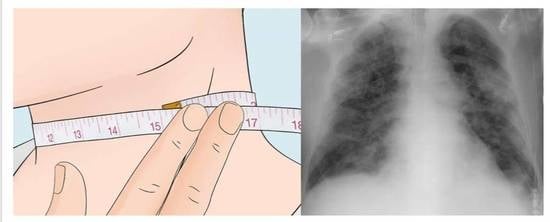
Neck Circumference Predicts Mortality in Hospitalized COVID-19 Patients
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thomas, K.S.; Zhang, W.; Dosa, D.M.; Carder, P.; Sloane, P.; Zimmerman, S. Estimation of Excess Mortality Rates Among US Assisted Living Residents During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2113411. [Google Scholar] [CrossRef]
- Guo, W.; Li, M.; Dong, Y. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab. Res. Rev. 2020, 36, e3319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carter, S.J.; Baranauskas, M.N.; Fly, A.D. Considerations for obesity, vitamin D, and physical activity amid the COVID-19 pandemic. Obesity 2020, 28, 1176–1177. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Murthy, S.; Diaz, J.V.; Slutsky, A.S.; Villar, J.; Angus, D.C.; Annane, D.; Azevedo, L.C.P.; Berwanger, O.; Cavalcanti, A.B.; et al. WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group. Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis. JAMA 2020, 324, 1330–1341. [Google Scholar]
- REMAP-CAP Investigators; ACTIV-4a Investigators; ATTACC Investigators. Therapeutic Anticoagulation with Heparin in Critically Ill Patients with COVID-19. N. Engl. J. Med. 2021, 385, 777–789. [Google Scholar] [CrossRef]
- Antonello, R.M.; Dal Bo, E.; De Cristofaro, P.; Luzzati, R.; Di Bella, S. The seXY side of COVID-19: What is behind female protection? Infez. Med. 2020, 2, 288–289. [Google Scholar]
- Chowdhury, A.I.; Alam, M.R.; Rabbi, M.F.; Rahman, T.; Reza, S. Does higher body mass index increase COVID-19 severity? A systematic review and meta-analysis. Obes. Med. 2021, 23, 100340. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Williams, C.; Vega, G.L. Upper body fat predicts metabolic syndrome similarly in men and women. Eur. J. Clin. Investig. 2018, 48, e12941. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saklayen, M.G. The global epidemic of the metabolic syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [Green Version]
- Srikanthan, K.; Feyh, A.; Visweshwar, H.; Shapiro, J.I.; Sodhi, K. Systematic Review of Metabolic Syndrome Biomarkers: A Panel for Early Detection, Management, and Risk Stratification in the West Virginian Population. Int. J. Med. Sci. 2016, 13, 25–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tal, S.; Litovchik, I.; Klar, M.M.; Maresky, H.S.; Grysman, N.; Wiser, I.; Vitkon-Barkay, I.; Marcus, G.; Tzuman, O.; Pereg, D.; et al. The association between neck adiposity and long-term outcome. PLoS ONE 2019, 14, e0215538. [Google Scholar] [CrossRef] [Green Version]
- Preis, S.R.; Massaro, J.M.; Hoffmann, U.; D’Agostino Sr, R.B.; Levy, D.; Robins, S.J.; Meigs, J.B.; Vasan, R.S.; O’Donnell, C.J.; Fox, C.S. Neck circumference as a novel measure of cardiometabolic risk: The framingham heart study. J. Clin. Endocrinol. Metab. 2010, 95, 3701–3710. [Google Scholar] [CrossRef] [Green Version]
- Di Bella, S.; Cesareo, R.; De Cristofaro, P.; Palermo, A.; Sanson, G.; Roman-Pognuz, E.; Zerbato, V.; Manfrini, S.; Giacomazzi, D.; Dal Bo, E.; et al. Neck circumference as reliable predictor of mechanical ventilation support in adult inpatients with COVID-19: A multicentric prospective evaluation. Diabetes Metab. Res. Rev. 2021, 37, e3354. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Meigs, J.B. Ectopic fat and cardiometabolic and vascular risk. Int. J. Cardiol. 2013, 169, 166–176. [Google Scholar] [CrossRef]
