Acceptability and Practicality of a Quick Musculoskeletal Examination into Sports Medicine Pre-Participation Evaluation
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
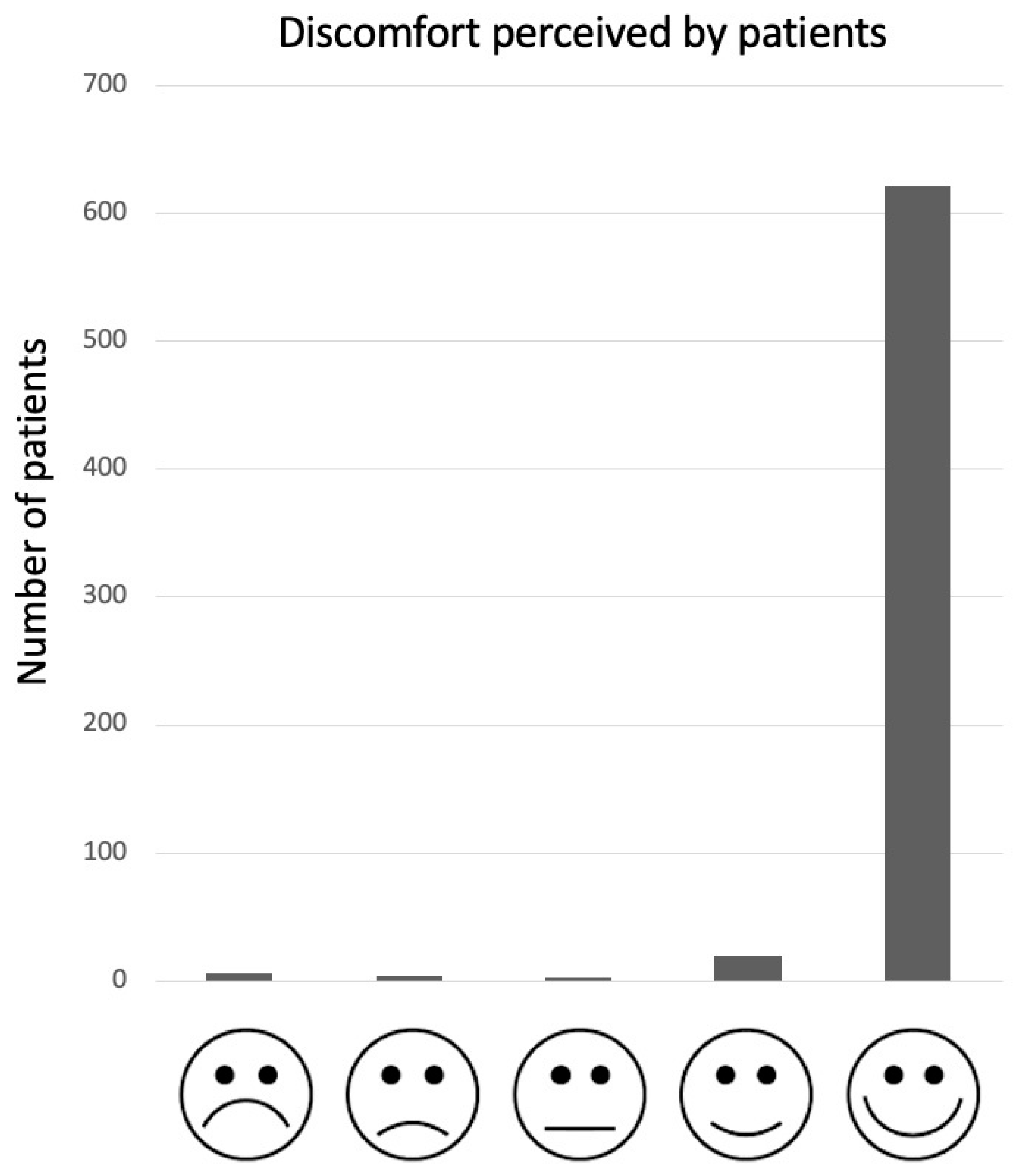
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Palermi, S.; Iacono, O.; Sirico, F.; Modestino, M.; Ruosi, C.; Spera, R.; De Luca, M. The complex relationship between physical activity and diabetes: An overview. J. Basic Clin. Physiol. Pharmacol. 2021. [Google Scholar] [CrossRef]
- Yeo, M.; Sawyer, S. Chronic illness and disability. BMJ 2005, 330, 721–723. [Google Scholar] [CrossRef] [PubMed]
- Rhee, H.; Miles, M.S.; Halpern, C.T.; Holditch-Davis, D. Prevalence of recurrent physical symptoms in U.S. adolescents. Pediatr. Nurs. 2005, 31, 314. [Google Scholar]
- Rosenfeld, S.B.; Schroeder, K.; Watkins-Castillo, S.I. The Economic Burden of Musculoskeletal Disease in Children and Adolescents in the United States. J. Pediatr. Orthop. 2018, 38, e230–e236. [Google Scholar] [CrossRef]
- Henschke, N.; Harrison, C.; McKay, D.; Broderick, C.; Latimer, J.; Britt, H.; Maher, C.G. Musculoskeletal conditions in children and adolescents managed in Australian primary care. BMC Musculoskelet. Disord. 2014, 15, 164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, A.; Strauss, V.Y.; Protheroe, J.; Dunn, K.M. Epidemiology of paediatric presentations with musculoskeletal problems in primary care. BMC Musculoskelet. Disord. 2018, 19, 40. [Google Scholar] [CrossRef] [Green Version]
- Gonçalves, M.; Terreri, M.T.R.A.; Barbosa, C.M.P.L.; Len, C.A.; Lee, L.; Hilário, M.O.E. Diagnosis of malignancies in children with musculoskeletal complaints. Sao Paulo Med. J. 2005, 123, 21–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Legault, É.P.; Descarreaux, M.; Cantin, V. Musculoskeletal symptoms in an adolescent athlete population: A comparative study. BMC Musculoskelet. Disord. 2015, 16, 210. [Google Scholar] [CrossRef] [Green Version]
- Kamper, S.J.; Henschke, N.; Hestbaek, L.; Dunn, K.M.; Williams, C.M. Musculoskeletal pain in children and adolescents. Braz. J. Phys. Ther. 2016, 20, 275–284. [Google Scholar] [CrossRef] [Green Version]
- Vessella, T.; Zorzi, A.; Merlo, L.; Pegoraro, C.; Giorgiano, F.; Trevisanato, M.; Viel, M.; Formentini, P.; Corrado, D.; Sarto, P. The Italian preparticipation evaluation programme: Diagnostic yield, rate of disqualification and cost analysis. Br. J. Sports Med. 2020, 54, 231–237. [Google Scholar] [CrossRef] [Green Version]
- Palermi, S.; Serio, A.; Vecchiato, M.; Sirico, F.; Gambardella, F.; Ricci, F.; Iodice, F.; Radmilovic, J.; Russo, V.; D’Andrea, A. Potential role of an athlete-focused echocardiogram in sports eligibility. World J. Cardiol. 2021, 13, 271–297. [Google Scholar] [CrossRef]
