Psychopathological and Organic Features of Atypical Anorexia Nervosa in Developmental Age: A Systematic Review
Abstract
1. Introduction
1.1. Definition
1.2. Evolution of the Concept of “Atypical Anorexia Nervosa”
1.3. AAN in the Recent Literature
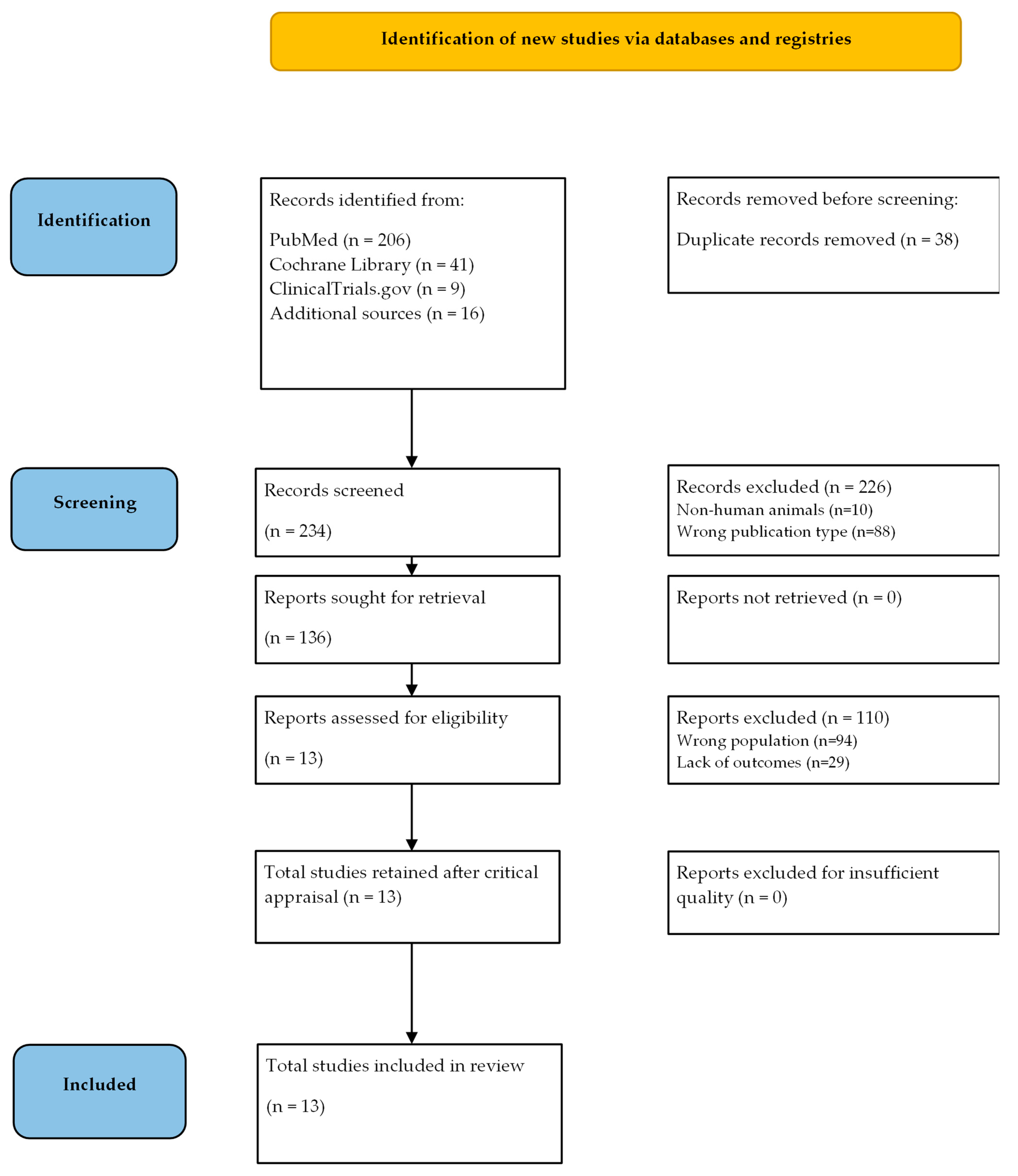
2. Materials and Methods
- If released in a language other than English.
