamura, K.; Tanaka, A.; Yachi, K.; Yasutomi, M. Hepatic immunopotentiation by galactose-entrapped liposomal IL-2 compound in the treatment of liver metastases. Surg. Today 1998, 28, 64–69. [Google Scholar] [CrossRef]
- Khanna, C.; Hasz, D.E.; Klausner, J.S.; Anderson, P.M. Aerosol delivery of interleukin 2 liposomes is nontoxic and biologically effective: Canine studies. Clin. Cancer Res. 1996, 2, 721–734. [Google Scholar]
- Anderson, P.M.; Katsanis, E.; Leonard, A.S.; Schow, D.; Loeffler, C.M.; Goldstein, M.B.; Ochoa, A.C. Increased local antitumor effects of interleukin 2 liposomes in mice with MCA-106 sarcoma pulmonary metastases. Cancer Res. 1990, 50, 1853–1856. [Google Scholar]
- Neville, M.E.; Robb, R.J.; Popescu, M.C. In situ vaccination against a non-immunogenic tumour using intratumoural injections of liposomal interleukin 2. Cytokine 2001, 16, 239–250. [Google Scholar] [CrossRef]
- Katsanis, E.; Xu, Z.; Anderson, P.M.; Dancisak, B.B.; Bausero, M.A.; Weisdorf, D.J.; Blazar, B.R.; Ochoa, A.C. Short-term ex vivo activation of splenocytes with anti-CD3 plus IL-2 and infusion post-BMT into mice results in in vivo expansion of effector cells with potent anti-lymphoma activity. Bone Marrow Transplant. 1994, 14, 563–572. [Google Scholar]
- Saxton, M.L.; Longo, D.L.; Wetzel, H.E.; Tribble, H.; Alvord, W.G.; Kwak, L.W.; Leonard, A.S.; Ullman, C.D.; Curti, B.D.; Ochoa, A.C. Adoptive transfer of anti-CD3-activated CD4+ T cells plus cyclophosphamide and liposome-encapsulated interleukin-2 cure murine MC-38 and 3LL tumors and establish tumor-specific immunity. Blood 1997, 89, 2529–2536. [Google Scholar] [CrossRef]
- Loeffler, C.M.; Platt, J.L.; Anderson, P.M.; Katsanis, E.; Ochoa, J.B.; Urba, W.J.; Longo, D.L.; Leonard, A.S.; Ochoa, A.C. Antitumor effects of interleukin 2 liposomes and anti-CD3-stimulated T-cells against murine MCA-38 hepatic metastasis. Cancer Res. 1991, 51, 2127–2132. [Google Scholar]
- Oya, M. Antitumor effect of interleukin-2 entrapped in liposomes on murine renal cell carcinoma. Keio J. Med. 1994, 43, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Konno, H.; Yamashita, A.; Tadakuma, T.; Sakaguchi, S. Inhibition of growth of rat hepatoma by local injection of liposomes containing recombinant interleukin-2. Antitumor effect of IL-2 liposome. Biotherapy 1991, 3, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Cabanes, A.; Even-Chen, S.; Zimberoff, J.; Barenholz, Y.; Kedar, E.; Gabizon, A. Enhancement of antitumor activity of polyethylene glycol-coated liposomal doxorubicin with soluble and liposomal interleukin 2. Clin. Cancer Res. 1999, 5, 687–693. [Google Scholar]
- Dong, L.-F.; Mei, H.-S.; Song, S.-X.; Lu, Z.-J. Synergistic role between rhIL-2 and adriamycin long circulating temperature-sensitive liposome in targeting therapy on tumor. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 2005, 21, 296–300. [Google Scholar] [PubMed]
- Corona-Ortega, T.; Rangel-Corona, R.; Hernández-Jiménez, M.; Baeza, I.; Ibáñez, M.; Weiss-Steider, B. Characterization of cationic liposomes having IL-2 expressed on their external surface, and their affinity to cervical cancer cells expressing the IL-2 receptor. J. Drug Target. 2009, 17, 496–501. [Google Scholar] [CrossRef]
- Zheng, Y.; Stephan, M.T.; Gai, S.A.; Abraham, W.; Shearer, A.; Irvine, D.J. In vivo targeting of adoptively transferred T-cells with antibody- and cytokine-conjugated liposomes. J. Control. Release 2013, 172, 426–435. [Google Scholar] [CrossRef]
