Excess Mortality Stratified by Age and Sex for Croatia and Croatian Counties during the 2020–2021 COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Excess Mortality on the National Level
3.1.1. Excess Mortality for the Whole Population
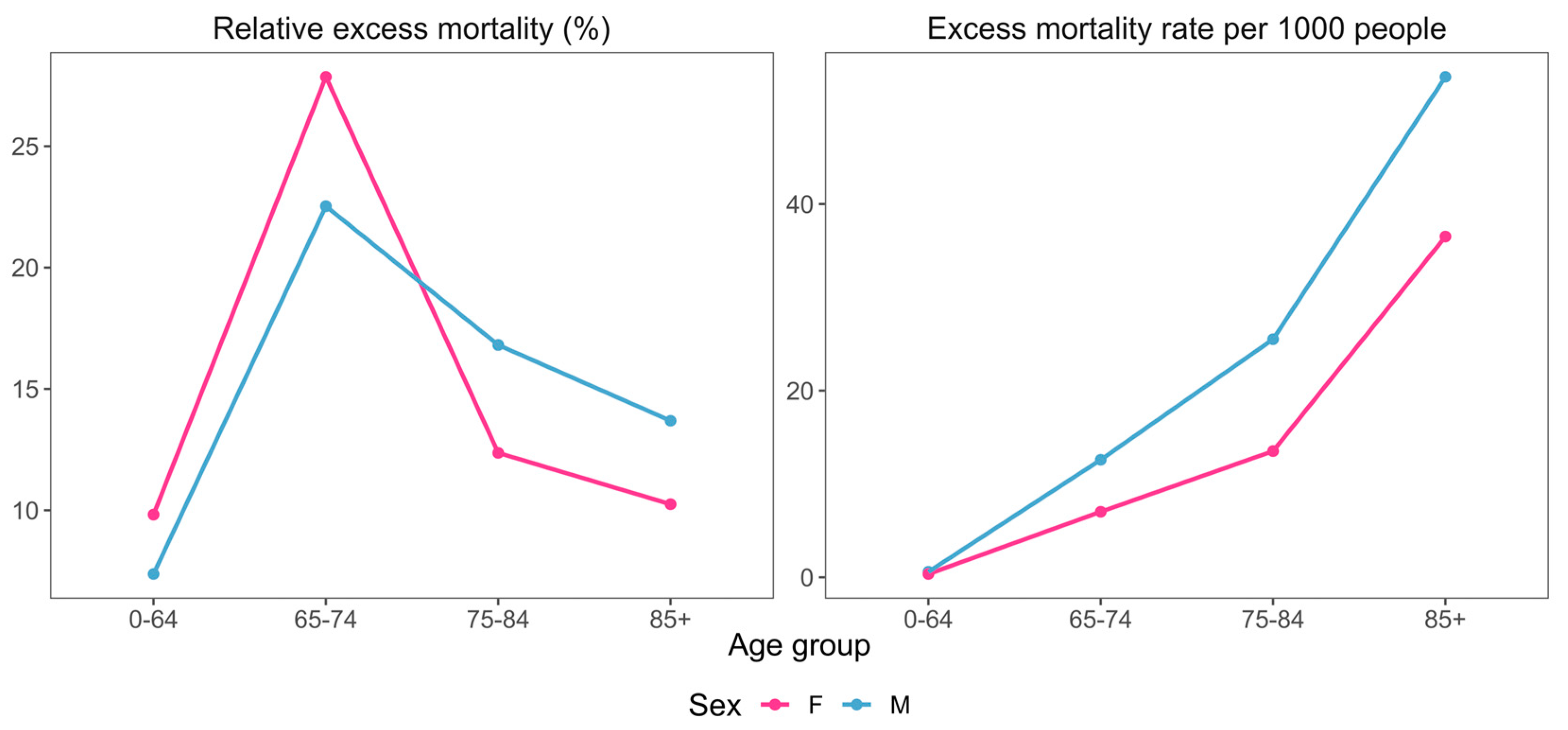
3.1.2. Excess Mortality with Respect to Age and Sex Differences
3.1.3. Excess Mortality vs. Official COVID-19 Mortality
3.2. Excess Mortality over Different Counties
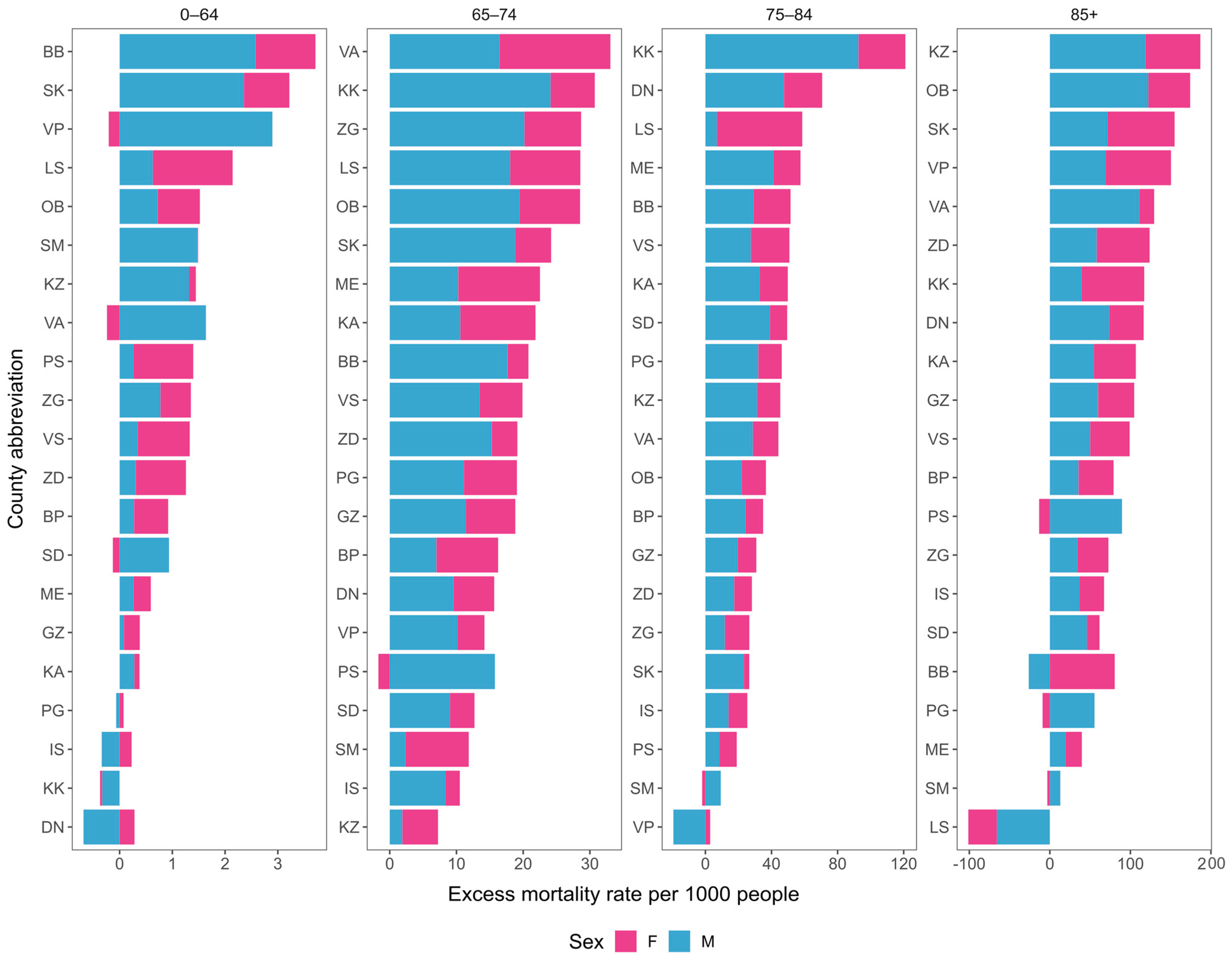
3.2.1. Excess Mortalities over Entire County Populations
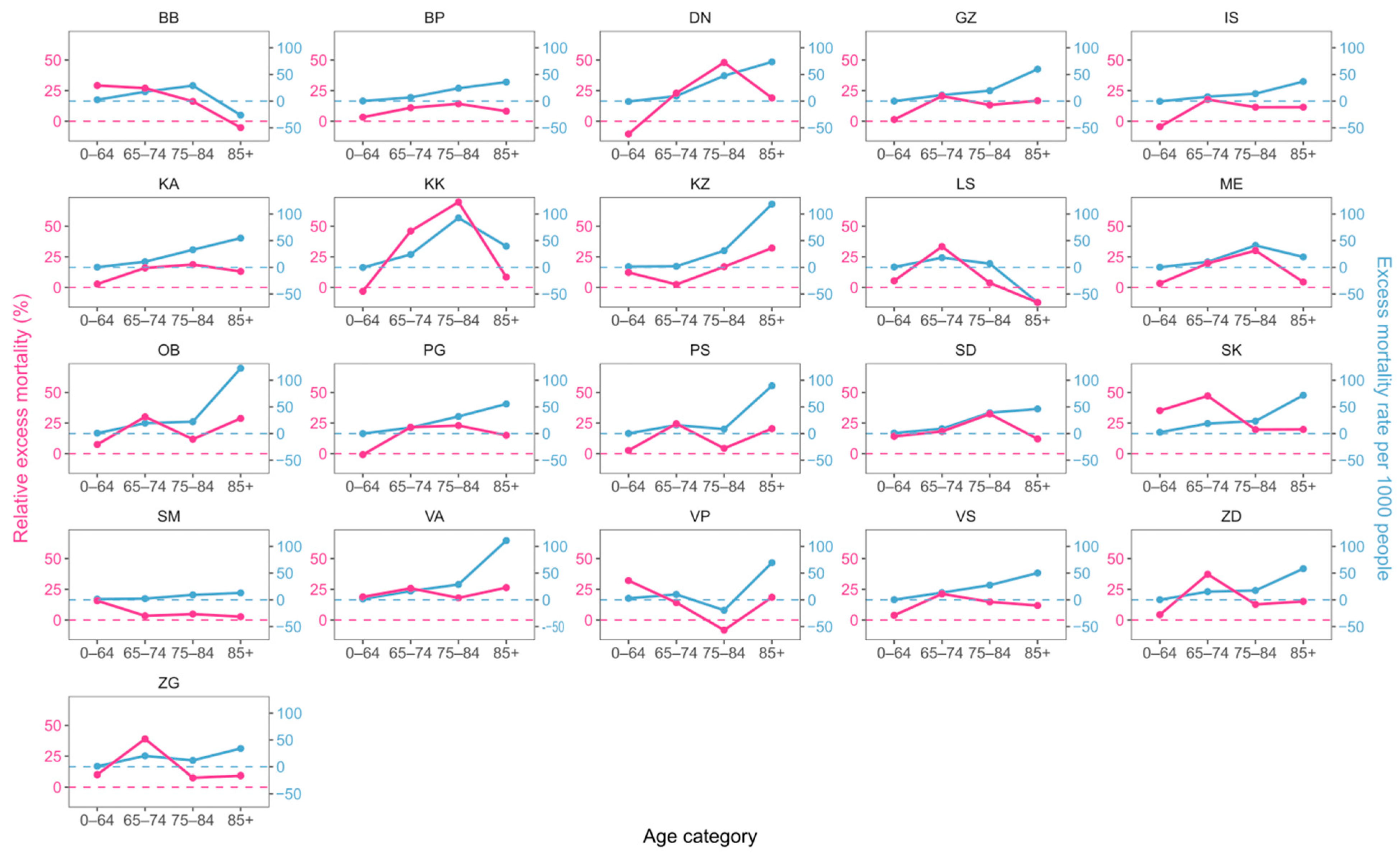
3.2.2. Excess Mortality across Counties with Respect to Age and Sex Differences
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| County | Abbreviation |
|---|---|
