Abstract
Background: The integration of artificial intelligence (AI) in the organization of nursing care has continually evolved, driven by the need for innovative solutions to ensure quality of care. The aim is to synthesize the evidence on the use of artificial intelligence in the organization of nursing care. Methods: A scoping review was carried out based on the Joanna Briggs Institute methodology, following the PRISMA-ScR guidelines, in the MEDLINE, CINAHL Complete, Business Source Ultimate and Scopus® databases. We used ProQuest—Dissertations and Theses to search gray literature. Results: Ten studies were evaluated, identifying AI-mediated tools used in the organization of nursing care, and synthesized into three tool models, namely monitoring and prediction, decision support, and interaction and communication technologies. The contributions of using these tools in the organization of nursing care include improvements in operational efficiency, decision support and diagnostic accuracy, advanced interaction and efficient communication, logistical support, workload relief, and ongoing professional development. Conclusions: AI tools such as automated alert systems, predictive algorithms, and decision support transform nursing by increasing efficiency, accuracy, and patient-centered care, improving communication, reducing errors, and enabling earlier interventions with safer and more efficient quality care.
1. Introduction
Over time, the evolution of quality and safety in nursing care has been significant; hence, there is great concern for and focus on improving healthcare services [1,2]. Several factors have contributed to these advances, including client involvement, professional and organizational engagement, and the development of client-centered care standards, with an emphasis on safety and evidence-based practice [3,4]. These trends have shaped and enhanced nursing practice globally, influencing the conception and implementation of care.
The organization of nursing care is fundamental to guaranteeing positive results for patients. The Portuguese Order of Nurses, in line with international guidelines, believes that the organization of nursing care involves nurses adopting methodologies for organizing nursing care [5]. These methodologies are aimed at designing, planning, implementing and evaluating the nursing care to be provided to patients according to their needs. It is also important to highlight the implementation of standardized practices, the appropriate allocation of material and human resources, performance monitoring, effective communication, risk management, investment in professional training, continuous training and the use of technological resources as fundamental to care management [6]. These factors can differentiate the provision of high-quality care.
The increasing demand for healthcare services, associated with more complex care requirements, drives the search for innovative solutions to optimize nursing practices [7]. In this context, Artificial Intelligence (AI) has emerged as a disruptive and promising force, offering various tools and techniques that support clinical practice and decision-making. The integration of AI has the potential to bring substantial changes in how nursing care is organized, managed, and delivered [8,9].
The integration of AI into the workflow and work organization of nurses significantly contributes to improving the quality of care, efficiency, and effectiveness of healthcare institutions, resulting in increased satisfaction for both patient and nursing staff satisfaction [10]. In this context, AI can be classified into three domains: clinical, remote care, and care management. In the clinical domain, AI can support decision-making through real-time patient monitoring and automated triage, in addition to improving safety by preventing errors and assessing risks [11]. In the domain of remote care, AI enables remote monitoring and support for teleconsultations, as well as automated interventions in emotional support and mental health for both professionals and patients [12]. In the care management domain, AI optimizes resource allocation based on workload and allows for the automation of administrative tasks [13].
However, it is crucial to address the challenges arising from the implementation of this technology, including ethical issues and the need for adequate training to maximize benefits and minimize risks [14].
Given the importance of this topic and the emerging need to rethink new strategies for the conception, implementation, and organization of nursing care, we identified that there are no systematic reviews or scoping reviews conducted or ongoing on this topic. Thus, we highlight that the organization of nursing care has gained prominence in recent years, which aligns with the growing concern for improving healthcare quality and the need for better health outcomes [15,16]. The lack of systematic evidence on the integration of AI into the organization of nursing care and the potential benefits that could support safer and more patient-centered nursing practice motivated the conduct of this study.
Based on these premises, it is understood that mapping the available evidence on how AI can contribute to the organization and enhancement of nursing care is crucial. Additionally, filling this gap could provide valuable insights for clinical practice and health policy formulation. Thus, the aim is to synthesize the evidence on the use of artificial intelligence in the organization of nursing care.
2. Materials and Methods
This review was conducted following the methodology proposed by the Joanna Briggs Institute for scoping reviews, and its writing adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses for Scoping Reviews (PRISMA-ScR) guidelines [17,18]. The protocol for this review was developed and is registered with the Open Science Framework (https://doi.org/10.17605/OSF.IO/VX6TD (accessed on 1 April 2024).
We used the Population, Concept, and Context (PCC) framework to construct the research question: What is the contribution of artificial intelligence to the organization of nursing care? Hence, we emphasize that the PCC framework was followed for defining the eligibility criteria in accordance with the guidelines recommended by the Joanna Briggs Institute [17].
In terms of the population, we considered primary articles that featured nursing professionals as the population, regardless of their category.
