Using Visualization to Build Transparency in a Healthcare Blockchain Application
Abstract
:1. Introduction
2. Background
2.1. Blockchain in Healthcare
2.2. Increasing Trust through Visibility
3. The Proposed Methodology: A Blockchain-Based Solution
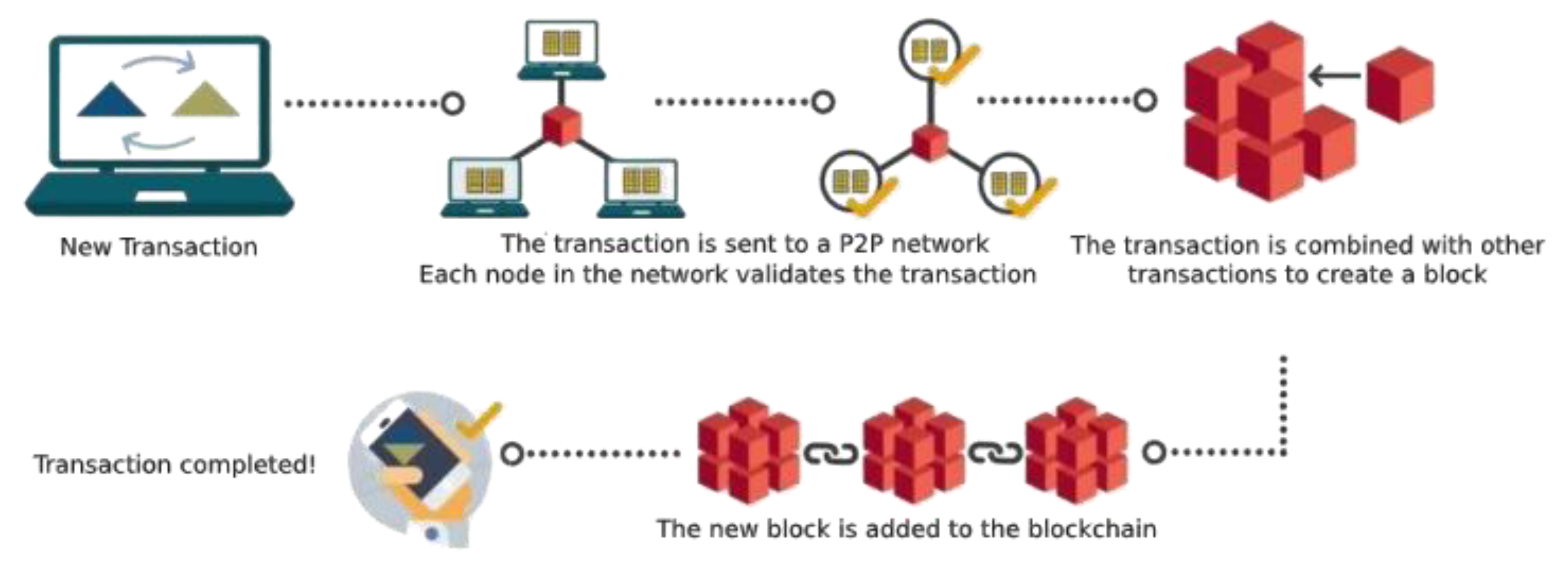
- (1)
- Create the blockchain with the different network nodes, where each node corresponds to different users who will participate in data sharing. In our case study the nodes correspond to patients who decide to share their files as well as the buyers of information from these files.
- (2)
- Manage the transactions generated by different nodes. Here, we will focus on authentication, file transfer, and visualization. These transactions are combined with other transactions to create a new block.
- (3)
- Configure and customize the information to be visualized after choosing a tool for the network visualization.
- (4)
- Connect or integrate the blockchain with the visualization tool.
- (5)
- Demonstrate the visualization of how nodes are interacting during a transaction.