- Kibler, W.B.; Chandler, T.J.; Uhl, T.; Maddux, R.E. A musculoskeletal approach to the preparticipation physical examination. Preventing injury and improving performance. Am. J. Sports Med. 1989, 17, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Toivo, K.; Kannus, P.; Kokko, S.; Alanko, L.; Heinonen, O.J.; Korpelainen, R.; Savonen, K.; Selänne, H.; Vasankari, T.; Kannas, L.; et al. Musculoskeletal examination in young athletes and non-athletes: The Finnish Health Promoting Sports Club (FHPSC) study. BMJ Open Sport Exerc. Med. 2018, 4, e000376. [Google Scholar] [CrossRef] [PubMed]
- Caine, D.; Maffulli, N.; Caine, C. Epidemiology of injury in child and adolescent sports: Injury rates, risk factors, and prevention. Clin. Sports Med. 2008, 27, 19–50. [Google Scholar] [CrossRef] [PubMed]
- Palermi, S.; Massa, B.; Vecchiato, M.; Mazza, F.; De Blasiis, P.; Romano, A.M.; Di Salvatore, M.G.; Della Valle, E.; Tarantino, D.; Ruosi, C.; et al. Indirect Structural Muscle Injuries of Lower Limb: Rehabilitation and Therapeutic Exercise. J. Funct. Morphol. Kinesiol. 2021, 6, 75. [Google Scholar] [CrossRef]
- Sirico, F.; Palermi, S.; Massa, B.; Corrado, B. Tendinopathies of the hip and pelvis in athletes: A narrative review. J. Hum. Sport Exerc. 2020, 15, S748–S762. [Google Scholar]
- Foster, H.; Kay, L.; May, C.; Rapley, T. Pediatric regional examination of the musculoskeletal system: A practice- and consensus-based approach. Arthritis Care Res. 2011, 63, 1503–1510. [Google Scholar] [CrossRef]
- Kraus, K.; Schütz, E.; Taylor, W.R.; Doyscher, R. Efficacy of the functional movement screen: A review. J. Strength Cond. Res. 2014, 28, 3571–3584. [Google Scholar] [CrossRef]
- Doherty, M.; Dacre, J.; Dieppe, P.; Snaith, M. The “GALS” locomotor screen. Ann. Rheum. Dis. 1992, 51, 1165–1169. [Google Scholar] [CrossRef]
- Goff, I.; Bateman, B.; Myers, A.; Foster, H. Acceptability and practicality of musculoskeletal examination in acute general pediatric assessment. J. Pediatr. 2010, 156, 657–662. [Google Scholar] [CrossRef]
- Rowan, A.L.; Jandial, S.; Myers, A.; Bateman, B.; Friswell, M.; Foster, H.E. pGALS performs well in the hands of a medical student. Pediatric Rheumatol. Online J. 2008, 6, 152. [Google Scholar] [CrossRef] [Green Version]
- Foster, H.E.; Kay, L.J.; Friswell, M.; Coady, D.; Myers, A. Musculoskeletal screening examination (pGALS) for school-age children based on the adult GALS screen. Arthritis Rheum. 2006, 55, 709–716. [Google Scholar] [CrossRef] [PubMed]
- Abernethy, K.; Jandial, S.; Hill, L.; Sánchez, E.S.; Foster, H. Acceptability and practicality of a Spanish translation of paediatric Gait Arms Legs and Spine (pGALS) in Peruvian children. Pediatr. Rheumatol. 2014, 12, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sukharomana, M.; Charuvanij, S. The Thai Translation of the Pediatric Gait, Arms, Legs, Spine Tool is Useful for Pediatric Residents in Detecting Musculoskeletal Abnormalities in Children. J. Clin. Rheumatol. Pract. Rep. Rheum. Musculoskelet. Dis. 2021, 27, e323–e329. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Torres, L.A.; Hernández-Garduño, A.G.; Arellano-Valdés, C.A.; Salinas-Rodríguez, A.; Rubio-Perez, N.; Peláez-Ballestas, I. Cross-cultural validation of the paediatric Gait, Arms, Legs, Spine (pGALS) tool for the screening of musculoskeletal disorders in Mexican children. Rheumatol. Int. 2016, 36, 495–503. [Google Scholar] [CrossRef]