- Neville, M.E.; Boni, L.T.; Pflug, L.E.; Popescu, M.C.; Robb, R.J. Biopharmaceutics of liposomal interleukin 2, Oncolipin. Cytokine 2000, 12, 1691–1701. [Google Scholar] [CrossRef]
- Simpson-Abelson, M.R.; Purohit, V.S.; Pang, W.M.; Iyer, V.; Odunsi, K.; Demmy, T.L.; Yokota, S.J.; Loyall, J.L.; Kelleher, R.J., Jr.; Balu-Iyer, S.; et al. IL-12 delivered intratumorally by multilamellar liposomes reactivates memory T cells in human tumor microenvironments. Clin. Immunol. 2009, 132, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Hu, L.; Wang, Y.; Liu, Q.; Liu, J.; Long, H.; Li, Q.; Luo, L.; Peng, Y. Local administration of mRNA encoding cytokine cocktail confers potent anti-tumor immunity. Front. Immunol. 2024, 15, 1455019. [Google Scholar] [CrossRef] [PubMed]
- Barberio, A.E.; Smith, S.G.; Pires, I.S.; Iyer, S.; Reinhardt, F.; Melo, M.B.; Suh, H.; Weinberg, R.A.; Irvine, D.J.; Hammond, P.T. Layer-by-layer interleukin-12 nanoparticles drive a safe and effective response in ovarian tumors. Bioeng. Transl. Med. 2023, 8, e10453. [Google Scholar] [CrossRef] [PubMed]
- Meraz, I.M.; Savage, D.J.; Segura-Ibarra, V.; Li, J.; Rhudy, J.; Gu, J.; Serda, R.E. Adjuvant cationic liposomes presenting MPL and IL-12 induce cell death, suppress tumor growth, and alter the cellular phenotype of tumors in a murine model of breast cancer. Mol. Pharm. 2014, 11, 3484–3491. [Google Scholar] [CrossRef]
- Liu, J.; Han, Y.; Zhao, M.; Wang, L.; Hu, H.; Chen, D. Unlocking the power of immunotherapy: Combinatorial delivery of plasmid IL-15 and gemcitabine to synergistically remodeling the tumor microenvironment. Int. J. Pharm. 2024, 655, 124027. [Google Scholar] [CrossRef]
- Madhankumar, A.B.; Slagle-Webb, B.; Mintz, A.; Sheehan, J.M.; Connor, J.R. Interleukin-13 receptor-targeted nanovesicles are a potential therapy for glioblastoma multiforme. Mol. Cancer Ther. 2006, 5, 3162–3169. [Google Scholar] [CrossRef]
- Saito, M.; Fan, D.; Lachman, L.B. Antitumor effects of liposomal IL1 alpha and TNF alpha against the pulmonary metastases of the B16F10 murine melanoma in syngeneic mice. Clin. Exp. Metastasis 1995, 13, 249–259. [Google Scholar] [CrossRef]
- Son, J.S.; Chow, R.; Kim, H.; Lieu, T.; Xiao, M.; Kim, S.; Matuszewska, K.; Pereira, M.; Nguyen, D.L.; Petrik, J. Liposomal delivery of gene therapy for ovarian cancer: A systematic review. Reprod. Biol. Endocrinol. 2023, 21, 75. [Google Scholar] [CrossRef]
- Balazs, D.A.; Godbey, W. Liposomes for use in gene delivery. J. Drug Deliv. 2011, 2011, 326497. [Google Scholar] [CrossRef]
- Liu, C.; Zhang, L.; Zhu, W.; Guo, R.; Sun, H.; Chen, X.; Deng, N. Barriers and strategies of cationic liposomes for cancer gene therapy. Mol. Ther. Methods Clin. Dev. 2020, 18, 751–764. [Google Scholar] [CrossRef]
- Morse, M.A. Technology evaluation: Gene therapy (IL-2), Valentis Inc. Curr. Opin. Mol. Ther. 2000, 2, 448–452. [Google Scholar] [PubMed]
- Li, D.; Jiang, W.; Bishop, J.S.; Ralston, R.; O’Malley, B.W., Jr. Combination surgery and nonviral interleukin 2 gene therapy for head and neck cancer. Clin. Cancer Res. 1999, 5, 1551–1556. [Google Scholar]
- Horiguchi, Y.; Larchian, W.A.; Kaplinsky, R.; Fair, W.R.; Heston, W.D. Intravesical liposome-mediated interleukin-2 gene therapy in orthotopic murine bladder cancer model. Gene Ther. 2000, 7, 844–851. [Google Scholar] [CrossRef]