Regarding the concept, we included studies that addressed the concepts of artificial intelligence, the organization of nursing care and their relationship. Artificial intelligence is an innovative technology that enables computers to perform tasks requiring intelligence and critical thinking identical to humans [19]. In the healthcare domain, AI can be divided into two categories, namely virtual and physical. Virtual AI includes applications such as electronic health record systems and neural network-based guidance for treatment decisions, while physical AI involves the use of robots assisting in surgeries and smart prosthetics for individuals with disabilities, among others [20].
The organization of nursing care is a multifaceted process that can be executed through one or more work methods. These methods are defined as the infrastructure necessary to facilitate the provision of care to clients in different nursing practice contexts. They depend on the competencies acquired by nurses and the expected outcomes of care delivery. Nurses’ work methods play a crucial role in task allocation and decision-making processes and can reflect aspects such as social values, management ideologies, human resources, or the organizational policies of the institution [21].
Regarding the context, we included studies conducted in any clinical practice context of nurses, as we aimed to conduct a comprehensive review on the topic without specifying contexts.
It is important to highlight that this scoping review will include quantitative studies, experimental, quasi-experimental, prospective, retrospective, case-control, and cross-sectional studies. It will also cover observational studies, qualitative studies such as phenomenological, ethnographic, or descriptive studies, mixed methods studies, reviews, and grey literature. This breadth of studies allows for greater sensitivity in searches aimed at mapping the available evidence.
We followed a three-phase search strategy. Initially, we conducted a limited search in MEDLINE (PubMed) and CINAHL (Cumulative Index to Nursing and Allied Health Literature; EBSCO) to identify articles on the topic under study. By reviewing these studies, we were able to identify terms and keywords to develop a comprehensive and sensitive search strategy. Subsequently, we conducted a second search using the identified keywords and terms in the following databases: MEDLINE (PubMed), CINAHL (EBSCO), Business Source Ultimate (EBSCO), and Scopus®. For grey literature, we utilized ProQuest—Dissertations and Theses. The search was conducted in January 2024 using the terms “Artificial Intelligence,” “Nurse Administrators,” and “Nurse Manager,” along with their related terms (Table 1).

Table 1.
Search strategy in databases.
We used MeSH terms and CINAHL headings to determine the search terms across several databases. We considered both published literature and grey literature in any language and without a time limit. During the third phase of the search, we reviewed the reference lists of included studies but did not find any additional relevant studies.