- Batu, E.D.; Coskun, Ö.K.; Sönmez, H.E.; Karali, D.; Aydin, E.A.; Bilginer, Y.; Saygi, E.K.; Özen, S. Acceptability and Practicality of the Turkish Translation of Pediatric Gait Arm Legs and Spine in Turkish Children. J. Clin. Rheumatol. Pract. Rep. Rheum. Musculoskelet. Dis. 2017, 23, 421–424. [Google Scholar] [CrossRef]
- Foster, H.E.; Jandial, S. pGALS—Paediatric Gait Arms Legs and Spine: A simple examination of the musculoskeletal system. Pediatr. Rheumatol. Online J. 2013, 11, 44. [Google Scholar] [CrossRef] [Green Version]
- Sirico, F.; Fernando, F.; Bianco, A.; Loiacono, C.; Nuccio, F.; Gambardella, F.; Palermi, S.; Montagnani, S.; Biffi, A. Parental Perception of Children’s Weight Status: Love Overpasses Scientific Evidence! A Cross-Sectional Observational Study. High Blood Press. Cardiovasc Prev. Off. J. Ital. Soc. Hypertens. 2020, 27, 29–34. [Google Scholar] [CrossRef]
- Biffi, A.; Fernando, F.; Adami, P.E.; Messina, M.; Sirico, F.; Di Paolo, F.; Coluccia, R.; Borghi, C.; D’Ascenzi, F.; Volpe, M. Ferrari Corporate Wellness Program: Results of a Pilot Analysis and the “Drag” Impact in the Workplace. High Blood Press. Cardiovasc. Prev. Off. J. Ital. Soc. Hypertens. 2018, 25, 261–266. [Google Scholar] [CrossRef]
- Biffi, A.; Gallo, G.; Fernando, F.; Sirico, F.; Signorello, M.G.; Messina, M.; Manole, G.; Triglione, N.; Volpe, M. Usefulness of the corporate wellness projects in primary prevention at the population level: A study on the prevalence, awareness, and control of hypertension in the Ferrari company. J. Hum. Hypertens. 2022, 36, 308–314. [Google Scholar] [CrossRef]
- Biffi, A.; Gallo, G.; Fernando, F.; Sirico, F.; Signorello, M.G.; De Martino, L.; Manole, G.E.; Palermi, S.; Volpe, M. Relationship Between Cardiorespiratory Fitness, Baseline Blood Pressure and Hypertensive Response to Exercise in the Ferrari Corporate Population. High Blood Press. Cardiovasc. Prev. Off. J. Ital. Soc. Hypertens. 2022, 29, 81–88. [Google Scholar] [CrossRef]
- Sirico, F.; Fernando, F.; Di Paolo, F.; Adami, P.E.; Signorello, M.G.; Sannino, G.; Bianco, A.; Cerrone, A.; Baioccato, V.; Filippi, N.; et al. Exercise stress test in apparently healthy individuals-where to place the finish line? The Ferrari corporate wellness programme experience. Eur. J. Prev. Cardiol. 2019, 26, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.; Molyneux, E.; Heikens, G.T.; Foster, H. Acceptability and practicality of pGALS in screening for rheumatic disease in Malawian children. Clin. Rheumatol. 2012, 31, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Giray, E.; Kenis-Coskun, O.; Karadag-Saygi, E.; Ozyemisci-Taskiran, O. Interrater Reliability, Acceptability, and Practicality of Real-Time Video Pediatric Gait, Arms, Legs, and Spine for Musculoskeletal Assessment of Children During Telemedicine Visits. J. Clin. Rheumatol. 2022; online ahead of print. [Google Scholar]
