Bibliometric Review of the Knowledge Base on Healthcare Management for Sustainability, 1994–2018
Abstract
:1. Introduction
- RQ1: What are key growth trends in research on healthcare management for sustainability?
- RQ2: What authors and documents in the literature on sustainable healthcare management have had the greatest impact on citations over the past 25 years?
- RQ3: What is the intellectual structure of the knowledge base on sustainable healthcare management?
- RQ4: What topics in the sustainable healthcare management literature have been studied with the greatest frequency and are currently attracting the greatest attention?
2. Background Literature
3. Methodology
3.1. Identifying Sources for the Review
3.2. Data Analysis
4. Results
4.1. Descriptive Trends in the SHM Literature
4.2. Analysis of Influential Authors and Documents
4.3. Intellectual Structure of the Healthcare Management Knowledge Base
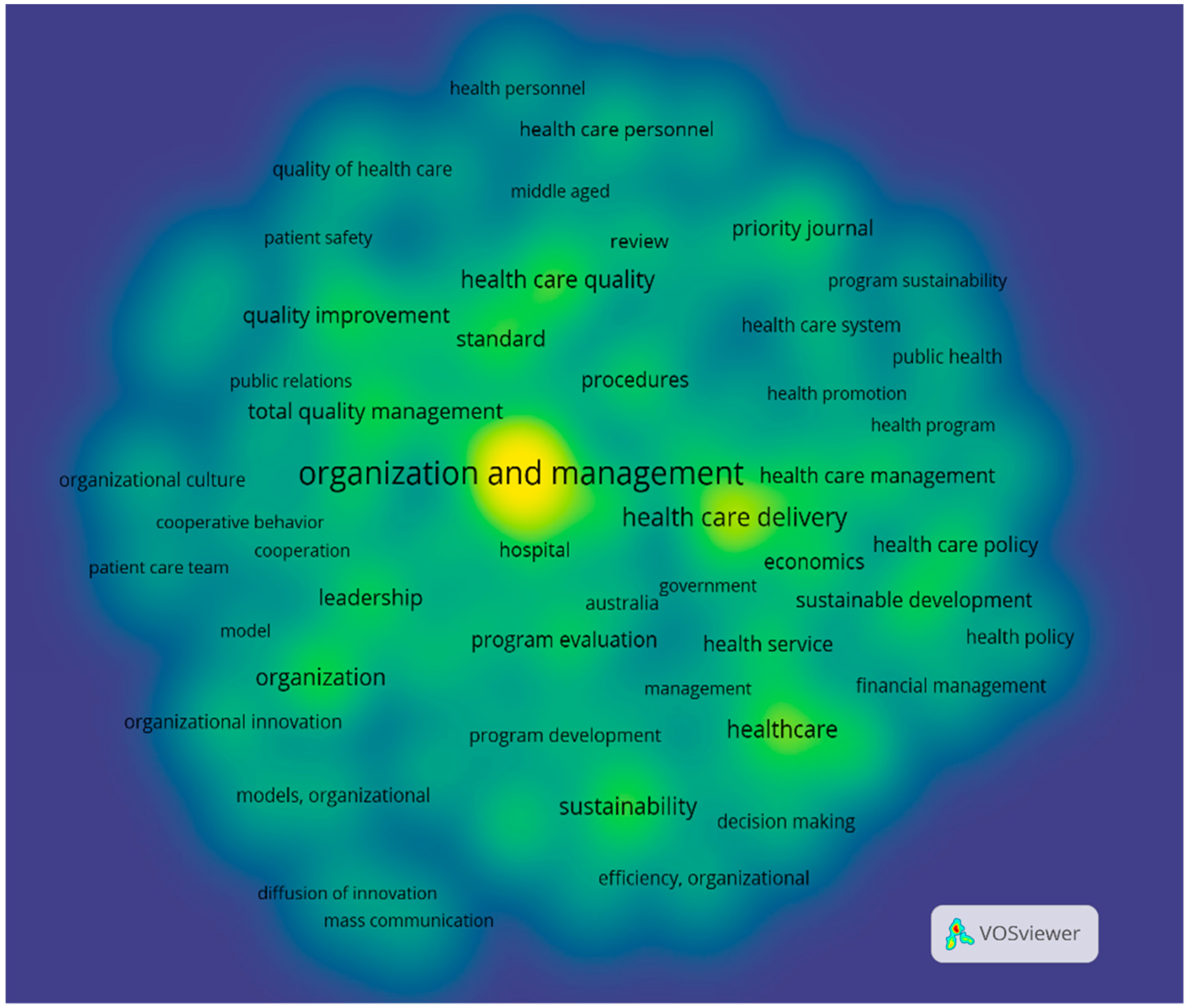
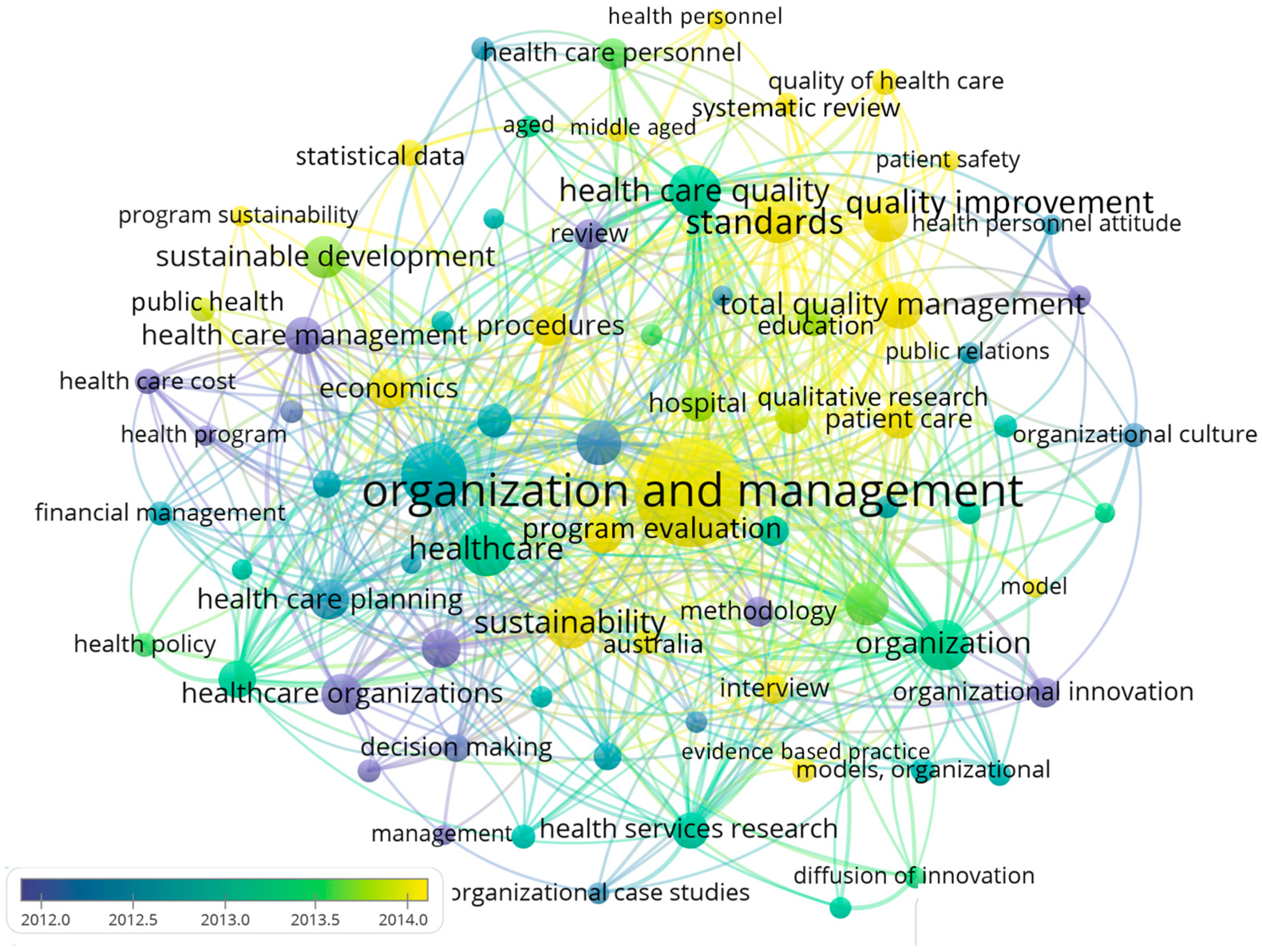
4.4. Topical Foci of the Healthcare Management for Sustainability Knowledge Base
5. Discussion
5.1. Limitations