| Bjelovar-Bilogora County | BB |
| Brod-Posavina County | BP |
| Dubrovnik-Neretva County | DN |
| Istria County | IS |
| Karlovac County | KA |
| Koprivnica-Križevci County | KK |
| Krapina-Zagorje County | KZ |
| Lika-Senj County | LS |
| Međimurje County | ME |
| Osijek-Baranja County | OB |
| Požega-Slavonia County | PS |
| Primorje-Gorski Kotar County | PG |
| Sisak-Moslavina County | SM |
| Split-Dalmatia County | SD |
| Varaždin County | VA |
| Virovitica-Podravina County | VP |
| Vukovar-Srijem County | VS |
| Zadar County | ZD |
| Zagreb | GZ |
| Zagreb County | ZG |
| Šibenik-Knin County | SK |
References
- Beaney, T.; Clarke, J.M.; Jain, V.; Golestaneh, A.K.; Lyons, G.; Salman, D.; Majeed, A. Excess Mortality: The Gold Standard in Measuring the Impact of COVID-19 Worldwide? J. R. Soc. Med. 2020, 113, 329–334. [Google Scholar] [CrossRef]
- Karlinsky, A.; Kobak, D. Tracking Excess Mortality across Countries during the COVID-19 Pandemic with the World Mortality Dataset. eLife 2021, 10, e69336. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Excess Mortality Collaborators. Estimating Excess Mortality due to the COVID-19 Pandemic: A Systematic Analysis of COVID-19-Related Mortality, 2020–2021. Lancet 2022, 399, 1513–1536. [Google Scholar] [CrossRef] [PubMed]
- United Nations. World Population Prospects 2019: Department of Economic and Social Affairs. World Population Prospects 2019. Available online: https://population.un.org/wpp/ (accessed on 15 February 2024).
