Edge AI for Early Detection of Chronic Diseases and the Spread of Infectious Diseases: Opportunities, Challenges, and Future Directions
Abstract
:1. Introduction
- We describe the synergy between AI and edge computing in healthcare to create opportunities for healthcare providers. These opportunities include cutting-edge tools that provide instant data and deep insights. These tools help accelerate disease detection and create tailored treatment plans. The plans consider the unique characteristics and needs of individual patients.
- We review the various applications of Edge AI in the early prediction of health issues and the detection of chronic and infectious diseases.
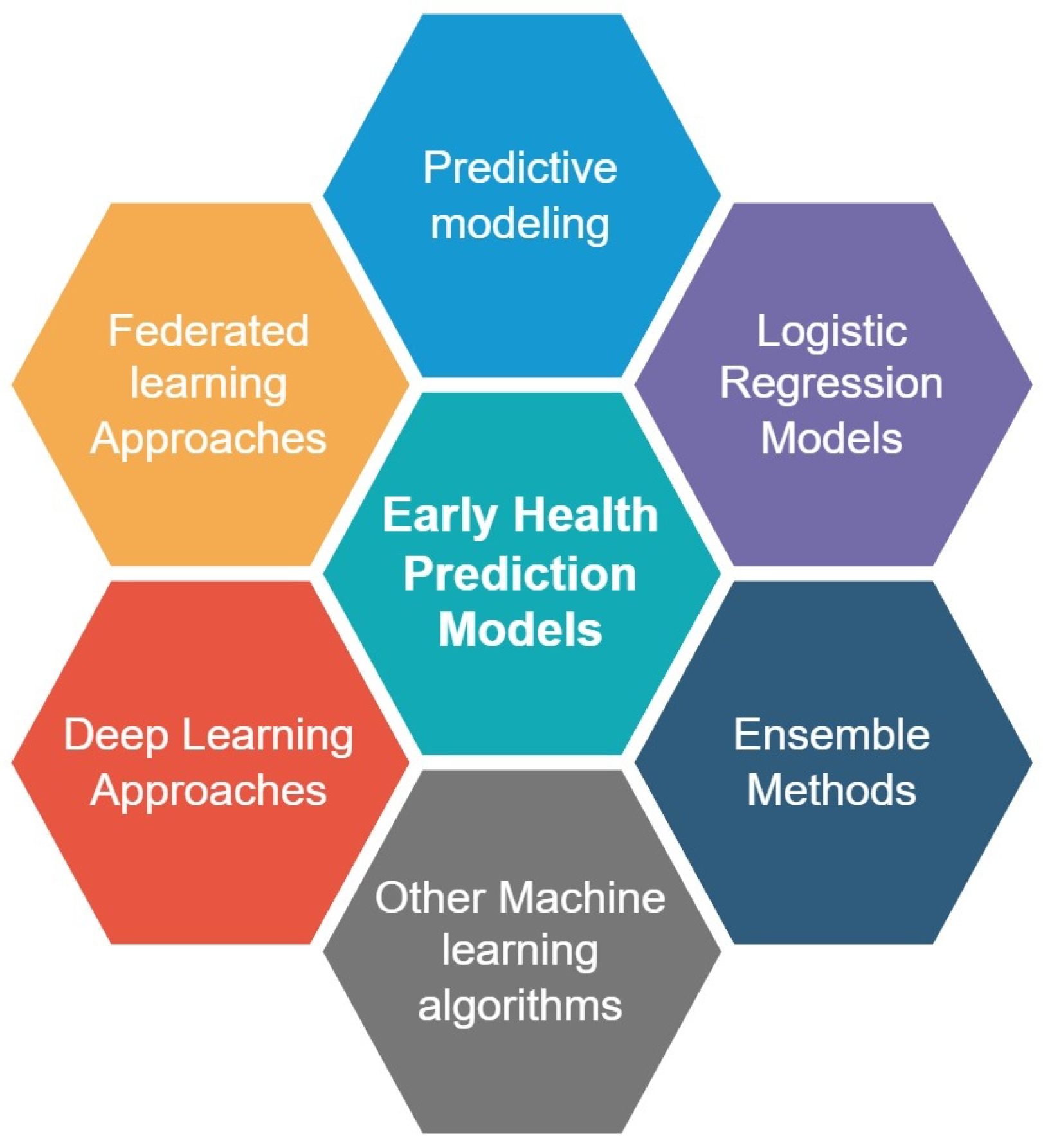
- We scrutinize machine learning and deep learning models instrumental in early health prediction and detection of chronic and infectious diseases.
- We review the various applications of federated learning for disease and mortality prediction and highlight the critical dimension of privacy in early health prediction.
- We identify and elaborate on the challenges faced by Edge AI in the healthcare domain, such as privacy, data accuracy, model bias, interoperability, and integration with existing health systems. Furthermore, we outline for each challenge the future research directions, emphasizing the transformative potential of Edge AI in the context of early health prediction.
2. Edge AI Overview
3. AI and Edge Computing Synergy in Healthcare
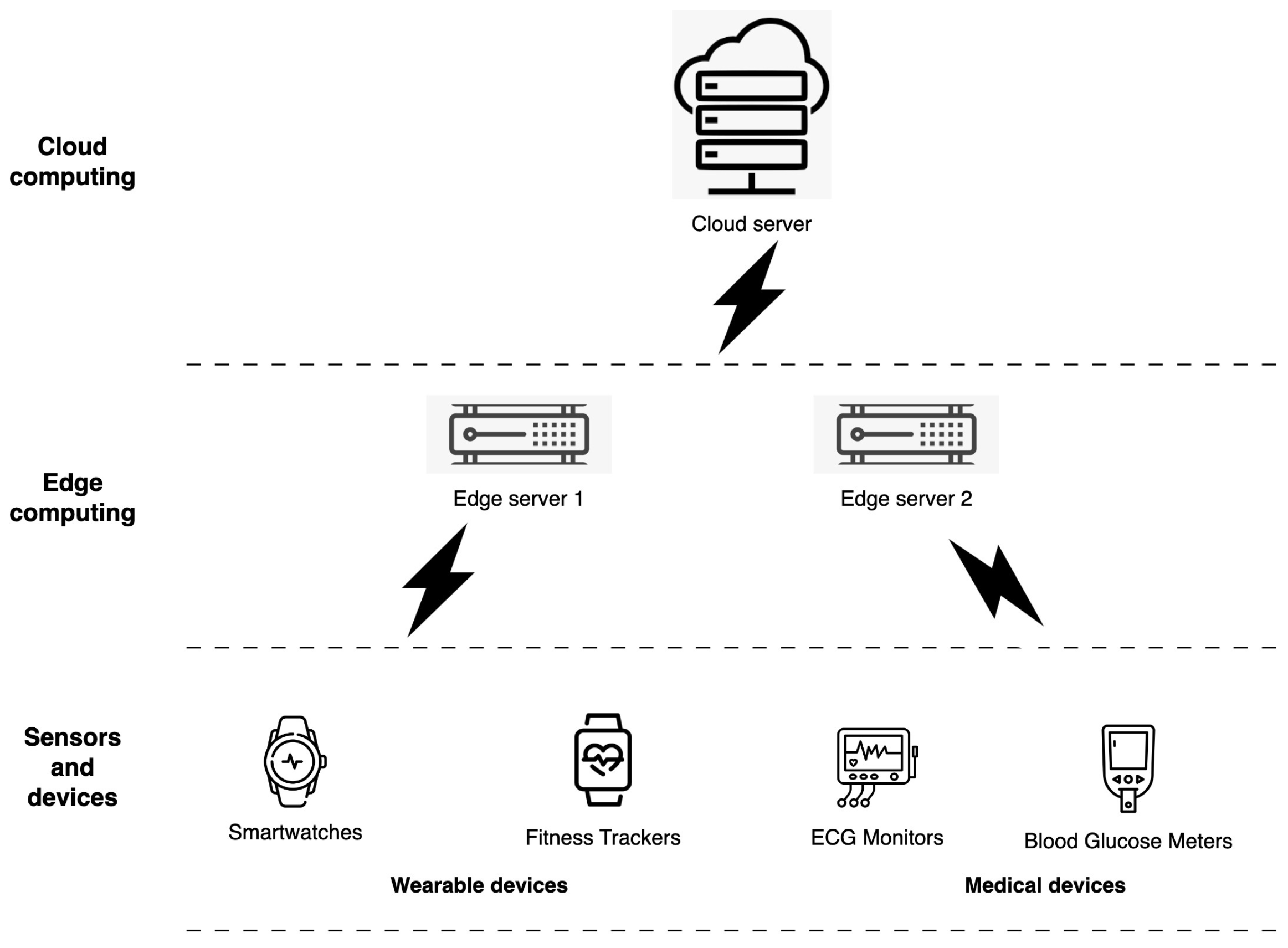
- Wearable devices: Wearable technology, which includes devices such as fitness trackers and smartwatches, is evolving into a comprehensive data repository that contains various details about a person’s physical movements, heart behavior, and sleep dynamics during nighttime hours (see Figure 2). The use of edge computing facilitates the instant processing of data originating from wearable devices. This accelerates the detection of changes in a person’s health status that may serve as precursors to the onset of chronic disease. In a recent study by the authors in [21], several research papers were analyzed to examine the use of wearable devices in detecting and predicting cardiovascular disease. The study results suggest that wearable devices can effectively detect, predict, and treat cardiovascular disease. However, more research is needed to improve their use. In addition, in [34], the authors proposed a secure edge-computing-based framework for smart health systems. This framework focuses on real-time health monitoring and ensures data security and confidentiality through clustering approaches for anomaly detection and attribute-based encryption (ABE) for secure access to biosignal data. Experimental results of the proposed framework show an improved performance, an accuracy up to 98.5%, and data security.