5.2. Conclusion and Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Khandakar, S.; Saad Andaleeb, S.; Siddiqui, N. Doctors’ service orientation in public, private, and foreign hospitals. Int. J. Health Care Qual. Assur. 2007, 20, 253–263. [Google Scholar]
- Greenhalgh, T.; Macfarlane, F.; Barton-Sweeney, C.; Woodard, F. “If We Build It, Will It Stay?” A Case Study of the Sustainability of Whole-System Change in London. Milbank Q. 2012, 90, 516–547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ament, S.M.C.; Gillissen, F.; Maessen, J.M.C.; Dirksen, C.D.; van der Weijden, T.; von Meyenfeldt, M.F. Sustainability of healthcare innovations (SUSHI): Long term effects of two implemented surgical care programmes (protocol). BMC Health Serv. Res. 2012, 12, 423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goh, C.Y.; Marimuthu, M. The Path towards Healthcare Sustainability: The Role of Organisational Commitment. Procedia Soc. Behav. Sci. 2016, 224, 587–592. [Google Scholar] [CrossRef] [Green Version]
- Ramirez, B.; West, D.J.; Costell, M.M. Development of a culture of sustainability in health care organizations. J. Health Organ. Manag. 2013, 27, 665–672. [Google Scholar] [CrossRef] [PubMed]
- GGHC—Tools: Green Guide for Health Care Version 2.2: Overview. Available online: https://www.gghc.org/tools.2.2overview.php (accessed on 9 June 2019).