- Cipin, I.; Mustac, D.; Medjimurec, P. Impact of COVID-19 on Mortality in Croatia. Stanovnistvo 2021, 59, 1–16. [Google Scholar] [CrossRef]
- Starke, K.R.; Reissig, D.; Petereit-Haack, G.; Schmauder, S.; Nienhaus, A.; Seidler, A. The Isolated Effect of Age on the Risk of COVID-19 Severe Outcomes: A Systematic Review with Meta-Analysis. BMJ Glob. Health 2021, 6, e006434. [Google Scholar] [CrossRef]
- Levin, A.T.; Hanage, W.P.; Owusu-Boaitey, N.; Cochran, K.B.; Walsh, S.P.; Meyerowitz-Katz, G. Assessing the Age Specificity of Infection Fatality Rates for COVID-19: Systematic Review, Meta-Analysis, and Public Policy Implications. Eur. J. Epidemiol. 2020, 35, 1123–1138. [Google Scholar] [CrossRef]
- Nielsen, J.; Nørgaard, S.K.; Lanzieri, G.; Vestergaard, L.S.; Moelbak, K. Sex-Differences in COVID-19 Associated Excess Mortality Is Not Exceptional for the COVID-19 Pandemic. Sci. Rep. 2021, 11, 20815. [Google Scholar] [CrossRef]
- Scully, E.P.; Haverfield, J.; Ursin, R.L.; Tannenbaum, C.; Klein, S.L. Considering How Biological Sex Impacts Immune Responses and COVID-19 Outcomes. Nat. Rev. Immunol. 2020, 20, 442–447. [Google Scholar] [CrossRef]
- Peckham, H.; de Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male Sex Identified by Global COVID-19 Meta-Analysis as a Risk Factor for Death and ITU Admission. Nat. Commun. 2020, 11, 6317. [Google Scholar] [CrossRef]
- Croatian Institute of Public Health. Croatian Health Statistics Yearbooks 2017–2021. Available online: https://www.hzjz.hr/cat/hrvatski-zdravstveno-statisticki-ljetopis/ (accessed on 15 February 2024).
- Croatian Bureau of Statistics, Population Census 2021. Available online: https://dzs.gov.hr/vijesti/objavljeni-konacni-rezultati-popisa-2021/1270 (accessed on 15 February 2024).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computin: Vienna, Austria, 2022; Available online: https://www.R-Project.org/ (accessed on 15 February 2024).
- Croatian Institute of Public Health. Mortality Statistics. Available online: https://www.hzjz.hr/tag/mortalitet-statistika/ (accessed on 15 February 2024).
- Levitt, M.; Zonta, F.; Ioannidis, J.P.A. Comparison of Pandemic Excess Mortality in 2020–2021 across Different Empirical Calculations. Environ. Res. 2022, 213, 113754. [Google Scholar] [CrossRef] [PubMed]
- The Economist. Tracking COVID-19 Excess Deaths. Available online: https://www.economist.com/graphic-detail/coronavirus-excess-deaths-tracker (accessed on 15 February 2024).
- Estimated 2020–2021 Excess Death Count Based on Karlinsky and Kobak Methods. Available online: https://ourworldindata.org/excess-mortality-covid (accessed on 15 February 2024).
- Estimated 2020–2021 Excess Death Count from the Economist. Available online: https://ourworldindata.org/excess-mortality-covid (accessed on 15 February 2024).
