The Effectiveness of NIV and CPAP Training on the Job in COVID-19 Acute Care Wards: A Nurses’ Self-Assessment of Skills
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Sample and Setting
2.3. Procedure
2.4. Data Collection and Instrument
- -
- Maintenance frequency of patients with CPAP-helmet or NIV in Fowler position (Frequency Fowler position).
- -
- Check frequency of the Helmet-CPAP system and/or NIV, and surveillance of patients during the treatment (NIV patients check frequency).
- -
- Frequency of respiratory rate measurement in patients with COVID-19 (RR assessment frequency).
- -
- Frequency of application of 24 h expiring HEPA filters on the exit port of the CPAP-Helmet (HEPA 24-h application frequency).
- -
- Check frequency of pulse-oximetry during helmet CPAP removal pauses or NIV mask breaks (Check SpO2 frequency).
- -
- Frequency of setting up of the Helmet-CPAP to the patients by 2 healthcare professionals (Frequency of helmet set-up by 2 nurses).
- -
- Frequency of assessment of the Helmet-CPAP system effective performance by appreciating with gloved hands the presence of continuous gas flow leaving the PEEP valve during inspiration and exhalation (CPAP system working check frequency).
- -
- Frequency of use of the Helmet armpits outside the arms of the patient, placing weights (sandbags) to maintain the system in place and limit air leaks [10] (Helmets armpits outside frequency).
- -
- Frequency of use the “off” function instead of “standby” to pause the NIV mask session delivered with a single tube intentional leaks NIV ventilator (Off ventilator frequency).
- -
- Frequency of use of traditional oxygen therapy systems (reservoir masks, standard masks, Venturi masks, nasal cannula) during breaks from Helmet-CPAP and/or NIV mask (O2 therapy for NIV breaks frequency).
- -
- Frequency of autonomously setting up of a single tube intentional leaks NIV ventilator (Autonomous set-up of NIV circuit frequency).
- -
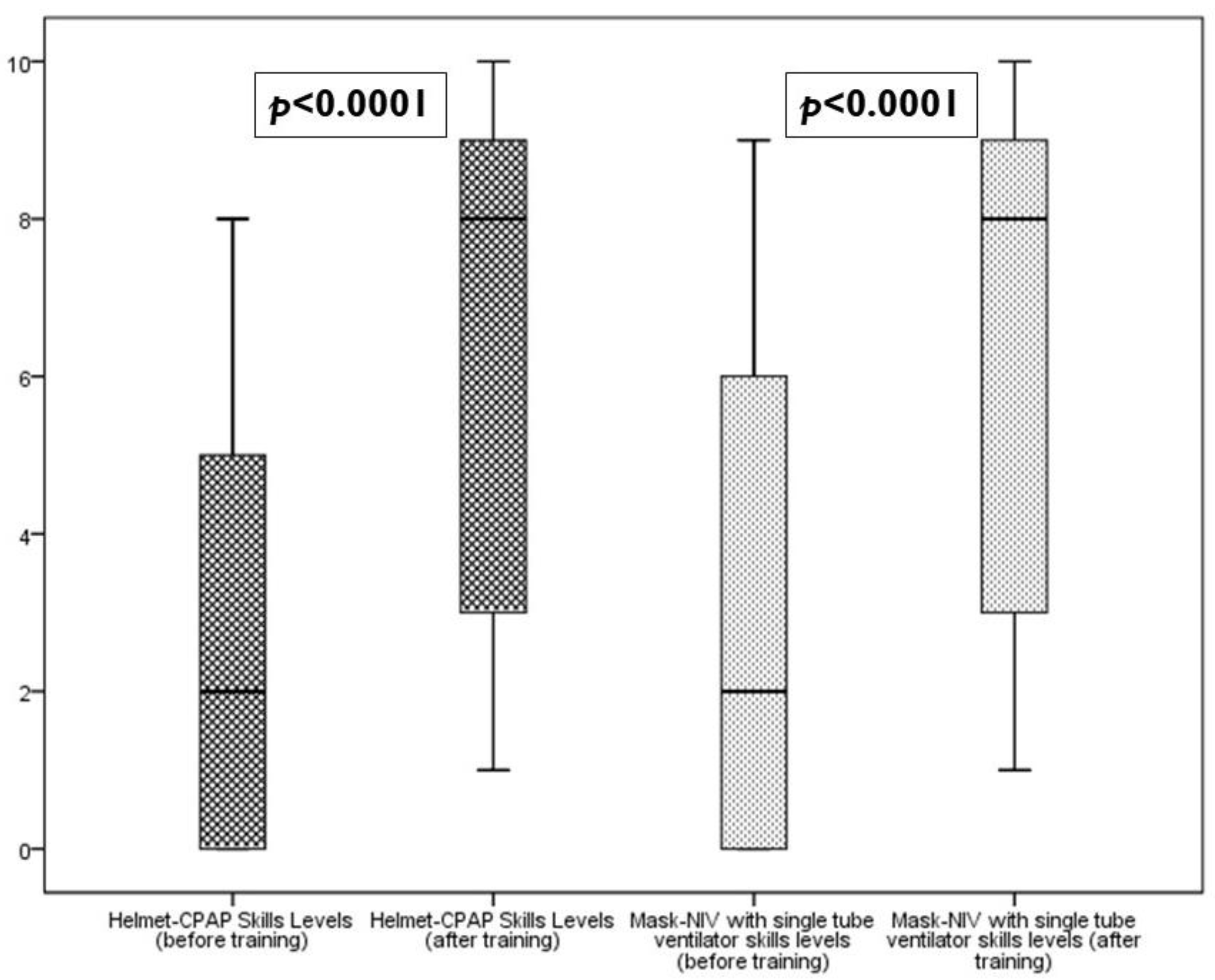
- Self-perception of skills levels in patient management with Helmet-CPAP (Helmet-CPAP skill levels).
- -
- Self-perception of skills levels in patient management with NIV mask through single tube intentional leaks NIV ventilator (NIV skills levels).
2.5. Statistical Analysis
2.6. Ethical Issues
3. Results
3.1. Characteristics of Participants
3.2. Results of the “Brief Skills Self-Report Tool”
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Crimi, C.; Noto, A.; Princi, P.; Esquinas, A.; Nava, S. A European survey of noninvasive ventilation practices. Eur. Respir. J. 2010, 36, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Crimi, C.; Noto, A.; Princi, P.; Nava, S. Survey of non-invasive ventilation practices: A snapshot of Italian practice. Minerva Anestesiol. 2011, 77, 971–978. [Google Scholar] [PubMed]