- Dpicampaigns. About the Sustainable Development Goals. Available online: https://www.un.org/sustainabledevelopment/sustainable-development-goals/ (accessed on 9 June 2019).
- SDGs: Sustainable Development Knowledge Platform. Available online: https://sustainabledevelopment.un.org/sdgs (accessed on 9 June 2019).
- Ramirez, B.; Oetjen, R.M.; Malvey, D. Sustainability and the health care manager: Part I. Health Care Manag. 2011, 30, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, B.; Oetjen, R.M.; Malvey, D. Sustainability and the health care manager: Part II. Health Care Manag. 2011, 30, 261–265. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Robert, G.; Macfarlane, F.; Bate, P.; Kyriakidou, O. Diffusion of innovations in service organizations: Systematic review and recommendations. Milbank Q. 2004, 82, 581–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gruen, R.L.; Elliott, J.H.; Nolan, M.L.; Lawton, P.D.; Parkhill, A.; McLaren, C.J.; Lavis, J.N. Sustainability science: An integrated approach for health-programme planning. Lancet Lond. Engl. 2008, 372, 1579–1589. [Google Scholar] [CrossRef] [Green Version]
- Scheirer, M.A. Is Sustainability Possible? A Review and Commentary on Empirical Studies of Program Sustainability. Am. J. Eval. 2005, 26, 320–347. [Google Scholar] [CrossRef] [Green Version]
- Zupic, I.; Čater, T. Bibliometric Methods in Management and Organization. Organ. Res. Methods 2015, 18, 429–472. [Google Scholar] [CrossRef]
- Nerur, S.P.; Rasheed, A.A.; Natarajan, V. The intellectual structure of the strategic management field: An author co-citation analysis. Strateg. Manag. J. 2008, 29, 319–336. [Google Scholar] [CrossRef]
- White, H.D.; McCain, K.W. Visualizing a discipline: An author co-citation analysis of information science, 1972–1995. J. Am. Soc. Inf. Sci. 1998, 49, 327–355. [Google Scholar]
- Sheth, A.; Price, A.D.F.; Glass, J.; Achour, N. Reviewing the sustainability of existing healthcare facilities. In Proceedings of the 23rd Annual Conference of Association of Researchers in Construction Management (ARCOM), Cardiff, UK, 3–5 September 2008; pp. 1193–1202. [Google Scholar]
- Chauhan, A.; Singh, A. Healthcare waste management: A state-of-the-art literature review. Int. J. Environ. Waste Manag. 2016, 18, 120–144. [Google Scholar] [CrossRef]
- Nichols, A. Sustainable Practice and Behaviour change in Healthcare Waste Management: A Review of the Literature. In Proceedings of the 1st World Sustainability Forum, Basel, Switzerland, 1–30 November 2011; p. 551. [Google Scholar]
- Proctor, E.; Luke, D.; Calhoun, A.; McMillen, C.; Brownson, R.; McCrary, S.; Padek, M. Sustainability of evidence-based healthcare: Research agenda, methodological advances, and infrastructure support. Implement. Sci. 2015, 10, 88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vest, J.R.; Gamm, L.D. A critical review of the research literature on Six Sigma, Lean and StuderGroup’s Hardwiring Excellence in the United States: The need to demonstrate and communicate the effectiveness of transformation strategies in healthcare. Implement. Sci. 2009, 4, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Andreamatteo, A.; Ianni, L.; Lega, F.; Sargiacomo, M. Lean in healthcare: A comprehensive review. Health Policy 2015, 119, 1197–1209. [Google Scholar] [CrossRef]
- Anuar, A.; Saad, R.; Yusoff, R.Z. Sustainability through lean healthcare and operational performance in the private hospitals: A proposed framework. Int. J. Supply Chain Manag. 2018, 7, 221–227. [Google Scholar]
- Leape, L.L.; Berwick, D.; Clancy, C.; Conway, J.; Gluck, P.; Guest, J.; Lawrence, D.; Morath, J.; O’Leary, D.; O’Neill, P.; et al. Transforming healthcare: A safety imperative. BMJ Qual. Saf. 2009, 18, 424–428. [Google Scholar] [CrossRef]