- If the study’s methodology—a narrative review, a systematic review, a study protocol, or any other study type—was unambiguously stated as such (RCT, cohort studies, cross-sectional studies, retrospective studies, etc. were included) or if the population that was included was unambiguously stated as being exclusively made up of animals other than humans.
- If one of the exclusion criteria (population: non-humans, language: non-English, study design: descriptive studies, reviews, procedures, case report/case series) remained after suitability screening.
- If the study excluded children and adolescents or included a mixed group of children/adolescents and adults, but did not publish separate data for the two age groups.
- If no one was given a DSM-5-based diagnosis of AAN.
3. Results
3.1. Diagnostic Criteria and Epidemiology
3.2. Eating Disorder-Specific and General Psychopathology
3.3. Organic and Neurobiological Findings
3.4. Treatment Interventions
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Sawyer, S.M.; Whitelaw, M.; Le Grange, D.; Yeo, M.; Hughes, E.K. Physical and Psychological Morbidity in Adolescents With Atypical Anorexia Nervosa. Pediatrics 2016, 137, e20154080. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Marti, C.N.; Rohde, P. Prevalence, Incidence, Impairment, and Course of the Proposed DSM-5 Eating Disorder Diagnoses in an 8-Year Prospective Community Study of Young Women. J. Abnorm. Psychol. 2013, 122, 445–457. [Google Scholar] [CrossRef] [PubMed]
- Zanna, V.; Criscuolo, M.; Mereu, A.; Cinelli, G.; Marchetto, C.; Pasqualetti, P.; Tozzi, A.E.; Castiglioni, M.C.; Chianello, I.; Vicari, S. Restrictive Eating Disorders in Children and Adolescents: A Comparison between Clinical and Psychopathological Profiles. Eat. Weight Disord. 2021, 26, 1491–1501. [Google Scholar] [CrossRef]
- Crow, S.J. Atypical Anorexia Nervosa: In Need of Further Study. Int. J. Eat. Disord. 2022, 56, 824–825. [Google Scholar] [CrossRef] [PubMed]
- Harrop, E.N.; Mensinger, J.L.; Moore, M.; Lindhorst, T. Restrictive Eating Disorders in Higher Weight Persons: A Systematic Review of Atypical Anorexia Nervosa Prevalence and Consecutive Admission Literature. Int. J. Eat. Disord. 2021, 54, 1328–1357. [Google Scholar] [CrossRef] [PubMed]
- Freizinger, M.; Recto, M.; Jhe, G.; Lin, J. Atypical Anorexia in Youth: Cautiously Bridging the Treatment Gap. Children 2022, 9, 837. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Garber, A.K.; Cheng, J.; Accurso, E.C.; Adams, S.H.; Buckelew, S.M.; Kapphahn, C.J.; Kreiter, A.; Le Grange, D.; Machen, V.I.; Moscicki, A.-B.; et al. Weight Loss and Illness Severity in Adolescents With Atypical Anorexia Nervosa. Pediatrics 2019, 144, e20192339. [Google Scholar] [CrossRef] [PubMed]
- Tragantzopoulou, P.; Giannouli, V. “You Feel That You Are Stepping into a Different World”: Vulnerability and Biases in the Treatment of Anorexia Nervosa. Eur. J. Psychother. Couns. 2023, 25, 351–368. [Google Scholar] [CrossRef]
- Peebles, R.; Hardy, K.K.; Wilson, J.L.; Lock, J.D. Are Diagnostic Criteria for Eating Disorders Markers of Medical Severity? Pediatrics 2010, 125, e1193–e1201. [Google Scholar] [CrossRef]
- Swenne, I. Influence of Premorbid BMI on Clinical Characteristics at Presentation of Adolescent Girls with Eating Disorders. BMC Psychiatry 2016, 16, 81. [Google Scholar] [CrossRef]