After conducting the search, we uploaded all identified studies to the Rayyan platform, and duplicates were identified and removed. Two independent reviewers assessed the titles and abstracts to determine eligibility criteria and conducted a pilot screening of the first 25 titles and abstracts to ensure that the previously defined eligibility criteria were sensitive to the desired outcomes and that consensus was reached among the reviewers. The full text of all studies that met or potentially met the eligibility criteria was analyzed by two independent reviewers. Any discrepancies between the reviewers were resolved through constructive discussion, without the need to involve a third reviewer.
Data extraction was independently conducted by two reviewers who analyzed the full text and recorded all reasons for the exclusion of studies. A data extraction table was developed by the authors for data extraction. The extracted information included details about the studies such as authors, year of publication, country of origin, objective and study type, and the main results that addressed the research question and objective. After data extraction, we performed a thematic analysis of the findings, followed by a narrative synthesis of the main findings.
3. Results
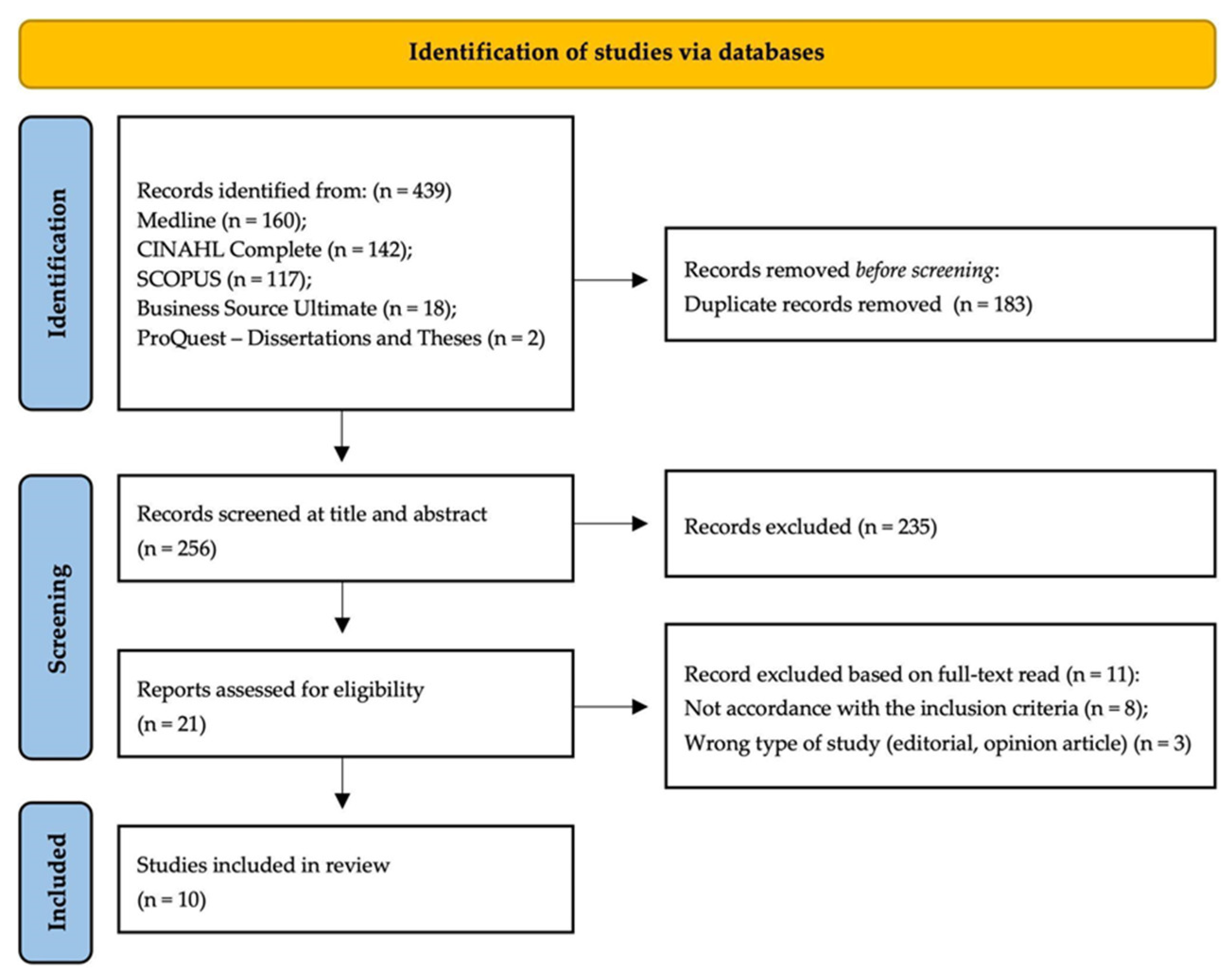
We identified a total of 439 studies across five databases, and 256 studies remained after removing duplicates. After screening the titles and abstracts, 235 studies were excluded. The full text of 21 studies was then read and assessed for compliance with the predefined eligibility criteria. Upon completing all phases of analysis and evaluation, 10 studies were included in this review. The results of the search conducted, as well as the reasons for study exclusion, are presented in the PRISMA flow diagram (Figure 1) [22].
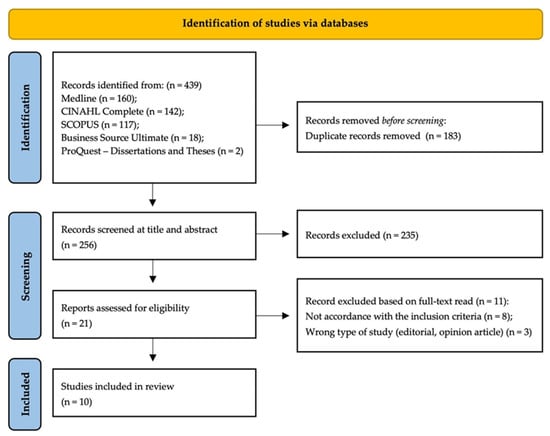
Figure 1.
PRISMA flow diagram.
The studies included in the review were published between 2008 and 2022. The countries of origin included China [23,24,25], Colombia [26], Spain [27], the United States of America [28,29,30], Finland [31], and Turkey [32] (Table 2).

Table 2.
Characterization of included studies.
The results were synthesized and organized into two themes, namely tools for the organization of nursing care using artificial intelligence, and contributions of using tools for the organization of nursing care using artificial intelligence.
3.1. Tools for the Organisation of Nursing Care Using Artificial Intelligence
Within the organization of nursing care, a variety of AI tools are increasingly being used to improve the efficiency, quality, and safety of nursing care. By mapping the articles of this review, numerous AI-mediated tools used in nursing care organization were identified, which were then divided into three models of tools, namely monitoring and prediction, decision support, and interaction and communication technologies.
The monitoring and prediction tools for nursing care included automated alert systems using residential sensor data for health assessment [23,27,31]; machine learning models to predict the development of pressure injuries based on nursing assessment phenotypes [31]; predictive algorithms to identify nursing diagnoses [24,26,32]; surveillance systems [28]; fall risk prevention [27]; and the Rothman index [30].
On the other hand, the decision support tools in nursing care included decision support systems for triage management [31]; clinical decision support systems [23,24,27,28]; nursing expert systems [28]; and health information management systems [23,24,27].