- Horinaga, M.; Harsch, K.M.; Fukuyama, R.; Heston, W.; Larchian, W. Intravesical interleukin-12 gene therapy in an orthotopic bladder cancer model. Urology 2005, 66, 461–466. [Google Scholar] [CrossRef]
- Parker, S.E.; Khatibi, S.; Margalith, M.; Anderson, D.; Yankauckas, M.; Gromkowski, S.H.; Latimer, T.; Lew, D.; Marquet, M.; Manthorpe, M.; et al. Plasmid DNA gene therapy: Studies with the human interleukin-2 gene in tumor cells in vitro and in the murine B16 melanoma model in vivo. Cancer Gene Ther. 1996, 3, 175–185. [Google Scholar]
- Wang, Q.; Cao, X.; Wang, J. Activation of macrophages from lymphoma-bearing mice by liposome mediated intraperitoneal IL-2 and IL-6 gene therapy. Zhonghua Xue Ye Xue Za Zhi 1997, 18, 364–367. [Google Scholar] [PubMed]
- Cao, X.; Wang, Q.; Ju, D.W.; Tao, Q.; Wang, J. Efficient inducation of local and systemic antitumor immune response by liposome-mediated intratumoral co-transfer of interleukin-2 gene and interleukin-6 gene. J. Exp. Clin. Cancer Res. 1999, 18, 191–200. [Google Scholar] [PubMed]
- Wang, Q.; Cao, X.; Wang, J.; Zhang, W.; Tao, Q.; Ye, T. Macrophage activation of lymphoma-bearing mice by liposome-mediated intraperitoneal IL-2 and IL-6 gene therapy. Chin. Med. J. 2000, 113, 281–285. [Google Scholar]
- Rodriguez, B.L.; Blando, J.M.; Lansakara, P.D.; Kiguchi, Y.; DiGiovanni, J.; Cui, Z. Antitumor activity of tumor-targeted RNA replicase-based plasmid that expresses interleukin-2 in a murine melanoma model. Mol. Pharm. 2013, 10, 2404–2415. [Google Scholar] [CrossRef]
- Raeber, M.E.; Sahin, D.; Karakus, U.; Boyman, O. A systematic review of interleukin-2-based immunotherapies in clinical trials for cancer and autoimmune diseases. eBioMedicine 2023, 90, 104539. [Google Scholar] [CrossRef]
- Mayer, A.; Andratschke, M.; Pauli, C.; Reitberger, E.; Kolbow, K.; Wollenberg, B. Liposomal transfection of squamous carcinoma cells of the head and neck with IL-2 and B7 plasmids inducing an autologous immune response in vitro. Anticancer. Res. 2005, 25, 3917–3923. [Google Scholar] [PubMed]
- Missol-Kolka, E.; Sochanik, A.; Szala, S. Combined therapy of B16(F10) murine melanoma using E. coli cytosine deaminase gene and murine interleukin-4 gene. Neoplasma 1998, 45, 305–311. [Google Scholar]
- Missol, E.; Sochanik, A.; Szala, S. Introduction of murine Il-4 gene into B16(F10) melanoma tumors by direct gene transfer with DNA-liposome complexes. Cancer Lett. 1995, 97, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Park, S.H. Anti-cancer activity of microbubble conjugated with Sorafenib containing liposome and IL4R-targeting peptide in kidney cancer cells. Cell Mol. Biol. 2023, 69, 266–271. [Google Scholar]
- Yoon, S.J.; Heo, D.S.; Kang, J.O.; Kim, N.K. Combination gene therapy of IL-12 and allogeneic MHC class I gene via stimulating NK cytolytic activity. Anticancer. Res. 1999, 19, 4337–4342. [Google Scholar] [PubMed]
- Wang, K.M.; Xia, A.D.; Chen, S.S. Combination therapy of experimental murine hepatoma with mIL-12 gene and MHC I gene mediated by liposome. Ai Zheng 2002, 21, 1041–1046. [Google Scholar]
- Charoensit, P.; Kawakami, S.; Higuchi, Y.; Yamashita, F.; Hashida, M. Enhanced growth inhibition of metastatic lung tumors by intravenous injection of ATRA-cationic liposome/IL-12 pDNA complexes in mice. Cancer Gene Ther. 2010, 17, 512–522. [Google Scholar] [CrossRef]