- Hughes, E.K.; Le Grange, D.; Court, A.; Sawyer, S.M. A Case Series of Family-Based Treatment for Adolescents with Atypical Anorexia Nervosa. Int. J. Eat. Disord. 2017, 50, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Forney, K.J.; Brown, T.A.; Holland-Carter, L.A.; Kennedy, G.A.; Keel, P.K. Defining “Significant Weight Loss” in Atypical Anorexia Nervosa. Int. J. Eat. Disord. 2017, 50, 952–962. [Google Scholar] [CrossRef] [PubMed]
- Engelhardt, C.; Föcker, M.; Bühren, K.; Dahmen, B.; Becker, K.; Weber, L.; Correll, C.U.; Egberts, K.M.; Ehrlich, S.; Roessner, V.; et al. Age Dependency of Body Mass Index Distribution in Childhood and Adolescent Inpatients with Anorexia Nervosa with a Focus on DSM-5 and ICD-11 Weight Criteria and Severity Specifiers. Eur. Child. Adoles.c Psychiatry 2021, 30, 1081–1094. [Google Scholar] [CrossRef] [PubMed]
- Whitelaw, M.; Gilbertson, H.; Lee, K.J.; Sawyer, S.M. Restrictive Eating Disorders among Adolescent Inpatients. Pediatrics 2014, 134, 758–767. [Google Scholar] [CrossRef] [PubMed]
- Whitelaw, M.; Lee, K.J.; Gilbertson, H.; Sawyer, S.M. Predictors of Complications in Anorexia Nervosa and Atypical Anorexia Nervosa: Degree of Underweight or Extent and Recency of Weight Loss? J. Adolesc. Health 2018, 63, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Agostino, H.; Burstein, B.; Moubayed, D.; Taddeo, D.; Grady, R.; Vyver, E.; Dimitropoulos, G.; Dominic, A.; Coelho, J.S. Trends in the Incidence of New-Onset Anorexia Nervosa and Atypical Anorexia Nervosa Among Youth During the COVID-19 Pandemic in Canada. JAMA Netw. Open 2021, 4, e2137395. [Google Scholar] [CrossRef] [PubMed]
- Mitchison, D.; Hay, P.; Slewa-Younan, S.; Mond, J. The Changing Demographic Profile of Eating Disorder Behaviors in the Community. BMC Public Health 2014, 14, 943. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.J.; Vartanian, L.R.; Brownell, K.D. The Relationship between Eating Disorder Not Otherwise Specified (EDNOS) and Officially Recognized Eating Disorders: Meta-Analysis and Implications for DSM. Psychol. Bul. 2009, 135, 407–433. [Google Scholar] [CrossRef] [PubMed]
- Phillipou, A.; Beilharz, F. Should We Shed the Weight Criterion for Anorexia Nervosa? Aust. N. Z. J. Psychiatry 2019, 53, 501–502. [Google Scholar] [CrossRef]
- Matthews, A.; Gordon, K.; Kramer, R.; Lin, J.; Ziv, A. Clinical Characteristics of Medically Hospitalized Youth with Anorexia Nervosa/Atypical Anorexia Nervosa and Premorbid Overweight/Obesity. Eat. Disord. 2023, 31, 201–211. [Google Scholar] [CrossRef]
- Silén, Y.; Raevuori, A.; Jüriloo, E.; Tainio, V.M.; Marttunen, M.; Keski-Rahkonen, A. Typical Versus Atypical Anorexia Nervosa Among Adolescents: Clinical Characteristics and Implications for ICD-11. Eur. Eat. Disord. Rev. 2015, 23, 345–351. [Google Scholar] [CrossRef]
- Fairweather-Schmidt, A.K.; Wade, T.D. DSM-5 Eating Disorders and Other Specified Eating and Feeding Disorders: Is There a Meaningful Differentiation? Int. J. Eat. Disord. 2014, 47, 524–533. [Google Scholar] [CrossRef]
- Levinson, C.A.; Brosof, L.C.; Ram, S.S.; Pruitt, A.; Russell, S.; Lenze, E.J. Obsessions Are Strongly Related to Eating Disorder Symptoms in Anorexia Nervosa and Atypical Anorexia Nervosa. Eat. Behav. 2019, 34, 101298. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, T.P.R.I.S.M.A. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- JBI’s Critical Appraisal Tools. Available online: https://jbi.global/critical-appraisal-tools (accessed on 10 July 2024).