- Medical Devices: IoT sensors integrated into medical devices provide valuable data for early health prediction and continuous monitoring of patient’s health conditions. Edge computing is a viable option for processing data obtained from medical devices such as blood glucose meters in real time. Processing data is an indispensable component that helps detect changes in a person’s health that could indicate the development of chronic diseases such as diabetes [35]. Currently, there are several medical devices that use edge computing technology for their operations:
- Smart insulin pens: Smart insulin pens, used to control blood glucose levels in diabetic patients, are advanced medical devices that integrate sensors and connectivity to track insulin doses and blood glucose levels and provide real-time feedback to patients [36]. These devices can process data in real time and provide patients with personalized insights through edge computing.
- Wearable electrocardiogram (ECG) monitors: Wearable ECG monitors are medical devices used to monitor the patient’s heart’s electrical activity continuously. These monitors are attached to various areas of the body, such as the wrist, chest, or torso, and are aimed at individuals struggling with heart problems [37]. By integrating edge computing, these devices are able to analyze ECG data instantly. As a result, they are able to quickly detect irregular heart rhythms and other critical abnormalities, warranting immediate medical intervention.
- Smart inhalers: Smart inhalers are devices designed to treat asthma or chronic obstructive pulmonary disease (COPD). They are equipped with sensors and connectivity features that allow them to track medication use and provide feedback to patients [38,39]. The use of edge computing in smart inhalers has further enhanced their functionality by enabling real-time data processing and personalized patient insights.
- Vital sign monitors: Vital sign monitors are medical devices that monitor various physiological parameters such as heart rate, blood pressure, and oxygen saturation. These devices can be used in hospitals, clinics, or at home and allow real-time monitoring of the patient’s health status. Using edge computing, these devices can analyze vital signs in real time and alert healthcare providers to anomalies [40,41].
- Real-time data analysis: Edge computing offers the ability to analyze large datasets in a timely manner, thereby detecting changes in a person’s health status in virtually real time. Timely detection of potential health problems is critical for early health prognosis, enabling health professionals to identify potential health problems before they worsen and become more difficult to treat.
- Shortened latency: By processing data at the periphery of the network and closer to its source, edge computing effectively reduces the latency that typically occurs when data are transmitted to a central data center for analysis. Incorporating edge computing technology can provide significant benefits to healthcare providers by enabling rapid data analysis and informed decision making regarding a patient’s health status.
- Improved data security: Edge computing is a notable advancement that aims to protect sensitive data from security breaches through localized data processing at the network perimeter. Limiting the need for extensive data transmission over the internet provides a critical solution for early health prognosis. This attribute plays a central role in maintaining the confidentiality of an individual’s private health information, ensuring that their information is used only to promote their well-being.
- Cost efficiency: The increased cost efficiency of edge computing makes it particularly beneficial for healthcare providers, as they have the ability to leverage artificial intelligence and other cutting-edge technologies to improve healthcare outcomes.
- Scalability: Edge computing is a highly scalable framework, making it a suitable choice for health predictive initiatives that operate at scale. By performing data processing at the periphery of the network, edge computing can handle large amounts of data, enabling real-time monitoring of the health status of multiple individuals simultaneously.
4. Methodology
4.1. Search Criteria Formulation
- C1: (“Edge computing” OR “IoT” OR “wearables” OR “wearable sensors”) AND (“chronic” OR “infectious”) AND (“disease”);
- C2: (“AI” OR “edge intelligence” OR “machine learning” OR “deep learning” OR “federated learning”) AND (“chronic” OR “infectious”) AND (“disease” OR “health prediction”);
- C3: (“predictive models”) AND (“chronic” OR “infectious”) AND (“disease”);
- C4: “Privacy” AND “health prediction”.
- RQ-1: What are the myriad applications of Edge AI in early health prediction? This research question seeks to uncover research efforts and breakthroughs in the use of Edge AI for the early detection of chronic and infectious diseases.
- RQ-2: What machine learning and deep learning models are used in early health prediction?
- RQ-3: What techniques and methods are used to preserve privacy in early health prediction and detection of the onset of chronic and infectious diseases?
- RQ-4: What are the potential open research issues and future directions of Edge AI for early health prediction and detection of chronic and infectious diseases? This question seeks to define the unanswered inquiries and unexplored paths that hold the key to unlocking the full potential of Edge AI in early health prediction. By unraveling the challenges that can hinder their widespread adoption and delving into research directions, this query drives researchers to understand the current landscape of Edge AI and early disease detection, unraveling novel insights and paving the way for transformative advancements in this domain.
4.2. Source Selection and Approach
5. Edge AI for Early Health Prediction
5.1. Stakeholders and Architecture
- Sensors and Devices: The foundation of AI-driven edge systems for early health prediction depends on the use of sensors and devices that collect and transmit patient data. These devices typically include wearable devices such as fitness trackers and smartwatches and medical devices such as ECG monitors and glucometers.
- Edge Computing Devices: Edge computing devices are responsible for processing and analyzing data at the point of origin. They include a variety of components, such as edge gateways, edge servers, and edge routers.
- AI Algorithms: AI algorithms play a central role in carefully examining data collected by sensors and devices and facilitating the detection of latent health anomalies. By leveraging historical patient data, these algorithms can be trained to improve their accuracy in detecting patterns and trends indicative of an imminent health problem.
- Cloud Platforms: Cloud platforms serve as repositories for data acquired by Edge AI systems. The information thus obtained can be used for deeper analysis and modeling. Subsequently, these data are even used to refine AI algorithms through training.
- User Interfaces: User interfaces allow patients and healthcare providers to access the data and insights generated by Edge AI systems. Accessible through a variety of media, including desktop computers, mobile devices, or other internet-connected platforms, these interfaces play a critical communicative role.
- Data Management and Security: Edge AI-based early health prediction systems require robust data management and security systems to protect patient data. This includes increased data storage, data encryption, and the implementation of strict access control protocols.
5.2. Early Detection of Chronic and Infectious Diseases
5.3. Prediction of Future Health Outcomes
5.3.1. Predictive Modeling
5.3.2. Machine Learning Algorithms
5.3.3. Deep Learning Approaches
- Convolutional Neural Networks (CNNs). CNNs are pivotal in edge analytics, excelling in object detection and recognition. Their capacity to handle substantial quantities of visual data and discern complicated patterns is of utmost importance in the interpretation of meaningful observations from visual information.
- Recurrent Neural Networks (RNNs). RNNs serve a pivotal function in video analysis by effectively managing tasks such as tracking, segmentation, and action recognition. With their proficiency in processing sequential data, RNNs are well suited for analyzing videos, which are essentially temporal image sequences.
5.3.4. Federated Learning (FL)
5.3.5. Evaluation Metrics of Edge AI Algorithms
- Accuracy. Accuracy refers to the measure of how well the algorithm performs in correctly identifying or classifying data in the edge devices or edge computing systems. It quantifies the level of agreement between the algorithm’s predictions and the ground truth or desired outcomes.
- Precision and Recall. Precision and recall are two important metrics used to evaluate the performance of classification models. They provide insights into how well the algorithm is identifying and classifying data at the edge devices or edge computing systems. Precision measures the accuracy of positive predictions made by the algorithm. It is the ratio of true positives (correctly predicted positive instances) to the sum of true positives and false positives (incorrectly predicted positive instances). In other words, precision indicates the proportion of correctly identified positive instances out of all the instances predicted as positive. A higher precision value indicates a lower rate of false positives. Recall, also known as sensitivity or the true positive rate, measures the algorithm’s ability to correctly identify positive instances. It is the ratio of true positives to the sum of true positives and false negatives (positive instances incorrectly classified as negative). Recall represents the proportion of correctly identified positive instances out of all the actual positive instances. A higher recall value indicates a lower rate of false negatives.
- Intersection over Union (IoU). The IoU metric is particularly useful in evaluating the performance of object detection algorithms. It helps assess how well the algorithm accurately localizes and identifies objects within an image or video frame. By comparing the predicted and ground truth regions, IoU provides insights into the algorithm’s ability to detect and segment objects accurately. It is used in Edge AI algorithms dealing with visual data to measure the overlap between the predicted bounding box or region and the ground truth bounding box or region in object detection and segmentation tasks. It provides a quantitative measure of the accuracy of the algorithm’s predictions. IoU is calculated by dividing the area of intersection between the predicted and ground truth regions by the area of their union. The resulting value indicates the extent of overlap between the two regions. A higher IoU value indicates a better match between the predicted and ground truth regions. IoU is often used as a threshold to determine whether a predicted bounding box or region is considered a true positive or a false positive. If the IoU value exceeds a certain threshold (commonly 0.5 or 0.7), the prediction is considered a true positive. Otherwise, it is classified as a false positive.