- Cao, L.; Zeng, Q.; Xu, C.; Shi, S.; Zhang, Z.; Sun, X. Enhanced antitumor response mediated by the codelivery of paclitaxel and adenoviral vector expressing IL-12. Mol. Pharm. 2013, 10, 1804–1814. [Google Scholar] [CrossRef]
- Speroni, L.; Gasparri, J.; de Ios, A.B.V.; Chiaramoni, N.S.; Smagur, A.; Szala, S.; Taira, M.C.; del V Alonso, S. Antitumoral effect of IL-12 gene transfected via liposomes into B16F0 cells. Acta Biochim. Pol. 2009, 56, 249–253. [Google Scholar] [CrossRef]
- Chen, W.; Shao, C.S.; Shen, J.G.; Pan, Y.; Zheng, S. Therapeutic effect of cationic liposome-mediated interleukin-12 gene delivery on murine melanoma in vivo. Zhejiang Da Xue Xue Bao Yi Xue Ban 2005, 34, 73–76. [Google Scholar]
- Baradaran, B.; Mohammadi, A.; Shamekhi, S.; Majidazar, N.; Dilmaghani, A.; Soofiyani, S.R.; McMillan, N.A.; Lotfipour, F.; Hallaj-Nezhadi, S. A novel method for the development of plasmid DNA-loaded nanoliposomes for cancer gene therapy. Drug Deliv. Transl. Res. 2022, 12, 1508–1520. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, R.; Namai, E.; Oda, Y.; Nishiie, N.; Otake, S.; Koshima, R.; Hirata, K.; Taira, Y.; Utoguchi, N.; Negishi, Y.; et al. Cancer gene therapy by IL-12 gene delivery using liposomal bubbles and tumoral ultrasound exposure. J. Control Release 2010, 142, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Zhang, X.-M.; Zhang, N.; Cheng, L.; Li, C.; Zhang, S.; Zhang, J.-F.; Dai, L.; Tian, H.-W.; Yan, N.; et al. IL15 combined with Caspy2 provides enhanced therapeutic efficiency against murine malignant neoplasm growth and metastasis. Cancer Gene Ther. 2012, 19, 460–467. [Google Scholar] [CrossRef]
- Matsumoto, K.; Kikuchi, E.; Horinaga, M.; Takeda, T.; Miyajima, A.; Nakagawa, K.; Oya, M. Intravesical Interleukin-15 Gene Therapy in an Orthotopic Bladder Cancer Model. Hum. Gene Ther. 2011, 22, 1423–1432. [Google Scholar] [CrossRef]
- Teng, X.; Zhou, X.-K.; Zhang, Y.-B.; Qiu, J.; Mao, Y.-Q.; Deng, H.-X.; Li, J. Antitumoral efficacy by systemic delivery of cationic liposome-plasmid interleukin-15 complexes in murine models of lung metastasis. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 2012, 28, 148–152. [Google Scholar]
- Lei, S.; Zhang, X.; Men, K.; Gao, Y.; Yang, X.; Wu, S.; Duan, X.; Wei, Y.; Tong, R. Efficient colorectal cancer gene therapy with IL-15 mRNA nanoformulation. Mol. Pharm. 2020, 17, 3378–3391. [Google Scholar] [CrossRef] [PubMed]
- Xiong, B.; Zhu, M.-X.; Jin, Q.-M.; Song, F.-X. Construction and in vitro study of eukaryotic expression vector carrying GITRL and IL-21 gene. Zhongguo Shi Yan Xue Ye Xue Za Zhi 2014, 22, 1295–1300. [Google Scholar]
- Fieni, C.; Sorrentino, C.; Ciummo, S.L.; Fontana, A.; Lotti, L.V.; Scialis, S.; Garcia, D.C.; Caulo, M.; Di Carlo, E. Immunoliposome-based targeted delivery of the CRISPR/Cas9gRNA-IL30 complex inhibits prostate cancer and prolongs survival. Exp. Mol. Med. 2024, 56, 2033–2051. [Google Scholar] [CrossRef] [PubMed]
- Petersen, G.H.; Alzghari, S.K.; Chee, W.; Sankari, S.S.; La-Beck, N.M. Meta-analysis of clinical and preclinical studies comparing the anticancer efficacy of liposomal versus conventional non-liposomal doxorubicin. J. Control. Release 2016, 232, 255–264. [Google Scholar] [CrossRef]
- Boucher, Y.; Baxter, L.T.; Jain, R.K. Interstitial pressure gradients in tissue-isolated and subcutaneous tumors: Implications for therapy. Cancer Res 1990, 50, 4478–4484. [Google Scholar]