- Shediac-Rizkallah, M.C.; Bone, L.R. Planning for the sustainability of community-based health programs: Conceptual frameworks and future directions for research, practice and policy. Health Educ. Res. 1998, 13, 87–108. [Google Scholar] [CrossRef] [Green Version]
- Pinzone, M.; Lettieri, E.; Masella, C. Sustainability in healthcare: Combining organizational and architectural levers. Int. J. Eng. Bus. Manag. 2012, 4, 38. [Google Scholar] [CrossRef] [Green Version]
- Rich, C.R.; Singleton, J.K.; Wadhwa, S.S. Sustainability for Healthcare Management: A Leadership Imperative; Routledge: London, UK, 2018. [Google Scholar]
- Robinson, S.; Williams, I.; Dickinson, H.; Freeman, T.; Rumbold, B. Priority-setting and rationing in healthcare: Evidence from the English experience. Soc. Sci. Med. 2012, 75, 2386–2393. [Google Scholar] [CrossRef] [PubMed]
- Robinson, S.; Williams, I.; Spence, K.; Daniels, T. Tackling disinvestment in health care services: The views of resource allocators in the English NHS. J. Health Organ. Manag. 2013, 27, 762–780. [Google Scholar]
- Pasqualine, A.; Plytiuk, C.F.; da Costa, S.E.G.; de Lima, E.P. Performance Management in Healthcare: A bibliometric review. In Proceedings of the Institute of Industrial and Systems Engineers (IISE), Orlanda, FL, USA, 19–23 May 2012; p. 1. [Google Scholar]
- Bradea, I.; Delcea, C.; Paun, R. Healthcare Risk Management Analysis—A Bibliometric Approach. J. East. Eur. Res. Bus. Econ. 2015, 2015, 1–11. [Google Scholar] [CrossRef]
- Koseoglu, M.A.; Akdeve, E.; Gedik, İ.; Bertsch, A. A bibliometric analysis of strategic management articles in healthcare management literature: Past, present, and future. Int. J. Healthc. Manag. 2015, 8, 27–33. [Google Scholar] [CrossRef]
- Adunlin, G.; Diaby, V.; Xiao, H. Application of multicriteria decision analysis in health care: A systematic review and bibliometric analysis. Health Expect. 2015, 18, 1894–1905. [Google Scholar] [CrossRef] [Green Version]
- Mongeon, P.; Paul-Hus, A. The journal coverage of Web of Science and Scopus: A comparative analysis. Scientometrics 2016, 106, 213–228. [Google Scholar] [CrossRef]
- Hallinger, P.; Kovačević, J. A Bibliometric Review of Research on Educational Administration: Science Mapping the Literature, 1960 to 2018. Rev. Educ. Res. 2019, 89, 335–369. [Google Scholar] [CrossRef]
- Archambault, É.; Campbell, D.; Gingras, Y.; Larivière, V. Comparing bibliometric statistics obtained from the Web of Science and Scopus. J. Am. Soc. Inf. Sci. Technol. 2009, 60, 1320–1326. [Google Scholar] [CrossRef]
- Falagas, M.E.; Pitsouni, E.I.; Malietzis, G.A.; Pappas, G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: Strengths and weaknesses. FASEB J. 2008, 22, 338–342. [Google Scholar] [CrossRef]
- Moher, D. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Small, H. Visualizing science by citation mapping. J. Am. Soc. Inf. Sci. 1999, 50, 799–813. [Google Scholar] [CrossRef]
- van Eck, N.J.; Waltman, L. Citation-based clustering of publications using CitNetExplorer and VOSviewer. Scientometrics 2017, 111, 1053–1070. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franche, R.-L.; Cullen, K.; Clarke, J.; Irvin, E.; Sinclair, S.; Frank, J.; Cole, D.; Dacombe, J.; Guzman, J.; Hogg-Johnson, S.; et al. Workplace-based return-to-work interventions: A systematic review of the quantitative literature. J. Occup. Rehabil. 2005, 15, 607–631. [Google Scholar] [CrossRef] [PubMed]
- Wiltsey Stirman, S.; Kimberly, J.; Cook, N.; Calloway, A.; Castro, F.; Charns, M. The sustainability of new programs and innovations: A review of the empirical literature and recommendations for future research. Implement. Sci. 2012, 7, 17. [Google Scholar] [CrossRef] [Green Version]
- Légaré, F.; Ratté, S.; Stacey, D.; Kryworuchko, J.; Gravel, K.; Graham, I.D.; Turcotte, S. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst. Rev. Online 2010, 5, CD006732. [Google Scholar]