- Latency. Latency in Edge AI algorithms refers to the time it takes for an algorithm to process input data and produce an output on edge devices or edge computing platforms. It is a measure of the delay or response time experienced during the execution of the algorithm. In the context of Edge AI, latency is a critical factor as it directly impacts the real-time performance and responsiveness of the system. Edge devices, such as smartphones, IoT devices, or edge servers, often have limited computational resources compared to cloud-based servers. This constraint can lead to a higher latency in executing AI algorithms on the edge. The latency in Edge AI algorithms depends on various factors, including the complexity of the algorithm, the computational power of the edge device, data processing requirements, and network connectivity. The goal is to minimize latency to ensure efficient and timely decision making at the edge.
| Ref. | Year | Application | Methods | Results |
|---|---|---|---|---|
| [45] | 2022 | Identification and prediction of chronic diseases using machine learning. | Data collection from various sources. Training with CNN and KNN algorithms | CNN and KNN models outperformed Naive Bayes, decision tree, and logistic regression algorithms. CNN and KNN achieved a higher precision, recall, and F1-score. |
| [75] | 2022 | A survey on Federated Learning for Privacy Preservation in Smart Healthcare Systems | FL for privacy preservation in IoMT. Advanced FL architectures incorporating DRL, digital twins, and GANs | Description of some advanced FL architectures incorporating deep reinforcement learning (DRL), digital twins, and generative adversarial networks (GANs) for detecting privacy threats. |
| [72] | 2022 | Review of Federated Learning for Healthcare | Systematic literature review methodology. Definition of research questions | Systematic literature review on FL in healthcare. Proposed architecture for FL applied to healthcare data |
| [63] | 2022 | Machine learning models used for early diabetes prediction. | SVM-ANN ensemble. SVM, KNN, NB, C4.5 DT, Adaboost DT with Bagging, Bagged DT, K-means clustering and RF, KNN and AB, Fusion ML Decision, LR ensemble, RF, Multilayer Perceptron, SVM with feed backward feature elimination | Random forest (RF) model achieved the highest accuracy of 82.26% in predicting diabetes. The Naive Bayes (NB) model performed the worst, with an accuracy rate of 70.56%. |
| [59] | 2019 | Health risk prediction models incorporating personality data. | Informal rule for cross-validation error. Anti-conservative approach to protect against overfitting | Four-year incidence rate of possible MCI is roughly 20%. Model C with personality data shows a significant improvement in overall performance. |
| [66] | 2015 | Comparison of predictive models for early hospital readmissions. | Logistic regression with maximum likelihood estimator. Logistic regression with multi-step heuristic approach | Random forest and penalized logistic regressions are the best methods for predicting early readmissions. Deep learning methods outperform regression methods in the healthcare literature. |
| [67] | 2021 | Predicting mortality among patients with liver cirrhosis. | Deep neural network (DNN), random forest (RF), and logistic regression (LR) algorithms. Multiple imputation for missing values in variables. | Models with all variables outperformed those with four MELD-NA variables. The DNN model achieved a higher AUC than the LR and RF models. |
| [76] | 2022 | Clinical prediction models to estimate disease probability and health outcomes. | Split-sample method for model development and internal validation. Resampling methods, especially the bootstrap method, for stable estimates | Overview of developing and validating clinical prediction models by applying traditional regression models or machine learning models. |
| [49] | 2023 | AI models for predicting and early diagnosis of pancreatic cancer. | Scoping review conducted following PRISMA-ScR guidelines. Two reviewers independently performed study selection and data extraction | Initially identified 18,285 articles from various databases. After screening and exclusion, 30 articles were included. |
| [64] | 2022 | Edge computing-based heart disease prediction. | Decision-tree-based classifier for analyzing health data. Pre-trained machine learning processing module for analysis | The decision tree classifier shows 99% accuracy for classifying the subject’s position. The decision tree classifier shows 98% accuracy for heart disease prediction. |
| [77] | 2023 | Clinical language models for a wide range of clinical and operational predictive tasks. | Pretraining datasets: NYU Notes, NYU Notes-Manhattan, NYU Notes-Brooklyn. Fine-tuning datasets: NYU Readmission | NYUTron has an AUC of 78.7–94.9%. NYUTron improves the AUC by 5.36–14.7% compared to traditional models. |
| [78] | 2023 | Prediction of mental health problems after military deployment. | Neural network models used for prediction. Pre-deployment registry data combined with post-deployment questionnaire data | Approximately 95% of participants were male. The percentage of individuals deployed in a combat unit was highest for the first deployment (32.7%), compared to the second (25.6%) and the third (20.8%) deployment. |
| [65] | 2022 | Early-stage Alzheimer’s prediction. | Decision tree, random forest, Support Vector Machine, Gradient Boosting, and voting classifiers. Machine learning techniques applied to Alzheimer’s disease datasets. | Evaluation metrics: precision, recall, accuracy. Men are more likely to have dementia than women. Achieved 83% accuracy on test data |
| [57] | 2014 | Risk predictive modeling for diabetes and cardiovascular disease | Collection of data during a prospective study. Estimation of regression coefficients for predictor–outcome association | Emphasizes the importance of validating existing CVD and diabetes prediction models to improve their adoption in routine practice. |
| [68] | 2019 | Identifications of patients at risk of uncontrolled hypertension. | Logistic regression and recurrent neural networks | Best model achieved an AUROC of 0.719. Linear models performed better than recurrent neural networks |
| [79] | 2021 | Predicting critical state after COVID-19 diagnosis | Prognostic model trained on US electronic health records. Feature reduction process based on SHAP values | ROC AUC: 0.861 [0.838, 0.883]. Precision–recall AUC: 0.434 [0.414, 0.485] |
| [61] | 2022 | Machine learning for healthcare wearable devices. | Homomorphic Encryption (HE). Secure Multiparty Computation (SMPC) | Review of different areas of machine learning research for wearable healthcare devices. |
| [58] | 2018 | Clinical prediction models (CPMs) with statistical updating models. | Regression coefficient updating. Meta-model updating | Original ES overestimated mortality (calibration intercept—1.06, slope—0.97). All updating strategies improved calibration performance. |
| [80] | 2019 | Continuous risk predictions for acute kidney injury. | Binary variable prediction for AKI occurrence. Eight future time horizons for predictions. | Model achieves a higher ROC AUC in shorter time windows. The model achieves a lower PR AUC in shorter time windows. |
| [71] | 2019 | Deep learning models for early prediction of acute adverse events. | Developing deep learning continuous risk models. Integrating domain knowledge into the technical specification | Continuous risk models identified 55.8% of AKI cases up to 48 h early with a false positive rate of 2:1. The model correctly predicted 90.2% of AKI cases requiring dialysis within 90 days. |
| [48] | 2020 | AI in digital pathology for breast cancer diagnosis. | Image analysis with deep learning (DL). Non-CNN algorithms for segmentation and detection | Review of the basics of digital pathology and AI and the challenges in the field. |
6. Federated Learning for Early Health Prediction
- Preserving Data Privacy: In federated learning, patient data are securely stored on edge devices such as medical devices and wearables without being transferred to a central server for storage. This decentralized approach ensures strict data privacy and security and mitigates the risk of data breaches or violations.
- Access to Multiple Data Sources: Federated learning enables healthcare providers to access diverse patient data collected by wearables and medical devices. This data diversity promotes the development of more robust and accurate predictive models by encompassing a wide range of health-related information from multiple sources.
- Leveraging Large-Scale Data: With federated learning, healthcare providers can leverage a vast amount of data from a distributed patient network. By aggregating and combining these disparate datasets, healthcare professionals can build comprehensive models capable of capturing nuanced patterns and early health indicators, resulting in highly accurate predictions and timely interventions.
- Continuous Learning and Adaptation: As patients continuously use wearables and medical devices, new data become available over time. Federated learning facilitates continuous training of the model and adaptation to changing health conditions. The global model can be periodically updated with the latest aggregated parameters to incorporate new knowledge and improve the system’s predictive capabilities.
- Personalized and Adaptive Models: Federated learning facilitates the creation of personalized models tailored to individual patients. By training local models based on their specific data, the system can tailor predictions and interventions to individual health profiles, leading to highly personalized healthcare and early detection of health problems.
- Reduced Data Transfer and Computational Overhead: Federated learning minimizes the need to transfer huge amounts of raw patient data to a central server. Instead, the focus is on transferring aggregated model parameters, significantly reducing bandwidth requirements and computational overhead while carefully protecting the privacy of patient data.