- Moosavian, S.A.; Bianconi, V.; Pirro, M.; Sahebkar, A. Challenges and pitfalls in the development of liposomal delivery systems for cancer therapy. Semin. Cancer Biol. 2021, 69, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Gabizon, A.; Chisin, R.; Amselem, S.; Druckmann, S.; Cohen, R.; Goren, D.; Fromer, I.; Peretz, T.; Sulkes, A.; Barenholz, Y. Pharmacokinetic and imaging studies in patients receiving a formulation of liposome-associated adriamycin. Br. J. Cancer 1991, 64, 1125–1132. [Google Scholar] [CrossRef] [PubMed]
- Dams, E.T.; Laverman, P.; Oyen, W.J.; Storm, G.; Scherphof, G.L.; van Der Meer, J.W.; Corstens, F.H.; Boerman, O.C. Accelerated blood clearance and altered biodistribution of repeated injections of sterically stabilized liposomes. J. Pharmacol. Exp. Ther. 2000, 292, 1071–1079. [Google Scholar] [CrossRef]
- Connor, J.; Huang, L. pH-sensitive immunoliposomes as an efficient and target-specific carrier for antitumor drugs. Cancer Res. 1986, 46, 3431–3435. [Google Scholar]
- Milan, A.; Mioc, A.; Prodea, A.; Mioc, M.; Buzatu, R.; Ghiulai, R.; Racoviceanu, R.; Caruntu, F.; Şoica, C. The Optimized Delivery of Triterpenes by Liposomal Nanoformulations: Overcoming the Challenges. Int. J. Mol. Sci. 2022, 23, 1140. [Google Scholar] [CrossRef] [PubMed]
- Amin, M.; Seynhaeve, A.L.B.; Sharifi, M.; Falahati, M.; Ten Hagen, T.L.M. Liposomal drug delivery systems for cancer therapy: The Rotterdam Experience. Pharmaceutics 2022, 14, 2165. [Google Scholar] [CrossRef]
- Fang, J.; Islam, W.; Maeda, H. Exploiting the dynamics of the EPR effect and strategies to improve the therapeutic effects of nanomedicines by using EPR effect enhancers. Adv. Drug Deliv. Rev. 2020, 157, 142–160. [Google Scholar] [CrossRef]
- Shi, Y.; van der Meel, R.; Chen, X.; Lammers, T. The EPR effect and beyond: Strategies to improve tumor targeting and cancer nanomedicine treatment efficacy. Theranostics 2020, 10, 7921–7924. [Google Scholar] [CrossRef]
- Shi, J.; Kantoff, P.W.; Wooster, R.; Farokhzad, O.C. Cancer nanomedicine: Progress, challenges and opportunities. Nat. Rev. Cancer 2017, 17, 20–37. [Google Scholar] [CrossRef]
- Alhamhoom, Y.; Kakinani, G.; Rahamathulla, M.; Ali, M.; Osmani, R.; Hani, U.; Yoonus Thajudeen, K.; Kiran Raj, G.; Gowda, D.V. Recent advances in the liposomal nanovesicles based immunotherapy in the treatment of cancer: A review. Saudi Pharm. J. 2023, 31, 279–294. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kubbara, E.A.; Bolad, A.; Malibary, H. Advances in Liposomal Interleukin and Liposomal Interleukin Gene Therapy for Cancer: A Comprehensive Review of Preclinical Studies. Pharmaceutics 2025, 17, 383. https://doi.org/10.3390/pharmaceutics17030383
Kubbara EA, Bolad A, Malibary H. Advances in Liposomal Interleukin and Liposomal Interleukin Gene Therapy for Cancer: A Comprehensive Review of Preclinical Studies. Pharmaceutics. 2025; 17(3):383. https://doi.org/10.3390/pharmaceutics17030383
Chicago/Turabian StyleKubbara, Eman A., Ahmed Bolad, and Husam Malibary. 2025. "Advances in Liposomal Interleukin and Liposomal Interleukin Gene Therapy for Cancer: A Comprehensive Review of Preclinical Studies" Pharmaceutics 17, no. 3: 383. https://doi.org/10.3390/pharmaceutics17030383
APA StyleKubbara, E. A., Bolad, A., & Malibary, H. (2025). Advances in Liposomal Interleukin and Liposomal Interleukin Gene Therapy for Cancer: A Comprehensive Review of Preclinical Studies. Pharmaceutics, 17(3), 383. https://doi.org/10.3390/pharmaceutics17030383