- Cunningham, F.C.; Ranmuthugala, G.; Plumb, J.; Georgiou, A.; Westbrook, J.I.; Braithwaite, J. Health professional networks as a vector for improving healthcare quality and safety: A systematic review. BMJ Qual. Saf. 2012, 21, 239–249. [Google Scholar] [CrossRef] [Green Version]
- Jordan, J.E.; Briggs, A.M.; Brand, C.A.; Osborne, R.H. Enhancing patient engagement in chronic disease self-management support initiatives in Australia: The need for an integrated approach. Med. J. Aust. 2008, 189, S9–S13. [Google Scholar] [CrossRef] [Green Version]
- Huryk, L.A. Factors influencing nurses’ attitudes towards healthcare information technology. J. Nurs. Manag. 2010, 18, 606–612. [Google Scholar] [CrossRef]
- Lee, H.; Cummings, G.G. Factors influencing job satisfaction of front line nurse managers: A systematic review. J. Nurs. Manag. 2008, 16, 768–783. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Berry, L.L.; Quan, X.; Parish, J.T. A conceptual framework for the domain of evidence-based design. Health Environ. Res. Des. J. 2011, 4, 95–114. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Robert, G.; Bate, P.; Macfarlane, F.; Kyriakidou, O. Diffusion of Innovations in Health Service Organisations: A Systematic Literature Review; John Wiley & Sons: New York, NY, USA, 2008. [Google Scholar]
- Greenhalgh, T.; Robert, G.; MacFarlane, F.; Bate, P.; Kyriakidou, O.; Peacock, R. Storylines of research in diffusion of innovation: A meta-narrative approach to systematic review. Soc. Sci. Med. 2005, 61, 417–430. [Google Scholar] [CrossRef] [PubMed]
- Robert, G.; Morrow, E.; Maben, J.; Griffiths, P.; Callard, L. The adoption, local implementation and assimilation into routine nursing practice of a national quality improvement programme: The Productive Ward in England. J. Clin. Nurs. 2011, 20, 1196–1207. [Google Scholar] [CrossRef] [PubMed]
- Staines, A.; Thor, J.; Robert, G. Sustaining improvement? The 20-year jönköping quality improvement program revisited. Qual. Manag. Health Care 2015, 24, 21–37. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Robert, G.; Bate, P.; Macfarlane, F.; Kyriakidou, O. Diffusion of Innovations in Health Service Organisations: A Systematic Literature Review; John Wiley & Sons: New York, NY, USA, 2008. [Google Scholar]
- Wong, G.; Greenhalgh, T.; Westhorp, G.; Pawson, R. Realist methods in medical education research: What are they and what can they contribute? Med. Educ. 2012, 46, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Best, A.; Greenhalgh, T.; Lewis, S.; Saul, J.E.; Carroll, S.; Bitz, J. Large-system transformation in health care: A realist review. Milbank Q. 2012, 90, 421–456. [Google Scholar] [CrossRef] [Green Version]
- Fraser, S.W.; Greenhalgh, T. Complexity science: Coping with complexity: Educating for capability. Br. Med. J. 2001, 323, 799–803. [Google Scholar] [CrossRef]
- Radnor, Z.J.; Holweg, M.; Waring, J. Lean in healthcare: The unfilled promise? Soc. Sci. Med. 2012, 74, 364–371. [Google Scholar] [CrossRef] [Green Version]
- Braithwaite, J.; Marks, D.; Taylor, N. Harnessing implementation science to improve care quality and patient safety: A systematic review of targeted literature. Int. J. Qual. Health Care 2014, 26, 321–329. [Google Scholar] [CrossRef]
- Braithwaite, J.; Testa, L.; Lamprell, G.; Herkes, J.; Ludlow, K.; McPherson, E.; Campbell, M.; Holt, J. Built to last? The sustainability of health system improvements, interventions and change strategies: A study protocol for a systematic review. BMJ Open 2017, 7, e018568. [Google Scholar] [CrossRef] [Green Version]