Lastly, the interaction and communication technologies tools for nursing care involved automated classification systems for unstructured clinical notes to aid in the organization and analysis of clinical information [31]; voice recognition systems for direct documentation [31]; electronic reminders [29]; mobile app for emergency services [25]; chatbots and virtual assistance [23,24,27]; robots programmed to assist in patient transfer and mobilization [32]; mobile applications; transparent and explainable AI systems [30]; and process automation for patients [26].
Table 3 summarizes all the tools found and their respective descriptions.

Table 3.
Tools for nursing care organization using artificial intelligence.
The AI-based tools for nursing care organization encompass a variety of innovative resources aimed at improving the efficiency, quality, and safety of care provided. These technologies include automated alerts, machine learning models, decision support, classification systems, and voice recognition, among others. The use of these tools aims to optimize clinical information management, support the decision-making process, prevent risks, and promote a more effective and proactive approach to nursing care delivery.
3.2. Contributions of Using Tools for Nursing Care Organization Utilizing Artificial Intelligence
The integration of Artificial Intelligence (AI)-based tools in the organization of nursing care is significantly transforming the practice of nursing, bringing a set of contributions ranging from improved efficiency and quality of care to the promotion of safer and more patient-centered care. These technological innovations are reshaping how nursing professionals interact with data, make decisions, and perform daily tasks, contributing to a more modern and responsive healthcare environment.
Amongst the contributions, operational efficiency in nursing care [23,24,25,26,28,29,31,32] is significantly enhanced with the use of AI tools. Automated alert systems [24,28] and predictive algorithms [26,32] allow real-time monitoring of patients’ health using data from residential and hospital sensors. These systems can identify patterns and anomalies that might go unnoticed in the overloaded day-to-day workload of healthcare professionals. The ability to predict adverse events [24,29,30,31] is considered one of the main advantages, as it enables early and preventive interventions, reducing complications and improving clinical outcomes.
Another contribution involves decision support [23,24,25,28,29,31,32], with AI tools involving clinical decision support systems in nursing and providing a solid foundation for informed decision-making. These systems use advanced algorithms and evidence-based data to analyze clinical information and offer precise and personalized recommendations [23,24,28,29,30,31]. Hence, they help overcome variability in clinical practice, ensuring that the care provided is consistent and of high quality. Moreover, by alleviating part of the cognitive load on nursing professionals, these tools grant more time to be devoted to direct patient care, strengthening the nurse–patient relationship, and improving patient satisfaction [23,24,27,28,29].
Advanced interaction [29] and communication is another contribution to the use of AI tools, as chatbots and voice recognition systems [23] facilitate efficient and accurate communication both among healthcare professionals and between professionals and patients. These technologies allow direct documentation and quick access to clinical information [28,31], optimization of workflow [26,27] and minimization of errors [23,24,25,26,28,29,30,31]. Additionally, the introduction of mobile apps facilitates nursing professionals to access real-time information and updates [25,28,31], serving as a crucial bridge between the patient’s needs and the caregiver’s actions in dynamic environments.
Logistical support [32] and workload relief [26,27] stand out as contributions of using AI tools in the context of nursing care, as robots programmed to perform non-clinical tasks, such as patient mobility and heavy load transportation, are reconfiguring the work routine of nursing professionals. By taking on these physical and repetitive tasks, robots help reduce the risk of occupational injuries among healthcare professionals and increase their productivity. This allows nursing professionals to focus their efforts and skills on more complex and patient-centered activities, raising the overall standard of care provided [32].
Finally, it is evident that the technological evolution driven by AI also offers numerous opportunities for continuous professional development. Thus, training and education focused on AI are becoming essential to prepare nursing professionals for the future demands of healthcare. By learning to use AI tools effectively, healthcare professionals can expand their competencies and stay updated with evidence-based practices. Continuous development is crucial to ensure that technological innovations are integrated ethically and effectively into daily practice, promoting patient-centered care that respects the individuality and dignity of each person [23,28].
4. Discussion
The studies included in this review demonstrate that artificial intelligence has contributed to the organization of nursing care, aiming to improve the efficiency, quality, and safety of the care provided [9,33]. Furthermore, it is noted that AI is not viewed as a replacement but rather as a complement to nursing practice [34].
Artificial intelligence plays a crucial role in monitoring and predicting nursing care, both in hospital environments and in home settings. Its application is particularly significant in data collection and the continuous monitoring of health conditions over time, allowing for the early identification of signs that indicate either deterioration or improvement in a patient’s condition. Furthermore, the insights generated by AI facilitate more precise care, helping to reduce adverse events and directly enhancing the overall quality of care provided [35,36,37,38,39]. The use of AI has demonstrated a positive impact, particularly in enhancing diagnostic accuracy, promoting client-centered care, and reducing adverse events [37,40,41].