- Barbieri, M.; Wilmoth, J.R.; Shkolnikov, V.M.; Glei, D.; Jasilionis, D.; Jdanov, D.; Boe, C.; Riffe, T.; Grigoriev, P.; Winant, C. Data Resource Profile: The Human Mortality Database (HMD). Int. J. Epidemiol. 2015, 44, 1549–1556. [Google Scholar] [CrossRef]
- Human Mortality Database: University of California Berkeley (USA) and Max Planck Institute for Demographic Research (Germany). Available online: https://www.mortality.org (accessed on 15 February 2024).
- López-Gigosos, R.; Vegas-Romero, M.; Mariscal, A.; Mariscal-López, E.; Fang, J.; Gutiérrez-Bedmar, M. Excess Mortality in 22 European Countries in 2020 and 2021: Relationship with Socioeconomic Indicators. Perspect. Public Health 2023, 17579139231180800. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, J.P.A.; Zonta, F.; Levitt, M. Variability in Excess Deaths across Countries with Different Vulnerability during 2020–2023. Proc. Natl. Acad. Sci. USA 2023, 120, e2309557120. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.-E.; Woo Park, S.; Weinberger, D.M.; Olson, D.; Simonsen, L.; Grenfell, B.T.; Viboud, C. Direct and Indirect Mortality Impacts of the COVID-19 Pandemic in the United States, March 1, 2020 to January 1, 2022. eLife 2023, 12, e77562. [Google Scholar] [CrossRef]
- Riou, J.; Hauser, A.; Fesser, A.; Althaus, C.L.; Egger, M.; Konstantinoudis, G. Direct and Indirect Effects of the COVID-19 Pandemic on Mortality in Switzerland. Nat. Commun. 2023, 14, 90. [Google Scholar] [CrossRef] [PubMed]
- Adlhoch, C.; Mook, P.; Lamb, F.; Ferland, L.; Melidou, A.; Amato-Gauci, A.J.; Pebody, R. Very Little Influenza in the WHO European Region during the 2020/21 Season, Weeks 40 2020 to 8 2021. Eurosurveillance 2021, 26, 2100221. [Google Scholar] [CrossRef] [PubMed]
- Janke, A.T.; Mei, H.; Rothenberg, C.; Becher, R.D.; Lin, Z.; Venkatesh, A.K. Analysis of Hospital Resource Availability and COVID-19 Mortality Across the United States. J. Hosp. Med. 2021, 16, 211–214. [Google Scholar] [CrossRef]
- Tchicaya, A.; Lorentz, N.; Leduc, K.; de Lanchy, G. COVID-19 Mortality with Regard to Healthcare Services Availability, Health Risks, and Socio-Spatial Factors at Department Level in France: A Spatial Cross-Sectional Analysis. PLoS ONE 2021, 16, e0256857. [Google Scholar] [CrossRef]
- Kunz, J.S.; Propper, C. JUE Insight: Is Hospital Quality Predictive of Pandemic Deaths? Evidence from US Counties. J. Urban Econ. 2023, 133, 103472. [Google Scholar] [CrossRef]
- Čivljak, R.; Markotić, A.; Capak, K. Earthquake in the Time of COVID-19: The Story from Croatia (CroVID-20). J. Glob. Health 2020, 10, 3–6. [Google Scholar] [CrossRef]
- Maršanić, V.B.; Dobrović, N.; Tadić, M.F.; Flander, G.B. 2020 Double Crisis in Croatia: Earthquakes in the Time of COVID-19. Eur. Child Adolesc. Psychiatry 2021, 30, 1309–1313. [Google Scholar] [CrossRef] [PubMed]
- Civil Protection Headquarter, Earthquake Information. Available online: https://potresinfo.gov.hr/sisacko-moslavacka-zupan (accessed on 15 February 2024).