4. Case Study
Processes for Uploading and Accessing Health Data
5. Implementation
5.1. Blockchain Creation
5.2. Transaction Management: Patient Permission, File Transmission and Block Creation
5.3. File Reception
5.4. Visualization Configuration and Connection with the Blockchain Network
5.4.1. Installation and Configuration
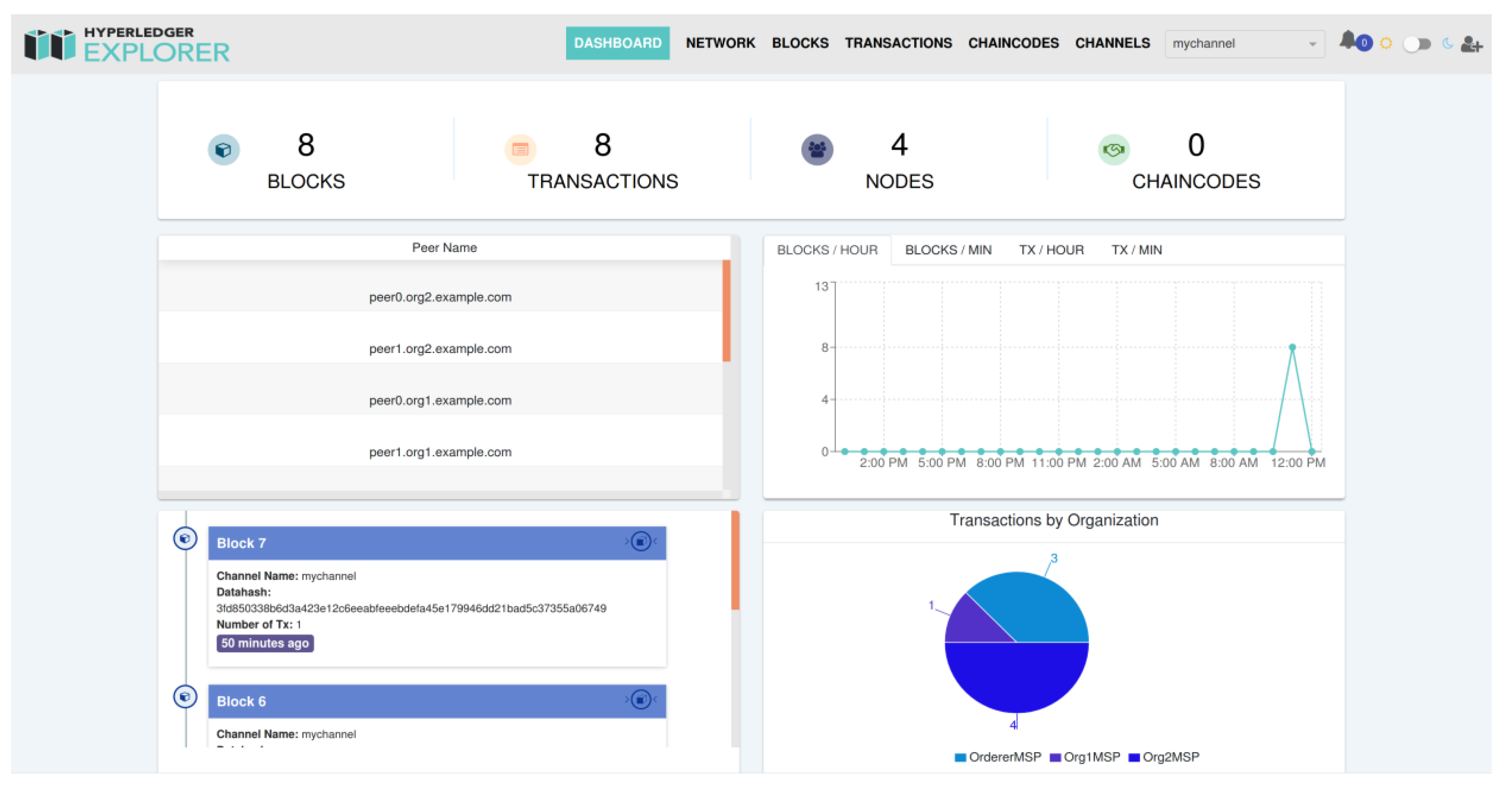
5.4.2. Visualization
- Channel Name: The name of the channel through which the block has been created. A channel is a mechanism by which a set of components of a blockchain network interact and exchange information. They provide privacy to the network. There can be different channels, and users can access one or another, depending on how their permissions are configured.
- Datahash: This is an encrypted code that contains all the information of the block. Here, you can find information about the sender of the file, the receiver of the file, and the file itself.
- Number of Tx: This represents the number of transactions per block.
5.5. User Study
6. Discussion
6.1. Future Research Directions
6.2. Limitations
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A. Screenshots of Terminal Windows






References
- Aghina, W.; De Smet, A.; Weerda, K. Agility: It rhymes with stability. McKinsey Quarterly. December 2015. Available online: https://www.mckinsey.com/business-functions/organization/our-insights/agility-it-rhymes-with-stability (accessed on 6 June 2020).