- Available online: https://www.ohri.ca//Programs/Clinical_Epidemiology/Oxford.Asp (accessed on 1 May 2024).
- Available online: https://bmjopen.bmj.com/content/bmjopen/10/1/E030266/DC4/embed/inline-supplementary-material-4.pdf?download=true (accessed on 1 May 2024).
- Kimber, M.; Dimitropoulos, G.; Williams, E.P.; Singh, M.; Loeb, K.L.; Hughes, E.K.; Garber, A.; Elliott, A.; Vyver, E.; Le Grange, D. Tackling Mixed Messages: Practitioner Reflections on Working with Adolescents with Atypical Anorexia and Their Families. Eat. Disord. 2019, 27, 436–452. [Google Scholar] [CrossRef]
- Gledhill, L.J.; Cornelissen, K.K.; Cornelissen, P.L.; Penton-Voak, I.S.; Munafò, M.R.; Tovée, M.J. An Interactive Training Programme to Treat Body Image Disturbance. Br. J. Health Psychol. 2017, 22, 60–76. [Google Scholar] [CrossRef]
- Breithaupt, L.; Kahn, D.L.; Slattery, M.; Plessow, F.; Mancuso, C.; Izquierdo, A.; Dreier, M.J.; Becker, K.; Franko, D.L.; Thomas, J.J.; et al. Eighteen-Month Course and Outcome of Adolescent Restrictive Eating Disorders: Persistence, Crossover, and Recovery. J. Clin. Child Adolesc. Psychol. 2022, 51, 715–725. [Google Scholar] [CrossRef]
- Forman, S.F.; McKenzie, N.; Hehn, R.; Monge, M.C.; Kapphahn, C.J.; Mammel, K.A.; Callahan, S.T.; Sigel, E.J.; Bravender, T.; Romano, M.; et al. Predictors of Outcome at 1 Year in Adolescents With DSM-5 Restrictive Eating Disorders: Report of the National Eating Disorders Quality Improvement Collaborative. J. Adolesc. Health 2014, 55, 750–756. [Google Scholar] [CrossRef]
- Fisher, M.; Gonzalez, M.; Malizio, J. Eating Disorders in Adolescents: How Does the DSM-5 Change the Diagnosis? Int. J. Adolesc. Med. Health 2015, 27, 437–441. [Google Scholar] [CrossRef]
- Olivo, G.; Solstrand Dahlberg, L.; Wiemerslage, L.; Swenne, I.; Zhukovsky, C.; Salonen-Ros, H.; Larsson, E.M.; Gaudio, S.; Brooks, S.J.; Schiöth, H.B. Atypical Anorexia Nervosa Is Not Related to Brain Structural Changes in Newly Diagnosed Adolescent Patients. Int. J. Eat. Disord. 2018, 51, 39–45. [Google Scholar] [CrossRef]
- Olivo, G.; Zhukovsky, C.; Salonen-Ros, H.; Larsson, E.-M.; Brooks, S.; Schiöth, H.B. Functional Connectivity Underlying Hedonic Response to Food in Female Adolescents with Atypical AN: The Role of Somatosensory and Salience Networks. Transl. Psychiatry 2019, 9, 276. [Google Scholar] [CrossRef] [PubMed]
- Pauls, A.; Dimitropoulos, G.; Marcoux-Louie, G.; Singh, M.; Patten, S.B. Psychological Characteristics and Childhood Adversity of Adolescents with Atypical Anorexia Nervosa versus Anorexia Nervosa. Eat. Disord. 2022, 30, 210–222. [Google Scholar] [CrossRef]
- Engelmann, J.B.; Pogosyan, M. Emotion Perception across Cultures: The Role of Cognitive Mechanisms. Front. Psychol. 2013, 4, 41789. [Google Scholar] [CrossRef]
| Study | Patients | Intervention (Administered Diagnostic Tool/Clinical Intervention) | Comparison | Outcome |
|---|---|---|---|---|
| [9] | AAN = 50, AN = 66; age: 16.5 ± 2.6 years; F = 91% | Proctored questionnaires, growth records, medical history, socioeconomic status, date of last menstruation; biochemicals and instrumental analysis; self-administered EDE-Q | AN | Historical BMI, %mBMI and %mBMI at admission higher in AAN. No significant differences in weight history, amenorrhea, lowest heart rate and electrolytes. Higher systolic blood pressure, EDE-Q and all subscales except “concern for nutrition” higher in AAN. |