- Mărginean, C.O.; Meliţ, L.E.; Chinceşan, M.; Mureşan, S.; Georgescu, A.M.; Suciu, N.; Pop, A.; Azamfirei, L. Communication skills in pediatrics—The relationship between pediatrician and child. Medicine 2017, 96, e8399. [Google Scholar] [CrossRef] [PubMed]
- Jandial, S.; Myers, A.; Wise, E.; Foster, H.E. Doctors likely to encounter children with musculoskeletal complaints have low confidence in their clinical skills. J. Pediatr. 2009, 154, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Myers, A.; McDonagh, J.E.; Gupta, K.; Hull, R.; Barker, D.; Kay, L.J.; Foster, H.E. More “cries from the joints”: Assessment of the musculoskeletal system is poorly documented in routine paediatric clerking. Rheumatology 2004, 43, 1045–1049. [Google Scholar] [CrossRef] [Green Version]
- Chan, M.O.; Sen, E.S.; Hardy, E.; Hensman, P.; Wraith, E.; Jones, S.; Rapley, T.; Foster, H.E. Assessment of musculoskeletal abnormalities in children with mucopolysaccharidoses using pGALS. Pediatr. Rheumatol. Online J. 2014, 12, 32. [Google Scholar] [CrossRef] [Green Version]
- Sadeghi-Demneh, E.; Jafarian, F.; Melvin, J.M.A.; Azadinia, F.; Shamsi, F.; Jafarpishe, M. Flatfoot in school-age children: Prevalence and associated factors. Foot Ankle Spec. 2015, 8, 186–193. [Google Scholar] [CrossRef]
- Labelle, H.; Richards, S.B.; De Kleuver, M.; Grivas, T.B.; Luk, K.D.K.; Wong, H.K.; Thometz, J.; Beauséjour, M.; Turgeon, I.; Fong, D.Y.T. Screening for adolescent idiopathic scoliosis: An information statement by the scoliosis research society international task force. Scoliosis 2013, 8, 17. [Google Scholar] [CrossRef] [Green Version]
- Evans, A.M.; Rome, K. A Cochrane review of the evidence for non-surgical interventions for flexible pediatric flat feet. Eur. J. Phys. Rehabil. Med. 2011, 47, 69–89. [Google Scholar]
- Launay, F. Sports-related overuse injuries in children. Orthop. Traumatol. Surg. Res. 2015, 101, S139–S147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castori, M. Joint hypermobility in children: A neglected sign needing more attention. Minerva Pediat. 2020, 72, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Jelinek, E.M.; Bittersohl, B.; Martiny, F.; Scharfstädt, A.; Krauspe, R.; Westhoff, B. The 8-plate versus physeal stapling for temporary hemiepiphyseodesis correcting genu valgum and genu varum: A retrospective analysis of thirty five patients. Int. Orthop. 2012, 36, 599–605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Circi, E.; Atalay, Y.; Beyzadeoglu, T. Treatment of Osgood-Schlatter disease: Review of the literature. Musculoskelet Surg. 2017, 101, 195–200. [Google Scholar] [CrossRef] [PubMed]