- Bossert, O.; Laartz, J.; Ramsey, T.J. Running your company at two speeds. McKinsey Quarterly. December 2014. Available online: https://www.mckinsey.com/business-functions/mckinsey-digital/our-insights/running-your-company-at-two-speeds (accessed on 6 June 2020).
- Lusch, R.F.; Nambisan, S. Service Innovation: A Service-Dominant Logic Perspective. MIS Quart. 2015, 39, 155–175. [Google Scholar]
- Tanniru, M.; Khuntia, J.; Weiner, J. Hospital Leadership in Support of Digital Transformation. Pac. Asia J. Assoc. Inf. Syst. 2018, 10, 1–24. [Google Scholar] [CrossRef] [Green Version]
- Vargo, S.L.; Lusch, R.F. Service-Dominant Logic: What it is, What it is not, What it might be. In The Service-Dominant Logic of Marketing: Dialog, Debate, and Directions; Vargo, S.L., Lusch, R.F., Eds.; M.E. Sharpe: Armonk, NY, USA, 2006; pp. 43–55. [Google Scholar]
- Nuckols, T.K.; Fingar, K.R.; Barrett, M.; Steiner, C.A.; Stocks, C.; Owens, P.L. The shifting landscape in utilization of inpatient, observation, and emergency department services across payers. J. Hosp. Med. 2017, 12, 443–446. [Google Scholar] [CrossRef] [Green Version]
- Sanborn, B.J. Outpatient shift, digitization, shortages, and telehealth will shape healthcare systems of tomorrow. Healthcare Finance. May 2018. Available online: https://www.healthcarefinancenews.com/news/outpatient-shift-digitization-shortages-and-telehealth-will-shape-healthcare-systems-tomorrow (accessed on 6 June 2020).
- Tanniru, M.; Sandhu, K. Engagement leading to empowerment-Digital Innovation Strategies for Patient Care Continuity. In Proceedings of the Australasian Conference on Information Systems, Sydney, Australia, January 2018; Available online: https://aisel.aisnet.org/cgi/viewcontent.cgi?article=1039&context=acis2018 (accessed on 6 June 2020).
- Johnston, L.; Zemanek, J.; Reeve, M.J.; Grills, N. The evidence for using mHealth technologies for diabetes management in low- and middle-income countries. J. Hosp. Manag. Health Policy 2018, 2. Available online: http://jhmhp.amegroups.com/article/view/4403/5182 (accessed on 6 June 2020).
- Agarwal, R.; Gao, G.; DesRoches, C.M.; Jha, A.K. Research Commentary—The Digital Transformation of Healthcare: Current Status and the Road Ahead. Inform. Syst. Res. 2010, 21, 796–809. [Google Scholar] [CrossRef] [Green Version]
- Ghosh, K.; Khuntia, J.; Chawla, S.; Deng, X. Media Reinforcement for Psychological Empowerment in Chronic Disease Management. Commun. Assoc. Inf. Syst. 2014, 34, 419–438. [Google Scholar] [CrossRef]
- Tanniru, M. Transforming public health using value lens and extended partner networks. Learn. Health Syst. 2020. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/lrh2.10234 (accessed on 6 June 2020).
- Dowell, D.; Haegerich, T.; Chou, R. No Shortcuts to Safer Opioid Prescribing. N. Engl. J. Med. 2019, 380, 2285–2287. [Google Scholar] [CrossRef]
- Rahman, A.; Rashid, M.; Kernec, J.L.; Phillippe, B.; Barnes, S.J.; Fioranell, F.; Yang, S.; Romain, O.; Abbasi, Q.; Loukas, G.; et al. A Secure Occupational Therapy Framework for Monitoring Cancer Patients Quality of Life. Sensors 2019, 19, 5258. [Google Scholar] [CrossRef] [Green Version]
- Boots, L.M.M.; de Vugt, M.E.; van Knippenberg, R.J.M.; Kempen, G.I.J.M.; Verhey, F. A Systematic Review of Internet-Based Supportive Interventions for Caregivers of Patients with Dementia. Int. J. Geriatr. Psych. 2013, 29, 331–344. [Google Scholar] [CrossRef]
- Carretero, S.; Stewart, J.; Centeno, C. Information and Communication Technologies for Informal Carers and Paid Assistants: Benefits from Micro-, Meso-, And Macro-Levels. Eur. J. Ageing. 2015, 12, 163–173. [Google Scholar] [CrossRef] [Green Version]
- Crosby, M.; Nachiappan; Pattanayak, P.; Verma, S.; Kalyanaraman, V. Blockchain technology: Beyond bitcoin. Appl. Innov. Rev. 2016, 2, 6–19. Available online: http://scet.berkeley.edu/wp-content/uploads/AIR-2016-Blockchain.pdf (accessed on 6 June 2020).