- Ventrella, F.; Giancola, A.; Cappello, S.; Pipino, M.; Minafra, G.; Carbone, M.; Caccetta, L.; Insalata, M.; Iamele, L. Use and performance of non-invasive ventilation in Internal Medicine ward: A real-life study. Ital. J. Med. 2015, 9, 260–267. [Google Scholar] [CrossRef][Green Version]
- Oranger, M.; Gonzalez-Bermejo, J.; Dacosta-Noble, P.; Llontop, C.; Guerder, A.; Trosini-Desert, V.; Faure, M.; Raux, M.; Decavele, M.; Demoule, A.; et al. Continuous positive airway pressure to avoid intubation in SARS-CoV-2 pneumonia: A two-period retrospective case-control study. Eur. Respir. J. 2020, 56, 2001692. [Google Scholar] [CrossRef] [PubMed]
- Franco, C.; Facciolongo, N.; Tonelli, R.; Dongilli, R.; Vianello, A.; Pisani, L.; Scala, R.; Malerba, M.; Carlucci, A.; Negri, E.A.; et al. Feasibility and clinical impact of out-of-ICU noninvasive respiratory support in patients with COVID-19-related pneumonia. Eur. Respir. J. 2020, 56, 2002130. [Google Scholar] [CrossRef]
- Coppadoro, A.; Zago, E.; Pavan, F.; Foti, G.; Bellani, G. The use of head helmets to deliver noninvasive ventilatory support: A comprehensive review of technical aspects and clinical findings. Crit. Care 2021, 25, 327. [Google Scholar] [CrossRef]
- Cammarota, G.; Esposito, T.; Azzolina, D.; Cosentini, R.; Menzella, F.; Aliberti, S.; Coppadoro, A.; Bellani, G.; Foti, G.; Grasselli, G.; et al. Noninvasive respiratory support outside the intensive care unit for acute respiratory failure related to coronavirus-19 disease: A systematic review and meta-analysis. Crit. Care 2021, 25, 268. [Google Scholar] [CrossRef]
- Burns, G.P.; Lane, N.D.; Tedd, H.M.; Deutsch, E.; Douglas, F.; West, S.D.; Macfarlane, J.G.; Wiscombe, S.; Funston, W. Improved survival following ward-based non-invasive pressure support for severe hypoxia in a cohort of frail patients with COVID-19: Retrospective analysis from a UK teaching hospital. BMJ Open Respir. Res. 2020, 7, e000621. [Google Scholar] [CrossRef]
- Lucchini, A.; Giani, M.; Elli, S.; Villa, S.; Rona, R.; Foti, G. Nursing Activities Score is increased in COVID-19 patients. Intensive Crit. Care Nurs. 2020, 59, 102876. [Google Scholar] [CrossRef]
- Lucchini, A.; Giani, M.; Isgrò, S.; Rona, R.; Foti, G. The “helmet bundle” in COVID-19 patients undergoing non invasive ventilation. Intensive Crit. Care Nurs. 2020, 58, 102859. [Google Scholar] [CrossRef]
- Jackson, D.; Bradbury-Jones, C.; Baptiste, D.; Gelling, L.; Morin, K.; Neville, S.; Smith, G.D. Life in the pandemic: Some reflections on nursing in the context of COVID-19. J. Clin. Nurs. 2020, 29, 2041–2043. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, D.; Frederiksen, K.; Grøfte, T.; Lomborg, K. Practical wisdom: A qualitative study of the care and management of non-invasive ventilation patients by experienced intensive care nurses. Intensive Crit. Care Nurs. 2013, 29, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Torheim, H.; Gjengedal, E. How to cope with the mask? Experiences of mask treatment in patients with acute chronic obstructive pulmonary disease-exacerbations. Scand J. Caring Sci. 2010, 24, 499–506. [Google Scholar] [CrossRef] [PubMed]