The AI developed to support decision-making in nursing care has proven to be a valuable resource. The results indicate the use of algorithms for analyzing data recorded by nurses during patient care, allowing for the processing of large volumes of clinical information, such as medical history, test results, and vital signs. Thus, it is evident that AI can play a significant role in enhancing critical thinking and clinical decision-making [34]. The data provided by healthcare professionals facilitate the assessment and management of patient conditions, allowing for the identification of diagnoses, personalization of care plans, and prioritization of interventions, thus increasing the efficiency of care provided. In this context, AI is crucial for real-time decision-making in challenging health situations, where patient conditions may be more unstable, making it a client-centered strategy and an essential facilitator for clinical practice [42].
Other types of AI have significantly contributed to the management and continuity of patient care, enhancing communication between nurses and the entire healthcare team, as well as optimizing material and human resources, especially in the execution of administrative tasks. The main AI tools used in the management process of nursing work include virtual assistants, chatbots, clinical decision support systems, telemedicine platforms, remote monitoring devices, big data analysis, and augmented and virtual reality technologies [43,44]. Similarly, mobile applications have provided quick access to relevant data, aiding in the organization, delivery, and transition of care [45]. These, AI tools facilitate clinical documentation and enhance communication among healthcare professionals, contributing to safer and more integrated care [46,47].
In this context, AI significantly impacts the nurses’ work, not only by facilitating activity management and time availability but also by reducing workload, allowing greater focus on direct patient care by identifying actual needs and improving care quality [48,49]. It is important to emphasize that, for nursing managers, AI can help organize teamwork, improving effectiveness and professional performance. Additionally, the introduction of robots for non-professional tasks, such as transporting heavy objects, can increase the productivity of the nursing staff [34].
Despite technological advances and improvements in nursing practice, the implementation of AI in nursing care organizations still faces significant barriers. A notable aspect is the lack of clarity on how these technologies can be integrated efficiently and safely, which emphasizes the importance of nurse training, focusing on their professional and continuous development and covering topics such as the use of AI and awareness of its clinical applicability. Thus, the need for workplace training to familiarize nurses with tools available to nursing care organization becomes essential [50]. Likewise, the need for investment in professional training regarding new AI-based tools is essential to ensure they also benefit patients [51].
It is crucial to highlight a fundamental aspect related to the ethical and safe use of AI, safeguarding each client’s integrity and individuality. Ensuring privacy, integrity, and individuality and avoiding potential algorithmic biases or discrimination are essential when using AI [52]. Healthcare organizations must invest not only in adopting these technologies but also in creating an environment that promotes innovation and the acceptance of AI use by healthcare professionals [53]. This involves developing clear policies, fostering a culture of continuous learning, and ensuring all team members understand AI’s benefits and limitations. By investing in such initiatives, it is possible to maximize potential gains in efficiency and quality in nursing care delivery [54].
Despite the transformative potential of AI in nursing practice, which spans from clinical decision-making to work organization and the promotion of patient-centered care, as evidenced by the results of this study, a limitation to consider is that the included studies focus on the use of AI in specific contexts, without clearly demonstrating its contribution to the broader organization of nursing care.
5. Conclusions
The increasing integration of AI into nursing care organizations has demonstrated a significant impact on the efficiency, effectiveness, and quality of services provided. These technologies should be seen as complementary to the clinical practice of nurses, as they facilitate quick decision-making, especially in contexts where patients’ clinical conditions are challenging. Additionally, AI enables the implementation of a more patient-centered approach, promoting a more efficient allocation of resources and contributing to the safety of care.
The use of AI also supports timely access to relevant data, assisting nurses in organizing and delivering care, which makes nursing practice more agile and effective. The responsible and secure integration of AI into nursing practice has the potential to positively transform the way care is delivered, from clinical decision-making to work organization and the promotion of patient-centered care. However, the use of AI must be conducted with caution, always safeguarding patient privacy and security through ethical and responsible use of technology.
In summary, AI represents a valuable contribution to the organization of nursing care and should be used as a complement to nursing practice to support quick and accurate decision-making, especially in complex clinical situations.
Author Contributions
Conceptualization, J.V.-S., M.M.M., L.d.L.T. and O.M.P.L.R.; methodology, J.V.-S., S.P., S.S.Z. and O.M.P.L.R.; formal analysis, J.V.-S., S.P. and S.S.Z.; resources, J.V.-S., A.d.C.A.F., S.P. and S.S.Z.; data curation, J.V.-S., S.P., S.S.Z. and O.M.P.L.R.; writing—original draft preparation, J.V.-S., L.d.L.T., S.S.Z. and O.M.P.L.R.; writing—review and editing, J.V.-S., L.d.L.T., S.P., S.S.Z. and O.M.P.L.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Public Involvement Statement
There was no public participation in any aspect of this research.
Guidelines and Standards Statement
This manuscript was written according to the Joanna Briggs Institute methodology for scoping review research.