- DePaola, K.; Cuddihy, L.A. Pediatric Spine Disorders. Pediatr. Clin. N. Am. 2020, 67, 185–204. [Google Scholar] [CrossRef]
- Akbar, M.; Wiedenhöfer, B. Korrektur der Adoleszentenkyphose: Was ist State of the Art? Orthopade 2011, 40, 682–689. [Google Scholar] [CrossRef]
- Spera, R.; Belviso, I.; Sirico, F.; Palermi, S.; Massa, B.; Mazzeo, F.; Montesano, P. Jump and balance test in judo athletes with or without visual impairments. J. Hum. Sport Exerc. 2019, 14, S937–S947. [Google Scholar]

| Category | Screening Maneuvers | What Is Being Assessed? |
|---|---|---|
| Gait |
|
|
| Arm |
|
|
| Leg |
|
|
| Spine |
|
|
| Component of pGALS Screen | Number of Abnormal Subjects | Most Frequent Abnormal Detail |
|---|---|---|
| Gait | 152 (23.2%) |
|
| Arms | 15 (2.3%) |
|
| Legs | 33 (5.0%) |
|
| Spine | 82 (12.5%) |
|
| Category | What Can Be Pathological | Outcome on Future Health, If Not Treated |
|---|---|---|
| Gait | Flat feet [40] |
|
| Pes cavus |
| |
| Heel Pain (suspected Sever Blank disease) [41] |
| |
| Arm | Hyperlaxity of ligaments [42] |
|
| Leg | Genu valgum/genu varum [43] |
|
| Tibial plateau pain (suspected Osgood Schlatter disease) [44] |
| |
| Spine | Scoliosis [45] |
|
| Dorsal kyphosis (suspected Scheuermann disease) [46] |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palermi, S.; Annarumma, G.; Spinelli, A.; Massa, B.; Serio, A.; Vecchiato, M.; Demeco, A.; Brugin, E.; Sirico, F.; Giada, F.; et al. Acceptability and Practicality of a Quick Musculoskeletal Examination into Sports Medicine Pre-Participation Evaluation. Pediatr. Rep. 2022, 14, 207-216. https://doi.org/10.3390/pediatric14020028
Palermi S, Annarumma G, Spinelli A, Massa B, Serio A, Vecchiato M, Demeco A, Brugin E, Sirico F, Giada F, et al. Acceptability and Practicality of a Quick Musculoskeletal Examination into Sports Medicine Pre-Participation Evaluation. Pediatric Reports. 2022; 14(2):207-216. https://doi.org/10.3390/pediatric14020028
Chicago/Turabian StylePalermi, Stefano, Giada Annarumma, Alessandro Spinelli, Bruno Massa, Alessandro Serio, Marco Vecchiato, Andrea Demeco, Erica Brugin, Felice Sirico, Franco Giada, and et al. 2022. "Acceptability and Practicality of a Quick Musculoskeletal Examination into Sports Medicine Pre-Participation Evaluation" Pediatric Reports 14, no. 2: 207-216. https://doi.org/10.3390/pediatric14020028
APA StylePalermi, S., Annarumma, G., Spinelli, A., Massa, B., Serio, A., Vecchiato, M., Demeco, A., Brugin, E., Sirico, F., Giada, F., & Biffi, A. (2022). Acceptability and Practicality of a Quick Musculoskeletal Examination into Sports Medicine Pre-Participation Evaluation. Pediatric Reports, 14(2), 207-216. https://doi.org/10.3390/pediatric14020028