- Braithwaite, J.; Mannion, R.; Matsuyama, Y.; Shekelle, P.G.; Whittaker, S.; Al-Adawi, S.; Ludlow, K.; James, W.; Ting, H.P.; Herkes, J.; et al. The future of health systems to 2030: A roadmap for global progress and sustainability. Int. J. Qual. Health Care 2018, 30, 823–831. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Gray, L.C. Telemedicine across the ages. Med. J. Aust. 2009, 190, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Scuffham, P.; Wootton, R. The costs and potential savings of a novel telepaediatric service in Queensland. BMC Health Serv. Res. 2007, 7, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grimshaw, J.M.; Eccles, M.P. Is evidence-based implementation of evidence-based care possible? Med. J. Aust. 2004, 180, S50–S51. [Google Scholar] [CrossRef] [PubMed]
- Grol, R.; Grimshaw, J. From best evidence to best practice: Effective implementation of change in patients’ care. Lancet 2003, 362, 1225–1230. [Google Scholar] [CrossRef]
- Grol, R.; Grimshaw, J. Evidence-based implementation of evidence-based medicine. Jt. Comm. J. Qual. Improv. 1999, 25, 503–513. [Google Scholar] [CrossRef]
- Grimshaw, J.M.; Thomas, R.E.; MacLennan, G.; Fraser, C.; Ramsay, C.R.; Vale, L.; Whitty, P.; Eccles, M.P.; Matowe, L.; Shirran, L.; et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Int. J. Technol. Assess. Health Care 2005, 21, 149. [Google Scholar] [CrossRef] [Green Version]
- Bate, P.; Robert, G.; Bevan, H. The next phase of healthcare improvement: What can we learn from social movements? BMJ Qual. Saf. 2004, 13, 62–66. [Google Scholar] [CrossRef] [Green Version]
- Scheirer, M.A. Linking sustainability research to intervention types. Am. J. Public Health 2013, 103, e73–e80. [Google Scholar] [CrossRef]
- Scheirer, M.A.; Dearing, J.W. An agenda for research on the sustainability of Public Health Programs. Am. J. Public Health 2011, 101, 2059–2067. [Google Scholar] [CrossRef]
- Harris, C.; Green, S.; Ramsey, W.; Allen, K.; King, R. Sustainability in Health care by allocating resources effectively (SHARE) 1: Introducing a series of papers reporting an investigation of disinvestment in a local healthcare setting. BMC Health Serv. Res. 2017, 17, 323. [Google Scholar] [CrossRef] [PubMed]
- Harris, C.; Garrubba, M.; Allen, K.; King, R.; Kelly, C.; Thiagarajan, M.; Castleman, B.; Ramsey, W.; Farjou, D. Development, implementation and evaluation of an evidence-based program for introduction of new health technologies and clinical practices in a local healthcare setting. BMC Health Serv. Res. 2015, 15, 575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, C.; Allen, K.; Brooke, V.; Dyer, T.; Waller, C.; King, R.; Ramsey, W.; Mortimer, D. Sustainability in Health care by Allocating Resources Effectively (SHARE) 6: Investigating methods to identify, prioritise, implement and evaluate disinvestment projects in a local healthcare setting. BMC Health Serv. Res. 2017, 17, 370. [Google Scholar] [CrossRef] [PubMed]
- Harris, C.; Garrubba, M.; Melder, A.; Voutier, C.; Waller, C.; King, R.; Ramsey, W. Sustainability in Health care by Allocating Resources Effectively (SHARE) 8: Developing, implementing and evaluating an evidence dissemination service in a local healthcare setting. BMC Health Serv. Res. 2018, 18, 151. [Google Scholar] [CrossRef] [PubMed]
- Harris, C.; Green, S.; Elshaug, A.G. Sustainability in Health care by Allocating Resources Effectively (SHARE) 10: Operationalising disinvestment in a conceptual framework for resource allocation. BMC Health Serv. Res. 2017, 17, 632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, C.; Green, S.; Ramsey, W.; Allen, K.; King, R. Sustainability in Health care by Allocating Resources Effectively (SHARE) 9: Conceptualising disinvestment in the local healthcare setting. BMC Health Serv. Res. 2017, 17, 633. [Google Scholar] [CrossRef] [Green Version]
- Harris, C.; Allen, K.; Waller, C.; Dyer, T.; Brooke, V.; Garrubba, M.; Melder, A.; Voutier, C.; Gust, A.; Farjou, D. Sustainability in Health care by Allocating Resources Effectively (SHARE) 7: Supporting staff in evidence-based decision-making, implementation and evaluation in a local healthcare setting. BMC Health Serv. Res. 2017, 17, 430. [Google Scholar] [CrossRef]