| [2] | AAN = 42, AN = 118; age: 15.49 vs. 15.4 years; F = 88% (both groups) | Recording of anthropometric data, eating disorder symptoms and psychiatric comorbidities | AN | In AAN: higher rates of premorbid overweight or obesity, weight loss over longer periods, related discomfort to nutrition and body size |
| [3] | 496 females completing annual diagnostic interviews over 8 years; 12–15 years | BMI, ED symptoms, Social Adjustment Scale-Self Report for Youth, K-SADS, frequency of visits to mental health | AN, BN, BED, subthreshold BN, subthreshold BED, PD, EDNOS and controls | AAN episodes last longer than other EDs, and AAN showed higher psychopathological distress, excluding suicidal risk in AN and BMI in BN, subthreshold BN, and BED. |
| [30] | Comments of 23 practitioners on AN and AAN adolescents | Individual semi-structured interview administered to 23 professionals of health from four countries | AN | AAN often starts at higher pre-existing weights and receives more weight-based teasing. Unique hurdles, such as navigating mixed messages about eating disorders and weight loss, understanding and supporting the legitimate fear of gaining weight, and addressing the heightened risks of collusion. |
| [31] | Study 1: 40 students (1–20: 18.2 ± 0.4 years, 21–40: 19 ± 1.3 years), F. Study 2: 21 AAN; F = 100%; age: 27.7 ± 7.5 years | Training program to recalibrate perception of body size Study 1: BMI; BSQ, EDE-Q, BDI, RSE; categorical perception task with computer-generated images. Study 2: BMI, BSQ, EDE-Q; WAIS-R IQ Digit Span task | Study 1: college students without FED; Study 2: only F with AAN | Study 2: In AAN, full training is associated with a cumulative shift in the categorical boundary toward heavier bodies and significant reductions in the EDE-Q subscales related to food restriction and body size concerns persisted for up to one month |
| [32] | AAN = 26; AN = 40; ARFID = 16; age: 10–23 years | Semi-structured interviews | AN and ARFID | Persistence of binge eating/purging and atypical presentations (AAN) showed less consistency over follow-up. Notable transitioning between binge eating/purging and restricting behaviors. |
| [33] | AAN = 238, AN = 375, ARFID = 87; F = 83.2% vs. 90.4% vs. 77.0%; age: 9–21 years | Demographic data, weight and height at intake and follow-up, treatment before intake and treatment during the follow-up year | AN and ARFID | AAN: fewer males than ARFID; ARFID were younger, had longer illness duration before presentation, and fewer prior visits compared to AAN. Significant differences in %MBMI at intake and regular menses, with AAN showing distinct patterns. Higher %MBMI at intake predicted weight recovery significantly. AAN had higher odds of weight recovery compared to ARFID. |
| [34] | AN = 100, AAN = 93, ARFID = 60, BN = 29, PD = 18, UFED = 4, subthreshold BN = 2, subthreshold BED = 2, BED = 1. | Gender, age, ethnicity, weight, height, diagnosis according to DSM-IV and DSM-5 | AN, ARFID, BN, PD, UFED, subthreshold BN, subthreshold BED, BED | AAN more frequent females, slightly older age, and higher weights than AN. ARFID: higher male representation and younger age than AAN. Non-white patients trend toward higher ratio of BN/PD to AN/AAN compared to white patients. |
| [35] | AAN = 22; HC = 38; F = 100%; age: 14.7 vs. 14.8 years. | Basic clinical data; EDE-Q, BIS-11, nd OCI-R; study of brain structure through voxel-based morphometric analysis of MRI | HCs | Significant differences in terms of BMI, EDE-Q total score and OCI-R; no differences in regional gray matter volume could be detected |