- Swan, M. Blockchain: Blueprint for a new economy, 1st ed.; McGovern, T., Ed.; O’Reilly Media: Sebastopol, CA, USA, 2015. [Google Scholar]
- Zhao, J.L.; Fan, S.; Yan, J. Overview of business innovations and research opportunities in blockchain and introduction to the special issue. Financ. Innov. 2016, 2, 28. [Google Scholar] [CrossRef] [Green Version]
- Casino, F.; Dasaklis, T.K.; Patsakis, C. A systematic literature review of blockchain-based applications: Current status, classification, and open issues. Telemat. Inform. 2019, 36, 55–81. [Google Scholar]
- Beninger, P.; Ibara, M.A. Pharmacovigilance and Biomedical Informatics: A Model for Future Development. Clin. Ther. 2016, 38, 2514–2525. [Google Scholar] [CrossRef] [Green Version]
- Sankar, L.S.; Sindhu, M.; Sethumadhavan, M. Survey of consensus protocols on blockchain applications. In Proceedings of the 2017 4th International Conference on Advanced Computing and Communication Systems (ICACCS), Coimbatore, India, 6–7 January 2017; pp. 1–5. [Google Scholar] [CrossRef]
- McGhin, T.; Choo, K.K.R.; Liu, C.Z.; He, D. Blockchain in healthcare applications: Research challenges and opportunities. J. Netw. Comput. Appl. 2019, 135, 62–75. [Google Scholar] [CrossRef]
- Azaria, A.; Ekblaw, A.; Vieira, T.; Lippman, A. MedRec: Using blockchain for medical data access and permission management. In Proceedings of the 2016 2nd International Conference on Open and Big Data (OBD), Vienna, Austria, 22–24 August 2016; pp. 25–30. [Google Scholar] [CrossRef]
- Yue, X.; Wang, H.; Jin, D.; Li, M.; Jiang, W. Healthcare Data Gateways: Found Healthcare Intelligence on Blockchain with Novel Privacy Risk Control. J. Med. Syst. 2016, 40, 218. [Google Scholar] [CrossRef]
- Yüksel, B.; Küpçü, A.; Özkasap, Ö. Research issues for privacy and security of electronic health services. Future Gener. Comput. Syst. 2017, 68, 1–13. [Google Scholar] [CrossRef]
- Griggs, K.N.; Ossipova, O.; Kohlios, C.P.; Baccarini, A.N.; Howson, E.A.; Hayajneh, T. Healthcare Blockchain System Using Smart Contracts for Secure Automated Remote Patient Monitoring. J. Med. Syst. 2018, 42, 1–7. [Google Scholar] [CrossRef]
- Xia, Q.; Sifah, E.B.; Asamoah, K.O.; Gao, J.; Du, X.; Guizani, M. MeDShare: Trust-Less Medical Data Sharing among Cloud Service Providers via Blockchain. IEEE Access 2017, 5, 14757–14767. [Google Scholar] [CrossRef]
- Abouelmehdi, K.; Beni-Hssane, A.; Khaloufi, H.; Saadi, M. Big data security and privacy in healthcare: A Review. Procedia Comput. Sci. 2017, 113, 73–80. [Google Scholar] [CrossRef]
- Small, A.; Wainwright, D. Privacy and security of electronic patient records – Tailoring multimethodology to explore the socio-political problems associated with Role Based Access Control systems. Eur. J. Oper. Res. 2018, 265, 344–360. [Google Scholar]
- Kshetri, N. Blockchain’s roles in strengthening cybersecurity and protecting privacy. Telecommun. Policy 2017, 41, 1027–1038. [Google Scholar] [CrossRef] [Green Version]
- Ramani, V.; Kumar, T.; Bracken, A.; Liyanage, M.; Ylianttila, M. Secure and Efficient Data Accessibility in Blockchain Based Healthcare Systems. In Proceedings of the 2018 IEEE Global Communications Conference (GLOBECOM), Abu Dhabi, UAE, 9–13 December 2018; pp. 206–212. [Google Scholar] [CrossRef] [Green Version]