Use of Artificial Intelligence
AI or AI-assisted tools were not used in drafting any aspect of this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Encarnação, R.; Manuel, T.; Palheira, H.; Neves-Amado, J.; Alves, P. Artificial Intelligence in Wound Care Education: Protocol for a Scoping Review. Nurs. Rep. 2024, 14, 627–640. [Google Scholar] [CrossRef] [PubMed]
- Osei Afriyie, D.; Masiye, F.; Tediosi, F.; Fink, G. Purchasing for high-quality care using National Health Insurance: Evidence from Zambia. Health Policy Plan. 2023, 38, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Dhopeshwarkar, R.V.; Freij, M.; Callaham, M.; Desai, P.J.; Harrison, M.; Swiger, J.; Lomotan, E.; Dymek, C.; Dullabh, P. Lessons Learned from a National Initiative Promoting Publicly Available Standards-Based Clinical Decision Support. Appl. Clin. Inform. 2023, 14, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Seegan, P.L.; Miller, L.; Young, A.S.; Parrish, C.; Cullen, B.; Reynolds, E.K. Enhancing Quality of Care Through Evidence-Based Practice: Training and Supervision Experiences. Am. J. Psychother. 2023, 76, 100–106. [Google Scholar] [CrossRef]
- Ordem dos Enfermeiros. Padrões de Qualidade dos Cuidados de Enfermagem: Enquadramento Conceptual, Enunciados Descritivos; Ordem dos Enfermeiros: Lisboa, Portugal, 2012. [Google Scholar]
- Choi, J.; Woo, S.; Ferrell, A. Artificial intelligence assisted telehealth for nursing: A scoping review. J. Telemed. Telecare 2023, OnlineFirst. [Google Scholar] [CrossRef]
- Odone, A.; Buttigieg, S.; Ricciardi, W.; Azzopardi-Muscat, N.; Staines, A. Public health digitalization in Europe. Eur. J. Public Health 2019, 29, 28–35. [Google Scholar] [CrossRef]
- Koski, E.; Murphy, J. AI in Healthcare. Stud. Health Technol. Inform. 2021, 284, 295–299. [Google Scholar]
- Tursunbayeva, A.; Renkema, M. Artificial intelligence in health-care: Implications for the job design of healthcare professionals. Asia Pac. J. Hum. Resour. 2023, 61, 845–887. [Google Scholar] [CrossRef]
- Vasquez, B.; Moreno-Lacalle, R.; Soriano, G.P.; Juntasoopeepun, P.; Locsin, R.C.; Evangelista, L.S. Technological machines and artificial intelligence in nursing practice. Nurs. Health Sci. 2023, 25, 474–481. [Google Scholar] [CrossRef]
- Douthit, B.J.; Walden, R.L.; Cato, K.; Coviak, C.P.; Cruz, C.; D’Agostino, F.; Forbes, T.; Gao, G.; Kapetanovic, T.A.; Lee, M.A.; et al. Data Science Trends Relevant to Nursing Practice: A Rapid Review of the 2020 Literature. Appl. Clin. Inform. 2022, 13, 161–179. [Google Scholar] [CrossRef]
- Wilton, A.R.; Sheffield, K.; Wilkes, Q.; Chesak, S.; Pacyna, J.; Sharp, R.; Croarkin, P.E.; Chauhan, M.; Dyrbye, L.N.; Bobo, W.V.; et al. The Burnout Prediction Using Wearable and ArtIficial Intelligence (BROWNIE) study: A decentralized digital health protocol to predict burnout in registered nurses. BMC Nurs. 2024, 23, 114. [Google Scholar] [CrossRef] [PubMed]
- Rony, M.K.K.; Kayesh, I.; Bala, S.D.; Akter, F.; Parvin, M.R. Artificial intelligence in future nursing care: Exploring perspectives of nursing professionals—A descriptive qualitative study. Heliyon 2024, 10, e25718. [Google Scholar] [CrossRef]
- Economou-Zavlanos, N.J.; Bessias, S.; Cary, M.P., Jr.; Bedoya, A.D.; Goldstein, B.A.; Jelovsek, J.E.; O’Brien, C.L.; Walden, N.; Elmore, M.; Parrish, A.B.; et al. Translating ethical and quality principles for the effective, safe and fair development, deployment and use of artificial intelligence technologies in healthcare. J. Am. Med. Inform. Assoc. 2024, 31, 705–713. [Google Scholar] [CrossRef]
- Ventura-Silva, J.M.A.; Martins, M.M.F.P.S.; Trindade, L.L.; Ribeiro, O.M.P.L.; Cardoso, M.F.P.T. Working methods of nurses in hospitals: Scoping review. J. Health NPEPS 2021, 6, 278–295. [Google Scholar]