- Collaborative Research and Knowledge Sharing: Federated learning promotes collaborative research and knowledge sharing among healthcare providers by pooling anonymized, aggregated parameters, insights, and discoveries can be shared without compromising patient privacy. This collective intelligence accelerates medical progress and improves early health prediction capabilities.
6.1. Federated Learning Methodology
- Data Distribution: The training data are distributed across multiple edge devices. Each device holds its own local data, which may be collected from different sources or users.
- Local Model Training: A local model is trained using its own local data on each edge device. The training process can be performed using various machine learning algorithms and techniques.
- Model Aggregation: After the local model training, the updated models from each edge device are sent to a central server or aggregator. The aggregator collects the models and performs model aggregation techniques, such as averaging or weighted averaging, to create a global model.
- Model Update: The global model is then sent back to the edge devices, where it replaces the local models. This updated global model incorporates the knowledge learned from all the edge devices’ local models.
- Iterative Process: The above steps are repeated iteratively, allowing the edge devices to continuously improve the global model by training on their local data. This iterative process helps capture the data diversity across different edge devices and improve the overall model performance.
- ∑ indicates the summation of local models across all edge devices.
- is the normalization factor to ensure that the aggregation results in an averaged global model.
- represents the weight assigned to the edge device i. Factors such as the amount of locally available data and the computational capacity of the edge device are considered in determining these weights.
- ∑ represents the sum of the weighted local models across all edge devices.
| Algorithm 1 Federated Learning with Averaging |
| Require: Global model W, Edge devices , Learning rate , Rounds T Ensure: Updated global model W
|
| Algorithm 2 Federated Learning with Weighted Averaging |
| Require: Global model W, Edge devices , Learning rate , Rounds T Ensure: Updated global model W
|
- SMPCAggregation is the secure multi-party computation aggregation function.
6.2. Federated Learning for Disease and Mortality Prediction
6.2.1. Cardiovascular Diseases
6.2.2. Heart Diseases
6.2.3. Chronic Kidney Diseases
6.2.4. Rare Diseases
6.2.5. ICU Mortality
6.2.6. COVID-19 Mortality
7. Challenges of Edge AI in Early Health Prediction and Future Directions
7.1. Privacy and Security
7.1.1. Privacy
- Data collection: Edge AI relies on collecting vast amounts of personal health data, including medical records, biometric data, and lifestyle information. Safeguarding the privacy of this sensitive data is crucial.
- Informed consent: Obtaining informed consent from individuals for data collection and usage can be challenging. Clear communication about the purpose, risks, and benefits of using their data in early health prediction is essential.
- Data anonymization: Anonymizing health data is critical to protecting individuals’ privacy. However, achieving complete anonymity while maintaining data utility for accurate predictions can be a complex task.
- Privacy-preserving algorithms: Developing advanced algorithms that can perform accurate health prediction while preserving privacy is a promising research direction. Techniques like federated learning and differential privacy can help achieve this goal.
- Consent mechanisms: Exploring innovative consent mechanisms that empower individuals to have more control over their data and make informed decisions regarding data usage in early health prediction.
- Privacy-enhancing technologies: Investigating the use of privacy-enhancing technologies such as secure multi-party computation (SMPC), differential privacy, and homomorphic encryption to enable analysis of sensitive health data without compromising privacy.
- Policy and regulation: Establishing comprehensive policies and regulations that govern the collection, storage, and usage of health data in Edge AI systems. This includes ensuring compliance with privacy laws and implementing ethical frameworks.
7.1.2. Security
- Data breaches: Edge AI systems store and process sensitive health data, making them potential targets for cyberattacks. Robust security measures must be in place to prevent unauthorized access and data breaches.
- Secure communication: Edge AI systems often rely on transmitting data between devices and cloud servers. Ensuring secure communication channels and encryption protocols is vital to protect data during transmission.
- Adversarial attacks: Edge AI models can be vulnerable to adversarial attacks, where malicious actors manipulate input data to deceive the system. Developing robust defenses against such attacks is crucial to maintaining the integrity of early health prediction.
- Robust authentication: Exploring advanced authentication mechanisms, such as multi-factor authentication and biometrics, to enhance the security of Edge AI systems and prevent unauthorized access.
- Secure hardware and firmware: Enhancing the security of edge devices, such as wearables and IoT devices, by implementing secure hardware components and regularly updating the firmware to mitigate potential vulnerabilities.
- Intrusion detection and prevention: Developing sophisticated intrusion detection and prevention systems specifically designed for Edge AI in early health prediction. This helps detect and mitigate potential security breaches.
- Resilient AI models: Designing AI models that are resilient to adversarial attacks and can identify and reject manipulated input data, ensuring the accuracy and trustworthiness of early health predictions.
7.2. Data Quality and Accuracy
- Labeling and Annotation: High-quality labeled data are crucial for training accurate and reliable AI models. However, in early health prediction, obtaining ground truth labels can be challenging. This may require expert knowledge, clinical validation, or long-term follow-up to confirm the accuracy of predictions.
- Data Variability: Health data collected at the edge can be highly variable due to various factors such as device sensors, user behavior, environmental conditions, and data collection protocols [97]. This variability can impact the performance and generalizability of AI models, making it essential to address data variability challenges.
- Data Imbalance: In health prediction tasks, class imbalances are common, where certain health conditions or outcomes may be significantly less frequent than others [98]. This can lead to biased models that perform poorly on minority classes. Techniques such as data augmentation, oversampling, or ensemble methods need to be explored to address data imbalance challenges.
- Data Quality Control: Ensuring the quality and reliability of collected health data is critical. Sensor errors, noise, missing values, and data corruption can negatively impact the performance of AI models [99]. Quality control mechanisms, data preprocessing techniques, and outlier detection methods need to be developed to improve data quality.
- Data Augmentation Techniques: Exploring data augmentation methods specifically tailored for health data to increase the diversity and size of the training dataset, improving model robustness and generalizability.
- Collaborative Data Sharing: Encouraging collaboration and data sharing among healthcare institutions while ensuring privacy and security. Pooling diverse datasets can help overcome data variability and improve the representativeness of AI models.
- Data Quality Assessment Frameworks: Developing standardized frameworks to assess the quality and reliability of health data collected at the edge. This can involve metrics, guidelines, and best practices for data collection, labeling, and preprocessing.
7.3. Model Bias
- Dataset Bias: AI models are trained on datasets that may not be representative of the diverse population they aim to serve. Biases in the data, such as under-representation of certain demographics or health conditions, can lead to biased predictions and inequitable healthcare outcomes [100].
- Algorithmic Bias: Biases can also be introduced through the design and implementation of AI algorithms [101]. If the training data contain inherent biases or if the algorithm itself is biased, this can perpetuate and amplify existing disparities in healthcare.
- Interpretability and Transparency: Lack of interpretability and transparency in AI models can make it challenging to identify and address biases. Understanding how the model makes predictions and uncovering any underlying biases require explainable AI techniques [102].
- Bias Detection and Mitigation: Designing methods to detect and quantify bias in AI models and developing techniques to mitigate its impact. This can include techniques like debiasing algorithms, data augmentation, and fairness-aware feature selection.
- Diverse and Representative Datasets: Collecting and using diverse and representative datasets that encompass different demographics, health conditions, and socio-economic backgrounds. This helps reduce dataset bias and improves the generalizability of AI models.
- Ethical Guidelines and Regulations: Establishing clear ethical guidelines and regulations for the development and deployment of AI in healthcare. This can help address biases, promote fairness, and ensure accountability and transparency in early health prediction.
- Collaboration and Interdisciplinary Research: Encouraging collaboration between AI researchers, healthcare professionals, ethicists, and policymakers to collectively address model bias challenges. Interdisciplinary research can provide a holistic perspective and help develop comprehensive solutions.
7.4. Interoperability
- Heterogeneous Data Sources: In early health prediction, data are collected from various sources such as wearable devices, electronic health records, and sensors. These sources often use different data formats, protocols, and standards, making it challenging to integrate and analyze data seamlessly.
- Data Integration and Fusion: Aggregating and fusing data from multiple sources are essential for building comprehensive AI models. However, the lack of interoperability can hinder this process, leading to difficulties in harmonizing and combining heterogeneous data effectively.
- Connectivity and Communication: Edge AI systems rely on efficient communication between edge devices, cloud infrastructure, and central servers. Interoperability issues can arise due to differences in communication protocols, network connectivity, and compatibility between devices and systems.
- Privacy and Security Concerns: Interoperability can raise privacy and security concerns, especially when sensitive health data are shared or exchanged between different systems. Ensuring secure data transmission, secure access controls, and compliance with privacy regulations becomes crucial.
- Standardization and Data Formats: Developing standardized data formats, protocols, and interfaces for health data exchange. This enables seamless interoperability between different systems and facilitates data integration and analysis.
- Ontologies and Semantic Interoperability: Utilizing ontologies and semantic models to establish a common understanding of health data and data relationships. This promotes interoperability by enabling efficient data integration, data mapping, and knowledge sharing across different platforms.