- Khan, S.I.; Hoque, A.S.M.L. Privacy and security problems of national health data warehouse: A convenient solution for developing countries. In Proceedings of the 2016 International Conference on Networking Systems and Security (NSysS), Dhaka, Bangladesh, 7–9 January 2016; pp. 1–6. [Google Scholar] [CrossRef]
- Rajkomar, A.; Oren, E.; Chen, K.; Dai, A.M.; Hajaj, N.; Hardt, M.; Liu, P.J.; Liu, X.; Marcus, J.; Sun, M.; et al. Scalable and accurate deep learning with electronic health records. Npj Digital Med. 2018, 1, 1–10. [Google Scholar] [CrossRef]
- Esposito, C.; De Santis, A.; Tortora, G.; Chang, H.; Choo, K.K.R. Blockchain: A Panacea for Healthcare Cloud-Based Data Security and Privacy? IEEE Cloud Comput. 2018, 5, 31–37. [Google Scholar] [CrossRef]
- Dagher, G.G.; Mohler, J.; Milojkovic, M.; Marella, P.B. Ancile: Privacy-preserving framework for access control and interoperability of electronic health records using blockchain technology. Sustain. Cities Soc. 2018, 39, 283–297. [Google Scholar] [CrossRef]
- Ekblaw, A.; Azaria, A.; Halamka, J.D.; Lippman, A. A Case Study for Blockchain in Healthcare: “MedRec” prototype for electronic health records and medical research data. White Paper, reprinted from 2nd International Conference on Open & Big Data, 22–24 August 2016, 1–13. Available online: https://www.media.mit.edu/publications/medrec-whitepaper/ (accessed on 6 June 2020).
- Roehrs, A.; da Costa, C.A.; da Rosa Righi, R. OmniPHR: A distributed architecture model to integrate personal health records. J. Biomed. Inform. 2017, 71, 70–81. [Google Scholar] [CrossRef]
- Kotz, D.; Gunter, C.A.; Kumar, S.; Weiner, J.P. Privacy and Security in Mobile Health: A Research Agenda. Computer 2016, 49, 22–30. [Google Scholar] [CrossRef] [Green Version]
- Sahi, M.; Abbas, H.; Saleem, K.; Yang, X.; Derhab, A.; Orgun, M.; Iqbal, W.; Rashid, L.; Yaseen, A. Privacy preservation in e-healthcare environments: State of the art and future directions. IEEE Access 2018, 6, 464–478. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, T.; Li, K.; Zhang, J. Improved visual correlation analysis for multidimensional data. J. Visual Lang. Comput. 2017, 41, 121–132. [Google Scholar] [CrossRef]
- Cecil, J.; Gupta, A.; Pirela-Cruz, M.; Ramanathan, P. An IoMT based cyber training framework for orthopedic surgery using Next Generation Internet technologies. Inf. Med. Unlocked 2018, 12, 128–137. [Google Scholar] [CrossRef]
- Joyia, G.J.; Liaqat, R.M.; Farooq, A.; Rehman, S. Internet of Medical Things (IOMT): Applications, Benefits and Future Challenges in Healthcare Domain. J. Commun. 2017, 12, 240–247. [Google Scholar] [CrossRef]
- Pilkington, M. Can Blockchain Improve Healthcare Management? Consumer Medical Electronics and the IoMT. SSRN 2017, 1–13. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3025393 (accessed on 6 June 2020).
- Hoy, M.B. An introduction to the blockchain and its implications for libraries and medicine. Med. Ref. Serv. Q. 2017, 36, 273–279. [Google Scholar]
- Kuo, T.T.; Kim, H.E.; Ohno-Machado, L. Blockchain distributed ledger technologies for biomedical and health care applications. J. Am. Med. Inform. Assoc. 2017, 24, 1211–1220. [Google Scholar]
- Dubovitskaya, A.; Xu, Z.; Ryu, S.; Schumacher, M.; Wang, F. How blockchain could empower ehealth: An application for radiation oncology. Lect. Notes Comput. Sci. 2017, 10494, 3–6. [Google Scholar] [CrossRef]
- Medicalchain. 2018. Whitepaper 2.1. Available online: https://medicalchain.com/Medicalchain-Whitepaper-EN.pdf (accessed on 6 June 2020).