- Lim, S.; Meigs, J.B. Links between ectopic fat and vascular disease in humans. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1820–1826. [Google Scholar] [CrossRef] [Green Version]
- Assyov, Y.; Gateva, A.; Tsakova, A.; Kamenov, Z. A comparison of the clinical usefulness of neck circumference and waist circumference in individuals with severe obesity. Endocr. Res. 2017, 42, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Voncken, S.F.J.; Feron, T.M.H.; Laven, S.A.J.S.; Karaca, U.; Beerhorst, K.; Klarenbeek, P.; Straetmans, J.M.J.A.A.; de Vries, G.J.; Kolfoort-Otte, A.A.B.; de Kruif, M.D. Impact of obstructive sleep apnea on clinical outcomes in patients hospitalized with COVID-19. Sleep Breath. 2021, 24, 1–9. [Google Scholar] [CrossRef]
- Beal, M.; Chesson, A.; Garcia, T.; Caldito, G.; Stucker, F.; Nathan, C.O. A pilot study of quantitative aspiration in patients with symptoms of obstructive sleep apnea: Comparison to a historic control group. Laryngoscope 2004, 114, 965–968. [Google Scholar] [CrossRef]
- Nagappa, M.; Wong, D.T.; Cozowicz, C.; Ramachandran, S.K.; Memtsoudis, S.G.; Chung, F. Is obstructive sleep apnea associated with difcult airway? Evidence from a systematic review and meta-analysis of prospective and retrospective cohort studies. PLoS ONE 2018, 13, e0204904. [Google Scholar] [CrossRef]
- Nadeem, R.; Molnar, J.; Madbouly, E.M.; Nida, M.; Aggarwal, S.; Sajid, H.; Naseem, J.; Loomba, R. Serum infammatory markers in obstructive sleep apnea: A meta-analysis. J. Clin. Sleep Med. 2013, 9, 1003–1012. [Google Scholar] [CrossRef] [PubMed]
- Jose, R.J.; Manuel, A. COVID-19 cytokine storm: The interplay between infammation and coagulation. Lancet Respir. Med. 2020, 8, e46–e47. [Google Scholar] [CrossRef]

| Full Population | “Large Neck” | p-Value | ||
|---|---|---|---|---|
| No | Yes | |||
| Demographics | ||||
| Age (years) | 0.619 | |||
| 18–54 | 113 (28.5%) | 82 (26.7%) | 21 (23.3%) | |
| 55–65 | 101 (25.4%) | 74 (24.1%) | 26 (28.9%) | |
| 66–76 | 97 (24.4%) | 74 (24.1%) | 25 (27.8%) | |
| >76 | 86 (21.7%) | 77 (25.1%) | 18 (20.0%) | |
| Sex (male) | 272 (68.5%) | 210 (68.4%) | 62 (68.9%) | 0.931 |
| Comorbid conditions | ||||
| Body mass index ≥ 35 kg/m2 [375] | 32 (8.1%) | 7 (2.4%) | 25 (29.1%) | <0.001 |
| Arterial hypertension | 205 (51.6%) | 148 (48.4%) | 57 (63.3%) | 0.012 |
| Heart disease | 105 (26.4%) | 80 (26.1%) | 25 (27.8%) | 0.758 |
| Diabetes mellitus | 90 (22.7%) | 60 (19.5%) | 30 (33.3%) | 0.006 |
| Biochemical tests | ||||
| Lymphocytes < 1500/μL [392] | 345 (88.0%) | 263 (86.8%) | 82 (92.1%) | 0.173 |
| D-dimer > 500 ng/mL FEU [371] | 298 (80.3%) | 226 (79.3%) | 72 (83.7%) | 0.366 |
| Albumin < 3.5 g/dL [378] | 237 (62.7%) | 187 (63.6%) | 50 (59.5%) | 0.495 |
| C-reactive protein ≥ 1.0 mg/dL [387] | 349 (90.2%) | 262 (87.9%) | 87 (97.8%) | 0.003 |
| CRP-to-albumin ratio > 56.6 [369] | 54 (14.6%) | 38 (13.3%) | 16 (19.3%) | 0.174 |
| 30-Days Follow-Up | 60-Days Follow-Up | |||||