- Interoperability Frameworks and Middleware: Designing interoperability frameworks and middleware that facilitate data exchange, communication, and integration among diverse edge devices, cloud systems, and healthcare infrastructure. These frameworks can provide standard APIs, data transformation capabilities, and connectivity support.
- Secure Data Sharing and Privacy-Preserving Mechanisms: Developing secure and privacy-preserving methods for data sharing and exchange. Techniques such as federated learning, differential privacy, and encryption can enable collaborative analysis while protecting sensitive health information.
- Collaborative Ecosystem: Encouraging collaboration between stakeholders, including researchers, healthcare providers, device manufacturers, and policymakers, to establish interoperability standards, guidelines, and best practices. Collaboration can drive the adoption of interoperable solutions and facilitate the seamless integration of Edge AI systems in healthcare.
7.5. Integration with Existing Health Systems
- Compatibility with Legacy Systems: Many healthcare organizations have established legacy systems and infrastructure that may not be designed to integrate with newer Edge AI technologies. These systems often have different data formats, protocols, and interfaces, making it difficult to seamlessly incorporate Edge AI solutions.
- Data Synchronization and Exchange: Integrating Edge AI for early health prediction requires smooth data synchronization and exchange between edge devices, cloud platforms, and existing healthcare systems. Ensuring data consistency, real-time updates, and bidirectional communication becomes crucial for effective integration.
- Workflow and Process Alignment: Integrating Edge AI into existing healthcare systems requires careful consideration of workflow and process alignment. The introduction of Edge AI should seamlessly fit into existing clinical workflows, ensuring minimal disruption and maximizing efficiency.
- Interoperability Standards: Developing industry-wide interoperability standards and guidelines that facilitate the integration of Edge AI technologies with existing healthcare systems. These standards should address data formats, communication protocols, and interoperability interfaces to ensure seamless integration [103].
- Application Programming Interfaces (APIs): Creating standardized APIs that enable easy integration between Edge AI systems and existing healthcare systems. These APIs should provide clear specifications for data exchange, functionality access, and system integration, simplifying the integration process.
- Middleware and Integration Platforms: Designing middleware and integration platforms specifically tailored for integrating Edge AI into existing healthcare systems. These platforms can provide tools, libraries, and frameworks that facilitate data integration, process alignment, and workflow integration.
- Proof-of-Concept Projects: Conducting pilot projects and proof-of-concept studies to demonstrate the feasibility and benefits of integrating Edge AI in early health prediction with existing healthcare systems. These projects can showcase successful integration strategies, identify challenges, and provide insights for future implementation.
- Collaboration and Partnerships: Encouraging collaboration and partnerships between Edge AI solution providers and healthcare organizations. Close collaboration can help identify integration requirements, co-design solutions, and establish a mutually beneficial integration process.
8. Conclusions
Funding
Conflicts of Interest
Sample Availability
References
- Yu, K.H.; Beam, A.L.; Kohane, I.S. Artificial intelligence in healthcare. Nat. Biomed. Eng. 2018, 2, 719–731. [Google Scholar] [CrossRef]
- Malik, P.; Pathania, M.; Rathaur, V.K. Overview of artificial intelligence in medicine. J. Family Med. Prim. Care 2019, 8, 2328–2331. [Google Scholar]
- Bohr, A.; Memarzadeh, K. Artificial Intelligence in Healthcare; Academic Press: Cambridge, MA, USA, 2020. [Google Scholar]
- Rong, G.; Mendez, A.; Bou Assi, E.; Zhao, B.; Sawan, M. Artificial Intelligence in Healthcare: Review and Prediction Case Studies. Proc. Est. Acad. Sci. Eng. 2020, 6, 291–301. [Google Scholar] [CrossRef]
- Shi, W.; Cao, J.; Zhang, Q.; Li, Y.; Xu, L. Edge Computing: Vision and Challenges. IEEE Internet Things J. 2016, 3, 637–646. [Google Scholar] [CrossRef]
- Satyanarayanan, M. The Emergence of Edge Computing. Computer 2017, 50, 30–39. [Google Scholar] [CrossRef]
- Ray, P.P.; Dash, D.; De, D. Edge computing for Internet of Things: A survey, e-healthcare case study and future direction. J. Netw. Comput. Appl. 2019, 140, 1–22. [Google Scholar] [CrossRef]
- Sodhro, A.H.; Luo, Z.; Sangaiah, A.K.; Baik, S.W. Mobile edge computing based QoS optimization in medical healthcare applications. Int. J. Inf. Manag. 2019, 45, 308–318. [Google Scholar] [CrossRef]
- Kamruzzaman, M.M.; Alrashdi, I.; Alqazzaz, A. New Opportunities, Challenges, and Applications of Edge-AI for Connected Healthcare in Internet of Medical Things for Smart Cities. J. Healthc. Eng. 2022, 2022, 2950699. [Google Scholar] [CrossRef]
- Rathi, V.K.; Rajput, N.K.; Mishra, S.; Grover, B.A.; Tiwari, P.; Jaiswal, A.K.; Hossain, M.S. An edge AI-enabled IoT healthcare monitoring system for smart cities. Comput. Electr. Eng. 2021, 96, 107524. [Google Scholar] [CrossRef]
- Dong, J.; Feng, T.; Thapa-Chhetry, B.; Cho, B.G.; Shum, T.; Inwald, D.P.; Newth, C.J.L.; Vaidya, V.U. Machine learning model for early prediction of acute kidney injury (AKI) in pediatric critical care. Crit. Care 2021, 25, 288. [Google Scholar] [CrossRef]
- Layeghian Javan, S.; Sepehri, M.M.; Layeghian Javan, M.; Khatibi, T. An intelligent warning model for early prediction of cardiac arrest in sepsis patients. Comput. Methods Programs Biomed. 2019, 178, 47–58. [Google Scholar] [CrossRef]
- Hong, W.; Lee, W.G. Wearable sensors for continuous oral cavity and dietary monitoring toward personalized healthcare and digital medicine. Analyst 2021, 145, 7796–7808. [Google Scholar] [CrossRef] [PubMed]
- Thipsawat, S. Early detection of diabetic nephropathy in patient with type 2 diabetes mellitus: A review of the literature. Diab. Vasc. Dis. Res. 2021, 18, 14791641211058856. [Google Scholar] [CrossRef] [PubMed]
- Wander, G.S.; Bansal, M.; Kasliwal, R.R. Prediction and early detection of cardiovascular disease in South Asians with diabetes mellitus. Diabetes Metab. Syndr. 2020, 14, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, J.D.; Fisher, P.G.; Gibbs, P. Early detection of cancer: Past, present, and future. Am. Soc. Clin. Oncol. Educ. Book 2015, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Zhu, S.; Wen, N. Deep reinforcement learning and its applications in medical imaging and radiation therapy: A survey. Phys. Med. Biol. 2022, 67, 22TR02. [Google Scholar] [CrossRef]
- Montagnon, E.; Cerny, M.; Cadrin-Chênevert, A.; Hamilton, V.; Derennes, T.; Ilinca, A.; Vandenbroucke-Menu, F.; Turcotte, S.; Kadoury, S.; Tang, A. Deep learning workflow in radiology: A primer. Insights Imaging 2020, 11, 22. [Google Scholar] [CrossRef]
- Cao, C.; Liu, F.; Tan, H.; Song, D.; Shu, W.; Li, W.; Zhou, Y.; Bo, X.; Xie, Z. Deep Learning and Its Applications in Biomedicine. Genom. Proteom. Bioinform. 2018, 16, 17–32. [Google Scholar] [CrossRef]
- Moshawrab, M.; Adda, M.; Bouzouane, A.; Ibrahim, H.; Raad, A. Reviewing Federated Machine Learning and Its Use in Diseases Prediction. Sensors 2023, 23, 2112. [Google Scholar] [CrossRef]
- Moshawrab, M.; Adda, M.; Bouzouane, A.; Ibrahim, H.; Raad, A. Smart Wearables for the Detection of Cardiovascular Diseases: A Systematic Literature Review. Sensors 2023, 23, 828. [Google Scholar] [CrossRef]
- Garcia Lopez, P.; Montresor, A.; Epema, D.; Datta, A.; Higashino, T.; Iamnitchi, A.; Barcellos, M.; Felber, P.; Riviere, E. Edge-centric Computing: Vision and Challenges. SIGCOMM Comput. Commun. Rev. 2015, 45, 37–42. [Google Scholar] [CrossRef]
- Grand View Research. Edge Computing Market Size, Share & Growth Report, 2023–2030. Available online: https://www.grandviewresearch.com/industry-analysis/edge-computing-market (accessed on 16 February 2023).