- Peterson, K.; Deeduvanu, R.; Kanjamala, P.; Boles, K. A blockchain-based approach to health information exchange networks. In Proc. NIST Workshop Blockchain Healthcare. 2016. Available online: https://pdfs.semanticscholar.org/c1b1/89c81b6fda71a471adec11cfe72f6067c1ad.pdf?_ga=2.151693625.186512466.1597711686-512884126.1594177302 (accessed on 6 June 2020).
- Ahram, T.; Sargolzaei, A.; Sargolzaei, S.; Daniels, J.; Amaba, B. Blockchain technology innovations. In Proceedings of the 2017 IEEE Technology and Engineering Management Society Conference (TEMSCON), Santa Clara, CA, USA, 8–10 June 2017; pp. 137–141. [Google Scholar] [CrossRef]
- Al Omar, A.; Rahman, M.S.; Basu, A.; Kiyomoto, S. MediBchain: A blockchain based privacy preserving platform for healthcare data. In Proceedings of the 10th International Conference on Security, Privacy and Anonymity in Computation, Communication and Storage, Guangzhou, China, 12–15 December 2017; pp. 534–543. [Google Scholar] [CrossRef]
- Borioli, G.S.; Couturier, J. How blockchain technology can improve the outcomes of clinical trials. Br. J. Health Care Manag. 2018, 24, 156–162. [Google Scholar]
- Mamoshina, P.; Ojomoko, L.; Yanovich, Y.; Ostrovski, A.; Botezatu, A.; Prikhodko, P.; Izumchenko, E.; Aliper, A.; Romantsov, K.; Zhebrak, A.; et al. Converging blockchain and next-generation artificial intelligence technologies to decentralize and accelerate biomedical research and healthcare. Oncotarget 2018, 9, 5665–5690. [Google Scholar]
- Lee, S.H.; Yang, C.S. Fingernail analysis management system using microscopy sensor and blockchain technology. Int. J. Distrib. Sens. Netw. 2018, 14, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Shae, Z.; Tsai, J.J.P. On the Design of a Blockchain Platform for Clinical Trial and Precision. In Proceedings of the 2017 IEEE 37th International Conference on Distributed Computing Systems (ICDCS), Atlanta, GA, USA, 5–8 June 2017; pp. 1972–1980. [Google Scholar] [CrossRef]
- Frentrup, M.; Theuvsen, L. Transparency in supply chains: Is trust a limiting factor? Presented at the 99th EAAE Seminar Trust and Risk in Business Networks, Bonn, Germany, 8–10 February 2006; Available online: https://www.semanticscholar.org/paper/Transparency-in-supply-chains%3A-is-trust-a-limiting-Frentrup-Theuvsen/8fa45abcce7d8231c756af48810c6c797fea1f2a (accessed on 6 June 2020).
- Weissgerber, T.L.; Milic, N.M.; Winham, S.J.; Garovic, V.D. Beyond bar and line graphs: Time for a new data presentation paradigm. PLoS Biol. 2015, 13, 1–10. [Google Scholar] [CrossRef]
- Weissgerber, T.L.; Garovic, V.D.; Savic, M.; Winham, S.J.; Milic, N.M. From Static to Interactive: Transforming Data Visualization to Improve Transparency. PLoS Biol. 2016, 14, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Weiner, J.; Balijepally, V.; Tanniru, M. Integrating Strategic to Operational Decision-Making using Data-Driven Dashboard Implementation: The Case of St. Joseph Mercy Oakland Hospital. J. Healthc. Manag. 2015, 60, 319–331. [Google Scholar] [CrossRef]
- Selig, W.J.; Johannes, J.D. Reasoning visualization in expert systems-the applicability of algorithm animation techniques. In Proceedings of the 3rd international conference on Industrial and engineering applications of artificial intelligence and expert systems, New York, NY, USA, 15–18 July 1990; pp. 457–466. [Google Scholar] [CrossRef]
- Trainer, E.H. Supporting Trust in Globally Distributed Software Teams: The Impact of Visualized Collaborative Traces on Perceived Trustworthiness. Doctoral Dissertation, University of California, La Jolla, CA, USA, 2012. [Google Scholar]
- Perlmutter, L.; Kernfeld, E.; Cakmak, M. Situated language understanding with human-like and visualization-based transparency. In Proceedings of the Robotics: Science and Systems Conference, Ann Arbor, MI, USA, 18–22 June 2016; pp. 1–10. [Google Scholar] [CrossRef]
- Liu, Z.; Stasko, J. Mental Models, Visual Reasoning and Interaction in Information Visualization: A Top-down Perspective. IEEE Trans. Vis. Comput. Graph. 2010, 16, 999–1008. [Google Scholar] [CrossRef] [Green Version]
- Hebert, C.; Di Cerbo, F. Secure blockchain in the enterprise: A methodology. Perv. Mob. Comput. 2019, 59, 101038. [Google Scholar] [CrossRef]
- Yaraghi, N. Who should profit from the sale of patient data? The Brookings Institution. Available online: https://www.brookings.edu/blog/techtank/2018/11/19/who-should-profit-from-the-sale-of-patient-data/ (accessed on 6 June 2020).