- Desmet, K.; Wacziarg, R. JUE Insight: Understanding Spatial Variation in COVID-19 across the United States. J. Urban Econ. 2022, 127, 103332. [Google Scholar] [CrossRef] [PubMed]
- Pascoal, R.; Rocha, H. Population Density Impact on COVID-19 Mortality Rate: A Multifractal Analysis Using French Data. Phys. A Stat. Mech. Appl. 2022, 593, 126979. [Google Scholar] [CrossRef] [PubMed]
- Parkes, B.; Stafoggia, M.; Fecht, D.; Davies, B.; Bonander, C.; De’ Donato, F.; Michelozzi, P.; Piel, F.B.; Strömberg, U.; Blangiardo, M. Community Factors and Excess Mortality in the COVID-19 Pandemic in England, Italy and Sweden. Eur. J. Public Health 2023, 33, 695–703. [Google Scholar] [CrossRef]
- Harris, J.E.; Boarnet, M.; Boynton, K.; Brodsky, G.; Cardone, P.; Cohen-gould, L.; Cooley, P.; Cragg, M.; Diamond, P.; Everett, D.; et al. The Subways Seeded the Massive Coronavirus Epidemic in New York City; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar] [CrossRef]


| Age | Sex | Population | Excess Mortality | z-Score 1 |
|---|---|---|---|---|
| 0–64 | M | 1,503,611 | 878 | 1.98 |
| 0–64 | F | 1,498,983 | 525 | 2.15 |
| 65–74 | M | 230,234 | 2900 | 23.7 |
| 65–74 | F | 277,484 | 1949 | 7.27 |
| 75–84 | M | 103,737 | 2647 | 4.82 |
| 75–84 | F | 165,837 | 2243 | 2.23 |
| 85+ | M | 27,547 | 1477 | 5.36 |
| 85+ | F | 64,400 | 2352 | 2.28 |
| All ages | Both sexes | 3,871,833 | 14,963 | 5.09 |
| County | Population | 0–64 | 65–74 | 75–84 | 85+ |
|---|---|---|---|---|---|
| BB | 101,879 | 76.8 | 13.9 | 6.9 | 2.4 |
| BP | 130,267 | 77.4 | 13.1 | 7.2 | 2.3 |
| DN | 115,564 | 77.5 | 13.0 | 6.9 | 2.6 |
| GZ | 767,131 | 79.3 | 11.6 | 6.8 | 2.3 |
| IS | 195,237 | 75.8 | 14.1 | 7.2 | 2.8 |
| KA | 112,195 | 75.5 | 13.9 | 7.6 | 3.1 |
| KK | 101,221 | 78.0 | 13.0 | 6.9 | 2.1 |
| KZ | 120,702 | 79.2 | 12.1 | 6.4 | 2.2 |
| LS | 42,748 | 73.7 | 13.9 | 8.7 | 3.6 |
| ME | 105,250 | 79.4 | 12.2 | 6.3 | 2.1 |
| OB | 258,026 | 78.0 | 13.3 | 6.7 | 2.0 |
| PG | 265,419 | 74.2 | 15.4 | 7.6 | 2.8 |
| PS | 64,084 | 77.1 | 13.3 | 7.3 | 2.2 |
| SD | 423,407 | 78.2 | 12.8 | 6.5 | 2.4 |
| SK | 96,381 | 72.6 | 15.5 | 8.5 | 3.3 |
| SM | 139,603 | 75.3 | 14.7 | 7.6 | 2.5 |
| VA | 159,487 | 79.2 | 12.1 | 6.6 | 2.1 |
| VP | 70,368 | 78.0 | 13.2 | 6.6 | 2.1 |
| VS | 143,113 | 77.2 | 13.6 | 7.1 | 2.2 |
| ZD | 159,766 | 76.0 | 14.0 | 7.5 | 2.5 |
| ZG | 299,985 | 78.7 | 12.9 | 6.4 | 2.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Šošić, M.; Boban, Z.; Erceg, M.; Boban, N. Excess Mortality Stratified by Age and Sex for Croatia and Croatian Counties during the 2020–2021 COVID-19 Pandemic. Infect. Dis. Rep. 2024, 16, 142-153. https://doi.org/10.3390/idr16020011
Šošić M, Boban Z, Erceg M, Boban N. Excess Mortality Stratified by Age and Sex for Croatia and Croatian Counties during the 2020–2021 COVID-19 Pandemic. Infectious Disease Reports. 2024; 16(2):142-153. https://doi.org/10.3390/idr16020011
Chicago/Turabian StyleŠošić, Mara, Zvonimir Boban, Marijan Erceg, and Nataša Boban. 2024. "Excess Mortality Stratified by Age and Sex for Croatia and Croatian Counties during the 2020–2021 COVID-19 Pandemic" Infectious Disease Reports 16, no. 2: 142-153. https://doi.org/10.3390/idr16020011
APA StyleŠošić, M., Boban, Z., Erceg, M., & Boban, N. (2024). Excess Mortality Stratified by Age and Sex for Croatia and Croatian Counties during the 2020–2021 COVID-19 Pandemic. Infectious Disease Reports, 16(2), 142-153. https://doi.org/10.3390/idr16020011