- Mohsen, F.; Ali, H.; El Hajj, N.; Shah, Z. Artificial intelligence-based methods for fusion of electronic health records and imaging data. Sci. Rep. 2022, 12, 17981. [Google Scholar] [CrossRef]
- Briganti, G.; Le Moine, O. Artificial Intelligence in Medicine: Today and Tomorrow. Front. Med. 2020, 7, 27. [Google Scholar] [CrossRef]
- Lavecchia, A. Deep learning in drug discovery: Opportunities, challenges and future prospects. Drug Discov. Today 2019, 24, 2017–2032. [Google Scholar] [CrossRef] [PubMed]
- Mak, K.K.; Pichika, M.R. Artificial intelligence in drug development: Present status and future prospects. Drug Discov. Today 2019, 24, 773–780. [Google Scholar] [CrossRef]
- Jiménez-Luna, J.; Grisoni, F.; Weskamp, N.; Schneider, G. Artificial intelligence in drug discovery: Recent advances and future perspectives. Expert Opin. Drug Discov. 2021, 16, 949–959. [Google Scholar] [CrossRef] [PubMed]
- Topol, E.J. High-performance medicine: The convergence of human and artificial intelligence. Nat. Med. 2019, 25, 44–56. [Google Scholar] [CrossRef]
- Adegun, A.A.; Viriri, S.; Ogundokun, R.O. Deep Learning Approach for Medical Image Analysis. Comput. Intell. Neurosci. 2021, 2021, 6215281. [Google Scholar] [CrossRef]
- Fraiwan, M.; Audat, Z.; Fraiwan, L.; Manasreh, T. Using deep transfer learning to detect scoliosis and spondylolisthesis from X-ray images. PLoS ONE 2022, 17, e0267851. [Google Scholar] [CrossRef]
- Panayides, A.S.; Amini, A.; Filipovic, N.D.; Sharma, A.; Tsaftaris, S.A.; Young, A.; Foran, D.; Do, N.; Golemati, S.; Kurc, T.; et al. AI in Medical Imaging Informatics: Current Challenges and Future Directions. IEEE J. Biomed. Health Inform. 2020, 24, 1837–1857. [Google Scholar] [CrossRef]
- Coronato, A.; Naeem, M.; De Pietro, G.; Paragliola, G. Reinforcement learning for intelligent healthcare applications: A survey. Artif. Intell. Med. 2020, 109, 101964. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Chatterjee, K. Edge computing based secure health monitoring framework for electronic healthcare system. Clust. Comput. 2022, 26, 1205–1220. [Google Scholar] [CrossRef]
- Klonoff, D.C. Fog Computing and Edge Computing Architectures for Processing Data From Diabetes Devices Connected to the Medical Internet of Things. J. Diabetes Sci. Technol. 2017, 11, 647–652. [Google Scholar] [CrossRef]
- American Diabetes Association. What Is a Smart Insulin Pen? 2023. Available online: https://diabetes.org/about-diabetes/devices-technology/smart-insulin-pen (accessed on 18 February 2023).
- Kamga, P.; Mostafa, R.; Zafar, S. The Use of Wearable ECG Devices in the Clinical Setting: A Review. Curr. Emerg. Hosp. Med. Rep. 2022, 10, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Findair. IoT with the Use of Smart Inhalers-Resources-Blog. 2021. Available online: http://findair.eu/resources/blog/iot-with-the-use-of-smart-inhalers/ (accessed on 18 February 2023).
- Dey, A.; Haque, K.A.; Nayan, A.A.; Kibria, M.G. IoT Based Smart Inhaler For Context-Aware Service Provisioning. In Proceedings of the 2020 2nd International Conference on Advanced Information and Communication Technology (ICAICT), Dhaka, Bangladesh, 28–29 November 2020; pp. 410–415. [Google Scholar]
- Mohan, H.M.; Anitha, S.; Chai, R.; Ling, S.H. Edge Artificial Intelligence: Real-Time Noninvasive Technique for Vital Signs of Myocardial Infarction Recognition Using Jetson Nano. Adv. Hum.-Comput. Interact. 2021, 2021, 6483003. [Google Scholar] [CrossRef]
- Islam, K.; Alam, F.; Zahid, A.I.; Khan, M.M.; InamAbbasi, M. Internet of Things- (IoT-) Based Real-Time Vital Physiological Parameter Monitoring System for Remote Asthma Patients. Proc. Int. Wirel. Commun. Mob. Comput. Conf. 2022, 2022, 1191434. [Google Scholar] [CrossRef]
- Paul, A.; Pinjari, H.; Hong, W.H.; Seo, H.C.; Rho, S. Fog Computing-Based IoT for Health Monitoring System. J. Sens. 2018, 2018, 1386470. [Google Scholar] [CrossRef]
- Jiang, Q.; Zhou, X.; Wang, R.; Ding, W.; Chu, Y.; Tang, S.; Jia, X.; Xu, X. Intelligent monitoring for infectious diseases with fuzzy systems and edge computing: A survey. Appl. Soft Comput. 2022, 123, 108835. [Google Scholar] [CrossRef]
- Zhu, G.; Li, J.; Meng, Z.; Yu, Y.; Li, Y.; Tang, X.; Dong, Y.; Sun, G.; Zhou, R.; Wang, H.; et al. Learning from Large-Scale Wearable Device Data for Predicting the Epidemic Trend of COVID-19. Discrete Dyn. Nat. Soc. 2020, 2020, 6152041. [Google Scholar] [CrossRef]
- Alanazi, R. Identification and Prediction of Chronic Diseases Using Machine Learning Approach. J. Healthc. Eng. 2022, 2022, 2826127. [Google Scholar] [CrossRef]
- Manjulatha, B.; Pabboju, S. An Ensemble Model for Predicting Chronic Diseases Using Machine Learning Algorithms. In Smart Computing Techniques and Applications; Springer: Singapore, 2021; pp. 337–345. [Google Scholar]
- Chhabra, D.; Juneja, M.; Chutani, G. An efficient ensemble based machine learning approach for predicting Chronic Kidney Disease. Curr. Med. Imaging Rev. 2023. Online ahead of print. [Google Scholar]
- Ibrahim, A.; Gamble, P.; Jaroensri, R.; Abdelsamea, M.M.; Mermel, C.H.; Chen, P.H.C.; Rakha, E.A. Artificial intelligence in digital breast pathology: Techniques and applications. Breast 2020, 49, 267–273. [Google Scholar] [CrossRef]
- Jan, Z.; El Assadi, F.; Abd-Alrazaq, A.; Jithesh, P.V. Artificial Intelligence for the Prediction and Early Diagnosis of Pancreatic Cancer: Scoping Review. J. Med. Internet Res. 2023, 25, e44248. [Google Scholar] [CrossRef]
- Huang, J.D.; Wang, J.; Ramsey, E.; Leavey, G.; Chico, T.J.A.; Condell, J. Applying Artificial Intelligence to Wearable Sensor Data to Diagnose and Predict Cardiovascular Disease: A Review. Sensors 2022, 22, 8002. [Google Scholar] [CrossRef]
- Tran, N.K.; Kretsch, C.; LaValley, C.; Rashidi, H.H. Machine learning and artificial intelligence for the diagnosis of infectious diseases in immunocompromised patients. Curr. Opin. Infect. Dis. 2023, 36, 235. [Google Scholar] [CrossRef]
- Parums, D.V. Editorial: Infectious Disease Surveillance Using Artificial Intelligence (AI) and its Role in Epidemic and Pandemic Preparedness. Med. Sci. Monit. 2023, 29, e941209-1–e941209-4. [Google Scholar] [CrossRef]
- Shah, W.; Aleem, M.; Iqbal, M.A.; Islam, M.A.; Ahmed, U.; Srivastava, G.; Lin, J.C.W. A Machine-Learning-Based System for Prediction of Cardiovascular and Chronic Respiratory Diseases. J. Healthc. Eng. 2021, 2021, 2621655. [Google Scholar] [CrossRef]
- Ramesh, T.R.; Lilhore, U.K.; Poongodi, M.; Simaiya, S.; Kaur, A.; Hamdi, M. Predictive analysis of heart diseases with machine learning approaches. Malays. J. Comput. Sci. 2022, 2022, 132–148. [Google Scholar]
- Chaki, J.; Thillai Ganesh, S.; Cidham, S.K.; Ananda Theertan, S. Machine learning and artificial intelligence based Diabetes Mellitus detection and self-management: A systematic review. J. King Saud Univ. Comput. Inf. Sci. 2022, 34, 3204–3225. [Google Scholar] [CrossRef]
- Dayan, I.; Roth, H.R.; Zhong, A.; Harouni, A.; Gentili, A.; Abidin, A.Z.; Liu, A.; Costa, A.B.; Wood, B.J.; Tsai, C.S.; et al. Federated learning for predicting clinical outcomes in patients with COVID-19. Nat. Med. 2021, 27, 1735–1743. [Google Scholar] [CrossRef]
- Kengne, A.P.; Masconi, K.; Mbanya, V.N.; Lekoubou, A.; Echouffo-Tcheugui, J.B.; Matsha, T.E. Risk predictive modelling for diabetes and cardiovascular disease. Crit. Rev. Clin. Lab. Sci. 2014, 51, 1–12. [Google Scholar] [CrossRef]
- Su, T.L.; Jaki, T.; Hickey, G.L.; Buchan, I.; Sperrin, M. A review of statistical updating methods for clinical prediction models. Stat. Methods Med. Res. 2018, 27, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Chapman, B.P.; Lin, F.; Roy, S.; Benedict, R.H.B.; Lyness, J.M. Health risk prediction models incorporating personality data: Motivation, challenges, and illustration. Personal. Disord. 2019, 10, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Beniczky, S.; Karoly, P.; Nurse, E.; Ryvlin, P.; Cook, M. Machine learning and wearable devices of the future. Epilepsia 2021, 62 (Suppl. S2), S116–S124. [Google Scholar] [CrossRef] [PubMed]