- Hertzog, E.; Benartzi, G.; Benartzi, G.; Bancor Protocol. Continuous Liquidity for Cryptographic Tokens through their Smart Contracts. Available online: https://storage.googleapis.com/website-bancor/2018/04/01ba8253-bancor_protocol_whitepaper_en.pdf (accessed on 6 June 2020).
- A Blockchain Platform for the Enterprise. Hyperledger. Available online: https://hyperledger-fabric.readthedocs.io/en/release-2.0/ (accessed on 15 May 2020).
- Josefsson, S. The Base16, Base32, and Base64 Data Encodings; RFC 4648, The Internet Society. 2006. Available online: https://www.semanticscholar.org/paper/The-Base16%2C-Base32%2C-and-Base64-Data-Encodings-Josefsson/2718f599c9bbb96aecd81180167d10dcf9c65c47 (accessed on 6 June 2020).
- Van Landuyt, D.; Sion, L.; Vandeloo, E.; Joosen, W. On the Applicability of Security and Privacy Threat Modeling for Blockchain Applications. In Computer Security; Katsikas, S., Cuppens, F., Cuppens, N., Lambrinoudakis, C., Kalloniatis, C., Mylopoulos, J., Antón, A., Gritzalis, S., Pallas, F., Pohle, J., et al., Eds.; Springer: Cham, Switzerland, 2020; Volume 11980, pp. 195–203. [Google Scholar] [CrossRef]
- AnaReyna, A.; Martín, C.; Chen, J.; Soler, E.; Díaz, M. On blockchain and its integration with IoT–Challenges and opportunities. Future Gener. Comput. Syst. 2018, 88, 173–190. [Google Scholar] [CrossRef]
- Zheng, Z.; Xie, S. Blockchain challenges and opportunities: A Survey. Int. J. Web Grid. Serv. 2018, 14, 352–375. [Google Scholar] [CrossRef]
- Almashaqbeh, G.; Bishop, A.; Cappos, J. ABC: A Cryptocurrency-Focused Threat Modeling Framework. In Proceedings of the IEEE INFOCOM 2019-IEEE Conference on Computer Communications Workshops (INFOCOM WKSHPS), Paris, France, 29 April–2 May 2019; pp. 859–864. [Google Scholar] [CrossRef] [Green Version]








© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peral, J.; Gallego, E.; Gil, D.; Tanniru, M.; Khambekar, P. Using Visualization to Build Transparency in a Healthcare Blockchain Application. Sustainability 2020, 12, 6768. https://doi.org/10.3390/su12176768
Peral J, Gallego E, Gil D, Tanniru M, Khambekar P. Using Visualization to Build Transparency in a Healthcare Blockchain Application. Sustainability. 2020; 12(17):6768. https://doi.org/10.3390/su12176768
Chicago/Turabian StylePeral, Jesús, Eduardo Gallego, David Gil, Mohan Tanniru, and Prashant Khambekar. 2020. "Using Visualization to Build Transparency in a Healthcare Blockchain Application" Sustainability 12, no. 17: 6768. https://doi.org/10.3390/su12176768
APA StylePeral, J., Gallego, E., Gil, D., Tanniru, M., & Khambekar, P. (2020). Using Visualization to Build Transparency in a Healthcare Blockchain Application. Sustainability, 12(17), 6768. https://doi.org/10.3390/su12176768