- Elliott, M.W.; Confalonieri, M.; Nava, S. Where to perform noninvasive ventilation? Eur. Respir. J. 2002, 19, 1159–1166. [Google Scholar] [CrossRef] [PubMed]
- Rose, L. Management of critically ill patients receiving noninvasive and invasive mechanical ventilation in the emergency department. Open Access Emerg. Med. 2012, 4, 5–15. [Google Scholar] [CrossRef]
- Cox, C.E.; Carson, S.S.; Ely, E.W.; Govert, J.A.; Garrett, J.M.; Brower, R.G.; Morris, D.G.; Abraham, E.; Donnabella, V.; Spevetz, A.; et al. Effectiveness of medical resident education in mechanical ventilation. Am. J. Respir. Crit. Care Med. 2003, 167, 32–38. [Google Scholar] [CrossRef]
- Bierer, G.B.; Soo Hoo, G.W. Noninvasive ventilation for acute respiratory failure: A national survey of Veterans Affairs hospitals. Respir. Care 2009, 54, 1313–1320. [Google Scholar]
- Cabrini, L.; Esquinas, A.; Pasin, L.; Nardelli, P.; Frati, E.; Pintaudi, M.; Matos, P.; Landoni, G.; Zangrillo, A. An international survey on noninvasive ventilation use for acute respiratory failure in general non-monitored wards. Respir. Care 2015, 60, 586–592. [Google Scholar] [CrossRef]
- Nápolis, L.M.; Jeronimo, L.M.; Baldini, D.V.; Machado, M.P.; de Souza, V.A.; Caruso, P. Availability and use of noninvasive ventilation in the intensive care units of public, private and teaching hospitals in the greater metropolitan area of São Paulo, Brazil. J. Bras Pneumol. 2006, 32, 29. [Google Scholar] [CrossRef]
- Tallo, F.S.; de Campos Vieira Abib, S.; de Andrade Negri, F.P.C.; Delascio Lopes, R.; Lopes, A.C. Evaluation of Self-perception of Mechanical Ventilation Knowledge among Brazilian Final-year Medical Students, Residents and Emergency Physicians. Clinics (Sao Paulo) 2017, 72, 65–70. [Google Scholar] [CrossRef]
- Scala, R.; Windisch, W.; Köhnlein, T.; Cuvelier, A.; Navalesi, P.; Pelosi, P.; European Respiratory Society Respiratory Intensive Care Assembly. Targeting European Respiratory Society Group activities: A survey of the Noninvasive Ventilatory Support Group. Eur. Respir. Rev. 2014, 23, 258–260. [Google Scholar] [CrossRef]
- Raurell-Torredà, M.; Argilaga-Molero, E.; Colomer-Plana, M.; Ruiz-García, T.; Galvany-Ferrer, A.; González-Pujol, A. Análisis comparativo de los conocimientos en ventilación mecánica no invasiva de profesionales de cuidados intensivos. Intensive Care Unit Prof. Knowl. About Non Invasive Vent. Comp. Anal. Enferm Intensiva 2015, 26, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Goligher, E.C.; Ferguson, N.D.; Kenny, L.P. Core competency in mechanical ventilation: Development of educational objectives using the Delphi technique. Crit. Care Med. 2012, 40, 2828–2832. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.D.; Gentile, M.A. What does it take to have a successful noninvasive ventilation program? Respir. Care 2009, 54, 53–61. [Google Scholar] [PubMed]