- Sabry, F.; Eltaras, T.; Labda, W.; Alzoubi, K.; Malluhi, Q. Machine Learning for Healthcare Wearable Devices: The Big Picture. J. Healthc. Eng. 2022, 2022, 4653923. [Google Scholar] [CrossRef]
- Castelli Gattinara Di Zubiena, F.; Menna, G.; Mileti, I.; Zampogna, A.; Asci, F.; Paoloni, M.; Suppa, A.; Del Prete, Z.; Palermo, E. Machine Learning and Wearable Sensors for the Early Detection of Balance Disorders in Parkinson’s Disease. Sensors 2022, 22, 9903. [Google Scholar] [CrossRef]
- Chang, V.; Ganatra, M.A.; Hall, K.; Golightly, L.; Xu, Q.A. An assessment of machine learning models and algorithms for early prediction and diagnosis of diabetes using health indicators. Healthc. Anal. 2022, 2, 100118. [Google Scholar] [CrossRef]
- Jenifer, A.; Jeba, G.; Paulraj, L.; Kumar, N.; Yuvaraj, T.; Alen, G.; Rozario, P.; Amoli, R. Edge-based heart disease prediction device using internet of things. In Proceedings of the 2022 International Conference on Applied Artificial Intelligence and Computing (ICAAIC), Salem, India, 9–11 May 2022. [Google Scholar]
- Kavitha, C.; Mani, V.; Srividhya, S.R.; Khalaf, O.I.; Tavera Romero, C.A. Early-Stage Alzheimer’s Disease Prediction Using Machine Learning Models. Front. Public Health 2022, 10, 853294. [Google Scholar] [CrossRef]
- Futoma, J.; Morris, J.; Lucas, J. A comparison of models for predicting early hospital readmissions. J. Biomed. Inform. 2015, 56, 229–238. [Google Scholar] [CrossRef]
- Guo, A.; Mazumder, N.R.; Ladner, D.P.; Foraker, R.E. Predicting mortality among patients with liver cirrhosis in electronic health records with machine learning. PLoS ONE 2021, 16, e0256428. [Google Scholar] [CrossRef]
- Mohammadi, R.; Jain, S.; Agboola, S.; Palacholla, R.; Kamarthi, S.; Wallace, B.C. Learning to Identify Patients at Risk of Uncontrolled Hypertension Using Electronic Health Records Data. AMIA Jt. Summits Transl. Sci. Proc. 2019, 2019, 533–542. [Google Scholar]
- Nikhila. Chronic Kidney Disease Prediction using Machine Learning Ensemble Algorithm. In Proceedings of the 2021 International Conference on Computing, Communication, and Intelligent Systems (ICCCIS), Greater Noida, India, 19–20 February 2021; pp. 476–480. [Google Scholar]
- Khalid, H.; Khan, A.; Zahid Khan, M.; Mehmood, G.; Shuaib Qureshi, M. Machine Learning Hybrid Model for the Prediction of Chronic Kidney Disease. Comput. Intell. Neurosci. 2023, 2023, 9266889. [Google Scholar] [CrossRef]
- Tomašev, N.; Glorot, X.; Rae, J.W.; Zielinski, M.; Askham, H.; Saraiva, A.; Mottram, A.; Meyer, C.; Ravuri, S.; Protsyuk, I.; et al. Developing Deep Learning Continuous Risk Models for Early Adverse Event Prediction in Electronic Health Records: An AKI Case Study. Protoc. Exch. 2019. [Google Scholar] [CrossRef]
- Antunes, R.S.; André da Costa, C.; Küderle, A.; Yari, I.A.; Eskofier, B. Federated Learning for Healthcare: Systematic Review and Architecture Proposal. ACM Trans. Intell. Syst. Technol. 2022, 13, 1–23. [Google Scholar] [CrossRef]
- Nazir, S.; Kaleem, M. Federated Learning for Medical Image Analysis with Deep Neural Networks. Diagnostics 2023, 13, 1532. [Google Scholar] [CrossRef] [PubMed]
- Sohan, M.F.; Basalamah, A. A systematic review on federated learning in medical image analysis. IEEE Access 2023, 11, 28628–28644. [Google Scholar] [CrossRef]
- Ali, M.; Naeem, F.; Tariq, M.; Kaddoum, G. Federated Learning for Privacy Preservation in Smart Healthcare Systems: A Comprehensive Survey. IEEE J. Biomed. Health Inform. 2022, 27, 778–789. [Google Scholar] [CrossRef] [PubMed]
- Iwagami, M.; Matsui, H. Introduction to Clinical Prediction Models. Ann. Clin. Epidemiol. 2022, 4, 72–80. [Google Scholar] [CrossRef]
- Jiang, L.Y.; Liu, X.C.; Nejatian, N.P.; Nasir-Moin, M.; Wang, D.; Abidin, A.; Eaton, K.; Riina, H.A.; Laufer, I.; Punjabi, P.; et al. Health system-scale language models are all-purpose prediction engines. Nature 2023, 619, 357–362. [Google Scholar] [CrossRef]
- Karstoft, K.I.; Eskelund, K.; Gradus, J.L.; Andersen, S.B.; Nissen, L.R. Early prediction of mental health problems following military deployment: Integrating pre- and post-deployment factors in neural network models. J. Psychiatr. Res. 2023, 163, 109–117. [Google Scholar] [CrossRef]
- Rinderknecht, M.D.; Klopfenstein, Y. Predicting critical state after COVID-19 diagnosis: Model development using a large US electronic health record dataset. NPJ Digit. Med. 2021, 4, 113. [Google Scholar] [CrossRef]
- Tomašev, N.; Glorot, X.; Rae, J.W.; Zielinski, M.; Askham, H.; Saraiva, A.; Mottram, A.; Meyer, C.; Ravuri, S.; Protsyuk, I.; et al. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature 2019, 572, 116–119. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.C.; Pham, Q.V.; Pathirana, P.N.; Ding, M.; Seneviratne, A.; Lin, Z.; Dobre, O.; Hwang, W.J. Federated Learning for Smart Healthcare: A Survey. ACM Comput. Surv. 2022, 55, 1–37. [Google Scholar] [CrossRef]
- Yang, Q.; Liu, Y.; Chen, T.; Tong, Y. Federated Machine Learning: Concept and Applications. ACM Trans. Intell. Syst. Technol. 2019, 10, 1–19. [Google Scholar] [CrossRef]
- Beaussart, M.; Grimberg, F.; Hartley, M.A.; Jaggi, M. WAFFLE: Weighted averaging for personalized federated learning. arXiv 2021, arXiv:2110.06978. [Google Scholar]
- Kalapaaking, A.P.; Khalil, I.; Yi, X. Blockchain-based Federated Learning with SMPC Model Verification against Poisoning Attack for Healthcare Systems. arXiv 2023, arXiv:2304.13360. [Google Scholar] [CrossRef]
- Randl, K.; Armengol, N.L.; Mondrejevski, L.; Miliou, I. Early prediction of the risk of ICU mortality with Deep Federated Learning. In Proceedings of the 2023 IEEE 36th International Symposium on Computer-Based Medical Systems (CBMS), L’Aquila, Italy, 22–24 June 2023; pp. 706–711. [Google Scholar]
- Yaqoob, M.M.; Nazir, M.; Khan, M.A.; Qureshi, S.; Al-Rasheed, A. Hybrid Classifier-Based Federated Learning in Health Service Providers for Cardiovascular Disease Prediction. NATO Adv. Sci. Inst. Ser. E Appl. Sci. 2023, 13, 1911. [Google Scholar] [CrossRef]
- Bharathi, K.; Dhavamani, M.; Niranjan, K. A federated learning based approach for heart disease prediction. In Proceedings of the 2022 6th International Conference on Computing Methodologies and Communication (ICCMC), Erode, India, 29–31 March 2022. [Google Scholar]
- Nandhini, J.M.; Joshi, S.; Anuratha, K. Federated learning based prediction of chronic kidney diseases. In Proceedings of the 2022 1st International Conference on Computational Science and Technology (ICCST), Chennai, India, 9–10 November 2022. [Google Scholar]
- Farooq, K.; Syed, H.J.; Alqahtani, S.O.; Nagmeldin, W.; Ibrahim, A.O.; Gani, A. Blockchain Federated Learning for In-Home Health Monitoring. Electronics 2022, 12, 136. [Google Scholar] [CrossRef]
- Chen, B.; Chen, T.; Zeng, X.; Zhang, W.; Lu, Q.; Hou, Z.; Zhou, J.; Helal, S. DFML: Dynamic Federated Meta-Learning for Rare Disease Prediction. IEEE/ACM Trans. Comput. Biol. Bioinform. 2023. Online ahead of print. [Google Scholar]
- Vaid, A.; Jaladanki, S.K.; Xu, J.; Teng, S.; Kumar, A.; Lee, S.; Somani, S.; Paranjpe, I.; De Freitas, J.K.; Wanyan, T.; et al. Federated Learning of Electronic Health Records to Improve Mortality Prediction in Hospitalized Patients With COVID-19: Machine Learning Approach. JMIR Med. Inform. 2021, 9, e24207. [Google Scholar] [CrossRef] [PubMed]
- Vaid, A.; Jaladanki, S.K.; Xu, J.; Teng, S.; Kumar, A.; Lee, S.; Somani, S.; Paranjpe, I.; De Freitas, J.K.; Wanyan, T.; et al. Federated Learning of Electronic Health Records Improves Mortality Prediction in Patients Hospitalized with COVID-19. medRxiv 2020. Preprint. [Google Scholar]
- Jiang, D.; Shi, G. Research on Data Security and Privacy Protection of Wearable Equipment in Healthcare. J. Healthc. Eng. 2021, 2021, 6656204. [Google Scholar] [CrossRef]
- Arias, O.; Wurm, J.; Hoang, K.; Jin, Y. Privacy and Security in Internet of Things and Wearable Devices. IEEE Trans. Multi-Scale Comput. Syst. 2015, 1, 99–109. [Google Scholar] [CrossRef]