|---|---|---|---|---|---|---|
| Survived | Dead | p-Value | Survived | Dead | p-Value | |
| Demographics | ||||||
| Age > 76 years | 66 (19.1%) | 29 (55.8%) | <0.001 | 60 (18.0%) | 35 (55.6%) | <0.001 |
| Sex (male) | 240 (69.6%) | 32 (61.5%) | 0.245 | 233 (69.8%) | 39 (61.9%) | 0.218 |
| Comorbid conditions | ||||||
| Arterial hypertension | 170 (49.3%) | 35 (68.6%) | 0.010 | 160 (47.9%) | 45 (72.6%) | <0.001 |
| Heart disease | 74 (21.4%) | 31 (60.8%) | <0.001 | 69 (20.7%) | 36 (58.1%) | <0.001 |
| Diabetes mellitus | 67 (19.4%) | 23 (44.2%) | <0.001 | 64 (19.2%) | 26 (41.3%) | <0.001 |
| Biochemical tests | ||||||
| Lymphocytes < 1500/μL | 303 (88.9%) | 42 (82.4%) | 0.182 | 293 (88.8%) | 52 (83.9%) | 0.274 |
| D-dimer > 500 ng/mL FEU | 265 (79.1%) | 33 (91.7%) | 0.079 | 259 (79.2%) | 39 (88.6%) | 0.097 |
| Albumin < 3.5 g/dL | 197 (59.7%) | 40 (83.3%) | 0.002 | 189 (59.2%) | 48 (81.4%) | 0.001 |
| C-reactive protein ≥ 10 mg/L | 309 (90.4%) | 40 (88.9%) | 0.789 | 301 (90.7%) | 48 (87.3%) | 0.434 |
| CRP-to-Albumin ratio > 56.6 | 40 (12.2%) | 14 (34.1%) | <0.001 | 39 (12.3%) | 15 (29.4%) | 0.001 |
| Dependent Variable | Predictor | Unadjusted Risk a χ2; p-Value | Adjusted Risk b HR (95% CI); p-Value |
|---|---|---|---|
| 30-day mortality | “Large neck” phenotype | 3.515; 0.061 | 2.499 (1.180–5.294); 0.017 |
| Age > 77 years | / | 7.570 (3.309–17.317); <0.001 | |
| CRP-to-Albumin ratio > 56.6 | / | 2.620 (1.248–5.500); 0.011 | |
| Heart disease | / | 2.601 (1.246–5.428); 0.011 | |
| 60-day mortality | “Large neck” phenotype | 2.585; 0.108 | 2.257 (1.143–4.457); 0.019 |
| Age > 77 years | / | 6.547 (3.209–13.356); <0.001 | |
| CRP-to-Albumin ratio > 56.6 | / | 2.220 (1.115–4.419); 0.023 | |
| Heart disease | / | 2.338 (1.213–4.510); 0.011 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Bella, S.; Zerbato, V.; Sanson, G.; Roman-Pognuz, E.; De Cristofaro, P.; Palermo, A.; Valentini, M.; Gobbo, Y.; Jaracz, A.W.; Bozic Hrzica, E.; et al. Neck Circumference Predicts Mortality in Hospitalized COVID-19 Patients. Infect. Dis. Rep. 2021, 13, 1053-1060. https://doi.org/10.3390/idr13040096
Di Bella S, Zerbato V, Sanson G, Roman-Pognuz E, De Cristofaro P, Palermo A, Valentini M, Gobbo Y, Jaracz AW, Bozic Hrzica E, et al. Neck Circumference Predicts Mortality in Hospitalized COVID-19 Patients. Infectious Disease Reports. 2021; 13(4):1053-1060. https://doi.org/10.3390/idr13040096
Chicago/Turabian StyleDi Bella, Stefano, Verena Zerbato, Gianfranco Sanson, Erik Roman-Pognuz, Paolo De Cristofaro, Andrea Palermo, Michael Valentini, Ylenia Gobbo, Anna Wladyslawa Jaracz, Elizabeta Bozic Hrzica, and et al. 2021. "Neck Circumference Predicts Mortality in Hospitalized COVID-19 Patients" Infectious Disease Reports 13, no. 4: 1053-1060. https://doi.org/10.3390/idr13040096
APA StyleDi Bella, S., Zerbato, V., Sanson, G., Roman-Pognuz, E., De Cristofaro, P., Palermo, A., Valentini, M., Gobbo, Y., Jaracz, A. W., Bozic Hrzica, E., Bresani-Salvi, C. C., Galindo, A. B., Crovella, S., & Luzzati, R. (2021). Neck Circumference Predicts Mortality in Hospitalized COVID-19 Patients. Infectious Disease Reports, 13(4), 1053-1060. https://doi.org/10.3390/idr13040096