- Nava, S.; Ceriana, P. Causes of failure of noninvasive mechanical ventilation. Respir. Care 2004, 49, 295–303. [Google Scholar]
- McQueen, S.; Dickinson, M.; Pimblett, M. Human patient simulation can aid staff training in non-invasive ventilation. Nurs. Times 2010, 106, 20. [Google Scholar]
- Brill, A.K.; Moghal, M.; Morrell, M.J.; Simonds, A.K. Randomized crossover trial of a pressure sensing visual feedback system to improve mask fitting in noninvasive ventilation. Respirology 2017, 22, 1343–1349. [Google Scholar] [CrossRef]
- Hare, A.; Simonds, A. Simulation-based education for non-invasive ventilation. Breathe 2013, 9, 366–374. [Google Scholar] [CrossRef]
- Bambi, S.; Giani, M.; Lucchini, A. Noninvasive ventilation: Skills, education and training. In Non-Invasive Ventilation. A Practical Handbook for Understanding the Causes of Treatment and Success; Esquinas, A., Ed.; Nova Medicine & Health Inc.: New York, NY, USA, 2019; Chapter 40; ISBN 978-1-53615-200-5. [Google Scholar]
- Nasa, P.; Azoulay, E.; Khanna, A.K.; Jain, R.; Gupta, S.; Javeri, Y.; Juneja, D.; Rangappa, P.; Sundararajan, K.; Alhazzani, W.; et al. Expert consensus statements for the management of COVID-19-related acute respiratory failure using a Delphi method. Crit. Care 2021, 25, 106. [Google Scholar] [CrossRef]
- Weerakkody, S.; Arina, P.; Glenister, J.; Cotterell, S.; Boscaini-Gilroy, G.; Singer, M.; Montgomery, H.E. Non-invasive respiratory support in the management of acute COVID-19 pneumonia: Considerations for clinical practice and priorities for research. Lancet Respir. Med. 2022, 10, 199–213, Erratum in Lancet Respir Med. 2021, 9, e114. [Google Scholar] [CrossRef]
- Alqahtani, J.S.; Aldabayan, Y.S.; AlAhmari, M.D.; AlRabeeah, S.M.; Aldhahir, A.M.; Alghamdi, S.M.; Oyelade, T.; Althobiani, M.; Alrajeh, A.M. Clinical Practice and Barriers of Ventilatory Support Management in COVID-19 Patients in Saudi Arabia: A Survey of Respiratory Therapists. Saudi. J. Med. Med. Sci. 2021, 9, 223–229. [Google Scholar] [CrossRef]
- Karim, H.M.R.; Burns, K.E.A.; Ciobanu, L.D.; El-Khatib, M.; Nicolini, A.; Vargas, N.; Hernández-Gilsoul, T.; Skoczyński, S.; Falcone, V.A.; Arnal, J.M.; et al. Noninvasive ventilation: Education and training. A narrative analysis and an international consensus document. Adv. Respir. Med. 2019, 87, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Lanza, A.; Sommariva, M.; Mariani, S.; Ferreyra, G.; Stagni, G.E.; Tombini, V.; Oppizzi, A.; Pontiggia, C.; Bellone, A. Prolonged non-invasive respiratory support in a COVID-19 patient with severe acute hypoxemic respiratory failure. Monaldi. Arch. Chest. Dis. 2021, 92. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, G.A.; Bozzolo, E.P.; Castelli, E.; Marinosci, A.; Angelillo, P.; Damanti, S.; Scotti, R.; Gobbi, A.; Centurioni, C.; Di Scala, F.; et al. Continuous positive airway pressure and pronation outside the intensive care unit in COVID 19 ARDS. Minerva Med. 2020, 113, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Bradley, P.; Wilson, J.; Taylor, R.; Nixon, J.; Redfern, J.; Whittemore, P.; Gaddah, M.; Kavuri, K.; Haley, A.; Denny, P.; et al. Conventional oxygen therapy versus CPAP as a ceiling of care in ward-based patients with COVID-19: A multi-centre cohort evaluation. EClinicalMedicine 2021, 40, 101122. [Google Scholar] [CrossRef]
- Robinson, R.E.; Nightingale, R.; Frost, F.; Green, T.; Jones, G.; Nwosu, N.; Hampshire, P.; Brown, D.; Beadsworth, M.; Aston, S.; et al. The rapid development and deployment of a new multidisciplinary CPAP service outside of a critical care environment during the early stages of the COVID-19 pandemic. Future Health J. 2021, 8, e156–e159. [Google Scholar] [CrossRef]

| Variable | Ward 1 | Ward 2 | Ward 3 | p |
|---|---|---|---|---|
| Gender Female—n. (%) | 14 (87.5) | 20 (87) | 14 (70) | 0.276 a |
| Age—Median (IQR; range) | 45 (38.5–49.75; 26–52) | 42 (33–50.25; 24–51) | 36 (29–48; 22–50) | 0.113 b |
| Total length of service as staff nurse—Median (IQR; range) | 19.5 (10–21.25; 6–28) | 16.5 (9.5–26.5; 2–30) | 13 (10–22; 4–38) | 0.819 b |
| Length of service in the ward of current assignation—Median (IQR; range) | 9 (4.5–17.25; 2–19) | 12 (4.5–20; 1–20) | 6 (1.5–8; 1–20) | 0.137 b |
| NIV/CPAP education courses in the last 5 years | 7 (41.2) | 11 (45.8) | 15 (60) | 0.428 a |
| Item (Abbreviated) | Before Training Median (IQR; Range) | After Training Median (IQR; Range) | Wilcoxon SIGNED Rank Test p |
|---|---|---|---|
| Frequency Fowler position | 6 (2–9; 0–10) | 9 (3–10; 2–10) | <0.0001 |
| NIV patients check frequency | 5 (2–8; 0–10) | 9 (3–10; 2–10) | <0.0001 |
| RR assessment frequency | 5 (2–7; 0–10) | 7 (3–10; 0–10) | <0.0001 |
| HEPA 24-h application frequency | 3 (0–7; 0–10) | 9 (3–10; 1–10) | <0.0001 |
| Check SpO2 frequency | 5 (3–9; 0–10) | 9 (3–10; 2–10) | <0.0001 |
| Frequency of helmet set-up by 2 nurses | 5 (2–8; 0–10) | 8 (3–10; 1–10) | <0.0001 |
| CPAP system working check frequency | 1 (0–3.25; 0–10) | 7 (3–10; 0–10) | <0.0001 |
| Helmets armpits outside frequency | 0 (0–0; 0–6) | 7 (2–9; 0–10) | <0.0001 |
| Off ventilator frequency | 2 (0–6; 0–10) | 8 (3–10; 0–10) | <0.0001 |
| O2 therapy for NIV breaks frequency | 8.5 (3–10; 0–10) | 9 (3–10; 2–10) | <0.0001 |
| Autonomous set-up of NIV circuit frequency | 2 (0–6.25; 0–10) | 6 (2.5–9; 0–10) | <0.0001 |
| Item (Abbreviated) | Ward 1 Median (IQR; Range) | Ward 2 Median (IQR; Range) | Ward 3 Median (IQR; Range) | Kruskall Wallis Test p |