- Böttcher, S.; Vieluf, S.; Bruno, E.; Joseph, B.; Epitashvili, N.; Biondi, A.; Zabler, N.; Glasstetter, M.; Dümpelmann, M.; Van Laerhoven, K.; et al. Data quality evaluation in wearable monitoring. Sci. Rep. 2022, 12, 21412. [Google Scholar] [CrossRef]
- Poli, A.; Cosoli, G.; Scalise, L.; Spinsante, S. Impact of Wearable Measurement Properties and Data Quality on ADLs Classification Accuracy. IEEE Sens. J. 2021, 21, 14221–14231. [Google Scholar] [CrossRef]
- Souza, J.; Caballero, I.; Vasco Santos, J.; Lobo, M.; Pinto, A.; Viana, J.; Sáez, C.; Lopes, F.; Freitas, A. Multisource and temporal variability in Portuguese hospital administrative datasets: Data quality implications. J. Biomed. Inform. 2022, 136, 104242. [Google Scholar] [CrossRef]
- Khushi, M.; Shaukat, K.; Alam, T.M.; Hameed, I.A.; Uddin, S.; Luo, S.; Yang, X.; Reyes, M.C. A Comparative Performance Analysis of Data Resampling Methods on Imbalance Medical Data. IEEE Access 2021, 9, 109960–109975. [Google Scholar] [CrossRef]
- Isgut, M.; Gloster, L.; Choi, K.; Venugopalan, J.; Wang, M.D. Systematic Review of Advanced AI Methods for Improving Healthcare Data Quality in Post COVID-19 Era. IEEE Rev. Biomed. Eng. 2023, 16, 53–69. [Google Scholar] [CrossRef]
- Vaughn, J.; Baral, A.; Vadari, M.; Boag, W. Dataset Bias in Diagnostic AI systems: Guidelines for Dataset Collection and Usage. In Proceedings of the ACM Conference on Health, Inference and Learning, Toronto, ON, Canada, 2–4 April 2020. [Google Scholar]
- Agarwal, R.; Bjarnadottir, M.; Rhue, L.; Dugas, M.; Crowley, K.; Clark, J.; Gao, G. Addressing algorithmic bias and the perpetuation of health inequities: An AI bias aware framework. Health Policy Technol. 2023, 12, 100702. [Google Scholar] [CrossRef]
- Ennab, M.; Mcheick, H. Designing an Interpretability-Based Model to Explain the Artificial Intelligence Algorithms in Healthcare. Diagnostics 2022, 12, 1557. [Google Scholar] [CrossRef]
- Lee, Y.F. An Interoperability Solution for Legacy Healthcare Devices. IT Prof. 2015, 17, 51–57. [Google Scholar] [CrossRef]




| Ref. | Year | Application | Methods | Results | Limitations |
|---|---|---|---|---|---|
| [85] | 2022 | Prediction of ICU mortality risk | Deep federated learning, centralized machine learning, and local machine learning. | Federated learning performs equally well as the centralized approach. Federated learning is substantially better than the local approach. | - The generalizability of the approach beyond the MIMIC-III dataset needs to be tested. - Does not address the performance of the FL workflow in predicting ICU mortality at an early stage using other datasets. - Does not discuss potential challenges or limitations of implementing FL in a healthcare setting. |
| [20] | 2023 | Review of federated learning being used for early health prediction in diseases such as cardiovascular disease, diabetes, and cancer. | Federated learning and FL aggregation algorithms. | Federated learning helps solve privacy concerns in machine learning; 32% of companies plan to implement federated learning. | - FL in disease prediction is still in the early stages. - Limited real-world examples and use of smart wearables - The paper acknowledges that there is no unified classification of FL challenges in the literature |
| [86] | 2023 | Early prediction of cardiovascular disease. | Modified artificial bee colony optimization with Support Vector Machine (MABC-SVM). Federated matched averaging for the HSP server. | The proposed hybrid technique for federated learning improves the prediction accuracy by 1.5% and achieves a 1.6% fewer classification errors | - The paper does not mention any limitations of the proposed hybrid classifier-based FL framework. - The paper does discuss the limitations or constraints of the dataset used for testing and evaluation - No mention of ethical or legal considerations associated with the collection, sharing, and use of biomedical data in the proposed framework. |
| [87] | 2022 | Federated learning to predict heart disease by training a shared model while keeping patient data distributed across multiple locations. | Logistic regression and Support Vector Machine (SVM). | Accuracy of around 89% on the UCI benchmark dataset. | - The paper does not provide details on the size or diversity of the dataset used for training the shared model. - The paper does not provide a comparison of the FL approach with other existing machine learning methods for heart disease prediction. |
| [88] | 2022 | Federated learning to predict chronic kidney diseases | Federated learning and image processing technique to identify the affected area. | Higher accuracy, efficiency, specificity, and sensitivity. Increased accuracy through training with a single image. | - No mention of the size or diversity of the decentralized data used for training the algorithm. - Lack of information on the dataset used for training and testing the model - Insufficient explanation of the image processing techniques employed for identifying the affected area of the kidney. |
| [89] | 2022 | Combining the IoT and blockchain in healthcare. Focus on individualized health monitoring and early disease detection using wearable gadgets. | Combining the IoT and blockchain technologies and applying blockchain-based federated learning. | Blockchain-based federated learning offers benefits such as smarter simulations, lower latency, lower power consumption, and privacy. | - Limited battery life of IoT devices is a major obstacle to integrating blockchain with the IoT. - High processing and bandwidth requirements for blockchain integration |
| [90] | 2023 | Dynamic federated meta-learning approach to improve rare disease prediction using federated learning. | Dynamic federated meta-learning (DFML) and inaccuracy-focused meta-learning (IFML) approach. | The proposed model improves the prediction accuracy by 13.28% and outperforms the original federated meta-learning algorithm in accuracy and speed. | - Lack of information on the specific rare diseases studied and the datasets used for evaluation. - Does not provide details on the computational resources required for implementing the DFML approach. - Does not compare the proposed DFML approach with other state-of-the-art methods for rare disease prediction. |
| [91,92] | 2021 | Federated learning to predict mortality in hospitalized patients with COVID-19 within 7 days using electronic health record data. | Logistic regression with L1 regularization/least absolute shrinkage and selection operator (LASSO) and multilayer perceptron (MLP) | The LASSO federated model outperformed the LASSO local model at three hospitals. The MLP federated model performed better than the MLP local model at all five hospitals. | - The study was limited to data collected from hospitals within the Mount Sinai Health System in NYC. - The study only included clinical data in the models. - The study only implemented two widely used classifiers within the framework. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Badidi, E. Edge AI for Early Detection of Chronic Diseases and the Spread of Infectious Diseases: Opportunities, Challenges, and Future Directions. Future Internet 2023, 15, 370. https://doi.org/10.3390/fi15110370
Badidi E. Edge AI for Early Detection of Chronic Diseases and the Spread of Infectious Diseases: Opportunities, Challenges, and Future Directions. Future Internet. 2023; 15(11):370. https://doi.org/10.3390/fi15110370
Chicago/Turabian StyleBadidi, Elarbi. 2023. "Edge AI for Early Detection of Chronic Diseases and the Spread of Infectious Diseases: Opportunities, Challenges, and Future Directions" Future Internet 15, no. 11: 370. https://doi.org/10.3390/fi15110370
APA StyleBadidi, E. (2023). Edge AI for Early Detection of Chronic Diseases and the Spread of Infectious Diseases: Opportunities, Challenges, and Future Directions. Future Internet, 15(11), 370. https://doi.org/10.3390/fi15110370