- Ventura-Silva, J.M.A.; Martins, M.M.F.P.S.; Trindade, L.L.; Faria, A.C.A.; Barros, S.C.C.; Melo, R.M.C.; Forte, E.C.N.; Ribeiro, O.M.P.L. Nurses’ Work Methods Assessment Scale: A study of content validation. Rev. Bras. Enferm. 2023, 76, e20220396. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Hamet, P.; Tremblay, J. Artificial intelligence in medicine. Metabolism 2017, 69, 36–40. [Google Scholar] [CrossRef]
- Amisha; Malik, P.; Pathania, M.; Rathaur, V.K. Overview of artificial intelligence in medicine. J. Fam. Med. Prim. Care 2019, 8, 2328–2331. [Google Scholar] [CrossRef]
- Ventura-Silva, J.; Martins, M.M.; Trindade, L.; Faria, A.; Barros, S.; Melo, R.; Ribeiro, O. Characterization of nurses’ work methods: The analysis of a Portuguese hospital. NPT 2023, 11, 34–43. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 1–9. [Google Scholar]
- Li, X.; Cheng, M.; Xu, J. Leaders’ innovation expectation and nurses’ innovation behaviour in conjunction with artificial intelligence: The chain mediation of job control and creative self-efficacy. J. Nurs. Manag. 2022, 30, 3806–3816. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.Y.; Huang, T.L.; Wong, M.K.; Ho, L.H.; Wu, C.N.; Teng, C.I. Robots Help Nurses Focus on Professional Task Engagement and Reduce Nurses’ Turnover Intention. J. Nurs. Scholarsh. 2021, 53, 237–245. [Google Scholar] [CrossRef]
- Dong, A.; Guo, J.; Cao, Y. Medical Information Mining-Based Visual Artificial Intelligence Emergency Nursing Management System. J. Healthc. Eng. 2021, 2021, 4253606. [Google Scholar] [CrossRef]
- Moreno-Fergusson, M.E.; Guerrero Rueda, W.J.; Ortiz Basto, G.A.; Arevalo Sandoval, I.A.L.; Sanchez-Herrera, B. Analytics and Lean Health Care to Address Nurse Care Management Challenges for Inpatients in Emerging Economies. J. Nurs. Scholarsh. 2021, 53, 803–814. [Google Scholar] [CrossRef]
- Ladios-Martin, M.; Cabañero-Martínez, M.J.; Fernández-de-Maya, J.; Ballesta-López, F.J.; Belso-Garzas, A.; Zamora-Aznar, F.M.; Cabrero-Garcia, J. Development of a predictive inpatient falls risk model using machine learning. J. Nurs. Manag. 2022, 30, 3777–3786. [Google Scholar] [CrossRef] [PubMed]
- Courtney, K.L.; Alexander, G.L.; Demiris, G. Information technology from novice to expert: Implementation implications. J. Nurs. Manag. 2008, 16, 692–699. [Google Scholar] [CrossRef][Green Version]
- Piscotty, R.J.; Kalisch, B.; Gracey-Thomas, A.; Yarandi, H. Electronic nursing care reminders: Implications for nursing leaders. J. Nurs. Adm. 2015, 45, 239–242. [Google Scholar] [CrossRef]
- Robert, N. How artificial intelligence is changing nursing. Nurs. Manag. 2019, 50, 30–39. [Google Scholar] [CrossRef]
- Gerich, H.; Moen, H.; Block, L.J.; Chu, C.H.; DeForest, H.; Hobensack, M.; Michalowski, M.; Mitchell, J.; Nibber, R.; Olalia, M.A.; et al. Artificial Intelligence -based technologies in nursing: A scoping literature review of the evidence. Int. J. Nurs. Stud. 2022, 127, 104153. [Google Scholar] [CrossRef]
- Ergin, E.; Karaarslan, D.; Şahan, S.; Çınar Yücel, Ş. Artificial intelligence and robot nurses: From nurse managers’ perspective: A descriptive cross-sectional study. J. Nurs. Manag. 2022, 30, 3853–3862. [Google Scholar] [CrossRef]
- Pailaha, A.D. The Impact and Issues of Artificial Intelligence in Nursing Science and Healthcare Settings. SAGE Open Nurs. 2023, 9, 23779608231196847. [Google Scholar] [CrossRef] [PubMed]
- Mohanasundari, S.K.; Kalpana, M.; Madhusudhan, U.; Vasanthkumar, K.B.R.; Singh, R.; Vashishtha, N.; Bhatia, V. Can Artificial Intelligence Replace the Unique Nursing Role? Cureus 2023, 15, e51150. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.C.; O’Connor, S.; Stanmore, E. The Application of Artificial Intelligence in Digital Physical Activity and Falls Prevention Interventions for Older Adults. J. Aging Phys. Act. 2023, 31, 887–889. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.H.; Xu, J.L. Applying artificial intelligence to predict falls for inpatient. Front. Med. 2023, 10, 1285192. [Google Scholar] [CrossRef] [PubMed]