|---|---|---|---|---|
| Frequency Fowler position | 9 (3.5–10; 2–10) | 9 (8–10; 2–10) | 7.5 (2.25–10; 2–10) | 0.270 |
| NIV patients check frequency | 8.5 (3.5–10; 2–10) | 9 (8–10; 2–10) | 7.5 (3–10; 2–10) | 0.509 |
| RR assessment frequency | 6.5 (3–9.75; 1–10) | 8 (3–10; 0–10) | 8 (2.25–10; 2–10) | 0.970 |
| HEPA 24-h application frequency | 9 (3.75–10; 2–10) | 9 (8–10; 2–10) | 8.5 (3–10; 1–10) | 0.476 |
| Check SpO2 frequency | 8 (3.5–9.75; 2–10) | 9.5 (7.25–10; 2–10) | 8 (3–10; 2–10) | 0.414 |
| Frequency of helmet set-up by 2 nurses | 8.5 (3.75–10; 2–10) | 8 (6–9; 2–10) | 7.5 (3–10; 1–10) | 0.641 |
| CPAP system working check frequency | 8 (3.25–9.75; 1–10) | 7 (2–10; 0–10) | 7 (3–10; 2–10) | 0.755 |
| Helmets armpits outside frequency | 7.5 (4–8.75; 2–10) | 7 (2–9; 0–10) | 7 (2–10; 0–10) | 0.764 |
| Off ventilator frequency | 9 (3–10; 1–10) | 8 (2–10; 0–10) | 8 (3–10; 2–10) | 0.674 |
| O2 therapy for NIV breaks frequency | 9 (4–10; 2–10) | 9 (8–10; 2–10) | 7 (3–10; 2–10) | 0.562 |
| Autonomous set-up of NIV circuit frequency | 7.5 (3–9.25; 2–10) | 6 (1–8; 0–10) | 3 (2.25–9; 0–10) | 0.492 |
| Helmet-CPAP skill levels | 8 (3.25–9; 1–10) | 8 (7–9; 1–10) | 8 (3–8.75; 1–10) | 0.466 |
| NIV skills levels | 8 (3–9; 2–9) | 7 (5.5–8.25; 1–10) | 8 (3–9; 1–10) | 0.977 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bambi, S.; Parente, E.; Bardacci, Y.; Baldassini Rodriguez, S.; Forciniti, C.; Ballerini, L.; Caruso, C.; El Aoufy, K.; Poggianti, M.; Bonacaro, A.; et al. The Effectiveness of NIV and CPAP Training on the Job in COVID-19 Acute Care Wards: A Nurses’ Self-Assessment of Skills. Nurs. Rep. 2023, 13, 17-28. https://doi.org/10.3390/nursrep13010002
Bambi S, Parente E, Bardacci Y, Baldassini Rodriguez S, Forciniti C, Ballerini L, Caruso C, El Aoufy K, Poggianti M, Bonacaro A, et al. The Effectiveness of NIV and CPAP Training on the Job in COVID-19 Acute Care Wards: A Nurses’ Self-Assessment of Skills. Nursing Reports. 2023; 13(1):17-28. https://doi.org/10.3390/nursrep13010002
Chicago/Turabian StyleBambi, Stefano, Eustachio Parente, Yari Bardacci, Samuele Baldassini Rodriguez, Carolina Forciniti, Lorenzo Ballerini, Christian Caruso, Khadija El Aoufy, Marta Poggianti, Antonio Bonacaro, and et al. 2023. "The Effectiveness of NIV and CPAP Training on the Job in COVID-19 Acute Care Wards: A Nurses’ Self-Assessment of Skills" Nursing Reports 13, no. 1: 17-28. https://doi.org/10.3390/nursrep13010002
APA StyleBambi, S., Parente, E., Bardacci, Y., Baldassini Rodriguez, S., Forciniti, C., Ballerini, L., Caruso, C., El Aoufy, K., Poggianti, M., Bonacaro, A., Rona, R., Rasero, L., & Lucchini, A. (2023). The Effectiveness of NIV and CPAP Training on the Job in COVID-19 Acute Care Wards: A Nurses’ Self-Assessment of Skills. Nursing Reports, 13(1), 17-28. https://doi.org/10.3390/nursrep13010002