| [36] | AAN = 28; HC = 33; F = 100%; age: 14.8 ± 1.6 vs. 15.3 ± 1.3 years. | Basic clinical data, semi-structured interviews. Clinical intervention: FBT and periodic follow-up; images of high- or low-calorie foods were shown in alternating blocks during functional MRI, contrast was calculated | HCs | When comparing images of high- and low-calorie foods, AAN subjects demonstrated greater connectivity than HCs: enhanced connections from the right anterior superior temporal gyrus, and decreased connectivity in the left area. |
| [4] | AAN = 59, AN-R = 193, BED = 14, ARFID = 94; F = 83%; age 15.8 ± 2.5 years | EDI-3, CDI, MASC, CBCL | AN and ARFID | AAN: higher EDI-3 (drive for thinness, bulimia, body dissatisfaction) scores (AAN > AN > ARFID); CDI higher in AAN and AN than in ARFID; no differences in terms of interpersonal insecurity, interoceptive deficit, emotional dysregulation and maturity fears. |
| [37] | AAN = 42, AN-R = 79; F = 88.1% vs. 93.7%; age: 15.9 vs. 15.6 years; | Examination of psychological morbidity and exposure to adverse childhood experiences exploring the connection between reaching the target weight and the likelihood of rehospitalization in adolescents with AN and AAN. | AN-R | AAN subjects had more severe drive for thinness, body dissatisfaction, and lower quality of life, but better global functioning. Adolescents with high adverse childhood experiences had over 5 times the odds of having AAN. No difference on low self-esteem or self-injury |
| [22] | Overall, 253 patients with AN or AAN; age: 10–22 years; 29.6% with and 70.4% without premorbid overweight or obesity | Retrospective review of clinical (sex) and psychopathological data, related to the ED | AN | Patients with/without premorbid overweight or obesity: more often cisgender males, diagnosed with AAN, and had lost a greater percentage of body weight. |
| Study | Selection | Comparability | Exposure (Case–Control)/ Outcome (Cohort) | Quality | Notes |
|---|---|---|---|---|---|
| [9] | ** | ** | *** | Good | |
| [2] | ** | ** | Poor | ||
| [3] | *** | * | *** | Good | |
| [30] | / | / | / | / | Qualitative study |
| [31] + Study 2 | *** | ** | *** | Good | |
| [32] | *** | ** | *** | Good | |
| [33] | *** | ** | *** | Good | |
| [34] | ** | * | Poor | ||
| [35] | *** | ** | *** | Good | |
| [36] | *** | ** | *** | Good | |
| [4] | ** | ** | ** | Fair | |
| [37] | ** | * | ** | Fair | |
| [22] | ** | ** | ** | Fair |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pruccoli, J.; Chiavarino, F.; Valeriani, B.; Petio, M.L.; Parmeggiani, A. Psychopathological and Organic Features of Atypical Anorexia Nervosa in Developmental Age: A Systematic Review. Pediatr. Rep. 2024, 16, 579-593. https://doi.org/10.3390/pediatric16030049
Pruccoli J, Chiavarino F, Valeriani B, Petio ML, Parmeggiani A. Psychopathological and Organic Features of Atypical Anorexia Nervosa in Developmental Age: A Systematic Review. Pediatric Reports. 2024; 16(3):579-593. https://doi.org/10.3390/pediatric16030049
Chicago/Turabian StylePruccoli, Jacopo, Francesca Chiavarino, Beatrice Valeriani, Maria Letizia Petio, and Antonia Parmeggiani. 2024. "Psychopathological and Organic Features of Atypical Anorexia Nervosa in Developmental Age: A Systematic Review" Pediatric Reports 16, no. 3: 579-593. https://doi.org/10.3390/pediatric16030049
APA StylePruccoli, J., Chiavarino, F., Valeriani, B., Petio, M. L., & Parmeggiani, A. (2024). Psychopathological and Organic Features of Atypical Anorexia Nervosa in Developmental Age: A Systematic Review. Pediatric Reports, 16(3), 579-593. https://doi.org/10.3390/pediatric16030049