- Van Bulck, L.; Couturier, R.; Moons, P. Applications of artificial intelligence for nursing: Has a new era arrived? Eur. J. Cardiovasc. Nurs. 2023, 22, 19–20. [Google Scholar] [CrossRef]
- Ng, Z.Q.P.; Ling, L.Y.J.; Chew, H.S.J.; Lau, Y. The role of artificial intelligence in enhancing clinical nursing care: A scoping review. J. Nurs. Manag. 2022, 30, 3654–3674. [Google Scholar] [CrossRef]
- Ribeiro, O.M.; Trindade, L.; Fassarella, C.; Pereira, S.C.; Teles, P.J.; Rocha, C.; Leite, P.C.; Ventura-Silva, J.M.; Sousa, C. Impact of COVID-19 on professional nursing practice environments and patient safety culture. J. Nurs. Manag. 2022, 30, 1105–1114. [Google Scholar] [CrossRef]
- Karargyris, A.; Umeton, R.; Sheller, M.J.; Aristizabal, A.; George, J.; Wuest, A.; Pati, S.; Kassem, H.; Zenk, M.; Baid, U.; et al. Federated benchmarking of medical artificial intelligence with MedPerf. Nat. Mach. Intell. 2023, 5, 799–810. [Google Scholar] [CrossRef]
- Wibowo, A.; Putri, L. Advancements in Personalized Medicine through Artificial Intelligence: A Detailed Study of Ethical Considerations and Practical Outcomes. QJCTH 2024, 9, 11–19. [Google Scholar]
- Loftus, T.J.; Balch, J.A.; Marquard, J.L.; Ray, J.M.; Alper, B.S.; Ojha, N.; Bihorac, A.; Melton-Meaux, G.; Khanna, G.; Tignanelli, C.J. Longitudinal clinical decision support for assessing decisions over time: State-of-the-art and future directions. Digit. Health 2024, 10, 20552076241249925. [Google Scholar] [CrossRef] [PubMed]
- Rony, M.K.K.; Parvin, M.R.; Ferdousi, S. Advancing nursing practice with artificial intelligence: Enhancing preparedness for the future. Nurs. Open 2024, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Zheng, X.; Ding, H. Existing Barriers Faced by and Future Design Recommendations for Direct-to-Consumer Health Care Artificial Intelligence Apps: Scoping Review. J. Med. Internet Res. 2023, 25, e50342. [Google Scholar] [CrossRef]
- Peltonen, L.M.; Topaz, M. Artificial intelligence in health care: Implications for nurse managers. J. Nurs. Manag. 2022, 30, 3641–3643. [Google Scholar] [CrossRef]
- Jauk, S.; Kramer, D.; Quehenberger, F.; Veeranki, S.P.K.; Hayn, D.; Schreier, G.; Leodolter, W. Information Adapted Machine Learning Models for Prediction in Clinical Workflow. Stud. Health Technol. Inform. 2019, 260, 65–72. [Google Scholar]
- Yoshimi, T.; Kato, K.; Aimoto, K.; Kondo, I. Robotic Care Equipment Improves Communication between Care Recipient and Caregiver in a Nursing Home as Revealed by Gaze Analysis: A Case Study. Int. J. Environ. Res. Public Health 2024, 21, 250. [Google Scholar] [CrossRef]
- Nashwan, A.J.; Abujaber, A.A. Nursing in the Artificial Intelligence (AI) Era: Optimizing Staffing for Tomorrow. Cureus 2023, 15, e47275. [Google Scholar] [CrossRef]
- Schäfer, F.; Walther, M.; Grimm, D.G.; Hübner, A. Combining machine learning and optimization for the operational patient-bed assignment problem. Health Care Manag. Sci. 2023, 26, 785–806. [Google Scholar] [CrossRef]
- Johnson, E.A.; Dudding, K.M.; Carrington, J.M. When to err is inhuman: An examination of the influence of artificial intelligence-driven nursing care on patient safety. Nurs. Inq. 2024, 31, e12583. [Google Scholar] [CrossRef]
- Topol, E.J. High-performance medicine: The convergence of human and artificial intelligence. Nat. Med. 2019, 25, 44–56. [Google Scholar] [CrossRef]
- Watson, A.L. Ethical considerations for artificial intelligence use in nursing informatics. Nurs. Ethics 2024. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, O.M.P.L.; Vicente, C.M.F.B.; Martins, M.M.F.P.S.; Vandresen, L.; Silva, J.M.A.V. Instruments for assessing professional nursing practice environments: An integrative review. Rev. Gaucha Enferm. 2020, 41, e20190381. [Google Scholar] [CrossRef] [PubMed]
- Meskó, B.; Hetényi, G.; Győrffy, Z. Will artificial intelligence solve the human resource crisis in healthcare? BMC Health Serv. Res. 2018, 18, 545. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).