- Harris, C.; Allen, K.; Ramsey, W.; King, R.; Green, S. Sustainability in Health care by Allocating Resources Effectively (SHARE) 11: Reporting outcomes of an evidence-driven approach to disinvestment in a local healthcare setting Milena Pavlova. BMC Health Serv. Res. 2018, 18, 386. [Google Scholar] [CrossRef] [Green Version]
- Polisena, J.; Clifford, T.; Elshaug, A.G.; Mitton, C.; Russell, E.; Skidmore, B. Case studies that illustrate disinvestment and resource allocation decision-making processes in health care: A systematic review. Int. J. Technol. Assess. Health Care 2013, 29, 174–184. [Google Scholar] [CrossRef]
- Elshaug, A.G.; Watt, A.M.; Mundy, L.; Willis, C.D. Over 150 potentially low-value health care practices: An Australian study. Med. J. Aust. 2012, 197, 556–560. [Google Scholar] [CrossRef] [Green Version]
- Elshaug, A.G.; Moss, J.R.; Littlejohns, P.; Karnon, J.; Merlin, T.L.; Hiller, J.E. Identifying existing health care services that do not provide value for money. Med. J. Aust. 2009, 190, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Mitton, C.; Donaldson, C. Health care priority setting: Principles, practice and challenges. Cost Eff. Resour. Alloc. 2004, 2, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, C.; Allen, K.; Waller, C.; Brooke, V. Sustainability in health care by allocating resources effectively (SHARE) 3: Examining how resource allocation decisions are made, implemented and evaluated in a local healthcare setting. BMC Health Serv. Res. 2017, 17, 340. [Google Scholar] [CrossRef] [PubMed]
- Harris, C.; Allen, K.; King, R.; Ramsey, W.; Kelly, C.; Thiagarajan, M. Sustainability in Health care by Allocating Resources Effectively (SHARE) 2: Identifying opportunities for disinvestment in a local healthcare setting. BMC Health Serv. Res. 2017, 17, 328. [Google Scholar] [CrossRef] [PubMed]
- Harris, C.; Ko, H.; Waller, C.; Sloss, P.; Williams, P. Sustainability in Health care by Allocating Resources Effectively (SHARE) 4: Exploring opportunities and methods for consumer engagement in resource allocation in a local healthcare setting. BMC Health Serv. Res. 2017, 17, 329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salem, M.A.; Shawtari, F.A.; Shamsudin, M.F.; Hussain, H.I. The relation between stakeholders’ integration and environmental competitiveness. Soc. Responsib. J. 2016, 12, 755–769. [Google Scholar] [CrossRef]
- Hussain, M.; Ajmal, M.M.; Gunasekaran, A.; Khan, M. Exploration of social sustainability in healthcare supply chain. J. Clean. Prod. 2018, 203, 977–989. [Google Scholar] [CrossRef]
- Lee, Y.-M.; Hu, J.-L. Integrated Approaches for Business Sustainability: The Perspective of Corporate Social Responsibility. Sustainability 2018, 10, 2318. [Google Scholar] [CrossRef] [Green Version]
- Ray, S.; Chaudhuri, B.R. Business Group Affiliation and Corporate Sustainability Strategies of Firms: An Investigation of Firms in India. J. Bus. Ethics 2018, 153, 955–976. [Google Scholar] [CrossRef]
- Lo, H.-W.; Liou, J.J.H.; Wang, H.-S.; Tsai, Y.-S. An integrated model for solving problems in green supplier selection and order allocation. J. Clean. Prod. 2018, 190, 339–352. [Google Scholar] [CrossRef]
- Chen, C.-C.; Shih, H.-S.; Shyur, H.-J.; Wu, K.-S. A business strategy selection of green supply chain management via an analytic network process. Comput. Math. Appl. 2012, 64, 2544–2557. [Google Scholar] [CrossRef] [Green Version]
- Piboolsravut, P. Sufficiency Economy. ASEAN Econ. Bull. 2004, 21, 127–134. [Google Scholar] [CrossRef]
- Hovlid, E.; Bukve, O.; Haug, K.; Aslaksen, A.B.; Von Plessen, C. Sustainability of healthcare improvement: What can we learn from learning theory? BMC Health Serv. Res. 2012, 12, 235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haas, M.; Hall, J.; Viney, R.; Gallego, G. Breaking up is hard to do: Why disinvestment in medical technology is harder than investment. Aust. Health Rev. Publ. Aust. Hosp. Assoc. 2012, 36, 148–152. [Google Scholar] [CrossRef] [PubMed]




| Author | Nation | Docu-Ments 1 | Scopus Citations | Citations Per Document | Scopus h-Index | Focus |
|---|---|---|---|---|---|---|
| Braithwaite J. | Australia | 5 | 163 | 32.6 | 41 | Health Care Quality |
| Ritchie J.A. | Canada | 4 | 107 | 26.8 | 24 | Health Care Innovation |
| Harris C. | Australia | 7 | 68 | 9.7 | 8 | Health Care Policy |
| Tudor T.L. | UK | 3 | 65 | 21.7 | 13” | Environmental Science |
| Denis J.L. | Canada | 3 | 57 | 19.0 | 31 | Health Care Innovation |
| Fleiszer A.R. | Canada | 3 | 57 | 19.0 | 8 | Health Care Innovation |
| Richer M.C. | Canada | 3 | 57 | 19.0 | 13 | Health Care Innovation |
| Semenic S.E. | Canada | 3 | 57 | 19.0 | 13 | Health Care Innovation |
| Allen K. | Australia | 5 | 50 | 10.0 | 11 | Health Care Policy |
| Lettieri E. | Italy | 3 | 44 | 14.7 | 14 | Health Care Management |
| King R. | Australia | 4 | 40 | 10.0 | 6 | Health Care Policy |
| Ramsey W. | Australia | 4 | 40 | 10.0 | 6 | Health Care Policy |
| Mazzocato P. | Sweden | 3 | 39 | 13.0 | 7 | Health Care Management |
| Waller C. | Australia | 4 | 38 | 9.5 | 6 | Health Care Policy |
| Garrubba M. | Australia | 3 | 30 | 10.0 | 5 | Health Care Policy |
| Brooke V. | Australia | 3 | 29 | 9.7 | 3 | Health Care Policy |
| Diallo M.S. | Korea | 3 | 28 | 9.3 | 26 | Environmental Science |
| Fromer N.A. | USA | 3 | 28 | 9.3 | 12 | Environmental Science |
| Jhon M.S. | USA | 3 | 28 | 9.3 | 51 | Environmental Science |
| Roca J. | Spain | 3 | 21 | 7.0 | 70 | Health Care Management |
| Rank | Author | Document | Focus | Scopus Cites | Type of Paper |
|---|---|---|---|---|---|
| 1 | Franche et al. (2005) | Workplace-based return-to-work interventions. [41] | Change | 415 | Rev |
| 2 | Wiltsey Stirman et al. (2012) | The sustainability of new programs and innovations. [42] | Change | 372 | Rev |
| 3 | Légaré et al. (2010) | Interventions for improving the adoption of shared decision making by health care professionals. [43] | Social | 277 | Rev |
| 4 | Vest & Gamm (2009) | A critical review of the research literature on Six Sigma, Lean and Studer Group’s Hardwiring Excellence in the U.S. [21] | Economic | 129 | Rev |
| 5 | D’Andreamatteo et al. (2015) | Lean in health care: A comprehensive review. [22] | Economic | 114 | Rev |
| 6 | Cunningham et al. (2012) | Health professional networks as a vector for improving health care quality and safety: A systematic review. [44] | Social | 107 | Rev |
| 7 | Jordan et al. (2008) | Enhancing patient engagement in chronic disease self-management support initiatives in Australia. [45] | Social | 94 | Con |
| 8 | Huryk (2010) | Factors influencing nurses’ attitudes towards health care information technology. [46] | Change | 90 | Rev |
| 9 | Lee & Cummings (2008) | Factors influencing job satisfaction of front line nurse managers [47] | Change | 88 | Rev |
| 10 | Ulrich et al. (2011) | A conceptual framework for the domain of evidence-based design. [48] | Economic | 88 | Con |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Punnakitikashem, P.; Hallinger, P. Bibliometric Review of the Knowledge Base on Healthcare Management for Sustainability, 1994–2018. Sustainability 2020, 12, 205. https://doi.org/10.3390/su12010205
Punnakitikashem P, Hallinger P. Bibliometric Review of the Knowledge Base on Healthcare Management for Sustainability, 1994–2018. Sustainability. 2020; 12(1):205. https://doi.org/10.3390/su12010205
Chicago/Turabian StylePunnakitikashem, Prattana, and Philip Hallinger. 2020. "Bibliometric Review of the Knowledge Base on Healthcare Management for Sustainability, 1994–2018" Sustainability 12, no. 1: 205. https://doi.org/10.3390/su12010205





